Frequent urination after childbirth
What’s ‘normal’ after giving birth?
Pregnancy and childbirth bring about many changes to our bodies. The process of recovery can be confusing and even overwhelming, and there is a great deal of misinformation out there.
Women come to InterMed Pelvic Floor Physical Therapy with many questions about their post-pregnancy bodies and symptoms. Our patients want to know if the changes are permanent. Will their symptoms ever go away, or do they just need to live with them as a new normal? What kind of recovery can be expected after giving birth? How long will that take?
The confusion often comes because some symptoms are considered normal for a period of time, and then become abnormal if they continue beyond that timeframe.
Our goal here is to answer questions and provide information about what is normal and to be expected with the three most common post pregnancy issues that result in a referral to Physical Therapy: bladder health and leakage, pain with sex, and Diastasis Recti Abdominus, a gap between your abdominal muscles.
What is considered normal bladder health after giving birth?
Urinary incontinence, or involuntary leakage of urine, is common for the first few months after giving birth. During the first 3 months, it’s normal to leak when you cough, sneeze, laugh, or lift your baby. It’s also normal to urinate more frequently or to have strong sudden urges. After the initial 3 months, normal urinary control should return. Some women see their symptoms gradually resolve, while others continue to struggle.
The strongest predictors of postpartum incontinence are:
- Low pelvic floor strength
- Incontinence prior to pregnancy
- New onset of incontinence during pregnancy
- Size of your newborn (greater than 6.6 pounds)
Women who do pelvic floor squeezes during their pregnancy and again at 12 weeks postpartum develop less incontinence than women who don’t do squeezes. Guidelines indicate that women who experience incontinence or other symptoms after 3 months would benefit from at least three physical therapy sessions focused on pelvic floor rehabilitation. Strengthening and coordinating these important muscles results in real positive changes for women.
Strengthening and coordinating these important muscles results in real positive changes for women.
Incontinence is generally treatable with physical therapy because it is a symptom of specific issues in the pelvic floor. As those issues are addressed, the incontinence should stop.
There is good research to support the benefit of seeking help. Studies have shown that women who receive pelvic floor physical therapy for incontinence after delivery continued to show benefits from treatment one year later. One study showed that pelvic floor training with biofeedback (a way for you to see how your muscles are working) resulted in an 88 percent improvement in symptoms.
No one is destined to leak after delivery. We often hear stories from patients who thought that they were supposed to leak because their mother did. If you find that you are still dealing with incontinence — even years later — ask for a referral. We’re here to help you.
Is sex supposed to hurt after having a baby?
During pregnancy, our pelvic floor muscles endure pressure as they support the growing baby.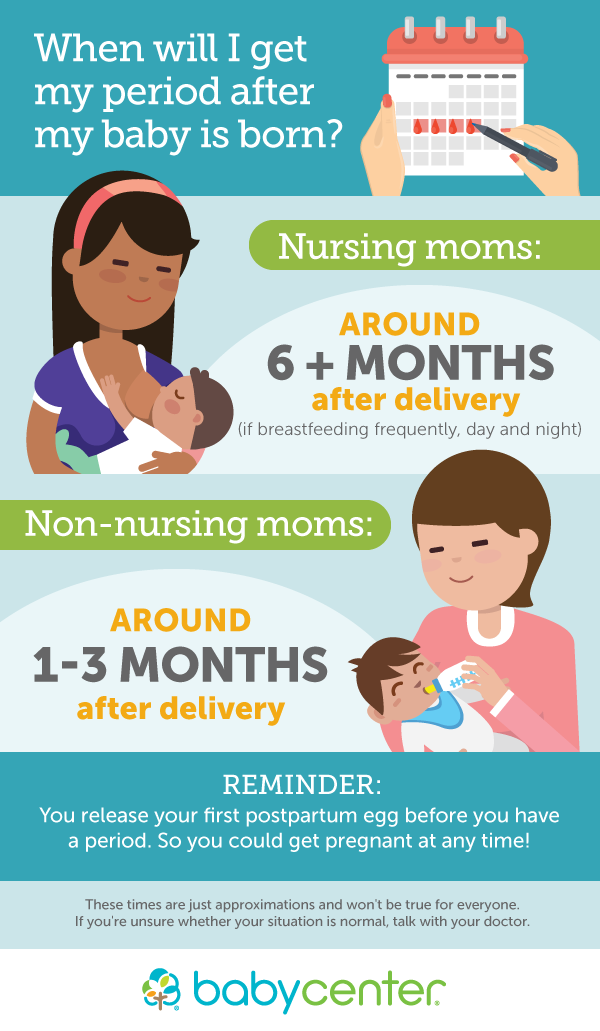 Our muscles also have to work harder to stabilize postural changes as the baby grows larger and heavier. During delivery, our pelvic muscles relax and stretch to allow the baby to be delivered. If the baby is large, or the delivery is difficult, these muscles can be injured. This can cause pain with sex. Returning to sex after having a baby can be a little scary. For the first few times, a little discomfort is normal, especially if there was a tear that required stitches.
Our muscles also have to work harder to stabilize postural changes as the baby grows larger and heavier. During delivery, our pelvic muscles relax and stretch to allow the baby to be delivered. If the baby is large, or the delivery is difficult, these muscles can be injured. This can cause pain with sex. Returning to sex after having a baby can be a little scary. For the first few times, a little discomfort is normal, especially if there was a tear that required stitches.
Pain during sex is called Dyspareunia. Studies have estimated that 85 percent of women experienced pain on their first attempt at sex postnatally. For most, pain decreases over time. For one in five women, the pain persists beyond a year.
Discomfort with intercourse and penetration should not continue. If dyspareunia isn’t getting better, speak with your provider. We are happy to help you find comfort again.
Is it normal to feel a split in my abdominal muscles above my belly button?
As the baby grows larger, the abdominal wall and abdominal muscles stretch to make room. After delivery, the muscles return to their starting point, but the soft tissue between the muscles can stay stretched out. This soft tissue, the linea alba, connects the left and right rectus abdominus muscles, often called the “six pack.” When this happens, the weak area in the center is called a Diastasis Recti Abdominus, or DRA. It can appear as a raised ridge in the middle of the abdomen above or below the belly button and is more prominent when you strain. A DRA is not a hernia because the abdominal wall is intact, just stretched out and thinned.
After delivery, the muscles return to their starting point, but the soft tissue between the muscles can stay stretched out. This soft tissue, the linea alba, connects the left and right rectus abdominus muscles, often called the “six pack.” When this happens, the weak area in the center is called a Diastasis Recti Abdominus, or DRA. It can appear as a raised ridge in the middle of the abdomen above or below the belly button and is more prominent when you strain. A DRA is not a hernia because the abdominal wall is intact, just stretched out and thinned.
Most women experience a DRA after delivery. For most, it will resolve or significantly lessen within 8 weeks. A DRA that is greater than 2cm (approximately the width of 2 finger tips side by side) is not normal and can contribute to a feeling of instability or back pain. Your physician can do a quick test to diagnose this common condition. Physical Therapy can help you to re-stabilize your abdominal muscles. It’s not enough to just strengthen – please don’t do crunches, as this can make the DRA worse.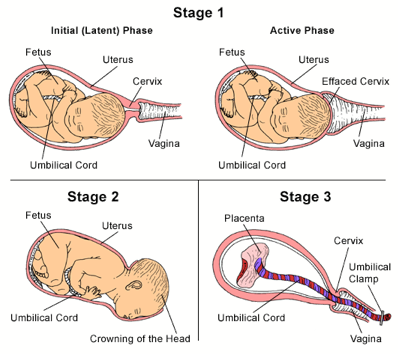 It’s important to learn to use your muscles in the pattern that supports core stability, and also gives your body the best chance of healing.
It’s important to learn to use your muscles in the pattern that supports core stability, and also gives your body the best chance of healing.
By Kate Bergeron PT, DPT, WCS; Jessica Clark, MPT; Nadia Sanchez, PT,DPT; Rosemarie Wagner PT,DPT
Is Overactive Bladder Normal After Birth?: BostonUrogyn: Urogynecologists
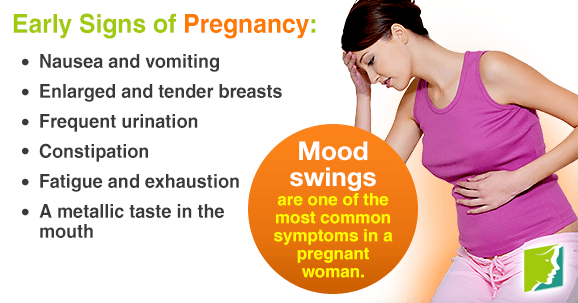
Is Overactive Bladder Normal After Birth?: BostonUrogyn: Urogynecologists During the COVID-19 Pandemic and Beyond, BostonUrogyn is Determined To Be There for You. We are now offering HIPAA-compliant Telemedicine Consultations, as well as Office Visits.When you were pregnant, you probably found yourself using the bathroom frequently, especially as your baby grew larger and put more pressure on your bladder. Maybe you’re noticing that this common issue doesn’t necessarily end just because you deliver.
Dr. Neeraj Kohli at Boston Urogyn understands the impact that bladder issues can have on your life. As a national and international leader in urogynecology and reconstructive pelvic surgery, he can identify what’s causing your urinary incontinence and offer innovative treatments to help.
As a national and international leader in urogynecology and reconstructive pelvic surgery, he can identify what’s causing your urinary incontinence and offer innovative treatments to help.
Understanding incontinence
There are several kinds of urinary incontinence. Two of the most common types associated with pregnancy are stress incontinence and overactive bladder.
Stress incontinence
Stress incontinence develops when you have increased pressure on your bladder. This can be due to your growing baby or from actions like coughing, laughing, or sneezing.
Overactive bladder
Overactive bladder typically causes an intense and urgent need to go. This issue usually occurs because your bladder muscles begin flexing and contracting involuntarily.
Approximately 54% of pregnant women have urinary incontinence symptoms that hinder their quality of life, both physically and emotionally. And, at least 7 million new mothers continue to struggle with bladder control issues, even after an uneventful pregnancy and delivery.
Pregnancy, childbirth, and incontinence
When you go through pregnancy and childbirth, several things can lead to incontinence problems, including:
- Weakening of the pelvic floor muscles
- Damage to nerves controlling your bladder
- Movement of your bladder and urethra during pregnancy
You also experience specific hormonal changes that prepare your body for childbirth. These changes, which are important because they increase the elasticity of your joints and tissues, also reduce bladder support.
For many women, urinary incontinence issues resolve within a year of childbirth. However, 30-50% report still having unwanted urinary leakage five years after delivery.
Treating overactive bladder and incontinence issues
Just because bladder issues are a normal part of pregnancy, you don’t have to continue to endure it. Dr. Kohli offers numerous solutions based on the severity of your symptoms.
During your appointment, Dr. Kohli performs a full physical exam to identify the specific cause of your incontinence issues. To treat problems like overactive bladder, he often recommends:
Kohli performs a full physical exam to identify the specific cause of your incontinence issues. To treat problems like overactive bladder, he often recommends:
- Medications designed to relax your bladder
- Physical therapy techniques to strengthen your pelvic floor muscles
- Botox® injections to temporarily disable your bladder muscles
- The InterStim™ system to restore healthy nerve function in the area
In addition to medical interventions for urinary incontinence, Dr. Kohli often makes lifestyle and behavioral recommendations as well. These approaches often include tracking your diet and fluid intake, addressing weight management issues, and undergoing bladder training. For severe incontinence cases, Dr. Kohli could suggest surgery.
To find help for your post-pregnancy overactive bladder and incontinence issues, visit one of our convenient locations in Wellesley or South Weymouth, Massachusetts. Give us a call at Boston Urogyn, send us a message here on our website, or request an appointment using our convenient online feature.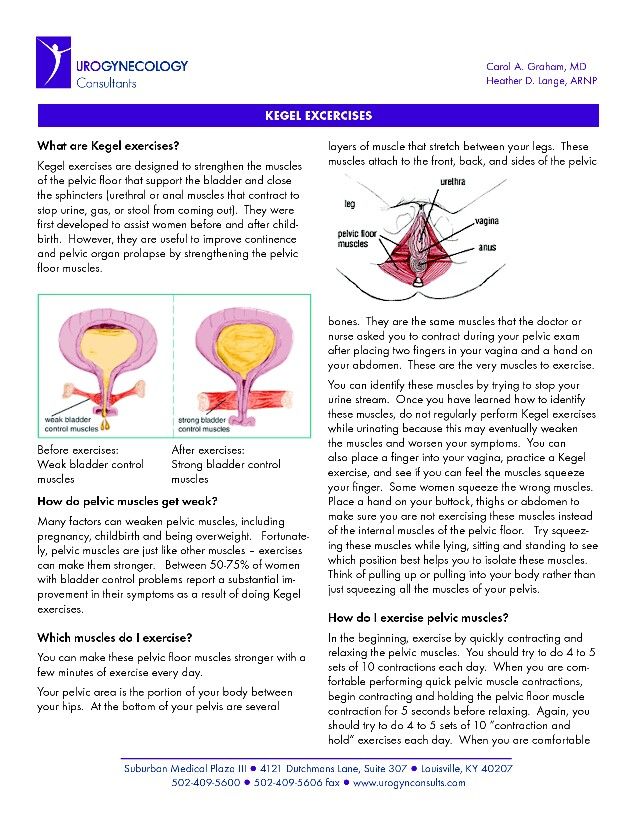
5 Common Signs of Lichen Sclerosus
Lichen sclerosus is an uncommon condition that affects the skin, most often around the genitals. Read on to learn the signs of lichen sclerosus and how it can be managed.
Signs That You Are Suffering from Vaginal Mesh Complications
Vaginal mesh is a treatment for women dealing with conditions like prolapse and urinary incontinence, but it’s not without problems. Here are signs you may be experiencing vaginal mesh complications.
Treatable Causes of Chronic Pelvic Pain
Your pelvis is the lowest part of your abdomen and is responsible for numerous bodily functions. Pain there can happen for a variety of reasons, but you don’t need to live with it. Let's look at some causes of pelvic pain and how we treat them.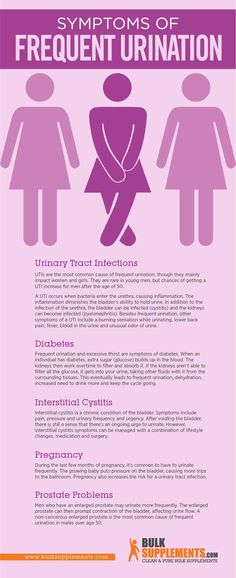
Axonics for Your Bladder and Bowel: What to Expect
The sudden urge to urinate associated with an overactive bladder can be embarrassing and disruptive to your quality of life. Many patients also experience fecal urgency and accidental bowel leakage. Read on to find out how Axonics® Therapy can help.
Nutrition Tips to Help Manage Fecal Incontinence
Fecal incontinence can dramatically affect your quality of life, so treating it is important to allow you to do the things you enjoy. The food you eat can play a role in managing or even preventing this condition. Read on to find out more.
It Shouldn’t Hurt When You Have Sex
Sex is a fundamental part of our lives, but experiencing pain while having sex shouldn’t be. If you’re a woman, read on to find out how you can avoid or treat painful intercourse.
Problems with urination after childbirth: pain, cramps, burning
PreviousNext
- Problems with urination after childbirth
- How to speed up the recovery of bladder functions
- It is recommended to consult a doctor
Contents:
During the postpartum period, many women have difficulty urinating. Lack of urge or, conversely, too frequent urge, pain, leakage when coughing or laughing is a consequence of stretching the muscles of the pelvic floor and reducing the tone of the bladder.
Problems with urination after childbirth
After giving birth, a woman may not feel like going to the toilet at all, even when her bladder is already full.
This is due to the fact that the pressure of the uterus on the bladder disappears, the tone of the bladder decreases, it increases in size, swells and begins to accumulate a lot of fluid. His sensitivity may decrease due to the use of painkillers in childbirth, muscle spasms, or fear of pain.
His sensitivity may decrease due to the use of painkillers in childbirth, muscle spasms, or fear of pain.
This problem does not require special treatment: gradually the tone of the bladder increases, the swelling subsides, and urination returns to normal. It’s just worth at first regularly reminding yourself that you need to visit the toilet.
Frequent and profuse urination in the first days after childbirth indicates the removal of excess fluid from the body. If you often want to go to the toilet, and the amount of urine is scanty, it is better to consult a doctor, as this may be a sign of the onset of inflammation of the bladder or urethra.
Most often, burning and pain are explained by the ingress of urine on abrasions that appeared during childbirth, and unhealed sutures. To reduce discomfort, you can urinate while standing in the shower with your legs wide apart so that the stream of urine does not touch the external genitalia.
If painful urination does not go away after healing of abrasions and stitches (usually on the second or third day) or the bladder itself hurts, this may be a symptom of urethritis or cystitis.
After natural childbirth, the pelvic floor muscles stretch and lose elasticity, relieving pressure on the bladder and urethra. As a result, the bladder loses its ability to close completely, so when laughing or coughing, a few drops of urine may be released. Many women are embarrassed by this delicate problem, but in fact, it can be dealt with with the help of sanitary pads and Kegel exercises.
How to speed up recovery of bladder function
If you find it difficult to get up, use the vessel, but not cold, but preheated. Urination can be caused reflexively - the sound of flowing water. If you couldn’t go to the toilet on your own, inform the nurse who will put the catheter.
-
Bladder exercise: do not reduce fluid intake, especially if breastfeeding.
-
Force the bladder to work: in the first days after childbirth, go to the toilet every two hours, even if you do not feel the urge.
-
Walk more: this stimulates the normal functioning of the intestines and bladder.
-
Do special pelvic floor exercises called Kegel exercises.
In a lying or sitting position, tighten the muscles of the vagina and anus as if you are holding back urination, stay in this position for a few seconds, and then completely relax the muscles. When doing the exercises, do not strain your stomach and buttocks and do not move your legs together. Kegel exercises are recommended to be done at least 3 times a day, and preferably more often. In one approach, it is optimal to perform 8–10 muscle contractions.
-
Refuse to use drinks and foods that irritate the bladder - coffee, hot spices, pickles, smoked meats.
It may take from several days to one and a half months to restore the normal functioning of the bladder. If during this time the incontinence does not go away, you need to inform the gynecologist about this at the scheduled examination, which usually happens six weeks after the birth.
It is recommended to see a doctor if:
-
after healing of tears or incisions in the perineum, you still experience pain or burning in the urethra or in the bladder area;
-
frequent urge to urinate, but scant amount of urine;
-
urine cloudy and with a sharp, unpleasant odor;
-
body temperature is increased, even slightly.
These symptoms may be a sign of the development of a urinary tract infection, which, if not properly treated, will cause pyelonephritis. Treatment today can be successfully combined with breastfeeding, so do not be afraid to seek medical help if your bladder does not work like clockwork after childbirth.
| Authors: | Huggies experts |
References:
-
Caring for your Bladder During and after Delivery.
 University of Michigan Health System.
University of Michigan Health System. -
Chaunie Brusie. Postpartum Incontinence Causes and Treatment. Verywell family. Updated on August 04, 2019.
-
After birth—bladder assessment. Mater Mothers' Hospital.
-
Urinary Incontinence and Pregnancy. WebMD.
-
10 truths: leaking urine in pregnancy and after birth. NCT UK.
Read us on Yandex Zen
PreviousNext
Urinary incontinence and other health issues after childbirth - Useful articles
There are two types of incontinence: in one case it is associated with an irresistible urge (as they say, "did not reach the toilet"), in the other case, involuntary urination occurs when intra-abdominal pressure increases during exercise , laughing, coughing, sneezing, etc. There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
The problem in most cases is not solved by itself, causing physical and psychological inconvenience and suffering (the need to walk around with pads and diapers) and reducing the quality of life, including intimate life. They are embarrassed to talk about it, and compared to how many people are prone to this problem, only a few seek help. Often they simply do not know who exactly to turn to - they go to a gynecologist, and to a therapist, and to a neuropathologist, while this should be done comprehensively and always with the participation of a urologist.
Therapeutic exercise for incontinence
In women after childbirth, disorders of vascular circulation and nervous regulation in the pelvic area are not uncommon. If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
1. Slow contractions: tighten the muscles as if to stop urination, slowly count to three. To relax.
2. Contractions: tense and relax these same muscles as quickly as possible.
3. Push-ups: tense the perineum and abdominal muscles.
Special therapeutic exercises also help to strengthen the muscles of the small pelvis.
1. I.P. lying on your back. We exhale, draw in the stomach, pull the knees to the chest.
2. I.P. Same. Alternately raise straight legs and make circular movements out and in with full amplitude.
3. From the same position, on exhalation, we pull the chest to the bent knees and clasp them with our hands.
4. Now we raise the upper part of the body and sit down, wrapping our arms around our knees.
5. At the expense of 1-2-3, raise the upper body and one leg, to which we reach with the same hand. We go down to count 4.
6. Knees bent. At the expense of 1-2-3, we raise the pelvis, squeeze the buttocks, retract the anus. On the count of 4, lower the pelvis and relax.
7. From the same position, we lay bent knees to the right and left of the body.
8. I.P. standing, with support. On the inhale we rise on our toes, on the exhale we squat, holding on to the chair.
9. In the same position, holding on to the support, we roll from toes to heels and back.
10. I.P. On knees. Sit on your heels, stretch your arms up.
11. From the same position, alternately straighten the legs and pull them back. Shoulders-back-leg at the same time form one straight line.
12. Standing on all fours, alternately pull opposite arm and leg: straighten on the count of times, hold 2-3, return to the starting position on the count of 4. Be careful not to arch your back.
Be careful not to arch your back.
13. From the same starting position on count 1 stretch one leg back, on count 2-3 take it to the side parallel to the floor, bending at the knee, on count 4 return to the starting position.
14. I.P. hands on the belt, one foot is on the chair. We lean forward and reach for the raised leg, bending it at the knee as much as possible.
There is no need to despair: although treatment is not an easy process due to the large number of components involved in the formation of this syndrome, it is very effective. In all cases, it begins with conservative methods: medicines, physiotherapy and, of course, the therapeutic exercises we have already mentioned. Refrain from activities that increase intra-abdominal pressure. If conservative treatment does not help, low-traumatic surgical methods come to the rescue in the form of imposing various types of loops.
Problems in the perineum
During childbirth, injuries to the soft tissues of the perineum are possible.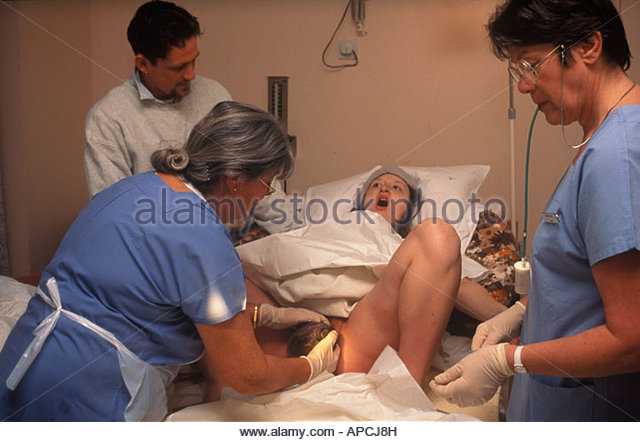 Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Sometimes an episiotomy is done for the benefit of the baby and mother. Healing is very fast due to tissue matching and a powerful hormonal explosion. The main task of the mother, if she has stitches, is to keep them clean. This, of course, is hygiene (washing twice a day, from front to back, you can use a decoction of chamomile or a weak solution of potassium permanganate) and ensuring oxygen access. Associated with the latter is the ban on underwear and pads, which causes violent protest among women in maternity hospitals.
One should not underestimate such an important moment as the normalization of the stool on the third day after childbirth. Defecation does not provoke the divergence of the sutures, on the contrary, this stool retention can lead to trouble, so try to achieve a soft and spontaneous stool by the third day, and upon returning from the hospital, consult a doctor to make sure that the sutures are healing correctly, without divergence and suppuration.
Uterus and vagina
Some women who have recently given birth complain of vaginal gaping, even asking to "sew it up so that it was like before." Bringing the vaginal ring back to normal is really very important, but this process takes some time. During childbirth, the vagina stretches to let the baby through. Closing occurs within six months, which can be accelerated, for example, by the already mentioned Kegel exercise or the mixing-breeding of the legs.
Immediately after delivery, the uterus should empty well, so turn over, give a vertical load. This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
The return of the tone of the soft tissues of the perineum will also be helped by sexual intercourse, which improves tissue nutrition. Please note: they are allowed when the placental site has been restored in the uterine cavity and there is no longer a risk of inflammation. If you feel pain during intercourse, do not hesitate to tell the doctor about it - he will find out the reason and advise the appropriate position.
Hemorrhoids
Another problem after the birth of a baby is hemorrhoids - a frequent manifestation of varicose veins.