Starting of labour
Signs that labour has begun
Know the signs
There are several signs that labour might be starting, including:
- contractions or tightenings
- a "show", when the plug of mucus from your cervix (entrance to your womb, or uterus) comes away
- backache
- an urge to go to the toilet, which is caused by your baby's head pressing on your bowel
- your waters breaking
The early (latent) stage of labour can take some time.
Urgent advice: Call your midwife or maternity unit if:
- your waters break
- you have vaginal bleeding
- your baby is moving less than usual
- you're less than 37 weeks pregnant and think you might be in labour
These signs mean you need to see a midwife or doctor.
Latent phase of labour
The start of labour is called the latent phase. This is when your cervix becomes soft and thin, and starts opening for your baby to be born. This can take hours or sometimes days.
You'll probably be advised to stay at home during this time. If you go to the hospital or maternity unit, they may suggest you go back home.
Find out more about the stages of labour and what you can do at home during the latent phase.
Call your midwife if you're unsure or worried about anything.
What do contractions feel like
When you have a contraction, your womb tightens and then relaxes. For some people, contractions may feel like extreme period pains.
You may have had contractions during your pregnancy, particularly towards the end. These tightenings are called Braxton Hicks contractions and are usually painless.
These tightenings are called Braxton Hicks contractions and are usually painless.
Your contractions tend to become longer, stronger and more frequent as your labour progresses. During a contraction, the muscles tighten and the pain increases. If you put your hand on your abdomen, you'll feel it getting harder; when the muscles relax, the pain fades and you will feel the hardness ease.
The contractions are pushing your baby down and opening the entrance to your womb (the cervix), ready for your baby to go through.
Your midwife will probably advise you to stay at home until your contractions become frequent.
Call your midwife or maternity unit for guidance when your contractions are in a regular pattern and:
- last at least 60 seconds
- come every 5 minutes or
- you think you are in labour
Read more information on when to go to hospital
Backache often comes on in labour
You may get backache or a heavy, aching feeling.
A "show" can signal the start of labour
During pregnancy, there's a plug of mucus in your cervix. This mucus comes away just before labour starts, or when in early labour, and it may pass out of your vagina. This sticky, jelly-like pink mucus is called a show.
It may come away in 1 blob or in several pieces. It's pink because it contains a small amount of blood.
If you're losing more blood, it may be a sign something is wrong, so phone your hospital or midwife straight away.
A show indicates that the cervix is starting to open. Labour may quickly follow or may take a few days. Sometimes there is no show.
What happens when my waters break
It's likely your waters will break during labour, but it can also happen before labour starts.
Your baby develops and grows inside a bag of fluid called the amniotic sac. When it's time for your baby to be born, the sac usually breaks and the amniotic fluid drains out through your vagina. This is your waters breaking. Sometimes when you're in labour, a midwife or doctor may offer to break your waters.
When it's time for your baby to be born, the sac usually breaks and the amniotic fluid drains out through your vagina. This is your waters breaking. Sometimes when you're in labour, a midwife or doctor may offer to break your waters.
If your waters break naturally, you may feel a slow trickle or a sudden gush of water you cannot control. To prepare for this, you could keep a sanitary towel (but not a tampon) handy if you're going out, and put a protective sheet on your bed.
Amniotic fluid is clear and pale. Sometimes it's difficult to tell amniotic fluid from urine. When your waters break, the water may be a little bloodstained to begin with.
Tell your midwife immediately if:
- the waters are smelly or coloured
- you're losing blood
This could mean you and your baby need urgent attention.
If your waters break before labour starts, call your midwife. Use a sanitary pad (not a tampon) so your midwife can check the colour of the waters.
Use a sanitary pad (not a tampon) so your midwife can check the colour of the waters.
If labour does not start after your waters break
It's usual to go into labour within 24 hours of the waters breaking. You'll be offered an induction if you do not because, without amniotic fluid, there's an increased risk of infection for your baby.
Until your induction, or if you choose to wait for labour to start naturally, tell your midwife immediately if:
- your baby moves less than usual
- there's any change in the colour or smell of any fluid coming from your vagina
You should take your temperature every 4 hours when you're awake, and tell your midwife if it's raised. A raised temperature is usually above 37.5C, but you may need to call before this – check with your midwife.
