Signs of miscarriage while on birth control
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.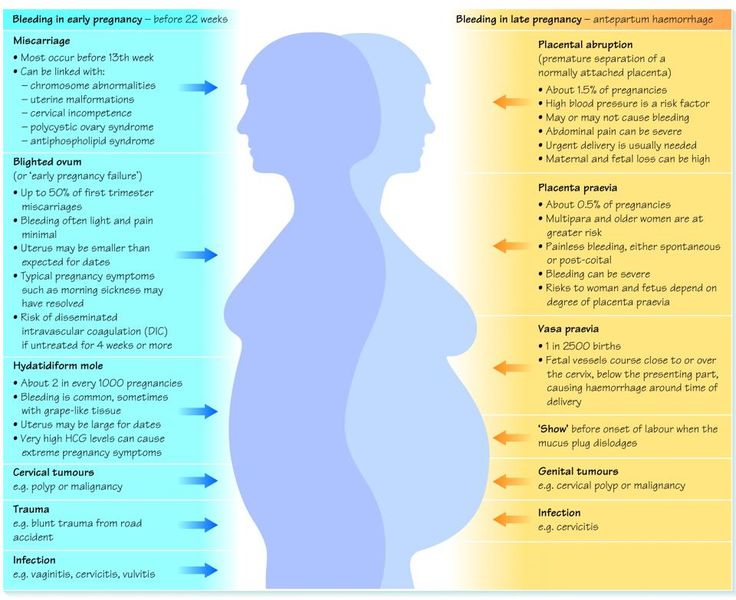
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
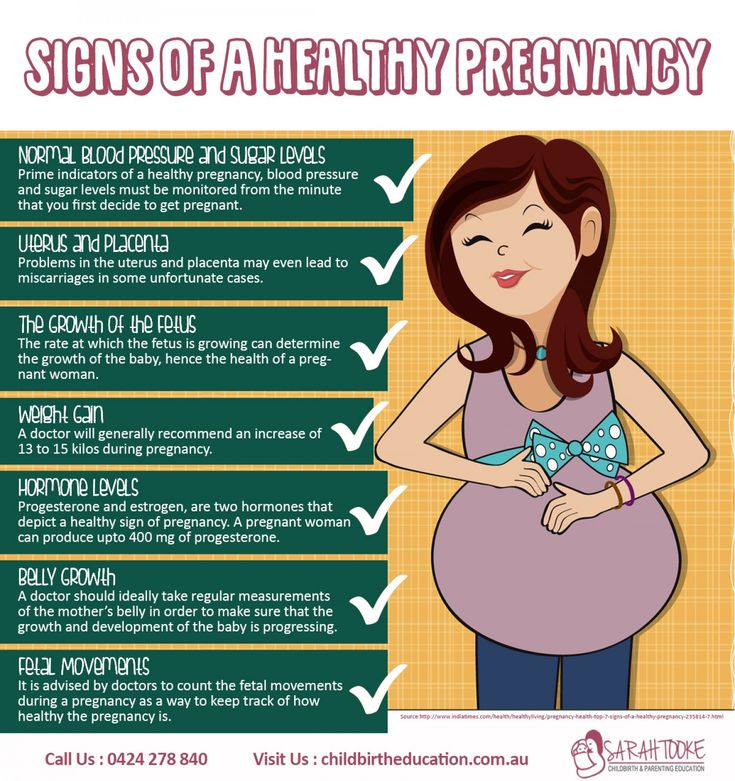
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress. If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining.
