Second trimester pains
The Honeymoon Period, What to Expect
Written by Stephanie Watson
In this Article
- Changes in Your Body
- Emergency Symptoms
- Baby’s Growth in the Second Trimester
- Second Trimester Tips for Twins
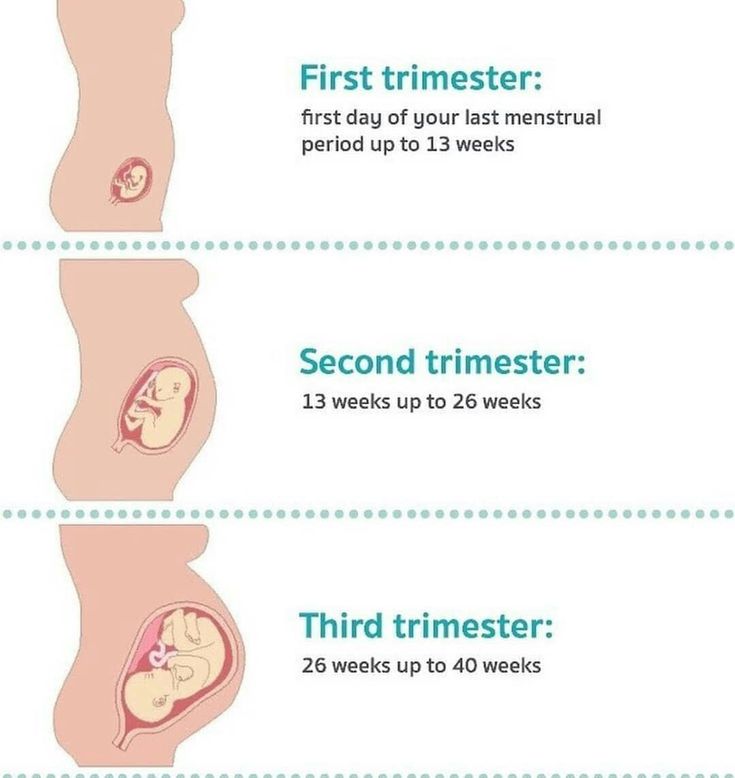
The second trimester of your pregnancy lasts from week 13 to 28, or months 4, 5, and 6. It’s the middle phase of pregnancy, when you may start to see your “baby bump” and feel your baby move for the first time.
As you enter your second trimester of pregnancy, the morning sickness and fatigue you may have felt during the last 3 months should fade.
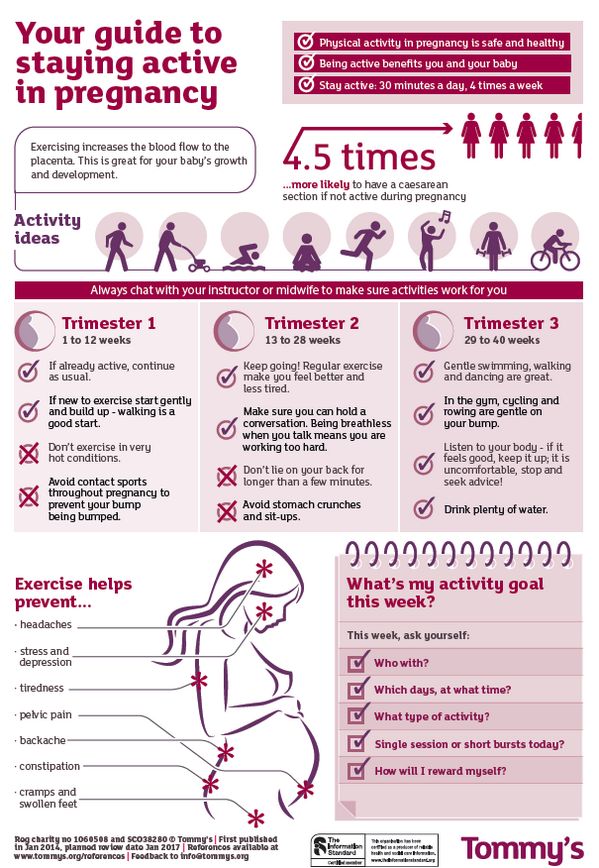
The second trimester is, for many women, the easiest 3 months of pregnancy. Take the time now, while you're feeling better and your energy is up, to start planning for your baby's arrival.
During the second trimester, your baby is growing quickly. Between your 18th and 22nd week of pregnancy you'll have an ultrasound so your doctor can see how your baby is progressing. You also can learn the sex of your baby, unless you'd rather be surprised. And if you’re having twins, you might find that out during this trimester.
Although you should be feeling better now, big changes are still taking place inside your body. Here's what you can expect.
Changes in Your Body
Achiness in your lower abdomen. In your second trimester, you may notice some cramps or aches in your lower belly. Cramps happen because as your uterus expands during pregnancy, it puts pressure on nearby muscles and ligaments. During your second trimester, your round ligament muscle often cramps as it stretches. You feel it as a dull ache in your lower abdomen, but you may also feel sharp stabs of pain. Minor cramps are normal, and may be caused by constipation, gas, or even sex. To relieve the aches, try a warm bath, relaxation exercises, changing your body’s position, or pressing a hot water bottle wrapped in a towel to your lower belly.
Backache. The extra weight you've gained in the last few months is starting to put pressure on your back, making it achy and sore. To ease the pressure, sit up straight and use a chair that provides good back support. Sleep on your side with a pillow tucked between your legs. Avoid picking up or carrying anything heavy. Wear low-heeled, comfortable shoes with good arch support. If the pain is really uncomfortable, ask your partner to rub the sore spots, or treat yourself to a pregnancy massage.
The extra weight you've gained in the last few months is starting to put pressure on your back, making it achy and sore. To ease the pressure, sit up straight and use a chair that provides good back support. Sleep on your side with a pillow tucked between your legs. Avoid picking up or carrying anything heavy. Wear low-heeled, comfortable shoes with good arch support. If the pain is really uncomfortable, ask your partner to rub the sore spots, or treat yourself to a pregnancy massage.
