Anatomy of birth canal
Your baby in the birth canal Information | Mount Sinai
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal
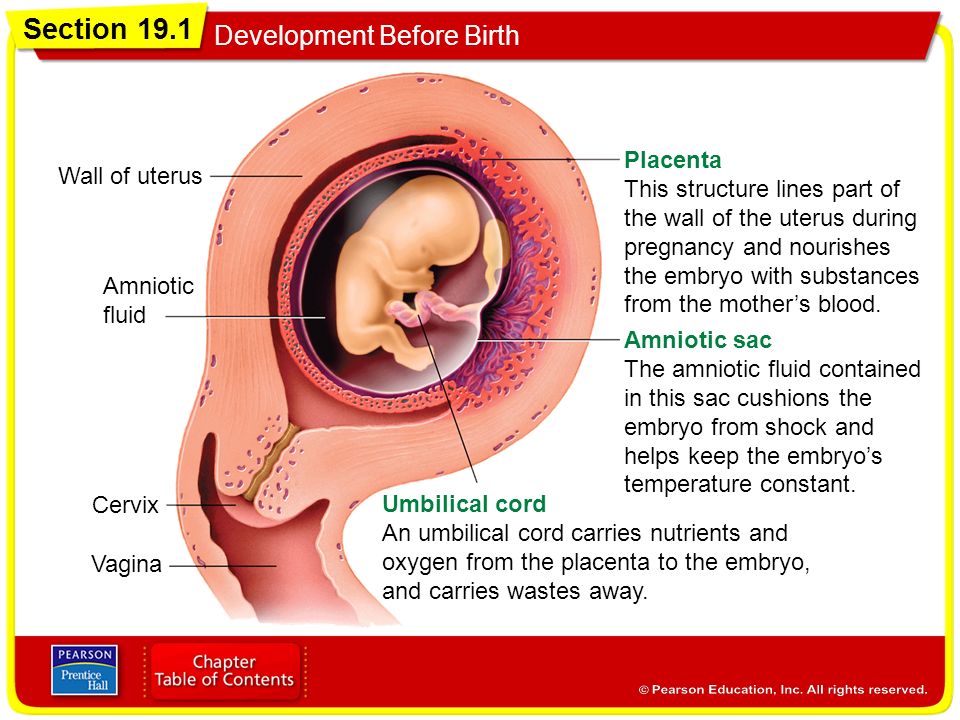
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Childbirth is really a series of four stages that culminate in the actual birth and short period thereafter. For more specific information regarding emergency delivery see the information on childbirth, emergency delivery.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Cephalic (head first) presentation is considered normal, but a breech (feet or buttocks first) delivery can be very difficult, even dangerous for the mother and the baby.
In a normal pregnancy, the baby is positioned head down in the uterus.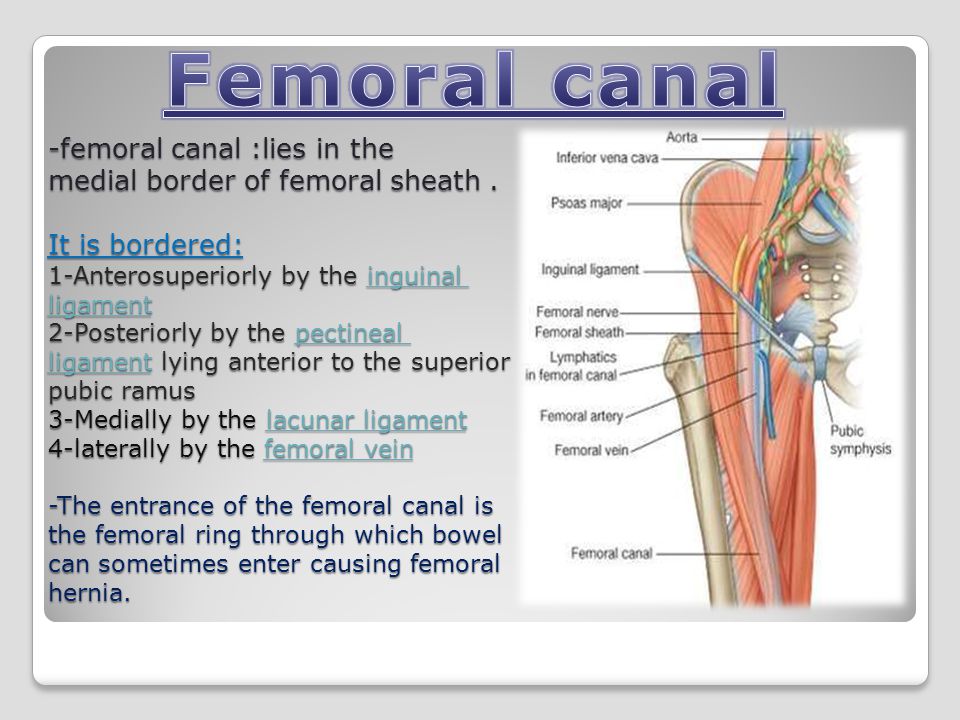
The term fetal presentation refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.

- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
FETAL LIE
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between his head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
Engagement
- This is when the widest part of your baby's head has entered the pelvis.

- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
Descent
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
Flexion
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
Extension
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
Expulsion
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Last reviewed on: 12/3/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Birth Anatomy - A Guide to Mother's Birth Anatomy
The Bones of the Pelvis
Our bones are held together by flexible tendons, cartilage and ligaments. In pregnancy, the joints between the bones become more mobile. Waddling is an example of what happens when the leg and pelvic joints get softer. The baby passes through a mobile pelvis.
The hormone relaxin helps cartilage become more mobile. The muscles to the legs and pelvis are more effective when long and supple. Together the joints and muscles allow the pelvis to become a dynamic, flexible passageway.
The muscles to the legs and pelvis are more effective when long and supple. Together the joints and muscles allow the pelvis to become a dynamic, flexible passageway.
A drawing showing the four joints of the pelvis.
The bony pelvis has four joints. In the front of the pelvis is the symphysis pubis joint. Movement here really isn’t that comfortable. Sometimes a pregnancy belt holds this joint stable for walking and rolling over in bed. Symmetry in the symphysis pubis (pubic bone) reduces spasm in the round ligaments and helps the sacrum, around back, to be aligned properly.
On either side of the sacrum are the SI joints (Sacroiliac joints). These are located where the dimples are. Many plastic baby dolls have SI dimples above their bum. The SI joints are a common location for aches when the pelvis is weak or crooked.
Symmetry in the SI joints will help the sacrum be lined up with the pelvic brim. Then the baby can get into a nice, head down position. A chiropractic adjustment helps get the symphysis and the SI joints aligned.
The sacrum, rather than fused, is slightly mobile and in the birth process actually moves to allow the head past.
The tailbone is connected by a joint to the lower end of the sacrum. Sometimes this needs an adjustment, too, especially after birthing a baby. Ligaments connecting to the sacrum and tailbone (coccyx) will become more symmetrical and their tone will be more relaxed and less in spasm after bodywork on the pelvis.
Important Landmarks in the Pelvis
The baby first passes into the brim when engaging in the pelvis. The angle of the baby’s head in relation to the brim of the pelvis plays a role in whether engagement is lengthy or more easy. Some babies engage before labor but when contractions get strong for a while and baby remains high at the brim, it may be because baby’s head is riding up on the brim or pressed against a portion of the inlet at an unfavorable angle.
When the bottom of the pelvis, the outlet, is more narrow than the top, labor can slow down here as well.
The good news is that the body is pliable, and muscles can be released, joints loosened, and fascia smoothed with simple and quick stretches or birth positions – when smartly chosen to match the need of the individuals birth.
Understanding inlet and outlet diameters can help match appropriate techniques and strategies for labor progress.
Why don’t I have Pelvic Types listed here?
The pelvic passage for birth is made from the shape of the bones around 3-dimension space. The beginning (inlet), end (outlet) and mobility of the pelvis lets us divide the passage into three levels. Each level is associated with a shape and the shape of the inlet can vary from circle to oblong to triangle. There is less variation in outlet shape but outlet width or narrowness will play a role in childbirth.
Pelvic types are widely used in childbirth literature as typing pelvises was a way to organize the various shapes and other bony attributes of the human pelvis. Unfortunately, the doctors who published a widespread categorization of the female pelvis were raised and educated in our racially biased society and they attributed racist values to their pelvic typing. Later research showed a gross overgeneralization to separate the scattering of shapes into basically what was not called but easily inferred “white female,” “white male” and “black” pelvises. The names are gynecoid, android, and anthropoid.
Later research showed a gross overgeneralization to separate the scattering of shapes into basically what was not called but easily inferred “white female,” “white male” and “black” pelvises. The names are gynecoid, android, and anthropoid.
Shaping is a result of nature, typing is a result of human interpretation. In other words, pelvises do have shapes, but categorizing them in “types” with values is based on human ideology around those values. “Pelvic types” is a human construct and on this topic has been typed in gender and racial ways that are not accurate, consistent or helpful, and have hurt people or lessened the quality of care some people receive, and limited care options, due to the categorization feeding racial inequity in the maternity system.
Kuliukas (2015). looked at 64 women and did not find a clustering of four types but a range throughout. The heavier, triangular pelvis did seem to appear with its unique characteristics, whereas there were many pelvises with a combination of round and oblong, or greater side-to-side and greater-front-to-back and everything in between without making two clear types of gynecoid or anthropoid.