 This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause. Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage. But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
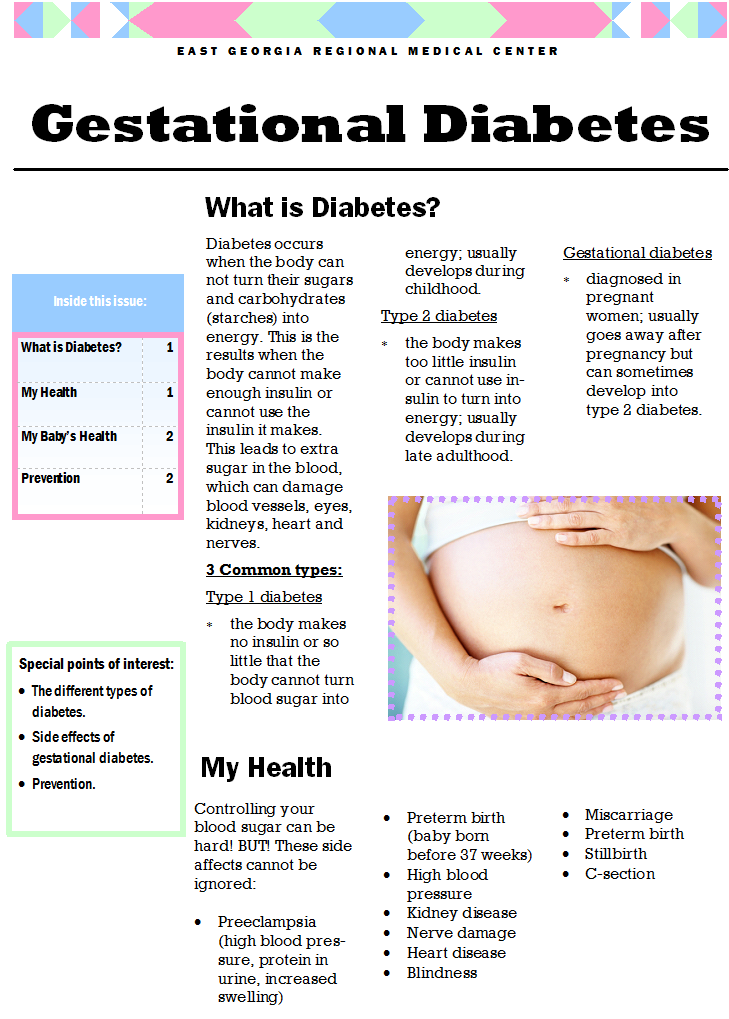
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
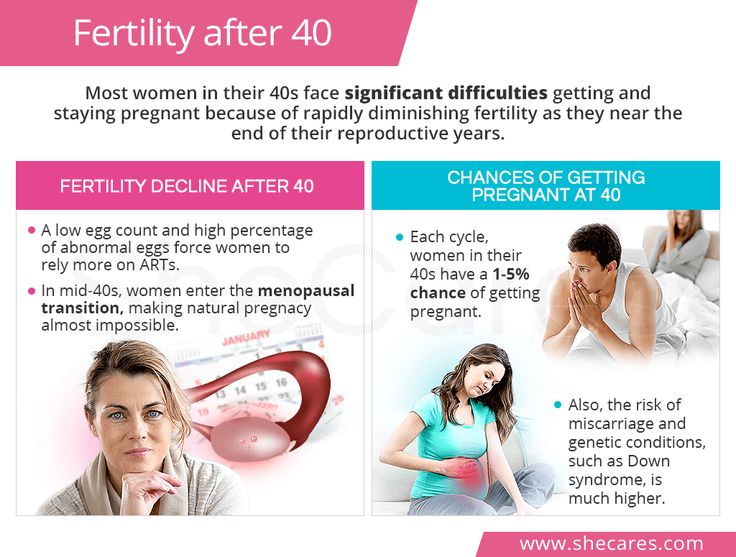
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks. This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week. It will take about four to eight weeks for your regular period to return.
It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment. You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
Miscarriage Signs & Symptoms | How to Recognize Miscarriage
In This Section
- Miscarriage
- How do I know if I'm having a miscarriage?
The most common signs of a miscarriage are bleeding and cramping.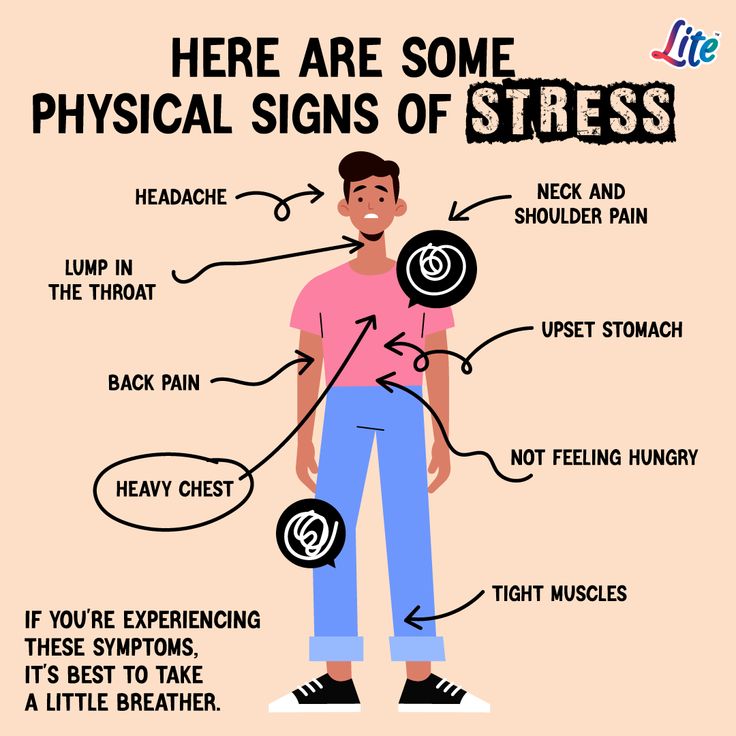 Call your doctor if you think you’re having a miscarriage.
Call your doctor if you think you’re having a miscarriage.
What are the signs of miscarriage?
Sometimes, there are no miscarriage symptoms and you don’t find out until an ultrasound, or you don’t feel pregnant anymore. Usually there are signs and symptoms. They include:
Other things that are less serious than miscarriage can also cause these symptoms. But if you think you might be having a miscarriage, see your doctor right away just to be safe.
What happens during a miscarriage?
Miscarriages are different for every person, but there are some common symptoms.
Not all miscarriages are physically painful, but most people have cramping. The cramps are really strong for some people, and light for others (like a period or less). It’s also common to have vaginal bleeding and to pass large blood clots up to the size of a lemon. Heavy miscarriage bleeding can be scary or surprising, but it’s usually normal.
The bleeding and cramping can end quickly, or it may last for several hours.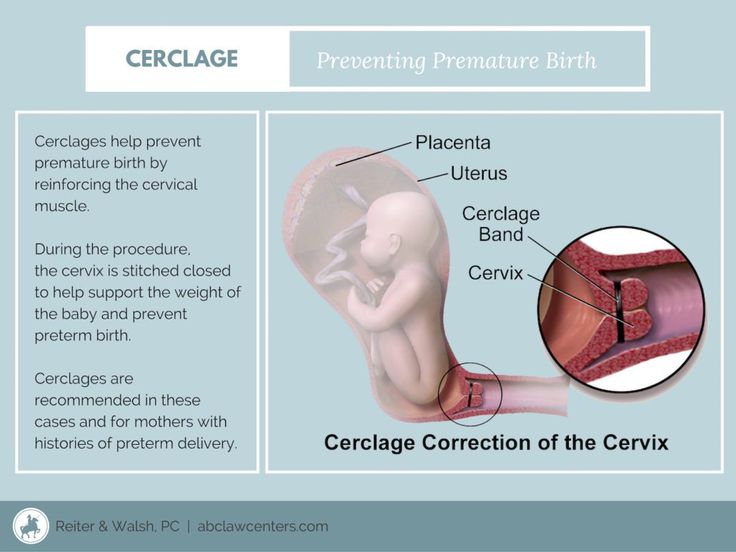 Your doctor can give you medicine and tips on how to manage pain and cramps during your miscarriage.
Your doctor can give you medicine and tips on how to manage pain and cramps during your miscarriage.
No matter how fast it happens or whether or not it hurts, miscarriage can be upsetting. Keep in touch with your doctor about what’s going on and how you’re feeling. Your doctor can let you know what is and isn’t normal, and give you resources for emotional support if you need it.
What can I expect to feel after having a miscarriage?
There’s no one way that all people feel after having a miscarriage. You may feel a mix of emotions, including disappointment, despair, shock, guilt, grief, and relief — sometimes all at the same time. All of these feelings are really normal, and usually fade as time passes.
Take care of yourself physically and emotionally, and give yourself permission to grieve your loss if you need to. Grief and sadness are very normal responses to miscarriage. Try to surround yourself with supportive and loving people who will let you grieve and comfort you.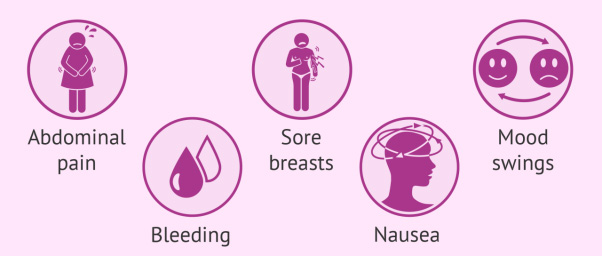 If you have a partner, they may be grieving the loss and dealing with a range of emotions, too. Talking about your feelings and supporting each other can help you both cope.
