Redness under neck baby
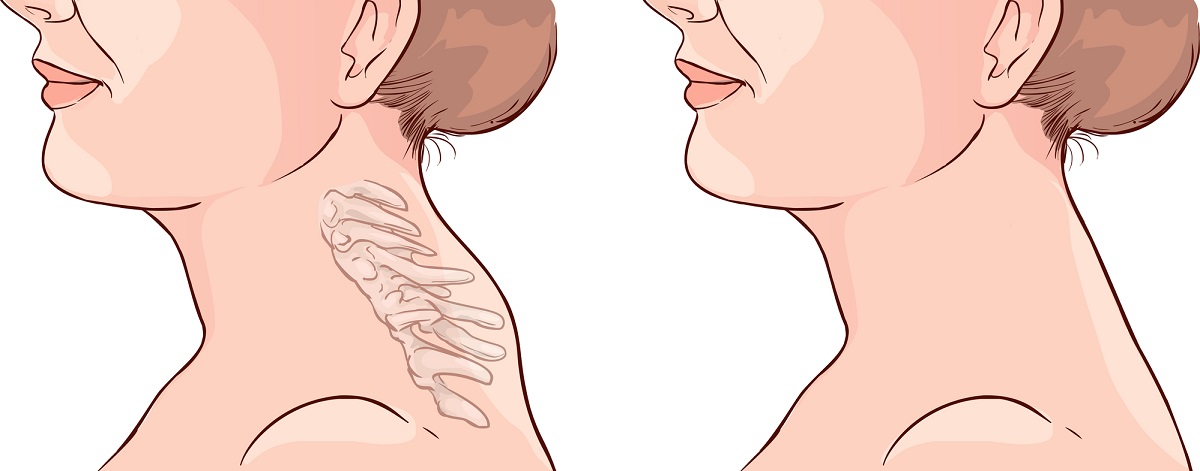
How to Prevent and Treat It
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Drooling can be a common side effect of teething, but many babies drool even when they aren’t getting new teeth.
The constant presence of saliva on your baby’s chin, neck, and even chest can turn into a red irritation known as a drool rash. Here’s what you need to know to treat existing drool rashes and prevent new ones from forming.
A drool rash can appear around the mouth and cheeks, in the folds of your baby’s neck, and on your baby’s chest as a result of too much saliva causing wet skin.
Drool rashes typically present as flat or slightly raised patches with small red bumps. They can also have a chapped appearance. Drooling is the most likely culprit, but your baby may develop a drool rash if they use a pacifier that keeps the skin around the mouth wet or if there’s smeared food left on their face for too long.
It can be difficult to keep your baby from drooling.
According to the UCSF Benioff Children’s Hospital, a baby’s salivary glands begin working between 2 and 3 months of age. This can lead to drooling, even though your baby isn’t teething.
To prevent a drool rash, have a soft burp cloth on hand at all times so you can gently wipe away any drool. Keeping your baby’s skin clean and dry is the most effective remedy against drool rash. Wipe your baby’s face and in the folds of his or her neck frequently, and especially after feedings. Use gentle pressure in a dabbing motion to avoid irritating your baby’s skin.
Keeping your baby’s skin clean and dry is the most effective remedy against drool rash. Wipe your baby’s face and in the folds of his or her neck frequently, and especially after feedings. Use gentle pressure in a dabbing motion to avoid irritating your baby’s skin.
If your baby drools enough to dampen his or her shirt, try using a bib. This will prevent the wet material from rubbing against your baby’s skin, which can lead to uncomfortable chafing and a drool rash.
Change bibs as soon as they become wet with drool to keep your baby’s skin clean and dry.
There are ways to make your baby more comfortable with drool rash.
Twice daily, gently wash the afflicted areas with warm water, then pat dry. Don’t rub, which can be irritating to already sensitive skin. Be sure your baby’s skin is completely dry.
Apply a thin coat of a healing ointment like Aquaphor or petroleum jelly, which will act as a barrier between your baby’s skin and the drool. These ointments can be soothing to your baby’s irritated skin.
At bath time, be sure to use a mild, unscented baby wash. Use a gentle, unscented lotion on your baby’s dry skin if necessary, but avoid using lotion on drool rashes. Skin should be kept dry and treated with a healing ointment. You may consider nonprescription-strength hydrocortisone cream, but ask your doctor how often and for how long to use it.
While your baby has a drool rash, it’s a good idea to reduce potential irritants in the immediate environment. Avoid making your baby’s rash worse by switching to a fragrance-free laundry detergent for your baby’s clothing, sheets, bibs, and burp cloths. Consider washing your clothing in the same detergent. Avoid perfumes and scented lotions as well. They can also be aggravating to your baby’s rash.
If you suspect that teething is triggering your baby’s excessive drooling, offer something cold (but not frozen) for your baby to gum. Try a teething ring or a cold washcloth. The coolness will have a mild numbing effect on your baby’s sore gums and any rash around their mouth. Be sure to gently pat dry your baby’s mouth afterward.
Be sure to gently pat dry your baby’s mouth afterward.
In most cases, drool rash is a minor irritation that will go away with regular at-home treatment. There are a few instances when it’s best to consult your pediatrician:
- if the rash is cracked, weepy, or causing your baby pain
- if the rash doesn’t show any improvement after roughly a week of home treatment
Your doctor may be able to prescribe creams that can help your baby’s drool rash heal faster and reduce your baby’s discomfort.
Baby Yeast Infection on the Neck: Causes and Treatment
One of the cutest — and most fragile — things about very young babies is how they’re like real-life bobblehead dolls. Most newborns can’t hold their head upright and still until they’re about 4 to 6 months old. This is because it takes time for a baby’s neck muscles to develop.
Before they reach this important muscle milestone, babies are prone to rashes on the neck because their drooping heads cause skin folds.
Sometimes a baby’s neck rash may be caused or worsened by a yeast infection. This happens when normal yeasts that live in and on our bodies grow a bit more than they should.
Don’t worry. Baby yeast infections on the neck are common and treatable. In most cases, they go away on their own once your baby is able to lift up their head more often (hello, tummy time!).
Here’s what to know and when you should see a pediatrician about baby’s neck yeast infection.
Yeasts are a type of fungus. A common kind of yeast called Candida is found on the skin and in the mouth, gut, and genital area.
When this kind of yeast overgrows, the infection is called candidiasis. Yes, this is the same kind of yeast that can cause a vaginal infection in adults!
At healthy levels, Candida and other yeast live harmoniously with bacteria and other friendly organisms in our body.
But sometimes, an imbalance happens and the yeast starts growing more than it should. This may happen in babies because their immune systems are still new and growing. Babies may also not yet have enough friendly gut bacteria to help keep yeast growth at bay.
This may happen in babies because their immune systems are still new and growing. Babies may also not yet have enough friendly gut bacteria to help keep yeast growth at bay.
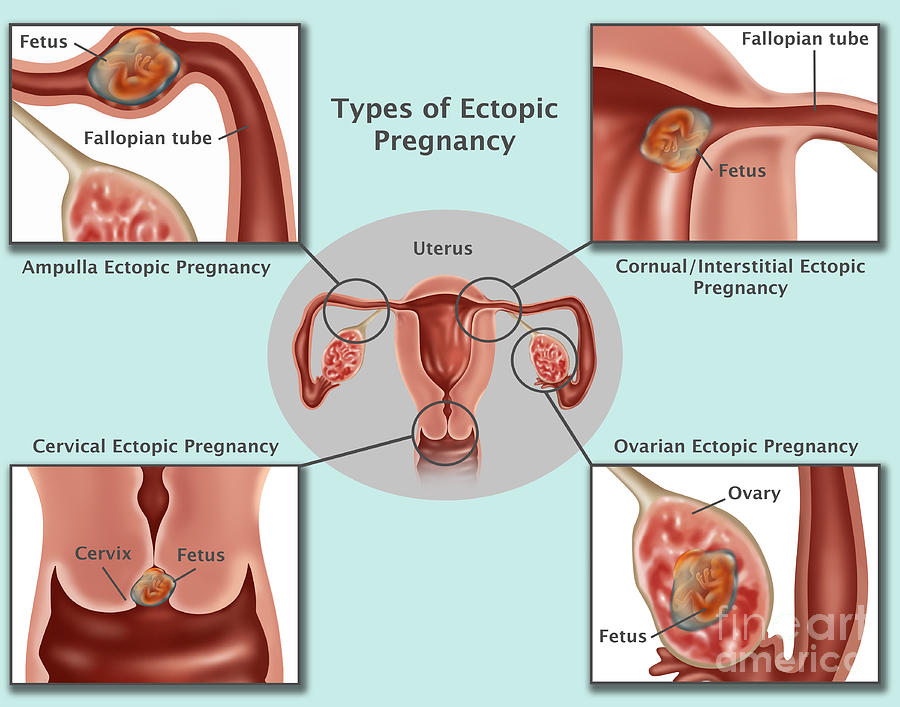
Candida can cause yeast infections called thrush in skin folds in the neck, armpits, groin, bottom, vagina, and legs. Babies can also have oral thrush, a yeast infection in the mouth and throat, and on the tongue. Some diaper rashes are also caused by a yeast infection.
A yeast infection on a baby’s neck might begin in the skin folds and spread to nearby neck skin. It may look like:
- redness in the skin folds
- pink, moist patches
- red or pink scaly or rough patches
- redness with raised edges
- redness with tiny bumps
- skin discoloration patches
- gray or white powdery patches on the skin
- redness with swelling
- a red sore in the skin folds with satellite spots or rashes around it
The soft folds of skin on a baby’s neck create the perfect warm, moist environment for a yeast infection to blossom. All that drooling and spit-up doesn’t help, either!
All that drooling and spit-up doesn’t help, either!
In fact, another kind of yeast infection that babies can have on their chin and other areas is called a drool rash. A thrush infection in a baby’s mouth or throat can sometimes spread to the neck through drool, spit-up, and vomit.
Yeast loves to grow in places that have wetness and less oxygen. Clothing or blankets can also cause friction, irritating a baby’s delicate neck skin. A sore or irritated area on the neck is more likely to get a yeast infection because it might ooze liquid.
Your doctor may check to see if your baby has a neck yeast infection by looking at the area carefully or gently wiping it with a cotton swab to test.
Some mild baby yeast infections on the neck go away on their own once your baby starts lifting their head more and has fewer skin folds.
Other yeast infections may need to be treated with antifungal skin (topical) medications. One kind of skin treatment for yeast infections is a combination of the antifungal medication miconazole and zinc oxide.
This antifungal treatment is available in ointment and spray form. Antifungal ointment shouldn’t be used on a baby younger than 4 weeks old.
Ask your baby’s pediatrician before using antifungal ointment or spray on your baby’s skin. Apply the antifungal ointment or spray with a cotton swab to help get it only where it’s needed on baby’s delicate skin.
If your baby has yeast infections on other parts of the body or in the mouth, your pediatrician may prescribe an oral antifungal medication such as fluconazole.
This medication comes in liquid form and can be given by mouth with a dropper or syringe. Babies typically get a low dose of fluconazole once every 2 to 3 days.
Most neck yeast infections in babies go away within 2 weeks after treatment begins. But they can happen again in the same areas.
Babies can get bacterial infections on the neck similar to how yeast neck infections happen. Yeast infections will likely look slightly different than other kinds of rashes, and they won’t get better with typical rash creams.
A bacterial infection on the neck may look more like a red, flat sore that’s only on one area of a skin fold. Baby eczema and dermatitis can also happen on the neck.
These kinds of infections may cause more itching than a yeast neck infection, so your baby might appear more uncomfortable.
You may not always be able to prevent a yeast infection on your baby’s neck. Tips to reduce the risk of a yeast neck infection or prevent it from worsening are similar to how to prevent a diaper rash or infection on other parts of the body. They include:
- Lay your baby flat on their back when sleeping to help straighten the neck. (This is necessary for safe sleeping, anyway.)
- Avoid letting your baby sleep in their car seat or any kind of seat where their head slouches over. (This is also a risk factor for sudden infant death syndrome (SIDS).)
- Avoid clothing or blankets around the neck when baby is indoors.
- Avoid dressing your baby in rough fabrics or tight clothing.
- Remove clothing and let your baby’s neck and chest air out in a warm, dry area after being bundled up.
- Wash your baby’s neck with a sterile washcloth and warm, soapy water.
- Clean and dry baby’s neck regularly — especially after feeding, drooling, spitting up, or vomiting (so basically whenever possible!).
- Check and sterilize baby’s pacifiers, bottle nipples, and teething toys with boiled or very hot water. Running them through the dishwasher on a high temperature is an easy way to do this.
- Avoid using antibacterial soap or cleanser anywhere on your baby’s skin. This may remove healthy skin bacteria and trigger a yeast infection.
- Similarly, avoid using antibacterial ointment or cream on your baby’s neck.
- Avoid using harsh or chemical soaps, shampoos, and laundry detergents. These may irritate baby’s skin, leading to skin infections.
- Avoid using moisturizer or lotion on your baby’s neck.
- Avoid touching or kissing your baby’s neck area.

Always let your baby’s doctor know about any kind of rash your baby has. A doctor can confirm whether it’s a yeast infection or another kind of rash. They can also determine whether your baby needs medical treatment.
An untreated yeast infection on a baby’s neck can worsen and spread to others areas of the skin and even inside to the blood.
Baby neck yeast infections are a kind of skin rash that can happen to babies of any age. They’re most common in babies under 4 months old because they have more neck skin folds. Yeast or fungi are a normal healthy part of our bodies, but they can sometimes overgrow, leading to an infection.
Yeast like to grow in warm and moist areas. Most babies outgrow yeast neck infections. In more serious cases, your pediatrician may prescribe antifungal treatment.
reasons and what to do about it
Red areas of the skin can be the result of a violation of the rules of care, that is, they can be caused by physiological causes, and also be one of the first symptoms of various dermatological diseases. In order to eliminate redness, you first need to establish the cause of the unpleasant phenomenon.
In order to eliminate redness, you first need to establish the cause of the unpleasant phenomenon.
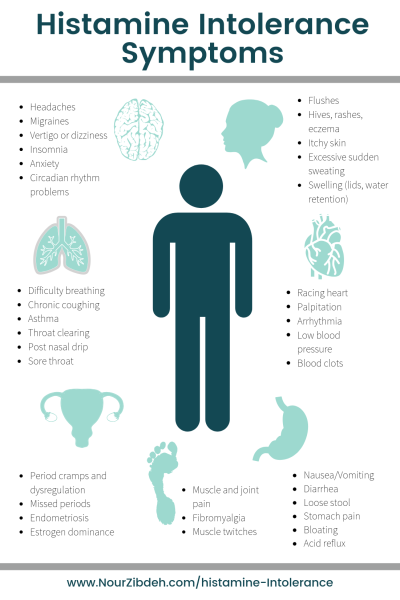
Pathological redness can be caused by an allergic reaction, a symptom of an infectious or autoimmune disease. nine0003
In a child, redness of the skin of the hands is often a sign of allergic dermatitis. External signs of this disease are usually localized in open areas of the body: face, hands, neck. In addition to redness of the skin, allergic dermatitis is accompanied by symptoms such as:
Severe forms of allergies include diseases such as eczema and Quincke's edema. With eczema, the skin is a reddened, itchy area covered with crusts or blisters. Angioedema usually occurs as an allergic reaction to insect bites or certain allergens. nine0003
Redness of the skin of the hands in a child can be caused by kidney or liver failure, infectious diseases, or be the result of exposure to detergents, care cosmetics.
Legs
Redness of the skin of the legs, accompanied by a rash, itching and increased dryness, should not be left out of the attention of parents. There may be several reasons for this phenomenon:
There may be several reasons for this phenomenon:
- urticaria or contact dermatitis - red patches varying in shape and size, may merge with each other, causing irritation, severe itching and discomfort; nine0018
- injuries, bruises and sprains - in addition to redness, the child has noticeable swelling;
- fungal infection - redness accompanied by peeling of the skin, the appearance of cracks and severe itching;
- bacterial infections - often resulting from reinfection through scratching and other skin breaks;
- Coxsackie virus, chicken pox, measles.
The appearance of redness on the skin of the legs requires an immediate visit to a doctor - a pediatrician or dermatologist. nine0003
Face and neck
The appearance of red spots on the cheeks usually indicates an allergic reaction. In infancy, the organs of the digestive system can not always successfully perform their function. In addition to redness, the child has nausea, constipation or diarrhea, abdominal pain, problems with appetite, irritability, sleep disturbances.
Food allergies are most often caused by cow's milk protein, chicken eggs, fish, honey, chocolate, strawberries, citrus fruits. Allergic reactions often occur when a baby tries a new food for the first time, especially when it comes to exotic fruits. nine0003
In the cold season, the child may experience redness around the mouth. The absence of sebaceous glands in the lips provokes drying, irritation and the appearance of painful points and small wounds.
The reasons for this phenomenon may be:
- allergic reactions;
- decreased general immunity;
- adverse weather conditions;
- deficiency of vitamins in the body; nine0018
- bad habits - eg thumb sucking;
- features of digestion.
Redness of the skin on the face also occurs with seborrheic dermatitis. With this disease, increased dryness and peeling are noted in certain parts of the body. The exact cause of seborrheic dermatitis has not been established, but it usually develops on oily skin and is not associated with allergic reactions or lack of hygiene.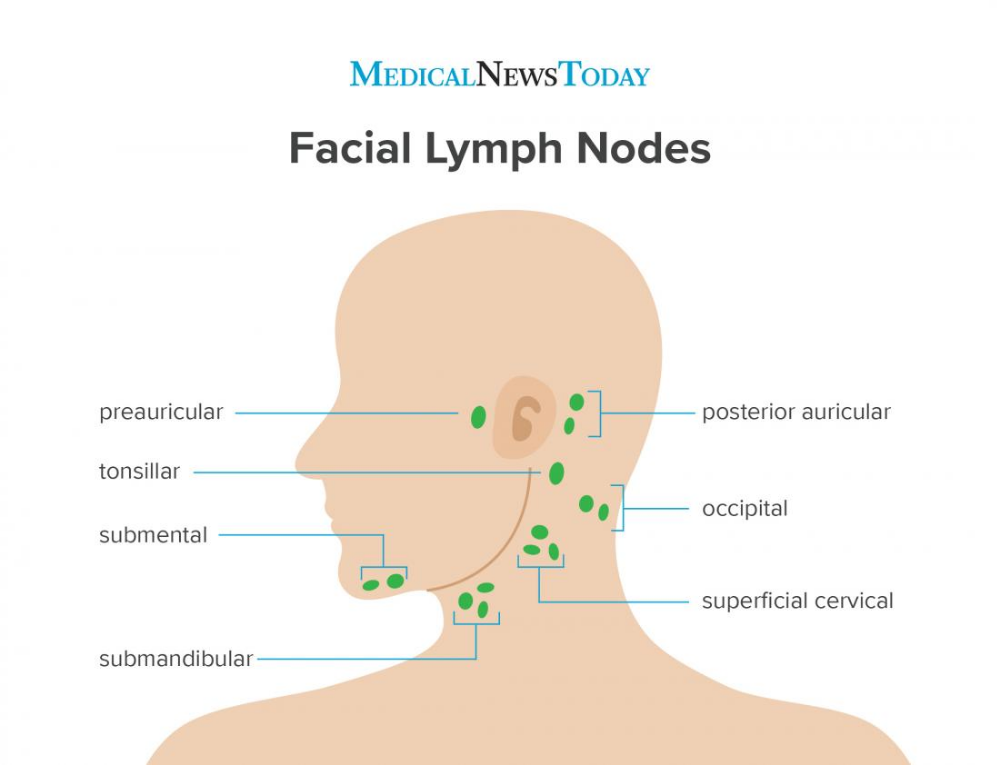
Peeling crusts are usually localized in the scalp, around the wings of the nose, eyebrows, ears, less often on the child's body. nine0003
Seborrheic dermatitis can appear at any age, this physiological deficiency is often observed in infants. Usually, the crusts do not present discomfort to the child and can be regarded mainly as an aesthetic defect. The scaly growths and redness do not cause pain or irritation and often go away on their own without treatment. It is believed that the cause of their appearance are maternal hormones transmitted to the child.
