Being sick in pregnancy
Vomiting and morning sickness - NHS
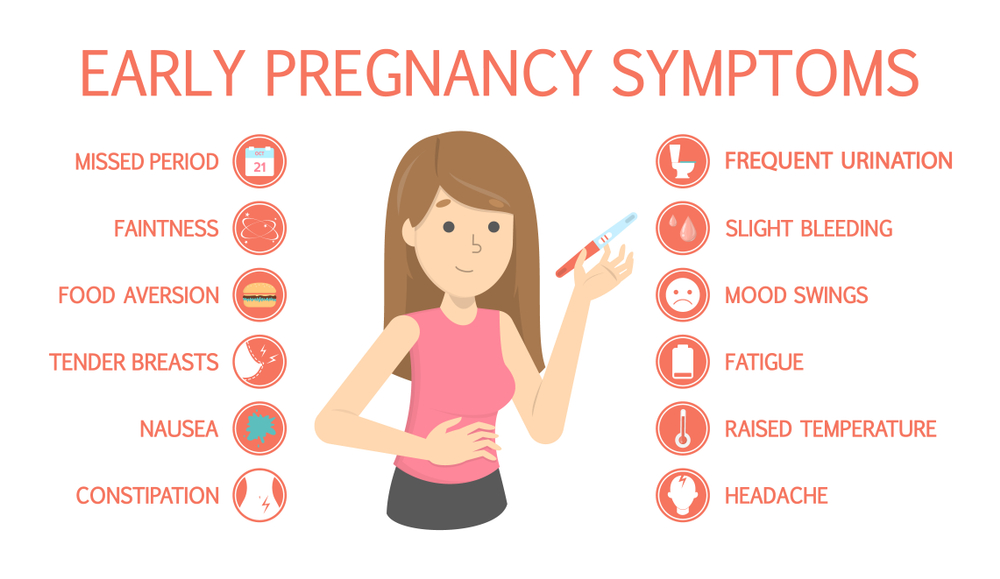
Nausea and vomiting in pregnancy, often known as morning sickness, is very common in early pregnancy.
It can affect you at any time of the day or night or you may feel sick all day long.
Morning sickness is unpleasant, and can significantly affect your day-to-day life. But it usually clears up by weeks 16 to 20 of your pregnancy and does not put your baby at any increased risk.
There is a chance of developing a severe form of pregnancy sickness called hyperemesis gravidarum. This can be serious, and there's a chance you may not get enough fluids in your body (dehydration) or not get enough nutrients from your diet (malnourishment). You may need specialist treatment, sometimes in hospital.
Sometimes urinary tract infections (UTIs) can also cause nausea and vomiting. A UTI usually affects the bladder, but can spread to the kidneys.
Non-urgent advice: Call your midwife, GP or 111 if:
you're vomiting and:
- have very dark-coloured urine or have not had a pee in more than 8 hours
- are unable to keep food or fluids down for 24 hours
- feel severely weak, dizzy or faint when standing up
- have tummy (abdominal) pain
- have a high temperature
- vomit blood
- have lost weight
Treatments for morning sickness
Unfortunately, there's no hard and fast treatment that will work for everyone’s morning sickness. Every pregnancy will be different.
But there are some changes you can make to your diet and daily life to try to ease the symptoms.
If these do not work for you or you're having more severe symptoms, your doctor or midwife might recommend medicine.
Things you can try yourself
If your morning sickness is not too bad, your GP or midwife will initially recommend you try some lifestyle changes:
- get plenty of rest (tiredness can make nausea worse)
- avoid foods or smells that make you feel sick
- eat something like dry toast or a plain biscuit before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones if the smell of hot meals makes you feel sick
- drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting)
- eat foods or drinks containing ginger – there's some evidence ginger may help reduce nausea and vomiting (check with your pharmacist before taking ginger supplements during pregnancy)
- try acupressure – there's some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
Find out more about vitamins and supplements in pregnancy
Anti-sickness medicine
If your nausea and vomiting is severe and does not improve after trying the above lifestyle changes, your GP may recommend a short-term course of an anti-sickness medicine, called an antiemetic, that's safe to use in pregnancy.
Often this will be a type of antihistamine, which are usually used to treat allergies but also work as medicines to stop sickness (antiemetic).
Antiemetics will usually be given as tablets for you to swallow.
But if you cannot keep these down, your doctor may suggest an injection or a type of medicine that's inserted into your bottom (suppository).
See your GP if you'd like to talk about getting anti-sickness medication.
Risk factors for morning sickness
It's thought hormonal changes in the first 12 weeks of pregnancy are probably one of the causes of morning sickness.
But you may be more at risk of it if:
- you're having twins or more
- you had severe sickness and vomiting in a previous pregnancy
- you tend to get motion sickness (for example, car sick)
- you have a history of migraine headaches
- morning sickness runs in the family
- you used to feel sick when taking contraceptives containing oestrogen
- it's your first pregnancy
- you're obese (your BMI is 30 or more)
- you're experiencing stress
Visit the pregnancy sickness support site for tips for you and your partner on dealing with morning sickness.
Find maternity services near you
Sign up for pregnancy emails
Sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Video: how can I cope with morning sickness?
In this video, a midwife gives advice on how to deal with morning sickness during your pregnancy.
Media last reviewed: 27 February 2017
Media review due: 27 March 2020
Page last reviewed: 13 April 2021
Next review due: 13 April 2024
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 16 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- being dehydrated. Symptoms of dehydration include, feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
- low blood pressure (hypotension) when standing
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See the healthtalk.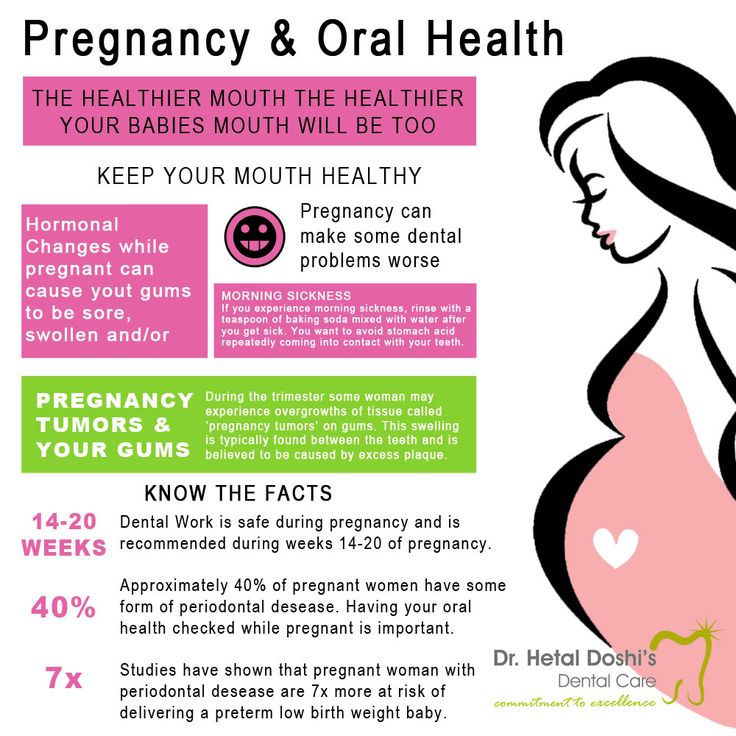 org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
What causes hyperemesis gravidarum?
It's not known what causes HG, or why some women get it and others do not. Some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given via a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
Other symptoms you may experience
Pregnancy Sickness Support is in touch with many women who have had HG, and who report having some or all of the following symptoms in addition to the main symptoms listed above:
- extremely heightened sense of smell
- excessive saliva production
- headaches and constipation from dehydration
If you experience these symptoms, you are not alone. Many women have them and they will go away when the HG stops or the baby is born.
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
You could also talk to your partner, family and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Colds during pregnancy: how to treat?
Any cold or respiratory disease in early pregnancy, during the primary formation of the fetus, can lead to unpredictable consequences and complications. The matter is complicated by the fact that most medications are absolutely contraindicated for use during gestation.
In this regard, the treatment and prevention of colds in pregnant women is an important issue, which should be approached especially responsibly! The main thesis is: be careful with medicines and apply mild preventive measures based on alternative medicine methods to avoid respiratory diseases and flu.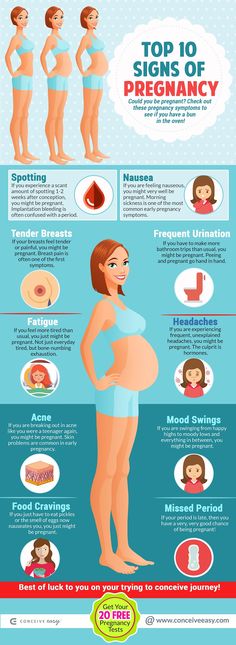 nine0003
nine0003
"One for two - immunity"
This is a very fragile system, it is not necessary to interfere in its work, but it is necessary to support and strengthen it. Pregnancy belongs to the category of special, albeit temporary, conditions during which a woman needs additional protection.
This issue will help simple recommendations that are available to everyone:
• During the period of frequent weather changes, it is necessary to dress warmer, paying special attention to footwear. nine0017 • During an epidemic, it is better for a pregnant woman to refrain from being in crowded places - transport, metro, shops and hospitals. If there is an urgent need, to prevent possible infection, a protective respiratory mask should be worn before leaving the house.
• Be especially careful about hygiene after visiting the street and public places. Upon returning home, the first thing to do is wash your hands thoroughly.
Interesting: More than 90% of all acute respiratory infections are caused by viruses, about 10% are bacteria and other pathogens. Accordingly, any soap can be used, not necessarily antibacterial.
• Before going outside, you can lubricate the nasal mucosa with oxolin ointment. Upon returning home, flush the upper respiratory tract with soda solution.
• Rationalization of nutrition and intake of vitamins will strengthen the immune defense. It is especially useful to eat fruits and vegetables that are enriched with vitamins and have not undergone heat treatment. nine0003
Interesting: our grandmothers used to say: in order not to get sick, you need to drink chicken broth! Strange, but until recently, scientists did not attach much importance to this prophylactic. Pulmonologist Stefan Rennard decided to find out if this was true or not. The professor conducted a study and proved that the use of chicken broth affects the mobility of neutrophils, leukocytes that protect the body from infections and activate the immune system.
- Vitamins can be taken using ready-made pharmaceutical multivitamin complexes. Before choosing a drug, you should consult your doctor. nine0035
- Compliance with the regimen and duration of sleep - at least 9 hours a day. The possibility of psychotraumatic situations should be minimized.
- Maintaining cleanliness in the living quarters (ventilation, wet cleaning).
- Air humidification is an important aspect in the prevention of influenza and respiratory diseases. If air conditioners or heaters are used in the pregnant woman's house, it would be best to purchase a mechanical humidifier. nine0035
Medications for prevention
- Grippferon - a drug in the form of drops for the nose, which provides prevention and treatment of influenza, is not contraindicated for pregnant and lactating women. The medicine stimulates an increase in immunity, has a pronounced antiviral effect that can protect against colds, infections and influenza varieties.
- Ascorbic acid - can be used as a separate source of vitamin C in a synthetic version, with a reduced daily intake from food. Ascorbic acid not only prevents infection, but also fights viruses that have already entered the body of a woman. nine0035
- Viferon - nasal ointment, which is prescribed for the prevention of influenza and respiratory infections during an epidemic. The ointment has protective and immunomodulatory effects, and also allows you to deal with disorders that are already occurring in the body at the time of use. Viferon in the form of a nasal ointment has no contraindications for use in pregnant women at any time, including the first trimester.
- Aquamaris is a natural drug in the form of a nasal spray that allows you to moisturize the nasal mucosa, thereby reducing the risk of influenza viruses entering the nasal cavity. nine0035
I would like to say a few words about such a method of prevention as vaccination. Most often, the expectant mother may be at risk of infection due to the annual influenza epidemic. This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media. Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus. nine0003
Most often, the expectant mother may be at risk of infection due to the annual influenza epidemic. This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media. Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus. nine0003
The most dangerous consequence of influenza in a pregnant woman is threatened miscarriage or premature birth!
It is quite natural that expectant mothers often wonder whether or not to vaccinate.
Studies have concluded that the use of inactivated ("killed") influenza vaccines does not have a teratogenic effect on the fetus and does not harm the health of a pregnant woman. After consulting with your doctor about such an inoculation, you can come to an optimal solution. nine0073 If an influenza epidemic is inevitable, and the pregnant woman has no contraindications, then the vaccine should be given. If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of the mother reduces the risk of influenza infection of the born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy. nine0003
After consulting with your doctor about such an inoculation, you can come to an optimal solution. nine0073 If an influenza epidemic is inevitable, and the pregnant woman has no contraindications, then the vaccine should be given. If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of the mother reduces the risk of influenza infection of the born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy. nine0003
In the period of a planned pregnancy, a flu shot is given 1 month before it: the formation of immunity occurs 2-4 weeks. Protection after vaccination lasts about a year.
If infection does occur, action should be taken immediately if at least one symptom of the disease is detected. The health of a pregnant woman and her unborn child depends entirely on her responsibility and respect for her own body.
Proven folk remedies will be used first. Since pregnant women cannot steam their legs, steam their hands, and this will facilitate nasal breathing. Bundle up, put on woolen socks and crawl under the covers: warmth, peace and sleep are good for colds. Do not forget to drink plenty of water - hot green tea with lemon and honey, lime blossom tea, cranberry juice, rosehip broth, dried fruit compote. Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning. nine0003
Various hot milk drinks are also suitable. Honey can be added to milk, and it is best to boil it on onions. It must be emphasized right away that not all herbs for colds during pregnancy can be used. Here is a list of medicinal plants that are contraindicated: aloe, anise, barberry, elecampane (grass and root), sweet clover, oregano, St. John's wort, strawberries (leaves), viburnum (berries), raspberries (leaves), lemon balm, lovage, wormwood, licorice root), celandine, sage. Accordingly, preparations containing these plants should not be taken. nine0003
Accordingly, preparations containing these plants should not be taken. nine0003
The use of medicines for colds during pregnancy must be treated with great care!
It is contraindicated to use the following drugs : Pertussin, Tussin plus, Joset, Glycodin, Ascoril, Travisil, Broncholitin, ACC, Grippeks, Codelac, Terpinkod. Do not use lozenges and lozenges for sore throat or cough are also undesirable due to the likelihood of allergic reactions.
Spray Pinosol, judging by the components indicated in the instructions, is not dangerous during pregnancy. However, the essential oils contained in the preparation - pine, peppermint, eucalyptus, thymol, guaiazulene (wormwood oil) - can lead to an allergic reaction with swelling of the nasal mucosa. nine0003
Viferon suppositories are allowed to be used only after 14 weeks from the start of conception. This drug contains recombinant human interferon alpha-2, ascorbic acid and alpha-tocopherol acetate and has antiviral, immunomodulatory and antiproliferative effects.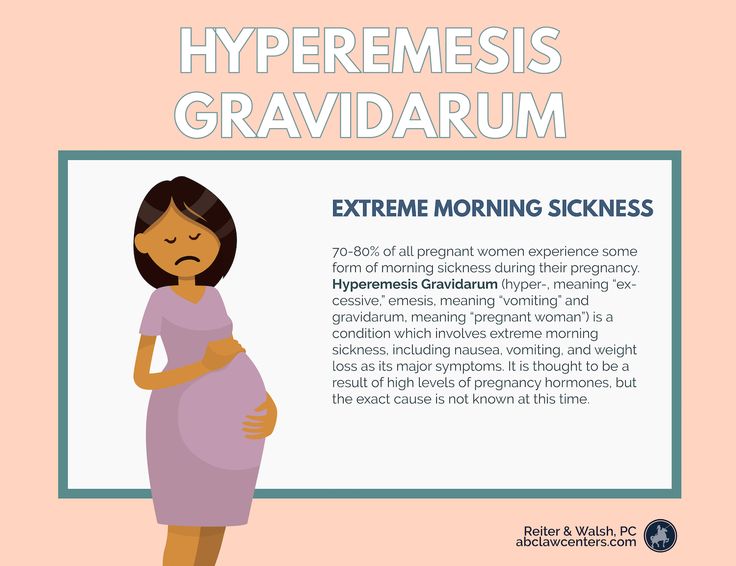 It is used in the treatment of various infectious and inflammatory diseases in adults and children (including newborns). In the form of an ointment, Viferon is used to treat herpetic lesions of the skin and mucous membranes. The ointment is applied in a thin layer to the affected areas of the skin 3-4 times a day for 5-7 days. nine0003
It is used in the treatment of various infectious and inflammatory diseases in adults and children (including newborns). In the form of an ointment, Viferon is used to treat herpetic lesions of the skin and mucous membranes. The ointment is applied in a thin layer to the affected areas of the skin 3-4 times a day for 5-7 days. nine0003
The homeopathic preparation Stodal, which includes predominantly herbal ingredients, acts on various types of cough and has an expectorant and bronchodilator effect.
Viburkol - homeopathic suppositories - have analgesic, anti-inflammatory, sedative, antispasmodic action. They are prescribed in the complex therapy of acute respiratory viral infections and other uncomplicated infections (including in newborns), as well as in inflammatory processes of the upper respiratory tract and inflammatory diseases of the genitourinary system. nine0003
So, you can try to eliminate a slight ailment on your own, but there are conditions under which you need to call a doctor at home:
- Prolonged fever;
- Myalgia, fatigue, fatigue, general malaise;
- Difficulty breathing, nasopharyngeal lumps and dry or wet barking cough;
- A pregnant woman is troubled by severe pressing headache.
 nine0035
nine0035
In conclusion, I would like to emphasize the importance of treating chronic diseases before pregnancy, a healthy lifestyle during childbearing and following all doctor's orders.
I wish expectant mothers and their loved ones to try to maintain a good mood: optimists live longer and happier, they are more productive. Remember your victories and pleasant moments more often and everything will be fine!
Colds ARI, SARS during pregnancy, consequences, treatment
Colds can suddenly take our wonderful future mothers by surprise.
What should I do if I get a cold (ARI/ARVI) during pregnancy?
Is it possible to protect yourself from SARS?
Which medicines are allowed and which are not?
Is it dangerous for the baby?
Pregnancy is a wonderful state, but, unfortunately, even this wonderful period in a woman’s life can be overshadowed by exacerbation of pre-existing chronic diseases of the respiratory system (almost 10% of the population suffers from one or another pathology of the respiratory organs and do not go to the doctor for treatment ). nine0003
nine0003
What is the danger of neglect in acute respiratory infections/ARVI during pregnancy
- The causative agents of viral and infectious diseases can contribute to miscarriage, increased blood loss during childbirth.
- Viruses can also activate existing in the body and other "dormant" infection, contribute to the development of inflammatory diseases of the internal genital organs.
- There is no particular predisposition to infection in pregnant women, but respiratory diseases of an infectious and viral nature in pregnant women are often more severe and give much more complications if treatment is not started on time. nine0035
- The most common diseases in pregnant women are SARS and influenza.
- Colds are dangerous during pregnancy, both in the 1st trimester, 2nd trimester, and 3rd trimester.
ARVI is an acute respiratory viral infection, i.e. The source of the disease is viruses that a sick person releases in large quantities when coughing, sneezing, talking. We are especially prone to viral infections during the cold season, as well as during the transitional periods of autumn and spring - when it is hot during the day, cold in the morning, and sometimes we dress completely inappropriate for the weather. nine0003
We are especially prone to viral infections during the cold season, as well as during the transitional periods of autumn and spring - when it is hot during the day, cold in the morning, and sometimes we dress completely inappropriate for the weather. nine0003
The onset of SARS is usually gradual with a general malaise, lethargy, slight fever, and a runny nose or sore throat.
Influenza, unlike SARS, is more severe and poses a great danger to both mother and fetus. Influenza epidemics recur almost every year, during which 30-40% of the population falls ill.
This is an acute viral disease transmitted by airborne droplets. The influenza virus penetrates through the respiratory tract, affects the mucous membrane, increases the permeability of the walls of blood vessels. The flu virus lowers the immune system, which can exacerbate chronic diseases. The onset of influenza is acute, sudden: 30 minutes ago everything seems to be fine, but now it’s temperature, chills, fever. nine0003
nine0003
What to do if you get SARS during pregnancy?
Treat for sure!!!
Do not hope that it will go away on its own and somehow manage to lie down. Even with a slight malaise, the likelihood of complications in a pregnant woman is high.
Be sure to visit a doctor, a competent therapist or general practitioner will give you comprehensive recommendations on drug therapy, as well as the use of home remedies that will not harm you and your baby. nine0003
Do not self-medicate, antiviral drugs, herbs, lozenges, antibiotics and antibacterial drugs should not be taken without a doctor's prescription. Your body during pregnancy may react differently than in normal life.
Is it possible to protect yourself from SARS during pregnancy?
SARS prevention measures are simple and affordable:
- dress for the season and the weather. nine0035
- Proper balanced nutrition, vitamin intake and more positive emotions are of great importance.

- After coming back from the street or working at home, it is a good idea to gargle with sea water and flush the nose.
- Before work, lubricate the nasal cavity with oxolin ointment or peach oil.
- At work and at home, take care of proper air humidification (ionizers, humidifiers)
- Important! Do not forget about regular walks in the fresh air, a full sexual life (if there are no contraindications) and sports (taking into account the physiological characteristics of the pregnant woman)
What medicines can be taken during pregnancy if you have ARVI?
- Medications are prescribed individually, based on the situation, the doctor selects.
- You can bring down the temperature with Paracetamol (both tablets and suppositories).
- Absolutely everyone is shown a warm alkaline fortified drink.
Is SARS dangerous for a baby?
- If you start treatment on time and be under the supervision of a doctor, your baby will not be harmed by a cold.