Lia Betti of the UK offers a dynamic exposure of racist categorization of pelvis shapes and gives a re-interpretation of pelvic difference in Shaping birth: variation in the birth canal and the importance of inclusive obstetric care. For providers, pelvic understanding helps avoid poor technique among the slight differences in pelvic shape when forceps or ventouse are used. For providers and parents, noticing how the labor signals progress or a stall can help redirect care or choice of birth position so that that a position may chosen to optimize all the space available for the baby to move through the pelvis.
Pelvis width associated with bone mass distribution at the proximal femur in children 10–11 years old.
The variety of pelvic shapes, combined with the variety of fetal head presentations, plus size variations, mean that labors vary greatly. Engagement is the phase of labor most affected by pelvic type.
In the drawing, we see a round pelvic inlet shape and the correlating round shape of the pubic arch at the outlet.
A pelvis with a roundish brim which allows fetal rotation when the muscles and ligaments in and around the pelvis aren’t tight and twangy.
The pelvic arch in front would allow three fingers to cover the urethra during a “potty dance” – the type of grabbing yourself and try not to pee your pants dance of a child waiting to get to the bathroom. Buttocks are round.
Hip size doesn’t indicate the roomy inside and a petite woman can birth a large baby. When the pelvic floor and other soft tissues aren’t overly tight, the birth tends to go well and a posterior baby can rotate at several various phases of labor.
Narrower in the front
Narrow in the front, this pelvis occasionally catches the posterior baby’s forehead. Back it up and let it turn!
A more triangular pubic arch may hang quite low, giving a fundal height reading higher than the compact bump may seem to justify. Closely-set, small buttock “muscles” of the android make small roundish or triangular cheeks to her “bottom. ” The pelvis with a 2 finger arch, rather than the 3 finger width, means baby fits best with an anterior position and good flexion (chin tucking). Upright positions and more time for pushing and stronger pushing may be part of the story for some with a triangular brim.
” The pelvis with a 2 finger arch, rather than the 3 finger width, means baby fits best with an anterior position and good flexion (chin tucking). Upright positions and more time for pushing and stronger pushing may be part of the story for some with a triangular brim.
Narrow in the front, this pelvis occasionally catches the posterior baby’s forehead. Back it up and let it turn!
Good fetal positioning, good flexibility in the pelvic joints, and balance in the soft tissues help the natural labor progress. The posterior baby will hope to rotate before engagement or may not be able to rotate until the head fully passes the pelvis rotating on the perineum. Manually rotating the baby’s head may be an option if a skilled doctor or midwife is present. A little help for the shoulders may be needed as the result of those women with low slung pubic bones. They may catch a shoulder.
Tall women with average size babies often birth without an issue even with a triangular pelvis but this shape is in noted in the medical literature for a higher rate of posteriors since babies can have a harder time rotating while their forehead is in between the narrower front shape of the triangular inlet and it’s corresponding narrower outlet. The triangular inlet will be more of an issue for shorter, older, or heavier bodies. Why a heavier body? Because of the correlation with weight and low thyroid and weight and posterior presentation (there is a correlation between low thyroid and posterior presentation). An advantage can be achieved by helping baby into the Left Occiput Anterior before fetal engagement.
The triangular inlet will be more of an issue for shorter, older, or heavier bodies. Why a heavier body? Because of the correlation with weight and low thyroid and weight and posterior presentation (there is a correlation between low thyroid and posterior presentation). An advantage can be achieved by helping baby into the Left Occiput Anterior before fetal engagement.
A woman told me her doctor felt she may not be able to have a vaginal birth after she previously had a cesarean for birthing her first child. She asked me what I thought. While I acknowledge there are more challenges with a triangular pelvis for some of these labors, most births through an android pelvis are going to be able to finish by the woman’s own efforts –and her baby’s. I said:
Adding body balance and helping baby into position is extremely important when birthing with any smaller pelvis. Body balancing and birth positioning could make a positive solution for many in this situation. If the posterior baby can back up to turn to left occiput anterior and try again, there is much reason to expect a vaginal birth. To help the baby do this, Side-lying Release followed by an inversion of some type during a contraction or two can be necessary.
To help the baby do this, Side-lying Release followed by an inversion of some type during a contraction or two can be necessary.
More important than shape is fetal position and more important than fetal position is the balanced joints and soft tissues of the pelvis. Particular crucial is the freedom of the sacrum to shift a tiny bit and to rise up in late labor.
