Pregnancy muscle pains
Body changes and discomforts | Office on Women's Health
Everyone expects pregnancy to bring an expanding waistline. But many women are surprised by the other body changes that pop up. Get the low-down on stretch marks, weight gain, heartburn and other "joys" of pregnancy. Find out what you can do to feel better.
Body aches
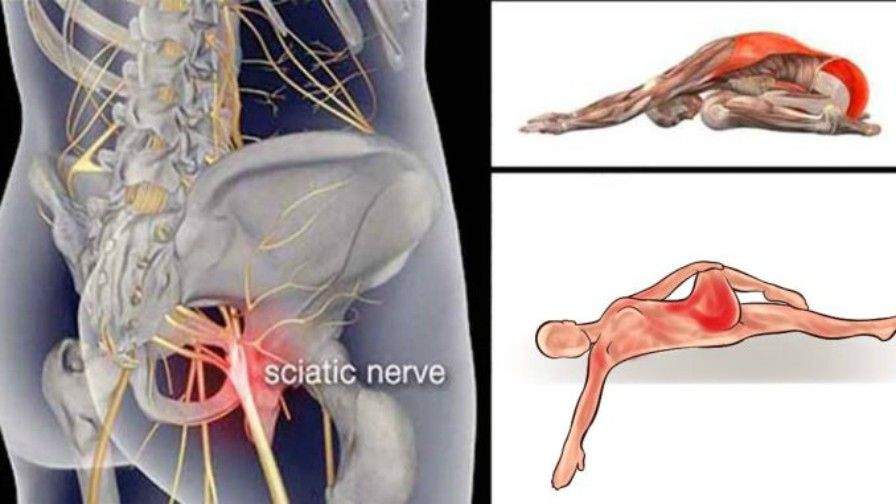
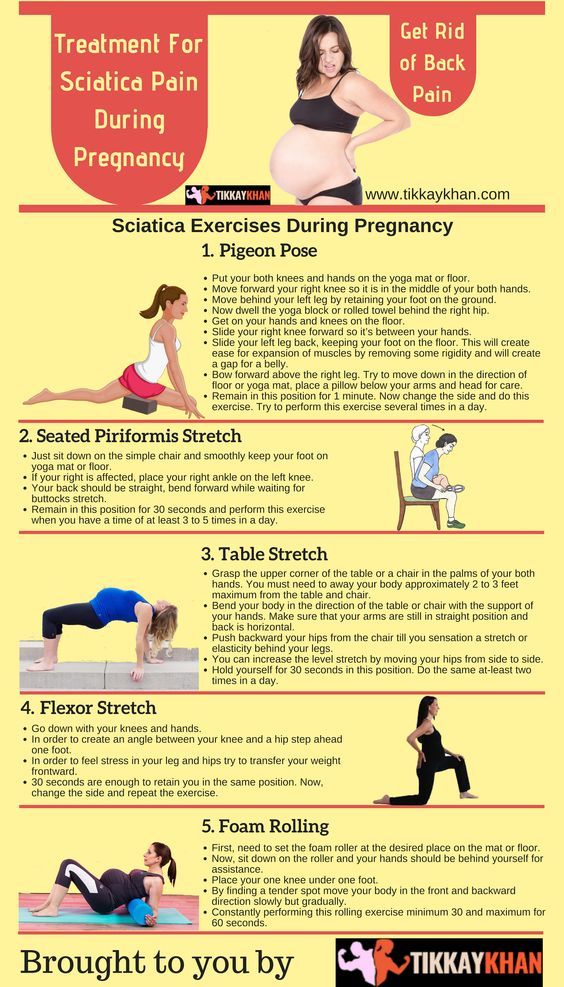
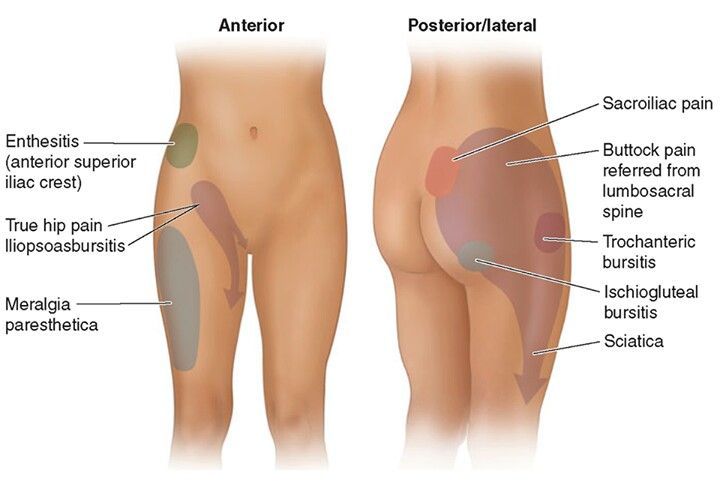
As your uterus expands, you may feel aches and pains in the back, abdomen, groin area, and thighs. Many women also have backaches and aching near the pelvic bone due the pressure of the baby's head, increased weight, and loosening joints. Some pregnant women complain of pain that runs from the lower back, down the back of one leg, to the knee or foot. This is called sciatica.(SYE-AT-ick-uh) It is thought to occur when the uterus puts pressure on the sciatic nerve.
What might help:
- Lie down.
- Rest.
- Apply heat.
Call the doctor if pain does not get better.
Breast changes
A woman's breasts increase in size and fullness during pregnancy. As the due date approaches, hormone changes will cause your breasts to get even bigger to prepare for breastfeeding. Your breasts may feel full, heavy, or tender.
In the third trimester, some pregnant women begin to leak colostrum (coh-LOSS-truhm) from their breasts. Colostrum is the first milk that your breasts produce for the baby. It is a thick, yellowish fluid containing antibodies that protect newborns from infection.
What might help:
- Wear a maternity bra with good support.
- Put pads in bra to absorb leakage.
Tell your doctor if you feel a lump or have nipple changes or discharge (that is not colostrum) or skin changes.
Constipation
Many pregnant women complain of constipation. Signs of constipation include having hard, dry stools; fewer than three bowel movements per week; and painful bowel movements.
Higher levels of hormones due to pregnancy slow down digestion and relax muscles in the bowels leaving many women constipated. Plus, the pressure of the expanding uterus on the bowels can contribute to constipation.
Plus, the pressure of the expanding uterus on the bowels can contribute to constipation.
What might help:
- Drink eight to 10 glasses of water daily.
- Don't drink caffeine.
- Eat fiber-rich foods, such as fresh or dried fruit, raw vegetables, and whole-grain cereals and breads.
- Try mild physical activity.
Tell your doctor if constipation does not go away.
Dizziness
Many pregnant women complain of dizziness and lightheadedness throughout their pregnancies. Fainting is rare but does happen even in some healthy pregnant women. There are many reasons for these symptoms. The growth of more blood vessels in early pregnancy, the pressure of the expanding uterus on blood vessels, and the body's increased need for food all can make a pregnant woman feel lightheaded and dizzy.
What might help:
- Stand up slowly.
- Avoid standing for too long.
- Don't skip meals.
- Lie on your left side.

- Wear loose clothing.
Call your doctor if you feel faint and have vaginal bleeding or abdominal pain.
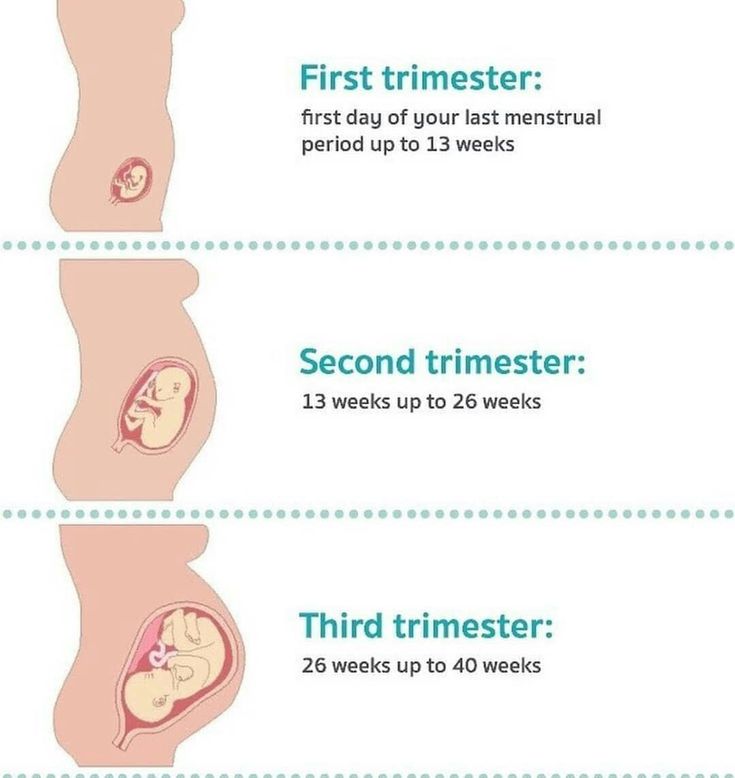
Fatigue, sleep problems
During your pregnancy, you might feel tired even after you've had a lot of sleep. Many women find they're exhausted in the first trimester. Don't worry, this is normal! This is your body's way of telling you that you need more rest. In the second trimester, tiredness is usually replaced with a feeling of well being and energy. But in the third trimester, exhaustion often sets in again. As you get larger, sleeping may become more difficult. The baby's movements, bathroom runs, and an increase in the body's metabolism might interrupt or disturb your sleep. Leg cramping can also interfere with a good night's sleep.
What might help:
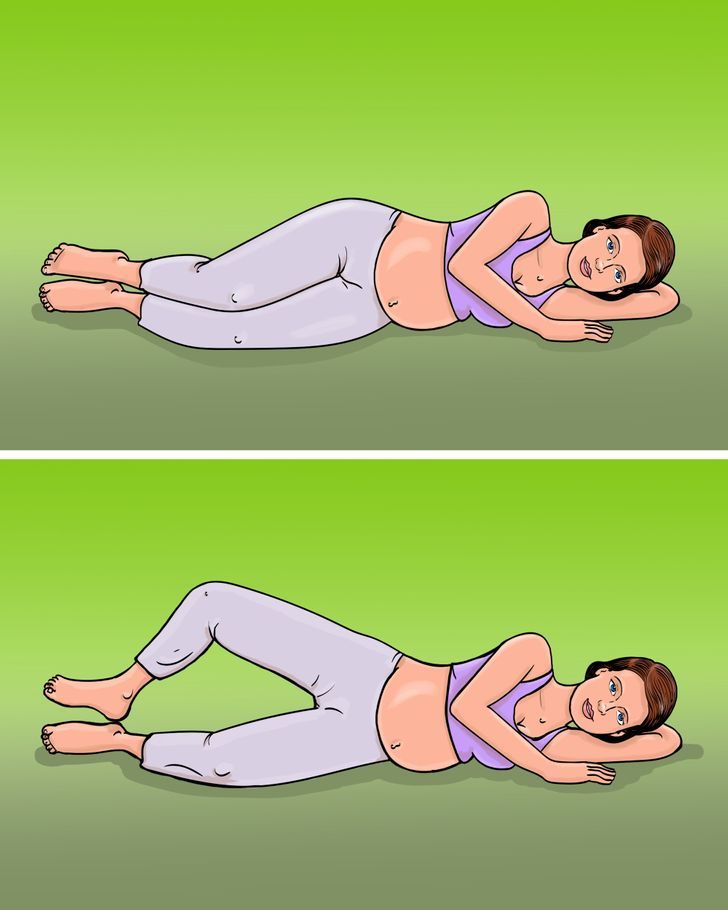
- Lie on your left side.
