Baby throwing up fever
Vomiting in children and babies
It's normal for babies and children to vomit occasionally. In most cases, it will last no longer than one to two days and isn't a sign of anything serious.
The most common cause of vomiting in children and babies is gastroenteritis. This is an infection of the gut usually caused by a virus or bacteria, which also causes diarrhoea. The symptoms can be unpleasant but your child will usually start to feel better after a few days.
However, persistent vomiting can sometimes cause your child to become severely dehydrated and occasionally it can be a sign of something more serious, such as meningitis.
This page outlines what to do if your child keeps vomiting and describes some of the common causes of vomiting in children and babies.
If your child has a high temperature, you can also read a separate page about fever in children.
What to do
If your child vomits, you should keep a close eye on them. Trust your instincts and contact your GP immediately if you're worried.
If the cause is just a tummy bug, your child should still be feeling well enough to eat, play and be their usual self. In this case, keep feeding them as normal and offer them regular drinks (see below).
But if they don't seem themself – for example, if they're floppy, irritable or less responsive – they may be seriously ill, so you should get medical help immediately.
When to get medical advice
You should contact your GP if:
- your child is repeatedly vomiting and is unable to hold down fluids
- you think they're dehydrated – symptoms of dehydration can include a dry mouth, crying without producing tears, urinating less or not wetting many nappies, and drowsiness
- their vomit is green or contains blood
- they have been vomiting for more than a day or two
Go to your nearest accident and emergency (A&E) department if your child is vomiting and develops sudden and severe tummy pain, or they're floppy, irritable or less responsive
Call 999 for an ambulance or go to your nearest A&E department immediately if they're vomiting and have a headache, stiff neck and a rash.
Looking after your child at home
In most cases, you can treat your child safely at home. The most important thing you can do is make sure they keep drinking fluids to prevent dehydration.
If your baby is vomiting, carry on breastfeeding or giving them milk feeds. If they seem dehydrated, they will need extra fluids. Ask your GP or pharmacist whether you should give your baby oral rehydration solution.
Oral rehydration solution is a special powder that you make into a drink. It contains sugar and salts to help replace the water and salts lost through vomiting and diarrhoea.
Children who are vomiting should keep taking small sips of clear fluid, such as water or clear broth. Fruit juice and fizzy drinks should be avoided until they're feeling better. If they're not dehydrated and haven't lost their appetite, it's fine for your child to eat solid foods as normal.
Again, speak to your GP or pharmacist if you're concerned about dehydration. They may recommend an oral rehydration solution for your child. Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
If your child has diarrhoea and is vomiting, they shouldn't go to school or any other childcare facility until 48 hours after the last episode of diarrhoea or vomiting.
Read more about treating gastroenteritis in children.
Causes of vomiting in children
There are a number of possible causes of vomiting in children, which are described below.
Gastroenteritis
Gastroenteritis is an infection of the gut. It's a common cause of vomiting in children and usually lasts a few days.
Food allergy
Food allergies can cause vomiting in children, as well as other symptoms, such as a raised, red, itchy skin rash (urticaria) and swelling of the face, around the eyes, lips, tongue or the roof of the mouth.
Watch out for foods that may bring on vomiting and see your GP for a diagnosis if you think your child may have a food allergy.
Other infections
Vomiting can sometimes be a sign of an infection other than gastroenteritis, such as urinary tract infections (UTIs), middle ear infections, pneumonia or meningitis.
Contact your child's GP if they're vomiting and experiencing additional symptoms of an infection, such as a high temperature (fever) and irritability.
Appendicitis
Appendicitis is a painful swelling of the appendix, a finger-like pouch connected to the large intestine. It causes severe tummy pain that gets worse over time.
If your child has tummy pain that's gradually getting worse, contact your GP, or if they aren't open call NHS 24's 111 service immediately. You should call 999 for an ambulance if they have pain that gets worse quickly and spreads across their tummy.
In most cases of appendicitis, the appendix will need to be surgically removed as soon as possible.
