Placental site scab
Postpartum symptoms: when to call us - Oula
Go Back
As you enter your “4th trimester,” you may notice changes in your body as you heal. We’ll be checking in with you a week after your birth, and again a few weeks later. Though you will be busy caring for your new baby, we encourage you to check in with yourself and monitor how you are feeling physically and emotionally. We are here to help you navigate this phase and answer your questions and, in particular, please reach out to if you are experiencing any of the below warning signs.
Postpartum bleeding
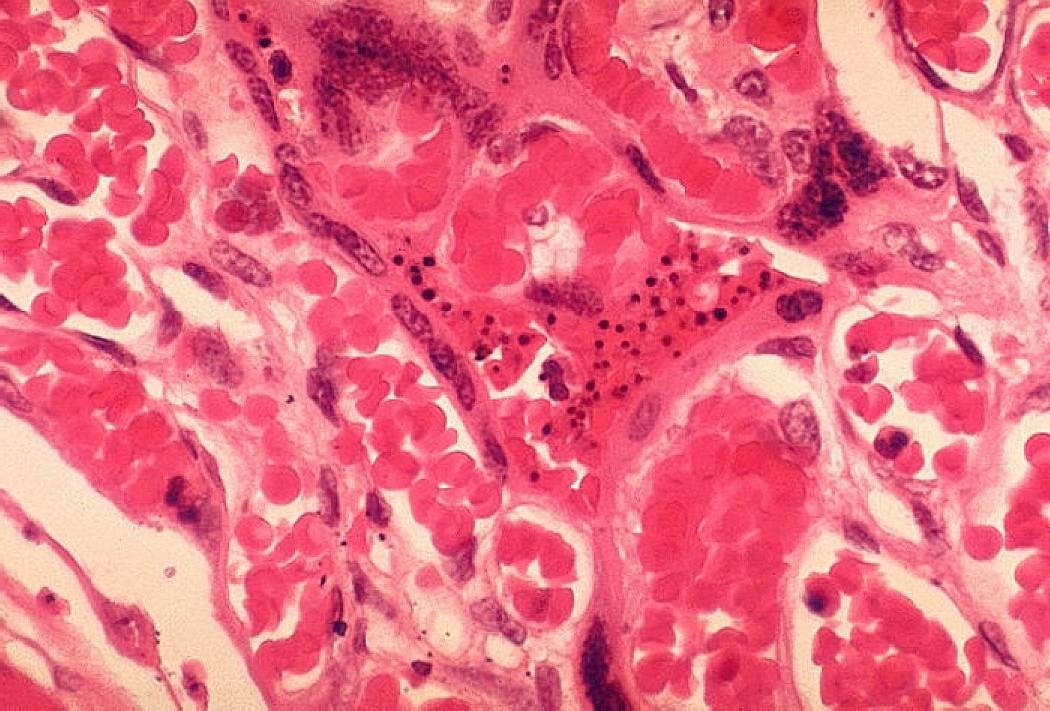
You can expect to have vaginal bleeding for about six weeks after the birth of your baby. The bleeding will taper from dark red to brown to yellow. In the first few days after the birth, you might notice that you pass some small blood clots. As you recover, you will notice that the bleeding might get heavier if you’ve had a busy day. This is normal. This bleeding is called “lochia. ” Lochia has an earthy smell.
