Signs of yeast infection pregnancy
Yeast Infections During Pregnancy: What To Do
Written by Camille Peri
Reviewed by Dan Brennan, MD on August 09, 2022
In this Article
- What is a Yeast Infection During Pregnancy?
- Symptoms of a Yeast Infection During Pregnancy
- Causes of a Yeast Infection During Pregnancy
- Treating a Yeast Infection During Pregnancy
- Preventing a Yeast Infection During Pregnancy:
What is a Yeast Infection During Pregnancy?
Yeast infections (also known as candidiasis) are common in women, especially when you're pregnant. Increased estrogen in your pregnant body can throw off the normal balance of yeast and bacteria in your vagina. This may let the yeast overgrow. Most yeast infections during pregnancy result from the fungus candida albicans. Two other kinds of yeast that can also cause them are candida glabrata and candida tropicalis.
Yeast infections aren't pleasant, but they won't hurt you or your baby. And they can be safely treated, usually with a topical cream.
Symptoms of a Yeast Infection During Pregnancy
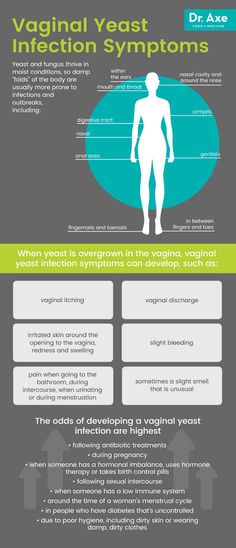
You might notice:
- Itching
- Burning
- Redness or swelling in your vulva, the area outside your vagina.
- Thick, white vaginal discharge that looks like cottage cheese.
Causes of a Yeast Infection During Pregnancy
- Taking antibiotics, which can cause that can change the balance of yeast and bacteria in your vagina.
- Diabetes that isn’t well controlled
- Conditions like HIV or medications, like corticosteroids that make it harder for your immune system to work well.
- If your sexual partner has a yeast infection, it can be passed to you during vaginal sex.
Treating a Yeast Infection During Pregnancy
It's safe to treat a yeast infection with over-the-counter (OTC) vaginal creams or suppositories that contain miconazole or clotrimazole.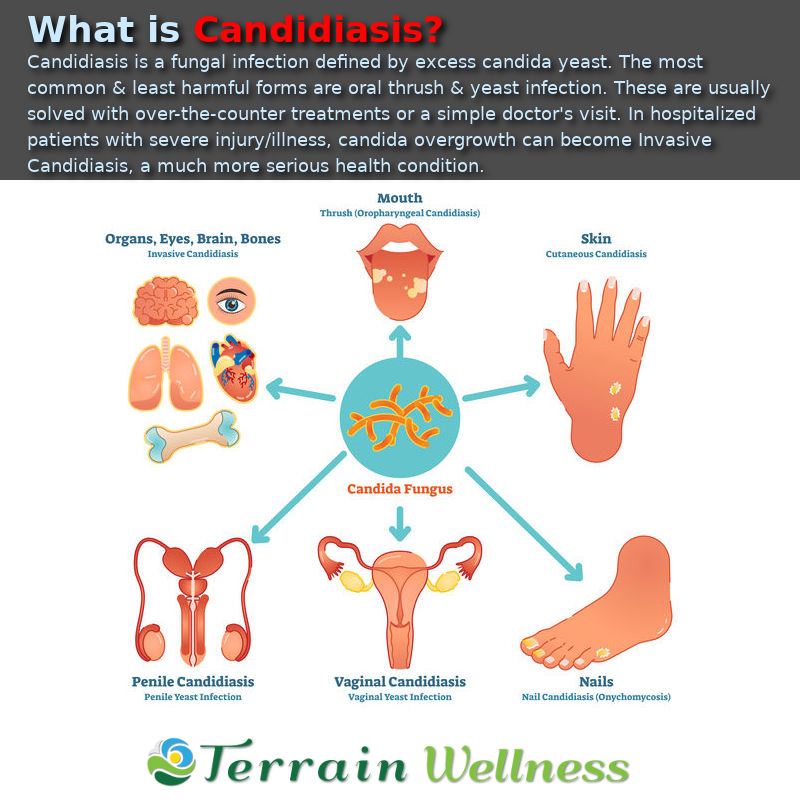
Don’t take an oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects.
If you think you have a yeast infection, call your doctor before using over-the-counter medications to treat it.
Preventing a Yeast Infection During Pregnancy:
- Wear cotton underwear and pantyhose with a cotton crotch to keep your vaginal area dry and let it "breathe."
- Always wipe from front to back after you go to the bathroom.
- Don't douche. It can upset the balance in your vagina. In late pregnancy, it may also cause your water to break.
- Avoid tight pants and pantyhose.
- Change out of a wet swimsuit or sweats immediately. This keeps the genital area dry.
- Avoid toilet paper, feminine sprays, bubble bath, and sanitary pads that are scented.
- Keep good control of your blood sugar if you have diabetes.
- Eat yogurt with live cultures; some research suggests this can help.
 All rights reserved. View privacy policy and trust info
All rights reserved. View privacy policy and trust info Yeast Infections During Pregnancy: What To Do
Written by Camille Peri
Reviewed by Dan Brennan, MD on August 09, 2022
In this Article
- What is a Yeast Infection During Pregnancy?
- Symptoms of a Yeast Infection During Pregnancy
- Causes of a Yeast Infection During Pregnancy
- Treating a Yeast Infection During Pregnancy
- Preventing a Yeast Infection During Pregnancy:
What is a Yeast Infection During Pregnancy?
Yeast infections (also known as candidiasis) are common in women, especially when you're pregnant. Increased estrogen in your pregnant body can throw off the normal balance of yeast and bacteria in your vagina. This may let the yeast overgrow. Most yeast infections during pregnancy result from the fungus candida albicans. Two other kinds of yeast that can also cause them are candida glabrata and candida tropicalis.
Yeast infections aren't pleasant, but they won't hurt you or your baby. And they can be safely treated, usually with a topical cream.
Symptoms of a Yeast Infection During Pregnancy
You might notice:
- Itching
- Burning
- Redness or swelling in your vulva, the area outside your vagina.
- Thick, white vaginal discharge that looks like cottage cheese.
Causes of a Yeast Infection During Pregnancy
- Taking antibiotics, which can cause that can change the balance of yeast and bacteria in your vagina.
- Diabetes that isn’t well controlled
- Conditions like HIV or medications, like corticosteroids that make it harder for your immune system to work well.
- If your sexual partner has a yeast infection, it can be passed to you during vaginal sex.
Treating a Yeast Infection During Pregnancy
It's safe to treat a yeast infection with over-the-counter (OTC) vaginal creams or suppositories that contain miconazole or clotrimazole.
Don’t take an oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects.
If you think you have a yeast infection, call your doctor before using over-the-counter medications to treat it.
Preventing a Yeast Infection During Pregnancy:
- Wear cotton underwear and pantyhose with a cotton crotch to keep your vaginal area dry and let it "breathe."
- Always wipe from front to back after you go to the bathroom.
- Don't douche. It can upset the balance in your vagina. In late pregnancy, it may also cause your water to break.
- Avoid tight pants and pantyhose.
- Change out of a wet swimsuit or sweats immediately. This keeps the genital area dry.
- Avoid toilet paper, feminine sprays, bubble bath, and sanitary pads that are scented.
- Keep good control of your blood sugar if you have diabetes.
- Eat yogurt with live cultures; some research suggests this can help.
 All rights reserved. View privacy policy and trust info
All rights reserved. View privacy policy and trust info Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for the occurrence of a recurrent form of thrush are those pregnant women who have already had episodes of thrush in their anamnesis the level of estrogens rises, in connection with which glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida.
Lactobacilli are the predominant microorganisms in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply.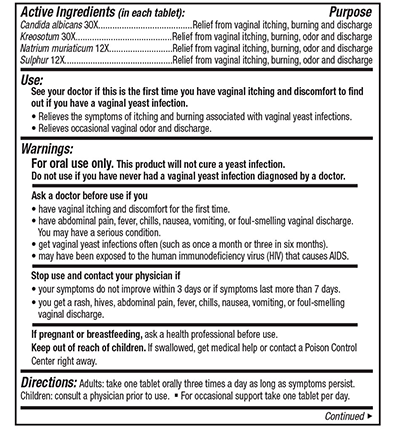 These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush.
These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush.
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and/or vagina, swelling and irritation in the vulva
- vaginal discharge with a "curdled character" and occasional foul odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor.
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and do not experience any discomfort or manifestation of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women
The earlier a pregnant woman is diagnosed and treated for thrush, the less the risk of negative consequences and complications for the course of pregnancy and for the health of the mother and her unborn child. In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosage and regimen.
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® in the treatment of thrush in pregnancyEcofucin
® is allowed at all stages of pregnancy and lactation 4
Natamycin
- practically not absorbed into the blood and has no systemic effect
- has a fungicidal effect - causes fungal cell death
- resistance to it does not develop
- does not inhibit the growth of natural microflora
+
Prebiotic 5
- actively fermented by the normal microflora of the vagina, stimulating the growth of lactobacilli 6
- causes restoration of the vaginal microflora, stimulates local immunity 6
The active substance 7 of the drug Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in the composition of the drug Ecofucin ® helps to restore the vaginal microflora and strengthen local immunity 6 .
Efficacy and safety of the drug Ecofucin proven by clinical studies
Ecofucin promotes faster recovery of patients with thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Ecofucin helps to increase the number of own lactobacilli in the vagina and reduce the risk of recurrence of thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Dosage and Administration
The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually.
Additional conditions for effective treatment of thrush are: giving up bad habits, a carbohydrate-restricted diet, wearing underwear made from natural fabrics, etc.
It is important to consult a gynecologist in a timely manner and exclude self-medication.
1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Farmateka No. 9, 2009, p. 64-70.
2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis". // 2013.
3. Kupert A.F., Akudovich N.V., Khoroshikh O.V., Vereshchagina S.A., Khmel T.V. Features of the clinic and treatment of vaginal candidiasis in pregnant women, depending on the type of fungi of the genus Candida. // Gynecology. v. 05, N 5b, 2003.
4. Instructions for use of the drug Ecofucin ® .
5. Excipient, lactulose.
6. Dikovskiy A.V., Dorozhko O.V., Rudoy B.A. Pharmaceutical composition of antimycotics and prebiotics and a method for the treatment of candidal vaginitis. // International publication WO 2010/039054 A1.
7. Active ingredient, natamycin.
symptoms, treatment (1st, 2nd, 3rd trimesters)
Did you know that every third woman in the world suffers from candidiasis? At the same time, thrush occurs three times more often in pregnant women. Let's take a look at the causes of thrush together, and also talk about the main symptoms and methods of treating thrush at different stages of pregnancy.
Lyudmila Starichenko
Higher qualifying category,
Chief physician of innovative technologies Clinic
Work experience 41 years
Learn the details on the site
of the cause of the thrush
Seumes and symptoms of thrush in pregnant women
Treatment Treatment pregnant women
What to avoid when treating thrush?
Why is thrush dangerous during pregnancy?
What if it doesn't go away?
Prevention
Causes of thrush
Thrush or vulvovaginal candidiasis is a common disease of the vaginal mucosa. The main reason for its appearance is a fungal infection.
The main reason for its appearance is a fungal infection.
Pregnant women are at particular risk. After all, in this position, the patient has a natural decrease in immunity, which can even lead to a decrease in local immunity. As a result, the inevitable growth of opportunistic microorganisms occurs. Among them are yeast-like fungi that cause candidiasis. Changes in the hormonal background, namely, an increase in the level of female sex hormones, can also affect the increased growth of yeast-like fungi. This is especially true for patients whose pregnancy goes with complications.
Read more about the causes of candidiasis in our material.
learn more
Signs and symptoms of thrush in pregnancy
The signs and symptoms of thrush in pregnancy are no different from the usual symptoms of thrush. They differ only in what particular organ is affected by thrush.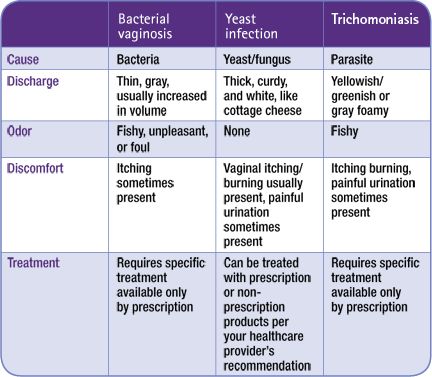
So, for example, with urogenital candidiasis, the most characteristic symptoms are discharge from the genital tract, itching, burning in the genital area and its intensification during sleep and water procedures.
Treatment of thrush in pregnant women
All medications during pregnancy must be selected by a doctor. Self-treatment is excluded here, because by wrong actions a woman can harm not only herself, but also her child!
As a rule, only local therapy is prescribed during pregnancy at any time.
First trimester
In the first trimester, use Natamycin 100 mg intravaginally for 6 days. The drug refuses fungicidal and antifungal action. Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Natamycin is active against most yeast-like fungi, and especially against fungi of the genus Candida. The advantage of this drug is that it does not have a systemic effect and is not absorbed into the gastrointestinal tract, acting only locally on the damaged mucous membrane. Of the possible side effects with topical application - only irritation and burning sensation at the site of application.
Second and third trimesters
In the II and III trimester, use Sertoconazole 300 mg intravaginally once. This drug has a powerful antifungal effect by increasing the permeability of the cell membrane, which leads to the destruction of the cells of the opportunistic fungus. Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
After appoint Econazole 150 mg intravaginally for 3 days. The drug has a local antifungal and antibacterial effect. It stops the biosynthesis of ergosterol and other sterols that regulate the permeability of the fungal cell wall. With intravaginal administration, patients did not experience pregnancy complications or other undesirable effects of therapy on reproduction. Local reactions are possible: rash, burning, irritation, itching, redness and dryness of the skin.
The last stage of treatment is Clotrimazole 100 mg intravaginally for 6-10 days. The drug belongs to a broad spectrum antifungal agent. It is applied topically only by the intravaginal method. Clotrimazole inhibits the growth and division of microorganisms.
The mechanism of action of the drug is associated with a change in the permeability of cell membranes.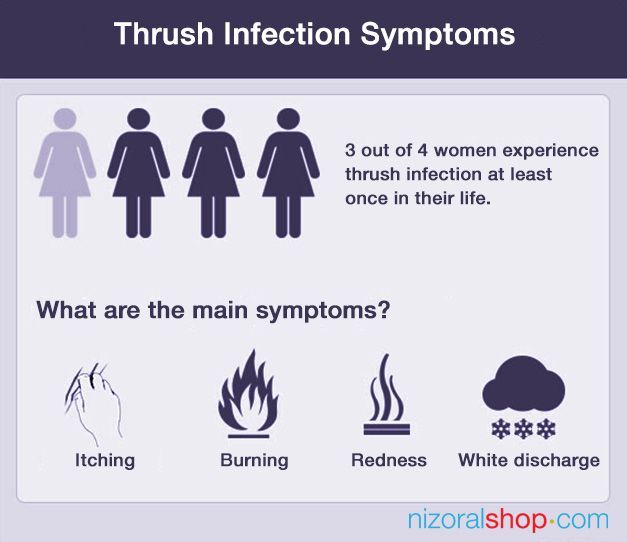 It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
In addition, when treating candidiasis, it is recommended to follow a diet. About what products can be consumed, and which are better not worth it, read in our material.
Folk methods
It should be said that the doctor we consulted does not advise using folk remedies for thrush, as they simply cannot help with this disease. But on the Internet, some means are indicated. Among them: douching and tar soap, soda and chamomile, potassium permanganate and sea buckthorn oil.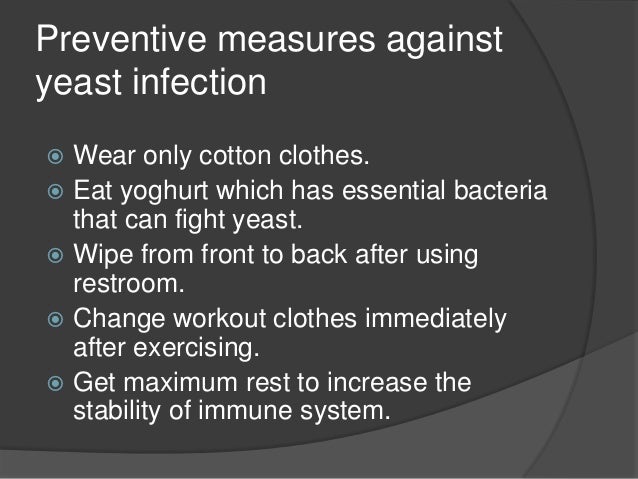
For more information on how to use these folk remedies, look in our material.
However, we want to remind you once again that none of the folk remedies is a panacea for thrush. Alternative recipes can reduce the intensity of unpleasant symptoms, but can not cure candidiasis. Therefore, we recommend that you seek professional medical help without fail and do not self-medicate.
find out how to get diagnosed
What to avoid when treating thrush?
First of all, do not self-medicate. This advice is especially relevant during pregnancy. Not all drugs are compatible with pregnancy, and which of them can or cannot be taken - only the attending physician can decide!
As we said above, during pregnancy, only local therapy is prescribed. Ignorance of these features can adversely affect the fetus.
Ignorance of these features can adversely affect the fetus.
Why is thrush dangerous during pregnancy?
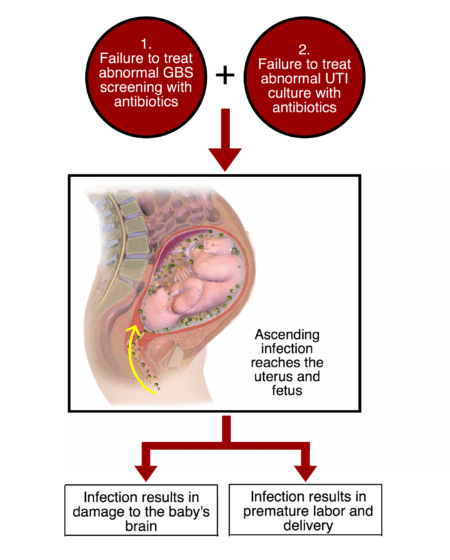
Thrush is dangerous during pregnancy. At this time, an ascending infection with intrauterine infection of the fetus and a newborn with the development of intrauterine infection is possible.
You shouldn't start this disease. This is fraught not only with unpleasant symptoms, but also with consequences for the body. Candidiasis carries the following complications: systemic damage to the pelvic organs, a significant decrease in the quality of life, constant discomfort, dysbiotic disorders of the microflora of the intestinal tract. During pregnancy, the effects may intensify.
What to do if it doesn't go away?
Unfortunately, thrush can easily develop from an active to a chronic form. This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
If candidiasis does not go away during pregnancy or returns, you should not fight it yourself according to the prepared scheme from the last time. The patient needs to contact the attending physician again to select the most effective drugs.
This is especially true for pregnant women. Drugs used outside of pregnancy can not only not help, but also harm.
Prevention
How to avoid unpleasant symptoms and consequences of thrush? This is not so difficult to do if you strictly follow the basic rules of prevention and hygiene. Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Conclusion
During pregnancy, a woman has a natural decrease in immunity, which may, unfortunately, lead to the milkpan. And if you do not start a fight with it in time, then the disease can be transmitted to the child. However, with timely treatment and elimination of the factors that cause the disease, it is possible to forget about this disease once and for all. The main thing is not to start thrush to a chronic form. Only a medical specialist will be able to individually select for you a treatment that will cope with the disease.