Signs of dairy intolerance in infants
Milk intolerance in babies and children
Milk intolerance in babies and children | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Some babies and children have a reaction when they drink cow's milk or formula made from cow's milk. This could be due to 2 things: a lactose intolerance or an allergy to milk. If your child has one of these conditions, you will have to alter their diet to cut down on milk or avoid it altogether.
Call triple zero (000) for an ambulance if your child has the following symptoms. They could be having a severe allergic reaction and will need urgent medical attention.
- wheezing or difficulty breathing
- a swollen tongue
- vomiting
- they are pale and floppy or unconscious
What is milk intolerance and milk allergy?
Around 1 in 10 young children has a reaction when they drink cow's milk. This could be because they have a lactose intolerance or a milk allergy. Milk allergy is much more common than lactose intolerance in children under 5.
Lactose intolerance is a problem with the digestive system – it means your child doesn't have the enzyme needed to digest lactose, which is the sugar in milk.
Milk allergy, however, is a problem with the immune system — the body reacts to the protein in milk. An allergy usually involves other parts of the body as well as the stomach, and may cause symptoms such as a skin rash or swelling of the face.
Your doctor can confirm whether your child is lactose-intolerant or has a milk allergy by doing some medical tests. Don't use unproven tests such as Vega, kinesiology, Alcat or allergy elimination tests for children. A milk intolerance is very unlikely to be the cause of mucus or coughing.
Many young children grow out of their intolerance or allergy. But don't start giving them cow's milk until your doctor tells you it's safe to do so.
Lactose intolerance
Causes
Lactose is the sugar found in the milk produced by all mammals, including humans. Sometimes people don't produce enough of the enzyme lactase in their gut to break down the lactose.
Very few babies have true lactose intolerance, a rare genetic condition where they're born without any lactase enzymes at all. (This is called primary lactose intolerance). However, many people develop lactose intolerance later in life, after the age of 5. It is more common in Aboriginal Australians and people from Asia, Africa, the Middle East and some Mediterranean countries.
Babies and young children can become intolerant to milk if the lining of their gut is damaged by an illness such as gastroenteritis, or an allergy or intolerance to another food. This is called secondary lactose intolerance and will go away once the gut heals, usually over a few months.
Symptoms and diagnosis
The symptoms of lactose intolerance in babies and children are:
- liquid, sometimes green, frothy stools
- being irritable
- stomach aches
- bloating
- passing a lot of gas
- not putting on weight
- nappy rash
All of these symptoms are common in babies and don't necessarily mean they have lactose intolerance.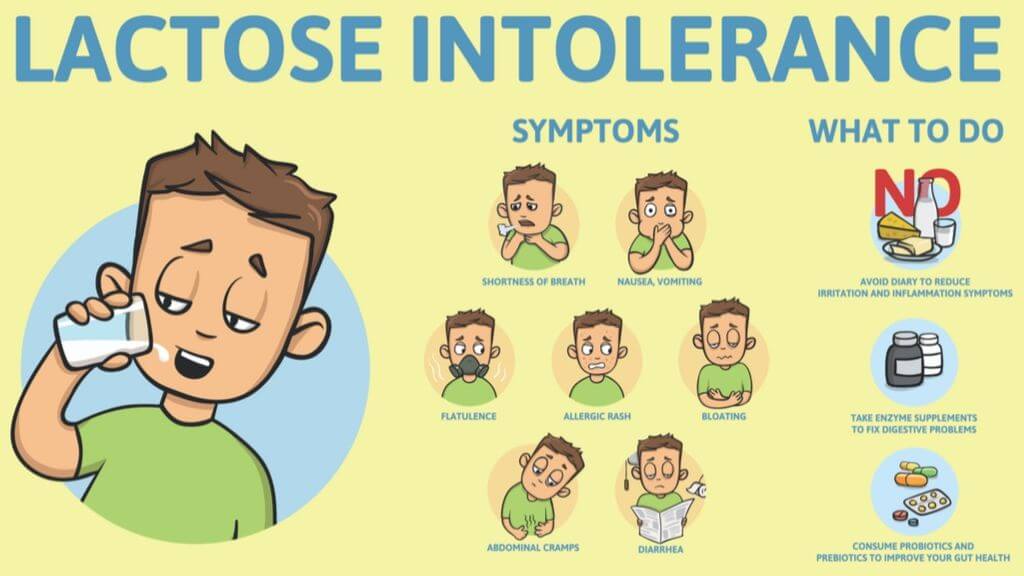 But if your child has diarrhoea and isn't putting on weight, see your doctor. Don't stop breastfeeding unless your doctor tells you to.
But if your child has diarrhoea and isn't putting on weight, see your doctor. Don't stop breastfeeding unless your doctor tells you to.
Tests include a breath test to measure the hydrogen in your child's breath, or cutting out dairy to see if their symptoms improve. This is known as an elimination diet.
Treatment
If the lactose intolerance is caused by a tummy upset, keep on breastfeeding. If your baby is formula fed, talk to your doctor or child and family health nurse before switching to low-lactose or lactose-free formula.
Older children will need to cut down on, but not eliminate, dairy foods from their diet. They can still have some cheeses, yogurt, calcium-fortified soy products, lactose-free milk, butter and cream. Your doctor or a dietitian will advise you on the best diet for your child.
Cow's milk allergy
Cow's milk allergy is one of the most common food allergies in young children. It usually disappears by the time they reach school age.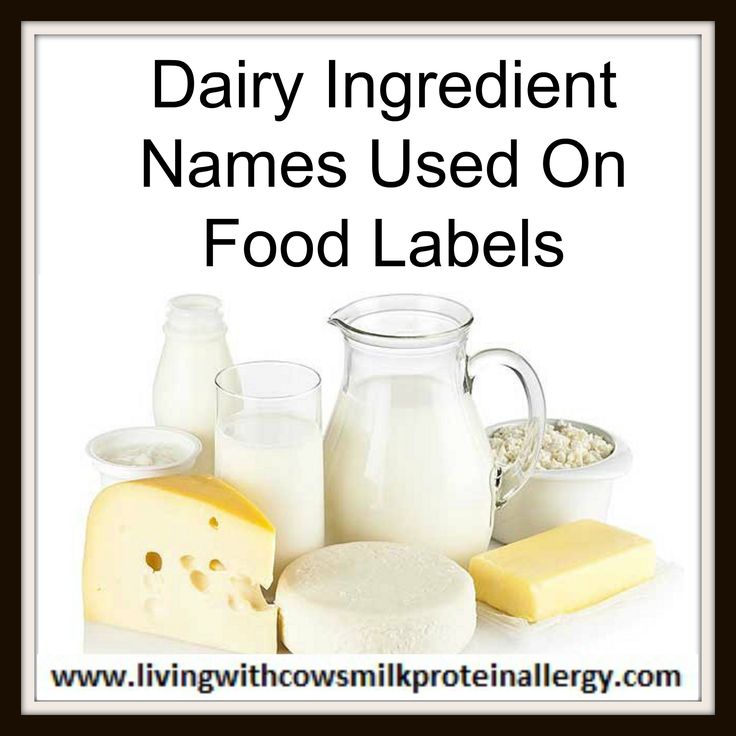 It occurs when your child's immune system reacts to the protein in milk.