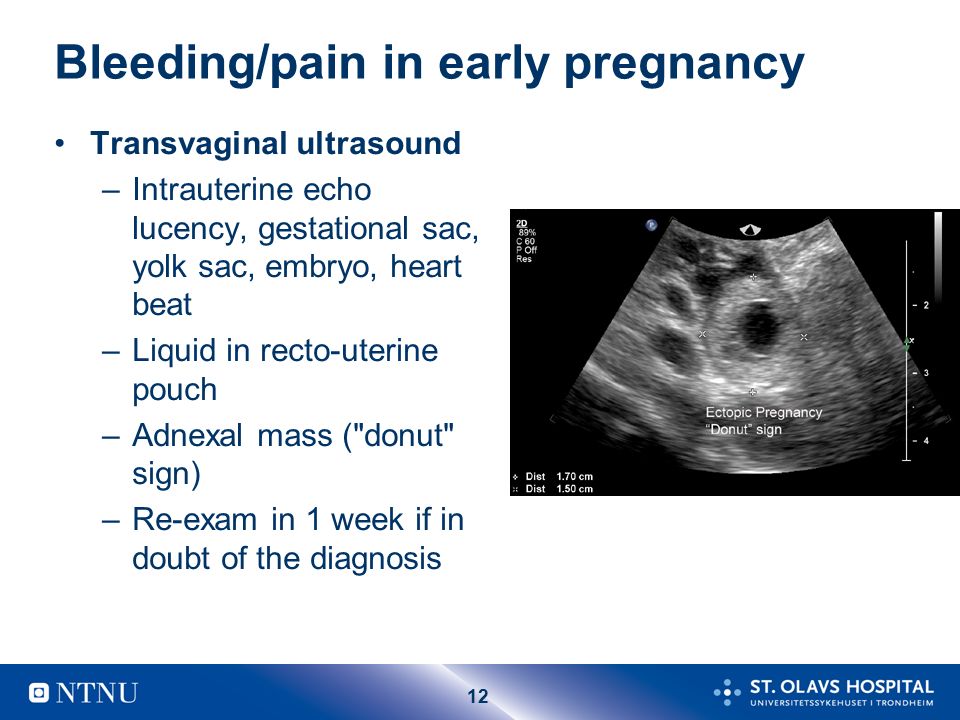
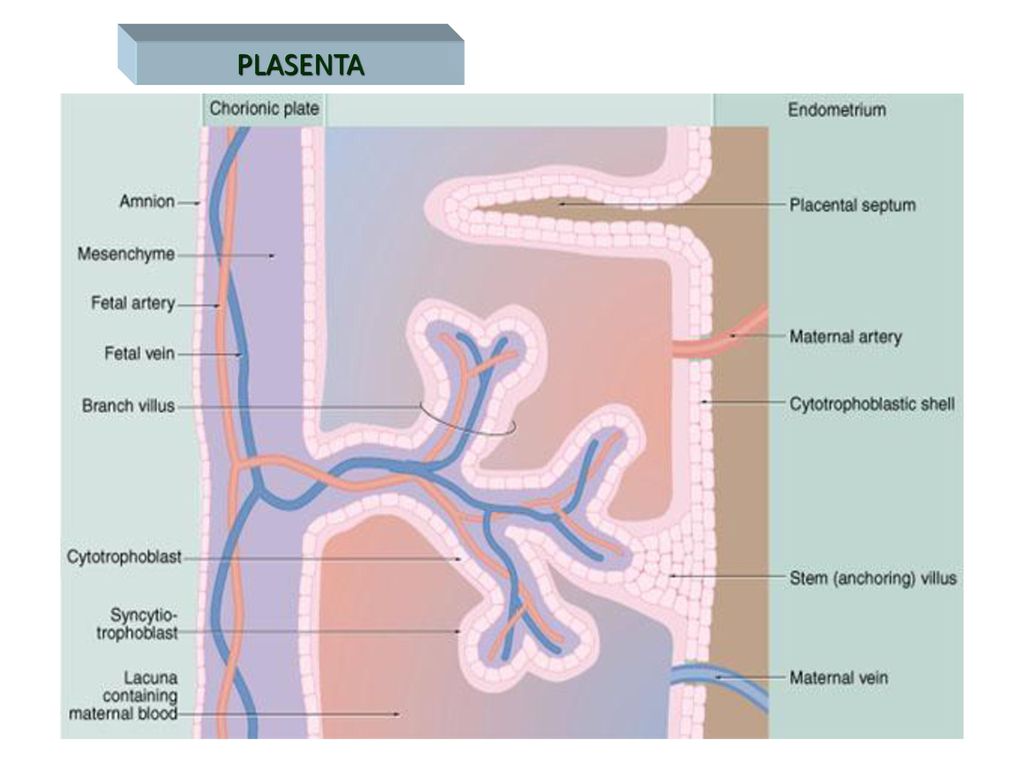
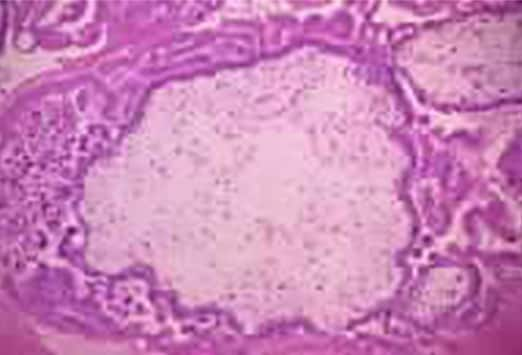
It is also normal to notice a return to bright red bleeding at about 7 to 10 days after the birth, this is called eschar. Eschar happens when the scab over the placental site breaks down – in much the same way that a scab on your knee might bleed if you disrupted it, the scab in your placenta can cause a day or two of red bleeding a week or two after the birth.
