Are bloody noses common during pregnancy
What causes nosebleeds in pregnancy, and tips to manage them | Your Pregnancy Matters
Pregnant women are more likely to get nosebleeds due to increased blood volume, which may cause vessels in the nose to rupture.Pregnancy is full of quirky side effects – including nosebleeds. One in five patients get nosebleeds during pregnancy (epistaxis), compared with 6% of women who get them when not pregnant.
Over the course of pregnancy, your total blood volume doubles to support the growing baby. To accommodate this extra blood, the blood vessels in your body dilate. The pressure of the extra blood can sometimes cause the more fragile vessels to rupture and bleed more easily.
Your nose is rich in tiny blood vessels that can get dried out from normal breathing, which can lead to breakage and bleeding. For most pregnant patients, the occasional minor nosebleed is no cause for alarm. It’s mostly just annoying.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist from UT Southwestern's Otolaryngology Department, to talk about what causes nosebleeds during pregnancy, how women can prevent them, and how to stop them when they do occur.
Colds, medications, and unruly sinuses
Dr. Ashleigh HaldermanEven when you aren't pregnant, you're more likely to get a nosebleed with a cold, sinus infection, or allergies. But approximately 20% of women experience pregnancy rhinitis – inflammation and swelling of the mucous membranes in the nose.
Pregnancy rhinitis causes congestion, postnasal drip, and runny nose. And when you're constantly blowing your nose, you're more susceptible to having a bloody nose.
Certain medical conditions such as high blood pressure or clotting disorders can cause nosebleeds as well.
You may also get a nosebleed if the membranes in your nose dry out and crack due to cold weather, dry air, or intense air conditioning.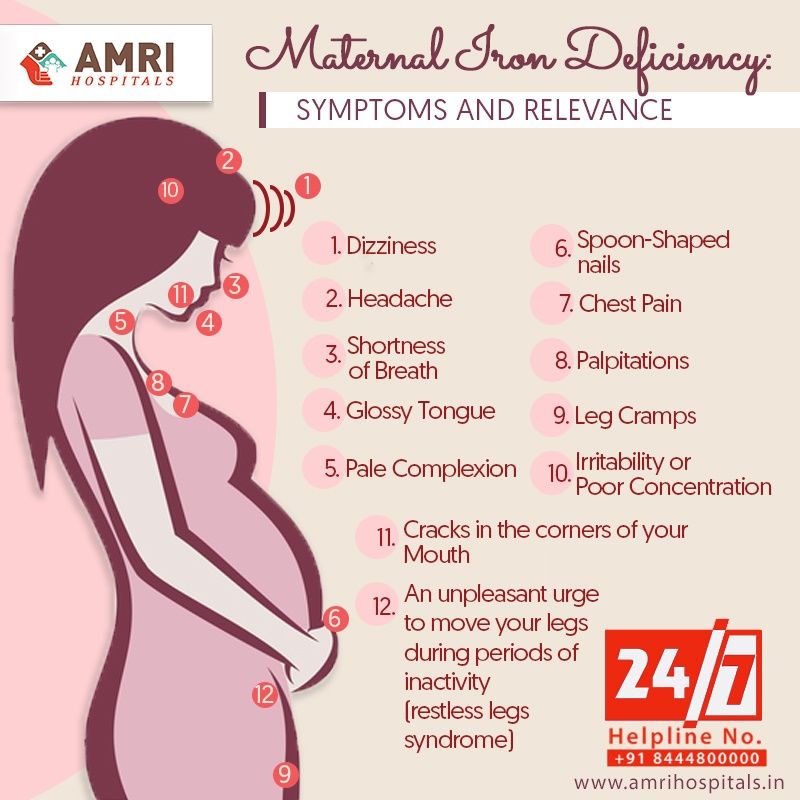
Pregnancy tumor: A rare cause of nosebleeds
Also known as a pyogenic granuloma, a pregnancy tumor is a noncancerous, rapidly growing mass of capillary blood vessels that bleeds easily. Research suggests the masses form due to the influx of hormones during pregnancy.
Approximately 5% of pregnant women develop pregnancy tumors, which typically form in the gums between the teeth but can also form in the nose. The masses can appear anywhere on the body and generally disappear after the baby is born.
Treatment usually consists of either a medicated gel or nasal spray, which helps control bleeding. Some women need to have the tumor removed if it is causing breathing problems or excessive nosebleeds. The exact procedure to remove the tumor depends on where the tumor is located. For pregnancy tumors of the nose, most can be removed endoscopically without any external incisions or stitches.