- Use pillows for support, such as behind your back, tucked between your knees, and under your tummy.
- Practice good sleep habits, such as going to bed and getting up at the same time each day and using your bed only for sleep and sex.
- Go to bed a little earlier.
- Nap if you are not able to get enough sleep at night.
- Drink needed fluids earlier in the day, so you can drink less in the hours before bed.
Heartburn and indigestion
Hormones and the pressure of the growing uterus cause indigestion and heartburn. Pregnancy hormones slow down the muscles of the digestive tract. So food tends to move more slowly and digestion is sluggish. This causes many pregnant women to feel bloated.
Hormones also relax the valve that separates the esophagus from the stomach. This allows food and acids to come back up from the stomach to the esophagus. The food and acid causes the burning feeling of heartburn. As your baby gets bigger, the uterus pushes on the stomach making heartburn more common in later pregnancy.
What might help:
- Eat several small meals instead of three large meals — eat slowly.
- Drink fluids between meals — not with meals.
- Don't eat greasy and fried foods.
- Avoid citrus fruits or juices and spicy foods.
- Do not eat or drink within a few hours of bedtime.
- Do not lie down right after meals.
Call your doctor if symptoms don't improve after trying these suggestions. Ask your doctor about using an antacid.
Hemorrhoids
Hemorrhoids (HEM-roidz) are swollen and bulging veins in the rectum. They can cause itching, pain, and bleeding. Up to 50 percent of pregnant women get hemorrhoids. Hemorrhoids are common during pregnancy for many reasons. During pregnancy blood volume increases greatly, which can cause veins to enlarge. The expanding uterus also puts pressure on the veins in the rectum. Plus, constipation can worsen hemorrhoids. Hemorrhoids usually improve after delivery.
What might help:
- Drink lots of fluids.
- Eat fiber-rich foods, like whole grains, raw or cooked leafy green vegetables, and fruits.
- Try not to strain with bowel movements.

- Talk to your doctor about using products such as witch hazel to soothe hemorrhoids.
Itching
About 20 percent of pregnant women feel itchy during pregnancy. Usually women feel itchy in the abdomen. But red, itchy palms and soles of the feet are also common complaints. Pregnancy hormones and stretching skin are probably to blame for most of your discomfort. Usually the itchy feeling goes away after delivery.
What might help:
- Use gentle soaps and moisturizing creams.
- Avoid hot showers and baths.
- Avoid itchy fabrics.
Call your doctor if symptoms don't improve after a week of self-care.
Leg cramps
At different times during your pregnancy, you might have sudden muscle spasms in your legs or feet. They usually occur at night. This is due to a change in the way your body processes calcium.
What might help:
- Gently stretch muscles.
- Get mild exercise.

- For sudden cramps, flex your foot forward.
- Eat calcium-rich foods.
- Ask your doctor about calcium supplements.
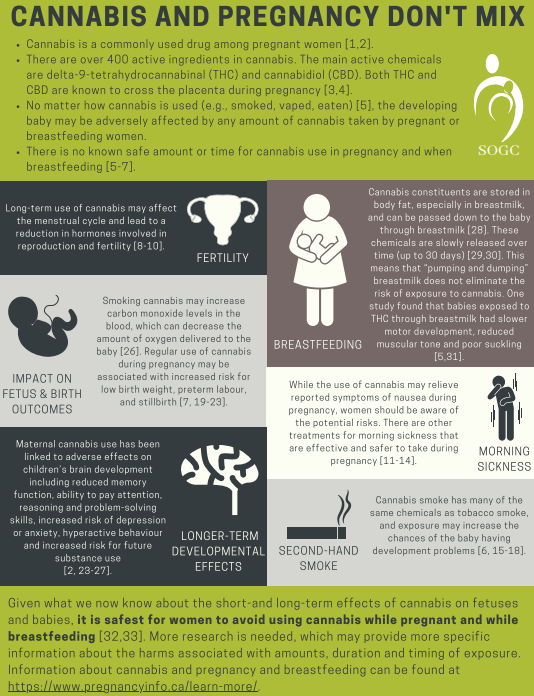
Morning sickness
In the first trimester hormone changes can cause nausea and vomiting. This is called "morning sickness," although it can occur at any time of day. Morning sickness usually tapers off by the second trimester.
What might help:
- Eat several small meals instead of three large meals to keep your stomach from being empty.
- Don't lie down after meals.
- Eat dry toast, saltines, or dry cereals before getting out of bed in the morning.
- Eat bland foods that are low in fat and easy to digest, such as cereal, rice, and bananas.
- Sip on water, weak tea, or clear soft drinks. Or eat ice chips.
- Avoid smells that upset your stomach.
Call your doctor if you have flu-like symptoms, which may signal a more serious condition.
Call your doctor if you have severe, constant nausea and/or vomiting several times every day.
Nasal problems
Nosebleeds and nasal stuffiness are common during pregnancy. They are caused by the increased amount of blood in your body and hormones acting on the tissues of your nose.
What might help:
- Blow your nose gently.
- Drink fluids and use a cool mist humidifier.
- To stop a nosebleed, squeeze your nose between your thumb and forefinger for a few minutes.
Call your doctor if nosebleeds are frequent and do not stop after a few minutes.
Numb or tingling hands
Feelings of swelling, tingling, and numbness in fingers and hands, called carpal tunnel syndrome, can occur during pregnancy. These symptoms are due to swelling of tissues in the narrow passages in your wrists, and they should disappear after delivery.
What might help:
- Take frequent breaks to rest hands.
- Ask your doctor about fitting you for a splint to keep wrists straight.
Stretch marks, skin changes
Stretch marks are red, pink, or brown streaks on the skin. Most often they appear on the thighs, buttocks, abdomen, and breasts. These scars are caused by the stretching of the skin, and usually appear in the second half of pregnancy.
Most often they appear on the thighs, buttocks, abdomen, and breasts. These scars are caused by the stretching of the skin, and usually appear in the second half of pregnancy.
Some women notice other skin changes during pregnancy. For many women, the nipples become darker and browner during pregnancy. Many pregnant women also develop a dark line (called the linea nigra) on the skin that runs from the belly button down to the pubic hairline. Patches of darker skin usually over the cheeks, forehead, nose, or upper lip also are common. Patches often match on both sides of the face. These spots are called melasma or chloasma and are more common in darker-skinned women.
What might help:
- Be patient — stretch marks and other changes usually fade after delivery.
Swelling
Many women develop mild swelling in the face, hands, or ankles at some point in their pregnancies. As the due date approaches, swelling often becomes more noticeable.
What might help:
- Drink eight to 10 glasses of fluids daily.
- Don't drink caffeine or eat salty foods.
- Rest and elevate your feet.
- Ask your doctor about support hose.
Call your doctor if your hands or feet swell suddenly or you rapidly gain weight — it may be preeclampsia.
Urinary frequency and leaking
Temporary bladder control problems are common in pregnancy. Your unborn baby pushes down on the bladder, urethra, and pelvic floor muscles. This pressure can lead to more frequent need to urinate, as well as leaking of urine when sneezing, coughing, or laughing.
What might help:
- Take frequent bathroom breaks.
- Drink plenty of fluids to avoid dehydration.
- Do Kegel exercises to tone pelvic muscles.
Call your doctor if you experience burning along with frequency of urination — it may be an infection.
Varicose veins
During pregnancy, blood volume increases greatly. This can cause veins to enlarge. Plus, pressure on the large veins behind the uterus causes the blood to slow in its return to the heart. For these reasons, varicose veins in the legs and anus (hemorrhoids) are more common in pregnancy.
This can cause veins to enlarge. Plus, pressure on the large veins behind the uterus causes the blood to slow in its return to the heart. For these reasons, varicose veins in the legs and anus (hemorrhoids) are more common in pregnancy.
Varicose veins look like swollen veins raised above the surface of the skin. They can be twisted or bulging and are dark purple or blue in color. They are found most often on the backs of the calves or on the inside of the leg.
What might help:
- Avoid tight knee-highs.
- Sit with your legs and feet raised.
More information on body changes and discomforts
Explore other publications and websites
- First Trimester Pregnancy: What to Expect (Copyright © Mayo Foundation) - This fact sheet discusses the physical changes and symptoms experienced in the first three months of pregnancy.
- Second Trimester Pregnancy: What to Expect (Copyright © Mayo Foundation) - This fact sheet discusses how the changes that began in the first weeks of pregnancy increase and accelerate during the second trimester.
 Of these, your growing uterus is probably the most obvious. But many other, unseen events are also taking place.
Of these, your growing uterus is probably the most obvious. But many other, unseen events are also taking place.
Connect with other organizations
- American Academy of Family Physicians
- American College of Nurse-Midwives
- American College of Obstetricians and Gynecologists
- Center for Research on Reproduction and Women's Health, University of Pennsylvania Medical Center
- Hyperemesis Education and Research Foundation
- March of Dimes
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
Body aches during pregnancy | BabyCenter
As your body changes during pregnancy, you'll feel new aches and pains. Body aches in early pregnancy may be due to hormonal changes. As pregnancy progresses, physical changes can lead to back pain, pelvic pain, round ligament pain, and sciatica. Applying heat or cold and staying physically active can help soothe and prevent pregnancy aches and pains – but sometimes they indicate a more serious issue.
As pregnancy progresses, physical changes can lead to back pain, pelvic pain, round ligament pain, and sciatica. Applying heat or cold and staying physically active can help soothe and prevent pregnancy aches and pains – but sometimes they indicate a more serious issue.
Is pregnancy a literal pain in your back (and just about everywhere else)? Growing a brand-new person is hard work – and it can take a toll on your body, starting in the first weeks of pregnancy.