When to call us: If you notice that your bleeding is heavy, bright red, and soaking through more than two pads per hour, or if you are passing clots the size of a lemon or larger.
Fever or Infection
Fever can be a sign of infection. Other signs of uterine infection include severe abdominal pain or foul-smelling discharge.
When to call us: If you have a fever higher than 100.4F, or severe pain and foul-smelling discharge.
Cramping
Cramping in your uterus is normal after birth. You might notice that the cramping is more intense when you are breast/chest feeding, especially if this is not your first baby. You can take Tylenol or Ibuprofen to help with the cramping.
You can take Tylenol or Ibuprofen to help with the cramping.
When to call us: If you have pain that is severe or that does not respond to medication.
Symptoms of Postpartum Preeclampsia / Headache
As your hormones fluctuate postpartum, headaches can be common. The lack of sleep can contribute as well! Make sure you are well hydrated.
However, a headache (especially a headache that does not resolve with ibuprofen or tylenol) can be a symptom of preeclampsia. Other signs of preeclampsia include swelling (you might notice it in your hands, your feet, or your face), visual changes such as flashing lights or blank spots in your field of vision, nausea/vomiting, or pain on the upper right side of your abdomen.
When to call us: If you have a headache that does not respond to Ibuprofen or Tylenol or any other signs of postpartum preeclampsia.
Breast Changes
Your body will make milk regardless of whether you are breast/chest feeding. Your breasts are likely to become engorged (full of milk) three or four days after the birth. Engorgement can also cause you to have a low-grade fever (less than 100.4F).
Your breasts are likely to become engorged (full of milk) three or four days after the birth. Engorgement can also cause you to have a low-grade fever (less than 100.4F).
If you are breastfeeding, it is important to put the baby to the breast, or otherwise drain the breast (pump, hand-express) every 2-4 hours, round the clock. This will give your body signals to make milk in the right amount for your baby.
It is possible to develop plugged milk ducts, and plugged ducts can lead to infection, also known as mastitis. If you notice that you have any lumps in your breast, you need to get that milk moving – stand in the shower and let the warm water run on the breast while you massage the lump. You can also try feeding the baby in alternative positions like the football hold or dangle feeds. Some women who are prone to plugged ducts also benefit from soy lecithin supplements (take one 1200 mg capsule 3-4 times per day, reduce dosage by one capsule per day when the blockage has resolved for one week).
If you have hard, painful areas in the breast that look red & feel warm to the touch, you may be developing mastitis. It is important to stay very well hydrated, take Ibuprofen for its anti-inflammatory properties, and drain the breast completely.
When to call us: If you develop symptoms of mastitis along with fever over 100.4F and malaise (you feel unwell), as you may need antibiotics.
Blood Clots
If you notice that you have one leg that is more swollen than the other, especially if the affected leg is dusky or grey/purple colored, or if you have pain in your calf or the back of your thigh, you might have developed a blood clot.
Go to the emergency room: If you have these symptoms and are also experiencing shortness of breath.
Mood Changes
Mood changes are very common in the first few weeks postpartum. About 85% of women experience the “baby blues” after birth. You might notice that you are laughing one moment and crying the next.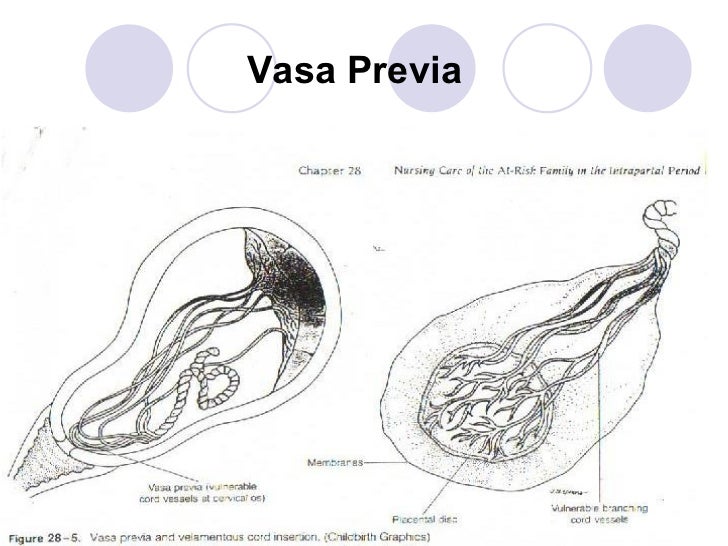 These mood swings are caused by hormone changes combined with the sleep deprivation and role changes that you experience as the parent of a newborn. Your mood should feel more stable by the time the baby is one month old.