Bleeding gums. About half of pregnant women develop swollen, tender gums. Hormone changes are sending more blood to your gums, making them more sensitive and causing them to bleed more easily. Your gums should go back to normal after your baby is born. In the meantime, use a softer toothbrush and be gentle when you floss, but don't skimp on dental hygiene. Studies show that pregnant women with gum disease (periodontal disease) may be more likely to go into premature labor and deliver a low-birth-weight baby.
Braxton-Hicks contractions. You may start to feel the muscles in your uterus tighten for a minute or two during the second trimester. These aren’t real contractions or signs of labor, but a normal symptom. They may come and go at random, and may feel irregular in their rhythm and strength. These muscle contractions often cause discomfort more than pain. Sex, intense exercise, dehydration, a full bladder, or even someone touching your baby bump can trigger Braxton-Hicks contractions. You can use these contractions to practice your breathing techniques for labor. To help yourself relax, take a warm bath, sip some warm herbal tea, change your body’s position, or drink more water.
Breast enlargement. Much of the breast tenderness you experienced during the first trimester should be wearing off, but your breasts are still growing as they prepare to feed your baby. Going up a bra size (or more) and wearing a good support bra can make you feel more comfortable.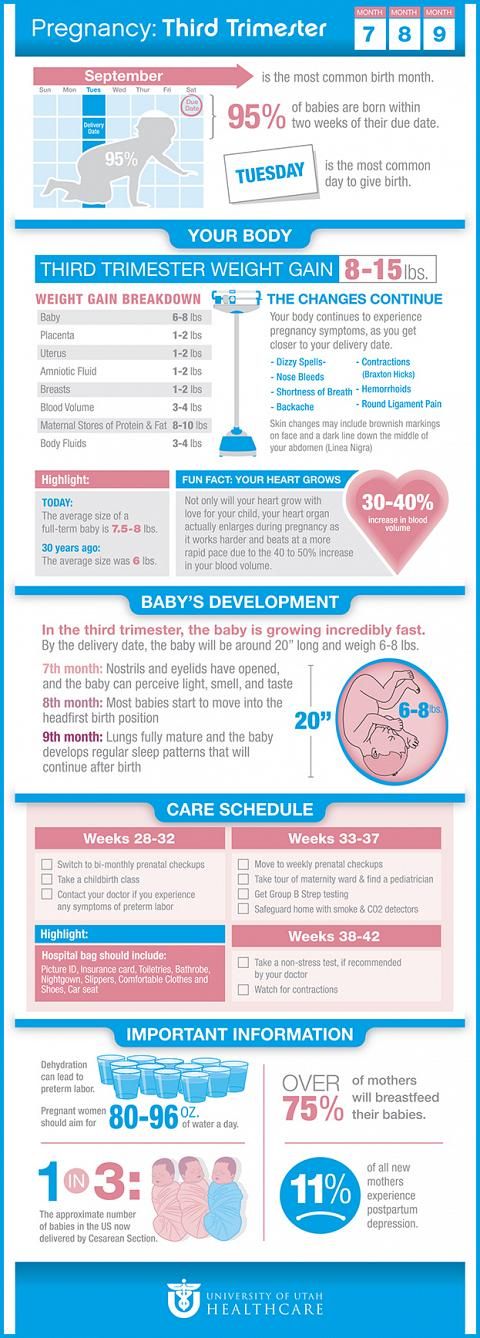
Congestion and nosebleeds. Hormonal changes cause the mucus membranes lining your nose to swell, which can lead to a stuffy nose and make you snore at night. These changes may also make your nose bleed more easily. Before using a decongestant, check with your doctor. Saline drops and other natural methods may be safer ways to clear congestion during pregnancy. You can also try using a humidifier to keep the air moist. To stop a nosebleed, keep your head up straight (don't tilt it back) and apply pressure to the nostril for a few minutes until the bleeding stops.
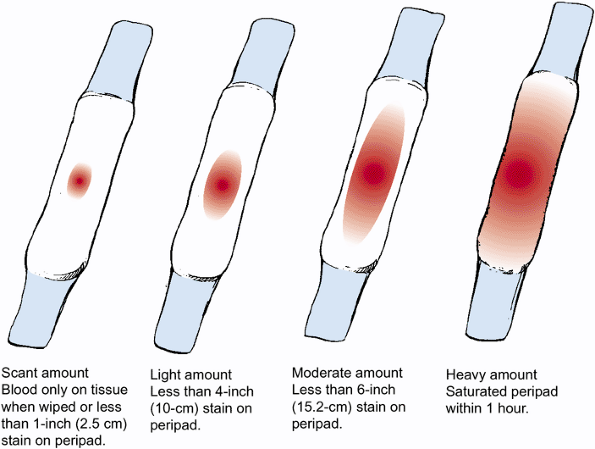
Discharge. It's normal to see a thin, milky white vaginal discharge (called leukorrhea) early in your pregnancy. You can wear a panty liner if it makes you feel more comfortable, but don't use a tampon because it can introduce germs into the vagina. If the discharge is foul-smelling, green or yellow, bloody, or if there's a lot of clear discharge, call your doctor.
Dizziness. As your uterus expands during the second trimester, it presses against blood vessels and causes you to feel dizzy at times. Other causes are low blood sugar or hormone changes during pregnancy. Try not to stand for too long. Rise slowly from chairs or bed. Eat regular meals and snacks. Stay hydrated. Wear loose clothes, avoid hot showers or baths, and try not to lie flat on your back for the rest of your pregnancy. Call your doctor if you feel faint or pass out, or if you also have vaginal bleeding or abdominal pain.
Frequent urination. Your uterus will rise away from the pelvic cavity during the second trimester, giving you a brief break from having to keep going to the bathroom. Don't get too comfortable, though. The urge to go will come back during the last trimester of your pregnancy.
Hair growth. Pregnancy hormones can boost hair growth -- and not always where you want it. The hair on your head will become thicker. You may also be seeing hair in places you never had it before, including your face, arms, and back. Shaving and tweezing might not be the easiest options, but they're probably your safest bets right now. Many experts don't recommend laser hair removal, electrolysis, waxing, or depilatories during pregnancy, because research still hasn't proven that they are safe for the baby. Check to see what your doctor recommends.
You may also be seeing hair in places you never had it before, including your face, arms, and back. Shaving and tweezing might not be the easiest options, but they're probably your safest bets right now. Many experts don't recommend laser hair removal, electrolysis, waxing, or depilatories during pregnancy, because research still hasn't proven that they are safe for the baby. Check to see what your doctor recommends.
Headache. Headaches are one of the most common pregnancy complaints. Try to get plenty of rest, and practice relaxation techniques, such as deep breathing. Aspirin and ibuprofen shouldn’t be taken during pregnancy, but your doctor may say it's OK for you to take acetaminophen if you're really uncomfortable.
Heartburn and constipation. These are caused by your body making more of a hormone called progesterone. This hormone relaxes certain muscles, including the ring of muscle in your lower esophagus that normally keeps food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (such as citrus fruits). For constipation, get more fiber and drink extra fluids to keep things moving more smoothly. Physical activity will also help move things along.
To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (such as citrus fruits). For constipation, get more fiber and drink extra fluids to keep things moving more smoothly. Physical activity will also help move things along.
Hemorrhoids. Hemorrhoids are actually varicose veins -- swollen blue or purple veins that form around the anus. These veins may enlarge during pregnancy because extra blood is flowing through them and there is increased pressure on them from the growing uterus. Varicose veins can be itchy and uncomfortable. To relieve them, try sitting in a warm tub or sitz bath. Ask your doctor whether you can use an over-the-counter hemorrhoid ointment.
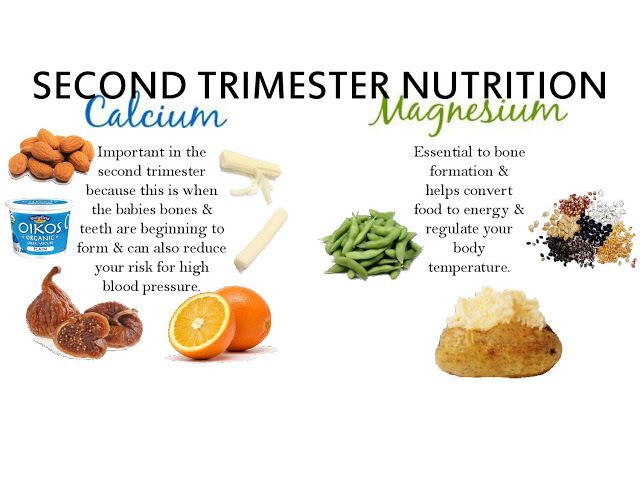
Leg cramps. You may feel muscles in your legs contract and cramp during the second trimester. This often happens at night. It’s unclear what causes them. To prevent cramps, try to stretch your leg muscles before you go to bed, get regular exercise, eat foods rich in magnesium like beans or whole grains, drink plenty of fluids, get the recommended amount of calcium, and wear comfy shoes. To ease a bout of leg cramps, stretching, ice, heat, or massage may help.
To ease a bout of leg cramps, stretching, ice, heat, or massage may help.
Quickening. By the midpoint of your pregnancy (20 weeks), you will probably have started to feel the first delicate flutters of movement in your abdomen, which is often called "quickening." If you aren't feeling your baby move yet, don't worry. Some women don't experience quickening until their sixth month of pregnancy.
Skin changes. Pregnant women often look as though they are "glowing" because changing hormone levels make the skin on the face appear flushed. An increase in the pigment melanin can also lead to brown marks on the face (often called the "mask of pregnancy") and a dark line (linea nigra) down the middle of the abdomen. All of these skin changes should fade after the baby is born. In the meantime, you can use makeup to conceal them. Your skin is also more sensitive to the sun right now, so make sure to wear a broad-spectrum (UVA/UVB protection) sunscreen with an SPF of at least 30 whenever you go outside.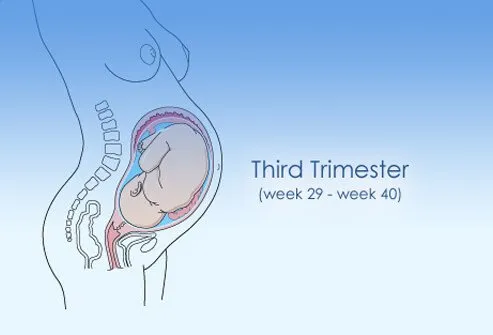 Limit your time in the sun, especially between 10 a.m. and 2 p.m., wearing long-sleeved clothes, pants, a broad-brimmed hat, and sunglasses. You may also notice thin, reddish-purple lines on your abdomen, breasts, or thighs. These stretch marks emerge as your skin expands to accommodate your growing belly. Although many creams and lotions claim to prevent or eliminate stretch marks, there is little evidence that they actually do. Using a moisturizer can help soften your skin and reduce itchiness. Most stretch marks should fade on their own after you deliver.
Limit your time in the sun, especially between 10 a.m. and 2 p.m., wearing long-sleeved clothes, pants, a broad-brimmed hat, and sunglasses. You may also notice thin, reddish-purple lines on your abdomen, breasts, or thighs. These stretch marks emerge as your skin expands to accommodate your growing belly. Although many creams and lotions claim to prevent or eliminate stretch marks, there is little evidence that they actually do. Using a moisturizer can help soften your skin and reduce itchiness. Most stretch marks should fade on their own after you deliver.
Spider and varicose veins. Your circulation has increased to send extra blood to your growing baby. That excess blood flow can cause tiny red veins, known as spider veins, to appear on your skin. These veins should eventually fade once your baby is born. Pressure on your legs from your growing baby can also slow blood flow to your lower body, causing the veins in your legs to become swollen and blue or purple. These are called varicose veins. Although there's no way to avoid varicose veins, you can prevent them from getting worse by getting up and moving throughout the day and propping up your legs on a stool whenever you have to sit for long periods of time. Wear support hose for extra support. Varicose veins should improve within 3 months after you deliver.
These are called varicose veins. Although there's no way to avoid varicose veins, you can prevent them from getting worse by getting up and moving throughout the day and propping up your legs on a stool whenever you have to sit for long periods of time. Wear support hose for extra support. Varicose veins should improve within 3 months after you deliver.
Urinary tract infections. Bacterial infections in your urinary tract or bladder, which sits on top of your uterus, are common in the second trimester. They’re caused by changes in your urinary tract or your growing uterus making it harder to empty your bladder. You may have symptoms like pain or burning when you pee, a frequent urge to pee, cloudy or smelly urine, pain during sex, lower belly pain, or traces of blood or mucus in your urine. Bladder infections can spread to your kidneys and cause early labor or low-weight babies, so see your doctor right away. They’ll give you a urinalysis and urine culture to diagnose the infection, and prescribe antibiotics to treat it.
Weight gain. Morning sickness usually diminishes by the end of the first trimester. After that, your appetite should return, and will probably grow. Although food is looking much more appetizing, be aware of how much you're eating. You only need about an extra 300 to 500 calories a day during the second trimester, and you should be gaining about 1/2 to 1 pound a week.
Emergency Symptoms
Any of these symptoms could be a sign that something is wrong with your pregnancy. Don't wait for your prenatal visit to talk about it. Call your doctor right away if you have:
- Severe abdominal pain or cramping
- Bleeding
- Severe dizziness
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain (less than 10 pounds at 20 weeks into the pregnancy)
- Jaundice
- Vomiting
- A lot of sweating
Baby’s Growth in the Second Trimester
During your second trimester, your baby grows up to 3 pounds in weight and up to 16 inches in length. Their brain and other organs grow and develop a great deal. Their heart moves 100 pints of blood a day. Their lungs are fully formed but not quite ready to breathe. And your baby can kick, move, turn around in your womb, swallow, suck, and hear your voice.
Their brain and other organs grow and develop a great deal. Their heart moves 100 pints of blood a day. Their lungs are fully formed but not quite ready to breathe. And your baby can kick, move, turn around in your womb, swallow, suck, and hear your voice.
Your baby’s eyes and ears move into the correct positions on its head. Their eyelids can open and shut. The baby sleeps and wakes up in a normal cycle. They grow eyelashes and eyebrows.
Your baby grows fingernails and toenails. The tiny fingers and toes separate. They develop distinct fingerprints and toe prints.
Hair grows on your baby’s head. They also sprout downy, fine hair all over called the lanugo. Their body is encased in a creamy, white, protective coating called the vernix caseosa, which is eventually absorbed into their skin.
Your baby’s placenta is also fully developed by this time. The placenta is an organ that gives your fetus oxygen and nutrients. It also removes waste. In the second trimester, your fetus also begins to build up fat on its body.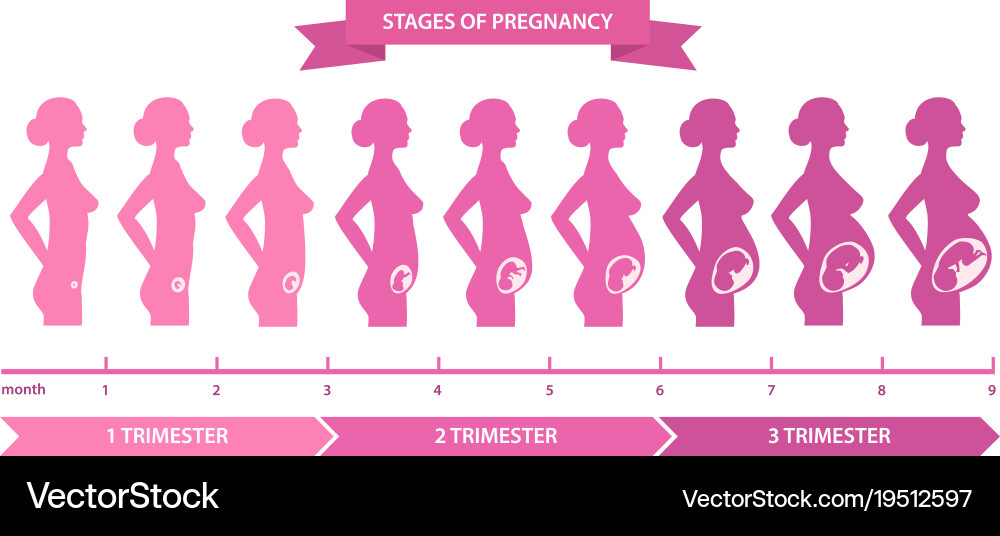
Second Trimester Tips for Twins
Carrying two? Here are some things to think about:
- Choose a doctor. Ask your OB about seeing a maternal fetal medicine (MFM) specialist, an OB who specializes in high-risk births.
- Go ahead -- nap!Don't feel guilty about taking a nap if you're tired. Even when resting, you're using 10% more energy than a woman carrying a single baby!
- Get your omega-3s. Getting enough omega-3 fatty acids is especially important when you're having twins. Like fish? Get omegas-3s from salmon, herring, sardines, and trout.
- Getting enough vitamins? Ask your doctor if a prenatal vitamin alone gives you all you need since you're carrying two.
- Don't double everything. Before you buy two of every baby gadget, wait and see what your babies like. Some babies enjoy swings and bouncy seats, and others don’t. You also won’t need an extra crib -- at least not at first.
 Your babies may sleep better when they're together.
Your babies may sleep better when they're together. - Eat for three. You need about 500 extra calories a day -- about as much as in two bowls of cereal with low-fat milk and a banana.
- Cut back on exercise? After 20 or 24 weeks, ask your doctor if you need to cut back on any types of exercise and, if so, what's still safe to do.
- Look into a breast pump. If your twins spend any time in the NICU, you may need to pump your milk at first. Having a pump ready will make this easier.
- Create a birth plan. This will let your birth team know your labor and delivery wishes. Just try to stay flexible if things don't go exactly as planned.
- Don't wait to find child care. The best caregivers and centers often have a waiting list. Start looking for child care early, especially since you'll need two slots instead of one.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Second trimester pains: Causes, symptoms, and treatment
Although all pregnancies are different, certain symptoms tend to occur in each trimester.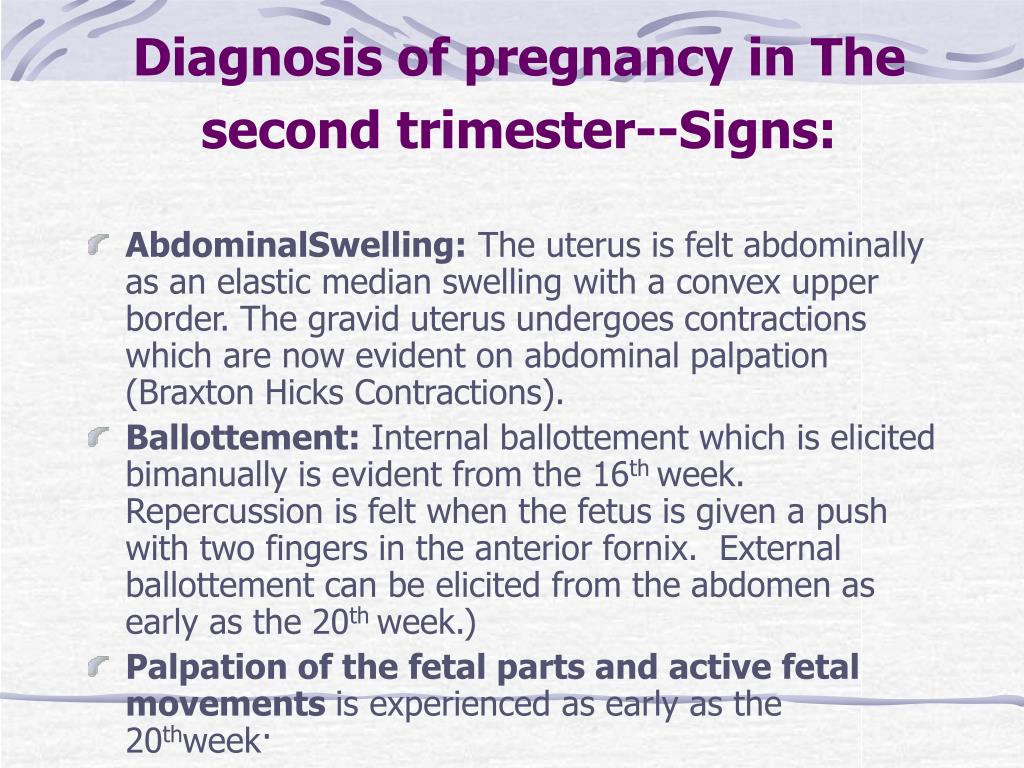 For some women, the second trimester means the end of morning sickness and fatigue, but it also means the onset of specific types of pain.
For some women, the second trimester means the end of morning sickness and fatigue, but it also means the onset of specific types of pain.
Pregnancy consists of three trimesters. The second trimester lasts from weeks 13 to 28.
In this article, learn what causes pain in the second trimester and how to find relief.
Second trimester pains are not uncommon, as the uterus and abdomen are expanding.
Increased pressure from a growing uterus, along with hormonal changes, can lead to various types of pain.
Some common causes of second trimester pains include:
Round ligament pain
Share on PinterestCommon causes of second trimester pains include round ligament pain and back pain.The round ligaments support the uterus and hold it in place. During pregnancy, the expanding uterus causes these ligaments to stretch.
Round ligament pain often starts as the belly grows in the second trimester.
Symptoms of round ligament pain include:
- a sharp or aching sensation, usually on one side of the belly
- pain that is more noticeable after exercise or when changing positions
- pain that may radiate to the groin or hip
Round ligament pain may last from a few seconds to several minutes.
Braxton-Hicks contractions
Braxton-Hicks contractions may start anytime in the second trimester of pregnancy. They involve the tightening of the uterus’ muscles.
These contractions differ from true labor in a few critical ways — they are brief and do not come at regular intervals.
Symptoms of Braxton-Hicks contractions include:
- squeezing or tightening of the uterus
- pain that occurs more frequently at night
- pain lasting anywhere from 30 seconds to 2 minutes
Braxton-Hicks contractions may be mild at first, but they can become more painful as pregnancy progresses.
Leg cramps
Leg cramps are a common cause of pain during the second and third trimesters of pregnancy.
They can develop when blood vessels or nerves in the legs are compressed. A lack of magnesium in the diet can also cause leg cramps.
Restless legs syndrome, which causes discomfort in the legs, can also occur during pregnancy.
Some research indicates that restless legs syndrome develops 2 to 3 times more often in pregnant women than the rest of the population.
Symptoms of leg cramps include:
- sudden pain in the calf or foot
- involuntary contractions of the muscles in the calf
- pain that may be worse at night
Symphysis pubis dysfunction
Symphysis pubis dysfunction, or pelvic girdle pain, may occur in about 31 percent of pregnant women.
The weight of the uterus can place extra stress on the pelvic joints, causing them to move unevenly.
Symphysis pubis dysfunction can also result from hormonal changes. During pregnancy, the body releases hormones that loosen and stretch certain ligaments in preparation for childbirth. These changes can contribute to pelvic pain.
Symptoms of symphysis pubis dysfunction include:
- pain in the center of the pubic bone
- pain radiating to the thighs or perineum (the area between the vagina and anus)
- difficulty walking
Back pain
Low back pain is one of the most common types to arise during pregnancy, and it often starts during the second trimester.
According to some research, about two-thirds of pregnant women develop low back pain.
Usually, it occurs because the growing abdomen is placing strain on the back muscles and causing changes in posture.
Symptoms of low back pain include:
- achy or dull pain in the lower back
- pain that worsens when bending forward
- stiffness in the back
Share on PinterestWomen who experience vaginal bleeding, vomiting, or fever during the second trimester should see a doctor.
Most common causes of second trimester pain do not require medical attention. However, pain at this stage of pregnancy can signify a problem, such as preterm labor, an infection, or another complication.
See a doctor if any of the following symptoms develop:
- contractions that occur at regular intervals
- vaginal pressure
- vaginal bleeding
- a severe headache
- sharp pain in the belly that persists, even after resting or changing positions
- vomiting, chills, or fever
- menstrual-like cramps that grow more severe over time
- fluid leaking from the vagina
Before using pain relievers during the second trimester, it is vital to speak to a doctor. Some pain medications are not safe to take during pregnancy.
Some pain medications are not safe to take during pregnancy.
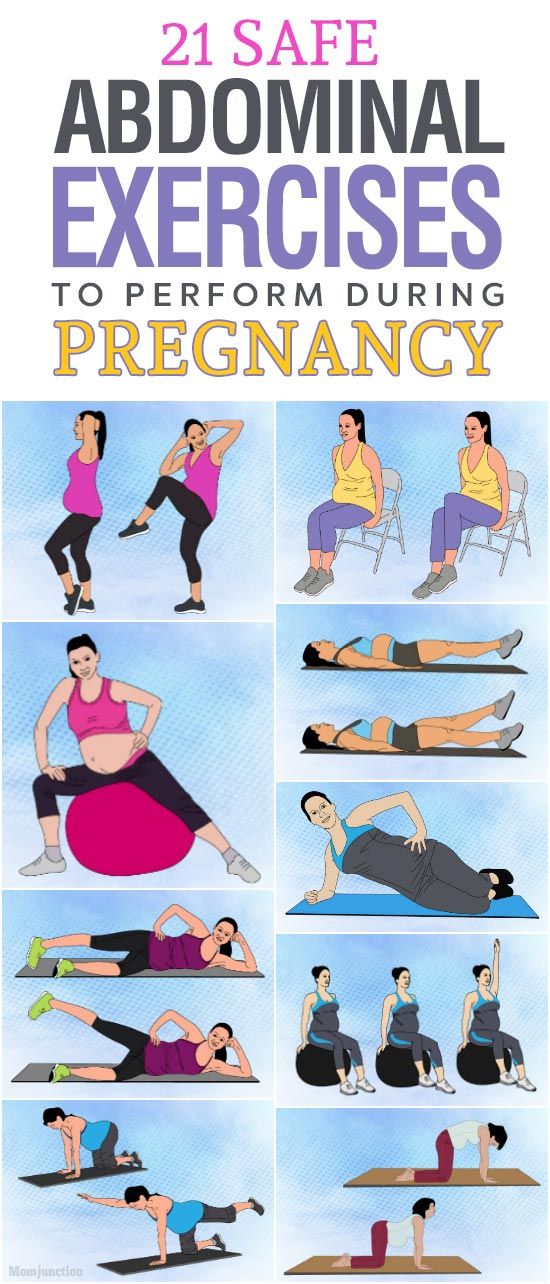
Certain complementary therapies may help reduce low back or pelvic pain.
A study involving 191 pregnant women found that complementary therapies, including acupuncture, aromatherapy, and reflexology, reduced symptoms in 85 percent of the participants.
Before trying any of these approaches during pregnancy, it is essential to talk with a doctor.
Home remedies can usually relieve second trimester pain, and the best approach will depend on the type of pain.
The following strategies may help:
- taking a warm (not hot) bath
- doing some light stretching to ease stiffness
- using a heating pad on the lower back
- wearing a maternity support belt
- using chairs with good back support
- avoiding standing in one spot for too long
- sleeping on the right or left side with a pillow between the legs
- avoiding changing positions too fast
- resting
Many types of pain can arise in the second trimester, including round ligament pain, back pain, and pain that results from symphysis pubis dysfunction.
In most cases, the underlying cause is a common issue, and a person can treat it at home.
In some instances, pain during the second trimester is a sign of something more serious. It is always best to see a doctor if the pain does not improve or otherwise causes concern.
causes of pain in the early stages and in the second trimester
From the moment of conception, the woman's body is rebuilt. The composition of the produced hormones changes, nutrients are distributed between the mother and the fetus. At an early stage, these changes are invisible to others. But the woman notices that menstruation did not begin at the appointed time. Taste preferences change, nausea appears in the morning, fatigue, drowsiness, irritability or unusual peace. If you notice signs of pregnancy, you need to see a doctor. A few days after the delay in menstruation, pregnancy can be confirmed by laboratory tests. The doctor will give advice on how to prevent the development of pathologies and bear a healthy child.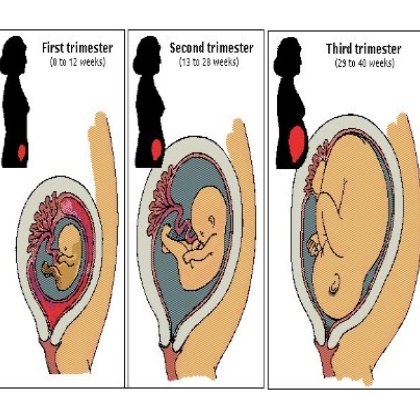
At the first appointment, the doctor will warn you about early symptoms that indicate a threat of miscarriage:
Lower back pain may occur during the first trimester of pregnancy. It is often encountered by women in the later stages. It arises due to increased weight and a shift in the center of gravity. But in the first trimester, the weight and size of the abdomen change slightly. You need to analyze your condition and understand if there is a danger.
Causes that do not cause concern
Pulling the lower back during pregnancy can be due to various processes occurring in the body. Some of them create inconvenience, but do not pose a threat.
Attachment of the ovum to the uterus
Attachment of the ovum to the wall of the uterus occurs 5-7 days after fertilization, even before the woman notices a delay in menstruation and thinks about a possible pregnancy. The process may be accompanied by an increase in vaginal discharge. They are not white, but pink. Women often believe that menstruation begins. Due to the production of various hormones, a few days can pull the lower back. These sensations are caused by natural, not pathological changes in the body. They are harmless, do not require treatment and disappear after 5-6 days.
The process may be accompanied by an increase in vaginal discharge. They are not white, but pink. Women often believe that menstruation begins. Due to the production of various hormones, a few days can pull the lower back. These sensations are caused by natural, not pathological changes in the body. They are harmless, do not require treatment and disappear after 5-6 days.