It occurs when your child's immune system reacts to the protein in milk.
Symptoms and diagnosis
Reactions to milk can occur within minutes or not for several days.
Rapid reactions include:
- hives (urticaria)
- swelling of the lips, face or eyes
- stomach pain
- vomiting
- diarrhoea
- noisy breathing or wheezing
- a swollen tongue
- a swollen or tight throat
- a hoarse voice
- change in consciousness or floppiness in babies or young children
Delayed reactions include:
- an increase in eczema
- blood or mucus in stools
- vomiting and/or diarrhoea 2-24 hours after having milk
It is very important to see a doctor if your child has the symptoms of milk allergy. The condition is diagnosed using the history of symptoms or can sometimes be confirmed with an allergy test.
Treatment
If your child is allergic to milk, you need to completely remove dairy products from their diet. Follow your doctor's or allergy specialist's advice and read food labels carefully. You may also need to avoid milk from other animals, such as goats, as well as coconut milk products. Watch out for other words used to describe milk on food labels, such as butter, buttermilk, cream, curd, ghee, milk, cheese, dairy, milk solids, whey, yoghurt, casein and caseinates.
Follow your doctor's or allergy specialist's advice and read food labels carefully. You may also need to avoid milk from other animals, such as goats, as well as coconut milk products. Watch out for other words used to describe milk on food labels, such as butter, buttermilk, cream, curd, ghee, milk, cheese, dairy, milk solids, whey, yoghurt, casein and caseinates.
If your baby is formula-fed, you can use soy protein formula (unless they are also allergic to soy), extensively hydrolysed formula (EHF) or amino acid-based formula (AAF). Do not use formula made from cow's milk, goat's milk, sheep milk, HA, A2 milk or lactose-free.
If your child is over the age of one, they can be given soy milk, calcium-enriched rice, and oat or nut milks. It is important to make sure they are getting enough calcium.
You may be advised to carry an Epipen adrenaline autoinjector if your child is allergic to milk. Severe allergic reactions can sometimes lead to anaphylaxis, which is serious and can even be fatal.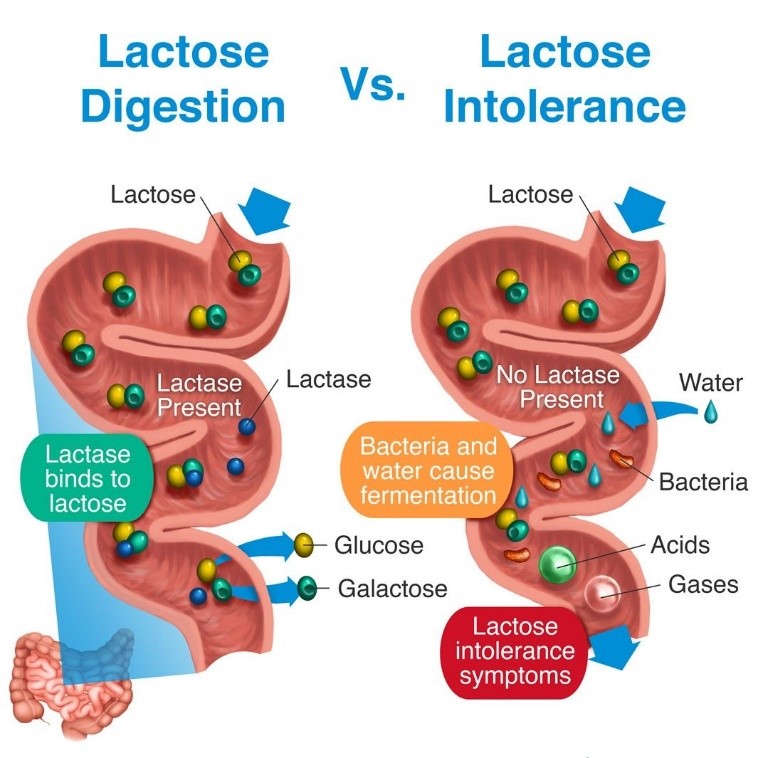 An adrenaline autoinjector can be used to give first aid in the event of anaphylaxis.
An adrenaline autoinjector can be used to give first aid in the event of anaphylaxis.
Breastfeeding a baby who can't tolerate milk
If your baby is lactose-intolerant, you don't need to change your diet. It doesn't matter how much dairy you consume, the amount of lactose in your milk will be the same.
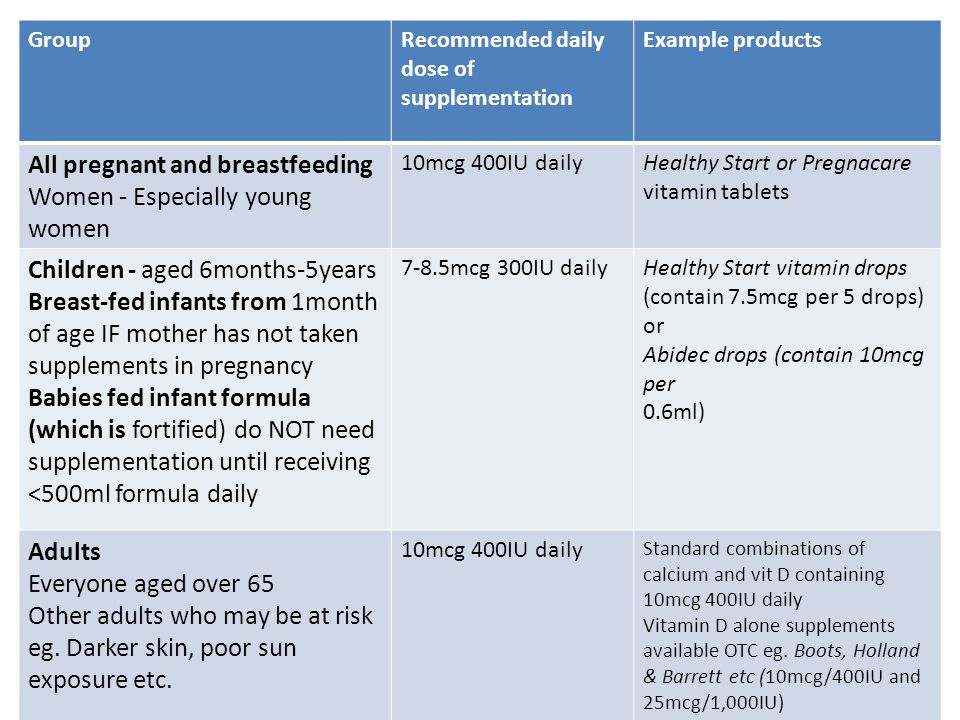
However, if your baby is diagnosed with milk allergy, you will need to remove all dairy from your own diet too. You will need calcium and vitamin D supplements every day. Your doctor or allergy specialist will advise you.
Where to seek more help
Don't try to deal with milk intolerance yourself. You can get help from:
- your doctor
- Pregnancy, Birth and Baby on 1800 882 436
- Australasian Society of Clinical Immunology and Allergy
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australasian Society of Clinical Immunology and Allergy (Cow's milk (dairy) allergy), Australasian Society of Clinical Immunology and Allergy (Infant Feeding and Allergy Prevention Clinical Update), Australian Breastfeeding Association (Lactose intolerance and the breastfed baby), Raising Children Network Australia (Lactose intolerance: babies, children and teenagers), Royal Children’s Hospital (Allergy and Immunology), Sydney Children’s Hospitals Network (Allergy - Milk allergy and milk-free diet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2020
Back To Top
Related pages
- Reactions to food
- How to introduce allergy foods
- Airborne allergies
Need more information?
Lactose intolerance - MyDr.com.au
Lactase deficient people do not have enough lactase, the enzyme that helps break down lactose and they suffer from lactose intolerance. The main symptoms of lactose intolerance are bloating and wind.
Read more on myDr website
Lactose intolerance - Better Health Channel
Symptoms of lactose intolerance include bloating, gas, abdominal pain and diarrhoea.
Read more on Better Health Channel website
ASCIA Guide for Milk Substitutes in Cow’s Milk Allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Guide for Milk Substitutes in Cow’s Milk Allergy
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy - Cow's milk allergy and milk free diet | Sydney Children's Hospitals Network
How common is cow’s milk allergy? Cow’s milk allergy is one of the most common food allergies in childhood affecting about 1-2% of preschool children
Read more on Sydney Children's Hospitals Network website
Cow's milk (dairy) allergy | Dietitians Australia
Cow's milk allergy is common in babies and children, and symptoms can range from mild to severe. Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Read more on Dietitians Australia website
Cow’s milk allergy - Better Health Channel
Milk allergy symptoms range from mild to a life-threatening severe allergic reaction. Avoid food containing milk only under strict medical supervision
Read more on Better Health Channel website
Food allergy versus food intolerance - MyDr.com.au
A food allergy is an immune response triggered by eating specific foods that cause certain well known symptoms to develop.
Read more on myDr website
Cow`s milk (dairy) allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Cow's milk is a common cause of food allergy in infants.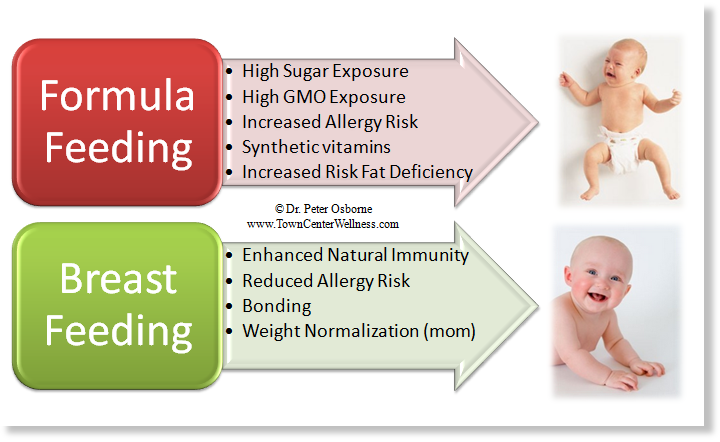 In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Food intolerances: children & teenagers | Raising Children Network
Food intolerance symptoms in children and teens include bloating, diarrhoea and stomach pain. If you think your child has food intolerance, talk to your GP.
Read more on raisingchildren.net.au website
Food intolerance - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Around 1 in 20 infants and 1 in 100 adults are allergic to food.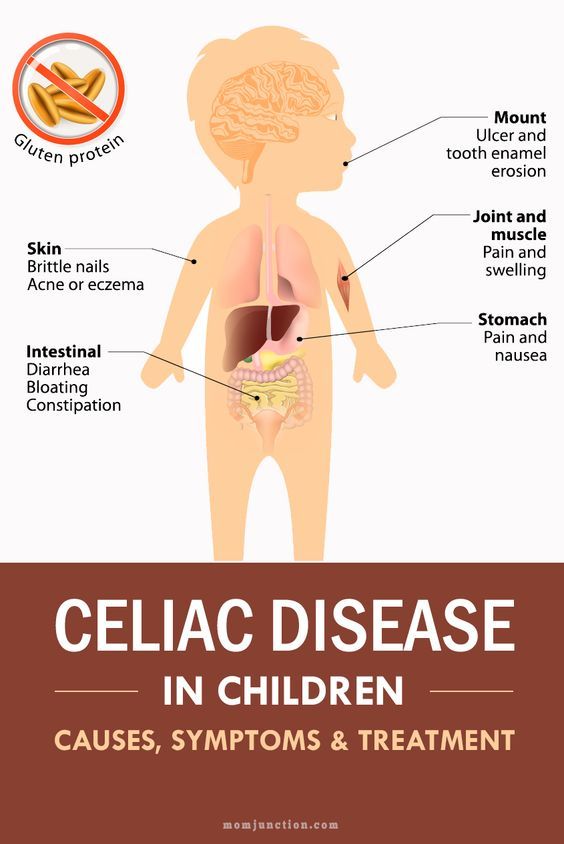 Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.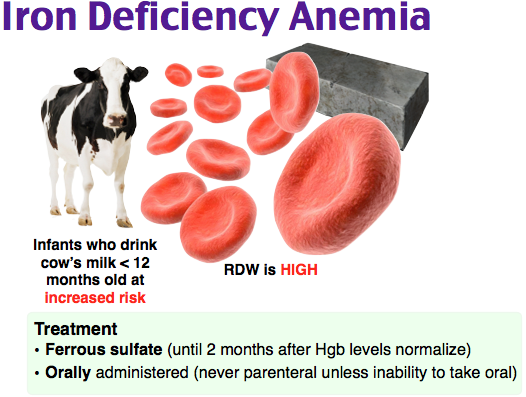
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.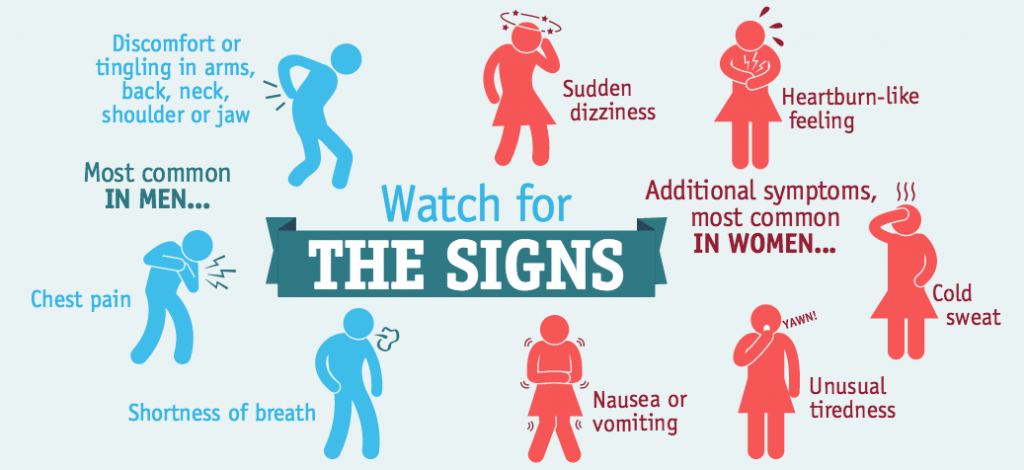
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Milk Allergy in Infants (for Parents)
What Is a Milk Allergy?
When a baby is allergic to milk, it means that his or her immune system, which normally fights infections, overreacts to proteins in cow's milk. Every time the child has milk, the body thinks these proteins are harmful invaders and works hard to fight them.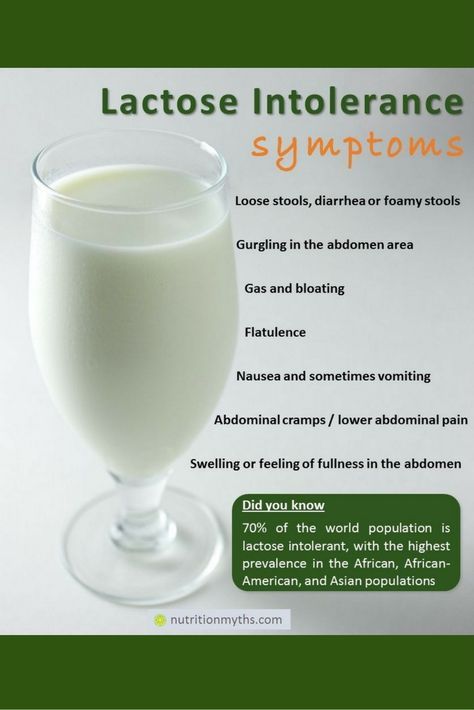 This causes an allergic reaction in which the body releases chemicals like
This causes an allergic reaction in which the body releases chemicals like
histamine.
Cow's milk is in most baby formulas. Babies with a milk allergy often show their first symptoms days to weeks after they first get cow milk-based formula. Breastfed infants have a lower risk of having a milk allergy than formula-fed babies.
People of any age can have a milk allergy, but it's more common in young children. Many kids outgrow it, but some don't.
If your baby has a milk allergy, keep two epinephrine auto-injectors on hand in case of a severe reaction (called anaphylaxis). An epinephrine auto-injector is an easy-to-use prescription medicine that comes in a container about the size of a large pen. Your doctor will show you how to use it.
What Are the Signs & Symptoms of a Milk Allergy?
In children who show symptoms shortly after they have milk, an allergic reaction can cause:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- stomach upset
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- swelling
- a drop in blood pressure causing lightheadedness or loss of consciousness
The severity of allergic reactions to milk can vary. The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
Children also can have:
- an intolerance to milk in which symptoms — such as loose stools, blood in the stool, refusal to eat, or irritability or colic — appear hours to days later
- lactose intolerance, which is when the body has trouble digesting milk
If you're not sure if your child has an intolerance versus an allergy, talk to your doctor.
If Your Child Has an Allergic Reaction
If your child has symptoms of an allergic reaction, follow the food allergy action plan your doctor gave you.
If your child has symptoms of a serious reaction (like swelling of the mouth or throat or difficulty breathing, or symptoms involving two different parts of the body, like hives with vomiting):
- Give the epinephrine auto-injector right away. Every second counts in an allergic reaction.

- Then, call 911 or take your child to the emergency room. Your child needs to be under medical supervision because, even if the worst seems to have passed, a second wave of serious symptoms can happen.
How Is a Milk Allergy Diagnosed?
If you think your infant is allergic to milk, call your baby's doctor. He or she will ask you questions and talk to you about what's going on. After the doctor examines your baby, some stool tests and blood tests might be ordered. The doctor may refer you to an allergist (a doctor who specializes in treating allergies).
The allergist might do skin testing. In skin testing, the doctor or nurse will place a tiny bit of milk protein on the skin, then make a small scratch on the skin. If your child reacts to the allergen, the skin will swell a little in that area like an insect bite.
If the allergist finds that your baby is at risk for a serious allergic reaction, epinephrine auto-injectors will be prescribed.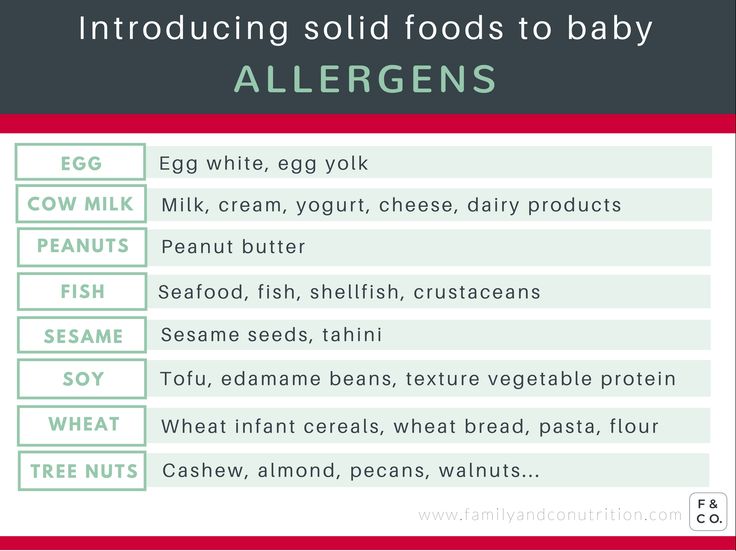
Avoiding a Milk Allergy Reaction
If You're Breastfeeding
If your breastfed infant has a milk allergy, talk to the allergist before changing your diet.
If You're Formula Feeding
If you're formula feeding, your doctor may advise you to switch to an extensively hydrolyzed formula or an amino acid-based formula in which the proteins are broken down into particles so that the formula is less likely to trigger an allergic reaction.
You also might see "partially hydrolyzed" formulas, but these aren't truly hypoallergenic and can lead to a significant allergic reaction.
If you're concerned about a milk allergy, it's always best to talk with your child's doctor and work together to choose a formula that's safe for your baby.
Do not try to make your own formula. Commercial formulas are approved by the U.S. Food and Drug Administration (FDA) and created through a very specialized process that cannot be duplicated at home. Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
If you have any questions or concerns, talk with your child's doctor.
Lactase deficiency in infants: symptoms and diagnosis
Signs of lactase deficiency in infants should be known to parents, because this will allow them to suspect this condition in a timely manner, identify its cause and improve the condition of the baby.
Signs of lactose intolerance
Signs of lactase deficiency in a child are diverse. This is a stool with a large water spot and a sour smell, bloating, rumbling, abdominal pain (colic). One of the most common symptoms that worries parents is frequent loose stools in a baby. It is watery, frothy and has a sour smell. It should be remembered that the younger the child, the more frequent his stool, and this is completely normal. So if the baby is developing well and feels good, and his feces are normal, you should not think that these are signs of lactose intolerance in newborns. nine0003
nine0003
Sometimes lactase deficiency in newborns is accompanied by poor weight gain and growth. This is due to the fact that the carbohydrates necessary for the child do not enter the body, and the baby may lack nutrients.
If the baby quickly grew out of the recently purchased sliders and sleepsuits, and his cheeks and handles are round and plump, you should not suspect lactase deficiency in the child.
Intestinal colic may be present in children with lactose intolerance. After eating, the child will experience bloating, anxiety, crying. These signs usually appear on the 3-6th week of a baby's life. This is probably due to an increase in milk consumption by an older baby. nine0003
The mechanism of such manifestations of lactose intolerance as intestinal colic, bloating and rumbling is as follows. Carbohydrates that are not digested due to the absence or lack of the lactase enzyme continue their movement through the intestines. In the colon, they are exposed to intestinal microflora, resulting in the formation of an excess of gases (hydrogen, methane, carbon dioxide). Gas stretches the walls of the intestines, causing bloating, pain and increased intestinal peristalsis. Violation of the normal chemical composition of intestinal contents can lead to disturbances in the composition of the intestinal microflora. nine0003
Gas stretches the walls of the intestines, causing bloating, pain and increased intestinal peristalsis. Violation of the normal chemical composition of intestinal contents can lead to disturbances in the composition of the intestinal microflora. nine0003
When should you not think about lactase deficiency?
Quite often in recent years, when there are problems with digestion, children are diagnosed with lactose intolerance. However, this is not always true. As mentioned above, the frequency of stool in infants is individual. Frequent or rare stools are not in themselves a sign of lactase deficiency in a child. The symptoms of this pathology are multiple.
Important!
Sometimes regurgitation is taken as a sign of lactose intolerance by parents. But even if regurgitation is frequent and plentiful, it is unlikely that this is lactase deficiency - the symptoms in children with this pathology are associated with the work of the intestines, and not the esophagus or stomach. nine0003
nine0003
How to identify lactose intolerance
The diagnosis of lactose intolerance usually begins with an organoleptic evaluation of feces. Unformed, watery, frothy yellow or green feces with a sour smell testify in favor of this pathology. In a chemical study, the reaction of feces is acidic (pH less than 5.5).
Another test method is to determine the content of carbohydrates in feces. Exceeding their value by 0.25% is typical for lactase deficiency. Despite the widespread use, this method is not the most accurate, since it does not allow you to determine which carbohydrates are present in the feces. nine0003
Important!
Whenever lactose intolerance is suspected, a specialist should be consulted. He will prescribe examinations that will allow you to say if the child has lactose intolerance, or if the symptoms are not associated with this condition.
Other methods are used in difficult cases. For example, a specific breath test based on determining the concentration of hydrogen in exhaled air after a load of lactose. The advantage of this method is its simplicity, the disadvantage is the possibility of false positive results and the impossibility of determining the degree of lactase deficiency. nine0003
The advantage of this method is its simplicity, the disadvantage is the possibility of false positive results and the impossibility of determining the degree of lactase deficiency. nine0003
Lactose curve is another test for lactose intolerance. Normally, lactose, under the action of the lactase enzyme, breaks down into simpler sugars, in particular, glucose. Subsequently, glucose is absorbed through the intestinal wall and enters the bloodstream. Accordingly, the determination of the level of glucose in the blood on an empty stomach and after taking lactose makes it possible to judge the breakdown of the latter under the influence of the lactase enzyme. If the rise in blood glucose levels after a lactose load is less than 20%, one should think about the insufficiency of this enzyme. nine0003
Reliable but rarely used methods for detecting lactose intolerance include intestinal biopsy and genetic testing.
A biopsy is an examination of cells in the lining of the small intestine.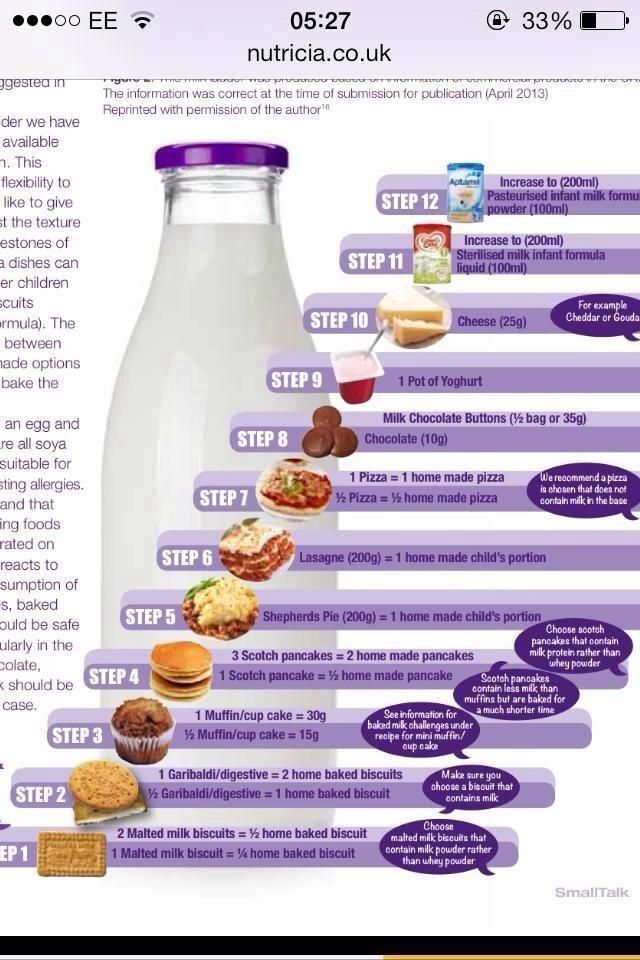 Intestinal tissue is taken during endoscopic examination. In the tissues obtained, the activity of intestinal digestion and absorption using enzymes is determined. This analysis for lactase deficiency is a reference. However, it is difficult to perform, invasive and expensive, so it is used quite rarely. nine0003
Intestinal tissue is taken during endoscopic examination. In the tissues obtained, the activity of intestinal digestion and absorption using enzymes is determined. This analysis for lactase deficiency is a reference. However, it is difficult to perform, invasive and expensive, so it is used quite rarely. nine0003
Diagnosis of lactase deficiency also includes a number of genetic tests to determine the defect in the genes responsible for the production of lactase.
Parents' attention to the health of the crumbs, knowledge of how lactase deficiency manifests itself, timely access to a specialist, effective diagnosis and strict adherence to recommendations will effectively cope with lactase deficiency and improve the health of the child.
Lactase deficiency - articles from the specialists of the clinic "Mother and Child"
what is it
The main food of babies is milk (breast or formula). It contains many different nutrients (proteins, fats, carbohydrates), which, with the help of special digestive enzymes, are broken down into simple components and digested.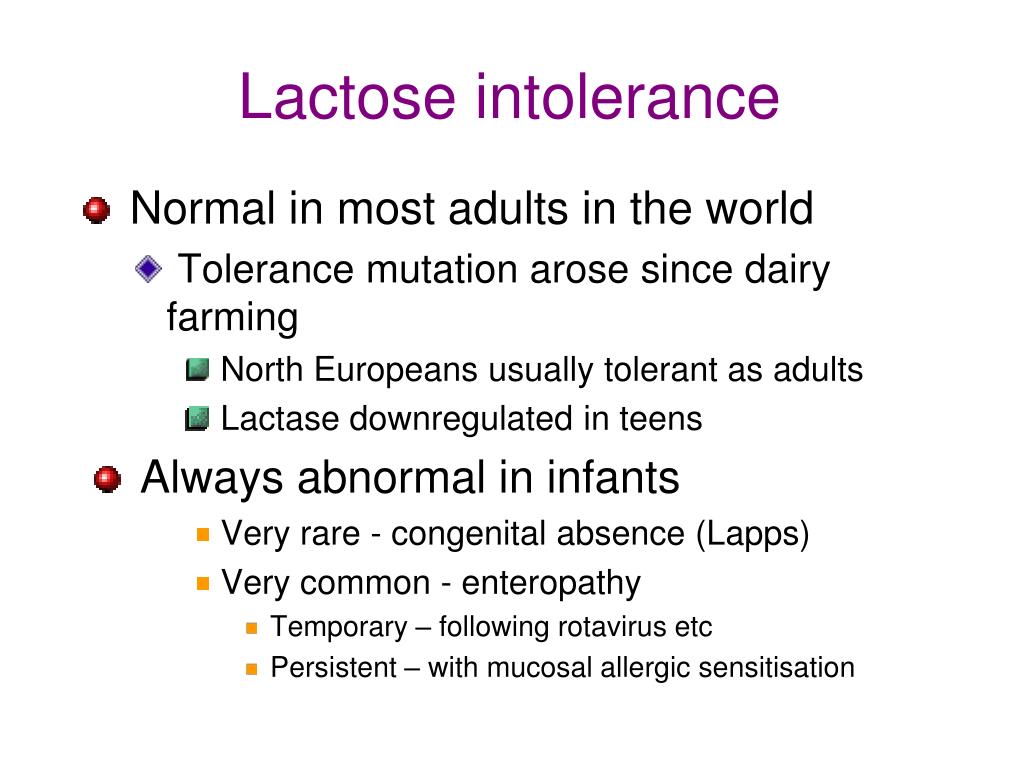 But in young children, the gastrointestinal tract is still immature, there are few enzymes in it, others are not at all or they are not yet working at full capacity. When the baby grows up, there will be more enzymes, the digestive system will mature, but for now there may be various problems with it. nine0003
But in young children, the gastrointestinal tract is still immature, there are few enzymes in it, others are not at all or they are not yet working at full capacity. When the baby grows up, there will be more enzymes, the digestive system will mature, but for now there may be various problems with it. nine0003
All milk (women's, cow's, goat's, artificial mixtures) and dairy products contain the carbohydrate lactose, also called "milk sugar". In order for lactose to be absorbed, the lactase enzyme must break it down, but if the child has little or no lactase enzyme, then lactose is not broken down and remains in the intestine. As a result, there is always a large amount of milk sugar in the intestines, which begins to ferment, and where there is fermentation, conditionally pathogenic flora actively reproduces. What we feel during fermentation: intestinal motility increases (it rumbles), plus gas formation increases (the stomach swells). But in an adult, this is usually a one-time situation due to some inaccuracies in nutrition, and it quickly passes. But in babies, everything is different, especially since they lack the enzyme not once, but constantly. What it looks like: The milk sugar lactose retains water, hence loose stools. In the child’s stomach, “rumbles and boils”, colic begins, the stool becomes frothy, greens, mucus and even blood may appear in it. If at first the stool was liquid, then constipation appears, and all this changes in a circle: yesterday there was diarrhea, today and tomorrow there is no stool at all, the day after tomorrow it is liquid again. And the most unpleasant thing is endless colic and endless crying, there is no rest for both the parents themselves and the baby. Mom at some point notices that the baby is crying just after feeding, and then a variety of advice falls upon her. “Your milk is bad, better give the mixture,” says the beloved mother-in-law. “Only breasts and nothing else!” - advise breastfeeding gurus. As a result, the mother tries one thing or the other, but neither breast milk nor artificial mixture gives relief to the child.
But in babies, everything is different, especially since they lack the enzyme not once, but constantly. What it looks like: The milk sugar lactose retains water, hence loose stools. In the child’s stomach, “rumbles and boils”, colic begins, the stool becomes frothy, greens, mucus and even blood may appear in it. If at first the stool was liquid, then constipation appears, and all this changes in a circle: yesterday there was diarrhea, today and tomorrow there is no stool at all, the day after tomorrow it is liquid again. And the most unpleasant thing is endless colic and endless crying, there is no rest for both the parents themselves and the baby. Mom at some point notices that the baby is crying just after feeding, and then a variety of advice falls upon her. “Your milk is bad, better give the mixture,” says the beloved mother-in-law. “Only breasts and nothing else!” - advise breastfeeding gurus. As a result, the mother tries one thing or the other, but neither breast milk nor artificial mixture gives relief to the child. Colic, crying and problems with the stomach and stool continue. The parents are in a panic because they don't understand what is going on. In fact, this is a typical picture of bright lactase deficiency (LN), or insufficient production of the lactase enzyme. nine0051 various reasons
Colic, crying and problems with the stomach and stool continue. The parents are in a panic because they don't understand what is going on. In fact, this is a typical picture of bright lactase deficiency (LN), or insufficient production of the lactase enzyme. nine0051 various reasons
There are several types of lactase deficiency, and it is with them that confusion arises.
Congenital lactase deficiency is a genetic and very rare disease (one case in several thousand newborns), it is difficult to confuse it with something, since it is very difficult. The diagnosis is made in the maternity hospital or in the first days after birth, the child does not have lactase at all, he quickly loses weight, he is immediately started to be fed intravenously or through a tube. Some experts (but not doctors) on breastfeeding read once that congenital lactase deficiency is an extremely rare disease, and that’s all - they further began to assure young mothers: “In fact, LN is extremely rare, you don’t have it, you don’t need to listen to doctors ", etc.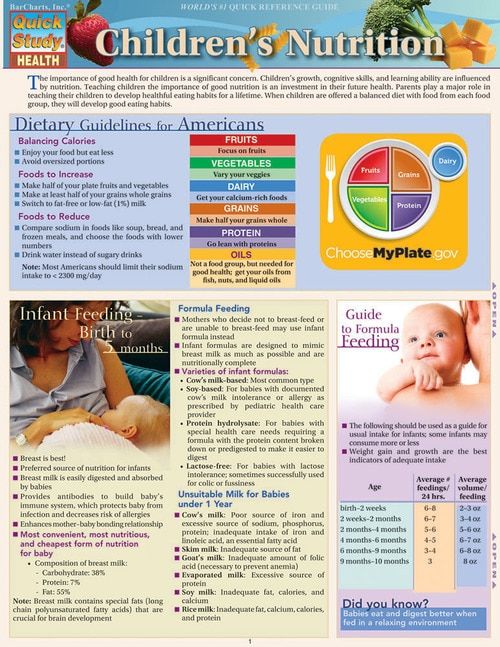 Yes, congenital LN is a rare disease, but the key word here is "congenital", and there are other types of lactase deficiency. nine0003
Yes, congenital LN is a rare disease, but the key word here is "congenital", and there are other types of lactase deficiency. nine0003
Transient lactase deficiency in infants . And this is exactly the condition that occurs very often. The baby was born, and so far he still has little lactase enzyme, plus little normal intestinal microflora. Hence the colic, and loose stools, and mucus, and greenery, and crying, and the nerves of the parents. After some time, the child's digestive system will fully mature, all enzymes will begin to work actively, the intestines will be populated with what is needed, and "lactase deficiency" will disappear. Therefore, such a LN is called "transient", that is, temporary, or passing. It passes for someone a month after birth, for someone longer - after six to seven months, and there are children in whom lactase deficiency completely disappears only by the age of one. nine0003
Secondary lactase deficiency. This condition appears if a person has had some kind of intestinal infection, and it does not matter if it is an adult or a baby.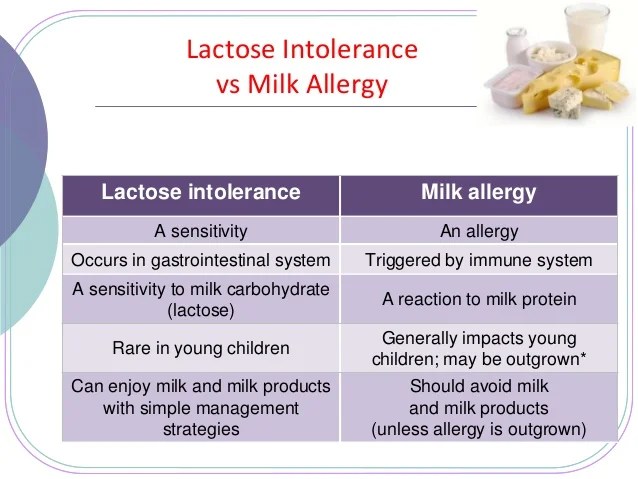 For some time after the illness, the child does not tolerate milk (any), and then with proper nutrition and sometimes even without treatment, everything quickly passes.
For some time after the illness, the child does not tolerate milk (any), and then with proper nutrition and sometimes even without treatment, everything quickly passes.
Lactase deficiency in adults. There are people in whom the lactase enzyme begins to be lacking only in adulthood, this happens for various reasons: for some, lactase ceases to be produced in the right amount after some kind of illness, for other people, the activity of this enzyme simply fades over time by itself. yourself. As a result, at some age, a person begins to tolerate milk and dairy products poorly, although before that everything was fine. The symptoms are the same as in babies: he drank milk and after that the stomach rumbles, boils, and the stool is liquid. Sooner or later, a person realizes that milk is not his product, and simply stops drinking it in its pure form. nine0051 what to do
If there is transient lactase deficiency, then what to do with it? First you need to understand if it exists at all. Why does the child have problems with the stomach, stool, why does he cry all the time? Is it neurology, common colic, errors in the mother's diet, an inappropriate mixture (if the baby is bottle-fed), improper breastfeeding technique, lactase deficiency, or a reaction to the weather? It can be difficult to figure it out right away, but if the tests show that there is lactase deficiency, then it is most likely in it. Now what to do next - treat it, wait for the enzymes to mature, or something else? Firstly, everything here will depend on how much the enzyme is lacking and, therefore, on how much LN worries the child and parents. Some children lack the enzyme quite a bit, so their colic is mild and children cry quite normally. Plus, the violation of the stool is also not very bright: there are a couple of times a slightly liquefied stool, but that's all. In other children, the lack of lactase is more pronounced, the child does not cry, but simply yells after each feeding, if at first he gained weight well, then after two months the increase is minimal, problems with stools begin in parallel (day - constipation, day - diarrhea), stool sometimes green, sometimes with mucus.
Why does the child have problems with the stomach, stool, why does he cry all the time? Is it neurology, common colic, errors in the mother's diet, an inappropriate mixture (if the baby is bottle-fed), improper breastfeeding technique, lactase deficiency, or a reaction to the weather? It can be difficult to figure it out right away, but if the tests show that there is lactase deficiency, then it is most likely in it. Now what to do next - treat it, wait for the enzymes to mature, or something else? Firstly, everything here will depend on how much the enzyme is lacking and, therefore, on how much LN worries the child and parents. Some children lack the enzyme quite a bit, so their colic is mild and children cry quite normally. Plus, the violation of the stool is also not very bright: there are a couple of times a slightly liquefied stool, but that's all. In other children, the lack of lactase is more pronounced, the child does not cry, but simply yells after each feeding, if at first he gained weight well, then after two months the increase is minimal, problems with stools begin in parallel (day - constipation, day - diarrhea), stool sometimes green, sometimes with mucus. Atopic dermatitis appears on the skin (the skin is the first to react to problems with the gastrointestinal tract). Parents have no rest day or night: the baby cries - he is fed - he cries again, they try to calm him down in other ways. But nothing helps. Mom and dad are in a panic, and no one has the strength anymore. nine0003
Atopic dermatitis appears on the skin (the skin is the first to react to problems with the gastrointestinal tract). Parents have no rest day or night: the baby cries - he is fed - he cries again, they try to calm him down in other ways. But nothing helps. Mom and dad are in a panic, and no one has the strength anymore. nine0003
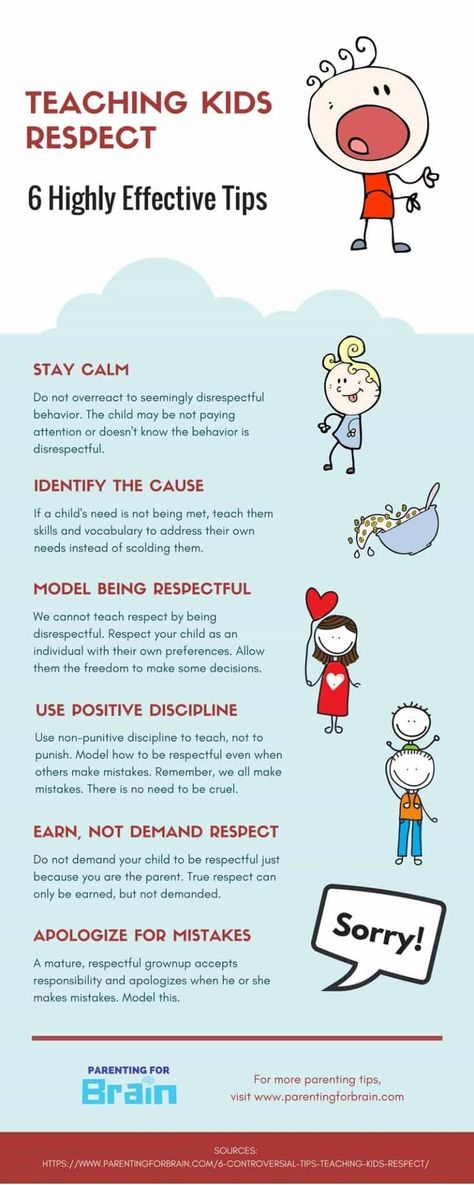
If parents see that the child may have signs of lactase deficiency, that he needs help, first of all, you need to look for a good doctor. Only an experienced pediatrician will be able to figure out why the baby has colic or green stools, what the numbers in the tests say, and what is the norm for one baby and the pathology for another. And of course, it is not necessary to cancel breastfeeding and immediately prescribe lactose-free or low-lactose artificial mixtures (even as a supplement). By itself, milk sugar lactose is very necessary for a child, when lactose is broken down, its components (glucose and galactose) go to the development of the brain, retina, for the life of normal intestinal microflora. So do not completely eliminate this sugar, you need to help it break down. With a strongly pronounced LN, the missing enzyme is given before each feeding (it has long been learned to produce and it is sold in pharmacies), with a dim clinic, its dose can be reduced. And it is also possible that there is lactase deficiency (even according to tests), but it does not need to be treated, there are almost no symptoms. nine0003
So do not completely eliminate this sugar, you need to help it break down. With a strongly pronounced LN, the missing enzyme is given before each feeding (it has long been learned to produce and it is sold in pharmacies), with a dim clinic, its dose can be reduced. And it is also possible that there is lactase deficiency (even according to tests), but it does not need to be treated, there are almost no symptoms. nine0003
But what cannot be done is to listen to non-specialists who deny either lactase deficiency itself or its treatment. They see the cause of all problems with the child's stomach and stool either in the wrong technique of breastfeeding, or partially admit that there is immaturity of the enzyme, but this is natural and will pass by itself. Yes, for some, LN is expressed easily and will pass quickly, but what about those parents whose child yells day and night, covered with a crust from atopic dermatitis and stopped gaining weight? Wait for the time to come and the enzymes to mature? Alas, with pronounced lactase deficiency (even if transient), enterocytes (intestinal cells) often suffer, so it is simply necessary to help such a child.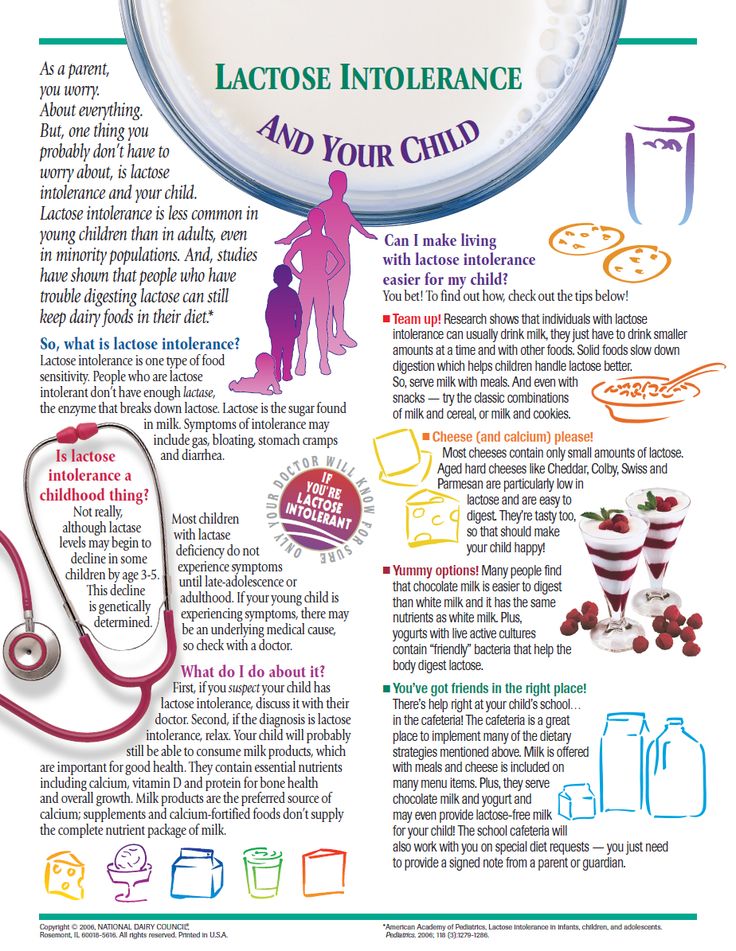 nine0051 If you see that your baby has signs of lactase deficiency, look for a doctor who is committed to maintaining breastfeeding and has extensive experience. He will definitely help to find out why the baby is crying, why he has a stomach ache or has problems with stool. And then the life of the parents and the child will return to normal.
nine0051 If you see that your baby has signs of lactase deficiency, look for a doctor who is committed to maintaining breastfeeding and has extensive experience. He will definitely help to find out why the baby is crying, why he has a stomach ache or has problems with stool. And then the life of the parents and the child will return to normal.
"Transient" (temporary) lactase deficiency in someone passes a month after birth, in someone longer - after six to seven months, and there are children in whom lactase deficiency completely disappears only by the age of one nine0051 If the tests show that there is a lactase deficiency, then the matter is most likely in it.
Milk sugar lactose is very necessary for a child: when lactose is broken down, its components (glucose and galactose) go to the development of the brain, retina, for the life of normal intestinal microflora
Parent Guide
1. In infants, transient (temporary) lactase deficiency is most common.