These mood swings are caused by hormone changes combined with the sleep deprivation and role changes that you experience as the parent of a newborn. Your mood should feel more stable by the time the baby is one month old.
Postpartum depression and anxiety are less common than the baby blues, but can cause mood changes up to a year after your birth. Please don’t discount mood changes that are causing issues for you, these issues are real and treatable.
When to call us: if you’d like to discuss what you’re feeling or if you’d like a referral to mental health therapist that specializes in postpartum. But if you have any thoughts of doing harm to yourself or the baby, you need emergency attention.
Wounds that aren’t healing
If you have an abdominal incision or perineal wound, you will need to keep those areas clean & dry as they heal. Let soapy water run over them in the shower and pat to dry. Be sure to expose the incision to good air-flow (don’t keep it covered all day).
Our c-section patients will come to the office two weeks after the birth so we can look at your incision and remove any remaining dressings.
If you have a perineal or vaginal laceration, the stitches will dissolve and do not need to be removed. You might notice pieces of the stitch material on your toilet paper about a week after the birth. Use the peri-bottle to spray the area to clean it and pat dry with toilet paper. You can keep ice on the area for the first 24 hours, and do warm sitz baths (shallow baths that dunk your perineum in warm water) 2-3 times per day until the area feels better. Sitz baths provide cleaning and improved circulation to this delicate area. They are soothing and therapeutic — don’t skip them! You can add healing herbs or epsom salts to the water in the sitz bath, but even plain warm water has the desired effect.
When to call us: If you notice that the incision is bleeding, opening, leaking pus, if areas of redness on the edges are getting larger, or if you are not able to manage your pain with the medications you were given.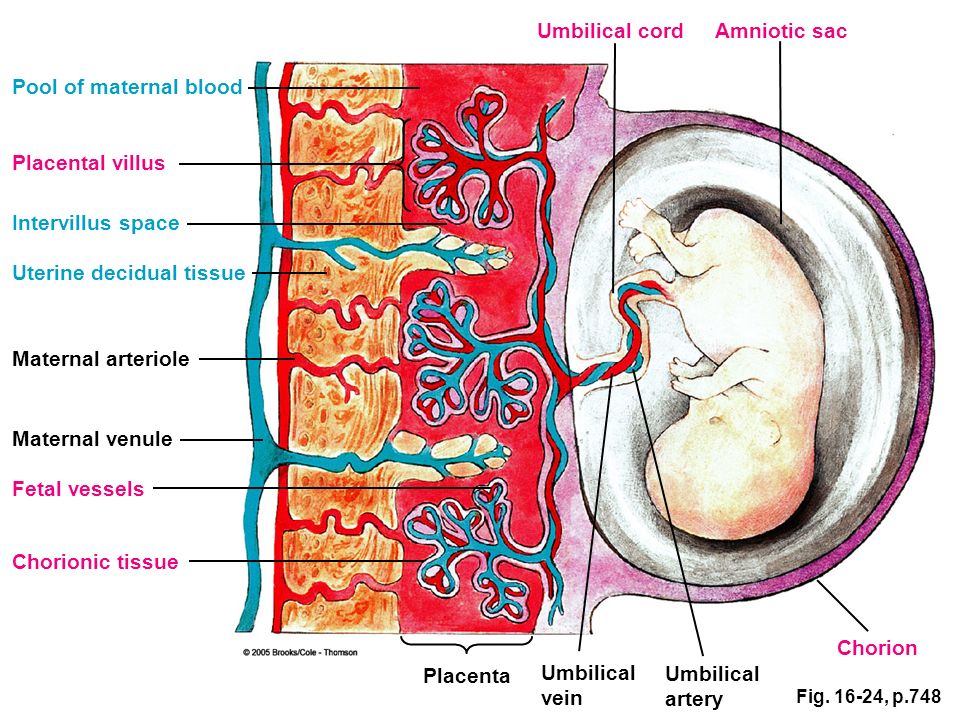
Bleeding — 4th Trimester Project
◄ Self Care Topics ◄ Healing / Recovery ◄ Bleeding
Bleeding after birth, (often called lochia), is a normal part of recovery. Quarter-sized blood clots are common the first few days. At 10-14 days after birth, many women notice a brief increase in bleeding. That’s thought to be scab over the place where the placenta was attached to the uterus coming off. Most moms have some red, brown, then yellow discharge for 4-6 weeks after birth, but women can bleed for as little as 2 days or as long as 90 days. Even women who deliver their baby by a c-section will still experience vaginal bleeding as part of recovery. The amount of bleeding should steadily decrease over the first few weeks.
