How to know if child has allergies
Allergies in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What are allergies in children?
Allergies are problems of the immune system. Most allergic reactions happen when the immune system reacts to a “false alarm.” Normally, the human body defends itself against harmful things such as viruses or bacteria. But sometimes the defenses violently attack mostly mild things, such as dust, mold, or pollen.
Normally, allergens are harmless. But when a person has allergies, the body thinks these allergens are harmful. The body then attacks allergens with antibodies called immunoglobulin E (IgE). These antibodies are attached to special cells called mast cells. Allergens stick to the antibodies. This makes the mast cells release histamine and other chemicals causing an allergic reaction. When the chemicals irritate nearby nasal tissue, this causes nasal allergy symptoms. When this happens in the lungs' breathing tubes, it can cause asthma symptoms such as cough and wheeze. When the reaction involves the whole body, this can be a severe allergic reaction.
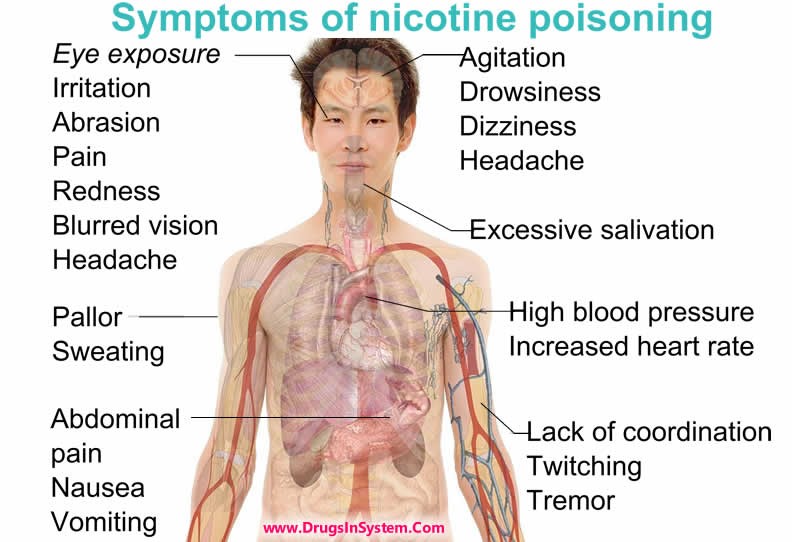
What are the symptoms of allergies in a child?
An allergic reaction can happen anywhere in the body. This includes the skin, eyes, lining of the stomach, nose, sinuses, throat, and lungs. These are the places where immune system cells are found to fight off germs that are breathed in, swallowed, or come in contact with the skin. Allergic reactions can cause:
- Stuffy nose, sneezing, itching, or runny nose, and itching in ears or roof of mouth
- Red, itchy, watery eyes
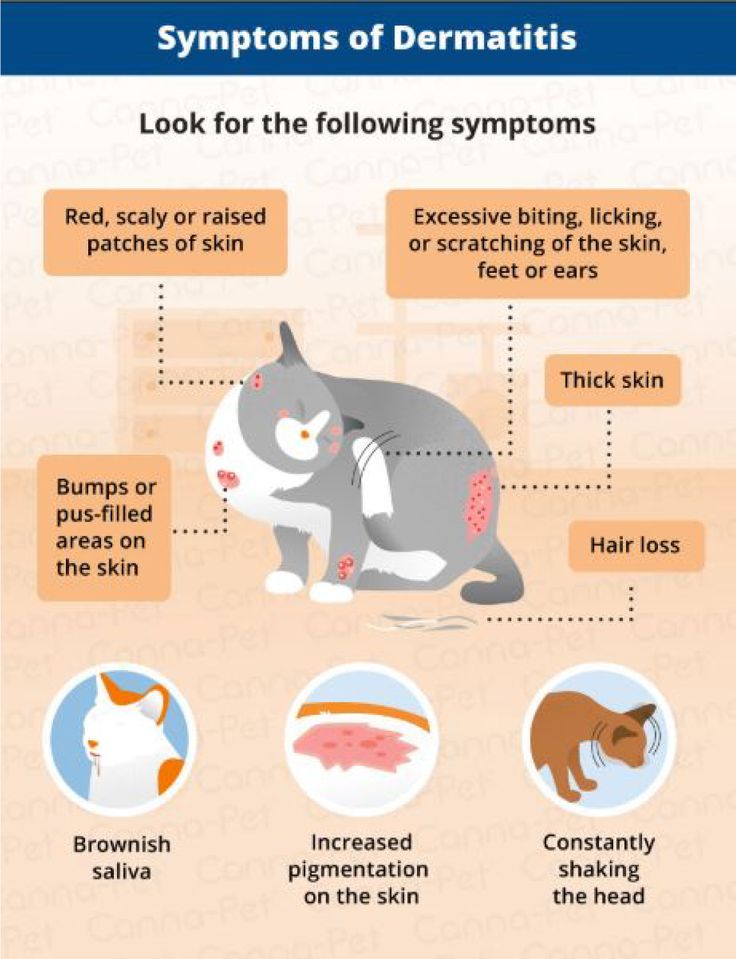
- Red, itchy, dry skin
- Hives or itchy welts
- Itchy rash
- Asthma symptoms, such as shortness of breath, coughing, wheezing
- A severe, life-threatening allergic reaction (anaphylaxis).
 This can cause trouble breathing, vomiting, diarrhea, low blood pressure, fainting, or death.
This can cause trouble breathing, vomiting, diarrhea, low blood pressure, fainting, or death.
What causes allergies in a child?
Many things can trigger allergic reactions. But the most common triggers or allergens are:
- Tree, grass, and weed pollens
- Natural rubber latex
- Molds
- Dust mites
- Animal dander, urine, and oil from skin
- Foods
- Medicines
- Feathers
- Bee stings
- Pests such as cockroaches and mice
Which children are at risk for allergies?
Allergies can affect anyone. It doesn't matter regardless of age, gender, race, or socioeconomic status. Generally, allergies are more common in children.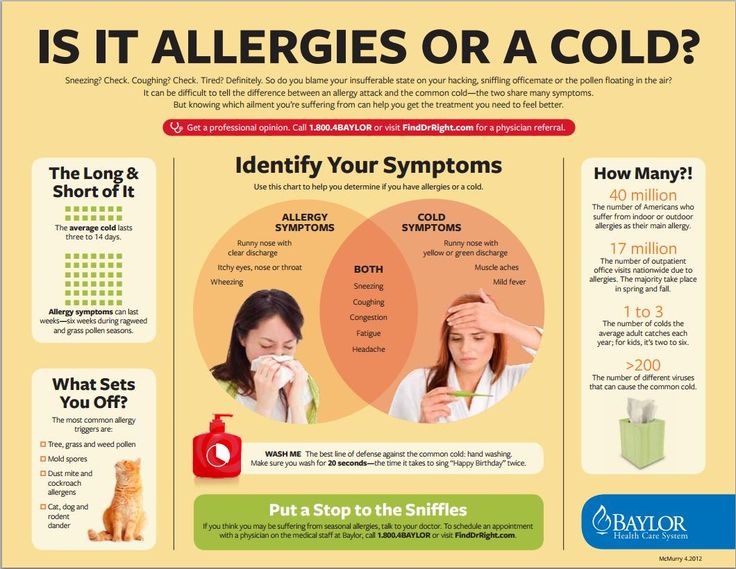 But allergies can happen at any age. And they can come back after being in remission for many years.
But allergies can happen at any age. And they can come back after being in remission for many years.
Allergies tend to happen in families. But the exact reason isn’t yet understood. Allergy symptoms often happen slowly over time.
How are allergies diagnosed in a child?
To diagnose an allergy, the healthcare provider will take a complete health history and examine your child. The provider may also do these tests:
- Skin test. This is the most common allergy test. Skin tests measure if there are IgE antibodies to certain allergens (like foods, pollens, or animal dander). A small amount of diluted allergen is placed on the skin. The area is pricked or scratched. If a person is allergic to the allergen, a small raised bump (like a mosquito bite) appears after about 15 minutes. Testing for many allergens may be done at the same time.
 An allergist may also do an intradermal test. In this test, a small amount of allergen is injected just under the skin. This type of skin testing is more sensitive than prick or scratch testing. Skin test results are available right after the testing is done.
An allergist may also do an intradermal test. In this test, a small amount of allergen is injected just under the skin. This type of skin testing is more sensitive than prick or scratch testing. Skin test results are available right after the testing is done. - Blood test. Blood tests for allergies measure IgE antibodies to certain allergens in the blood. The testing that is most often used is called RAST (radioallergosorbent test). Blood tests may be used when skin tests can't be done. For example, in people with certain skin conditions. Or people with a very recent severe allergic reaction. A positive blood test does not always mean that you have a certain allergy. Any positive blood test needs to be interpreted by a healthcare provider who is familiar with the tests and knows your child's health history.
 These tests take longer to get results. They may cost more than other allergy tests.
These tests take longer to get results. They may cost more than other allergy tests. - Challenge test. This test is supervised by an allergist. A very small amount of the allergen is given to the child by mouth. Or it is breathed in. Only a challenge test can figure out how severe an allergy is. Skin or blood test reactions only tell the likelihood of having any type of reaction, not what that reaction will be.
Any positive test needs to be explained by a healthcare provider who is familiar with the test and your child's health history.
How are allergies treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
The symptoms of allergies sometimes look like other conditions or health problems.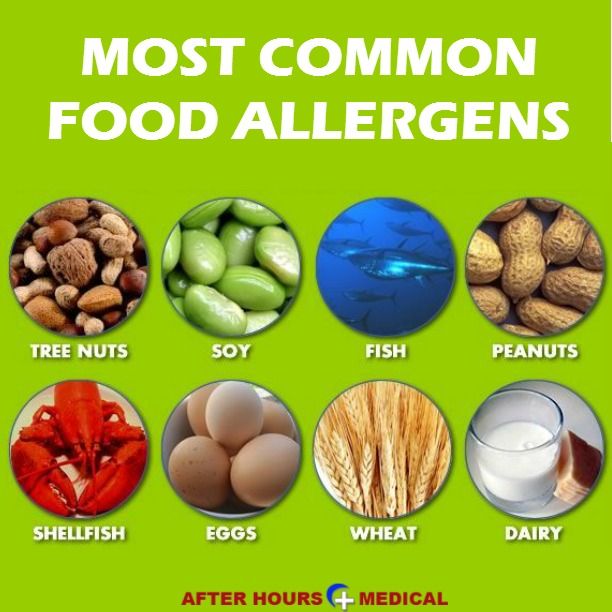 Always see your child's healthcare provider for a diagnosis.
Always see your child's healthcare provider for a diagnosis.
The 3 most effective ways to treat allergies are avoidance, allergy shots (immunotherapy), and medicine. Avoidance means staying away from something that gives you an allergic reaction.
Suggestions for staying away from allergens are:
- Stay indoors when the pollen count is high and on windy days.
- Control dust in the home, particularly your child’s bedroom.
- Use air conditioning instead of opening the windows.
- Put a dehumidifier in damp areas of the home. But remember to clean it often.
- After playing outside when the pollen counts are high, have your child take a bath or shower, wash his or her hair, and change clothes.
Take vacations in areas where pollen is not as common, such as near the ocean.
Your child’s healthcare provider will also have suggestions for staying away from the allergens that cause reactions.
Treatments for hay fever (rhinitis) may include:
- Antihistamines
- Nasal sprays
- Decongestants
- Medicines for asthma symptoms
- Allergy shots (allergy immunotherapy)
- Allergy tablets (sublingual immunotherapy)
Decongestants are not recommended for children younger than age 4. Talk with your child’s healthcare provider for more information about allergy medicine.
Key points about allergies in children
- Allergies are problems of the immune system. Most allergic reactions happen when the immune system reacts to a “false alarm.”
- Allergic reactions are often caused by tree, grass, and weed pollens, latex, molds, dust mites, foods, and medicines.

- Tests used to diagnosed allergies include skin tests, blood tests, or challenge tests.
- The 3 most effective ways to treat allergies are avoidance, allergy shots (immunotherapy), and medicine.
- Working with your child's healthcare provider or allergist can help reduce or get rid of allergies.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Children and Allergies | Symptoms & Treatment
Common Allergic Conditions in Children
Allergic
rhinitis (hay fever)Allergic rhinitis is the most common childhood ailment caused by allergies. Symptoms include a runny and itchy nose, sneezing, postnasal drip and nasal congestion (blockage). A child with allergies may also have itchy, watery, red eyes and chronic ear problems. Even though it’s commonly known as “hay fever,” allergic rhinitis isn’t triggered by hay and doesn’t cause fever.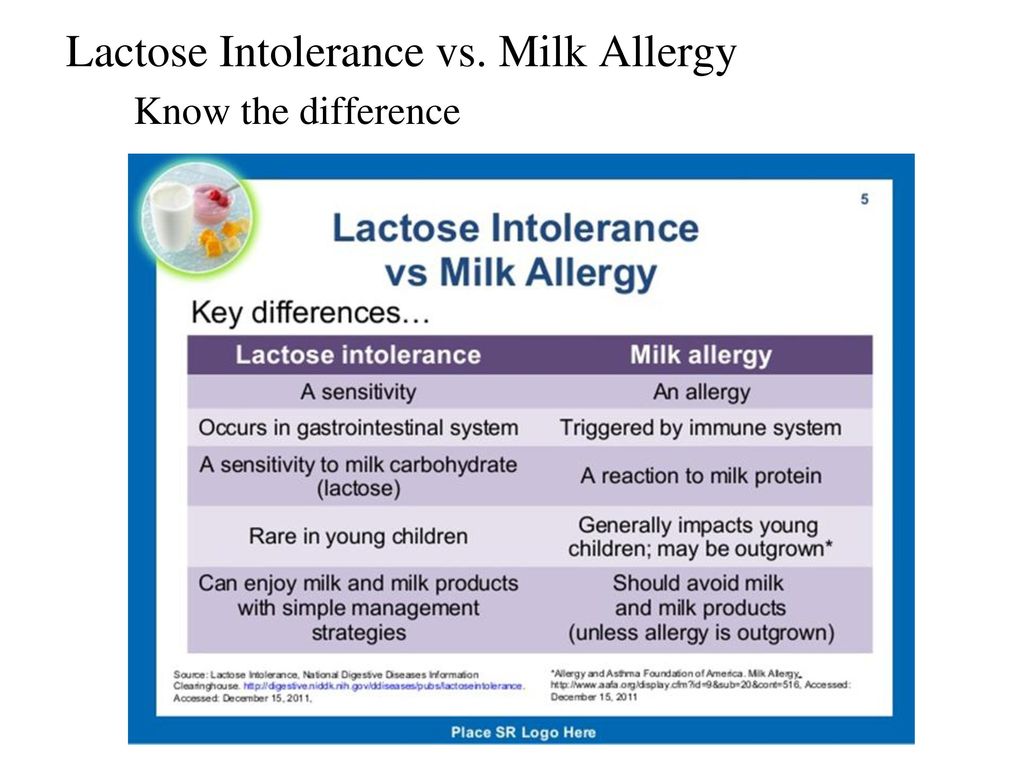
Nasal congestion
Allergies are the most common cause of chronic nasal congestion (a stuffy nose) in children. Sometimes a child’s nose is congested to the point that he or she breathes through the mouth, especially while sleeping. This may also cause the child to not get a restful night’s sleep and then be tired the next day. If the congestion and mouth-breathing are left untreated, they can affect the growth of teeth and the bones of the face. Early treatment of the allergies causing the nasal congestion may prevent these problems.
Ear infections
Allergies lead to inflammation in the ear and may cause fluid accumulation that can promote ear infections and decreased hearing. A baby whose hearing is impaired for any reason while learning to talk may develop poor speech. Allergies can cause earaches as well as ear itching, popping and fullness (“stopped-up ears”). Anyone with these symptoms should see an allergist for possible testing and treatment.
Food allergies
As many as 6 million children in the United States have some form of food allergy.
If a new mother is breast-feeding, some especially sensitive babies can have allergic reactions to foods their mothers eat. Babies can be tested for allergies. Eliminating these foods from the mother’s diet may provide relief for the child.
The most common allergies in children are to peanuts and milk; other frequently seen triggers include eggs, fish, shellfish (crab, lobster, crayfish and shrimp), soy, tree nuts (for example, pecans, cashews and walnuts) and wheat. The most severe reactions are typically to peanuts, tree nuts, fish and shellfish — all allergies that can last a lifetime. Children often outgrow allergies to milk, eggs, soy and wheat.
The most severe reactions are typically to peanuts, tree nuts, fish and shellfish — all allergies that can last a lifetime. Children often outgrow allergies to milk, eggs, soy and wheat.
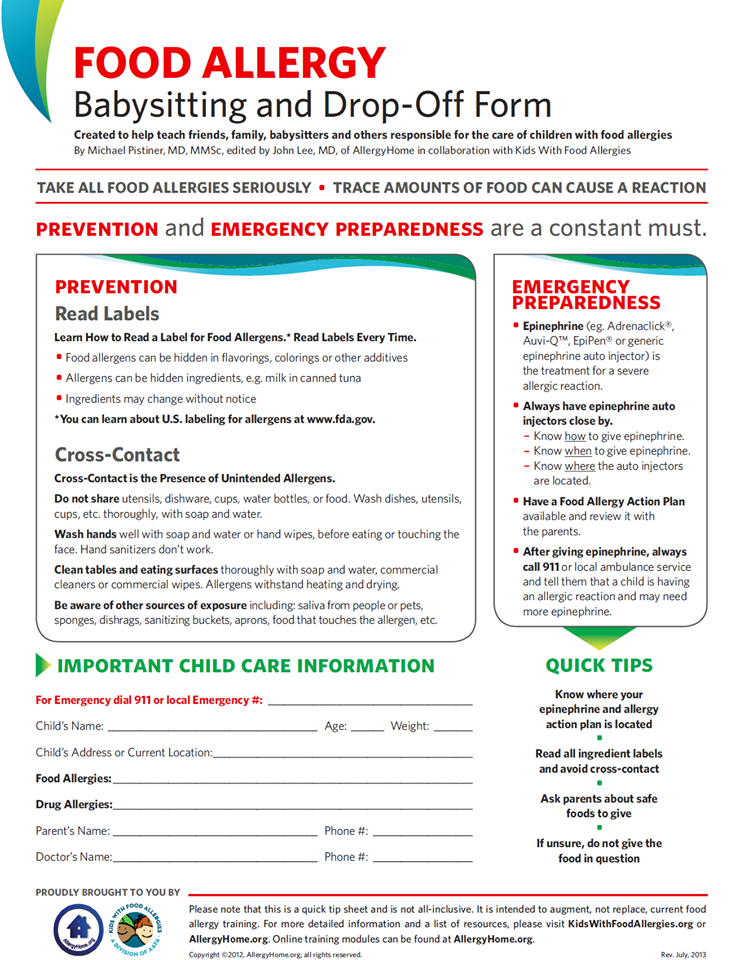
All parents of a child with a food allergy should be aware of the possibility of anaphylaxis — a potentially life-threatening reaction that impairs breathing, causes a sudden drop in blood pressure and can send a body into shock. For that reason, most children with food allergies are prescribed epinephrine (adrenaline), administered with an auto-injector as soon as symptoms develop.
Allergies and school
Your child’s school should be informed of any allergies. If your child has asthma or a severe allergy, give a copy of your child’s action plan to the school nurse or the administrative office. Also, discuss your child’s access to medication, including epinephrine (adrenaline), in case of an emergency.
- School pets: Furry animals in school may cause problems for allergic children. If your child has allergy or asthma symptoms while at school including coughing, difficulty breathing, a rash, runny nose or sneezing, it could be the class pet.
- Asthma and physical education: Physical education and sports are a big part of the school day for many children. Having asthma does not mean eliminating these activities. Children with asthma and other allergic diseases should be able to participate in any sport the child chooses, provided the doctor’s advice is followed.
 Asthma symptoms during exercise may indicate poor control, so be sure that your child is taking controller asthma medications on a regular basis. Often medication administered by an inhaler is prescribed before exercise to control symptoms.
Asthma symptoms during exercise may indicate poor control, so be sure that your child is taking controller asthma medications on a regular basis. Often medication administered by an inhaler is prescribed before exercise to control symptoms. - Dust irritation: At school, children with allergic problems may need to sit away from the blackboard to avoid irritation from chalk dust.
Do you suspect your child has an allergy? The symptoms could be a sign of a serious issue. Don’t delay: Find an allergist today.All
Allergy in an infant: who is to blame and what to do?
Allergic diseases in children are among the top problems of modern pediatrics. Allergic reactions, in addition to unpleasant external manifestations, disrupt the physical and psycho-emotional development of the child. In addition, starting in early childhood, allergies can accompany a person all his life, developing into more serious forms (the so-called "allergic march"). All these facts oblige to treat allergies as a serious problem, not to self-medicate, and if a child has alarming symptoms, immediately contact a pediatrician or an allergist.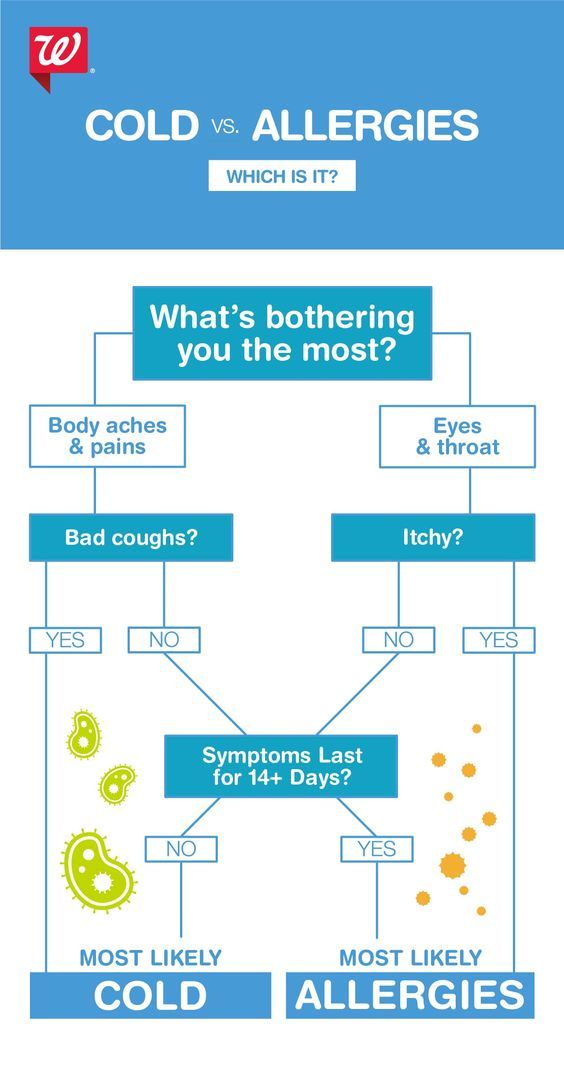
What could be the reason?
The direct cause of allergy is the contact of the child's body with the allergen. Among the most common allergens are the following:
Food
Allergies are more common in formula-fed children. Usually this is a reaction to cow's milk, which is part of an unadapted mixture. As complementary foods are introduced, a reaction to vegetable or animal protein may occur. That is why it is so important to introduce complementary foods gradually, in small portions, starting with the most “non-allergenic” foods.
Household
These are dust, animal dander, cleaning products, washing powders and other allergens found in the home.
Contact
These are various cosmetics and dyes that get on the baby's skin or come into contact with it, causing irritation (soap, cream, clothing dyes, diaper impregnations).
Medications
Taking medicines, which inexperienced parents like to practice, can cause an allergy in a child. Thus, a negative reaction of the immune system to a foreign agent is manifested. Therefore, any medicine should be given to the child strictly according to the prescription of the attending physician.
Thus, a negative reaction of the immune system to a foreign agent is manifested. Therefore, any medicine should be given to the child strictly according to the prescription of the attending physician.
In addition, there are a number of factors that increase the risk of developing allergies in babies.
First of all, it is heredity - parents suffering from certain forms of allergies can "give" this predisposition to their child. Moreover, the probability of inheriting the pathology increases if both parents have allergies.
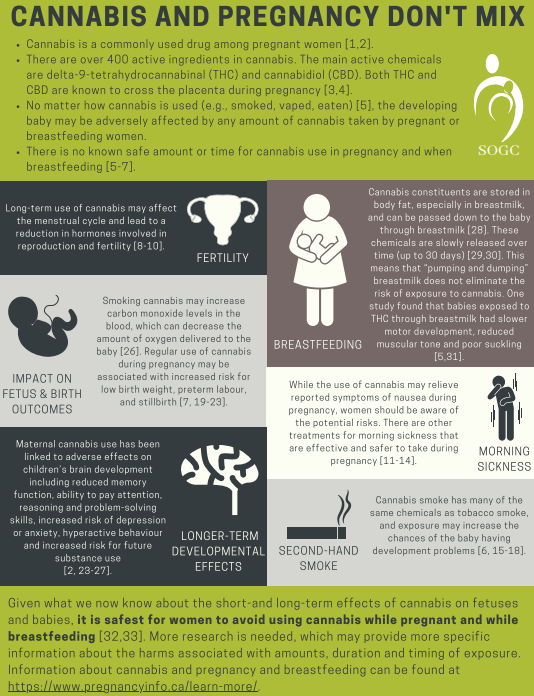
Intrauterine hypoxia, premature birth, mother's smoking at any stage of pregnancy, and even insufficiently varied diet of a pregnant woman, which does not allow the baby to get acquainted with certain foods in the womb, can become provoking factors.
Unfavorable environmental conditions can also play a negative role in the appearance of allergic reactions in a child.
Oddly enough, an excessive desire of parents to ensure sterile cleanliness in the house can provoke an allergy. It is not necessary to do this - it is important for the child to train his immune system by contacting with various microorganisms.
It is not necessary to do this - it is important for the child to train his immune system by contacting with various microorganisms.
How does an allergy manifest itself?
Most often, allergies in very young children manifest themselves in the form of a skin rash, itching, redness, dry skin, peeling, crusts on the head. Possible reactions from the gastrointestinal tract - bloating, diarrhea, severe colic, frequent regurgitation, discoloration of the stool. At the same time, the child behaves restlessly, sleeps poorly, refuses to feed, often cries.
Respiratory symptoms such as sneezing, coughing, clear nasal discharge, watery eyes and red eyes are also typical of allergies.
Fortunately, severe manifestations such as edema in the face, neck and chest, anaphylactic shock, generalized urticaria in infants are extremely rare.
How to diagnose allergies?
It is worth noting that allergies can have similar manifestations to prickly heat, parasitic or infectious diseases.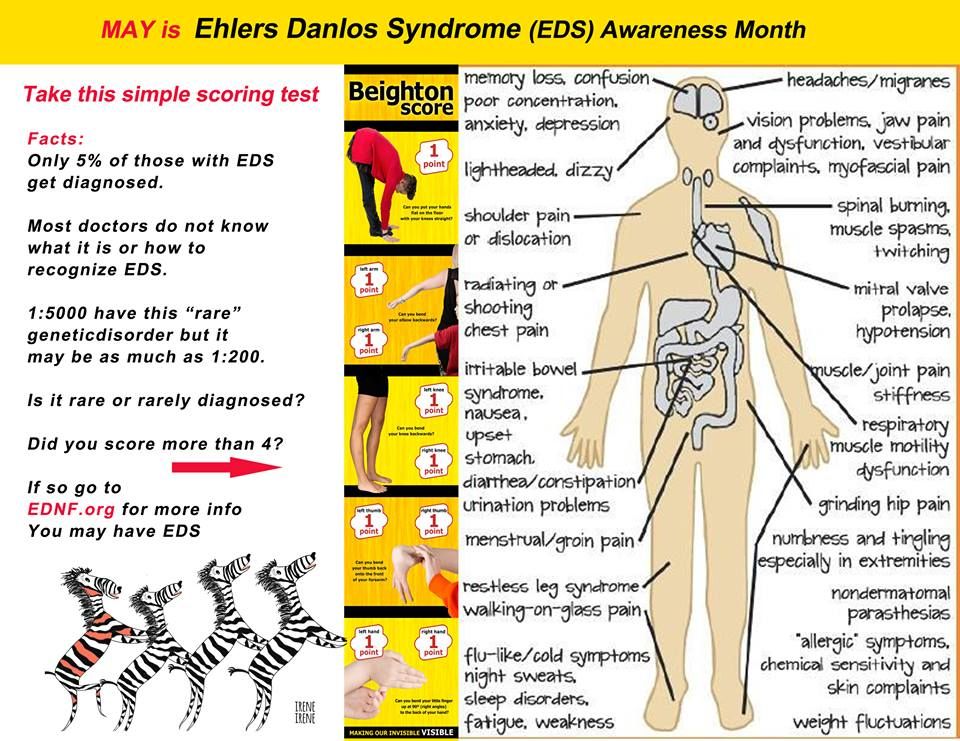 Therefore, one should not hurry with self-diagnosis, and even more so with treatment.
Therefore, one should not hurry with self-diagnosis, and even more so with treatment.
The first thing to do if you suspect an allergy is to contact a specialist. The doctor will perform an examination, prescribe a blood test for the presence of specific antibodies (skin tests are not taken from infants), and only after that will determine the treatment.
An allergen can also be identified by simple observation - to monitor how the child reacts to potential allergy triggers: dyes, powder, diapers, pets, etc. It is very effective for parents to keep a food diary, which indicates all new foods introduced as complementary foods, and the baby's reaction to them.
What to do if the diagnosis is established
The most important thing in the treatment of allergies is to eliminate provoking factors. It is important to switch to hypoallergenic cosmetics, perhaps change the manufacturer of diapers, limit contact with pets, use only baby powders for washing things.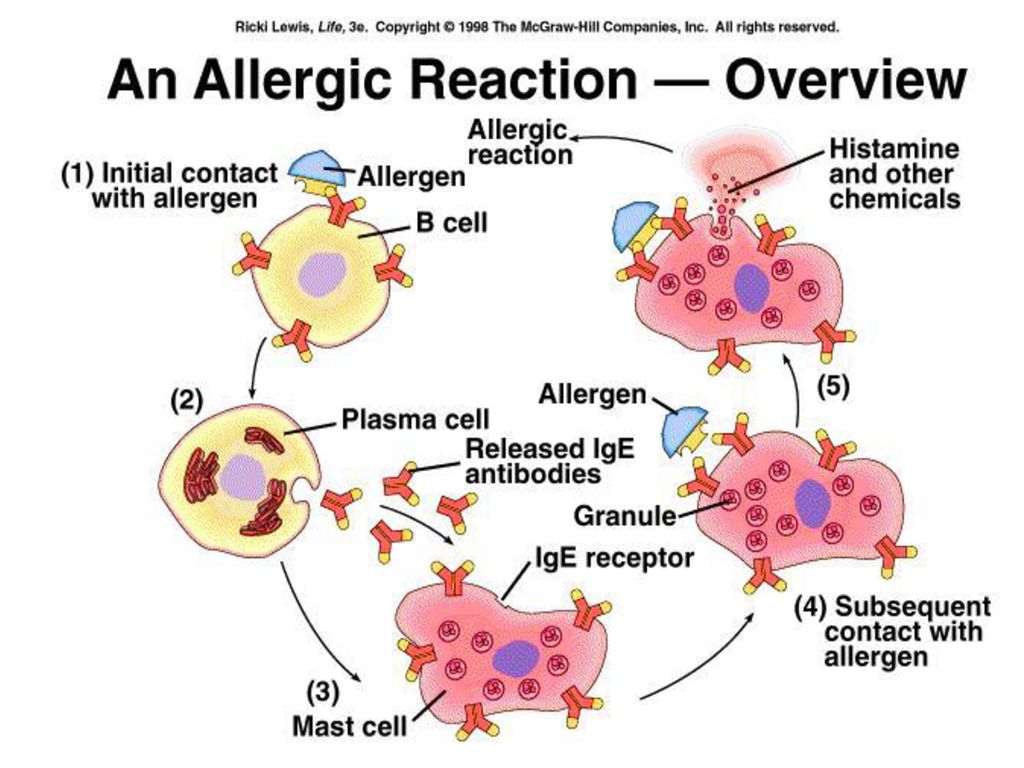
If an infant has a food allergy and is formula-fed, hypoallergenic formula milk is recommended. Complementary foods should be introduced according to the scheme approved by WHO, not earlier than the child reaches six months. And such obviously "allergic" products as citrus fruits, eggs, fish, nuts, should be introduced after two years of life.
As far as medication is concerned, it can only be prescribed by a doctor after the diagnosis has been made. Infants are prescribed antihistamines, topical anti-allergy agents with an anti-inflammatory component, as well as enzymes that help break down food, probiotics, and sorbents that bind excess allergens in the intestines.
Let's summarize. An allergy in a child is a serious pathology in which the immune system actively reacts to quite familiar substances. Only a doctor can diagnose it, and subsequently allergic children should be under special medical supervision. The main responsibility for effective treatment falls on the shoulders of parents, who need to provide full-fledged care for an allergic child, if possible, eliminating the "provocateur" of allergies from his life.
Allergy: how to find out what you are allergic to, manifestations, symptoms and diagnosis
Views: 203514 Published: / Updated:
- Allergy
General
Allergies occur when a person's immune system reacts to environmental substances that are harmless to most people. These substances are known as allergens. They are present in dust, pet hair, pollen, insects, mites, molds, foods, and some medicines.
What happens in an allergic reaction?
When a person who is allergic to a certain allergen comes into contact with it, an allergic reaction occurs. If an allergen, such as pollen, enters the body for the first time, it stimulates the production of antibodies and the formation of sensitized lymphocytes. Upon repeated contact of the pollen allergen with antibodies, antigen-antibody complexes are formed. The complexes are fixed on the surface of mast cells, causing their degranulation. As a result, histamine and other inflammatory mediators are released. Since mast cells are ubiquitous, an allergic reaction can occur in any organ. In humans, small vessels and bronchi are more often affected, so the clinic of their lesion manifests itself in the first place. Allergies come in a variety of forms: respiratory allergies (allergic rhinitis and bronchial asthma), allergic conjunctivitis, allergic dermatitis, allergic enteropathy, and the most severe and life-threatening condition - anaphylactic shock. Depending on the form, the symptoms vary widely.
The complexes are fixed on the surface of mast cells, causing their degranulation. As a result, histamine and other inflammatory mediators are released. Since mast cells are ubiquitous, an allergic reaction can occur in any organ. In humans, small vessels and bronchi are more often affected, so the clinic of their lesion manifests itself in the first place. Allergies come in a variety of forms: respiratory allergies (allergic rhinitis and bronchial asthma), allergic conjunctivitis, allergic dermatitis, allergic enteropathy, and the most severe and life-threatening condition - anaphylactic shock. Depending on the form, the symptoms vary widely.
The most typical symptoms of allergic reactions are:
- spontaneous coryza;
- frequent sneezing;
- tearing;
- rash;
- itching;
- vomiting;
- diarrhea;
- redness;
- edema;
- temperature increase.
Allergic reactions occur within 30 minutes after contact with the allergen.
The correct diagnosis can be made on the basis of the patient's history and symptoms, and can be confirmed by a special allergy test.
Seeking medical attention is especially important for children because a single primary allergy can quickly develop into multiple allergies and allergic rhinitis can cause asthma. Early diagnosis is justified by the fact that it allows for preventive treatment, minimizing the impact of allergies in the future.
History taking
The collection of anamnesis is given special attention. The presence of allergy symptoms, especially when associated with triggers described by the patient, speaks in favor of an allergic component.
Allergies often manifest themselves after ingestion of certain foods, inhalation of plant pollen, contact with animals, insect bites, taking certain medications, etc.
In patients with contact dermatitis or skin allergies, a history of contact with latex, metals, fabric fibers, detergents, etc. is significant.
is significant.
When a food allergy is detected, the patient is recommended to keep a food diary, which allows a more precise understanding of which food triggers the allergic reaction.
List of questions asked by the allergist at the appointment:
- How long does it take for a reaction to start after ingestion of a suspected food?
- Is there a consistent association of symptoms with certain foods?
- What amount of potentially allergenic food provokes symptoms?
- Does anyone else in the family who has eaten show similar symptoms?
Family history of allergies
When collecting anamnestic data, the doctor is always interested in whether one of the family members was sick or sick with allergies. The detection of first-degree relatives, such as parents and siblings, who suffer from allergies is important in the diagnosis of atopic conditions.
Atopy is a genetic (hereditary) tendency in the development of allergic diseases. People with atopy are said to be atopic.
People with atopy are said to be atopic.
The tendency to atopy is determined by both genes and environmental factors.
Allergy test
Skin tests (allergy tests) and blood tests can help determine if a person is really allergic.
Skin tests confirm the allergic nature of the disease. They are performed in the office of an allergist and allow you to quickly get an answer. Skin tests "provoke" an allergic reaction by introducing a small amount of an allergen, a substance that doctors think you may be allergic to. If there is an allergy, the skin will react, and something similar to a mosquito bite will appear at the site of the allergen.
There are three main types of skin tests: patch tests, scratch tests and prick tests.
1). Patch tests. When testing with patches, the doctor sticks test strips impregnated with the allergen. The patient should be with them for about 2 days, after which the doctor will evaluate the results at a second appointment.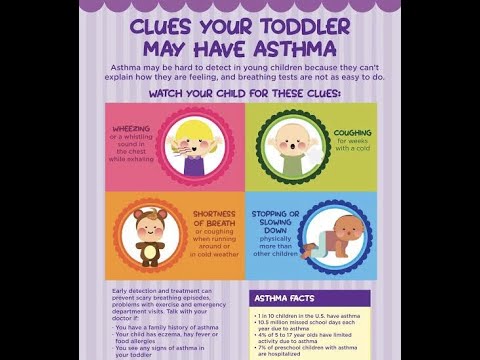 Such testing is used in the diagnosis of contact allergies.
Such testing is used in the diagnosis of contact allergies.
2). Scarification tests. Involves applying the allergen to scratches that the doctor makes with a lancet or needle. Scratches are applied to the forearm or upper back. If a reaction occurs at the site of damage to the skin - redness, scratching, etc., then this is a sure sign of an allergy. This method is the most popular in our country.
3). Prick tests. The method is similar to the previous one, only instead of scratching the skin is pierced with a thin needle. The method is easier to tolerate, but less common in our country.
In preparation for skin tests, it is important to stop taking antihistamines two weeks in advance; 7 days before their setting, stop using anti-allergic ointments.
Standard contraindications for skin testing are:
- exacerbation of chronic diseases;
- the presence of diseases in the acute stage;
- exacerbation of allergies.
Skin tests should be performed only when the child reaches 5 years of age. If there are clear indications, then they can be resorted to earlier, starting from the age of 2.
IgE blood test
In the blood, you can determine the total level of IgE and the presence of specific immunoglobulins. The general level of immunoglobulin E (IgE) in the blood indicates a tendency to allergies.
A blood test for specific IgE is used to confirm skin test results. Anti-immunoglobulin E (IgE) antibodies are substances produced by the body in response to an allergic reaction to a specific allergen. If high levels of specific IgE are detected in the blood, there is an appropriate history, then these data together help confirm the allergic nature of the disease. However, an increased result does not always indicate an allergic component. The result of the laboratory analysis should echo the clinical data and skin tests in favor of the allergy.