Here's how to get relief from your pregnancy aches and pains, as well as advice about when it's time to ask your healthcare provider for help.
What causes body aches in pregnancy?
Throughout your pregnancy, hormones relax your ligaments and joints to prepare your body for birth, which may result in body aches and pains.
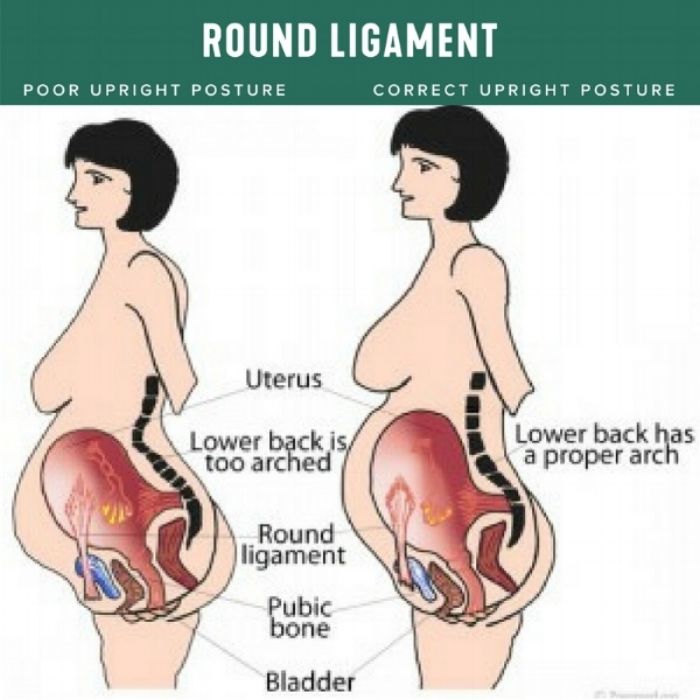
As pregnancy progresses – particularly from the second trimester on – you'll gain weight, which puts extra pressure on your joints. In addition, your growing belly pulls your center of gravity forward and stretches and weakens your abdominal muscles, which support your spine and back.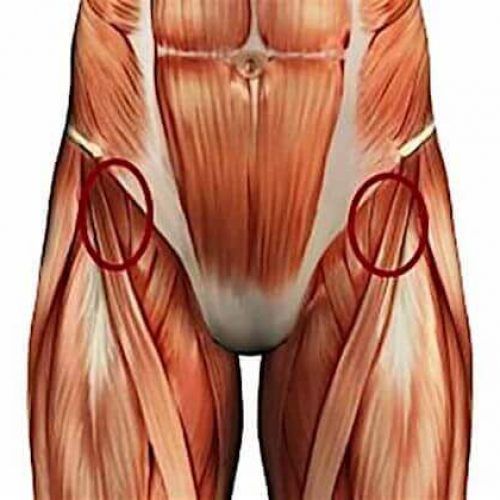 As your body adjusts to these changes, it's very common to feel lower back pain, as well as pain in your pelvis, groin, legs, and buttocks.
As your body adjusts to these changes, it's very common to feel lower back pain, as well as pain in your pelvis, groin, legs, and buttocks.
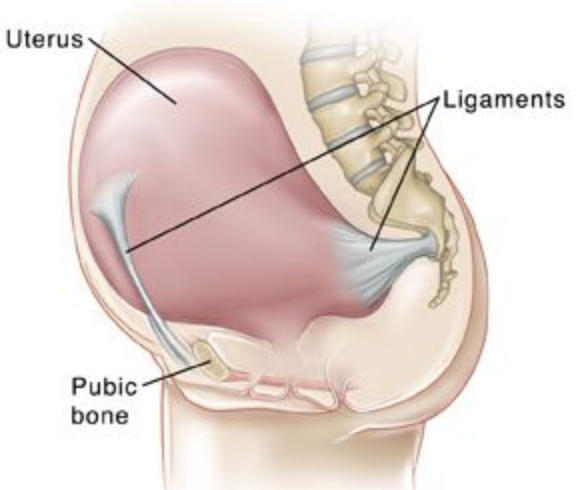
In addition, beginning in the second trimester you may experience what's known as round ligament pain: a brief, sharp, stabbing pain or a longer-lasting dull ache in your lower belly or groin. This generally harmless condition happens when the attachments between your growing uterus and abdominal wall (The "round ligaments") are pulled or stretched.
You may also experience sciatica as pressure from the weight of your baby and uterus presses on your sciatic nerve, sending shooting pain from your buttocks down the back of your leg.
Is it normal to have body aches in early pregnancy?
Yes. You may experience early pregnancy body aches and muscle pains all over due to hormonal changes, especially toward the end of the first trimester.
Pelvic pain (technically known as pelvic girdle pain) and lower back pain are the most frequent complaints.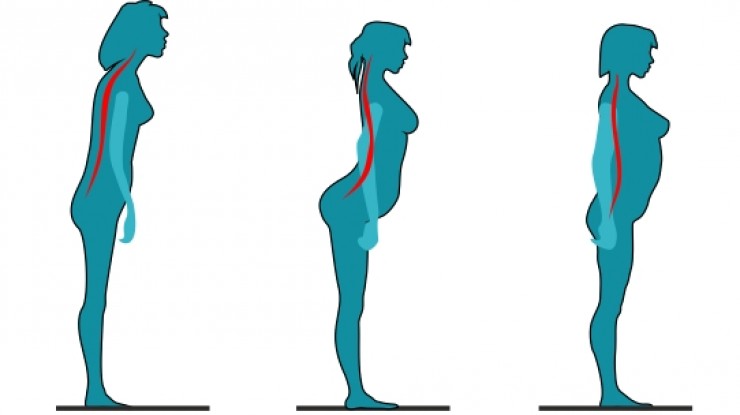 These discomforts can pop up at any point in pregnancy, although they're more common beginning in week 14 (the start of the second trimester).
These discomforts can pop up at any point in pregnancy, although they're more common beginning in week 14 (the start of the second trimester).
You may also experience mild uterine cramping in early pregnancy, similar to period pains, as your uterus begins to expand in size. You could also have stomach pains due to constipation or gas, both of which are common during pregnancy. Digestive problems are also linked to hormonal changes and start early in pregnancy.
Advertisement | page continues below
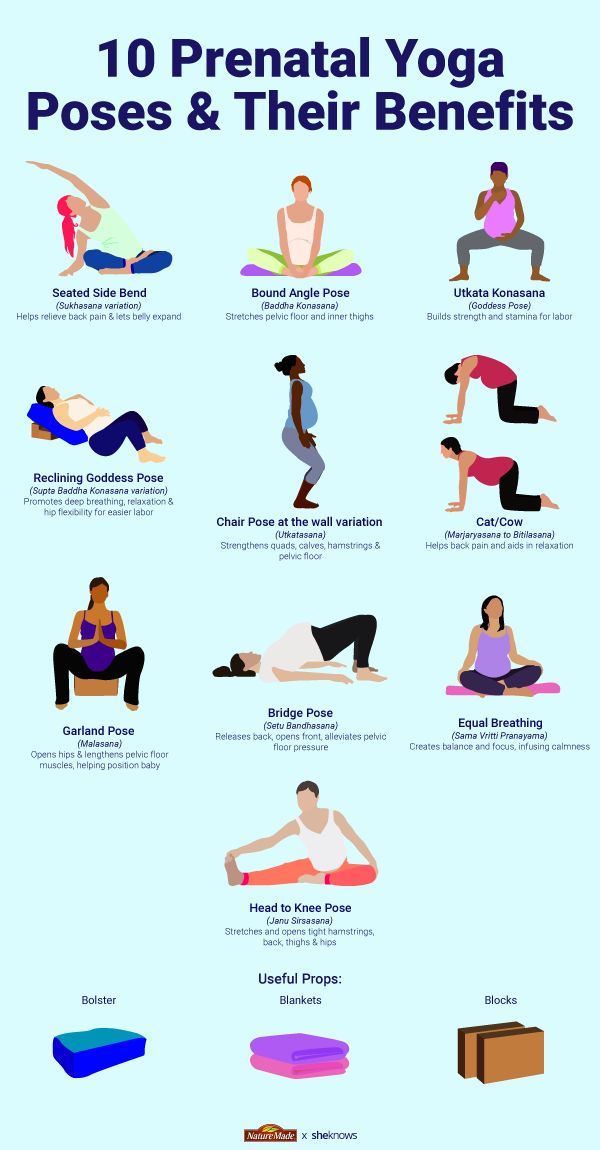
Relieving body aches in pregnancy
To relieve sore muscles and body aches in pregnancy, lie down, relax, and apply heat and/or cold to the affected areas. A cold pack can reduce inflammation and help to soothe muscle and back pain.
To apply heat, you can use an electric heating pad, hot water bottle, or microwaveable pad filled with flax or buckwheat. Don't apply heat to your abdomen for longer than ten minutes. You don't want to raise your internal temperature too much, as this can affect your developing baby.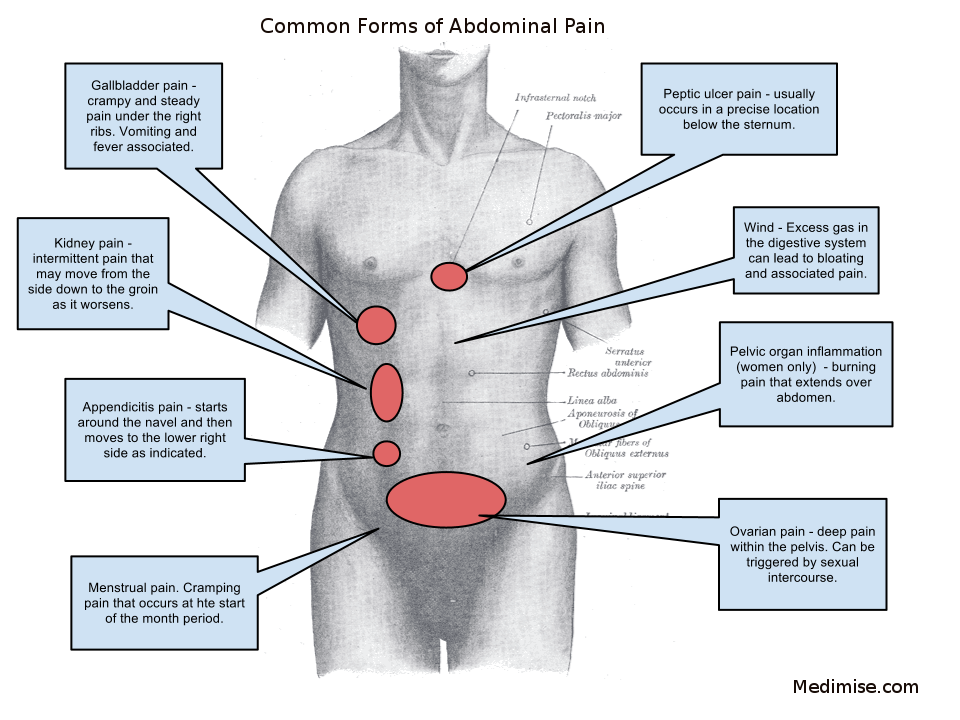
One of the best strategies to prevent and treat body aches in pregnancy is to stay physically active. While it may seem counterintuitive, exercise helps relieve all sorts of common pregnancy complaints, from back pain to constipation and gas. Pregnancy-safe exercise helps to keep pregnancy weight gain in check, strengthens and stretches your muscles, improves your posture, and supports your circulation.