Poison
Accidentally swallowing something poisonous can cause your child to vomit. If you think this is the case, contact your GP immediately or take your child to your nearest accident and emergency (A&E) department.
Causes of vomiting in babies
These include:
- gastroenteritis
- a food allergy or milk intolerance
- gastro-oesophageal reflux – where stomach contents escape back up the gullet
- too big a hole in the bottle teat, which causes your baby to swallow too much milk
- accidentally swallowing something poisonous
- congenital pyloric stenosis – a condition present at birth where the passage from the stomach to the bowel has narrowed, so food is unable to pass through easily; this causes projectile vomiting
- a strangulated hernia – your baby will vomit frequently and cry as if they are in a lot of pain; this should be treated as a medical emergency
- intussusception (where the bowel telescopes in on itself) – as well as vomiting, your baby may look pale, floppy and have symptoms of dehydration
Gastroenteritis | NHS inform
Gastroenteritis is a very common condition that causes diarrhoea and vomiting. It's usually caused by a bacterial or viral tummy bug.
It's usually caused by a bacterial or viral tummy bug.
It affects people of all ages, but is particularly common in young children.
Most cases in children are caused by a virus called rotavirus. Cases in adults are usually caused by norovirus (the "winter vomiting bug") or bacterial food poisoning.
Gastroenteritis can be very unpleasant, but it usually clears up by itself within a week. You can normally look after yourself or your child at home until you're feeling better.
Try to avoid going to your GP, as gastroenteritis can spread to others very easily. Phone the 111 service or your GP if you're concerned or need any advice.
This page covers:
Symptoms of gastroenteritis
What to do if you have gastroenteritis
When to get medical advice
Looking after a child with gastroenteritis
Getting medical advice for your child
How gastroenteritis is spread
Preventing gastroenteritis
Symptoms of gastroenteritis
The main symptoms of gastroenteritis are:
- sudden, watery diarrhoea
- feeling sick
- vomiting, which can be projectile
- a mild fever
Some people also have other symptoms, such as a loss of appetite, an upset stomach, aching limbs and headaches.
The symptoms usually appear up to a day after becoming infected. They typically last less than a week, but can sometimes last longer.
What to do if you have gastroenteritis
If you experience sudden diarrhoea and vomiting, the best thing to do is stay at home until you're feeling better. There's not always a specific treatment, so you have to let the illness run its course.
You don't usually need to get medical advice, unless your symptoms don't improve or there's a risk of a more serious problem.
To help ease your symptoms:
- Drink plenty of fluids to avoid dehydration – You need to drink more than usual to replace the fluids lost from vomiting and diarrhoea. Water is best, but you could also try fruit juice and soup.
- Take paracetamol for any fever or aches and pains.
- Get plenty of rest.
- If you feel like eating, try small amounts of plain foods, such as soup, rice, pasta and bread.
- Use special rehydration drinks made from sachets bought from pharmacies if you have signs of dehydration, such as a dry mouth or dark urine – read about treating dehydration.

- Take anti-vomiting medication (such as metoclopramide) and/or antidiarrhoeal medication (such as loperamide) if you need to – some types are available from pharmacies, but check the leaflet that comes with the medicine. You can also ask your pharmacist or GP for advice about whether they're suitable.
Gastroenteritis can spread very easily, so you should wash your hands regularly while you're ill and stay off work or school until at least 48 hours after your symptoms have cleared, to reduce the risk of passing it on (see Preventing gastroenteritis).
When to get medical advice
You don't normally need to see your GP if you think you have gastroenteritis, as it should get better on its own.
Visiting your GP surgery can put others at risk, so it's best to phone 111 or your GP if you're concerned or feel you need advice.
Get medical advice if:
- you have symptoms of severe dehydration, such as persistent dizziness, only passing small amounts of urine or no urine at all, or if you're losing consciousness
- you have bloody diarrhoea
- you're vomiting constantly and are unable to keep down any fluids
- you have a fever over 38C (100.