When to call your provider
If you experience so much bleeding that you must change your pads every hour or pass a clot larger than a golf ball, call your provider right away.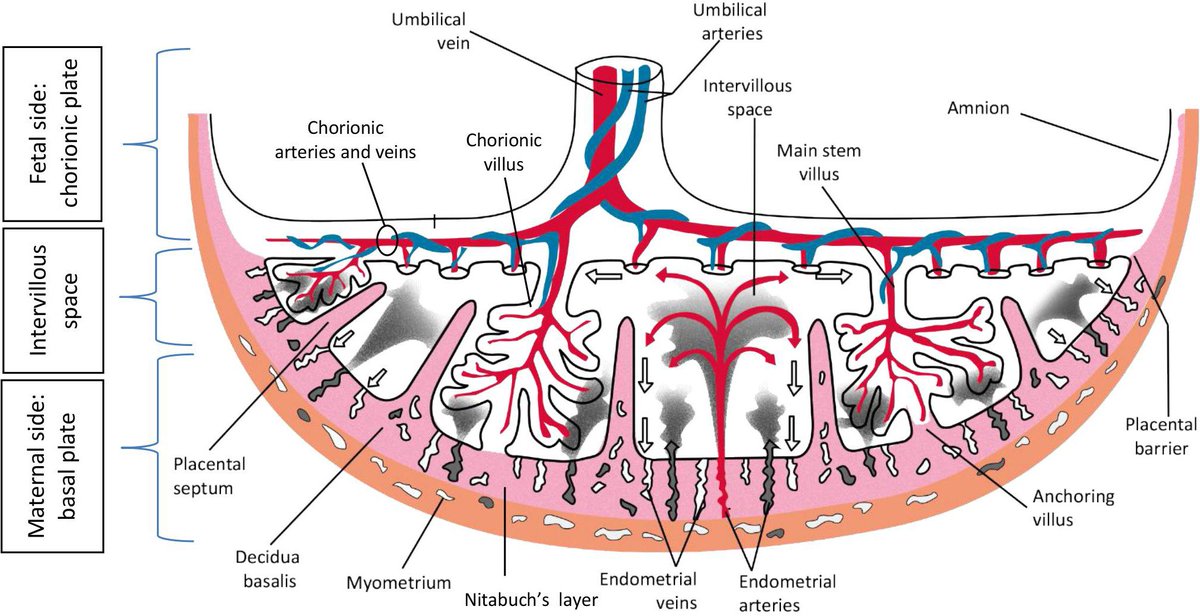 If the blood has a bad odor or you have fever and chills, you should call your health care provider right away. This could be a sign of an infection or a retained piece of placenta.
If the blood has a bad odor or you have fever and chills, you should call your health care provider right away. This could be a sign of an infection or a retained piece of placenta.
Things to do that might help
Make sure you have plenty of large and absorbent pads at home. Many women suggest selecting a pad with wings. If resources are a problem, ask for extra pads at the hospital. Your local diaper bank may be able to help you and your baby with supplies.
Tampons are not recommended as they are not absorbent enough, are a potential source of infection and may be very uncomfortable after a vaginal birth.
Squirt bottles (peribottles) with warm water can help keep this area clean.
Pay attention to how much you are bleeding especially in the first week – if you are bleeding a lot call your provider right away and let them know how many pads you are using in an hour.
Most women will have their first cycle within 7 to 9 weeks after birth.
 Nursing mothers frequently start menstrual periods by 12 weeks, but some mothers don’t start their periods until they have stopped breastfeeding. Egg production may return before the first menstrual period, which means you can become pregnant again.
Nursing mothers frequently start menstrual periods by 12 weeks, but some mothers don’t start their periods until they have stopped breastfeeding. Egg production may return before the first menstrual period, which means you can become pregnant again.It’s hard to know when bleeding will stop. To cut down on laundry, don’t wear light colored bottoms – stick with dark skirts and pants for the first month or so after birth.
TOPICS IN Healing / Recovery
Opioid Use
Recovering from a Cesarean Section
Recovering from a Vaginal Delivery
Infections
Bleeding
Aches and Pains
Body Changes
Postpartum Health Care
The content of this website is not intended for use as diagnosis or treatment of a health problem. If you have questions or concerns, please contact your health care provider. If you need emergency care, call 911 right away.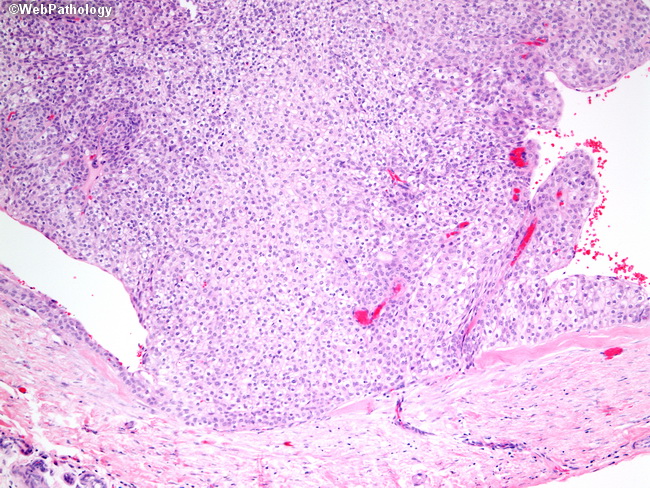
The 4th Trimester Project™ is a trademark.
Healing & RecoverySuzanne Woodwardhealing, recovery, pain, bleeding, vaginal bleeding, how much bleeding is normal
0 LikesContacts
Remote training
Professional retraining
Professional training
Classes
Teachers Teachers, educators
9000 Postal address: 344015, Rostov-on-Don, st. Blagodatnaya 170, GBOUDPORO "TsPK" Director's office: phone/fax: 8(863) 222-48-36, 8(863) 222-74-60, 8(863) 297-07-95 Working hours: Monday-Friday from 8:45 to 17:15 (break from 12:00 to 12:30) Saturday-Sunday - day off E-mail: Reception This email address is being protected from spambots. Director Dimitrova Lyudmila Vladimirovna This email address is being protected from spambots. You must have JavaScript enabled to view. Deputy Director for UMR Dvurechenskaya Valentina Mikhailovna This email address is being protected from spambots. You must have JavaScript enabled to view. Methodical room Nazarova Larisa Yurievna This email address is being protected from spambots. You must have JavaScript enabled to view. Chief Accountant Bobrus Olga Vladimirovna This email address is being protected from spambots. You must have JavaScript enabled to view. On the organization of the educational process (heads of departments): Voloshko Lyudmila Petrovna 8-918-561-58-80 This email address is being protected from spambots. Koroleva Irina Igorevna 8-918-561-55-25 This email address is being protected from spambots. You must have JavaScript enabled to view. Parshenkova Albina Nailevna 8-918-561-20-50 This email address is being protected from spambots. You must have JavaScript enabled to view. Reznikova Oksana Stanislavovna 8-918-561-26-36 This email address is being protected from spambots. You must have JavaScript enabled to view. Romanova Elena Viktorovna 8-918-561-58-00 This email address is being protected from spambots. Teslitskaya Elena Vasilievna 8-918-561-60-70 This email address is being protected from spambots. You must have JavaScript enabled to view. Titarenko Irina Yurievna 8-918-561-09-88 This email address is being protected from spambots. You must have JavaScript enabled to view. For enrollment: phone/fax: 8(863) 222-28-10 Petrova Anastasia Vladimirovna 8-989-620-06-86 This email address is being protected from spambots. You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, the date of training and the student's e-mail address) 8-989-620-04-16 For enrollment in CME cycles: cpknmo @ yandex . Pogodina Anna Gennadievna - 8-988-540-06-37 This email address is being protected from spambots. You must have JavaScript enabled to view. Sekunova Olga Nikolaevna – 8-918-550-13-47 This email address is being protected from spambots. You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, date of study, full name) For certification: Kozlova Svetlana Aleksandrovna 8-918-561-05-75 For accreditation: head of practice Galtseva Elena Alexandrovna 8-988-580-01-29 This email address is being protected from spambots. You must have JavaScript enabled to view. Human Resources: Calf Irina Valentinovna 8-918-561-60-01 Accounting: Osipova Tatyana Borisovna Semernikova Tatyana Sergeevna 8-918-561-60-01 Economist: Ivanova Uliana Yurievna 8 (863) 222-48-36 This email address is being protected from spambots. You must have JavaScript enabled to view. For acceptance of documents for passing the exam for the assignment of a qualification category -8-918-561-09-88 Titarenko Irina Yuryevna – e-mail address is being protected from spam. For webinars email address This email address is being protected from spambots. You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, full name, the word WEBINAR) From the bus station, railway station - fixed-route taxi No. 40A - to the stop "Regional Hospital". From the old bus station - minibuses No. 40, 40A - to the stop "Regional Hospital" Lochia after childbirth is normal. How long should they last? Why do they appear? What should be of concern? Find out the answers to these questions from this article. Lochia is released from the wound surface of the uterus during healing. They consist of mucus, blood, and remnants of the fetal membrane. The first 3-4 days of excretion are predominantly blood. Then, when hemostasis is fully established, they acquire a paler color and become brownish. By the end of the first week, the discharges contain predominantly bacteria and remnants of decidual material and become serous. The color of the discharge changes to yellowish. By about day 10, the lochia after childbirth should be completely white, without blood impurities. Sometimes in the first or second week, the volume of discharge increases. This is due to the fact that during this period the scab formed at the place of attachment of the placenta is rejected. The number of discharges is gradually decreasing. From the third week they become slimy and scarce. A specific, as if rotten smell is an indicator that lochia is formed and excreted normally. If the discharge has stopped in the first weeks, this should alert you. A similar symptom may be a sign that the uterus has a sharp inflection or its neck is clogged with a blood clot. Accumulation of lochia can lead to constant aching or cramping pain in the lower abdomen. In some cases, the body temperature may rise slightly, the patient may feel chills. If the lochia after childbirth is too abundant or after 4 days the discharge is too bright or prolonged, this should alert you. Also, the reason for contacting a gynecologist should be cloudy, purulent, foamy or abundant mucous lochia. This may signal that fragments of the baby's place remained in the uterus after childbirth, or the presence of inflammation or infection. 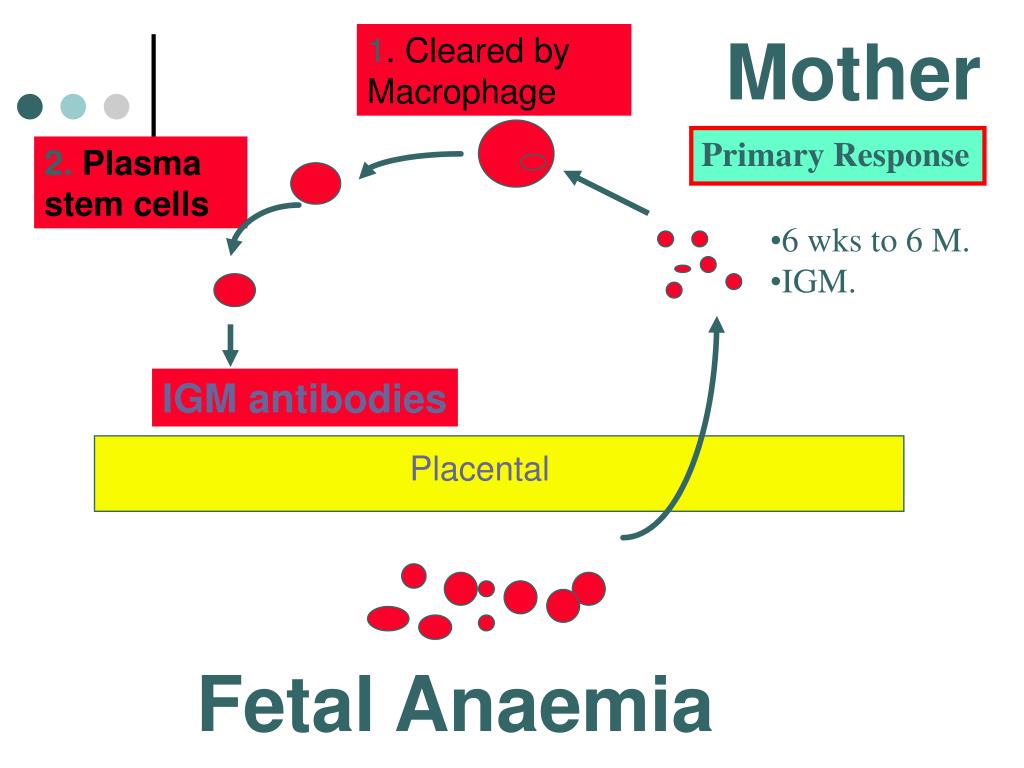 You must have JavaScript enabled to view.
You must have JavaScript enabled to view.  You must have JavaScript enabled to view.
You must have JavaScript enabled to view. 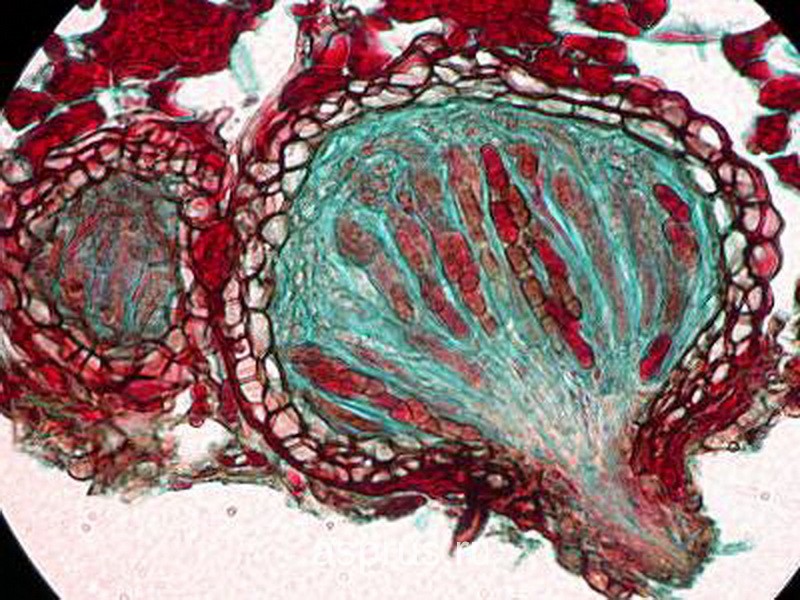 You must have JavaScript enabled to view.
You must have JavaScript enabled to view. 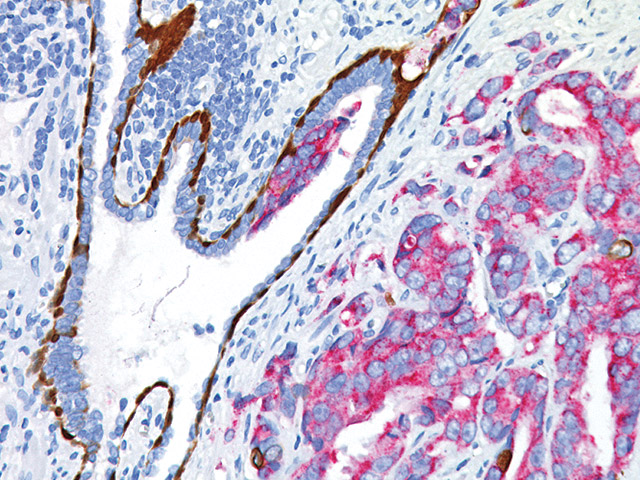 en
en 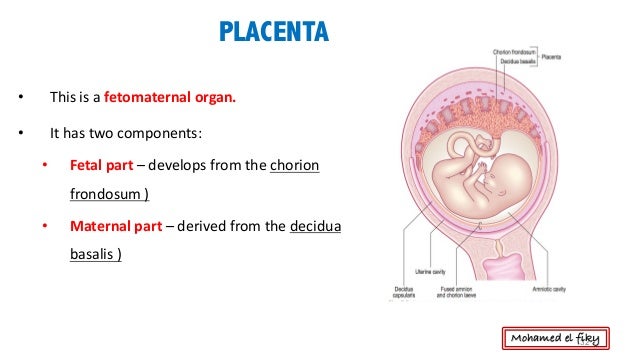
 You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, the date of training and the student's e-mail address, and the word DISTATEGORY - if documents are sent; or the word QUESTION - if you need to ask a question)
You must have JavaScript enabled to view. (in the subject of the letter, indicate the name of the cycle, the date of training and the student's e-mail address, and the word DISTATEGORY - if documents are sent; or the word QUESTION - if you need to ask a question)
Public transport: From the Central market - bus, route number 26, to the stop "Regional Hospital". Lochia after childbirth: what is it?
What is postpartum lochia?
How long does lochia last after childbirth?
 During this period, in most women, the endometrium has already fully recovered. By about the fifth or sixth week, the discharge stops.
During this period, in most women, the endometrium has already fully recovered. By about the fifth or sixth week, the discharge stops. Lochia after childbirth: duration and normal indicators