To relieve back and pelvic pain specifically, sit in a supportive chair, sit down when getting dressed, use proper form to lift heavier objects, and try to avoid standing for long periods of time if possible.
If these tips don't help, talk to your provider about whether to take a pregnancy-safe pain reliever (usually acetaminophen). You can also ask your ob-gyn or midwife for a referral to a physical therapist. Working with a physical therapist can help to relieve your pain and increase your strength as pregnancy progresses.
When to call your doctor or midwife
Sometimes, certain body aches and pains in pregnancy can be a sign of something more serious. Severe back pain may be a sign of a kidney infection; it's often accompanied by fever and a burning sensation when you urinate. Rarely, abdominal pain and cramping in the first trimester of pregnancy may be caused by ectopic pregnancy or miscarriage.
Severe back pain may be a sign of a kidney infection; it's often accompanied by fever and a burning sensation when you urinate. Rarely, abdominal pain and cramping in the first trimester of pregnancy may be caused by ectopic pregnancy or miscarriage.
Generalized body aches along with fevers and/or upper respiratory symptoms can also be caused by flu or COVID-19. Pregnant women are more susceptible to complications with both of these infections.
Call your provider if body aches don't improve with the simple treatments above, or if you have:
- Severe and constant abdominal pain, especially if it doesn't go away within an hour given rest
- Vaginal bleeding or spotting
- Fever
- Unusual vaginal discharge
- Pain or burning when you pee
Common body aches in pregnancy
In addition to general body aches and muscle pain in pregnancy – especially in the back and pelvis – you may experience these other discomforts:
Headaches
Feeling a squeezing pain or a steady dull ache on both sides of your head could signal a tension headache. This usually harmless pregnancy symptom is especially common during the first trimester, linked to hormonal changes and increased blood flow. (If you're in your second or third trimester and have a severe headache that won't go away, call your healthcare provider just to be safe.)
This usually harmless pregnancy symptom is especially common during the first trimester, linked to hormonal changes and increased blood flow. (If you're in your second or third trimester and have a severe headache that won't go away, call your healthcare provider just to be safe.)
Find out more about headaches during pregnancy.
Hemorrhoids
Hemorrhoids are unusually swollen blood vessels in the rectal area that are usually linked to constipation and straining during bowel movements. They can be merely itchy or downright painful and can sometimes cause rectal bleeding, especially during a bowel movement. Some women get hemorrhoids for the first time while they're pregnant, but if you've had them before you got pregnant, you're very likely to have them again now.
Find out more about hemorrhoids during pregnancy.
Heartburn
If you feel a burning sensation in your chest after you eat, it's probably heartburn (also called acid indigestion or acid reflux).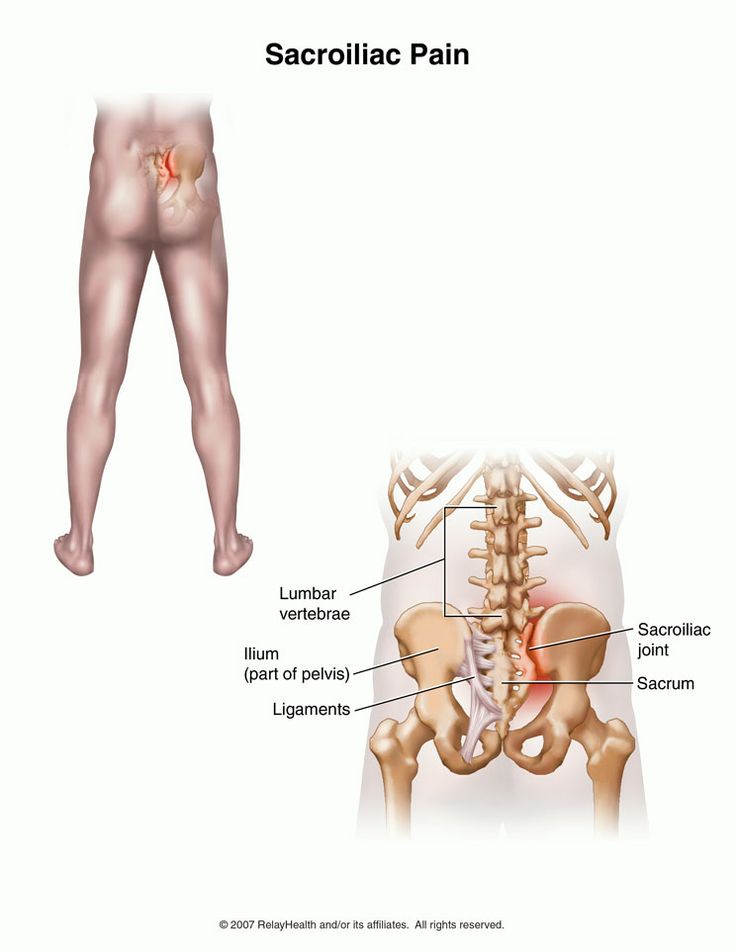 During pregnancy, hormones relax the lower esophageal sphincter, allowing stomach acid to climb back up and burn the esophagus. Later in pregnancy, your growing baby pushes up on the stomach and its contents, adding to the burn.
During pregnancy, hormones relax the lower esophageal sphincter, allowing stomach acid to climb back up and burn the esophagus. Later in pregnancy, your growing baby pushes up on the stomach and its contents, adding to the burn.
Find out more about heartburn during pregnancy.
Leg cramps
No one's really sure why spasms in the leg muscles are common during the second and third trimesters, but they could be from vitamin deficiencies, electrolyte imbalances, or changes in your activity level, among other reasons.
Find out more about leg cramps during pregnancy.
Carpal tunnel syndrome
If you feel tingling or numbness in your hands during pregnancy, it could be carpal tunnel syndrome. Extra fluid and swelling during pregnancy can press on the nerves that pass from the hand through the wrist to the forearm, causing these symptoms.
Find out more about carpal tunnel syndrome during pregnancy.
Muscle pain during pregnancy
Norm or pathology - muscle pain during pregnancy
Muscle pain during pregnancy is considered an inevitable phenomenon associated with natural processes, changes in the functioning of many organs and systems.
Literally from the first week of conception, the smooth muscles that line the hollow organs (uterus), striated muscles, the vascular and hormonal systems begin to “prepare” for childbirth. Such a general transformation of the body of the expectant mother really provokes discomfort of varying degrees of intensity, especially if the woman before pregnancy did not bother herself with sports, strengthening muscle fibers, and maintaining physical fitness. In this case, the contractile property of the muscles is initially reduced, and the activation of the function of muscle tissue provokes a pain symptom due to chronic hypertonicity, overstrain.
Causes of muscle pain during pregnancy
Pregnancy, in addition to bringing joyful expectation, sometimes causes quite understandable discomfort and even pain. Most often, pain is concentrated in muscle tissue and ligaments, since it is they who are subjected to increased stress, sprains.
The causes of muscle pain during pregnancy can be both physiological and pathological.
- Physiological causes of muscle pain in pregnant women.
- The woman's body becomes like a "double" - two hearts beat in it, her own and the heart of the fetus, respectively, an additional circle of blood flow appears.
- The heart muscle of a pregnant woman experiences an increased load and increases in size.
- The volume of blood flow increases to 6-7 liters.
- The body of a pregnant woman needs a double volume of oxygen for normal tissue nutrition, including muscle tissue.
- The spine and surrounding muscles are subjected to a special load, the weight of a pregnant woman can increase by 10-20 kilograms.
- 70-75% of women experience pain symptoms of varying intensity in the back due to temporary dysfunction of the spine.
- An increase in the size of the uterus inevitably entails a shift in the center of balance, gravity, respectively, the muscles of the lower back and pelvis are subjected to increased stress.

- The posture and gait of a woman changes, the muscles of the shoulder girdle, cervical, thoracic region have to work in hypertonicity mode.
- An increase in body weight leads to a violation of venous blood flow, respectively, leg muscles hurt.
- Overeating or vice versa, lack of nutrients due to nausea and vomiting caused by toxicosis, can disrupt the vitamin-mineral balance, respectively, the muscle tissue does not receive proper nutrition, myalgia develops.
- Pathological causes of muscle pain during pregnancy:
- Disease of the cardiovascular system, reduced blood supply to muscle tissue.
- Atherosclerotic changes in the vascular system.
- Inflammatory processes in muscles, fascia, joints caused by infections.
- Neurological conditions associated with osteochondrosis of the spinal column.
- History of fibromyalgia.
- Local muscle injury (ossifying process).
- Nephropathology (pyelonephritis).
- Infectious pathologies, most often genital herpes.
- Inguinal hernia, umbilical hernia.
- Varicose veins, including vaginal varicose veins.
Before proceeding to the enumeration of the reasons, here are some statistics:
In what areas can muscle pain occur during pregnancy?
- The most susceptible to changes are the muscles of the abdominal region - the rectus abdominis muscles. Before pregnancy, these skeletal muscles performed the function of maintaining an elastic press, forming it. After conception, the rectus muscles must perform a completely different task - to support the growing uterus. Atonic, untrained abdominal muscles are at risk of painful sprains, resulting in pain.
- Muscles of the pelvis, which not only support the uterus and other organs in their proper places, but are also directly involved in the process of labor.
- The muscles of the back may hurt due to an atypical shift in the center of gravity, excessive load on the growing body. The atonic muscle corset is not able to cope with the additional load, the muscles are stretched, inflamed, the woman feels back pain.
- Muscles of the legs that can hurt from the first trimester. The most typical cramps of the calf muscles during pregnancy, such a symptom most often develops in the initial phase of sleep, or at night, less often in the morning.
- Breast muscles, which are influenced by changes in hormonal balance, increase due to increased blood circulation, activated lymph flow.