There's no evidence that having a bath or shower after your waters have broken increases your risk of infection, but having sex might.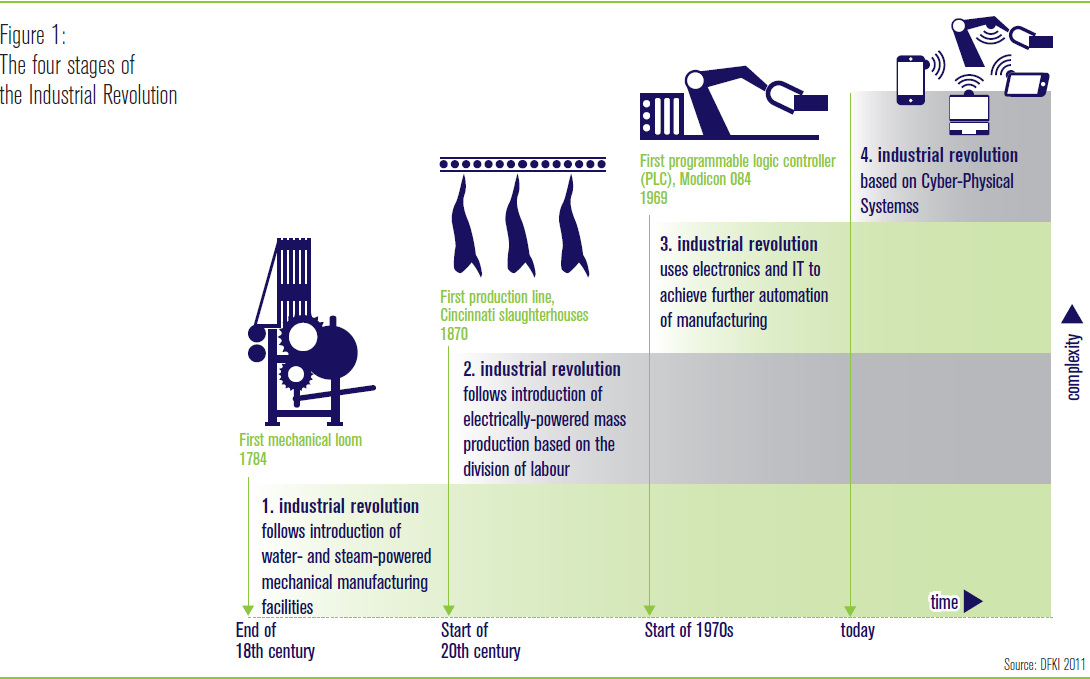
How to cope when labour begins
At the beginning of labour, you can:
- walk or move about, if you feel like it
- drink fluids – you may find sports (isotonic) drinks help keep your energy levels up
- have a snack, if you feel like it
- try any relaxation and breathing exercises you've learned to deal with contractions as they get stronger and more painful – your birth partner can help by doing these with you
- have your birth partner rub your back – this can help relieve pain
- take paracetamol according to the instructions on the packet – paracetamol is safe to take in labour
- have a warm bath
Find out what happens during labour and birth, and what you can do for pain relief in the early stages of labour.
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
Video: How will I know I am in labour?
In this video, a midwife describes the signs that mean labour may be starting.
Media last reviewed: 1 November 2019
Media review due: 1 November 2022
The stages of labour and birth
1st stage of labour
During the 1st stage of labour, contractions make your cervix gradually open (dilate). This is usually the longest stage of labour.
At the start of labour, your cervix starts to soften so it can open. This is called the latent phase and you may feel irregular contractions. It can take many hours, or even days, before you're in established labour.
It can take many hours, or even days, before you're in established labour.
Established labour is when your cervix has dilated to about 4cm and regular contractions are opening your cervix.
During the latent phase, it's a good idea to have something to eat and drink because you'll need energy for when labour is established.
If your labour starts at night, try to stay comfortable and relaxed. Sleep if you can.
If your labour starts during the day, stay upright and gently active. This helps your baby move down into your pelvis and helps your cervix to dilate.
Breathing exercises, massage and having a warm bath or shower may help ease pain during this early stage of labour.
When to contact a midwife
Contact your midwifery team if:
- your contractions are regular and you're having about 3 in every 10-minute period
- your waters break
- your contractions are very strong and you feel you need pain relief
- you're worried about anything
If you go into hospital or your midwifery unit before your labour has become established, they may suggest you go home again for a while.
Once labour is established, your midwife will check on you from time to time to see how you're progressing and offer you support, including pain relief if you need it.
You can either walk around or get into a position that feels comfortable to labour in.
Your midwife will offer you regular vaginal examinations to see how your labour is progressing. If you do not want to have these, you do not have to – your midwife can discuss with you why she's offering them.
Your cervix needs to open about 10cm for your baby to pass through it. This is what's called being fully dilated.
In a 1st labour, the time from the start of established labour to being fully dilated is usually 8 to 12 hours. It's often quicker (around 5 hours), in a 2nd or 3rd pregnancy.
When you reach the end of the 1st stage of labour, you may feel an urge to push.
Monitoring your baby in labour
Your midwife will monitor you and your baby during labour to make sure you're both coping well.
This will include using a small handheld device to listen to your baby's heart every 15 minutes. You'll be free to move around as much as you want.
Your midwife may suggest electronic monitoring if there are any concerns about you or your baby, or if you choose to have an epidural.
Electronic monitoring involves strapping 2 pads to your bump. One pad is used to monitor your contractions and the other is used to monitor your baby's heartbeat. These pads are attached to a monitor that shows your baby's heartbeat and your contractions
Sometimes a clip called a foetal heart monitor can be attached to the baby's head instead. This can give a more accurate measurement of your baby's heartbeat.
You can ask to be monitored electronically even if there are no concerns. Having electronic monitoring can sometimes restrict how much you can move around.
Having electronic monitoring can sometimes restrict how much you can move around.
If you have electronic monitoring with pads on your bump because there are concerns about your baby's heartbeat, you can take the monitor off if your baby's heartbeat is shown to be normal.
A foetal scalp monitor will usually only be removed just as your baby is born, not before.
Speeding up labour
Labour can sometimes be slower than expected. This can happen if your contractions are not coming often enough, are not strong enough, or if your baby is in an awkward position.
If this is the case, your doctor or midwife may talk to you about 2 ways to speed up your labour: breaking your waters or an oxytocin drip.
Breaking your waters
Breaking the membrane that contains the fluid around your baby (your waters) is often enough to make contractions stronger and more regular.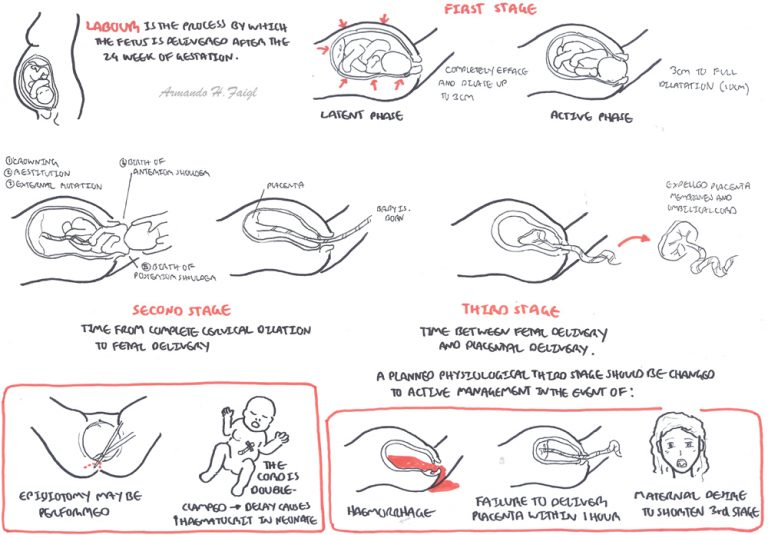 This is also known as artificial rupture of the membranes (ARM).
This is also known as artificial rupture of the membranes (ARM).
Your midwife or doctor can do this by making a small break in the membrane during a vaginal examination. This may make your contractions feel stronger and more painful, so your midwife will talk to you about pain relief.
Oxytocin drip
If breaking your waters does not work, your doctor or midwife may suggest using a drug called oxytocin (also known as syntocinon) to make your contractions stronger. This is given through a drip that goes into a vein, usually in your wrist or arm.
Oxytocin can make your contractions stronger and more regular and can start to work quite quickly, so your midwife will talk to you about your options for pain relief.
You will also need electronic monitoring to check your baby is coping with the contractions, as well as regular vaginal examinations to check the drip is working.
2nd stage of labour
The 2nd stage of labour lasts from when your cervix is fully dilated until the birth of your baby.
Finding a position to give birth in
Your midwife will help you find a comfortable position to give birth in. You may want to sit, lie on your side, stand, kneel, or squat, although squatting may be difficult if you're not used to it.
If you've had lots of backache while in labour, kneeling on all fours may help. It's a good idea to try some of these positions before you go into labour. Talk to your birth partner so they know how they can help you.
Find out what your birth partner can do.
Pushing your baby out
When your cervix is fully dilated, your baby will move further down the birth canal towards the entrance to your vagina. You may get an urge to push that feels a bit like you need to poo.
You may get an urge to push that feels a bit like you need to poo.
You can push during contractions whenever you feel the urge. You may not feel the urge to push immediately. If you have had an epidural, you may not feel an urge to push at all.
If you're having your 1st baby, this pushing stage should last no longer than 3 hours. If you've had a baby before, it should take no more than 2 hours.
This stage of labour is hard work, but your midwife will help and encourage you. Your birth partner can also support you.
What happens when your baby is born
When your baby's head is almost ready to come out, your midwife will ask you to stop pushing and take some short breaths, blowing them out through your mouth.
This is so your baby's head can be born slowly and gently, giving the skin and muscles in the area between your vagina and anus (the perineum) time to stretch.
Sometimes your midwife or doctor will suggest an episiotomy to avoid a tear or to speed up delivery. This is a small cut made in your perineum.
You'll be given a local anaesthetic injection to numb the area before the cut is made. Once your baby is born, an episiotomy, or any large tears, will be stitched closed.
Find out about your body after the birth, including how to deal with stitches.
Once your baby's head is born, most of the hard work is over. The rest of their body is usually born during the next 1 or 2 contractions.
You'll usually be able to hold your baby immediately and enjoy some skin-to-skin time together.
You can breastfeed your baby as soon as you like. Ideally, your baby will have their 1st feed within 1 hour of birth.
Read more about skin-to-skin contact and breastfeeding in the first few days.
3rd stage of labour
The 3rd stage of labour happens after your baby is born, when your womb contracts and the placenta comes out through your vagina.
There are 2 ways to manage this stage of labour:
- active – when you have treatment to make it happen faster
- physiological – when you have no treatment and this stage happens naturally
Your midwife will explain both ways to you while you're still pregnant or during early labour, so you can decide which you would prefer.
There are some situations where physiological management is not advisable. Your midwife or doctor can explain if this is the case for you.
What is active management?
Your midwife will give you an injection of oxytocin into your thigh as you give birth, or soon after. This makes your womb contract.
This makes your womb contract.
Evidence suggests it's better not to cut the umbilical cord immediately, so your midwife will wait to do this between 1 and 5 minutes after birth. This may be done sooner if there are concerns about you or your baby – for example, if the cord is wound tightly around your baby's neck.
Once the placenta has come away from your womb, your midwife pulls the cord – which is attached to the placenta – and pulls the placenta out through your vagina. This usually happens within 30 minutes of your baby being born.
Active management speeds up the delivery of the placenta and lowers your risk of having heavy bleeding after the birth (postpartum haemorrhage), but it increases the chance of you feeling and being sick. It can also make afterpains (contraction-like pains after birth) worse.
Read about preventing heavy bleeding on our page What happens straight after the birth.
What is physiological management?
No oxytocin injection is given, and the 3rd stage of labour happens naturally.
The cord is not cut until it has stopped pulsing. This means blood is still passing from the placenta to your baby. This usually takes around 2 to 4 minutes.
Once the placenta has come away from your womb, you should feel some pressure in your bottom and you'll need to push the placenta out. It can take up to an hour for the placenta to come away, but it usually only takes a few minutes to push it out.
If the placenta does not come away naturally or you begin to bleed heavily, you'll be advised by your midwife or doctor to switch to active management. You can do this at any time during the 3rd stage of labour.
Read more about what happens straight after you give birth.
Video: What positions are best for giving birth?
In this video, a midwife talks through some of the best positions to give birth.
Media last reviewed: 20 March 2020
Media review due: 20 March 2023
Fears during pregnancy | Nutriclub
Most women experience fear and anxiety during pregnancy. What most often worries expectant mothers and how to relieve excessive anxiety - we analyze the points
During pregnancy, serious changes occur in the body of the expectant mother. The feeling of anxiety and fear during this period is experienced by 90% of women - this is a natural psychological reaction to changes in hormonal levels and adaptation of the body to new conditions.
Is there something wrong with my child?
It is important to know that nature has done everything to protect your baby in the womb. And modern medicine is able to detect and prevent many diseases and deviations. Do your best - see your doctor regularly and stay active and healthy - and you'll be fine. Timely diagnosis will help to identify diseases and infections at the initial stage that can threaten the baby, and cure them in a timely manner.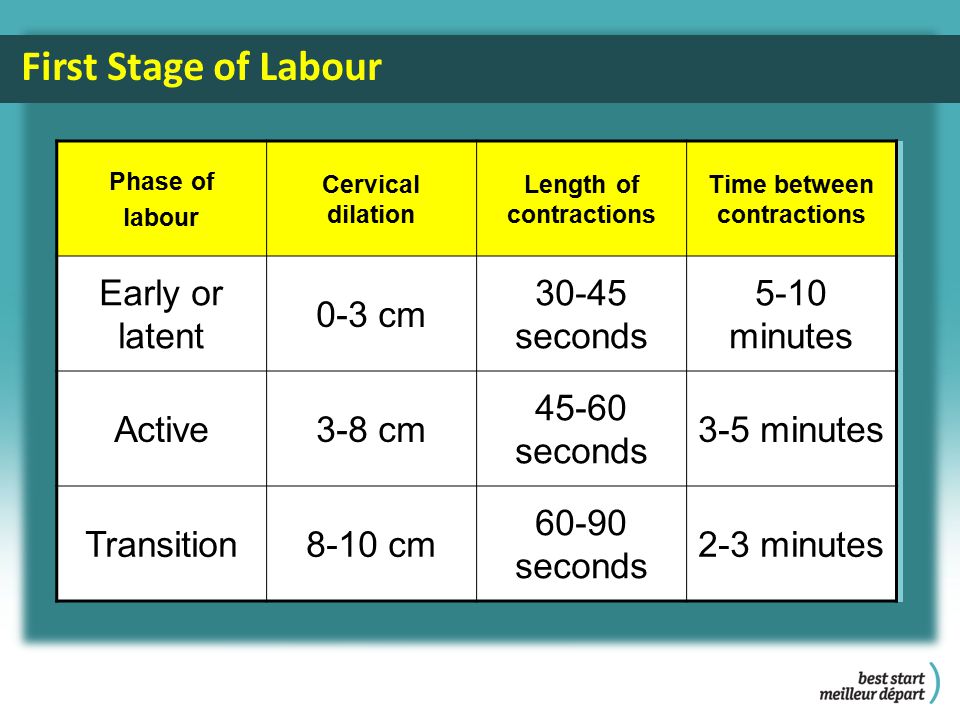 The expectant mother is tested, she is given an ultrasound scan and screenings to detect fetal pathologies. All this will help you relieve anxiety and fear for the health of the baby. In order to stop worrying, it is worth thinking about the positive experience of your acquaintances and girlfriends, remember that most children are born healthy and that many developmental disorders are successfully corrected after birth. Read less horror forums, attend yoga and pregnancy fitness classes, and walk more.
The expectant mother is tested, she is given an ultrasound scan and screenings to detect fetal pathologies. All this will help you relieve anxiety and fear for the health of the baby. In order to stop worrying, it is worth thinking about the positive experience of your acquaintances and girlfriends, remember that most children are born healthy and that many developmental disorders are successfully corrected after birth. Read less horror forums, attend yoga and pregnancy fitness classes, and walk more.
I am afraid of childbirth
Fear of childbirth is a natural fear of physical pain. In order to get rid of it, you can be like childbirth preparation courses, where you will be taught how to breathe and push properly. Such courses are also good because you will see how many women are in the same position as you. You can discuss your concerns with the obstetrician-gynecologist in advance, decide how you will give birth: alone or with a partner, which type of anesthesia is preferable for you, if such a need arises.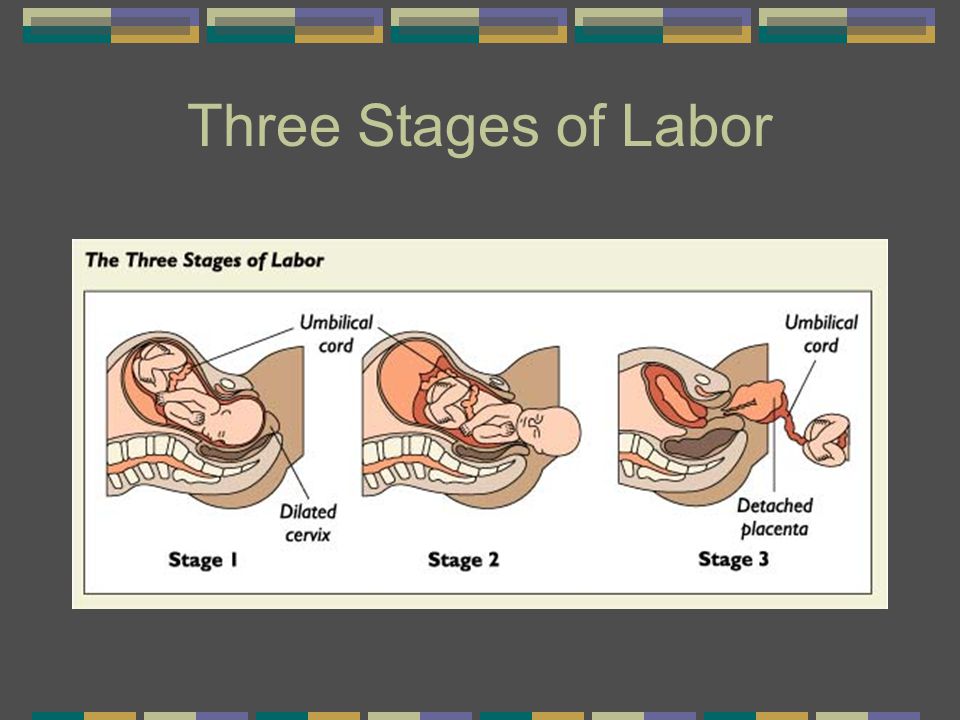 Remember that today doctors have a lot of opportunities to make the process of childbirth painless. In addition, you can prepare your body for childbirth by walking more, moving more and attending classes for pregnant women.
Remember that today doctors have a lot of opportunities to make the process of childbirth painless. In addition, you can prepare your body for childbirth by walking more, moving more and attending classes for pregnant women.
What if I'm a bad mom?
What if I take care of the child incorrectly and this will harm him? I will not have time to do everything that is necessary, because the child requires increased attention? I will not be able to properly feed and educate him? These are common fears that almost all women who give birth for the first time visit. It is important to know that there is nothing more natural than motherhood. You will cope with any number of children that will be born thanks to you. As a rule, as soon as the baby is born, everything comes by itself, and no one but you will understand your child better. And all your fears will dissipate in the first days of the baby's life. Not a single woman has a ready-made program for care and upbringing - instincts and daily practice help.
What if I can't breastfeed?
Only 5% of women cannot breastfeed for medical or psychological reasons. As a rule, these are such serious diseases as kidney pathology, heart defects, blood diseases, tumors, HIV infections, etc. There are acute psycho-emotional disorders that also prevent breastfeeding. If you do not have such diseases, then there is nothing to worry about. After childbirth, milk appears in all women without exception, and feeding on demand will provide the right amount of milk for the baby. Today, in many maternity hospitals, you can consult a nurse or even a breastfeeding specialist who will show you how to properly latch on to your baby. If you are concerned about cracks, then there are various products that are applied to the nipples before and after feeding, a breastfeeding specialist can also talk about this. And of course, a positive attitude is needed for successful feeding: remember that with mother's breast milk, the child receives absolutely all the trace elements he needs.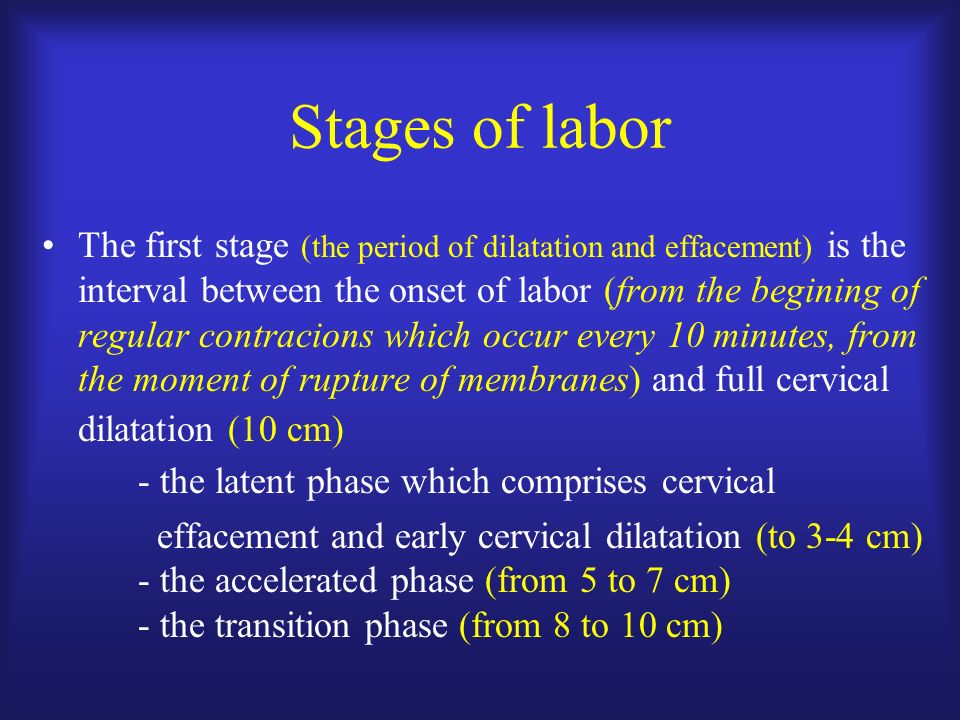
Will my life change?
Life will change, but definitely for the better. If before pregnancy your days were full of interesting people and things, then this will not disappear anywhere. Rather, on the contrary - after the birth of a child, new ideas and interests will appear. As many women note, a decree is a chance to learn new skills and abilities, and possibly change the field of activity if you have been thinking about it for a long time. The fact is that caring for a child can be combined with other activities, the main thing is to set yourself up correctly. Today there are great opportunities for distance learning and professional development. These are books, online courses, webinars, remote work.
There is a common myth that a child chains his mother to the house. It all depends on the desire of the woman: with the baby it is quite possible to go on a visit, to meet with friends or colleagues, to travel. Also, most babies sleep very soundly and won't be distracted if you invite guests.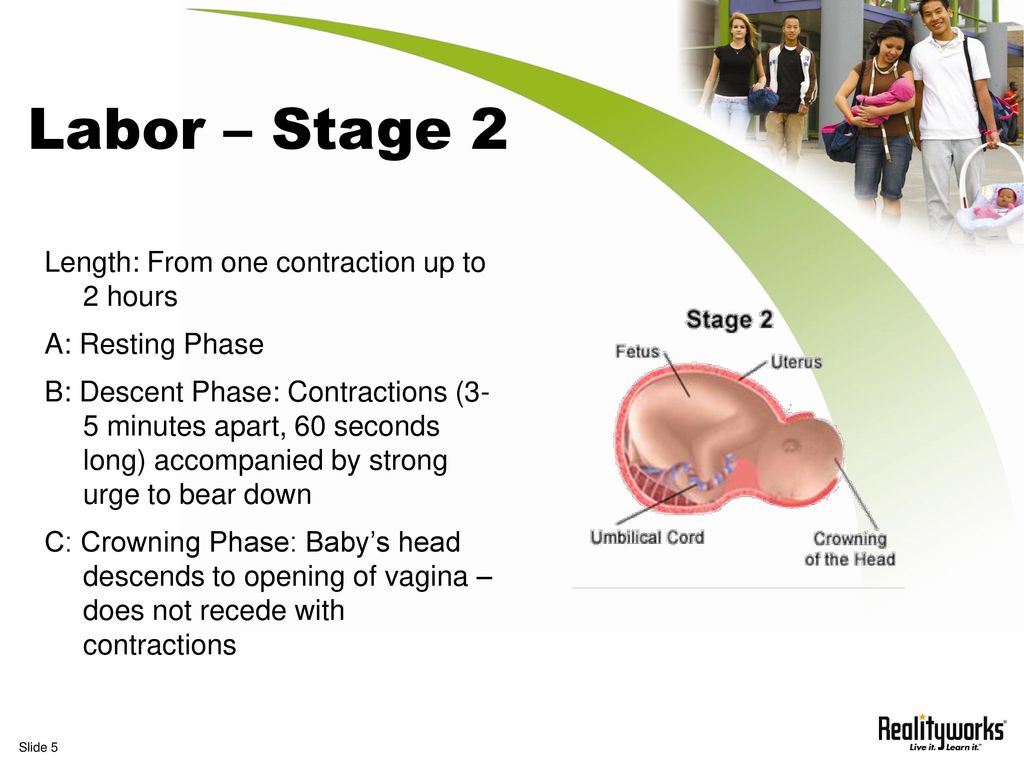
The main way to get rid of fears during pregnancy is to fill your life with events and people that make you happy. The condition of the mother is passed on to her child, and to please and take care of yourself is the most important thing you can do for the baby during this period.
When using any materials from the site nutriclub.ru, a link to the site is required.
© Nutriclub, 2020
You will also be interested
- Nutriclub - healthy nutrition and child development
- Pregnancy
- Pregnancy: lifestyle
- Fears during pregnancy | Nutriclub
Signs of labor initiation | Signs of the onset of labor
Pregnancy
Article
0 reviews
The due dates are approaching, the bag with things for the maternity hospital is ready, it remains to wait for this moment and pick up a little bundle of happiness as soon as possible.
4 min. for reading Feb. 17, 2022
The due dates are approaching, the bag with things for the maternity hospital is ready, it remains to wait for this moment and take a little bundle of happiness in your hands as soon as possible. The waiting period is the most exciting, a woman realizes that at this stage, childbirth can happen at any time and her feelings are a cocktail of fear, excitement and anticipation of a long-awaited meeting. Therefore, the expectant mother listens to herself in anticipation of recognizing the signs of the onset of labor.
Signs of the onset of labor and changes in the body of a woman
The period after 38 weeks is considered the optimal time for childbirth. At this time, the woman's body begins independent preparation for this event. The level of hormones responsible for bearing a fetus in the blood of a pregnant woman decreases, at this time another hormone that provokes labor activity rises.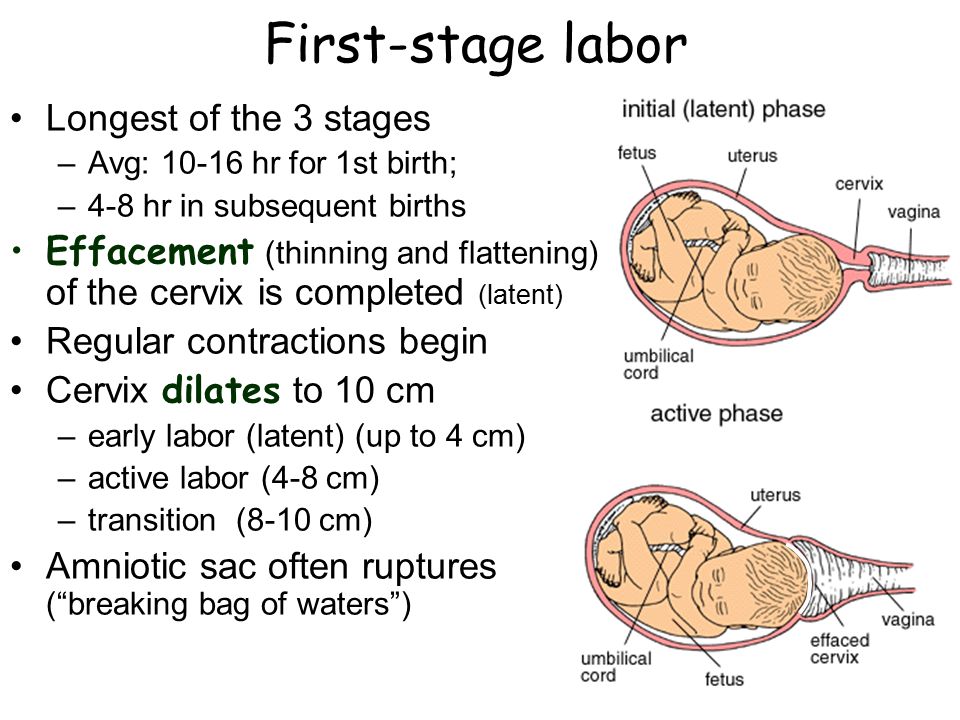
The moment of delivery occurs when the hormone levels reach their limit. Such hormonal changes in the body affect the condition of a woman and become harbingers of childbirth. Symptoms that indicate the approach of the birth process may not all appear, and they may also be felt in different ways, because a woman's body can have individual characteristics.
Shortly before labor activity, the baby becomes “combat ready”. His head sinks into the pelvic ring more densely, due to which the woman's stomach is lowered. At this stage, the woman feels changes:
- relief;
- breathing becomes easier;
- sit more comfortably;
- the digestive system returns to normal;
- heartburn and some other symptoms of pregnancy go away.
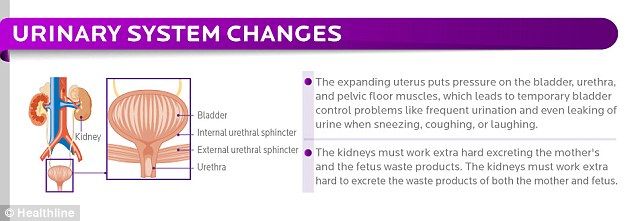
However, other unpleasant phenomena can be observed - mothers have frequent urination, because the fetus has descended and presses on the bladder and pelvic organs. The uterus and head may descend just before childbirth, or a few weeks before them.
Expansion of the pelvic bones
Women before childbirth may feel aching pain in the lumbar region, due to this expansion of the sacrum of the spine. The baby got stronger and became very heavy, he is ready to leave the nest and meet his mother, and therefore falls lower, which leads to the expansion of the pelvic bones. To alleviate pain and discomfort, doctors recommend a set of special exercises or swimming.
Also falling lower, the baby's head compresses the pelvic blood vessels, and this in turn causes swelling of the legs and cramps.
Braxton-Higgs contractions
Braxton-Higgs contractions are the body's warm-up before childbirth. The first false contractions may occur as early as 30 weeks, but become more frequent by 37-39 weeks. At this moment, a woman can imagine what she will feel before childbirth, only false contractions are not so painful and have a long interval. The first contractions preceding childbirth occur with a gap of 20 minutes, then the interval will be reduced.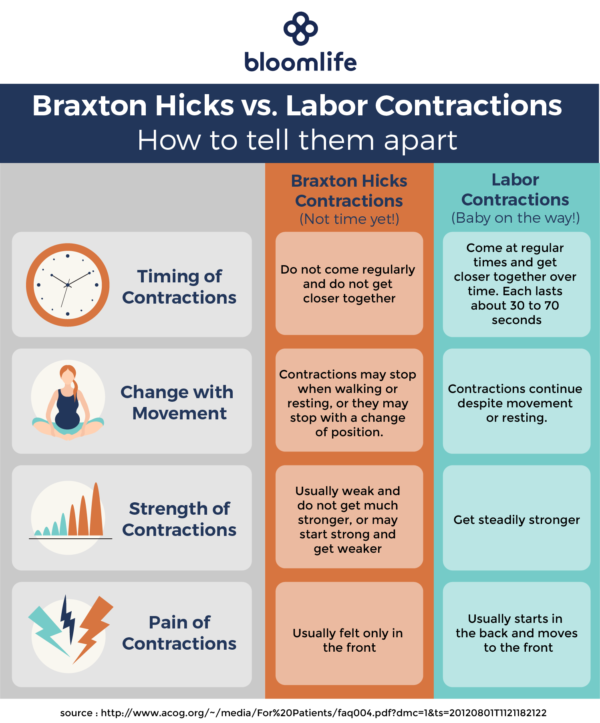 And false contractions are uneven, the gap between them can increase and decrease. Also, training contractions do not intensify, they are aimed at warming up, and not at opening the uterus.
And false contractions are uneven, the gap between them can increase and decrease. Also, training contractions do not intensify, they are aimed at warming up, and not at opening the uterus.
Removal of a mucus plug
The first symptoms of approaching labor include the removal of a mucus plug. The phenomenon manifests itself individually, in one woman she can leave a week or two before labor, in another just before the birth itself. The mucus plug sloughs off and exits through the vagina, this can happen piecemeal or all at once. Allocations are mucous clots of white, pinkish or red color. The latter indicate that labor activity will soon begin in the very near future.
Outflow of amniotic fluid
The main signs of approaching labor, preceding the onset of the process, are the discharge of amniotic fluid. The opening of the fetal bladder is considered normal not earlier than the middle of the first stage of labor. So, the cervix is only half dilated and mom has time to call an ambulance. At this moment, the baby feels discomfort, his house has become different and he wants to leave it. After the waters have broken, the fetus and uterus are vulnerable to infections from the outside world, and therefore you need to call an ambulance as soon as possible.
At this moment, the baby feels discomfort, his house has become different and he wants to leave it. After the waters have broken, the fetus and uterus are vulnerable to infections from the outside world, and therefore you need to call an ambulance as soon as possible.
Bladder rupture, most often does not cause pain. This may occur spontaneously and have no precursors in the form of spasms, contractions, or the urge to urinate. In order not to declare a false alarm and not confuse ordinary discharge with waste water, before childbirth, doctors recommend wearing a cotton diaper instead of a pad. The secretions will remain on the surface, and the diaper will absorb water.
Prenatal contractions
Signs of the onset of labor are regular and dynamic contractions. Such contractions begin with short spasms that do not cause severe pain. They occur with rhythmic frequency, and the interval between them is gradually reduced. Pauses allow the mother to gain strength and rest before the next contraction, because each time the contractions intensify, causing pain in the woman in labor.