Sleeping position during second trimester
Sleeping While Pregnant: Second Trimester
1.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia. (2019, June 30). Morning sickness. Retrieved August 24, 2020, from https://medlineplus.gov/ency/article/003119.htm
2.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia. (2018, October 30). Breast pain. Retrieved August 24, 2020, from https://medlineplus.gov/ency/article/003152.htm
3.
Reid, K. J., Facco, F. L., Grobman, W. A., Parker, C. B., Herbas, M., Hunter, S., Silver, R. M., Basner, R. C., Saade, G. R., Pien, G. W., Manchanda, S., Louis, J. M., Nhan-Chang, C. L., Chung, J. H., Wing, D. A., Simhan, H. N., Haas, D. M., Iams, J., Parry, S., & Zee, P. C. (2017). Sleep During Pregnancy: The nuMoM2b Pregnancy and Sleep Duration and Continuity Study. Sleep, 40(5), zsx045. https://doi.org/10.1093/sleep/zsx045
4.
Supakatisant, C., & Phupong, V. (2015). Oral magnesium for relief in pregnancy-induced leg cramps: a randomised controlled trial. Maternal & child nutrition, 11(2), 139–145. https://doi.org/10.1111/j.1740-8709.2012.00440.x
5.
Cherni, Y., Desseauve, D., Decatoire, A., Veit-Rubinc, N., Begon, M., Pierre, F., & Fradet, L. (2019). Evaluation of ligament laxity during pregnancy. Journal of gynecology obstetrics and human reproduction, 48(5), 351–357. https://doi.org/10.1016/j.jogoh.2019.02.009
6.
Casagrande, D., Gugala, Z., Clark, S. M., & Lindsey, R. W. (2015). Low Back Pain and Pelvic Girdle Pain in Pregnancy. The Journal of the American Academy of Orthopaedic Surgeons, 23(9), 539–549. https://doi.org/10.5435/JAAOS-D-14-00248
7.
Martin-Fairey, C. A., Zhao, P., Wan, L., Roenneberg, T., Fay, J., Ma, X., McCarthy, R., Jungheim, E. S., England, S. K., & Herzog, E. D. (2019). Pregnancy Induces an Earlier Chronotype in Both Mice and Women. Journal of biological rhythms, 34(3), 323–331. https://doi.org/10.1177/0748730419844650
8.
Sandoe, C. H., & Lay, C. (2019). Secondary Headaches During Pregnancy: When to Worry. Current neurology and neuroscience reports, 19(6), 27. https://doi.org/10.1007/s11910-019-0944-9
9.
Gilbey, P., McGruthers, L., Morency, A. M., & Shrim, A. (2012). Rhinosinusitis-related quality of life during pregnancy. American journal of rhinology & allergy, 26(4), 283–286. https://doi.org/10.2500/ajra.2012.26.3776
10.
Ferdinande, K., Dorreman, Y., Roelens, K., Ceelen, W., & De Looze, D. (2018). Anorectal symptoms during pregnancy and postpartum: a prospective cohort study. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland, 20(12), 1109–1116. https://doi.org/10.1111/codi.14324
11.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia. (2018, September 25). Common symptoms during pregnancy. Retrieved August 24, 2020, from https://medlineplus.gov/ency/patientinstructions/000583.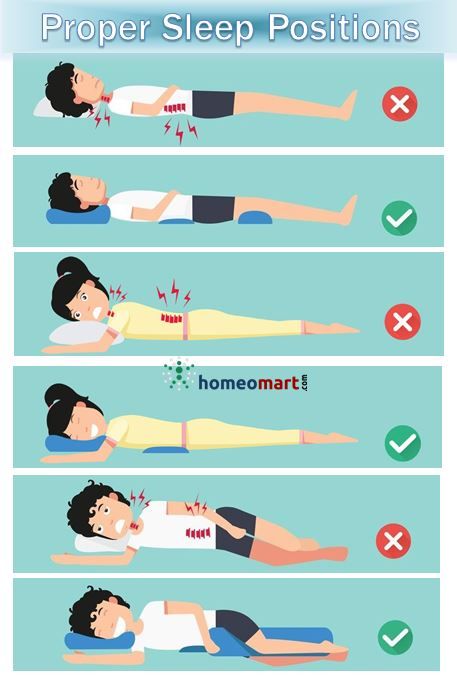 htm
htm
12.
The American College of Obstetricians and Gynecologists. (2018, April). How Your Fetus Grows During Pregnancy. Retrieved August 24, 2020, from https://www.acog.org/patient-resources/faqs/pregnancy/how-your-fetus-grows-during-pregnancy
13.
Rawal, S., Hinkle, S. N., Zhu, Y., Albert, P. S., & Zhang, C. (2017). A longitudinal study of sleep duration in pregnancy and subsequent risk of gestational diabetes: findings from a prospective, multiracial cohort. American journal of obstetrics and gynecology, 216(4), 399.e1–399.e8. https://doi.org/10.1016/j.ajog.2016.11.1051
14.
Gao, M., Hu, J., Yang, L., Ding, N., Wei, X., Li, L., Liu, L., Ma, Y., & Wen, D. (2019). Association of sleep quality during pregnancy with stress and depression: a prospective birth cohort study in China. BMC pregnancy and childbirth, 19(1), 444. https://doi.org/10.1186/s12884-019-2583-1
15.
Okun, M. L., Kline, C.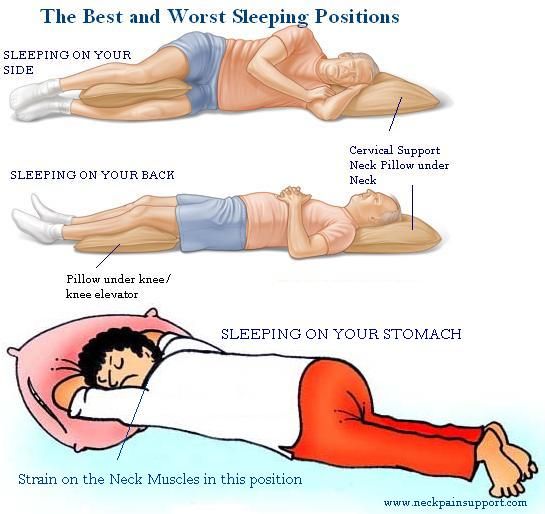 E., Roberts, J. M., Wettlaufer, B., Glover, K., & Hall, M. (2013). Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. Journal of women's health (2002), 22(12), 1028–1037. https://doi.org/10.1089/jwh.2013.4331
E., Roberts, J. M., Wettlaufer, B., Glover, K., & Hall, M. (2013). Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. Journal of women's health (2002), 22(12), 1028–1037. https://doi.org/10.1089/jwh.2013.4331
16.
Tsai, S. Y., Lee, P. L., Lin, J. W., & Lee, C. N. (2016). Cross-sectional and longitudinal associations between sleep and health-related quality of life in pregnant women: A prospective observational study. International journal of nursing studies, 56, 45–53. https://doi.org/10.1016/j.ijnurstu.2016.01.001
17.
Na-Rungsri, K., Lertmaharit, S., Lohsoonthorn, V., Totienchai, S., & Jaimchariyatam, N. (2016). Obstructive sleep apnea and the risk of preterm delivery. Sleep & breathing = Schlaf & Atmung, 20(3), 1111–1117. https://doi.org/10.1007/s11325-016-1339-7
18.
Jaimchariyatam, N., Na-Rungsri, K., Tungsanga, S., Lertmaharit, S., Lohsoonthorn, V. , & Totienchai, S. (2019). Obstructive sleep apnea as a risk factor for preeclampsia-eclampsia. Sleep & breathing = Schlaf & Atmung, 23(2), 687–693. https://doi.org/10.1007/s11325-018-1758-8
, & Totienchai, S. (2019). Obstructive sleep apnea as a risk factor for preeclampsia-eclampsia. Sleep & breathing = Schlaf & Atmung, 23(2), 687–693. https://doi.org/10.1007/s11325-018-1758-8
19.
Reutrakul, S., Zaidi, N., Wroblewski, K., Kay, H. H., Ismail, M., Ehrmann, D. A., & Van Cauter, E. (2013). Interactions between pregnancy, obstructive sleep apnea, and gestational diabetes mellitus. The Journal of clinical endocrinology and metabolism, 98(10), 4195–4202. https://doi.org/10.1210/jc.2013-2348
20.
Rossi, A., Cornette, J., Johnson, M. R., Karamermer, Y., Springeling, T., Opic, P., Moelker, A., Krestin, G. P., Steegers, E., Roos-Hesselink, J., & van Geuns, R. J. (2011). Quantitative cardiovascular magnetic resonance in pregnant women: cross-sectional analysis of physiological parameters throughout pregnancy and the impact of the supine position. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance, 13(1), 31. https://doi.org/10.1186/1532-429X-13-31
https://doi.org/10.1186/1532-429X-13-31
21.
Silver, R. M., Hunter, S., Reddy, U. M., Facco, F., Gibbins, K. J., Grobman, W. A., Mercer, B. M., Haas, D. M., Simhan, H. N., Parry, S., Wapner, R. J., Louis, J., Chung, J. M., Pien, G., Schubert, F. P., Saade, G. R., Zee, P., Redline, S., Parker, C. B., & Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (NuMoM2b) Study (2019). Prospective Evaluation of Maternal Sleep Position Through 30 Weeks of Gestation and Adverse Pregnancy Outcomes. Obstetrics and gynecology, 134(4), 667–676. https://doi.org/10.1097/AOG.0000000000003458
22.
Effati-Daryani, F., Mohammad-Alizadeh-Charandabi, S., Mirghafourvand, M., Taghizadeh, M., Bekhradi, R., & Zarei, S. (2018). Effect of Lavender cream with or without footbath on sleep quality and fatigue in pregnancy and postpartum: a randomized controlled trial. Women & health, 58(10), 1179–1191. https://doi.org/10.1080/03630242.2017.1414101
23.
OʼConnor, P. J., Poudevigne, M. S., Johnson, K. E., Brito de Araujo, J., & Ward-Ritacco, C. L. (2018). Effects of Resistance Training on Fatigue-Related Domains of Quality of Life and Mood During Pregnancy: A Randomized Trial in Pregnant Women With Increased Risk of Back Pain. Psychosomatic medicine, 80(3), 327–332. https://doi.org/10.1097/PSY.0000000000000559
24.
Gjestland, K., Bø, K., Owe, K. M., & Eberhard-Gran, M. (2013). Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. British journal of sports medicine, 47(8), 515–520. https://doi.org/10.1136/bjsports-2012-091344
25.
Watelain, E., Pinti, A., Doya, R., Garnier, C., Toumi, H., & Boudet, S. (2017). Benefits of physical activities centered on the trunk for pregnant women. The Physician and sportsmedicine, 45(3), 293–302. https://doi.org/10.1080/00913847.2017.1351286
26.
Crowley, S. K., O'Buckley, T. K., Schiller, C. E., Stuebe, A., Morrow, A. L., & Girdler, S. S. (2016). Blunted neuroactive steroid and HPA axis responses to stress are associated with reduced sleep quality and negative affect in pregnancy: a pilot study. Psychopharmacology, 233(7), 1299–1310. https://doi.org/10.1007/s00213-016-4217-x
27.
Latendresse, G., & Ruiz, R. J. (2010). Maternal coping style and perceived adequacy of income predict CRH levels at 14-20 weeks of gestation. Biological research for nursing, 12(2), 125–136. https://doi.org/10.1177/1099800410377111
28.
Solomonova, E., Lee, Y., Robins, S., King, L., Feeley, N., Gold, I., Hayton, B., Libman, E., Nagy, C., Turecki, G., & Zelkowitz, P. (2019). Sleep quality is associated with vasopressin methylation in pregnant and postpartum women with a history of psychosocial stress. Psychoneuroendocrinology, 107, 160–168. https://doi.org/10.1016/j.psyneuen.2019.05.010
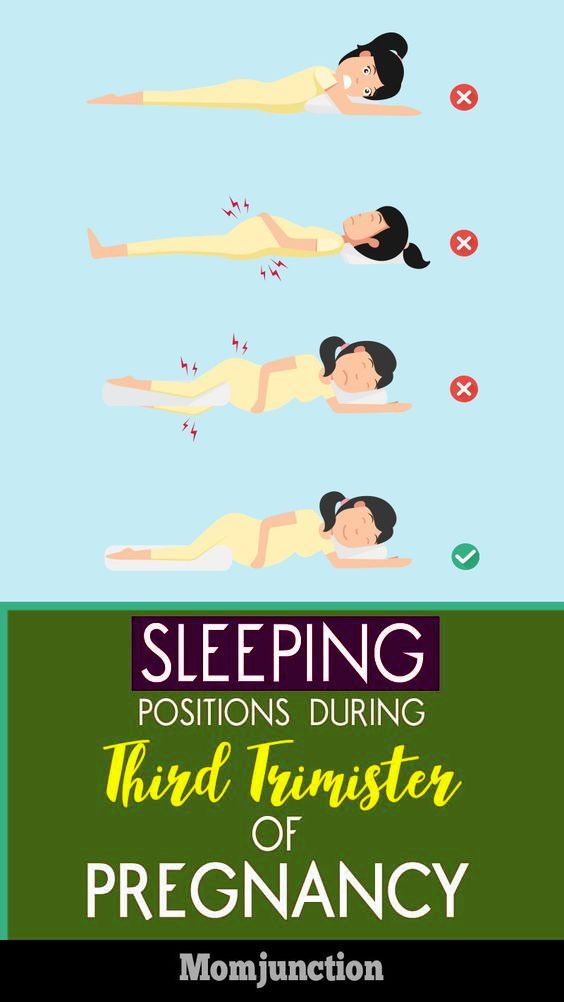
Best Sleeping Positions While Pregnant
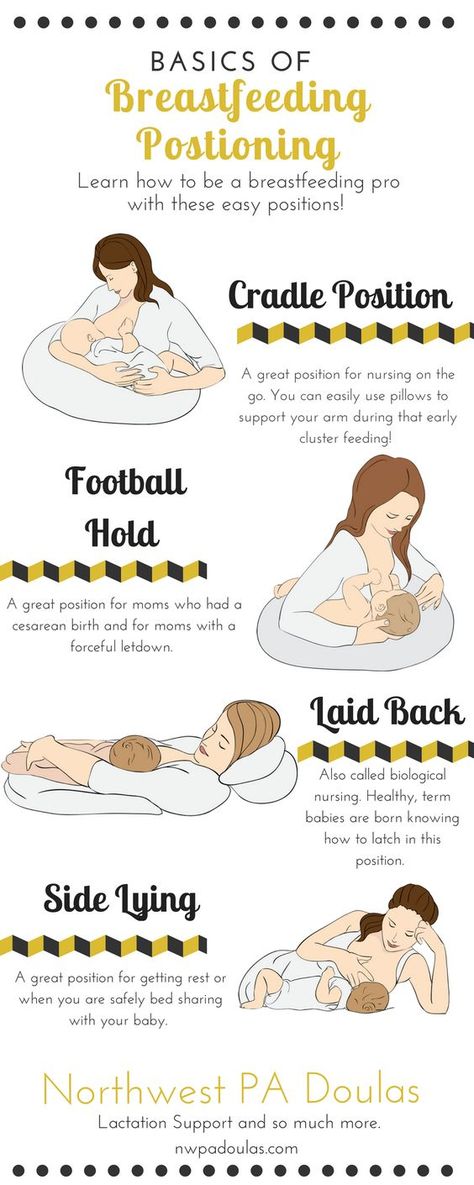
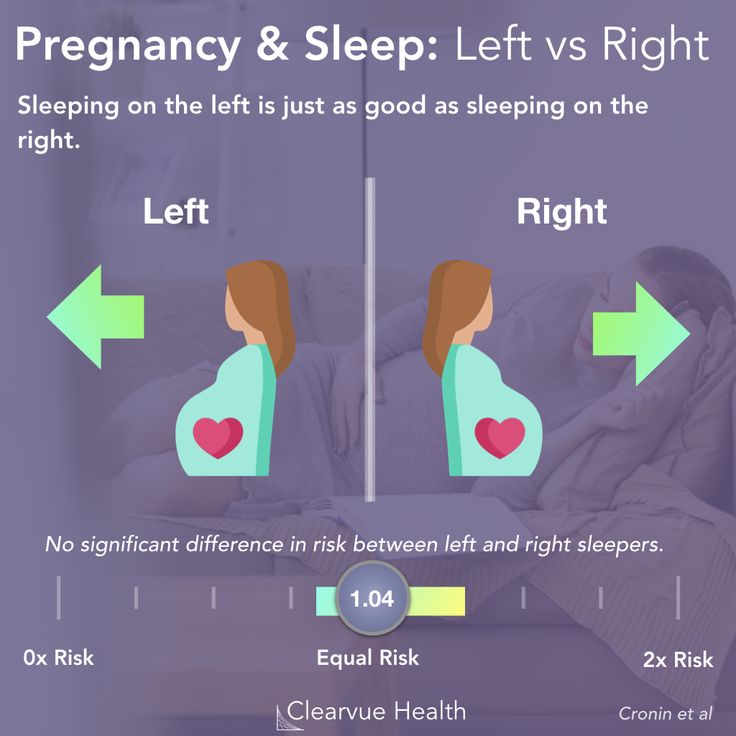
The best sleep position during pregnancy is “SOS” (sleep on side) because it provides the best circulation for you and your baby.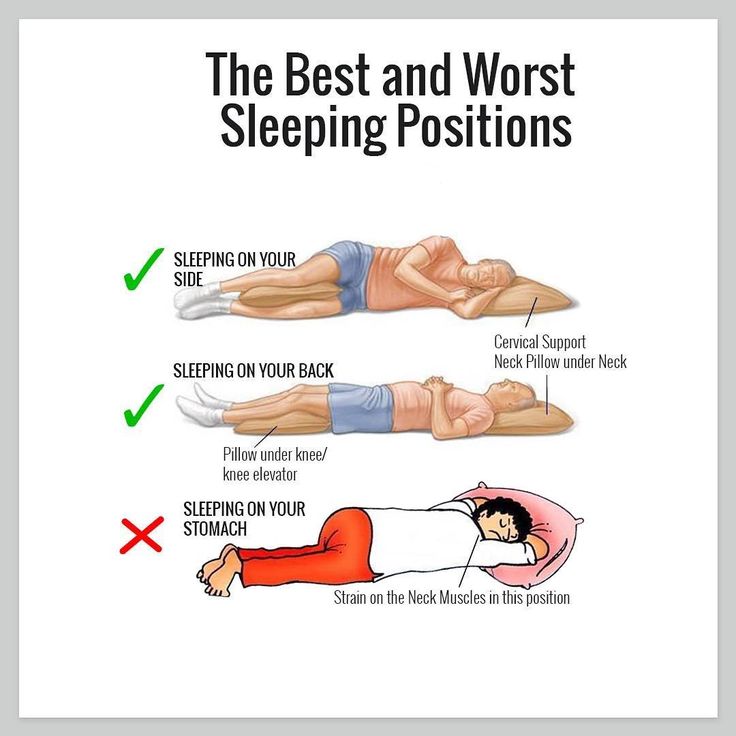 It also places the least pressure on your veins and internal organs. Sleeping on your left side will increase the amount of blood and nutrients that reach the placenta and your baby. Plus good circulation helps reduce potential swelling, varicose veins in your legs and hemorrhoids.
It also places the least pressure on your veins and internal organs. Sleeping on your left side will increase the amount of blood and nutrients that reach the placenta and your baby. Plus good circulation helps reduce potential swelling, varicose veins in your legs and hemorrhoids.
How Can I Sleep More Comfortably During Pregnancy?
Keep your legs and knees bent, and put a pillow between your legs to relieve the stress on your back.
- If you find that you are having problems with back pain, use the “SOS” position, and try placing a pillow under your abdomen as well.
- If you are experiencing heartburn during the night, you may want to try propping your upper body with pillows.
- In late pregnancy, you may experience shortness of breath. Try lying on your side or propped up with pillows.
These suggestions may not sound completely comfortable, especially if you are used to sleeping on your back or stomach, but try them out. You may find that they work. Keep in mind that you may not stay in one position all night, and rotating positions is fine.
Keep in mind that you may not stay in one position all night, and rotating positions is fine.
What Sleep Positions During Pregnancy Should I Avoid?
Sleeping on your back: This can cause problems with backaches, breathing, the digestive system, hemorrhoids, low blood pressure and cause a decrease in circulation to your heart and your baby. This is a result of your growing abdomen resting on your intestines and major blood vessels (the aorta and vena cava). You can also develop sleep apnea as you put on weight.
Sleeping on your stomach: When you are farther along in your pregnancy, your breasts become more tender and your abdomen continues to grow, both making sleeping on your tummy uncomfortable. Using a donut-shaped pillow (with a hole in the middle) may help you sleep comfortably on your stomach.
Reasons for your discomfort may include:
During pregnancy, you may find yourself wrestling in bed trying to get comfortable before falling asleep.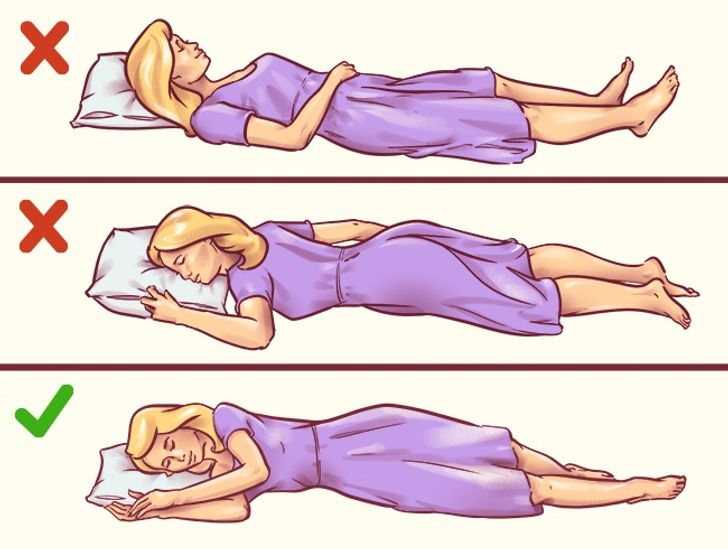 When you are pregnant your body goes through a variety of changes causing your regular sleeping positions to no longer work for you.
When you are pregnant your body goes through a variety of changes causing your regular sleeping positions to no longer work for you.
- Increased size of the abdomen
- Back pain
- Heartburn
- Shortness of breath
- Insomnia
More Steps to Sleeping Better While Pregnant
- Limit caffeine. Try not to drink coffee or caffeinated tea after 3 p.m.
- Brink plenty of water. Drink lot of water through out the day, but limit intake a couple of hours before bedtime so you don’t have to wake up and go to the bathroom.
- Exercise for 30 minutes. Exercise helps you sleep better, but don’t exercise within four hours of bedtime.
- Relaxing activities. A warm bath, foot or shoulder massage will help you relax.
- Peaceful bedroom. Keeping your bedroom dark, quiet and cool at night will help to drift off to sleep and stay asleep.
- 7 Discomforts of Pregnancy
- Nighfood Nighttime Ice Cream
- Pregnancy Week 15
Compiled using information from the following sources:
1. Nemours Foundation
Nemours Foundation
https://www.kidshealth.org
1. Your Pregnancy Week by Week Fifth Ed. Curtis, Glade B., OB/GYN, et al. Week 16
Comfortable sleeping positions during pregnancy
Pregnant women often have difficulty falling asleep. Firstly, because of the state of health, which is far from always normal. Secondly, because of the restlessness of the child, who is increasingly making itself felt. And thirdly, the stomach grows and it becomes more and more difficult to find a comfortable position for sleeping. There are special pillows for pregnant women, which are designed to help women in this situation. Do they really help? Maybe ordinary pillows are also suitable? Let's figure it out.
For those who like to sleep on their stomach, the difficulties will begin already in the first trimester. At this time, the chest begins to increase significantly in size and makes it difficult to sleep in the usual position. In the second trimester, it's time to get used to sleeping on your side, otherwise an enlarged and heavier belly can negatively affect blood circulation. The ideal position is to sleep on your left side. But in the third trimester, a woman will still have a hard time, even if she always sleeps on her left side, because the considerable weight of the abdomen, combined with the weakness of the joints - because the body is preparing for the process of childbirth - is likely to provoke great inconvenience and pain.
The ideal position is to sleep on your left side. But in the third trimester, a woman will still have a hard time, even if she always sleeps on her left side, because the considerable weight of the abdomen, combined with the weakness of the joints - because the body is preparing for the process of childbirth - is likely to provoke great inconvenience and pain.
It is during this period that many people think about a special pillow for pregnant women and the question of choice arises. But how do you know which of them can really provide convenience for you?
How to choose the right maternity pillow before buying it online
To start with, we recommend experimenting with regular pillows you have at home. Place them under your head and neck, as well as between your knees, lying on your left side. You can also adjust the pillow under the stomach to support the weight and ease the load on the spine. If you find it difficult to get used to sleeping on your left side, put a pillow under your back as well, it will serve as a barrier if you want to roll over in a dream. It is possible that the pillows available at home will do the job perfectly, and you do not have to buy a special one.
It is possible that the pillows available at home will do the job perfectly, and you do not have to buy a special one.
If regular pillows aren't comfortable, you'll be surprised at the variety of maternity bedding options. Some women like large square pillows that can be placed between the legs and support the stomach. Others prefer small wedge-shaped ones that are placed just under the stomach and thus flatten the entire body. And there are huge pillows-rollers in the form of a semicircle that cover the entire body. They simultaneously serve as a support for the back and abdomen, are conveniently located between the knees and support the head. They look the most comfortable of all, but still take your time with the purchase.
Things to consider before choosing a pregnancy pillow
Your own body will help you make the right choice. Think about how you usually sleep and what, in fact, you have difficulty. For example, if you usually lie on your back, then the same cushion-roller that supports both your back and stomach will suit you. But if you do not like the abundance of blankets and pillows on the bed, such a huge pillow will annoy you. Pay attention to smaller items. The advice of friends who have passed this period will be very useful. Perhaps one of them has used one or another pregnancy pillow, and you can try it out before buying.
But if you do not like the abundance of blankets and pillows on the bed, such a huge pillow will annoy you. Pay attention to smaller items. The advice of friends who have passed this period will be very useful. Perhaps one of them has used one or another pregnancy pillow, and you can try it out before buying.
Now let's talk about sleeping positions. For a pregnant woman, this is a very relevant issue, because her task is not only to get enough sleep herself, but also not to harm the child. First of all, avoid sleeping on your back from the beginning of your pregnancy. In the first trimester, it is safe, but it is better to start weaning this habit now, because in the future, the increasing weight of the abdomen will put pressure on the blood vessels and interfere with blood circulation, you will wake up with dizziness. In addition, circulatory problems prevent the supply of nutrients to the fetus.
What are the best sleeping positions for pregnant women
Sleeping on your stomach is fine at first, but after about the fifth month it becomes terribly uncomfortable due to the volume of the stomach and breasts.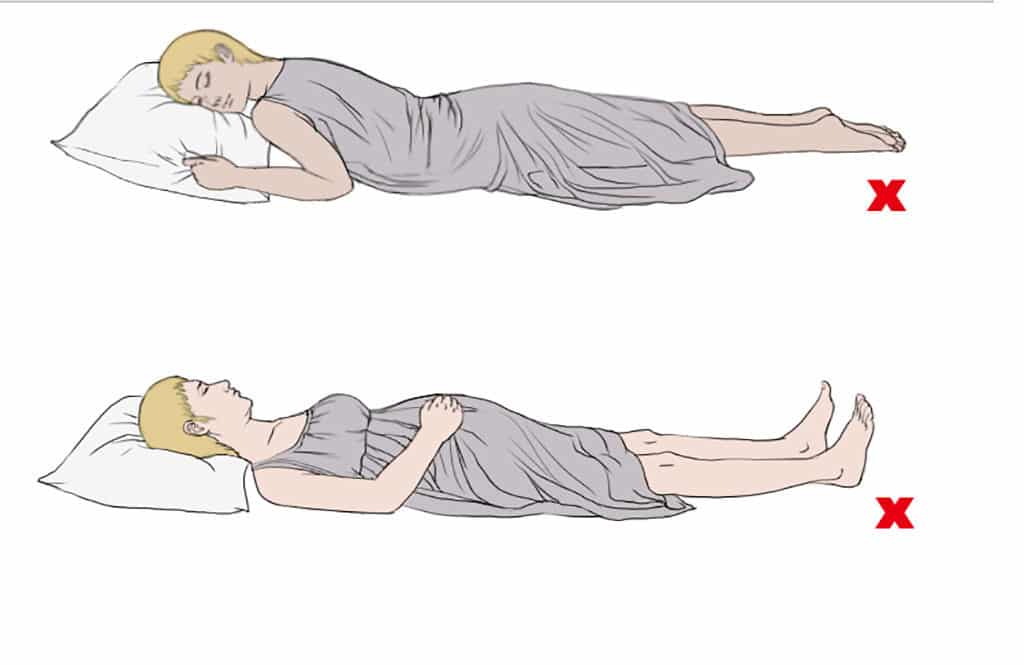 It's like trying to sleep while lying on a giant watermelon. Nevertheless, this position is safe for the baby, because even in the last month of pregnancy, the walls of the uterus reliably protect the baby. So this pose passes the control for medical reasons, but from the point of view of convenience - definitely not.
It's like trying to sleep while lying on a giant watermelon. Nevertheless, this position is safe for the baby, because even in the last month of pregnancy, the walls of the uterus reliably protect the baby. So this pose passes the control for medical reasons, but from the point of view of convenience - definitely not.
As mentioned above, the best sleeping position is on the left side. So the blood gets to the fetus as quickly as possible, and its weight does not put pressure on your liver. Use a pregnancy pillow that suits you, the variety of which you already know, so that you can lie comfortably. Also, sleeping on your left side improves the process of removing fluid from your body, and this reduces swelling in the legs and arms.
PLEASE SHARE THIS POST!
How to sleep during pregnancy
It is difficult to overestimate the role of sleep in the life of every person. A complete healthy rest allows you to fully restore the functioning of the nervous system, relieve stress, improve performance and increase activity. Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
The cause of insomnia can be :
- Anxiety;
- Frequent urination;
- Fears and phobias before a new stage of one's life;
- Nervousness and irritability;
- Digestive disorder;
- Toxicosis;
- Physical indisposition;
- Uncomfortable posture.
During the period of bearing a child, the female body experiences an extraordinary load, especially in the last trimester. The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
Let's try to figure out how to sleep during pregnancy, so as not only not to harm the health of your unborn baby, but to sleep well.
Looking for a comfortable sleeping position
Each person has his own favorite position, in which it is easy to fall asleep and sleep. Many do not imagine a comfortable rest on their backs, accustomed to sleeping on their stomachs. This habit will have to be sacrificed, as it is unsafe for the normal development of the fetus. If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position.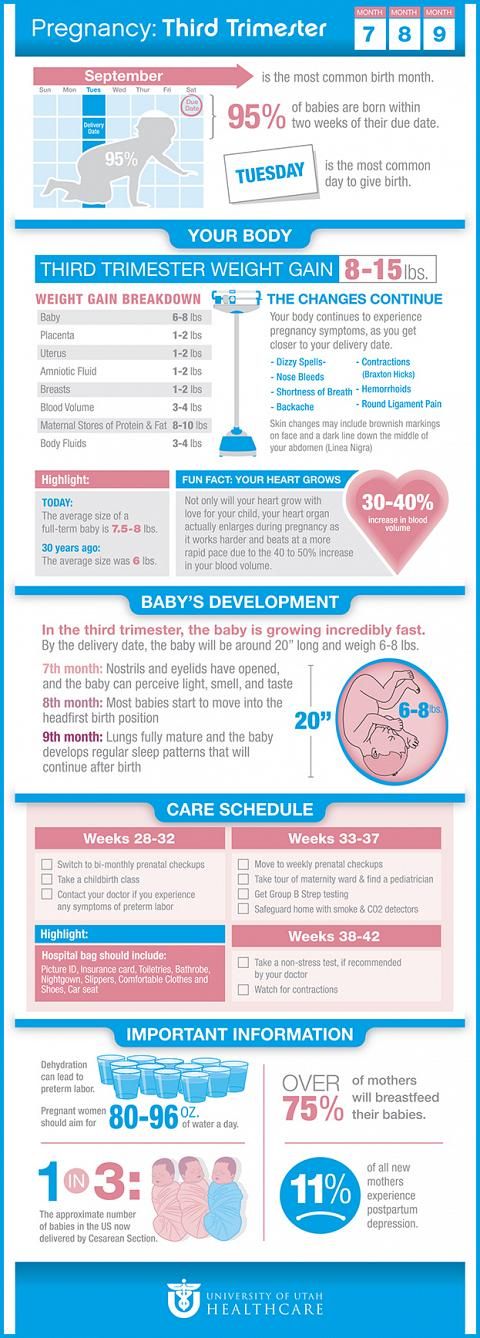 Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Back position
Even if you are used to sleeping in a Spartan position, on your back, with your arms spread wide, from the 28th week you will have to radically change your lifestyle. The fact is that as the fetus grows, the load on the intestines and vena cava will increase significantly, blocking the access of oxygen to the baby.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
If you sleep on your back during pregnancy, you may experience the following problems:
- Dizziness;
- Nausea;
- Convulsions;
- Numb limbs;
- Pressure reduction;
- Hemorrhoids;
- Heaviness of breathing.

If you feel these symptoms or the baby gives persistent signals, you need to urgently change your position, so squeezing the vena cava is fraught not only with poor health for the mother, but also with a lack of oxygen supply to the fetus.
Stomach position
One of the most beloved positions for many people, which allows you to quickly fall asleep while hugging a pillow. Many women, as soon as they find out about the change in their lives, are interested in the question, is it possible to sleep on your stomach during pregnancy? Doctors recommend abandoning this position already in the first weeks, even before the enlarged belly makes it impossible to fall asleep peacefully.
If you are afraid during sleep, without controlling your movements, to arbitrarily roll over on your stomach, you can put a large pillow that does not allow you to change position.
Side position
In order to normalize your sleep and not harm the health of the baby, experts recommend sleeping on your side during pregnancy.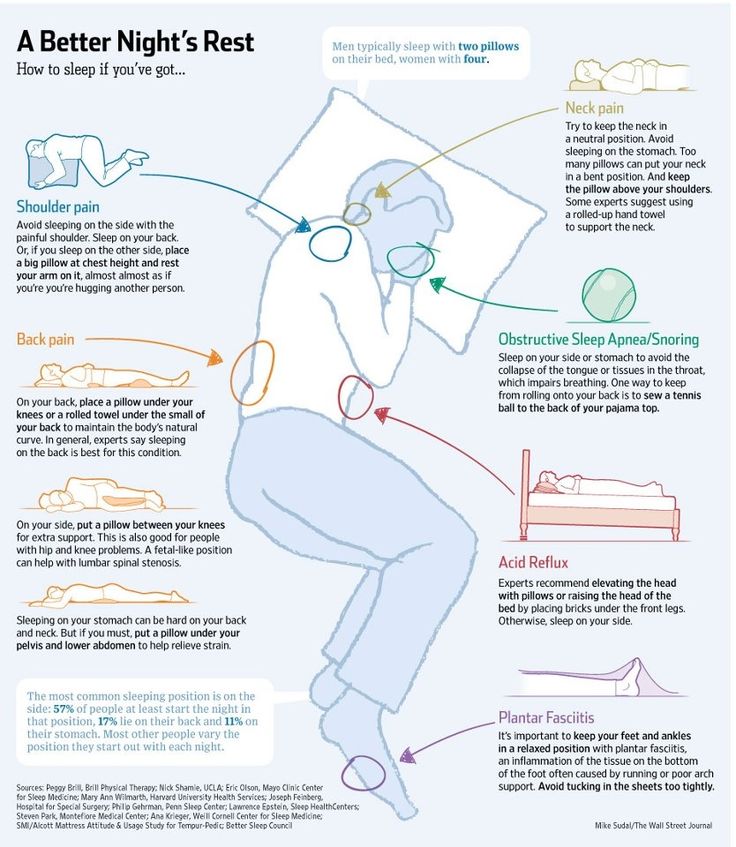 And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
Sleeping on the right side can cause squeezing of the kidney, which can have dire consequences. The ideal posture is lying on the left side. Thus, you not only do not injure the unborn baby, but also improve blood flow along with oxygen to the placenta.
But one should not ignore the individual characteristics of each organism and the position of the fetus in the uterus. When the baby is in a transverse position, choose the side where the baby's head is. And with a breech presentation, doctors recommend changing the position several times a night.
If you still cannot improve your sleep, you feel unwell and you are tormented by insomnia, then it is better to consult a specialist. A good gynecologist will analyze the situation and help solve the problem.