Related reading: 5 weird pregnancy symptoms you might not know about
How can I prevent nosebleeds during pregnancy?
While it’s not possible to prevent all nosebleeds, there are few things you can do to avoid irritating the sensitive blood vessels in your nose.
● Moisturize the inside of your nose: Use a bit of saline nasal gel to lubricate dry or irritated nasal passages.
● Use a humidifier: Because dry air increases the risk of nosebleeds, adding a little moisture to the air can do wonders.
● Drink plenty of fluids: This keeps your mucous membranes well hydrated and less likely to dry out and crack.
● Treat colds and allergies: Talk to your doctor about which over-the-counter medications may be best.
Be especially gentle after a nosebleed. Your nose needs to heal, so don’t blow it too hard or stuff tissues in the nostrils, which can prolong bleeding.
How to stop a nosebleed and when to see your doctor
If you do get a nosebleed during pregnancy (or any other time):
● Sit or stand up to keep your head higher than your heart
● Lean forward slightly to stop the blood from running down the back of your throat into your mouth
● Pinch both nostrils and maintain pressure for 10 to 15 minutes
● To help constrict the blood vessels and slow bleeding, you also can apply a cold pack or ice over the bridge of your nose or use a nasal spray such as Afrin before pinching the nostrils together
Call your health care provider if you experience more than a couple nosebleeds during pregnancy, or if:
● Bleeding doesn’t stop after 30 minutes
● Blood flow is heavy
● You have trouble breathing
● You become lightheaded or disoriented
Pregnancy can cause strange things to happen to your body. While nosebleeds generally are nothing to be overly concerned about, talk to your doctor if you are worried. We're always available to help you feel more comfortable during pregnancy.
While nosebleeds generally are nothing to be overly concerned about, talk to your doctor if you are worried. We're always available to help you feel more comfortable during pregnancy.
To visit with an Ob/Gyn, call 214-645-8300 or request an appointment online.
Nosebleeds during pregnancy | Pregnancy Birth and Baby
Nosebleeds during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Nosebleeds during pregnancy are fairly common. Although they can be alarming, in most cases there's no need to worry and you should be able to treat a bleeding nose yourself.
Why are nosebleeds common during pregnancy?
During your first trimester the amount of blood circulating in your body increases and your heart works harder. This means that the lining of your nasal passage (inside your nose) also receives more blood. You have tiny blood vessels inside your nose so the increased blood volume can sometimes damage those blood vessels and cause them to burst, resulting in a nosebleed.
This means that the lining of your nasal passage (inside your nose) also receives more blood. You have tiny blood vessels inside your nose so the increased blood volume can sometimes damage those blood vessels and cause them to burst, resulting in a nosebleed.
Changes in your hormones during pregnancy can also contribute to nosebleeds.
These changes can make your nose feel congested (stuffy) and it might get more blocked up than usual. Your gums may also feel swollen and may bleed.
A nosebleed may last for a few seconds or a few minutes, and can flow from one or both nostrils. The blood flow can be light or quite heavy. If a nosebleed happens at night, while you’re sleeping, you may wake up feeling the blood going down the back of your throat before you sit up. It will then come out of your nose.
Are nosebleeds during pregnancy a cause for concern?
Nosebleeds can give you a fright or be a nuisance, but as long as you don’t lose a lot of blood, they are generally nothing to be worried about. In most cases, a nosebleed won’t harm you or your baby.
In most cases, a nosebleed won’t harm you or your baby.
How do I stop a nosebleed if I have one?
- Sitting or standing, keep your head upright. This reduces the pressure in the blood vessels inside your nose and will help to slow down the bleeding.
- Pinch the soft part of your nose, underneath the bony ridge, between your thumb and forefinger. Once you have done this, the two sides of your nose should be pressed together.
- Keep pinching, without releasing, for 10 minutes.
- If your nose is bleeding a lot, you may want to lean slightly forward and breathe through your mouth so the blood runs out of your nose, rather than down the back of your throat.
- Spit out any blood that is in your mouth.
- You may also want to suck an ice cube or put an icepack on the back of your neck or forehead, or the bony part of your nose.
- After 10 minutes, gently release your pinch to see if the bleeding has stopped.
- If your nose is still bleeding, try this procedure again for another 10 minutes.