- Inguinal muscles can hurt for various reasons, but most often the pain symptom is due to physical overstrain or the effect of a specific hormone relaxin on the ligamentous apparatus. A pain symptom in the groin may not touch the muscle tissue, but the sensations are reflected precisely in the muscles, this happens with nephropathologies, diseases of the digestive tract, and even with constipation. Also, pain in the muscles of the groin during pregnancy can be caused by many non-physiological causes - varicose veins of the pubic joint, infectious diseases of the pelvic organs, and others.
- During pregnancy, the muscles of the vagina experience an increased vascular load, venous hemodynamics change, the elasticity of muscle tissue decreases, and pain appears.
- Statistics say that 70-75% of pregnant women experience pain in the lumbar region, the muscles of which are subject to increased stress due to increased body weight and physiological displacement of internal organs
It should be noted that during pregnancy, not all types of muscles spasm, there are those that, on the contrary, relax. Relaxation of smooth muscles, on the one hand, allows the delivery of oxygen and nutrients to the placenta, on the other hand, it can cause reflex radiating pain from excessively atonic organs (gall bladder, stomach, intestines).
Summarizing, we can say that the body of the expectant mother sometimes experiences an overwhelming load, comparable, according to experts, only with the intensity of the training of astronauts. Accordingly, a woman periodically feels pain symptoms, most often localized in the back, pelvic region, abdomen and legs.
Why do muscles hurt during pregnancy
Why does a pregnant woman experience muscle pain? The simplest answer is this - due to systemic physiological changes in the body. The stages and types of transformation can be described as follows:
The stages and types of transformation can be described as follows:
- Hormonal changes in the body.
- Progesterone and estrogen levels change, increased secretion of relaxin begins. Progesterone is needed to increase the tone of both the smooth muscles of the uterus and other muscle tissue, the production of progesterone in the first trimester is especially important so that the conception really goes into pregnancy and becomes fixed. In addition to influencing the state of the uterus, progesterone stimulates breast development, the muscles of the mammary glands soften, and the glands increase. In addition to the clearly beneficial effect on the body, progesterone inhibits the activity of the immune system so that it does not reject the embryo (fetus) that has invaded the uterus in the process of “recognition”. Thus, reduced immune protection is a potential risk of infectious, bacterial infections, diseases, often accompanied by muscle pain. Also, progesterone can contribute to the retention of salt and fluid in the body, which in turn disrupts the rate of normal blood circulation, venous outflow and provokes pain of a different nature, including myalgia.

- An increased level of estrogen performs the task of activating the growth of the uterus, if there is too much estrogen, it works like diuretin, sometimes too actively. As a result, a violation of the water-salt, electrolyte balance develops and muscle pain appears
- Chorionic gonadotropin and somatomammotropin do not provoke myalgia by themselves, but they accelerate all metabolic processes, and somewhat increase the muscle mass of the chest, less often than other body parts (buttocks, feet).
- Diseases of the organs and blood supply systems of the small pelvis in history can also be the answer to the question - why do muscles hurt during pregnancy. Among them, the following are common and most often diagnosed:
- Ovarian cyst.
- Uterine fibroids.
- Adnexitis.
- VRVMT - varicose veins of the small pelvis
- Pain in the muscle tissue during pregnancy can also be caused by the following pathologies and acute conditions:
- Pyelonephritis.

- Inflammation of the appendix.
- Cholelithiasis.
- Incarcerated inguinal hernia.
- Infringement of the intervertebral disc.
- Threatened miscarriage.
- Constipation, flatulence.
- Sprain.
- Muscle injuries.
- Placental abruption.
- IBS - irritable bowel syndrome.
- Intestinal obstruction.
- Genital herpes.
- Symphysitis (third trimester).
- General venous insufficiency, vein occlusion.
- Urolithiasis.
- Braxton Hicks contractions, false, training contractions.
Symptoms of muscle pain during pregnancy
Signs and symptoms of muscle pain in pregnant women are most often transient, more intense sensations, especially chronic ones, need immediate diagnosis, hospitalization and treatment.
Myalgia - pain in muscle tissue can be felt as:
- Shooting pain.
- Sharp, dagger pain (rare).
- Aching, pulling (often).
- Breaking.
- Burning, tingling.
Depending on the provoking factor, the symptoms of muscle pain during pregnancy can be temporary, situational, transient, or permanent, chronic. As a rule, discomfort in a particular area of the body in a future mother is transient, the pain may subside or even be neutralized during pregnancy, changing trimesters. This is due to constant changes in the body of a woman, which directly affect the state of muscle tissue.
Symptoms of physiologically acceptable conditions:
- Aching pain in the legs, subsiding with a change in body posture, at rest.
- Drawing pain in the back, relieved by light massage, relaxing procedures.
- Pain in groin that improves with rest.
- Bursting, drawing pain in the back, in the pelvic region, due to sprain.
- Cramping pain associated with exercise cramps, Braxton-Hicks contractions.
Warning signs that require a doctor's call, examination and medical attention:
- Sudden, spontaneous severe pain with a tendency to worsen.
- Pain that does not subside at rest or with a change in posture, body position.
- Myalgia, accompanied by fever.
- Muscle pain that lasts more than 2-3 days, not even sharp or intense.
- Cramping muscle pain with abnormal vaginal discharge (blood).
- Symptoms of "acute abdomen" - pain, drop in blood pressure, tachycardia, cyanosis of the skin.
Abdominal pain during pregnancy
A painful abdominal symptom in a pregnant woman is wrongly considered a common occurrence, a natural signal of muscle strain due to an increase in the uterus. Indeed, every day the uterus is getting bigger, this is especially noticeable in the second trimester, when the shifted center of balance provokes a change in the woman's gait. Pain in the abdominal muscles during pregnancy may indicate a pathological development of the process of bearing a fetus or other serious diseases - a cyst, inflammation of appendicitis. Fortunately, the pain symptom in pregnant women in the abdomen in 75-80% is due to tension and sprain of the round ligament, which performs the function of supporting the uterus. The bottom of the pelvis is lined with three-layer muscle tissue and fascia, which provides support for almost all organs of the reproductive system, as well as for the abdominal organs. The uterus is supported by thick ligaments, one of which, round, directly holds the uterus in place. An increase in the size of the uterus provokes a stretching of the round ligament, which is quite naturally accompanied by pain in the abdomen.
The bottom of the pelvis is lined with three-layer muscle tissue and fascia, which provides support for almost all organs of the reproductive system, as well as for the abdominal organs. The uterus is supported by thick ligaments, one of which, round, directly holds the uterus in place. An increase in the size of the uterus provokes a stretching of the round ligament, which is quite naturally accompanied by pain in the abdomen.
In the same way, the musculature is also subjected to stress, especially smooth (walls of the uterus) and abdominal muscles. If the expectant mother has not strengthened muscle tissue in advance through sports, exercise, the rectus and abdominal muscles during pregnancy are stretched or overstressed, as they have to participate in supporting the growing uterus. It is too fast stretching, muscle hypertonicity that provokes pain symptoms, while carrying a baby, the waist circumference can almost double, for example, from 65 to 100 centimeters.
The pain of the abdominal muscles during pregnancy most often does not require the intervention of a doctor and special treatment, however, a woman needs to be alert if the pain symptom does not subside when changing posture, rest, relaxation. Therefore, for any disturbing pain, it is better to consult with the attending gynecologist.
Therefore, for any disturbing pain, it is better to consult with the attending gynecologist.
The list of the main emergency conditions in which a painful muscle symptom in the abdomen may appear:
- Obstetrical conditions:
- Threatened miscarriage.
- Septic miscarriage (acute abdomen clinic).
- Ectopic pregnancy, ectopic pregnancy.
- Fibromyoma.
- Placental abruption.
- Rupture of an aneurysm (splenic artery, renal artery and others).
- Distension and rupture of the uterus.
- General pathologies manifested by abdominal pain, including muscle pain:
- Acute pyelonephritis.
- Appendicitis.
- Spontaneous hematoma in the rectus abdominis muscle (bleeding into the muscle tissue).
- Acute cholecystitis.
- Cystitis (pain in the lower abdomen, in the perineum).
- Chronic inflammation of the ovary.
- Umbilical hernia.
- Groin hernia.
If your leg muscles hurt during pregnancy
Most often, leg pain in pregnant women is either vascular disorders (varicose veins) that provoke aching, pulling pains, or convulsions, especially at night.
Why do leg muscles hurt during pregnancy?
- Flat feet, which, of course, was before pregnancy, but the period of gestation aggravates the load on the muscles and provokes their overstrain (hypertonicity). To prevent pain symptoms, which are most often localized in the calves of the legs and intensify when walking, a woman should purchase orthopedic insoles and choose shoes with a stable, medium heel with a fairly rigid sole that fixes the foot.
- Vascular dysfunctions. An increase in the weight of a pregnant woman inevitably entails an additional burden on the vascular system. If before pregnancy there was already a history of varicose veins, you should wear compression underwear, stockings to reduce pressure on the walls of blood vessels.
 Muscles with varicose veins hurt due to the fact that they do not receive proper nutrition.
Muscles with varicose veins hurt due to the fact that they do not receive proper nutrition. - Non-compliance with the rules of a complete, rational diet, as a result of which the muscle tissue does not receive the necessary proteins, carbohydrates, vitamins and microelements. Often, convulsive syndrome is observed in women who adhere to a strict vegetarian diet.
Often during pregnancy, the leg muscles in the calf area, that is, the calf muscles, hurt. Cramping is a severe pain that women describe as “bringing their legs together”. Night cramps of the calf muscles are the most common, which is due to the natural relaxation of the body and the dissonance between relaxation and chronic muscle hypertonicity. Also, hypnogogic convulsions, that is, muscle spasms before the deep sleep phase, often occur. Convulsive syndrome in 65% of cases is diagnosed in the middle of pregnancy, when the needs of the developing fetus are growing rapidly, and the resources of the mother's body are already significantly depleted.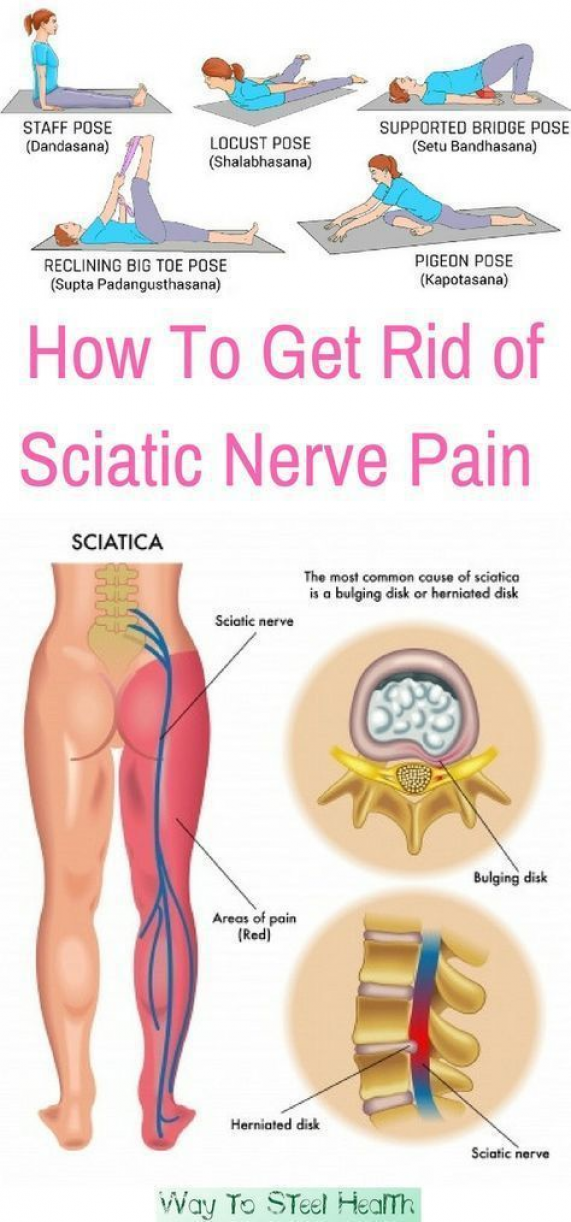
Possible causes of seizures:
- Deficiency of B vitamins, magnesium, potassium, calcium.