To eliminate crusts from the baby's head, before washing the affected area is smeared with vegetable oil, and then the hair is washed with a mild baby shampoo. nine0003
In order to eliminate redness and its accompanying symptoms, it is necessary to establish the cause of the phenomenon.
Buttocks
Redness of the skin on the pope in a child is the result of diaper rash (diaper dermatitis). The skin turns red in the perineum or in the folds, where moisture accumulates the most. Usually the baby reacts negatively to touch when changing a diaper, washing after a bowel movement.
The skin turns red in the perineum or in the folds, where moisture accumulates the most. Usually the baby reacts negatively to touch when changing a diaper, washing after a bowel movement.
An increased risk of diaper rash on the buttocks occurs when there are violations in the digestive system. Frequent rare stool irritates the delicate skin of the baby, causing redness of the skin. In this case, a review of the child's nutrition system can help. nine0003
The reasons for the appearance of redness of the buttocks in a baby can be:
- incorrectly fitted diaper;
- increased temperature in the room when the child develops prickly heat;
- taking certain medications;
- transition to a new milk formula;
- incorrect selection of detergents and cosmetics for skin care;
- urticaria;
- fungal diseases. nine0018
If redness is not associated with physiological causes, the child should be shown to the doctor.
Diagnosis of redness and irritation
Since the appearance of red patches of skin can be caused by a huge number of reasons, the diagnosis of this problem is of great importance. Depending on the cause of the disease, a pediatrician, dermatologist or other specialist will choose the most effective treatment methods.
In the course of diagnosis, data from an external examination of the child are used. At the same time, attention is paid to the localization of redness, spots and rashes, their size, shape and severity of manifestation. nine0003
Based on the results of the examination, it is recommended to conduct laboratory and instrumental studies. The patient is prescribed general and biochemical blood tests, allergy tests are performed to determine the allergen. If the reddening of the skin in a child is caused by infectious diseases, diagnostic measures are aimed at identifying the causative agent of the infection for the purpose of surgical treatment.
If a fungal infection is suspected, a skin scraping is taken for further examination under a microscope. nine0003
If redness is caused by physiological causes, parents are given recommendations on how to organize the child's nutrition and care procedures. These measures will minimize not only redness, but also other negative reactions from the skin, such as excessive dryness, irritation and roughness.
The treatment of redness as part of the symptoms of various diseases, first of all, is aimed at eliminating the cause that causes this phenomenon. It also aims to ensure that negative skin reactions that cause discomfort to the child are eliminated as soon as possible. nine0003
Prevention of redness and skin irritation
Negative reactions from the skin in childhood are rarely caused by serious diseases and in most cases this problem can be solved by timely treatment and preventive measures.
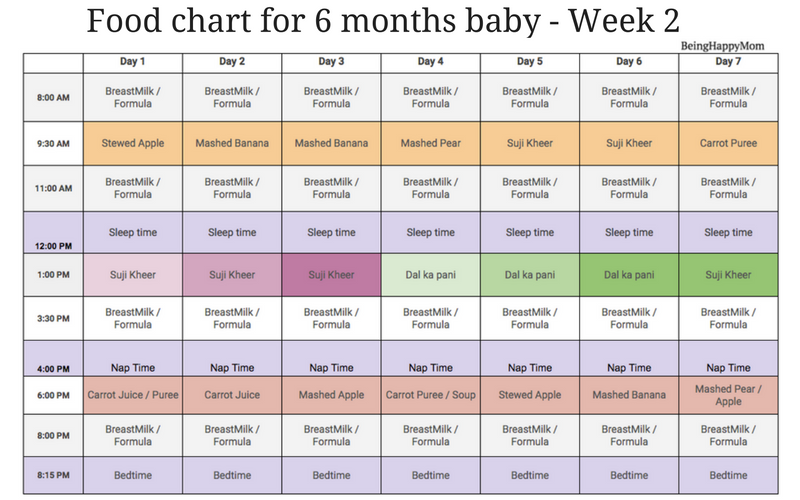
Prevention of atopic dermatitis:
- adjust the child's diet, exclude foods that cause negative reactions in the body; nine0017 moisturize the skin with hypoallergenic cosmetics;
- eliminate or minimize environmental allergens - pets, synthetic clothing, certain foods, harsh detergents;
- regularly carry out wet cleaning of the premises;
- for washing clothes and baby diapers, use special products.

In order to prevent the severe course of diseases caused by viral, bacterial or fungal infections, it is necessary to detect diseases in a timely manner and carry out appropriate treatment. nine0003
It is possible to prevent the appearance of redness and irritation of the baby's skin caused by diaper rash, subject to the following recommendations:
- bed linen and clothing of the child must be made of natural, breathable fabrics only;
- regularly change the baby's diapers or swaddling clothes, do not allow the baby to stay wet for a long time;
- after each bowel movement, the baby should be washed with warm water; nine0017 while bathing, it is recommended to add decoctions of string or chamomile to the bath;
- from time to time the baby should be left undressed on the changing table for air baths;
- only products intended for sensitive skin can be used while bathing;
- use soft towels to dry the body after washing, do not rub the skin;
- powders and care oils are used separately; nine0018
- ensure that the child is not deficient in vitamins.

To prevent allergic reactions, in which redness and irritation of the skin occurs, care must be taken when introducing new complementary foods. You can not introduce several products into the baby's diet at once, you need to start with vegetable or fruit purees. A new product is given in a limited amount (for example, a teaspoon) and the body's reaction is monitored. In the absence of allergies, the amount of the product is increased. nine0003
Of great importance in prevention belongs to walks in the fresh air. With the child you need to walk daily for 2-3 hours. During the heating period in the room, it is important to prevent the air from drying out. To do this, it is recommended to use special humidifiers or at least put a container of water in the room.
If redness, itching, skin irritation still occur, in addition to general treatment, it is necessary to use special cosmetics with effective local action. Their use is aimed at the rapid elimination of external manifestations of allergies and other diseases. nine0003
nine0003
Anti-irritants
You can quickly eliminate redness and irritation of the skin in a child with the help of emollients. The active substances in these cosmetic products help to soften, moisturize, relieve inflammation and regenerate the skin.
Emollients that are suitable for sensitive and delicate skin at any age are presented in the Emolium cosmetic series. Their regular use allows you to successfully deal with such phenomena as excessive dryness, roughness, inflammation and redness of the skin. Leading dermatologists and pediatricians took part in the development of the Emolium series. nine0003
Emolium products are successfully used in skin care prone to such diseases as atopic dermatitis, urticaria, seborrheic dermatitis. They can be recommended for children whose skin is prone to rashes, blisters and crusts.
Moisturizing the skin and maintaining its water-lipid barrier is of great importance. To do this, use the bathing emulsion of the Emolium series. The remedy can be prescribed from the first days of a baby's life in order to soften hard water and prevent dryness and irritation. nine0003
The remedy can be prescribed from the first days of a baby's life in order to soften hard water and prevent dryness and irritation. nine0003
"Emolium" is represented by three types of funds: basic, special and triactive series. You can learn more about the products by clicking on the link.
Intertrigo: advice to parents
September 8, 2021
Diaper rash, or diaper rash, is a common problem accompanied by baby crying.
nine0002 Irritation of the skin in newborns can occur for various reasons, for example, due to friction or constant contact with moisture under the diaper. In order for the baby to always be comfortable, parents should monitor the hygiene of the baby and the condition of his skin. What to do if you notice redness in a child?Features of children's skin
Diaper rash can also appear on the skin of an adult, but the skin of newborns is most susceptible to inflammation. The reason is simple - the skin of babies is different from the skin of adults, it is much softer, more sensitive and does not yet have the necessary protective functions, so it easily absorbs moisture and is damaged. In addition, there are folds on the body of a newborn child, in which sweat and pollution accumulate, which can trigger the inflammation process. nine0003
The reason is simple - the skin of babies is different from the skin of adults, it is much softer, more sensitive and does not yet have the necessary protective functions, so it easily absorbs moisture and is damaged. In addition, there are folds on the body of a newborn child, in which sweat and pollution accumulate, which can trigger the inflammation process. nine0003
Most often, irritation appears in the diaper area - in the groin, on the legs, between the buttocks, but it is also not uncommon for the skin to turn red on the neck, in the armpit area. If the skin is severely inflamed or foci of irritation are present on the entire body and face of the child, urgently seek help from a pediatrician.
Causes of diaper rash
Almost all infants have diaper rash. If you pay attention to the problem in time, you can easily avoid the development of complications. The main causes of diaper rash:
1. Long contact with moisture. Inflammation can appear if the skin has not had time to dry after bathing, and also if the baby is sweating.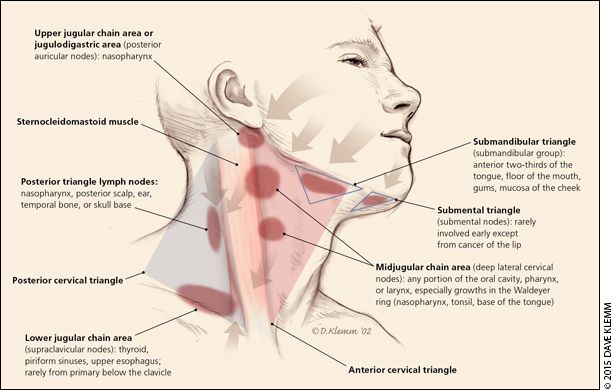 After bathing, allow the skin to dry on its own or blot moisture with a soft cloth before putting on a diaper or clothing. Dress your child according to the weather and make sure the temperature at home is comfortable.
After bathing, allow the skin to dry on its own or blot moisture with a soft cloth before putting on a diaper or clothing. Dress your child according to the weather and make sure the temperature at home is comfortable.
2. Infrequent diaper changes. Prolonged contact with enzymes in urine and feces irritates the baby's delicate skin. Check the diaper regularly and clean the skin thoroughly. If your baby has diarrhea, change the diaper as often as possible. nine0003
3. The baby has chafing in the diaper or clothes. The problem may arise due to the wrong size. Choose loose-fitting pieces in soft, natural fabrics. The diaper should be fastened securely, but not tight, so that air can circulate.
Treatment and prevention of diaper rash
Even the most attentive parents are not always able to prevent the appearance of diaper rash, because at the initial stage the child may not notice the appearance of irritation, and parents will see the problem only when changing the diaper. Treatment for diaper rash usually depends on the severity:
Treatment for diaper rash usually depends on the severity:
1. With a mild degree, only redness on the skin is visible, if you start treatment at this stage, you can avoid aggravating the situation.
2. The average degree is characterized not only by redness, but also by the presence of skin damage: erosion, microcracks.
3. At the third stage, pustules and ulcers appear on the reddened areas, the inflamed areas begin to get wet. Often a fungal or bacterial infection joins, which greatly complicates the treatment process. The child may have a fever, loss of appetite, worsen sleep. In such a situation, parents need to urgently consult a doctor. nine0003
To prevent and treat mild diaper dermatitis:
- Change diapers more often. It is important that the baby's skin stays dry for as long as possible.
- Thoroughly wash the baby's skin after removing the diaper and allow it to dry completely.
- Leave the baby without a diaper and clothes for a while to allow the skin to "breathe".