How can I avoid a nose bleed?
If you are blowing your nose, do so gently and try to avoid large sneezes. You should also avoid picking your nose. You could be more likely to get nosebleeds in winter months when the air is dryer, so you may like to use a dehumidifier in your home to moisten the air.
If you’ve recently had a nosebleed:
- Sneeze with your mouth open.
- Try to avoid bending down or vigorously exercising for at least 12 hours afterwards.
- Avoid hitting your nose on anything.
When should I see a doctor?
Let your doctor know straight away if your nosebleed happens after bumping your head.
You should also contact your doctor if:
- you have high blood pressure
- you have taken the steps above and your nosebleed hasn’t stopped after 20 minutes
- you have trouble breathing through your mouth
- there seems to be a large amount of blood
- you are getting nosebleeds frequently
- you have swallowed a lot of blood and vomited
- you have a fever or chill
For more information, or to discuss any concerns you might have about nosebleeds, call Pregnancy, Birth and Baby on 1800 882 436.
Sources:
Healthy WA (Healthy WA - Nose bleeds), Mater Mothers Hospital (Pregnancy information for women and families), NHS Choices (Nosebleeds in pregnancy), Raising Children Network (15 weeks pregnant), St John Ambulance Australia (First aid tip: nosebleeds)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2021
Back To Top
Need more information?
Nosebleeds - MyDr.com.au
What causes nosebleeds? How can I prevent them? What first aid measures can I use to stop a nosebleed? Find out here.
Read more on myDr website
Nosebleeds in children: what to do | Raising Children Network
Nosebleeds in children are very common. Nosebleed treatment starts with staying calm and applying pressure to the nose. Nosebleeds aren’t usually serious.
Nosebleed treatment starts with staying calm and applying pressure to the nose. Nosebleeds aren’t usually serious.
Read more on raisingchildren.net.au website
Nosebleeds - Better Health Channel
Bleeding from the nose is common in children and is usually not severe or serious.
Read more on Better Health Channel website
Nose bleeds
Nose bleeds can occur when the blood vessels or the lining or the nose become damaged.
Read more on WA Health website
Pale skin: babies, children & teens | Raising Children Network
Pale skin is usually nothing to worry about. But you might sometimes need to see your doctor if your child’s skin looks pale. This article explains.
This article explains.
Read more on raisingchildren.net.au website
Using your allergy nasal spray correctly - National Asthma Council Australia
Many people with asthma also use allergy nasal sprays for their hay fever. Using your nasal spray properly is important. With the right tech
Read more on National Asthma Council Australia website
Bruises & bruising in children & teens | Raising Children Network
If your child falls over or bumps himself, he might get bruises. Bruising is when blood vessels are damaged and bleed into the skin. First aid can help.
Read more on raisingchildren.net.au website
Pregnancy health problems & complications | Raising Children Network
Many pregnancy health problems are mild, but always call your doctor if you’re worried about symptoms. A healthy lifestyle can help you avoid health problems.
A healthy lifestyle can help you avoid health problems.
Read more on raisingchildren.net.au website
Childhood acute lymphoblastic leukaemia (ALL) - Leukaemia Foundation
Childhood acute lymphoblastic leukaemia (ALL) Listen What is childhood acute lymphoblastic leukaemia? Acute lymphoblastic leukaemia (ALL) is a type of cancer that affects immature lymphocytes developing in the bone marrow
Read more on Leukaemia Foundation website
Childhood acute myeloid leukaemia (AML) - Leukaemia Foundation
Childhood acute myeloid leukaemia (AML) Listen What is childhood AML? Acute myeloid leukaemia (AML) is a type of cancer that affects the blood and bone marrow
Read more on Leukaemia Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy rhinitis - why does it occur and how to treat it?
Rhinitis of pregnant women is not dangerous, but worsens the quality of life of a woman during pregnancy.Article rating
3.26 (Votes: 38)
Contents
- How long does pregnancy rhinitis occur and how long does it last?
- Symptoms of pregnancy rhinitis
- Causes of pregnancy rhinitis
- How to distinguish the symptoms of rhinitis during pregnancy from other pathologies?