- Persistence of bad habits - smoking, abuse of caffeinated drinks.
- Decreased blood sugar levels.
- Anemia, low hemoglobin level.
- Varicose veins.
- Syndromum venae cavae inferioris syndrome - the inferior pudendal vein, when in a horizontal position (at night) the uterus presses on a large vessel, venous outflow is disturbed, convulsions develop. This syndrome occurs in 80% of pregnant women in the third trimester.
- Misuse of diuretics to eliminate edema.
If the muscles between the legs hurt during pregnancy
Despite all the joyful and exciting moments of waiting for the baby, the period of gestation is accompanied by transient discomfort. In addition to the fact that the expectant mother has pain in the lower abdomen, in the lower back, there are many symptoms that can further complicate pregnancy, for example, the muscles between the legs hurt.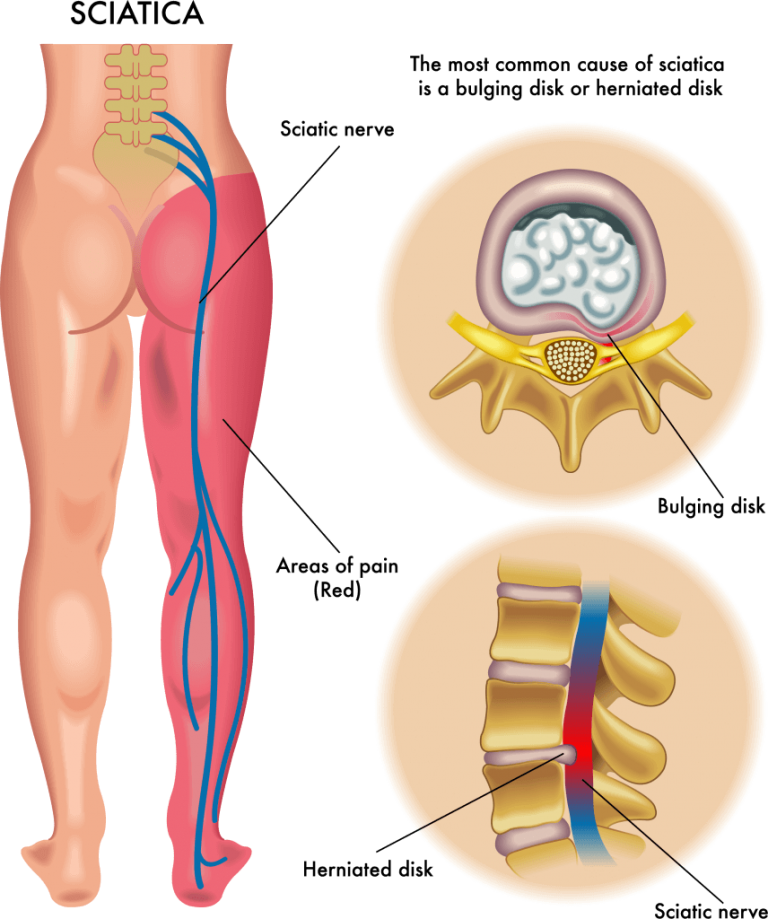 In fact, such pain most likely does not appear in the muscles, but in the ligaments, nerve endings.
In fact, such pain most likely does not appear in the muscles, but in the ligaments, nerve endings.
This is due to the increased secretion of a specific hormone - relaxin. Its main task is to reduce (inhibit) the contractile function of the uterus in the first trimester in order for the pregnancy to continue. In addition, later relaxin is needed to relax, soften the pelvic bones, symphysis, and prepare them for labor. Relaxin begins to be produced literally from the first week of conception, but the consequences of its influence are felt later, in the 2nd, and especially in the 3rd semester. Usually a pregnant woman complains of “muscles between her legs hurt” at precisely these times, pain is also felt in the hips, in the pubic region, and in the lower abdomen.
Another reason that provokes a pain symptom in the groin, between the legs, may be a neurological factor - infringement of the sciatic nerve. Pinching of the nerve roots occurs due to the pressure of the growing uterus, and the pain is projected onto the buttocks, groin area, and lower limbs. Such pain cannot be attributed to true myalgia, although it affects muscle tissue.
Such pain cannot be attributed to true myalgia, although it affects muscle tissue.
Pregnancy, the muscles between the legs hurt - this condition can be caused by a banal overstrain, when a woman overestimates her own physical capabilities and continues to engage in sports exercises without taking into account her special position. Such cases are not uncommon among professional dancers, athletes who continue their activities during pregnancy.
What can relieve pain in the muscles between the legs?
- Rest and reasonable physical activity (no overload).
- Bandage supporting muscles, ligaments.
- Gentle physiotherapy treatments (by prescription only).
- Warm compresses.
- Performing a set of special exercises for pregnant women for preparatory muscle stretching.
If your groin muscles hurt during pregnancy
The entire period of pregnancy there is an increase in venous pressure, especially for the vessels of the lower extremities.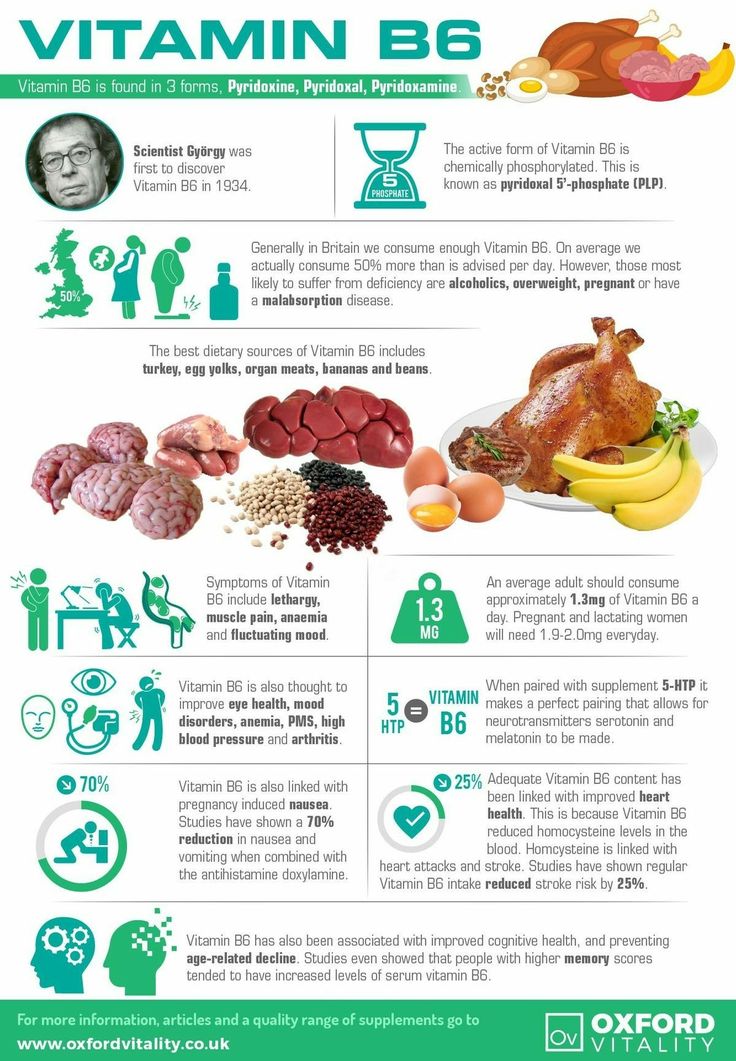 This process is due to increased venous pressure of the enlarging uterus and at the same time slower pressure in the veins of the groin and legs. The growing uterus compresses the pelvic veins, the outflow of blood from the legs is difficult, this is one of the reasons why the groin muscles hurt during pregnancy.
This process is due to increased venous pressure of the enlarging uterus and at the same time slower pressure in the veins of the groin and legs. The growing uterus compresses the pelvic veins, the outflow of blood from the legs is difficult, this is one of the reasons why the groin muscles hurt during pregnancy.
In addition, pain in the groin is explained by another physiologically acceptable reason.
In the second trimester, the round ligament is significantly stretched, the task of which is to support the uterus. Pain in the inguinal region during a sprain can be very acute, but short-term, it can be felt as a spasm, cramp, radiating down the abdomen.
In addition to physiological stretching, the following factors can explain why the groin muscles hurt during pregnancy:
- Inguinal hernia. The pain is localized to the right or left as a result of a decrease in the tone of the local supporting muscle tissue. As a result, intestinal loops can slip out under the pressure of an enlarging uterus right into the groin.
 A hernia looks like a bulge in the groin area, and when pinched by the muscles, it provokes pain. Strangulation is a medical emergency to avoid necrosis (blood supply cut off) and rupture of the intestine.
A hernia looks like a bulge in the groin area, and when pinched by the muscles, it provokes pain. Strangulation is a medical emergency to avoid necrosis (blood supply cut off) and rupture of the intestine. - Enlarged lymph nodes located in the groin. Enlarged lymph nodes may be a sign of an infectious inflammatory process in the pelvic organs. As a rule, a pregnant woman undergoes a thorough examination upon registration, and inflammations are recorded in the card. However, the very process of bearing a fetus can provoke an exacerbation of such diseases as adnexitis, parametritis, proctitis, endometritis, as a result, a pain symptom develops, including in the muscles.
- Urolithiasis also provokes pain, which in the form of renal colic can be reflected in the muscle tissues of the back, thighs or groin, depending on the location of the calculus. If the stone is localized low, the pain will manifest itself in the groin area.
- Pain in the muscles of the groin during pregnancy can be reflected when, due to the increased load on the spine, the nerve endings in the lumbosacral region are pinched.

- Bruise, blow to the groin.
- Genital herpes presenting as erythematous papules, itching, vaginal discharge, swollen lymph nodes, myalgia and pyrexia.
- VRVMT - varicose veins of the small pelvis, a disease that develops asymptomatically, but becomes acute during pregnancy. Venous hemodynamics is disturbed, pulling pains develop in the groin, in the legs.
When the muscles of the perineum hurt during pregnancy
The muscles of the intestines, gallbladder, esophagus and stomach are physiologically more relaxed during pregnancy, as they are directly involved in the nutrition of the fetus, but the muscles of the back, abdomen and perineal muscles, on the contrary, are subjected to increased stress and strain. This is perhaps the first and most common reason why the muscles of the perineum hurt during pregnancy.
In addition, the muscle tissue of the perineum can hurt due to the pressure of the growing uterus on the nerve endings and ligaments located in this area.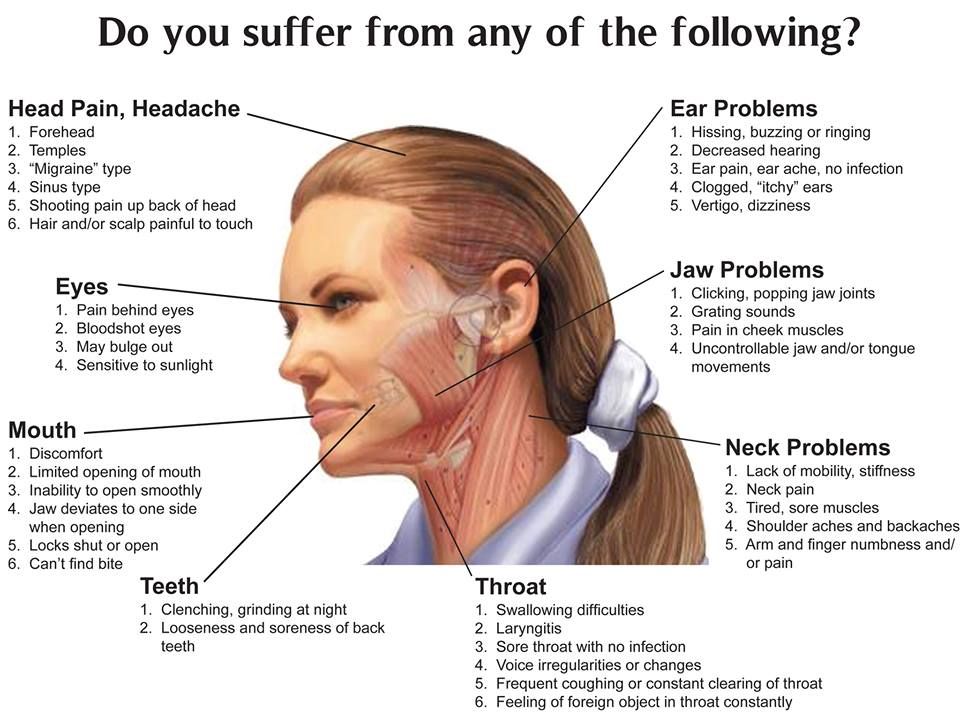 As a rule, pain in the perineum after childbirth subsides irrevocably, which proves the physiological and natural nature of the pain symptom. An exception may be pain caused by a strong stretching of the perineum due to symphysitis, which develops in the second half of pregnancy.
As a rule, pain in the perineum after childbirth subsides irrevocably, which proves the physiological and natural nature of the pain symptom. An exception may be pain caused by a strong stretching of the perineum due to symphysitis, which develops in the second half of pregnancy.
Symphysitis, in turn, is explained by calcium deficiency in bone tissue, primary or secondary. Pain with symphysis is aching, pulling, the sensation of ache spreads in the pelvic region, in the groin, in the perineum, especially if a woman, lying in bed, tries to straighten her legs.
Overload and a kind of "softening" of the pelvic bones, which, in addition to being subjected to pressure from the uterus, "prepare" for childbirth (the body secretes relaxin for this), lead to a pain symptom. It can be felt as a pulling or shooting pain in the lumbar region, lower abdomen and in the muscle tissue of the perineum. As a compensatory consequence of muscle hypertonicity, hypotension develops, a decrease in the elasticity of the bladder, urethra. For expectant mothers, involuntary urination is typical even with slight tension in the muscles of the abdomen or back - with laughter, with coughing. The same symptom is observed in some women when squatting or exerting pressure on the muscles of the perineum.
For expectant mothers, involuntary urination is typical even with slight tension in the muscles of the abdomen or back - with laughter, with coughing. The same symptom is observed in some women when squatting or exerting pressure on the muscles of the perineum.
Also, during the period of gestation, a woman may have muscle pain in this area due to venous stasis, insufficiency. If you have a history of varicose veins when registering, most likely a pain symptom in the groin, perineum, and legs will be inevitable, but reversible with the right treatment.
Why do vaginal muscles hurt during pregnancy
The vagina is an organ that contains many nerve endings, receptors, blood vessels, so it is very dependent on the quality of the circulatory system.
Do vaginal muscles hurt during pregnancy? There may be several reasons:
- Weight load on the pelvic area, respectively, a decrease in active blood flow and a decrease in the supply of vaginal tissues.
 Congestion, swelling is a typical condition that accompanies pregnancy, the result of which is transient pain in the groin and vagina. In addition to the pain symptom, a woman may feel itching, tingling, which, as a rule, subside at rest, in a horizontal position (blood outflow).
Congestion, swelling is a typical condition that accompanies pregnancy, the result of which is transient pain in the groin and vagina. In addition to the pain symptom, a woman may feel itching, tingling, which, as a rule, subside at rest, in a horizontal position (blood outflow). - Varicose veins, varicose veins of the labia. This pathological phenomenon can only be associated with the period of pregnancy, but can be observed before it. Varicose veins of the labia may be due to a weak valvular vascular system, overweight, inflammatory processes in the internal organs of the small pelvis, constant physical overstrain (carrying weights). In addition, pregnancy varicose veins can be explained by increased secretion of progesterone and estrogens, lengthening and expansion of the entire circulatory network, starting from the 10th week after conception. Uterine blood flow is activated during the entire period of gestation and reaches a peak (600-700 ml per minute) by the time of delivery.
 Accordingly, the fallopian tubes inevitably thicken and hyperemia, the cervix swells, the labia swells, and pain appears.
Accordingly, the fallopian tubes inevitably thicken and hyperemia, the cervix swells, the labia swells, and pain appears.
Symptoms of varicose veins can manifest themselves in the following signs:
- Drawing pain in the groin, in the vagina.
- Sensation of fullness in labia.
- Swelling of the vagina.
- Dryness, lack of lubrication, itching.
- Possible appearance of visible varicose veins on the labia, in the groin.
If the muscles of the vagina hurt during pregnancy, the cause can be looked for in the past. If a woman, long before conception, systematically took hormonal contraceptives or hormonal drugs for the treatment of a chronic disease, her vascular system got used to the help of hormones. During pregnancy, without the usual dose of hormonal substances, the vessels may not work at full strength, the venous outflow is disturbed, congestion develops in the lower abdomen and pain, including in the vagina
When abdominal muscles hurt during pregnancy
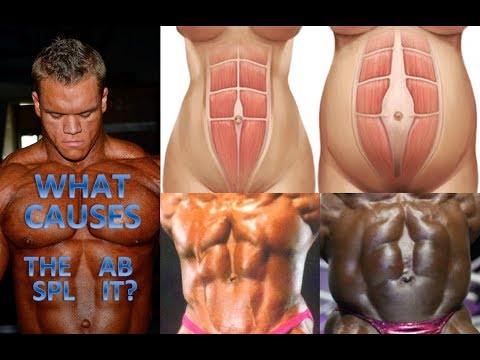
The abdominal muscles, which before conception were responsible for the condition and appearance of the press, during pregnancy should perform a completely different task. Support for the uterus and other internal organs is a new function of the rectus muscles, which are located in the anterior part of the peritoneum. The abdominal muscles are two muscles, the right rectus and the left rectus, which are connected in a place that is very poetically called the “white line” of the abdomen. The rectus muscles originate from the lower part of the sternum, from the lower ribs, extending down vertically along the abdominal region, reach the pubic bone, where they are fixed. The rectus muscles are crossed by specific tendon elements - jumpers, it is this combination of rectus and transverse muscles that gives the desired visual effect of the "cubes" of the press. However, for a normal pregnant woman, the cubes are not as important as the health of the baby and her own health, which is sometimes overshadowed by uncomfortable pain. Rectus muscles (abs) all 9months are subject to changes, because they must hold the growing uterus all the time. In this state, they are able to constantly close in place of the "white line" and gradually diverge evenly on the sides.
Support for the uterus and other internal organs is a new function of the rectus muscles, which are located in the anterior part of the peritoneum. The abdominal muscles are two muscles, the right rectus and the left rectus, which are connected in a place that is very poetically called the “white line” of the abdomen. The rectus muscles originate from the lower part of the sternum, from the lower ribs, extending down vertically along the abdominal region, reach the pubic bone, where they are fixed. The rectus muscles are crossed by specific tendon elements - jumpers, it is this combination of rectus and transverse muscles that gives the desired visual effect of the "cubes" of the press. However, for a normal pregnant woman, the cubes are not as important as the health of the baby and her own health, which is sometimes overshadowed by uncomfortable pain. Rectus muscles (abs) all 9months are subject to changes, because they must hold the growing uterus all the time. In this state, they are able to constantly close in place of the "white line" and gradually diverge evenly on the sides. It is this phenomenon that is called diastasis, it is this that explains why the abdominal muscles hurt during pregnancy.
It is this phenomenon that is called diastasis, it is this that explains why the abdominal muscles hurt during pregnancy.
Not every future mother may have diastasis, for those who previously went in for sports, led an active lifestyle, were on the move, strengthened the press, diastasis is observed very rarely. However, even in those who did not devote time to sports at all and “acquired” diastasis during pregnancy, it disappears 2-4 months after childbirth, such is the unique adaptive property of muscle tissue.
If the abdominal muscles hurt during pregnancy, this is considered quite acceptable, but under certain conditions and sensations:
- The abdominal muscles hurt only in the navel area, the pain is transient, appears after the 12th week and gradually subsides as the muscles are stretched adaptively.
- The rectus abdominis muscles hurt only during physical exertion.
- Pain in the abdominal area is not associated with an increase in body temperature, does not move down the abdomen and is not acute, intense.

- All other pain symptoms in the region of the rectus muscles need to be monitored by a doctor, in this sense it is better to play it safe and minimize the risk of possible complications.
Why groin muscles hurt during pregnancy
A pain symptom in the groin area in pregnant women can be triggered by various factors, the diagnosis of which is rather difficult. The fact is that the groin area is not considered a separate anatomical unit, rather it is a zone of connection between the hips and the articulation of the abdominal cavity. A large number of different muscles are attached to the groin, which are called adductor muscles, they are responsible for the movement of the hips and their attachment to the pelvis. Also in the inguinal zone there is a canal that includes one of the largest arteries of the body - the femoral vessels, there is also an important element - the round ligament of the uterus, which is subject to severe stretching during pregnancy.
Usually, groin pain is well known to athletes and those who undergo intense physical exertion, but the groin muscles also hurt during pregnancy.
What causes pain in the groin muscles in a pregnant woman?
- Physiological stretching of the round ligament that supports the uterus.
- Varicose veins.
- Infectious inflammatory diseases of the organs located in the pelvic region. Inflammation causes an increase in the lymphatic inguinal nodes, pain.
- Adnexitis, inflammation of the appendages, ovaries.
- Calcium deficiency associated with its increased consumption during pregnancy.
- Back pain radiating to the groin may not be related to muscle tissue, but felt like muscle pain. This happens with urolithiasis, its exacerbation, renal colic.
- Pain in the inguinal region can be provoked by constipation - both a physiological, hormonal factor, and caused by the psycho-emotional state of a pregnant woman (neurotic spastic constipation).

- Inguinal hernia.
- Varicose veins of the great vein of the leg, located under the skin in the inguinal region.
- Injury, bruised groin.
- Symphysitis in the second half of gestation (softening, stretching of the bones of the pubic joint).
- Excessive strain on the muscles of the thighs during stretching exercises for pregnant women.
If your back muscles hurt during pregnancy
About 70-75% of pregnant women experience pain of a different nature in the back, lower back.
Why do back muscles hurt during pregnancy?
- Physiologically acceptable hormonal changes, relaxin secretion, resulting in expansion and relaxation of the pelvic bones, intervertebral ligaments. At the same time, the muscles still try to perform a “corset” function, but are subject to increased stress, are in hypertonicity. Such pain subsides after the 20-22nd week, when the body is already prepared and the production of relaxin decreases.
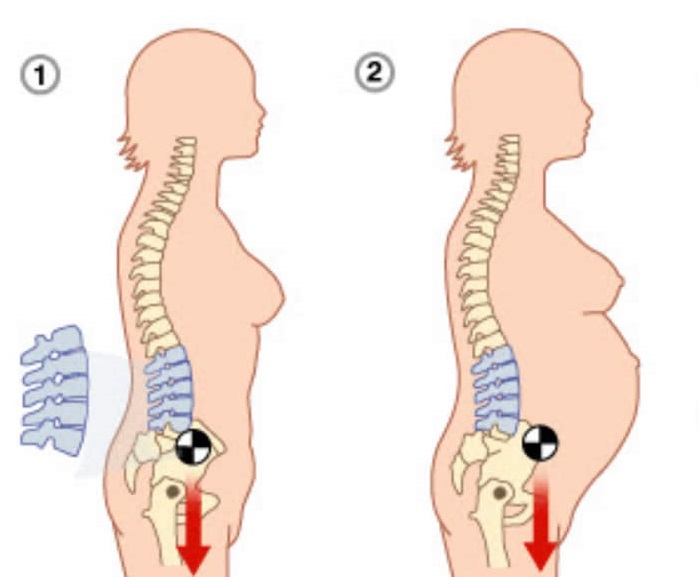
- Displacement of the main center of gravity due to an increase in the body weight of the expectant mother. The center is significantly shifted forward, respectively, all the muscles of the back are tensed with double strength. Sometimes the woman herself exacerbates the pain symptom, because she does not follow her posture, her back bends forward too much after her stomach.
- The pressure of the growing, growing uterus on the nerve endings of the spinal column is also compressed and vessels, blood flow and nutrition of the tissues surrounding the spinal discs are disturbed. Such shooting, strong, but short-term pains in the lumbosacral zone of the back are especially characteristic.
- A significant increase in the body weight of a pregnant woman provokes varicose veins, disrupts the venous outflow of blood in the pelvic area, legs and lower back hurt.
- Incorrectly selected shoes, especially high heels, which are not useful in principle, as they provoke an unphysiological gait,
Diastasis of the rectus abdominis muscles and diastasis of the womb.
 Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy — What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis.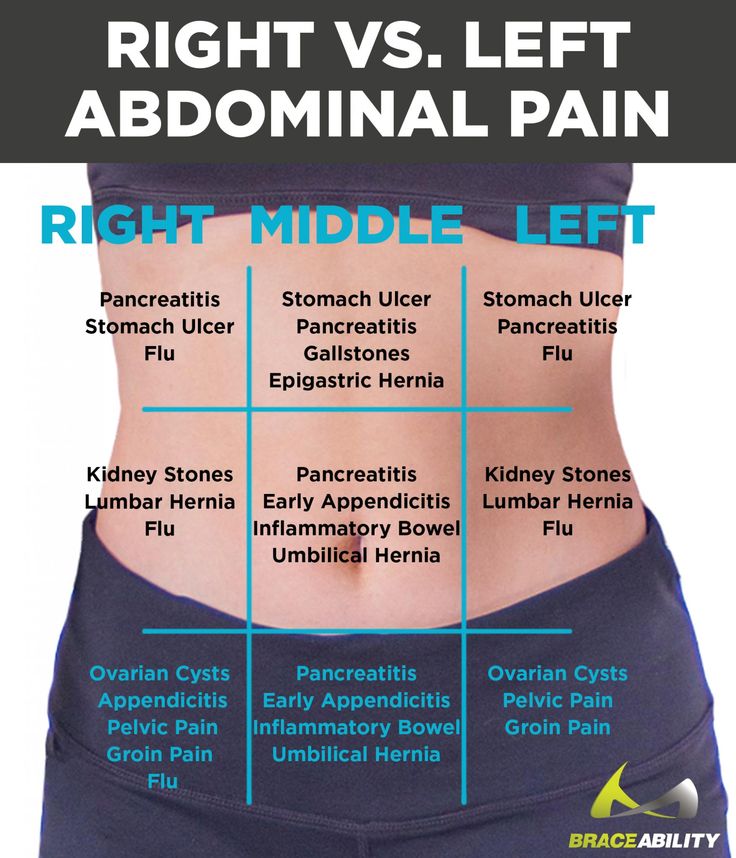 And they certainly have common causes for the appearance.
And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of collagen in the connective tissue. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
— Divergence of the rectus abdominis occurs in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and cartilage that connect the pubic bones suffer. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, such a patient may have a rupture of the pubic symphysis, may require surgery to restore it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat.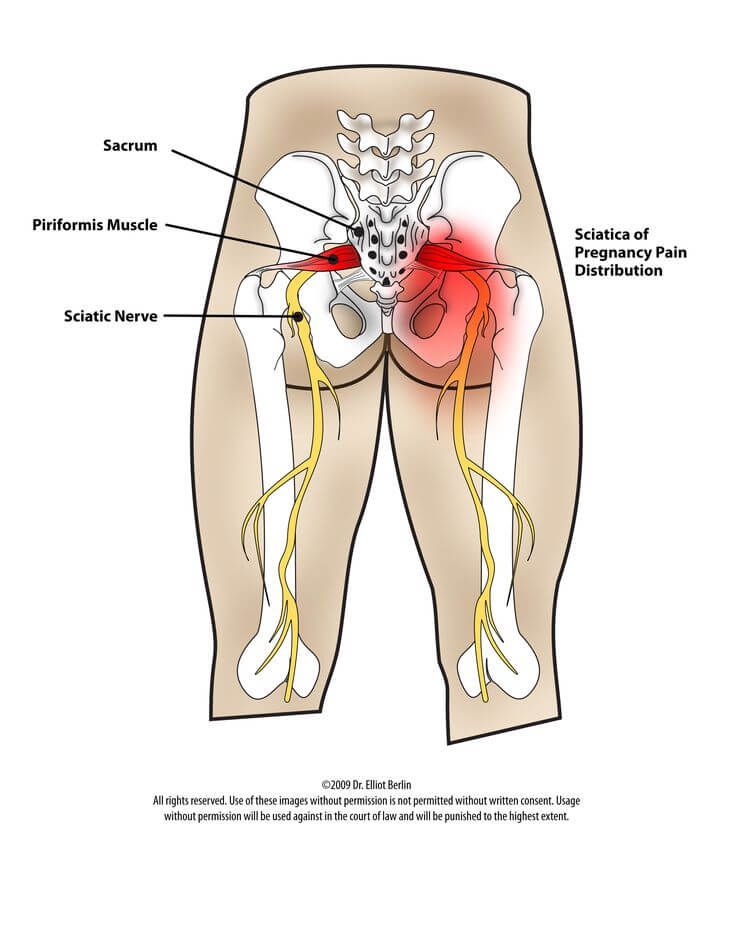 In this case, diastasis is defined as a vertical defect between the rectus muscles.
In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up.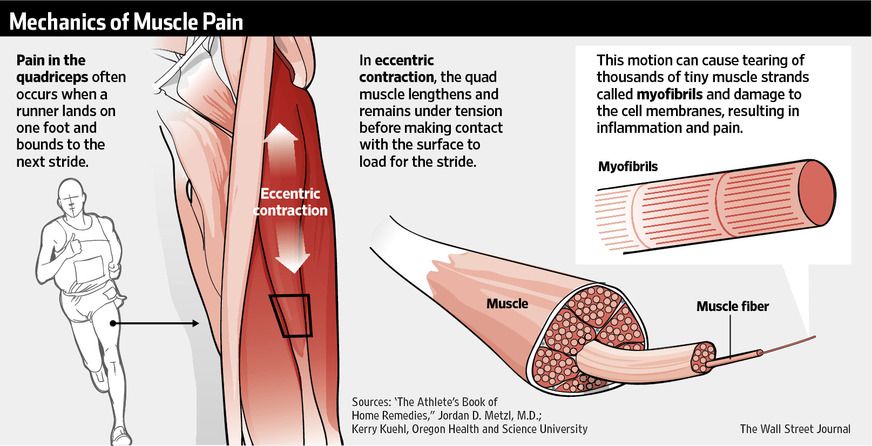 Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
In case of symphysiopathy, therapeutic exercises reduce back and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment for pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis.