Skin rashes in infants face
Skin rashes in babies | nidirect
It's normal for babies to develop rashes from as early as a few days old. If your baby has a rash but doesn’t show signs of illness, speak to your midwife, health visitor, or your GP. If your baby appears unwell, call your GP or GP out of hours service.
About skin rashes in babies
It's important to be aware of the symptoms of meningitis, see section below.
Also below is information on some of the most common rashes in babies. Most rashes are harmless and go away on their own.
This guide may give you a better idea of the cause of the rash. But don't use it to diagnose your baby's condition. Always speak to a health professional for a proper diagnosis.
- read about causes of rashes in older children
Baby acne (neonatal acne)
Baby acne is where pimples sometimes develop on a baby's cheeks, nose and forehead within a month of their birth.
About baby acne
- pimples tend to get worse before clearing up completely after a few weeks or months
- washing your baby's face with water and a mild moisturiser can improve the appearance of their skin
- avoid acne medicines intended for older children and adults
Pimples or blackheads that develop after three months of age (infantile acne) tend to be more severe. These often need medical treatment.
Cradle cap
Cradle cap is where yellowish, greasy, scaly patches develop on a baby's scalp.
About cradle cap
- occasionally, as well as the scalp, the face, ears and neck are also affected
- it isn't itchy and shouldn't bother your baby- if your baby is scratching or upset, they may have eczema (see below)
- it is a common condition that tends to develop within two or three months after birth
- it usually gets better without treatment in a few weeks or months
Gently washing your baby's hair and scalp with baby shampoo may help to prevent further patches developing.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked.
The most common form is atopic eczema. It mainly affects babies and children but can continue into adulthood.
About atopic eczema
- eczema in babies under six months is sometimes associated with allergies to milk and egg
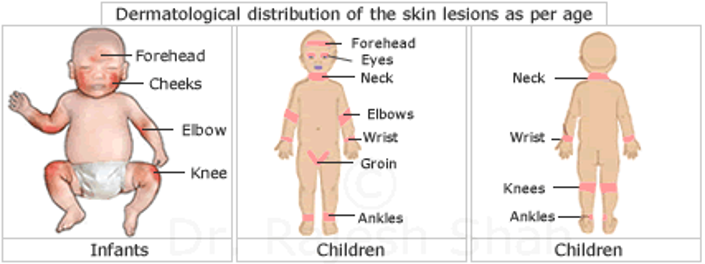
- it often starts in young babies as a red, itchy rash on the face, scalp and body
- as the child gets older, it usually starts to develop in areas with folds of skin, such as behind the knees or on the front of the elbows
Creams and ointments can often relieve the symptoms.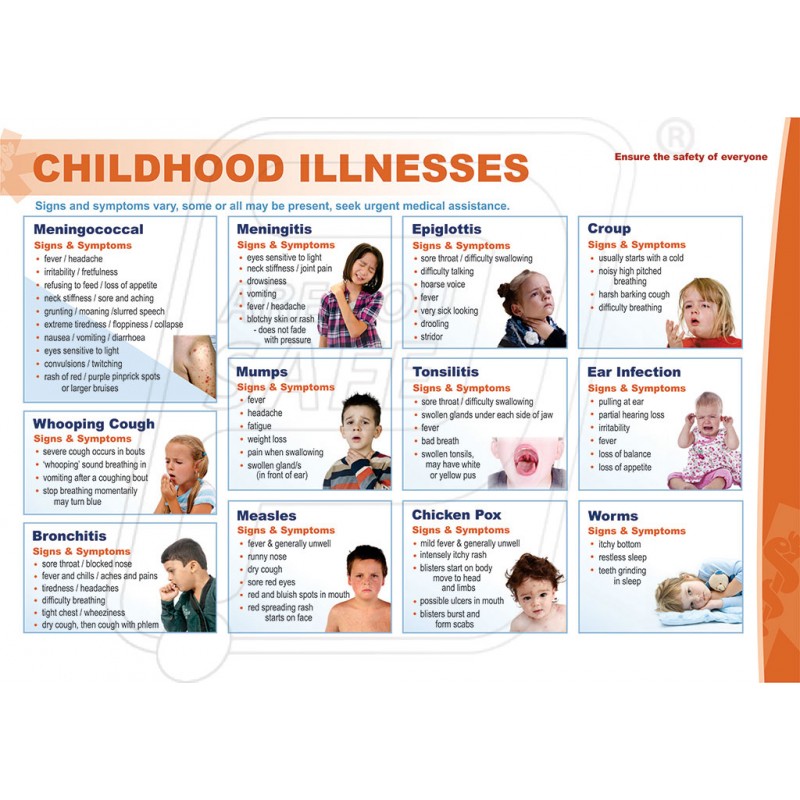
Erythema toxicum
Half of all newborns develop a blotchy red skin reaction called erythema toxicum. This is usually at two or three days old.
It's a normal newborn rash that won't bother your baby and clears after a few days.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, viral illness.
About hand, foot and mouth disease
- it causes a blistery rash on the palms of the hands and soles of the feet, as well as ulcers in the mouth
- your baby may also feel unwell and have a fever
Treatment isn't usually needed, as the baby's immune system clears the virus. The symptoms go away after about seven to 10 days. If you're worried, see your GP.
Hives (urticaria)
Hives is also known as urticaria.
About hives
- causes a raised, red itchy rash that appears on the skin
- happens when a trigger (such as a food that your baby is allergic to) causes a substance called histamine to be released into their skin
If your baby gets urticaria during feeding, the condition may be triggered by something they've had to eat or drink. The most common foods are egg and milk, but many other foods can sometimes be the cause.
The most common foods are egg and milk, but many other foods can sometimes be the cause.
The urticaria rash is usually short-lived and can be controlled with antihistamines. If your baby gets hives repeatedly, it's important to see your GP to discuss possible allergies.
Impetigo
Impetigo is a highly contagious bacterial infection of the surface layers of the skin. It causes sores and blisters.
It's not usually serious, but you can visit your GP for a prescription of antibiotics. This should clear the infection within seven to 10 days.
Milia
About half of all newborns develop tiny (1-2mm) white spots on their face. These are called milia.
These are just blocked pores. They usually clear within the first four weeks of life.
Nappy rash
Nappy rash occurs when the skin around the baby's nappy area becomes irritated.
About nappy rash
- is often caused by exposure to wee or poo for a long period of time
- can sometimes be the result of a fungal infection or rare skin condition
You can usually reduce nappy rash by taking simple steps to keep your baby's skin clean and dry.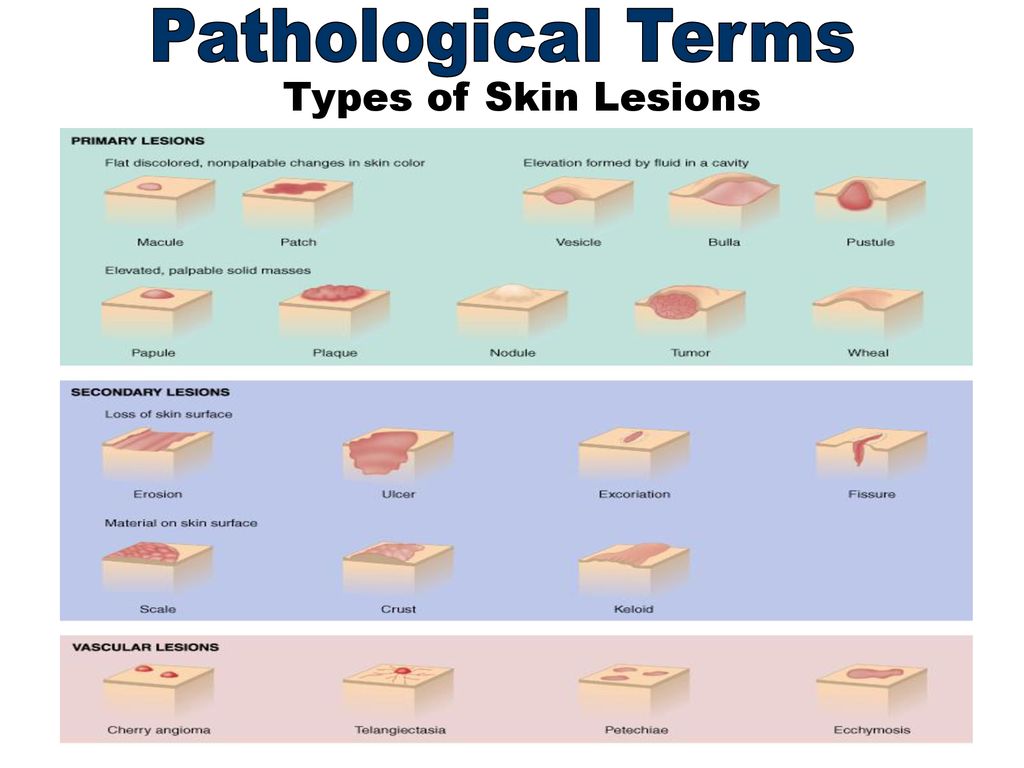 You can use a barrier cream if needed. Antifungal cream may be necessary if the rash is caused by a fungal infection.
You can use a barrier cream if needed. Antifungal cream may be necessary if the rash is caused by a fungal infection.
- read more about nappies and nappy rash
Ringworm
Ringworm is a common fungal skin infection. It causes a ring-like red rash almost anywhere on the body (the baby's scalp, feet and groin are common areas).
It's usually easily treated using over-the-counter creams.
Ask your pharmacist if you need advice about treatment.
Scabies
Scabies is a common infestation of the skin that can affect people of all ages.
About scabies
- it's caused by tiny mites that burrow into the skin
- it's often spread between family members, so when babies get scabies it's usually because someone else in the family had it recently
- babies with scabies develop tiny and very itchy spots all over the body, including on the soles of the feet, armpits and genital area
Treatment with creams that kill the scabies mite needs to be given to the whole family at the same time for it to be effective.
Visit your GP if you think your baby has scabies. It's not usually a serious condition, but it does need to be treated.
Your GP will discuss treatment with you. The treatments most widely used are a cream and lotion.
Slapped cheek syndrome
Slapped cheek syndrome is a viral infection particularly common in children and babies.
About slapped cheek syndrome
- it typically causes a bright red rash on both cheeks and a fever
- most babies won't need treatment, as slapped cheek syndrome is usually a mild condition that passes in a few days
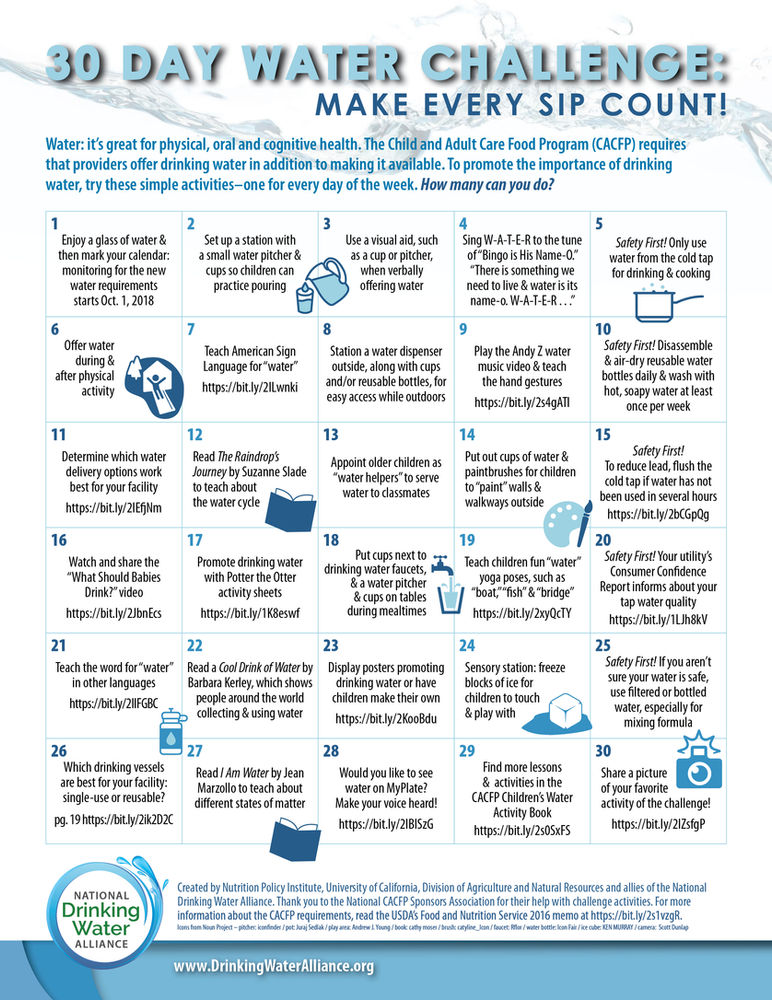
Sweat rash (miliaria)
A heat rash is sometimes called miliaria or prickly heat. It may flare up when your baby sweats. For example, because they're dressed in too many clothes or the environment is hot and humid.
It's a sign your baby's sweat glands have become blocked.
They may develop tiny red bumps or blisters on their skin, but these will soon clear without treatment.
Meningitis
Meningitis is an infection of the protective membranes that surround the brain and spinal cord (meninges).
About meningitis
- the classic rash associated with meningitis usually looks like small, red pinpricks at first
- it then quickly spreads over the body and turns into red or purple blotches
- it is a blotchy rash that doesn't fade when a glass is rolled over it (this won't always develop)
Meningitis warning signs
It's important to be aware of the warning signs of meningitis in your baby, which include:
- becoming floppy and unresponsive, or stiff with jerky movements
- becoming irritable and not wanting to be held
- unusual crying
- vomiting and refusing feeds
- pale and blotchy skin
- loss of appetite
- staring expression
- very sleepy with a reluctance to wake up
- fever
Some babies develop a swelling in the soft part of their head (fontanelle).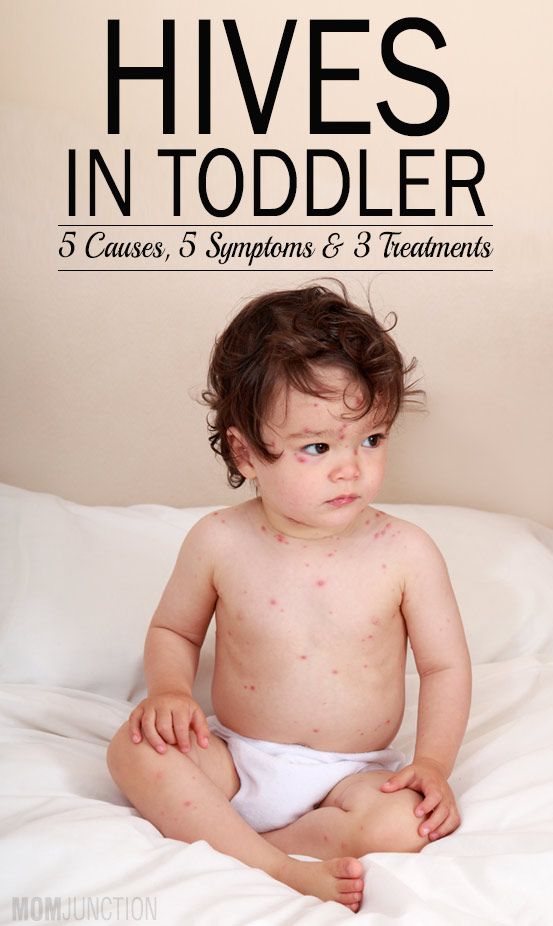
Trust your instincts. If you think your baby has meningitis, see your GP or GP out of hours service immediately or go to your nearest emergency department.
- find out more about skin rashes in babies on the NHS website
More useful links
- How to use your health services
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
What do you want to do?report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.
Enter your feedback
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
Treating nappy rashIf your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.
- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.
- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.
Other rashes in the nappy areaIf the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child.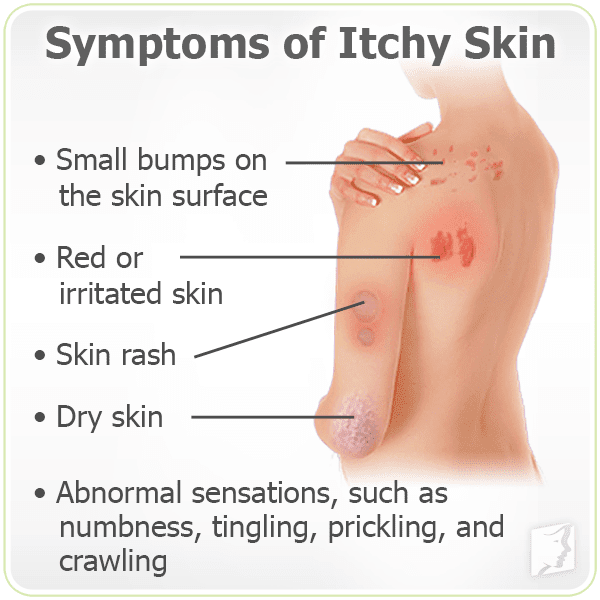 The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum.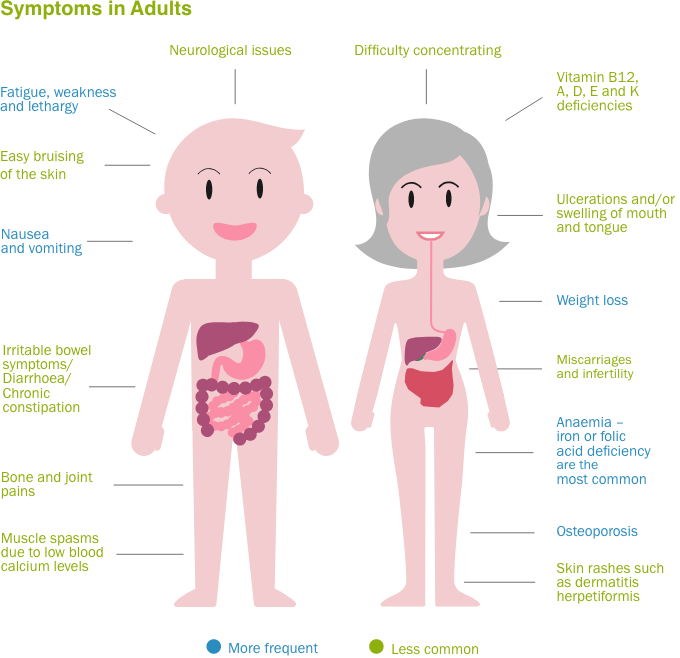 The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.![]()
Usually, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc.). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.
Author:
Eroshkina Maria Sergeevna
pediatrician
Red pimples on the face of a newborn: symptoms, causes and treatment
Allergic rash in a newborn
An allergy in a baby is an unfavorable immune response of a child's body to a potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberries;
- nuts.

The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.
Neonatal acne
Neonatal acne may appear in the first weeks of a child's life on the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the reason for the appearance of acne is increased production of sebum, which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system. The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Miliaria
Miliaria is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small vesicles with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Prickly heat by itself is not dangerous to the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection. In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn. These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
In fact, the disease is caused by high levels of maternal hormones in the blood or changes in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only to take care of proper care , but diligently removing the crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns. He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Milk crust cream which helps to completely remove milk crusts in an average of 7 days [5. 3].
3].
Atopic dermatitis
Atopic dermatitis is an allergic disease that is accompanied by chronic inflammation of the skin. Causes of an uncontrolled allergic reaction in infants are:
- food allergens - animal protein, soy products, certain types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.
Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.1]
- Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper area zone in infants. The rash appears as a result of prolonged contact of the body with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious).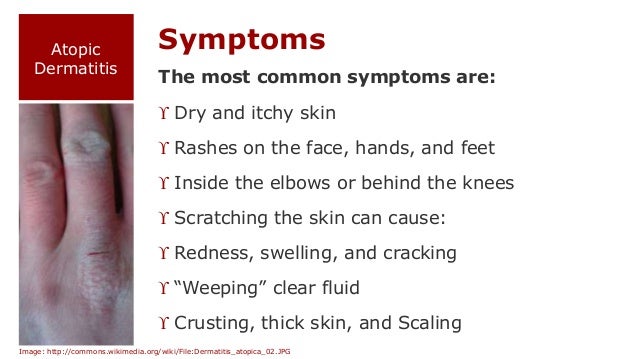 The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
For non-drug treatment of pathology, air baths [7], bathing in a decoction of string and celandine [8], and thorough hygiene procedures are indicated. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, repairs and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
____________________________________________________________________________________________
Literature:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Kherani M.I., Ando I. Acne in infancy and the genetics of acne // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3. Zanko NI Efficiency of new technologies for skin care in young children: Abstract of the thesis. dis. ... cand. honey. Sciences, M., 2000
4. Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis.
N Engle G Med. 360(4):387-96 (2009 January).
5. Results of the study 1035 F4.
5.1 Study results 1016F10.01.02
5.2 Study results 1008F4.01.16
5.3 Study results 1042F3.01.24
Dermatol. 2005; 53: S214-S219.
7. Galliamova Yu.A. Diaper dermatitis and skin trauma in children. Attending doctor.