- Treatment of rhinitis of pregnant women
- General recommendations for pregnant women who have symptoms of rhinitis
- Drugs for the treatment of rhinitis
Rhinitis of pregnancy (nasal obstruction) is a common pathology that occurs in about 30% of expectant mothers. Manifested by a typical triad of symptoms: nasal congestion, difficulty breathing, the presence of mucous secretions. By itself, it is not dangerous, but worsens the quality of life of a woman during pregnancy. The difficulty of stopping the pathology and relieving symptoms lies in the fact that during pregnancy there are restrictions on the use of a number of physiotherapeutic methods and drugs.
Manifested by a typical triad of symptoms: nasal congestion, difficulty breathing, the presence of mucous secretions. By itself, it is not dangerous, but worsens the quality of life of a woman during pregnancy. The difficulty of stopping the pathology and relieving symptoms lies in the fact that during pregnancy there are restrictions on the use of a number of physiotherapeutic methods and drugs.
When does pregnancy rhinitis occur and how long does it last?
Most often, pathology occurs:
- up to and including the 20th week of pregnancy - in this case, rhinitis usually resolves on its own (after about a month or two) and does not manifest itself in the later stages;
- after the 20th week of pregnancy - this condition can continue until childbirth and after them (after 2-3 weeks).
If the symptoms last longer than two months and are not relieved by any independent action (vasoconstrictor sprays are prohibited!), then the cause may be hiding in a chronic disease.
Symptoms of pregnancy rhinitis
- Difficult nasal breathing, nasal congestion;
- Nasal discomfort, sneezing;
- Presence of clear mucous discharge;
- Feeling of constriction in the region of the nose and sinuses;
- Mild headaches.
Difficulty in nasal breathing in the mother leads to sleep disturbance and hypoxia, which is also felt by the fetus.
Causes of pregnancy rhinitis
The pathogenesis of the disease is still a controversial issue. Most doctors are inclined to believe that it is of a hormonal nature and is associated with an increased level of estrogen and acetylcholine in the blood serum (as a result), which leads to hyperemia of the nasal mucosa and swelling. The concentration of estradiol, estrone, estriol in the bloodstream of pregnant women increases, in some future mothers, for this reason, the shape of the nose may change, it may increase in size.
There is evidence that pregnant women with symptoms of vasomotor rhinitis have elevated serum placental hormone levels. Another reason that can cause long-term nasal obstruction is the tone of smooth muscle cells under the influence of the inhibitory action of the steroid hormone progesterone. It causes fluid retention in the body and has such a side effect on the nasal mucosa.
Another reason that can cause long-term nasal obstruction is the tone of smooth muscle cells under the influence of the inhibitory action of the steroid hormone progesterone. It causes fluid retention in the body and has such a side effect on the nasal mucosa.
Histochemical studies have shown that nasal congestion may occur due to plethora due to hyperactivity of the parasympathetic nervous system in pregnant women.
How to distinguish the symptoms of pregnancy rhinitis from other pathologies?
Symptoms of rhinitis during pregnancy are really similar to manifestations of other diseases, for example, viral infections, sinusitis. It is difficult for a future mother to distinguish a pathology by external signs, therefore a doctor's consultation is necessary. Our clinic employs specialists with extensive experience who will quickly diagnose and prescribe treatment.
If the symptoms are accompanied by a sore throat, fever, then this indicates the presence of a bacterial and/or viral infection or other inflammatory process.
With sinusitis, mucous discharge may have a yellowish or greenish tint. When pressing in the area of the maxillary and frontal sinuses, there are painful sensations, when the head is tilted, the pain may intensify. Also, sinusitis often causes an increase in temperature, while with nasal obstruction, such symptoms are not observed.
Sometimes rhinitis of pregnancy is confused with allergic rhinitis, which may worsen, there may be sensitization to allergens to which patients have not previously reported sensitivity.
Treatment of pregnancy rhinitis
In our clinic, a thorough diagnosis is carried out in order to exclude diseases similar to rhinitis in terms of symptoms. After the examination, individual treatment is prescribed depending on the severity, severity and indications.
Treatment is complicated by the fact that many drugs can cause contraction of the myometrium and fetal circulation or vasoconstriction with impaired placental function. Therefore, a doctor should prescribe drug therapy, you can not use drugs on your own - they can cause a violation of the development of the fetus.
Therefore, a doctor should prescribe drug therapy, you can not use drugs on your own - they can cause a violation of the development of the fetus.
General advice for pregnant women with symptoms of rhinitis
- Washing the nose with mild saline solution (2 teaspoons of sea salt per glass of water). Salt solution improves the discharge of nasal mucus and reduces the feeling of congestion.