Changes in the circulatory system
After the attachment of the fetal egg in the uterus, the fetus begins to grow. He needs more nutrients and oxygen every day. To deliver them, the circulatory system begins to work differently, directing more blood to the uterus. Vessels from the pelvic area overflow, increase in volume and come into contact with the nerve endings in the lumbar region. There is a pulling pain. It is felt at 5-7 weeks of pregnancy. If the pain symptoms are not very pronounced, you can not worry. The body will rebuild, and the pain will pass without treatment.
Softening of the joints, ligaments
During childbirth, the joints and ligaments in the spine and pelvis should be well stretched. The body prepares in advance for the upcoming work. He already at an early stage begins to produce the hormone relaxin, which softens the joints and ligaments. Due to a change in their density, it can pull the lower back.
The body prepares in advance for the upcoming work. He already at an early stage begins to produce the hormone relaxin, which softens the joints and ligaments. Due to a change in their density, it can pull the lower back.
Uterine growth
At 9-10 weeks of pregnancy, the volume of the uterus already noticeably increases. The woman feels that the lower abdomen has become more firm and convex. The growing uterus begins to come into contact with other organs. With increased sensitivity, its pressure can be felt at an early stage. But more often women experience discomfort, mild pressing back pain in the second trimester.
Braxton-Higgs contractions
At the end of the first and beginning of the second trimester, spontaneous uterine contractions may occur, resembling labor pains, but less intense. Drawing cramping pain is given in the lower back. They can periodically disturb 2-3 weeks. If there are no other dangerous symptoms, medication, restriction of motor activity is not required.
Drawing back pain in pregnant women often occurs from natural causes. They do not pose a threat to the health of the expectant mother and the development of the fetus, do not require treatment. But it is necessary to tell the doctor about them in the antenatal clinic. He correlates them with other symptoms and will not miss the signs of an incipient miscarriage, other pathologies.
Dangerous conditions
Drawing pain in the lower back is often one of the signs of dangerous conditions:
- missed pregnancy, threatened miscarriage;
- diseases of the genitourinary system;
- osteochondrosis;
- symphysite;
- colds.
Missed pregnancy, threatened miscarriage
In case of missed pregnancy, threatened miscarriage, lower back pain is accompanied by bloody discharge from the vagina, cramping or constant aching pain in the lower abdomen. This is a dangerous condition. You need to immediately go to the hospital or call an ambulance.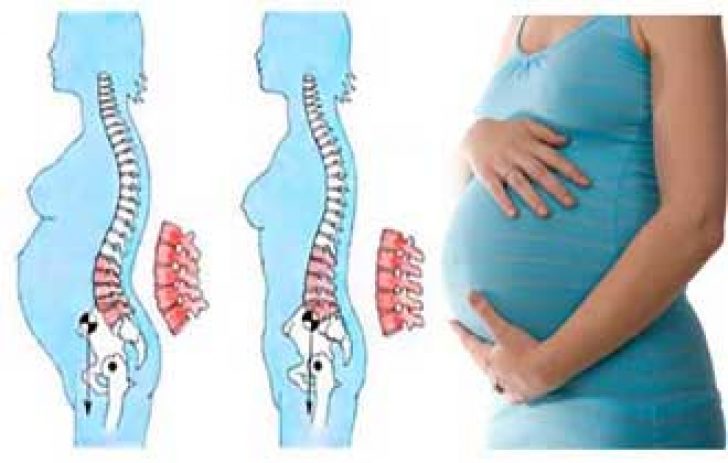 Do not refuse if the doctor suggests treatment in a hospital. To stop an incipient miscarriage, it is necessary to administer drugs intravenously, limit physical activity, and constantly monitor the condition of the woman and fetus.
Do not refuse if the doctor suggests treatment in a hospital. To stop an incipient miscarriage, it is necessary to administer drugs intravenously, limit physical activity, and constantly monitor the condition of the woman and fetus.
In case of miscarriage, examinations should be carried out to make sure that there are no particles of the fetus left in the uterus. This can cause a life-threatening inflammatory process or further infertility. Requires the introduction of drugs that enhance uterine contraction, relieve inflammation, or surgical intervention.
Diseases of the genitourinary system
Immunity in pregnant women is weakened. Hypothermia, malnutrition, increased stress can cause kidney disease. If the lower back is pulled during pregnancy on one side, on the right or on the left, check the functioning of the genitourinary system. Additional symptoms indicate problems with the kidneys: legs and arms swell, pressure and temperature rise, and pain occurs when urinating. Women with chronic kidney disease should be especially careful. They can worsen when the load on the diseased organ increases - in the second or third trimester, with a cold or eating salty, spicy, smoked, fatty foods. You cannot self-medicate. Taking the usual antibacterial drugs (Canephron, Levofloxacin, Furadonin) is undesirable for pregnant women. You need to see a nephrologist. He will prescribe a safe treatment.
Women with chronic kidney disease should be especially careful. They can worsen when the load on the diseased organ increases - in the second or third trimester, with a cold or eating salty, spicy, smoked, fatty foods. You cannot self-medicate. Taking the usual antibacterial drugs (Canephron, Levofloxacin, Furadonin) is undesirable for pregnant women. You need to see a nephrologist. He will prescribe a safe treatment.
Osteochondrosis
Starting from 7-8 weeks, the hormone relaxin begins to be produced, softening the joints and ligaments. If before conception a woman suffered from osteochondrosis, scoliosis, kyphosis, an exacerbation of diseases is possible even in the first or second trimester. An additional risk factor is rapid weight gain.
In women who have not previously suffered from osteochondrosis, it can develop in the later stages, when the spine is under a lot of stress due to a significant increase in body weight, a shift in the center of gravity, uterine pressure and softening of the joints and ligaments. The pain is pulling, exhausting, aggravated after a long stay in one position. With dystrophic tissue lesions, it can be felt on one side, left or right. Spinal problems can complicate childbirth. If you do not start treatment in a timely manner, do not engage in prevention, they will continue to progress after childbirth.