If you have a partner, they may be grieving the loss and dealing with a range of emotions, too. Talking about your feelings and supporting each other can help you both cope.
The amount of time it takes to emotionally heal after a miscarriage is different for everyone. Give yourself as much time as you need to grieve. Most people feel better when they have someone supportive to talk to. Even if you don’t think there’s anybody in your life you can lean on, know that you’re not alone. Your nurse or doctor can talk with you, or help you find a counselor or support group in your area. There are also many online support groups, where you can connect with others who are going through the same thing as you. All-Options has a free hotline that gives you a private space to talk about your feelings after a pregnancy loss.
If you want to get pregnant again, your doctor or local Planned Parenthood health center can give you advice on planning your next pregnancy and help you figure out when it’s best to start trying again. They can also give you tips on preventing pregnancy and help you get birth control if you don’t want to get pregnant right now.
They can also give you tips on preventing pregnancy and help you get birth control if you don’t want to get pregnant right now.
What if I’ve had more than 1 miscarriage?
If you’ve had 2 or more miscarriages in a row, your doctor might want to do some tests to help figure out if something specific is causing problems with your pregnancies. The tests will check for any hormonal imbalances, genetic disorders, or other problems. Some conditions can be treated to help you have a healthy pregnancy in the future.
More questions from patients:
What does a miscarriage look like?
Miscarriages look different for everyone, but there are some common symptoms. They include:
-
vaginal bleeding or spotting
-
severe belly pain
-
severe cramping
-
dull, lower-back ache, pressure, or pain
-
a change in vaginal discharge
Other things that are less serious than miscarriage can also cause these symptoms. But if you think you’re having a miscarriage, visit your doctor, your local Planned Parenthood health center, or a hospital right away to be safe.
But if you think you’re having a miscarriage, visit your doctor, your local Planned Parenthood health center, or a hospital right away to be safe.
If it’s a miscarriage, your symptoms may end quickly or last for several hours. The cramps are really strong for some people, and really light for others. The bleeding can be heavy, and you can pass large blood clots up to the size of a lemon.
Sometimes, there are no signs of a miscarriage and you don’t find out until you have an ultrasound, or you don’t feel pregnant anymore.
No matter how fast it happens or whether or not it hurts, going through a miscarriage can be really hard. Keep in touch with your doctor about what’s going on and how you’re feeling. Your doctor can let you know what is and isn’t normal, and give you resources for emotional support if you need it.
Was this page helpful?- Yes
- No
Help us improve - how could this information be more helpful?
How did this information help you?
Please answer below.
Are you human? (Sorry, we have to ask!)
Please don't check this box if you are a human.
You’re the best! Thanks for your feedback.
Thanks for your feedback.
Oral contraceptive use and pregnancy Online magazine
Every year, 1-10 women out of 10,000 of the fair sex who use this method of protection experience pregnancy on the background of combined oral contraceptives (COCs). Although, according to the instructions, it is recommended to additionally use a barrier method (condom or other) only in the first 7 days of taking COCs.
To determine how reliable this or that method of contraception is, an American biologist created the Pearl Index, based solely on experiments.
It reflects the number of pregnancies in 100 girls who use any contraceptive during one year. The lower the index value, the more reliable the contraceptive method under study. The most common method - a condom - has an index of 7-14%. Taking hormonal contraceptive pills is more effective (the index is 0.1 -0.9).
The most common method - a condom - has an index of 7-14%. Taking hormonal contraceptive pills is more effective (the index is 0.1 -0.9).
What is the reason for the “failure” of the drug? Let's try to figure it out, because, taking COC, every woman wants to be sure of the result.
1. "Wrong" choice of contraceptive
Often, when she becomes pregnant while taking COCs, the patient blames herself or the doctor for the fact that the pills were chosen incorrectly. Actually it is not. All COCs have a similar composition, contain estrogens (ethinyl estradiol) and gestagens (analogues of natural progesterone), and the differences between them are only in the chemical structure of these substances and their dosages. In any case, the mechanism of action of all such hormonal pills is to block ovulation.
Gestagen-containing birth control pills (mini-pills) block ovulation not in 100% of cases, but they thicken the cervical mucus, preventing the penetration of spermatozoa into the uterus and preventing the implantation of the fetal egg. More often they are prescribed for unstable ovulation, for nursing mothers, for example.
More often they are prescribed for unstable ovulation, for nursing mothers, for example.
Thus, all oral contraceptives are quite reliable.
2. Violation of the pill regimen
OCs are usually started on the 2-5th day of the menstrual cycle, that is, immediately after the next menstruation begins and there is confidence in the absence of pregnancy. Many people think that the contraceptive effect of the drug appears immediately, literally from the first pill, in fact it is not. That is why it is recommended to use additional methods of protection in the first 7-14 days from the start of taking COCs.
Also in the instructions for any COC it is said that the tablets should be taken every day at the same time. Violation of the intake regimen can actually cause pregnancy.
If the delay in taking the pill is more than 12 hours, you can not count on reliable protection. You should immediately take the missed dose, take the next one at the usual time, and use other means of protection in addition to COCs, such as a condom or spermicide, for the next seven days.
3. Disorders of the stomach
If vomiting occurs within three hours after taking another COC tablet, it is likely that the medicine was not absorbed and came out with vomit. If, after stopping vomiting, you do not immediately take an extraordinary dose of the drug, it is quite possible to weaken the contraceptive effect and the onset of pregnancy.
If diarrhea occurs, you should not worry, although you can play it safe and take another pill, there will be no harm from it, but protection will be enhanced and pregnancy will not occur - that's for sure.
4. Taking medications
Decreased effectiveness of hormonal protection may be caused by the interaction of COCs with other drugs. In particular, it has been proven that antibiotics from the group of rifampicin and ampicillin, non-steroidal anti-inflammatory drugs, as well as drugs that affect the enzymatic activity of the liver and accelerate the excretion of hormones from the body, affect the contraceptive ability of tablets.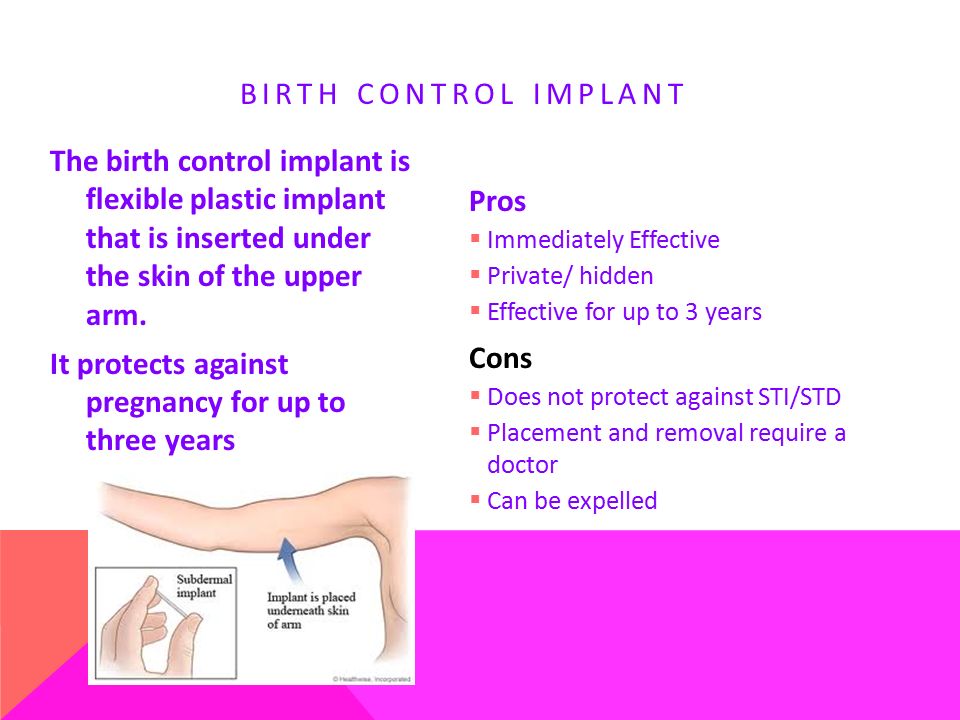
You should always inform your doctor about the use of a hormonal method of contraception and, if it is not possible to change the drug, use additional methods of protection against unwanted pregnancy. It is generally required to use a condom or spermicides within 4 weeks after stopping the medication prescribed for the disease. If there is a need for long-term treatment, you should stop taking COCs in favor of other methods of contraception.
5. Intermenstrual spotting
By itself, the discharge does not reduce the effectiveness of OK, rather, there is a feedback here. The appearance of bloody discharge between menstruation indicates that the woman's body does not have enough hormones introduced from the outside in order to reliably insure her against the occurrence of an unwanted pregnancy.
If bloody discharge from the genital tract occurs, it is recommended to stop taking the tablets from the package and discuss with the attending gynecologist the replacement of this drug with a higher dose. In conclusion, I would like to say that the onset of pregnancy while taking COCs does not threaten the woman and the unborn child in any way. Such a pregnancy can be left, the probability of fetal malformations in this case is the same as the average for the population.
In conclusion, I would like to say that the onset of pregnancy while taking COCs does not threaten the woman and the unborn child in any way. Such a pregnancy can be left, the probability of fetal malformations in this case is the same as the average for the population.
6. Pregnancy with OCs
What to beware of is more than 3 weeks of OCs during pregnancy. In the absence of another menstrual bleeding during the seven-day break in taking OK, you should not start the next pack until there is no certainty that there is no pregnancy. It is necessary to do a blood test for hCG or take a pregnancy test.
Threatened miscarriage: treatment, causes and symptoms, diagnosis and prevention
A miscarriage is a spontaneous abortion, in other words, the loss of a fetus that occurs in the early stages of pregnancy. According to statistics, about 15 percent of women who want to become mothers face such a problem. In some cases, even under the condition of a critical situation, a miscarriage can be prevented.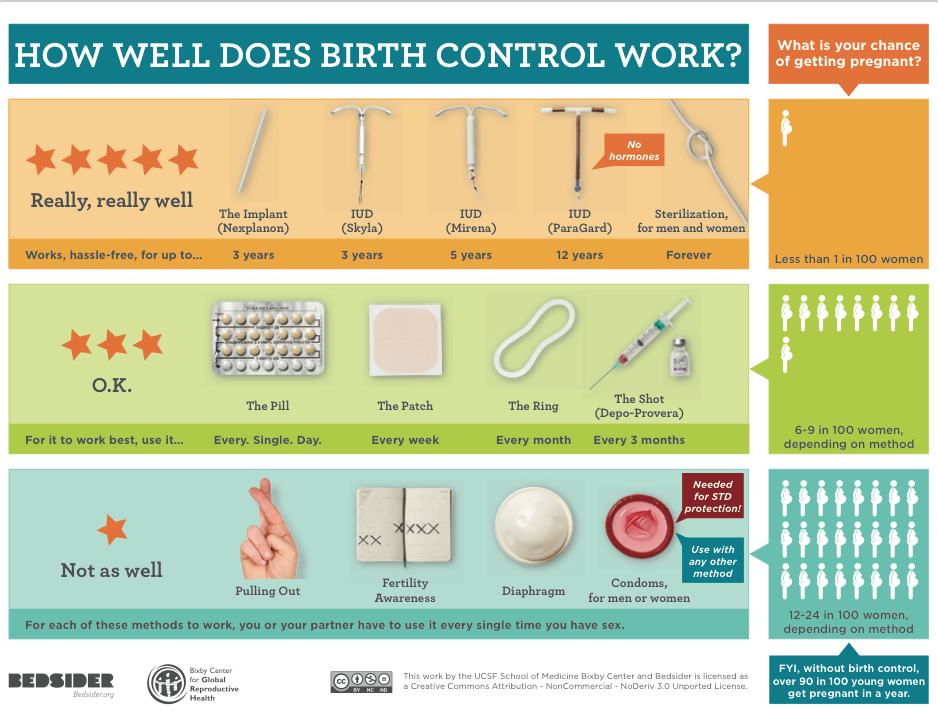 The purpose of preventive measures depends on the cause of the rejection of the fetus.
The purpose of preventive measures depends on the cause of the rejection of the fetus.
Obstetrician-gynecologist, ultrasound specialist
7 reviews
63
st. Victory, 17, m Victory Park
Obstetrician-gynecologist, ultrasound diagnostician, leading specialist
53 reviews
498
st. Victory, 17, m Victory Park
Obstetrician-gynecologist of the highest category, doctor of ultrasound diagnostics, Ph.D.
0 reviews
27
Engels Ave., 61, building 2, m Specific
Obstetrician-gynecologist, ultrasound specialist
114 reviews
713
st. Victory, 17, m Victory Park
Obstetrician-gynecologist, doctor of ultrasound diagnostics, candidate of medical sciences, head of the department of obstetrics and gynecology
83 reviews
574
Engels Ave.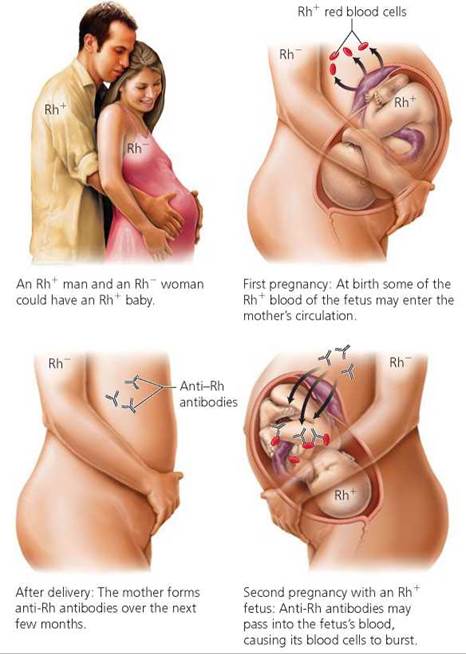 , 61, building 2, m Specific
, 61, building 2, m Specific
st. Victory, 17, m Victory Park
Would you like us to call you back?
Leave a request and we will answer all your questions in detail
Name Phone *
I have read privacy policy .
Why EMS Family Clinic
Medicine for the whole family, doctors in more than 30 specialties for adults and children
Integrative Anti-Aging Medicine Approach
Multidisciplinary team ready to provide a comprehensive approach
Modern diagnostic equipment of an expert class
What can lead to a miscarriage
Losing a baby early in pregnancy can be due to a number of reasons, including:
- Hormonal imbalances leading to progesterone deficiency and excess male hormones. Prevention in this case involves taking appropriate drugs to restore hormonal balance.
- Sexually transmitted infections. Treatment by a specialist will avoid possible complications.
- Past abortions.
- Weakness of the cervix.
- Taking medications and herbal preparations that lead to the opening of the cervix.
- Heavy lifting, hitting, falling.
- Smoking, drinking alcohol.
- Chromosomal abnormalities.
Characteristic symptoms
Miscarriage may be accompanied by pain in the lower abdomen and discharge of varying intensity: from spotting to uterine bleeding.
Miscarriage is characterized by several clinical stages:
- Threatened miscarriage. Unpleasant pulling pains in the lower abdomen, slight discharge. This situation can last until childbirth.
- The onset of a miscarriage. Increased discharge, pain from aching turns into cramping, accompanied by dizziness and weakness. Taking special drugs can eliminate the problem and save the pregnancy.
- Miscarriage in action. In this case, it is pointless to hope for the salvation of the child. Sharp pains covering the entire lumbar region indicate the death of the fetal egg.
- Contraction of the uterus, after which all pain disappears and the bleeding stops.
How to behave in case of a threatened miscarriage
The first thing to do in this case is to contact a doctor who will conduct the necessary examination and, based on its results, prescribe an adequate treatment. The examination involves the implementation of a number of tests - from the study of hormonal levels to the detection of infections, susceptibility to a number of diseases.
The main recommendation that all specialists give to patients with a threatened miscarriage is complete rest, and in some cases hospitalization and adherence to the established treatment regimen.
The doctors of our clinic have extensive experience in diagnosing, preventing and treating a number of diseases of the female genital area. Appointments can be made around the clock.
You might be interested
Newspaper "Na zdorove!" obstetrics and gynecology
Gardnerella, trichomonas, chlamydia and other bacteria that cause urogenital infections, unfortunately, are still frequent intruders in the body.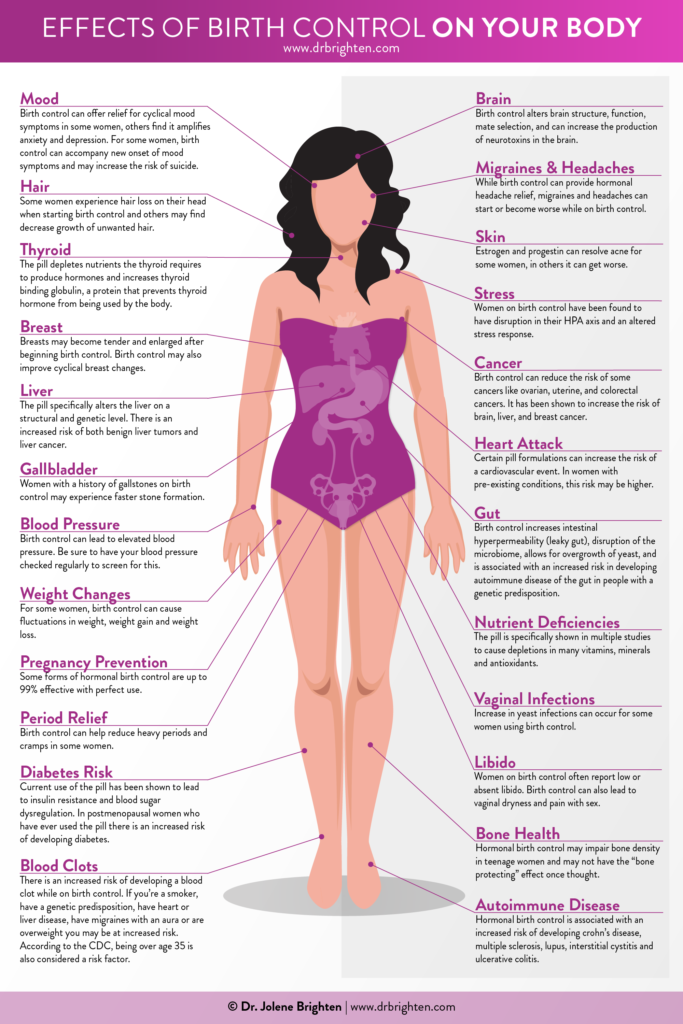 Getting rid of them is almost impossible, but taking control is easy. We talked about this with obstetrician-gynecologist Maria Viktorovna Chernisskaya.
Getting rid of them is almost impossible, but taking control is easy. We talked about this with obstetrician-gynecologist Maria Viktorovna Chernisskaya.
Gynecologists, who keep up with the times, no longer call women over 35 old-bearing, but some expectant mothers still have fears. Should women rush to have children? What does modern medicine say about this?
"Congratulations, you're pregnant!" - this phrase of the doctor is always as a starting point. What to do next? Here and for the second or third time (to say nothing about the first) there are hundreds of “why?”, “Is everything okay?” and “can I?”.
Come to the clinic in the summer - half-empty corridors and silence. But autumn comes, and again the doctors have more work to do. And, perhaps, there is no such doctor who would not have had more patients in September-October. Why do we get sick, it barely starts to get cold, and what to do in order not to mope at this time of the year, the doctors of the EMS clinic tell.
The Petersburgers have done it - survived the long dark winter and are ready to see the sun again. Increasingly, it looks into the windows and warms the streets. Is this not a reason for joy? Or is it still not? After all, as you know, what brings pleasure is often fraught with hidden threats. So it is with the sun. The doctors of the EMS clinic talk about the benefits and harms of its rays.
Perhaps there is no person who does not know what to take with a cold or headache. Everyone has their "proven means". Yes, and advertising suggests solutions for any ailment.
You can also ask for advice from friends, a pharmacist at a pharmacy or simply on the Internet. But is everything so simple and convenient? For what diseases can self-treatment be dangerous?
EMS also has a pharmacy, and our pharmacists regularly encounter requests from patients for advice on medicines, and doctors then deal with the results of self-treatment.
The EMS clinic has developed several screening programs for women's health.
In two visits to the doctor, patients can quickly and comfortably undergo an examination.
Why is this needed? We learned about this from the head of the department of obstetrics and gynecology, obstetrician-gynecologist, gynecologist-endocrinologist, ultrasound doctor Lyudmila Vladimirovna Mudragel.
Proper use of hormonal contraceptives gives a modern woman the opportunity to be realized not only in children. Head of the Department of Obstetrics
and gynecology EMS, obstetrician-gynecologist of the highest qualification category, gynecologist endocrinologist Lyudmila Vladimirovna Mudragel advises not to succumb to "hormonophobia" and use all the advantages of contraceptives, which are no less important for modern civilization than computers and the Internet.
Preparing for pregnancy is not reading forums and not measuring basal temperature. This is a set of measures that are aimed at preparing the body for conception and bearing a healthy child. Just do not turn it into work or exhausting work.