- Nasal douches (nose washers) are very helpful. You can use regular saline for them.
- Ventilate the room before going to bed, use humidifiers. Dry air can exacerbate unpleasant symptoms.
- Use a high pillow (or multiple pillows) to sleep with your head well above your torso.
- Walking in the fresh air before going to bed is useful.
- Do morning exercises and breathing exercises several times a day to reduce the symptoms of hypoxia.
- Do not wear perfume and stay away from smokers.
Do not use vasoconstrictor nasal drops during pregnancy as they may cause vasomotor rhinitis.
Preparations for the treatment of rhinitis
Preparations for use during pregnancy are selected with great care and individually. Pregnant women are not given oral systemic corticosteroids, although their effect on the fetus is not fully understood. In some cases, the doctor prescribes corticosteroids in the form of aerosols. Oral antihistamines are also not prescribed due to the increased risk of embryopathies. The choice of physiotherapy is also limited, because most methods negatively affect the development of the fetus.
If you suffer from rhinitis, headaches or other unpleasant symptoms, we advise you to see a doctor immediately. Timely treatment is the key to the quality of life of the mother, which is very important for bearing the fetus. And also allows you not to miss other more serious diseases that can adversely affect the health of the mother and child.
Important! Do not use drugs that were prescribed to you by a doctor before pregnancy, or drugs prescribed to someone else.
Rhinitis during pregnancy usually does not pose a threat to either the fetus or the mother, but improper treatment can lead to unpredictable consequences.
Seeing a doctor early can help keep you healthy.
Don't delay treatment, call now. We work around the clock in Moscow.
tel.: 8 (499) 501-15-53 (24 hours)
Rhinitis in pregnancy
Otorhinolaryngologist, surgeon at GMS Clinic Oleg Abramov talks in his article about rhinitis of pregnancy (hereinafter referred to as RH).
It was no coincidence that I chose this topic after a series of publications on the social network about allergic rhinitis (hereinafter referred to as AR), as recent studies note that although the cause of RB is not completely clear, the combination of AR, which is especially poorly controlled together with RB, can lead to severe nasal congestion, to insufficient oxygen supply, and, as a result, to increased fatigue, irritability, frequent SARS, sleep disturbance, which can certainly affect the development of the fetus. Moreover, the presence of AR is associated with snoring in women during pregnancy, and together they can provoke the development of sleep apnea syndrome (stopping breathing during sleep), which leads to arterial hypertension, preeclampsia, slowed fetal growth and low Apgar scores. Therefore, the relevance of this problem is only growing.
Moreover, the presence of AR is associated with snoring in women during pregnancy, and together they can provoke the development of sleep apnea syndrome (stopping breathing during sleep), which leads to arterial hypertension, preeclampsia, slowed fetal growth and low Apgar scores. Therefore, the relevance of this problem is only growing.
Definition and concept
Rhinitis of pregnancy is a disease accompanied by nasal congestion and discharge, periodic sneezing without signs of inflammation, allergies, or other causes. This condition can occur in any trimester of pregnancy and usually resolves within two weeks after delivery.
Occurrence
Nasal congestion is a very common problem during pregnancy (occurs in about 65% of cases), which can occur due to various reasons. RB, according to various sources, occurs in 9-40% of cases, and in one of the last observations there is an increasing incidence, that is, most of all RB is observed in the 3rd trimester - 38. 9%, including those who did not have problems in the 1st and 2nd trimesters.
9%, including those who did not have problems in the 1st and 2nd trimesters.
Causes and mechanism of occurrence
The mechanism of occurrence is not fully understood, and it is believed that RB occurs due to hormonal changes, in particular, under the influence of progesterone, estrogen, hCG and other hormones, the concentration of which gradually increases during pregnancy. Some authors believe that the occurrence of RB is associated with the worsening of concomitant AR. Some studies show that hormonal action leads to relaxation of the smooth muscles that make up the vessel wall of the nasal mucosa, resulting in nasal congestion. Such findings are supported by other studies that show that oral contraceptives cause similar effects in the nasal cavity (but not in everyone). Other studies show that elevated body mass index, overweight, multiple pregnancies provoke or aggravate RB.
Progression and potential risks
RB, in the absence of adequate treatment, has an adverse effect on the course of pregnancy and can lead to the development of rhinosinusitis, which is especially difficult to tolerate in the 3rd trimester. On the other hand, pregnancy is a special period in a woman's life, during which a large number of drugs are prohibited, and ENT pathologies, these restrictions have not been spared either. Very often I hear at the reception: "Doctor, I'm pregnant and I've been suffering with my nose all this time, but the doctors tell me - there's nothing to be done, I need to endure it." On the other hand, the opposite situation is often observed: “Doctor, I am pregnant and I cannot live without vasoconstrictor drops.” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all.
On the other hand, pregnancy is a special period in a woman's life, during which a large number of drugs are prohibited, and ENT pathologies, these restrictions have not been spared either. Very often I hear at the reception: "Doctor, I'm pregnant and I've been suffering with my nose all this time, but the doctors tell me - there's nothing to be done, I need to endure it." On the other hand, the opposite situation is often observed: “Doctor, I am pregnant and I cannot live without vasoconstrictor drops.” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all.
Diagnostics
At the moment, there is no specific test to confirm or exclude RB. The diagnosis is made on the basis of the patient's complaints and the exclusion of other pathologies of the nasal cavity.
Choice of therapeutic tactics
Saline solutions
Before considering more serious medications, we should start with our favorite saline solutions. It should be noted that we are not talking about ordinary saline solutions, but hypertonic saline solutions (with an increased salt content, approximately 19-23 g/l). Such sprays are sold in all pharmacies, but they will not be sold to you right away (you need to ask). Several studies have noted significant efficacy in reducing congestion when used in AR, chronic rhinosinusitis. Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
It should be noted that we are not talking about ordinary saline solutions, but hypertonic saline solutions (with an increased salt content, approximately 19-23 g/l). Such sprays are sold in all pharmacies, but they will not be sold to you right away (you need to ask). Several studies have noted significant efficacy in reducing congestion when used in AR, chronic rhinosinusitis. Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
Doctor, not helping...
As is known from past publications, intranasal glucocorticosteroids (iGCS) are the most effective in the treatment of AR today. They have proven efficacy in reducing nasal congestion, as well as nasal itching and watery eyes, and allow adequate control of symptoms. But, given their hormonal effect and possible harmful effects on the fetus, there are certain risks in their use. It should also be noted that at the moment there are no studies that provide reliable data confirming the danger of their use. Modern ICS — mometasone (nasonex, desrinit) and fluticasone (avamys, flixonase) has a very low systemic bioavailability, less than 1% and proven efficacy, thus can be considered as initial therapy for RB. The studies did not reveal a statistically significant relationship between the development of fetal defects and the use of these drugs.
It should also be noted that at the moment there are no studies that provide reliable data confirming the danger of their use. Modern ICS — mometasone (nasonex, desrinit) and fluticasone (avamys, flixonase) has a very low systemic bioavailability, less than 1% and proven efficacy, thus can be considered as initial therapy for RB. The studies did not reveal a statistically significant relationship between the development of fetal defects and the use of these drugs.
Who are the FDA in the US and why is everyone listening to them?
Everything is very simple (it’s a pity that everything is not so simple with us). I copy the explanation from Wikipedia: “An agency of the US Department of Health and Human Services, one of the federal executive departments. The department is engaged in quality control of food products, medicines, cosmetics, tobacco products and some other categories of goods, and also monitors compliance with legislation and standards in this area.
Budesonide (Tafen Nasal) is classified as category B according to the FDA's classification for drug effects on the fetus, which means that there is evidence that the drug is safe to use during pregnancy. The bioavailability of budesonide is 33%. This drug has moved from group C to group B, thanks to several high-quality studies in Sweden since the beginning of the 21st century, proving its safety.
The bioavailability of budesonide is 33%. This drug has moved from group C to group B, thanks to several high-quality studies in Sweden since the beginning of the 21st century, proving its safety.
Also, according to the current recommendations of the American Academy of Allergology and Immunology (AAAAI), ICS are considered safe and effective in the treatment of rhinitis and rhinosinusitis during pregnancy. But at the same time, there is no indication of specific drugs. Other competent medical associations also do not give any recommendations in terms of choosing a drug. Therefore, summing up all of the above, and also according to the latest review, mometasone, fluticasone, budesonide can be considered as safe and effective agents in the treatment of RB. It should also be noted that an experienced ENT doctor should be involved in prescribing the drug and managing the patient, since these drugs are sold without a prescription in the Russian Federation; we strongly recommend not to self-medicate.