 4F)
4F) - your symptoms haven't started to improve after a few days
- in the last few weeks you've returned from a part of the world with poor sanitation
- you have a serious underlying condition, such as kidney disease, inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your poo to a laboratory to check what's causing your symptoms. Antibiotics may be prescribed if this shows you have a bacterial infection.
Looking after a child with gastroenteritis
You can look after your child at home if they have diarrhoea and vomiting. There's not usually any specific treatment and your child should start feeling better in a few days.
You don't normally need to get medical advice unless their symptoms don't improve or there's a risk of a more serious problem.
To help ease your child's symptoms:
- Encourage them to drink plenty of fluids. They need to replace the fluids lost from vomiting and diarrhoea.
 Water is generally best. Avoid giving them fizzy drinks or fruit juice, as they can make their diarrhoea worse. Babies should continue to feed as usual, either with breast milk or other milk feeds.
Water is generally best. Avoid giving them fizzy drinks or fruit juice, as they can make their diarrhoea worse. Babies should continue to feed as usual, either with breast milk or other milk feeds. - Make sure they get plenty of rest.
- Let your child eat if they're eating solids and feel hungry. Try small amounts of plain foods, such as soup, rice, pasta and bread.
- Give them paracetamol if they have an uncomfortable fever or aches and pains. Young children may find liquid paracetamol easier to swallow than tablets.
- Use special rehydration drinks made from sachets bought from pharmacies if they're dehydrated. Your GP or pharmacist can advise on how much to give your child. Don't give them antidiarrhoeal and anti-vomiting medication, unless advised to by your GP or pharmacist.
Make sure you and your child wash your hands regularly while your child is ill and keep them away from school or nursery until at least 48 hours after their symptoms have cleared (see Preventing gastroenteritis).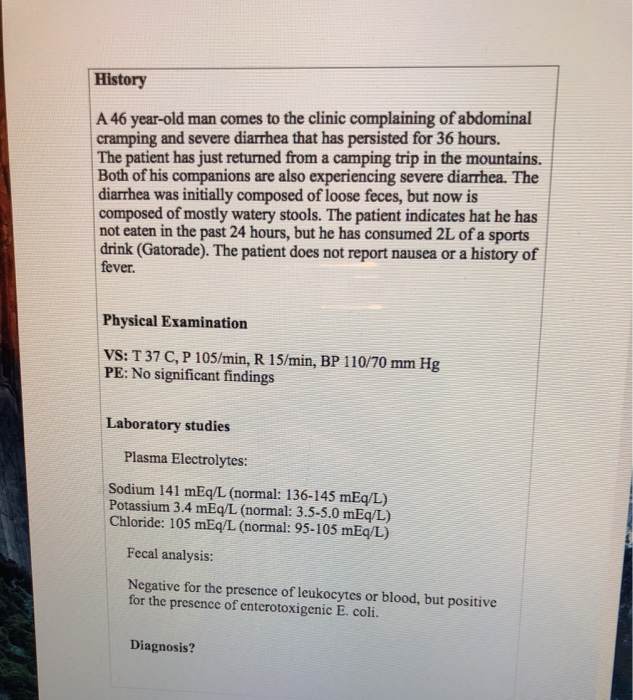
Getting medical advice for your child
You don't usually need to see your GP if you think your child has gastroenteritis, as it should get better on its own, and taking them to a GP surgery can put others at risk.
Phone the 111 service or your GP if you're concerned about your child, or they:
- have symptoms of dehydration, such as passing less urine than normal, being unusually irritable or unresponsive, pale or mottled skin, or cold hands and feet
- have blood in their poo or green vomit
- are vomiting constantly and are unable to keep down any fluids or feeds
- have had diarrhoea for more than a week
- have been vomiting for three days or more
- have signs of a more serious illness, such as a high fever (over 38C or 100.4F), shortness of breath, rapid breathing, a stiff neck, a rash that doesn't fade when you roll a glass over it or a bulging fontanelle (the soft spot on a baby's head)
- have a serious underlying condition, such as inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your child's poo to a laboratory to confirm what's causing their symptoms.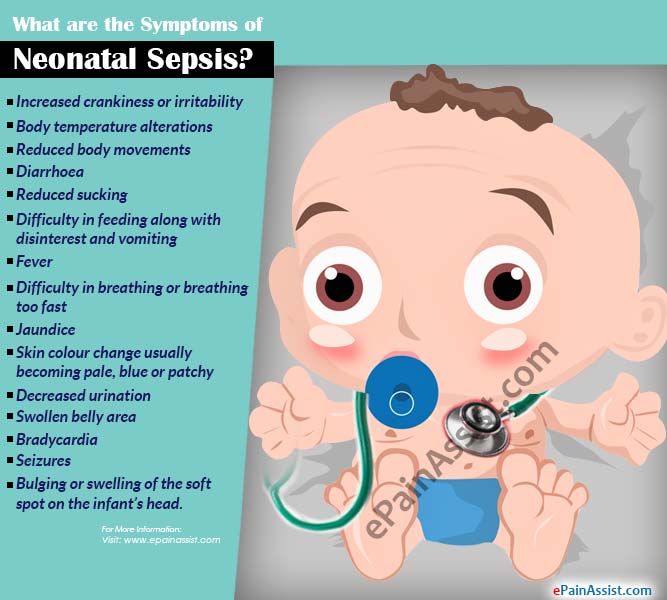 Antibiotics may be prescribed if this shows they have a bacterial infection.
Antibiotics may be prescribed if this shows they have a bacterial infection.
How gastroenteritis is spread
The bugs that cause gastroenteritis can spread very easily from person to person.
You can catch the infection if small particles of vomit or poo from an infected person get into your mouth, such as through:
- close contact with someone with gastroenteritis – they may breathe out small particles of vomit
- touching contaminated surfaces or objects
- eating contaminated food – this can happen if an infected person doesn't wash their hands before handling food, or you eat food that has been in contact with contaminated surfaces or objects, or hasn't been stored and cooked at the correct temperatures (read more about the causes of food poisoning)
A person with gastroenteritis is most infectious from when their symptoms start until 48 hours after all their symptoms have passed, although they may also be infectious for a short time before and after this.
Preventing gastroenteritis
It's not always possible to avoid getting gastroenteritis, but following the advice below can help stop it spreading:
- Stay off work, school or nursery until at least 48 hours after the symptoms have passed. You or your child should also avoid visiting anyone in hospital during this time.
- Ensure you and your child wash your hands frequently and thoroughly with soap and water, particularly after using the toilet and before preparing food. Don't rely on alcohol hand gels, as they're not always effective.
- Disinfect any surfaces or objects that could be contaminated. It's best to use a bleach-based household cleaner.
- Wash contaminated items of clothing or bedding separately on a hot wash.
- Don't share towels, flannels, cutlery or utensils while you or your child is ill.
- Flush away any poo or vomit in the toilet or potty and clean the surrounding area.
- Practice good food hygiene. Make sure food is properly refrigerated, always cook your food thoroughly, and never eat food that is past its use-by date – read more about preventing food poisoning.

Take extra care when travelling to parts of the world with poor sanitation, as you could pick up a stomach bug. For example, you may need to boil tap water before drinking it.
Young children can have the rotavirus vaccination when they’re 2 to 3 months old, which can reduce their risk of developing gastroenteritis.
Fever in children - NCCH
36.6˚ is the average normal body temperature for an adult. In children, the average body temperature is 0.3-0.4˚ C higher than in adults. In addition, the temperature in children is characterized by significant lability and its average fluctuations in newborns can be about 0.4 ° C, and in older children up to 1 ° C. Factors such as food intake, hunger, movement, restlessness, alternation of sleep and wakefulness. It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
Fever is an increase in body temperature ≥38˚ C, in most cases it is not dangerous, it is a normal physiological reaction of the body to infectious and non-infectious diseases. In young children, febrile illnesses are common and are usually caused by viral infections.
In the body, the role of the thermoregulation center is performed by the hypothalamus, the mechanism of its action is based on achieving a balance between heat production and heat loss.
Febrile convulsions are genetically determined, develop in 3-4% of children, as a rule, are not accompanied by epileptic activity of the brain, do not affect the further development of the child and do not recur after 6 years. In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever numbers.
In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever numbers.
Of course, one can understand the excitement of parents and grandparents when a child has a fever, but they need to remember that by lowering the temperature, especially low values, they calm themselves more than help the child. So, in most viral infections, only during an increase in temperature, antibodies to the virus and various active substances are produced that are responsible for the immune response and immunological memory. Therefore, an artificial decrease in temperature can lengthen the period of the disease. If a child has started antibiotic therapy for a bacterial infection, it is important to evaluate the effectiveness of the antibiotic, which can be seen primarily by self-reduction of body temperature. Against the background of antipyretics, this is quite difficult to do, and the sooner the child receives the correct treatment, the lower the risk of possible complications. Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Temperature reduction is carried out by physical cooling methods and, if necessary, medication. If the child does not have chills, marbling of the skin, the room should be ventilated, the child is open. With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin.
With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin. Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
It is not recommended to alternate paracetamol and ibuprofen, as well as to give their combined preparations, this combination is no more effective than monotherapy, but is fraught with serious side effects and can lead to acute renal failure. Also, nimesulide, acetylsalicylic acid preparations are not used in children with an antipyretic purpose, and metamizole (analgin) can only be administered intramuscularly in order to quickly reduce the temperature. All of these drugs can cause serious side effects that are incomparable to their antipyretic effect.
Usually a decrease in temperature by 0.5-1˚ C is sufficient to improve the child's well-being, it is not necessary to achieve a decrease in temperature to normal numbers. Large diurnal fluctuations in temperature may have a more significant negative effect than the fever itself.
We have already said above that fever in children is most often accompanied by acute infectious diseases, which can be of both viral and bacterial etiology. In the vast majority of cases, a viral infection does not require the appointment of an antibiotic (antibiotics do not act on viruses), children are treated with symptomatic agents and, if necessary, reduce the temperature. In the case of a proven bacterial etiology of the disease, it is necessary to prescribe antibiotic therapy. It is up to the doctor to decide what exactly the child is sick with, and, accordingly, how to treat him. However, if the disease begins with fever, runny nose and cough, the child's condition suffers slightly, with a high degree of probability one can think about the development of a respiratory viral infection and treat the child symptomatically. If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic. A disease that is not accompanied by catarrhal symptoms, a runny nose, should be more alert to both parents and doctors, due to the higher likelihood of any bacterial infection that needs to be diagnosed and treated in time. Although some viral infections, such as enterovirus, can also occur without any symptoms other than high fever.
Remember that antipyretics are also drugs! They have their side effects! In addition, the imaginary improvement in the child's well-being against the background of antipyretics should not be a reason for refusing timely examination by a pediatrician and prescribing the necessary treatment.
Site map - Nizhnevartovsk city emergency medical station
Version for the visually impaired
- Home
- About the establishment
- Documents
- Structure of the institution
- Community Council
- Information about medical workers
- Availability indicators
- Working hours of a medical organization
- Paid services
- Vacancies
- Supervisory authorities
- Photo reports
- Activities
- Information about work in the MHI system
- Unified portal of public services
- Career guidance.
 Targeted learning. Employment of graduates
Targeted learning. Employment of graduates - Anti-corruption activities
- Information for patients
- Social services to the population
- Patient Questionnaire
- How to get high-tech medical care
- Internal regulations for the consumer of services
- Standards for the scope of medical care
- Information for citizens in need of pain relief
- Target values of the criteria for the availability and quality of medical care
- Conditions and procedure for the provision of medical care established by the territorial CHI program
- Information materials on the implementation of the state guarantees program
- List of medicines, medical devices and specialty health foods
- List of types, forms and conditions for the provision of medical care, the provision of which is carried out free of charge
- List of drugs used in the outpatient treatment of children from large families
- Rights and obligations of citizens in the field of health care
- Rights and obligations of insured persons
- Contacts
- Make an appointment with a doctor
- For specialists
- Telephone directory
- Vacancies
- Information for medical staff
|