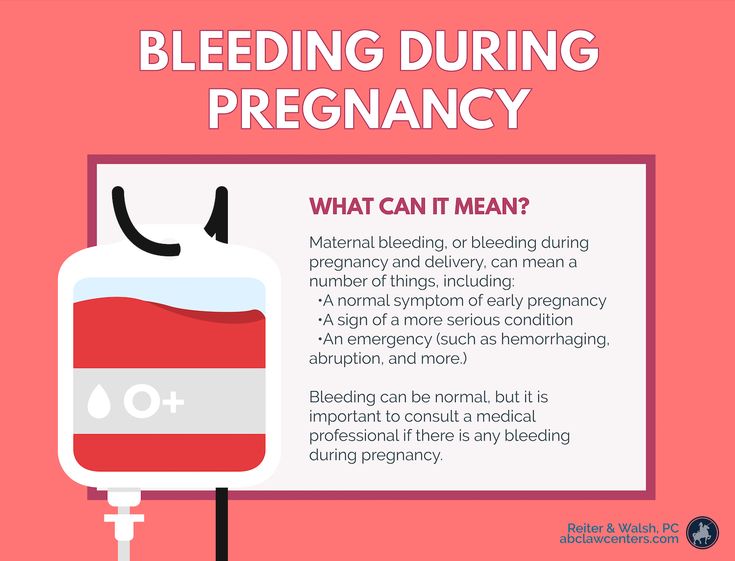
Spotting during end of pregnancy
Vaginal bleeding in late pregnancy Information | Mount Sinai
What Causes Bleeding Later in Pregnancy?
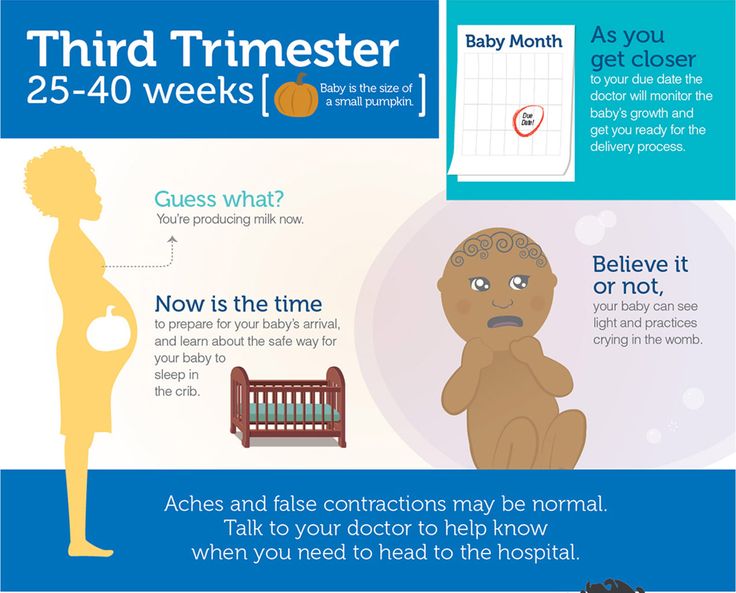
When labor begins, the cervix starts to open up more, or dilate. You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
Mid- or late-term bleeding may also be caused by:
- Having sex (most often just spotting)
- An internal exam by your provider (most often just spotting)
- Diseases or infections of the vagina or cervix
- Uterine fibroids or cervical growths or polyps
More serious causes of late-term bleeding may include:
- Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
- Placenta abruptio (abruption) occurs when the placenta separates from the inner wall of the uterus before the baby is born.
What to Tell Your Health Care Provider
To find the cause of your vaginal bleeding, your provider may need to know:
- If you have cramping, pain, or contractions
- If you have had any other bleeding during this pregnancy
- When the bleeding began and whether it comes and goes or is constant
- How much bleeding is present, and whether it is spotting or a heavier flow
- The color of the blood (dark or bright red)
- If there is an odor to the blood
- If you have fainted, felt dizzy or nauseated, vomited, or had diarrhea or a fever
- If you have had recent injuries or falls
- When you last had sex and if you bled afterward
What Should Happen Next?
A small amount of spotting without any other symptoms that occurs after having sex or an exam by your provider can be watched at home. To do this:
- Put on a clean pad and recheck it every 30 to 60 minutes for a few hours.
- If spotting or bleeding continues, call your provider.
- If the bleeding is heavy, your belly feels stiff and painful, or you are having strong and frequent contractions, you may need to call 911 or your local emergency number.
For any other bleeding, call your provider right away.
- You will be told whether to go to the emergency room or to the labor and delivery area in your hospital.
- Your provider will also tell you whether you can drive yourself or you should call an ambulance.
Baeseman ZJ. Vaginal bleeding in pregnancy. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier 2021:1227-1229.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Last reviewed on: 10/5/2020
Reviewed by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.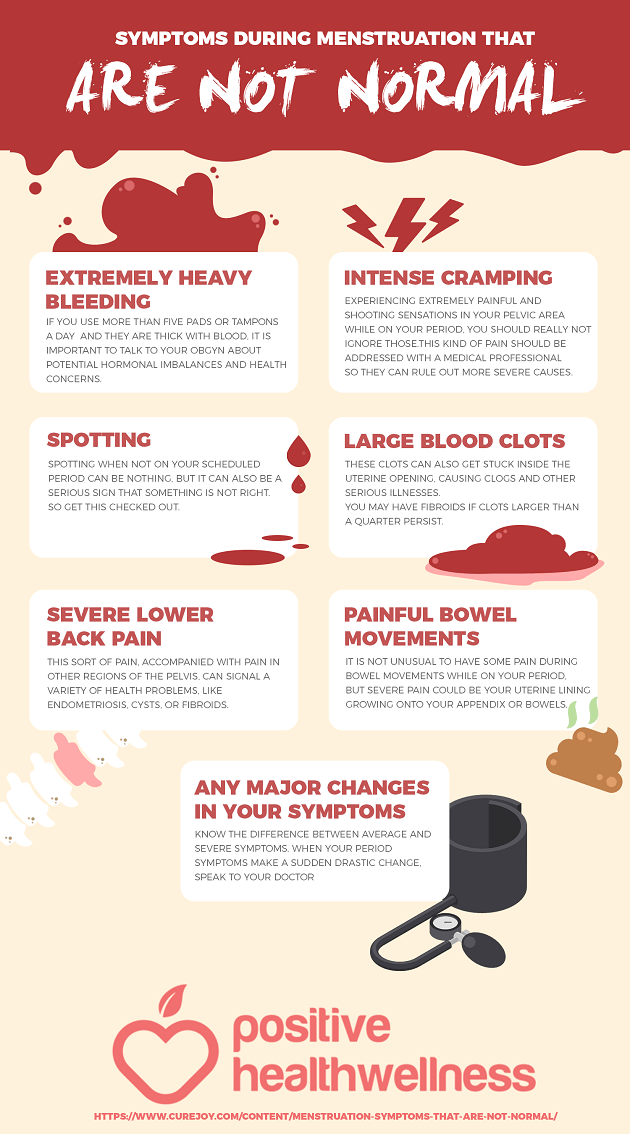 D.A.M. Editorial team.
D.A.M. Editorial team.
Vaginal bleeding in late pregnancy: MedlinePlus Medical Encyclopedia
One out of 10 women will have vaginal bleeding during their 3rd trimester. At times, it may be a sign of a more serious problem. In the last few months of pregnancy, you should always report bleeding to your health care provider right away.
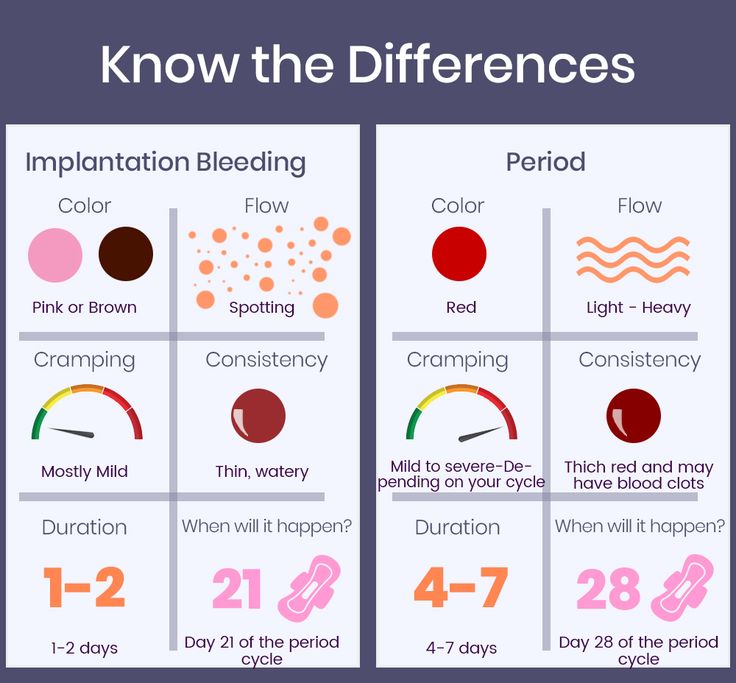
You should understand the difference between spotting and bleeding:
- Spotting is when you notice a few drops of blood every now and then on your underwear. It is not enough to cover a panty liner.
- Bleeding is a heavier flow of blood. With bleeding, you will need a liner or pad to keep the blood from soaking your clothes.
When labor begins, the cervix starts to open up more, or dilate. You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
Mid- or late-term bleeding may also be caused by:
- Having sex (most often just spotting)
- An internal exam by your provider (most often just spotting)
- Diseases or infections of the vagina or cervix
- Uterine fibroids or cervical growths or polyps
More serious causes of late-term bleeding may include:
- Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
- Placenta abruptio (abruption) occurs when the placenta separates from the inner wall of the uterus before the baby is born.
To find the cause of your vaginal bleeding, your provider may need to know:
- If you have cramping, pain, or contractions
- If you have had any other bleeding during this pregnancy
- When the bleeding began and whether it comes and goes or is constant
- How much bleeding is present, and whether it is spotting or a heavier flow
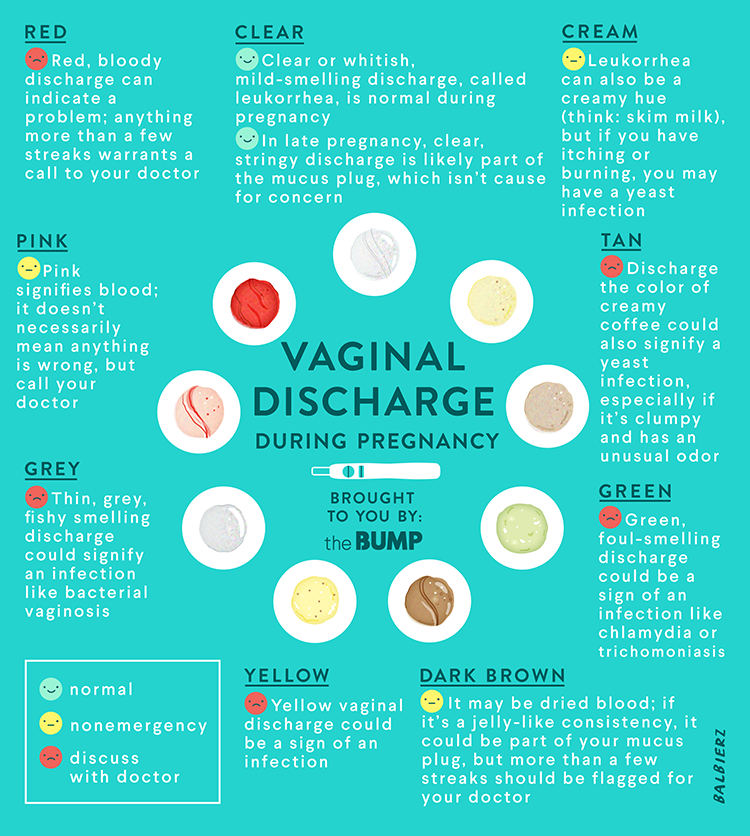
- The color of the blood (dark or bright red)
- If there is an odor to the blood
- If you have fainted, felt dizzy or nauseated, vomited, or had diarrhea or a fever
- If you have had recent injuries or falls
- When you last had sex and if you bled afterward
A small amount of spotting without any other symptoms that occurs after having sex or an exam by your provider can be watched at home. To do this:
- Put on a clean pad and recheck it every 30 to 60 minutes for a few hours.
- If spotting or bleeding continues, call your provider.
- If the bleeding is heavy, your belly feels stiff and painful, or you are having strong and frequent contractions, you may need to call 911 or your local emergency number.
For any other bleeding, call your provider right away.
- You will be told whether to go to the emergency room or to the labor and delivery area in your hospital.
- Your provider will also tell you whether you can drive yourself or you should call an ambulance.
Baeseman ZJ. Vaginal bleeding in pregnancy. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier 2021:1227-1229.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae.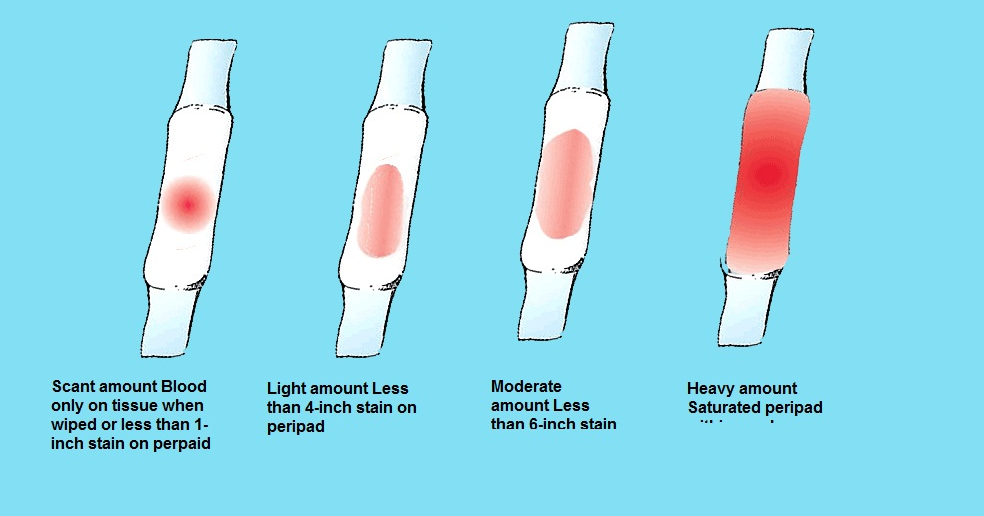 In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
What is it? Normal and abnormal discharge during pregnancy
Today we will talk with Elena Yurievna Romanova, an obstetrician-gynecologist at the Expert Center for Pregnancy Management at the Mother and Child Clinic, about what discharges during pregnancy should be feared and what discharges from the genital tract are regarded as normal.
Increased vaginal discharge during pregnancy is natural
Normal pregnancy discharge is milky white or clear mucus without a strong odor (although the smell may change from before pregnancy), this discharge does not irritate the skin and does not cause discomfort to the pregnant woman. The discharge can have a different color - from completely colorless (most often) to whitish and yellowish. The consistency of discharge at the beginning of pregnancy resembles raw chicken yolk - they are thick, jelly-like, often released in the form of clots. nine0003
With normal discharge, it is enough to use panty liners or change underwear twice a day.
Due to the activity of progesterone in the first 12 weeks of pregnancy, the discharge will be scarce and viscous.
Due to the increase in estrogen activity from 13 weeks, the discharge becomes less viscous and more abundant.
By the end of the pregnancy, vaginal discharge becomes more and more abundant.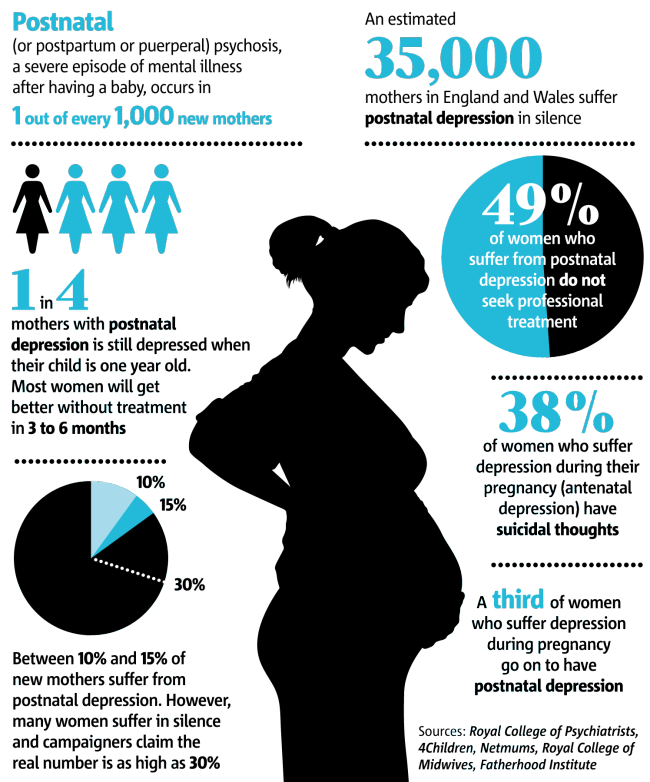 Each time you need to evaluate the nature of the discharge, change the gasket. If the fluid continues to ooze, this may mean leakage of amniotic fluid and the need to contact an obstetrician-gynecologist in the emergency department of a hospital with a maternity ward. There are auxiliary tests, thanks to which, as well as obstetric ultrasound, leakage of water can be excluded. nine0003
Each time you need to evaluate the nature of the discharge, change the gasket. If the fluid continues to ooze, this may mean leakage of amniotic fluid and the need to contact an obstetrician-gynecologist in the emergency department of a hospital with a maternity ward. There are auxiliary tests, thanks to which, as well as obstetric ultrasound, leakage of water can be excluded. nine0003
Not all discharge in pregnant women is the norm.
For example, a white, thick, crumbly, odorless discharge that itchs and burns the skin and causes discomfort during intercourse is likely a sign of a yeast infection (candidiasis).
White or grayish discharge, the smell of which after sex begins to resemble the smell of fish, is the main symptom of bacterial vaginosis, vaginal dysbacteriosis.
A yellowish or greenish discharge that has a strong unpleasant odor usually occurs with nonspecific vaginitis, and a foamy discharge is a sign of trichomoniasis, a sexually transmitted disease.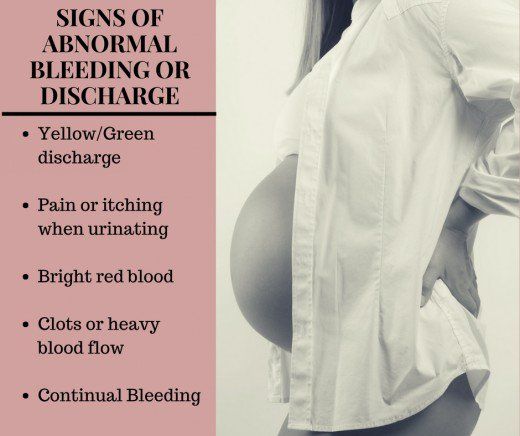 nine0003
nine0003
In all these cases, contact your doctor immediately. It should not be treated with over-the-counter drugs and folk remedies. According to some external signs, a diagnosis cannot even be made by a doctor, in addition, infections in pregnant women should be treated especially carefully and only by a professional. After proper treatment, the discharge returns to normal. There is no need to get rid of the usual discharge for pregnant women. After childbirth, they will stop naturally, and before that they are a sign of the normal course of pregnancy. nine0003
Allocations can change their nature and amount under the influence of irritants or intolerance to a particular substance, for example, when using panty liners. Such secretions are transparent and abundant, they stop when the irritant is removed.
"Thrush" is a disease caused by fungi of the genus Candida, present in small quantities in all women. During pregnancy, immunity decreases and fungi begin to actively multiply, causing inflammation, abundant white flocculent discharge with a sour smell, burning and itching in the vulva. The disease can manifest itself throughout pregnancy. nine0003
The disease can manifest itself throughout pregnancy. nine0003
Bloody discharge in the first half of pregnancy usually indicates a lack of the hormone progesterone, which can lead to spontaneous miscarriage. Discharge may be accompanied by pain in the lower abdomen and lower back. In the treatment of the threat of abortion, the appointment of progesterone drugs, such phenomena disappear.
If bleeding from the vagina appeared during pregnancy during the second or third trimester, then this is a sign of a formidable complication, namely, placenta previa or its premature detachment. With improper attachment of the placenta in the uterine cavity and overlapping of the placental tissue with the area of the internal pharynx, they speak of placenta previa. In this case, spotting occurs in a third of pregnant women. This most often occurs between 28 and 30 weeks, when the lower segment of the uterus is most prone to stretching and thinning. The discharge is repeated, the woman does not experience any pain, so it may be too late to see a doctor for an examination.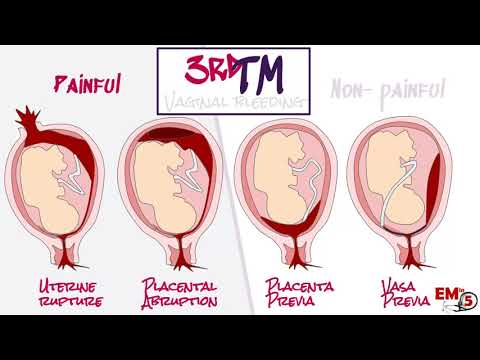 This threatens the child with a lack of nutrients and oxygen, because it is through the placenta that the fetus is nourished. For a pregnant woman, this is fraught with acute placental abruption and severe bleeding, which is always problematic to stop, especially at home. nine0003
This threatens the child with a lack of nutrients and oxygen, because it is through the placenta that the fetus is nourished. For a pregnant woman, this is fraught with acute placental abruption and severe bleeding, which is always problematic to stop, especially at home. nine0003
Bloody discharge during pregnancy should force a woman to immediately contact her obstetrician-gynecologist.
Brown discharge during pregnancy also indicates the threat of termination of pregnancy, or bleeding "erosion" (decidual polyp) of the cervix. Therefore, you should not understand these issues on your own; when brown discharge appears, it is better to consult your doctor.
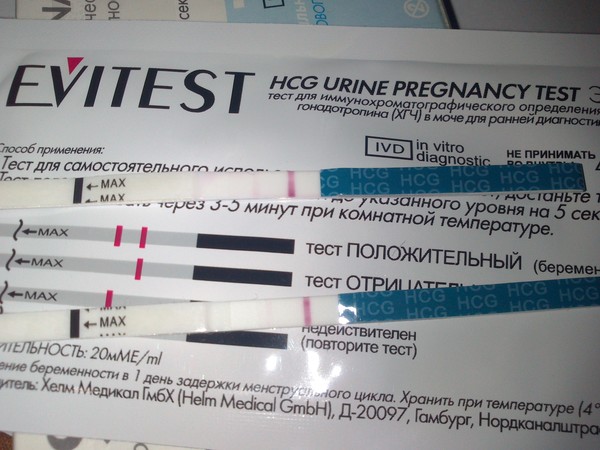
Brown discharge during a delay in menstruation as a sign of an ectopic pregnancy is very dangerous. This condition requires immediate surgical care, as the growing embryo can rupture the wall of the fallopian tube at any time and cause internal bleeding. Therefore, with pain in the lower abdomen, which is accompanied by brown discharge from the genital tract and delayed menstruation, you should immediately call an ambulance. nine0003
nine0003
When the vagina becomes inflamed, the mucous discharge acquires a mucopurulent character, a greenish-yellow color, an unpleasant odor, burning and itching appear in the genital area. This is how chlamydia, mycoplasmosis, ureaplasmosis, trichomoniasis manifest themselves. Is it necessary to treat the infection during pregnancy, or is it better to do it after childbirth?
All sexually transmitted infections in pregnant women require treatment, as they can pass to the fetus and cause intrauterine infection (IUI). IUI is very dangerous for a child - it leads to his death or serious illness. Infection of a child during childbirth can lead to such serious complications as pneumonia, severe damage to the brain, kidneys, liver, and blood poisoning (sepsis). nine0003
Today, obstetricians and gynecologists have learned to treat any infection in pregnant women in accordance with special guidelines for the timing of pregnancy, so that it is effective and safe for mother and fetus. It is not the treatment that should be feared, but the infection itself and its consequences.
It is not the treatment that should be feared, but the infection itself and its consequences.
Medicines that are used to treat pregnant women have passed the necessary clinical trials, during which it was proved that they do not have a negative effect on the pregnant woman and the fetus, including that they do not have a teratogenic effect (do not cause deformities in the fetus). nine0003
Sometimes the discharge is mucous in nature, occurs upon contact with an irritant or allergen. It can be synthetic tight underwear, allergies to fabrics, toiletries, personal care products. If irritation and allergens are not eliminated in time, then an infection that lives on the mucous membranes of the genital organs will definitely join.
Hygiene measures are mandatory for pregnant women. Twice a day you need to take a warm shower, using special gels for pregnant women to wash the genitals. Be sure to monitor the cleanliness of the whole body and underwear - it must be changed daily. Pads (but not tampons!) can be used for discharge. The oral cavity can become the source of infection, so you need to monitor your teeth, brush them twice a day and get an examination by a dentist. Good nutrition strengthens the immunity of a pregnant woman. The diet should contain fresh vegetables and fruits, lean meats and fish, daily dairy products, vegetable oil, a variety of cereals. nine0003
Pads (but not tampons!) can be used for discharge. The oral cavity can become the source of infection, so you need to monitor your teeth, brush them twice a day and get an examination by a dentist. Good nutrition strengthens the immunity of a pregnant woman. The diet should contain fresh vegetables and fruits, lean meats and fish, daily dairy products, vegetable oil, a variety of cereals. nine0003
A mobile lifestyle, therapeutic exercises and maximum exposure to fresh air are very important. Hiking is useful even at the very end of pregnancy - they will help not only maintain immunity, but also strengthen the muscles that will be required during childbirth. Be healthy!
Pregnancy discharge | What are the discharge during pregnancy? | Blog
In the absence of menstruation, girls usually suspect that conception has occurred. However, during pregnancy, the female body may continue to secrete a secret of a different color and character. We recommend that you keep a close eye on everything that happens so as not to miss the development of adverse events. We will talk about how to recognize problem situations during pregnancy in the article. nine0003
We will talk about how to recognize problem situations during pregnancy in the article. nine0003
What secretions can occur during conception
Many women note that immediately after the delay and in the later stages, the nature of the secretion changes. It can be:
- With or without scent.
- Depending on the color - transparent, white, cream, yellow, greenish, bloody.
- By consistency - thick, liquid, cheesy.
- As a symptom for assessing the state of health - threatening, safe.
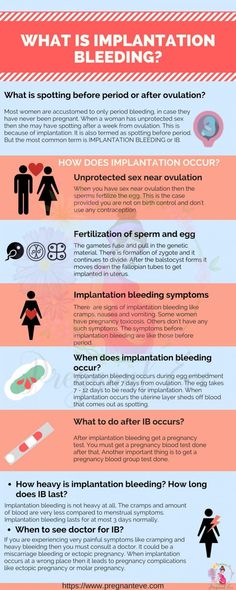
During ovulation, the egg is released from the ovary, its membrane is blown away, a small amount of fluid is released - so it becomes ready for fertilization. At this time, the thick mucus that fills the cervical canal of the cervix becomes less viscous. This makes it easier for the spermatozoa to penetrate and move further into the tubes for fertilization. At this time, you may notice an abundance of clear mucous secretion.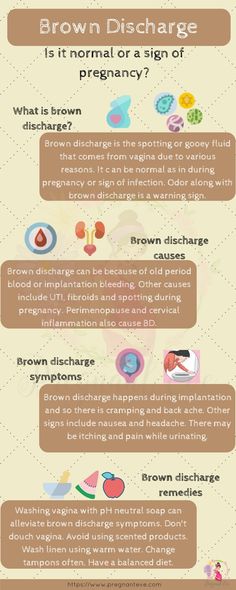
After the fusion of the egg with the spermatozoon, movement into the uterus begins, which should end with implantation in the inner layer. During penetration, its slight detachment may occur - this causes damage to the blood vessels that abundantly penetrate the muscular layer of the uterus. You may see light brown discharge, which is common during pregnancy. The color is due to the fact that the blood has time to clot. nine0003
Sometimes the discharge is brightly colored and some women mistake it for early menses. But in this case, a short duration is characteristic, a different shade (dark or scarlet), a slight mark on the linen.
With some features of the structure of the female genital organs (for example, with a bicornuate uterus), after implantation of the embryo in one part, rejection of the endometrium may begin in the other, as is usually the case with menstruation. This rarely happens.
Characteristics of discharge in case of threatened miscarriage
Spontaneous abortion is the rejection of an embryo in the early stages after conception. If at the first signs of pregnancy, you notice spotting, there is a high probability that a miscarriage begins.
If at the first signs of pregnancy, you notice spotting, there is a high probability that a miscarriage begins.
Also, miscarriage symptoms include:
- pulling or pressing on the lower abdomen, sacrum, lower back;
- the muscles of the uterus are tense.
The woman may experience cramps. This continues all the time or intermittently. From the vagina there are scarlet or brown discharge during pregnancy, which was previously confirmed. Sometimes the period may be still small, and the first signs did not have time to appear. nine0003
After 22 weeks, this phenomenon is called preterm labor. The child in this case is still weak, the organs are not sufficiently developed, and there is little chance of survival.
The following factors increase the risk of miscarriage:
- various diseases;
- progesterone deficiency;
- nervous and physical strain;
- pathologies in the genitals;
- fetal developmental defects.
To confirm the diagnosis, the doctor prescribes an ultrasound scan. If it shows that the fetal heart rate is disturbed, the tone of the uterus is increased, its size differs from normal for this period, hospitalization will be recommended to maintain pregnancy. nine0003
What discharge during pregnancy is considered normal
This secretion does not pose a threat to health:
- transparent;
- whitish;
- yellowish;
- odor free;
- mucous;
- without itching, burning, redness of the genitals.
Clear fluid on underwear is a symptom of ovulation. During pregnancy, the activity of ongoing processes in the body increases, so the amount of secretion secreted may increase. However, a violation of the norm is the leakage of amniotic fluid. You can determine the problem with the help of special diagnostic tests that the doctor will prescribe if he has suspicions. nine0003
White color, small amount, homogeneous structure should also not cause concern. The increased volume of fluid in this case is associated with increased hormonal activity.
The increased volume of fluid in this case is associated with increased hormonal activity.
One of the variants of the norm is mucous discharge, which smells of slight sourness. If there is no pain, discomfort, there is nothing to worry about.
Yellow discharge, there are signs of pregnancy, there is no unpleasant odor - you are all right. Some women had this color before conception, only they did not pay attention. Now there are more of them, therefore more noticeable. nine0003
Sometimes a woman observes that the laundry gets wet and there is a smell of urine. This may indicate incontinence due to the constant pressure of the growing uterus. In this case, it is recommended to go to the toilet more often, change underpants twice a day.
What discharge during pregnancy is considered a sign of infection?
White discharge during pregnancy with a cheesy texture is a symptom of thrush (candidiasis). In pregnant women, it is diagnosed quite often - the reason is a change in hormonal levels. The disease is accompanied by itching, redness of the vulva, a strong sour smell. Sometimes external manifestations are not detected, then treatment is not carried out. nine0003
The disease is accompanied by itching, redness of the vulva, a strong sour smell. Sometimes external manifestations are not detected, then treatment is not carried out. nine0003
Infection is indicated by pain, pain, skin irritation, ulcers, smell of rot or fish, gray or green color, frothy discharge, increased nervousness, large inguinal lymph nodes. The reason may lie in sexually transmitted infections. This includes syphilis, gonorrhea, trichomoniasis, chlamydia and others. They are dangerous because they cause premature birth and fetal developmental defects.
What kind of discharge during pregnancy should I pay special attention to and should I consult a doctor? nine0061
The following indicates that pregnancy is at risk:
- Severe pain in the perineum, bleeding, difficulty defecation, convulsions - these may be injuries to the vaginal mucosa.
- Nausea, profuse vomiting, edema, headaches, cough, hypertension, bright red secretion are symptoms of hydatidiform mole (abnormal development of the embryo).
- A drop in blood pressure, pallor, weakness, sweating, pulling sensations, bleeding during pregnancy against the background of a lack of growth of hCG in the blood - this is how an ectopic attachment manifests itself. nine0066
- Discharge of clots, sharp pain, vomiting, diarrhea may indicate a frozen fetus.
If you experience any of these symptoms, contact your doctor immediately.
It is also necessary to contact the clinic if you have been physically abused, had rough sex, had an accident, fell, hit. The likelihood that the situation will be resolved successfully is much higher if you do not delay the visit, listen to the symptoms and take good care of your health. nine0003
Remember, despite the fact that pregnancy is a normal state of health of the female body, the diagnosis and treatment tactics are still different, due to the many restrictions on manipulations and medications during pregnancy. That is why diagnosis and treatment during pregnancy should take place only under the supervision of a physician.