The pain is pulling, exhausting, aggravated after a long stay in one position. With dystrophic tissue lesions, it can be felt on one side, left or right. Spinal problems can complicate childbirth. If you do not start treatment in a timely manner, do not engage in prevention, they will continue to progress after childbirth.
Symphysitis
If the production of the hormone relaxin is strongly activated, premature softening of the joints occurs, which can cause the pubic bones to diverge. This increases the risk of preterm birth. With the divergence of the pubic bones, the pain is shooting, sharp. She gives to the lower abdomen and lower back. There are swelling in the pubic area. To diagnose symphysitis, the doctor examines blood and urine tests, conducts an additional ultrasound examination, observes the dynamics of the development of the disease and decides on the possibility of natural childbirth or the need for a planned caesarean section. In the later stages, motor activity may be limited, strict bed rest is recommended.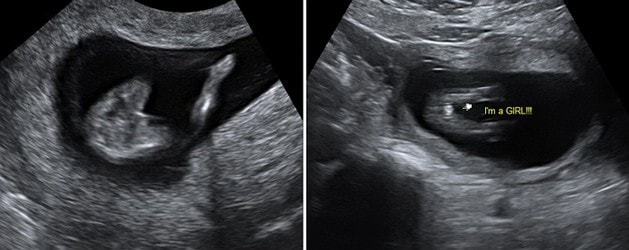
Colds
Pregnancy increases the risk of complications from colds. Especially dangerous is the early period when the organs of the fetus are formed. A significant increase in temperature, infection, uncontrolled use of antibiotics can provoke serious pathologies.
It is necessary to consult a doctor and start treatment at the first symptoms of a cold. Lower back pain and body aches can occur when the temperature rises. It passes if it is knocked down using traditional medicine recommended by a doctor. But if it hurts in the lower back on the right or left, the temperature rises to 39degrees, there was a strong cough, shortness of breath - pneumonia is possible. You need to call a doctor at home or an ambulance.
Prevention and treatment
If you have pain in your lower back during pregnancy, do not take painkillers. If the pain is severe, but examinations have not shown dangerous pathologies, consult a doctor. After studying the causes and symptoms of pain, he will choose safe ways to alleviate the condition.
In the first trimester, you need to be especially careful. A woman may still not know about pregnancy, but pain is already appearing. With a delay in menstruation, even for 2-3 days, you need to coordinate drug treatment with your doctor.
The second trimester is the time when a woman intensively gains weight and the load on the musculoskeletal system increases, pressure on the internal organs. The doctor will advise you to wear a bandage for pregnant women and other non-drug ways to relieve and prevent pain.
The third trimester - the body prepares for childbirth, the joints soften, the bones in the pelvic area diverge. If it pulls the lower back, the lower abdomen hurts, you need to lie down. If the pain intensifies, becomes cramping, childbirth may begin. If the period is less than 38 weeks, call the doctor who manages the pregnancy and describe the symptoms.
Prevention of pain in the lower back
To reduce the risk of lower back pain, the development of diseases of the musculoskeletal system:
- do not lift heavy loads, in the early term, power loads can provoke a miscarriage, in the late term - premature birth;
- do not wear tight shoes, shoes and boots with high heels, they create an additional load on the spine;
- watch your weight, no need to eat "for two";
- Eat more foods containing calcium, a mineral-vitamin complex recommended by your doctor;
- consult a doctor and start herbal medicine at the first sign of a cold, avoiding a significant increase in temperature;
- do not slouch, keep your back straight so that the load is distributed evenly;
- do not overwork, do not work for a long time in one position.
Keep fit. The muscular frame will reduce the load on the spine. Regular, but not too intense exercise, walks in the fresh air will strengthen the immune system, help control weight. Useful swimming in the pool or ponds with clean running water. Learn and regularly do a set of exercises for pregnant women.
Why does the stomach pull in early pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of having an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs.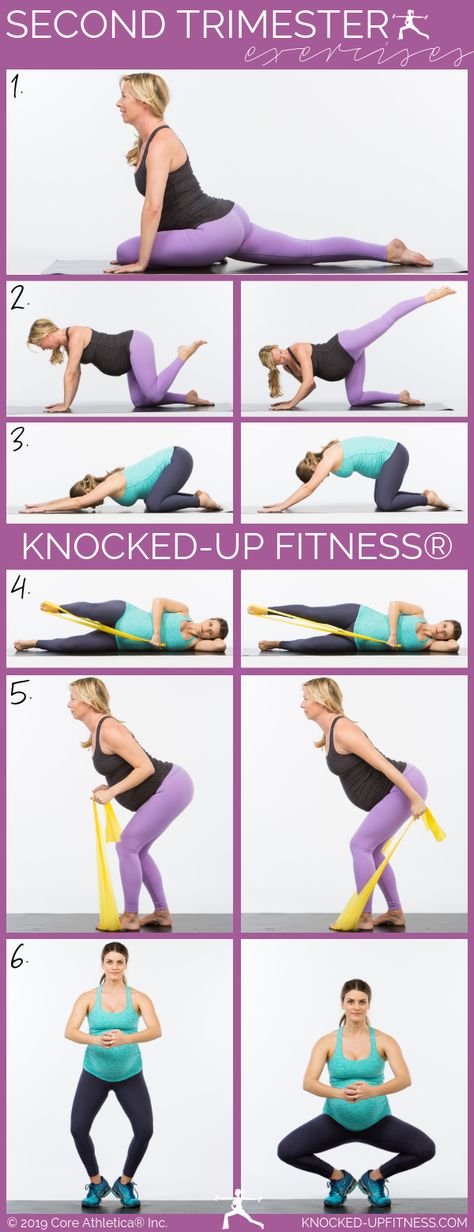 All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy can be:
- "obstetric";
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- missed pregnancy;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus.
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the insertion of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Among the reasons that can cause a miscarriage are:
- severe physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.

Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you should consult a doctor, as a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Illegal pregnancy
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Cystitis, due to the anatomical features of a woman, can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.
The bladder, located in the lower third of the abdomen, may give false symptoms of threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection.