Sour stomach in pregnancy
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.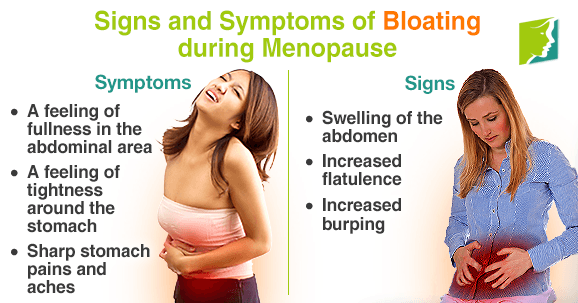
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms. However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Heartburn & Upset Stomach During Pregnancy
%PDF-1.4 % 1 0 obj /Producer(Adobe PDF Library 16.0.7)/Subject(Heartburn & Upset Stomach During Pregnancy)/Title(Heartburn & Upset Stomach During Pregnancy)/Trapped/False>> endobj 2 0 obj /MarkInfo>/Metadata 7 0 R/Names 8 0 R/Outlines 10 0 R/PageLayout/SinglePage/Pages 11 0 R/StructTreeRoot 109 0 R/Type/Catalog/ViewerPreferences>>> endobj 3 0 obj >/Font>>>/Fields[]>> endobj 4 0 obj > endobj 5 0 obj > endobj 6 0 obj > endobj 7 0 obj >stream application/pdf
 4 (Macintosh)uuid:2202572a-691e-4df2-a72a-2e0c700ba469xmp.did:69d55ac9-fcbc-4905-a26c-277147de1661xmp.id:875705b0-52cf-45d4-8986-47ccfc6c53b8proof:pdfxmp.iid:2c554508-fc72-4a15-b021-c94740d63a28xmp.did:049d1d1f-153f-452f-a99d-b4895a85a5dbxmp.did:69d55ac9-fcbc-4905-a26c-277147de1661default
4 (Macintosh)uuid:2202572a-691e-4df2-a72a-2e0c700ba469xmp.did:69d55ac9-fcbc-4905-a26c-277147de1661xmp.id:875705b0-52cf-45d4-8986-47ccfc6c53b8proof:pdfxmp.iid:2c554508-fc72-4a15-b021-c94740d63a28xmp.did:049d1d1f-153f-452f-a99d-b4895a85a5dbxmp.did:69d55ac9-fcbc-4905-a26c-277147de1661defaultArticle "Pregnancy and heartburn"
Hormonal changes that the body undergoes during pregnancy is the root cause of heartburn.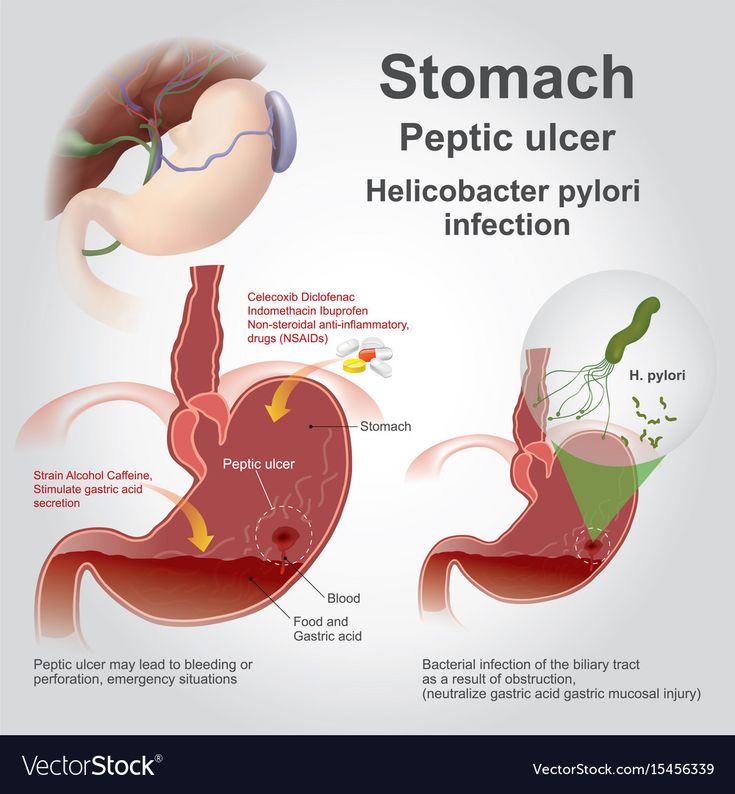 In early pregnancy, the ovaries, and then the placenta, produce the hormone progesterone, one of the main functions of which is to relax the smooth muscles of the body, including the muscles of the uterus. Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn. nine0003
In early pregnancy, the ovaries, and then the placenta, produce the hormone progesterone, one of the main functions of which is to relax the smooth muscles of the body, including the muscles of the uterus. Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn. nine0003
Another cause of heartburn in pregnant women is the weakening of motility - the wave-like movement of the gastrointestinal tract, slowing down the processes of digestion. Food passes through the digestive tract more slowly, lingering in the stomach. Heartburn in pregnant women is also provoked by the large size of the uterus, which increases intra-abdominal pressure and increases pressure on all the internal organs of the pregnant woman - the stomach and intestines as well. The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn. nine0003
Heartburn in pregnant women is also provoked by the large size of the uterus, which increases intra-abdominal pressure and increases pressure on all the internal organs of the pregnant woman - the stomach and intestines as well. The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn. nine0003
Heartburn can start at any stage of pregnancy, but is most common in the second and third trimesters. As a rule, discomfort occurs after 24 weeks, when the uterus rises above the navel, and becomes especially severe after 30 weeks. Especially intense heartburn can be in a woman if she had an increased acidity of gastric juice before pregnancy.
To avoid heartburn during pregnancy, first of all, you need to review your menu and exclude fatty, fried, spicy, salty foods from it, you must give up coffee and carbonated drinks.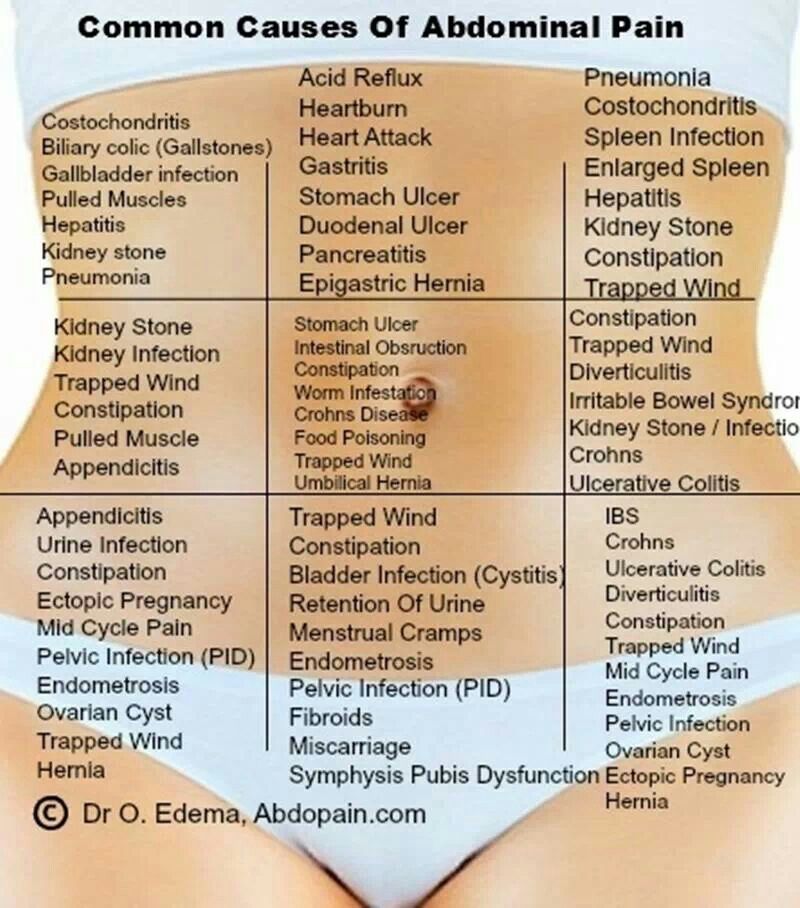 Include cereals, dairy products, lean meats and mashed vegetables in the diet. It is advisable to eat often and in small portions every 1.5-2 hours. Spend more time eating, remember to chew food thoroughly so that it is digested properly. Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it. nine0003
Include cereals, dairy products, lean meats and mashed vegetables in the diet. It is advisable to eat often and in small portions every 1.5-2 hours. Spend more time eating, remember to chew food thoroughly so that it is digested properly. Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it. nine0003
At the first signs of heartburn, you can drink a small amount of alkaline mineral water without gas or take a few sips of low-fat milk. Drink should be in small sips. Kissels work well. They envelop the esophagus and thus reduce burning sensation. The safest in the treatment of heartburn in pregnant women are antacids containing sodium bicarbonate, calcium carbonate, preparations containing magnesium and other substances.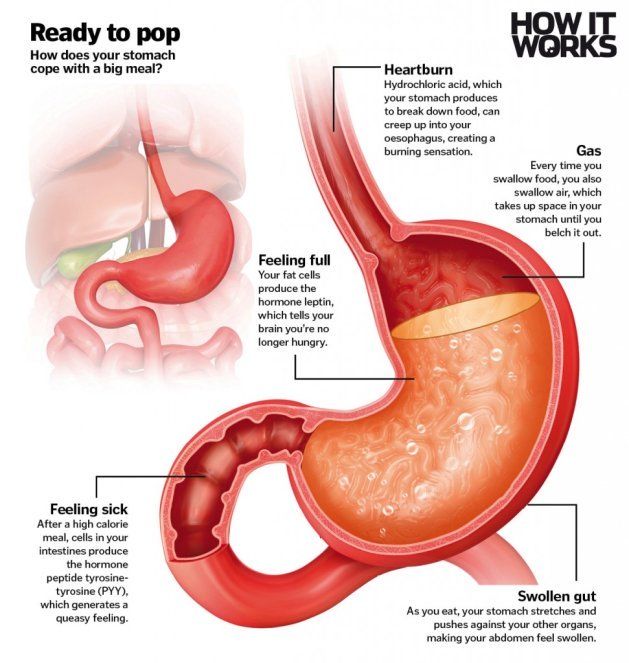 Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus. The effect of medicinal herbs on a pregnant woman and fetus, their effectiveness, and most importantly, safety have not been sufficiently studied, therefore it is better to avoid the use of herbal remedies for this purpose during pregnancy. Many herbs have a relaxing effect on the smooth muscles of the gastrointestinal tract and thus, on the contrary, can provoke heartburn attacks. Some women find unroasted hazelnuts or almonds helpful. You need to chew a few nucleoli to a mushy state, and then swallow. Reduces the acidity of the stomach and milk, which is a natural antacid. It is recommended to drink during the day in small portions. nine0003
Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus. The effect of medicinal herbs on a pregnant woman and fetus, their effectiveness, and most importantly, safety have not been sufficiently studied, therefore it is better to avoid the use of herbal remedies for this purpose during pregnancy. Many herbs have a relaxing effect on the smooth muscles of the gastrointestinal tract and thus, on the contrary, can provoke heartburn attacks. Some women find unroasted hazelnuts or almonds helpful. You need to chew a few nucleoli to a mushy state, and then swallow. Reduces the acidity of the stomach and milk, which is a natural antacid. It is recommended to drink during the day in small portions. nine0003
Despite all the discomfort during pregnancy heartburn, this condition does not affect the health of the fetus. But if heartburn during pregnancy is often a normal, physiological phenomenon, then outside of pregnancy, regular heartburn is a manifestation of the disease and a reason to see a doctor.
But if heartburn during pregnancy is often a normal, physiological phenomenon, then outside of pregnancy, regular heartburn is a manifestation of the disease and a reason to see a doctor.
At the EMC School of Moms, you can ask any questions about pregnancy and childbirth to our experienced specialists.
Pathology of the stomach during pregnancy | Online edition "Medicine and Pharmacy News"
During pregnancy, a woman's stomach is especially vulnerable. Often, pregnancy is accompanied by increased acid formation, although its decrease is not excluded. It is known that with increased acidity of the stomach, an increase in appetite is characteristic. However, loading the stomach with high acidity during pregnancy is not recommended. During pregnancy, the stomach produces more hydrochloric acid, not so much to increase appetite, but to increase the bactericidal content of its contents.
An unpleasant feeling of slight heat or burning in the stomach, sour eructation - all these symptoms are combined into one term "heartburn". During pregnancy, heartburn is caused by hormonal and physical changes in a woman's body. It is observed in approximately 50% of women during pregnancy at any time, but more often in the II and III trimesters, provoked by the use of abundant fatty, fried and spicy foods. Its occurrence is due to the reflux of acidic (much less often alkaline) gastric contents into the lower esophagus and its irritating effect. As you know, in pregnant women, the tone of the lower esophageal sphincter is significantly weakened, which is the result of the action of progesterone, and an increase in the uterus by the 25th week contributes to an increase in intra-abdominal pressure, which prevents the sphincter from completely closing. Progesterone also reduces contractions in the esophagus and intestines, slowing down digestion. The feeling of heartburn is accompanied by a feeling of melancholy, depressed mood. nine0003
During pregnancy, heartburn is caused by hormonal and physical changes in a woman's body. It is observed in approximately 50% of women during pregnancy at any time, but more often in the II and III trimesters, provoked by the use of abundant fatty, fried and spicy foods. Its occurrence is due to the reflux of acidic (much less often alkaline) gastric contents into the lower esophagus and its irritating effect. As you know, in pregnant women, the tone of the lower esophageal sphincter is significantly weakened, which is the result of the action of progesterone, and an increase in the uterus by the 25th week contributes to an increase in intra-abdominal pressure, which prevents the sphincter from completely closing. Progesterone also reduces contractions in the esophagus and intestines, slowing down digestion. The feeling of heartburn is accompanied by a feeling of melancholy, depressed mood. nine0003
Another symptom typical of gastric pathology is pain. The nature of pain in diseases of the stomach may indicate not only the disease, but also the presence of complications. Thus, the occurrence of burning pain in patients with gastritis, peptic ulcer disease may indicate the addition of a solarite. In pregnant women with chronic gastritis with a reduced secret function of the stomach, a feeling of heaviness, fullness in the epigastric region is usually noted. This feeling also appears with pyloric stenosis. In pregnant women with chronic gastritis with preserved secretion, the pain is often dull, aching in nature. The intensity of pain in diseases of the stomach can be different. In chronic gastritis, epigastric pain is usually of low intensity, and in gastric ulcer, and especially in duodenal ulcer, the pain is usually severe. With a perforated ulcer, the intensity of pain is so high that pain shock is possible. nine0003
Thus, the occurrence of burning pain in patients with gastritis, peptic ulcer disease may indicate the addition of a solarite. In pregnant women with chronic gastritis with a reduced secret function of the stomach, a feeling of heaviness, fullness in the epigastric region is usually noted. This feeling also appears with pyloric stenosis. In pregnant women with chronic gastritis with preserved secretion, the pain is often dull, aching in nature. The intensity of pain in diseases of the stomach can be different. In chronic gastritis, epigastric pain is usually of low intensity, and in gastric ulcer, and especially in duodenal ulcer, the pain is usually severe. With a perforated ulcer, the intensity of pain is so high that pain shock is possible. nine0003
According to some authors, chronic duodenitis occurs in pregnant women much more often than it is diagnosed, it is observed in the first trimester of pregnancy or 4-5 weeks before delivery and is characterized by a cyclical exacerbation (spring-autumn). Pain syndrome predominates in the clinical picture, night and hungry pains are characteristic, food intake reduces them. The goal of drug treatment for chronic duodenitis in pregnant women is to achieve remission of the disease. In the uncomplicated course of chronic gastritis or duodenitis, the condition of the patients is not significantly disturbed, and the disease does not have a noticeable effect on the course of pregnancy and its outcome. When vomiting of pregnant women occurs, the treatment of gastritis or duodenitis should be combined with the treatment of early toxicosis. nine0003
Pain syndrome predominates in the clinical picture, night and hungry pains are characteristic, food intake reduces them. The goal of drug treatment for chronic duodenitis in pregnant women is to achieve remission of the disease. In the uncomplicated course of chronic gastritis or duodenitis, the condition of the patients is not significantly disturbed, and the disease does not have a noticeable effect on the course of pregnancy and its outcome. When vomiting of pregnant women occurs, the treatment of gastritis or duodenitis should be combined with the treatment of early toxicosis. nine0003
The literature describes isolated information about the course of pregnancy against the background of Menetrier's disease. An analysis of the literature data does not allow us to draw conclusions about the etiology of the disease, although the role of cytomegalovirus is assumed. Along with complaints characteristic of chronic gastritis, lethargy appears in pregnant women, swelling of the lower extremities is possible. It is noted that in the second half of pregnancy the disease is severe, but it is not a contraindication for carrying a pregnancy. During pregnancy, the diagnosis is established on the basis of gastroscopy, in which the gastric mucosa is pale gray, edematous, easily vulnerable, eroded, with hemorrhages. The treatment is symptomatic, since, according to most researchers, gastrectomy is indicated outside of pregnancy. nine0003
It is noted that in the second half of pregnancy the disease is severe, but it is not a contraindication for carrying a pregnancy. During pregnancy, the diagnosis is established on the basis of gastroscopy, in which the gastric mucosa is pale gray, edematous, easily vulnerable, eroded, with hemorrhages. The treatment is symptomatic, since, according to most researchers, gastrectomy is indicated outside of pregnancy. nine0003
Peptic ulcer in pregnant women is quite common, but the exact incidence is difficult to estimate, since the diagnosis of peptic ulcer during pregnancy is difficult. The chance of encountering this disease in pregnant women has increased significantly, although in the vast majority of cases, pregnancy alleviates the clinical course of peptic ulcer. The reason for the favorable course of peptic ulcer in pregnant women is not fully understood. Some researchers believe that this is the result of an altered secretory (decrease in the production of hydrochloric acid and an increase in mucus formation) and motor functions of the stomach in the direction of its decrease, increased blood supply. It has been established that during pregnancy, in 40% of cases, remission of peptic ulcer of the stomach and duodenum occurs due to the high level of progesterone in the body, which stimulates the production of mucus, which is a protective mechanism of the gastric mucosa. Perhaps the overproduction of sex hormones, namely estrogens, is important. It has been established that estrogens perform a protective function, increase the intensity of regenerative processes, and improve blood supply to the gastroduodenal region. In most women, the disease does not affect the process of bearing and giving birth to a child. However, exacerbation of peptic ulcer during pregnancy, although unlikely, is still possible (in 10% of cases). Most pregnant women associate it with excessive excitement, fear of the upcoming birth and their outcome, probably because pregnancy itself is stressful for a woman. The main symptoms of peptic ulcer are: pain in the epigastric region (under the pit of the stomach), belching with air, food, nausea, sometimes vomiting, constipation, flatulence, weight loss.
It has been established that during pregnancy, in 40% of cases, remission of peptic ulcer of the stomach and duodenum occurs due to the high level of progesterone in the body, which stimulates the production of mucus, which is a protective mechanism of the gastric mucosa. Perhaps the overproduction of sex hormones, namely estrogens, is important. It has been established that estrogens perform a protective function, increase the intensity of regenerative processes, and improve blood supply to the gastroduodenal region. In most women, the disease does not affect the process of bearing and giving birth to a child. However, exacerbation of peptic ulcer during pregnancy, although unlikely, is still possible (in 10% of cases). Most pregnant women associate it with excessive excitement, fear of the upcoming birth and their outcome, probably because pregnancy itself is stressful for a woman. The main symptoms of peptic ulcer are: pain in the epigastric region (under the pit of the stomach), belching with air, food, nausea, sometimes vomiting, constipation, flatulence, weight loss. Peptic ulcer disease is dangerous for its complications, one of which is gastrointestinal bleeding, which dramatically increases the risk of fetal death. Massive bleeding during pregnancy is an indication for emergency surgery. nine0003
Peptic ulcer disease is dangerous for its complications, one of which is gastrointestinal bleeding, which dramatically increases the risk of fetal death. Massive bleeding during pregnancy is an indication for emergency surgery. nine0003
Stomach cancer is rare in pregnant women. The authors note that in case of stomach cancer in pregnant women, the first symptoms appear at the 15–16th week of pregnancy. There are pains in the epigastric region, lack of appetite, nausea, vomiting, melena is possible, but the symptoms are fuzzy and the clinical picture is blurred. The diagnosis is established on the basis of fibrogastroscopy with biopsy. Treatment is only surgical, since conservative treatment is not effective. According to most authors, the prognosis for the mother and fetus is unfavorable. nine0003
Resection of the stomach is one of the most common operations for its disease. It is known that pregnant women with a resected stomach are more likely to develop digestive system disorders, which is explained by the depletion of compensatory capabilities in this category of women. However, the question of the effect of pregnancy on the health of women with a resected stomach and on the course of pregnancy itself in this category of women has not yet been studied enough and is little covered in the literature.
However, the question of the effect of pregnancy on the health of women with a resected stomach and on the course of pregnancy itself in this category of women has not yet been studied enough and is little covered in the literature.
Pregnancy imposes significant restrictions on the choice of diagnostic methods and on the determination of treatment tactics. It is not recommended to conduct an X-ray examination of the stomach for pregnant women, therefore, the only diagnostic method for stomach pathology is esophagogastroduodenoscopy, although its implementation can be difficult. nine0003
Since there is no therapy aimed at destroying Helicobacter pylori during pregnancy, the diagnosis of this infection is performed after childbirth (if necessary, a breath test is performed). Recommended for use during exacerbations of peptic ulcer in pregnant women are antacids. Antacids containing aluminum, calcium, or magnesium are considered safe and effective in treating heartburn during pregnancy. However, magnesium-containing antacids should be avoided during the third trimester of pregnancy because they can induce preterm labor. In addition, antacids containing sodium bicarbonate should be avoided to avoid metabolic alkalosis. In addition, it is possible to prescribe enveloping and astringent agents of plant origin - decoctions of chamomile, St. John's wort. nine0003
However, magnesium-containing antacids should be avoided during the third trimester of pregnancy because they can induce preterm labor. In addition, antacids containing sodium bicarbonate should be avoided to avoid metabolic alkalosis. In addition, it is possible to prescribe enveloping and astringent agents of plant origin - decoctions of chamomile, St. John's wort. nine0003
H2-blockers of histamine receptors are also undesirable for taking by pregnant women. However, ranitidine has been found to be the only histamine h3 receptor antagonist that has been well studied during pregnancy. In a double-blind, placebo-controlled study by J.D. Larson et al. (1997) proved that ranitidine, taken several times a day by pregnant patients with heartburn (when antacids were ineffective), reduced its severity. No adverse effects on the fetus have been reported. A safety study on ranitidine by J.E. Richter (2003), showed that pregnant women taking it from the first trimester throughout pregnancy gave birth to healthy children. Taking proton pump inhibitors in acid-dependent conditions by pregnant women is undesirable and is possible only if antacids are ineffective. More recently (May 2010), new evidence has emerged of an increased risk of hip, wrist and spine fractures with long-term use or high doses of proton pump inhibitors, as well as an increased risk of having a child with heart defects by more than two times. Only when the threat to the health of the mother outweighs the potential risk to the fetus, short-term courses of proton pump inhibitors may be prescribed. Recently, evidence has emerged that lansoprazole and pantoprazole are priority representatives of drugs in this class, since their relative safety in pregnant women has been studied. Due to the fact that the range of drugs in the presence of acid-dependent conditions of the stomach during pregnancy is limited, an important role is given to dietary measures. In addition, it is recommended to limit physical activity, half-bed rest, fractional nutrition, strict adherence to diet No.
Taking proton pump inhibitors in acid-dependent conditions by pregnant women is undesirable and is possible only if antacids are ineffective. More recently (May 2010), new evidence has emerged of an increased risk of hip, wrist and spine fractures with long-term use or high doses of proton pump inhibitors, as well as an increased risk of having a child with heart defects by more than two times. Only when the threat to the health of the mother outweighs the potential risk to the fetus, short-term courses of proton pump inhibitors may be prescribed. Recently, evidence has emerged that lansoprazole and pantoprazole are priority representatives of drugs in this class, since their relative safety in pregnant women has been studied. Due to the fact that the range of drugs in the presence of acid-dependent conditions of the stomach during pregnancy is limited, an important role is given to dietary measures. In addition, it is recommended to limit physical activity, half-bed rest, fractional nutrition, strict adherence to diet No.