Releasing the tuberosacral ligaments in the back of the pelvis is a way to allow the sacrum to have mobility and therefore, more space for baby. The sacrum moves out of baby’s way, as it were, just before the body begins spontaneous pushing. Our blog has two good descriptions of this release.
Longest space is front-to-back
In this pelvis, the space for baby to enter is longer front-to-back and this spacing is true at the bottom, though baby may rotate a bit for the middle and then return to their starting position. The posterior baby fits more easily in this pelvis but babies are still usually anterior when they start labor. Either way, the Abdominal Lift and Tuck or a belly dance (figure 8 and front to back but not side to side moves) can be a help in helping baby get started into the pelvis (see instructions and what makes this work).
Either way, the Abdominal Lift and Tuck or a belly dance (figure 8 and front to back but not side to side moves) can be a help in helping baby get started into the pelvis (see instructions and what makes this work).
More posterior babies who are born vaginally may have the advantage of this pelvis’ longer front to back opening. Various vertical maternal positions and movements protect fetal engagement. Understanding the unique benefits of this pelvic type help birth finish by the mother’s own efforts.
Narrow front-to-back
The pubic arch is a wide 4 finger span what has been called the platypelloid pelvis, which is quite wide. Hips may seem wider side-to-side but mainly because the pelvis is flatter front to back. This allows for a flat (non-pregnant) belly look due to the short front-to-back distance of the bones.
At the bottom, the sitz bones are quite wide apart, more than the width of the person’s fist (if she can reach between them while lying down). Very few women have this situation but when a doctor spots it they may presuppose a cesarean is necessary. The best advantage for a vaginal birth is starting labor with baby in the Left Occiput Transverse position where baby is facing sideways. Body balancing can help baby get settled this way, but not simply gravity. Go for an broad and inclusive approach to body preparation, not strength but length in the muscles and more importantly, balance!
Very few women have this situation but when a doctor spots it they may presuppose a cesarean is necessary. The best advantage for a vaginal birth is starting labor with baby in the Left Occiput Transverse position where baby is facing sideways. Body balancing can help baby get settled this way, but not simply gravity. Go for an broad and inclusive approach to body preparation, not strength but length in the muscles and more importantly, balance!
Baby really needs to be in the LOT position to get INTO the pelvic brim for engagement. Long early labor is common, but if the baby isn’t LOT, the two days of labor will be all about getting baby rotated and strong contractions and mobility are essential. Once the baby is into the pelvis labor tends to move along, within 5-8 hours of engagement. Pushing may not be very long because the outlet of the pelvis is large. Using Daily Essentials: Activities for Pregnancy Comfort & Easier Childbirth, and Spinning Babies® Parent Class may help your baby get into a LOT or other ideal position.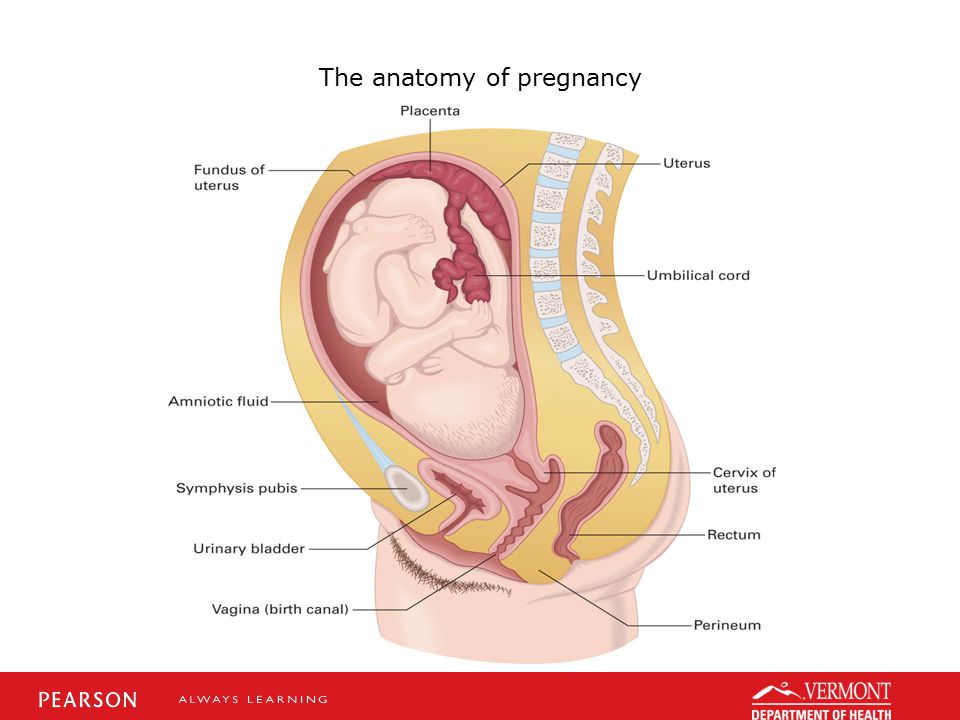
Pelvic cavities can have a MIX of opening or closing shapes
How to fit the pelvic shape into a label or category is less important to practice than having a set of skills to identify the relationship between the long axis of baby’s head with the short distance of the pelvic level where baby waits during a labor stall. This means, you may use a set of skills for helping babies through a diameter of the pelvis with a particular shape.
Knowing what is going on between the baby and the mother at the inlet or other diameters of the pelvis and what we can do to help when help is indeed appropriate. This is explained in the low-cost download, Spinning Babies® Quick Reference.
Pelvic Inlet diameters and lack of engagement
Occasionally a pelvic shape sets the fetal position. But this, I believe, is secondary to soft tissue “balance.” Some pelvises don’t accommodate posterior presentations. The baby must rotate or will not drop into the pelvis. When the mother can re-angle her pelvis to let the baby in (See steep inlet in Is baby engaged?). A birth stool, posterior pelvic tilt, and standing and leaning over a dresser feels right.
When the mother can re-angle her pelvis to let the baby in (See steep inlet in Is baby engaged?). A birth stool, posterior pelvic tilt, and standing and leaning over a dresser feels right.
Rarely, a pelvis is too small to let the baby enter the pelvis. When a pelvis is too small its called CephaloPelvic Disproportion (CPD, or baby’s too big). Rickets, injury or an actually too-big-baby may be the cause here. CPD is rare but does exist.
Before we suspect CPD in pregnancy, check to see if the baby is engaged. Until the baby is LOA or LOT and in one of those ideal starting positions, it’s too soon to call it CPD. We have an article on this called Will baby fit?
The Soft Tissues
The tone and relative symmetry of a woman’s uterine ligaments and muscles either makes room for baby or reduces room, if tight and twisty or so loose the uterus bends over.
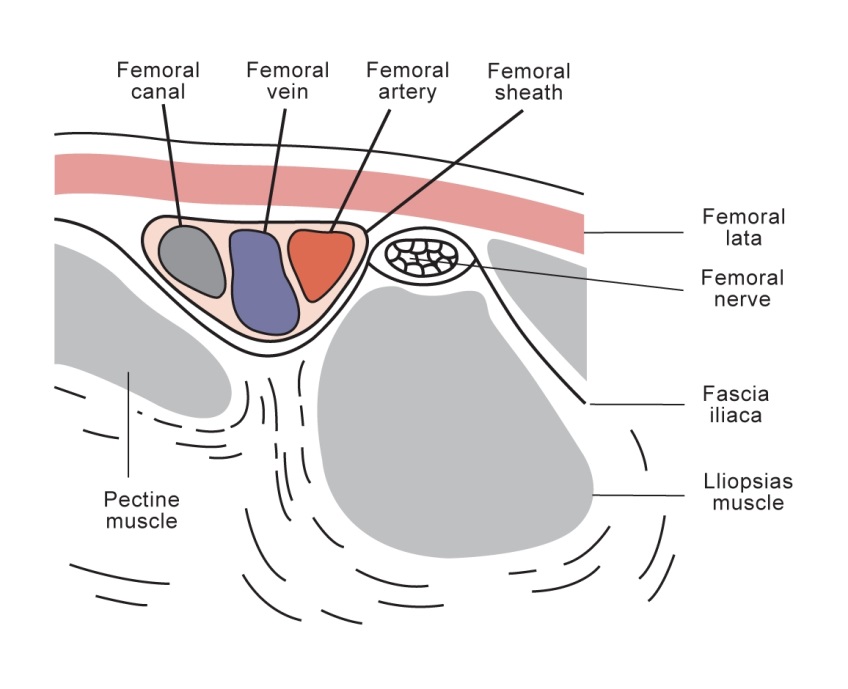
Our ability to stand depends on the psoas muscle pair. The psoas begins at T-12 vertebrae and sweeps around from the center of the sides of the spine over the pelvis to attach at the top of the thigh bone (femur). The muscle pair comes around like supporting arms, pulling up the legs so that our backs don’t fall over.
The muscle pair comes around like supporting arms, pulling up the legs so that our backs don’t fall over.
As the psoas comes across the pelvis, it makes a diagonal support for our organs. The support can be thought of as a shelf. When the uterus is large, at the end of pregnancy, a tight psoas can hold up a baby from descending and engaging in the womb. Many discomforts of the abdomen can stem from psoas tightness, but there are exercises to release the psoas. A great source is Liz Koch’s The Psoas Book.
As the psoas is balanced, so goes the birth!
So as I was saying… The Psoas.
The psoas is the lower triangle (pointing up) of two great muscle pair triangles that give core strength to the human body. The upper triangle (pointing down) is the trapezius, which is more of a diamond shape really, but I say two opposing triangles to help you to visualize of the polarity or pull between them to support our bodies.
The psoas additionally affects our pelvis and uterus because it shares the tendon connecting it to the thigh with another muscle pair, the iliacus. Together they team up to form the iliopsoas muscle group. The tone of the iliacus is dependent in part by the tone of the psoas. So, as the psoas goes, so goes the iliacus. This muscle spans from the top of the thigh (lesser trochanter) back over the pelvic brim to attach at the inside edge of the ilium (behind the hip bone but not as far to the center as the sacrum).
Together they team up to form the iliopsoas muscle group. The tone of the iliacus is dependent in part by the tone of the psoas. So, as the psoas goes, so goes the iliacus. This muscle spans from the top of the thigh (lesser trochanter) back over the pelvic brim to attach at the inside edge of the ilium (behind the hip bone but not as far to the center as the sacrum).
Pelvic floor
The pelvic floor is three layers of several muscles that rise into the lower pelvis to uplift the uterus, bladder, and other abdominal organs. The pelvic floor is open front to back to allow the urinary urethra, vagina, and rectum through to the body’s exterior. The lovely thing about the pelvic floor is the benefits of balance has far reaching benefits from better fetal positioning, easier and less painful birthing, better control and ease in peeing and pooping, walking, thinking, mood, breathing, and sexuality. Some benefits are very direct and others are secondary. A tight pelvic floor is not typically the best functioning, so beware of over kegeling.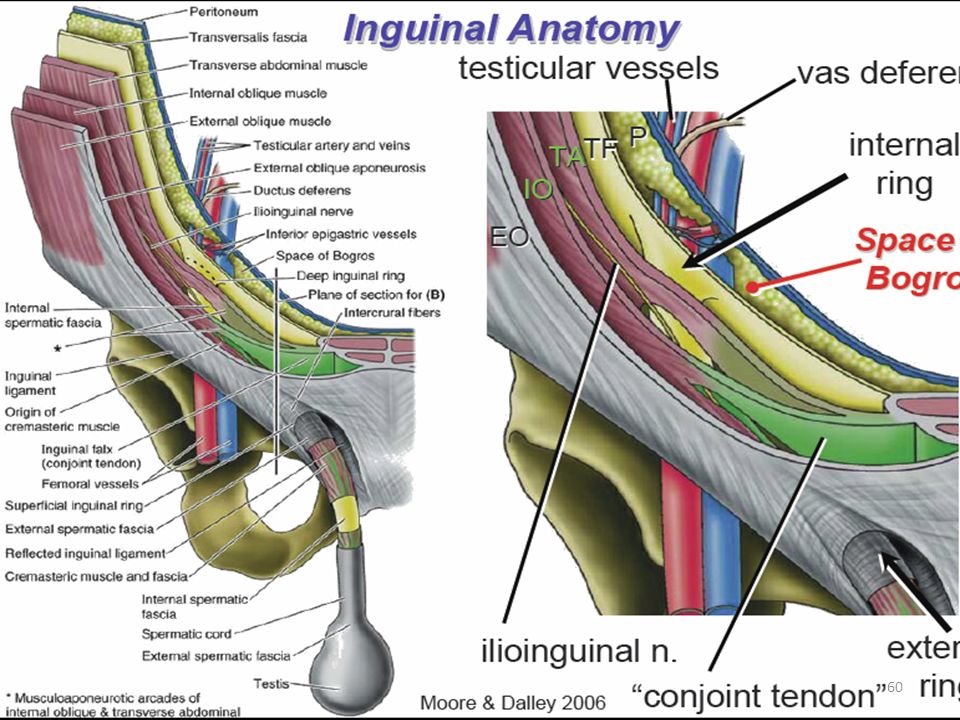 Combine the ball squeeze and anterior pelvic tilt shown in our daily activities
Combine the ball squeeze and anterior pelvic tilt shown in our daily activities
The pelvic floor should be considered as one unit since the three compartments work as one entity.
Uterine shape
The uterus is pear shaped before the first birth and apple shaped for future births, Jean Sutton, New Zealand midwife describes. The uterus is shaped to support a baby in a vertical position, and head down is common due to gravity.
Some spiraling and leaning to the right is considered normal for the uterus. But too much lean is not helpful for optimal uterine functioning, including birth. These are called dextrorotation and right obliquity.
The womb is supported by a series of ropes and slings called ligaments and fascia. The ligaments of the womb have a unique mixture of fibrous tissue and muscle cells. The muscle cells allow the ligaments to become longer during pregnancy so that the ligaments can grow with the uterus. Symmetry of the ligaments helps the womb be held upright.
Cervix
The cervix is part of the uterus, the part that opens for baby to be born. The cervix is pulled open by uterine contractions that first soften and thin the uterus. The cervix will be aligned properly, first aiming back in pregnancy and then, during birth, moving forward to line up with the birth canal.
Dilation is less painful when the cervix is not held to the side or back by spasming cervical ligaments. The baby’s head is better positioned with symmetrical ligaments because the lower uterine segment is not in a twist. We notice that Side-lying Release and Forward-leaning Inversion are two wonderful techniques (both from Carol Phillips) that help the uterus and baby line up with the cervix so it may open with less time and effort.
Fascia
The fascia is a 3D web of fibriles which are in constant movement. This web forms a membranous tissue that wraps every muscle, organ, and bone in the body. The fascia moves with the moving body but also seems to store the “memory” of an abrupt halt.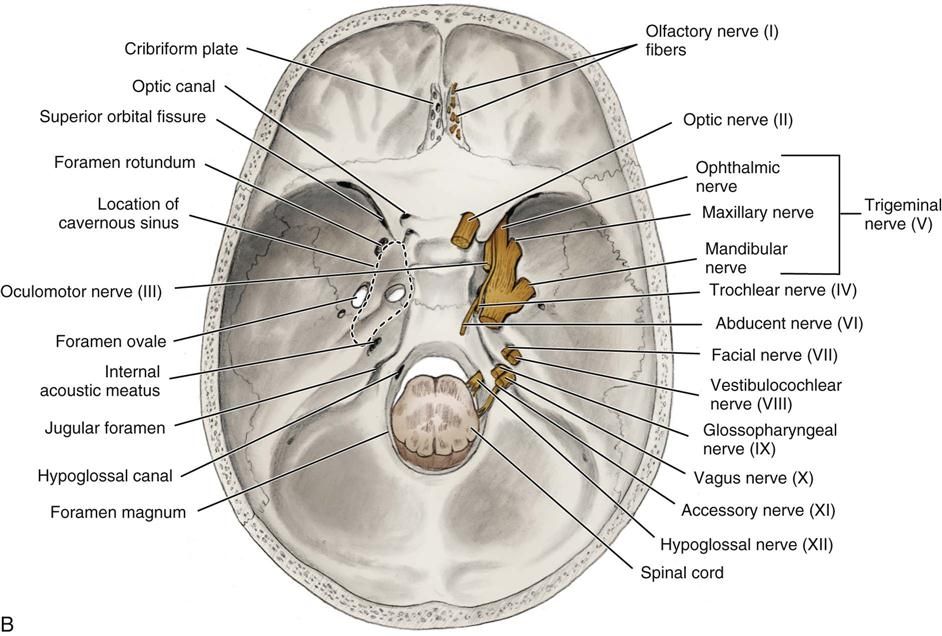 Whether that sudden stop has to do with a trauma or a long-time habit of poor posture, the fascia can thicken and then pull which can, over time, pull organs and bones out of alignment or symmetry. The function of the fascia in balance can be the most important contribution to overall health.
Whether that sudden stop has to do with a trauma or a long-time habit of poor posture, the fascia can thicken and then pull which can, over time, pull organs and bones out of alignment or symmetry. The function of the fascia in balance can be the most important contribution to overall health.
Fortunately, craniosacral therapists, fascial therapists and, to a lesser degree, chiropractic adjustments, can help to release the fascia and so, bring about a greater symmetry of the body. See more at Adrienne Caldwell’s blog. She shares insights and references about the fascia in her post which also talks about scar tissues after cesarean section and how multi-directional massage may reduce obstruction in motion and health.
Baby’s birth-related anatomy
The fetal head is heavy in comparison to the rest of the baby’s body. The vertical positions of walking, standing and sitting help the heavy head settle lower than the body during the third trimester, and sometimes in the second trimester.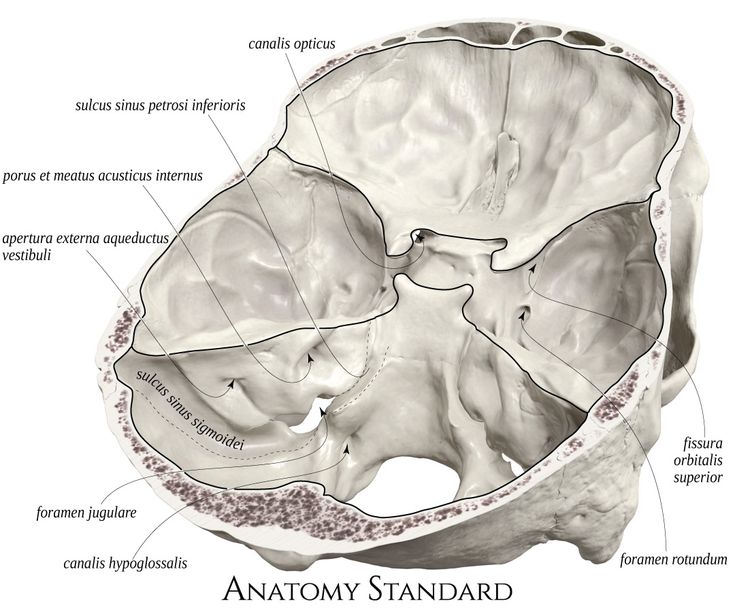
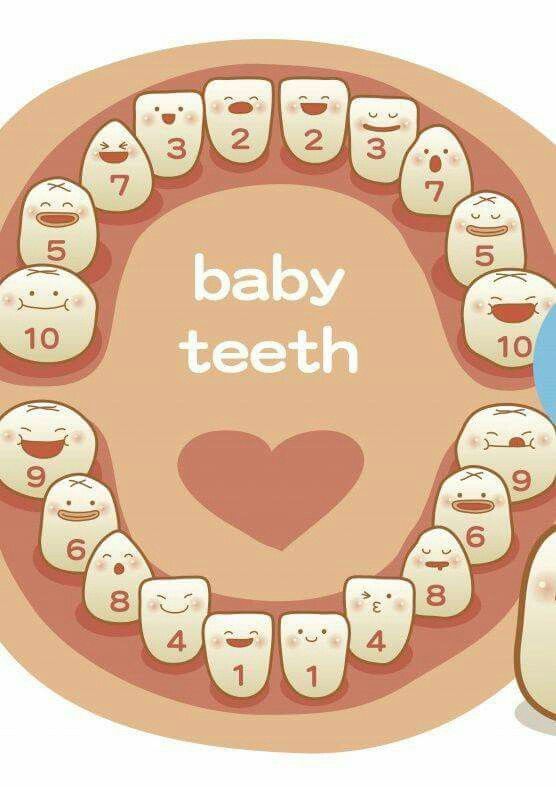
The fetal skull has not yet hardened and remains somewhat flexible for fitting through the pelvis. There are plates of bone and cartilage that are nearly finished coming together at birth. That nearly finished margin is what allows molding. These margins are called sutures.
The skull plates are held together by a coating for strong fascia. This membrane also wraps down the spine to the pelvis and legs. The fascia also connects to membranes that support the brain, called the tentorium cerebelli.
Which angle the head presses past, or onto, the bony pelvic passageway determines molding. When the crown of the head enters the pelvis first molding is most efficient. When a plate, rather than the margin between, or sutures, aims into the narrow part of pelvis, molding takes a long time and does less to reduce the diameter of the baby’s head. One example of this is the asynclitic baby. Second stage can take a long time and pushing can be quite strenuous when a baby is asynclitic.
The baby’s shoulders can also mold a bit for the birth process. The shoulder girdle is flexible and many times the shoulders are folded towards the chest for the actual emergence. Other times one shoulder comes out just ahead of the other in another natural variation to reduce shoulder breadth.
References:- Holistic Midwifery, Vol. II by Anne Frye
- Hands of Love by Carol Phillips
- The Female Pelvis by Blandine Calais-Germain
- A New Look at a Woman’s Body by Boston Womens’ Health Collective
- Gray’s Anatomy by Henry Gray
- Kuliukas, A., Kuliukas, L., Franklin, D., & Flavel, A.
 (2015). Female pelvic shape: Distinct types or nebulous cloud?. British Journal of Midwifery, 23(7).
(2015). Female pelvic shape: Distinct types or nebulous cloud?. British Journal of Midwifery, 23(7). - Cardadeiro, G., Baptista, F., Janz, K. F., Rodrigues, L. A., & Sardinha, L. B. (2014).
- Journal of bone and mineral metabolism, 32(2), 174-183.
- Maccioni, F., & Alt, C. D. (2018). MRI of the Pelvic Floor and MR Defecography. In Diseases of the Abdomen and Pelvis 2018-2021 (pp. 13-20). Springer, Cham.
You may also like to look at Amy Hoyt’s blog posts on Optimal Fetal Positioning with explanations and photos of the pelvis and baby (doll) on her blog: Natural Birth in Kitsap.
Page not found
Size:
AAA
Colour: C C C
Images On Off
Regular site version
RUENBY
Gomel State
Medical University
- university nine0018
- University
- History
- Manual
- Charter and Symbols nine0019 Educational activities
- Organization of the educational process
- International cooperation
- Quality management system nine0022
- Tips
- Faculties
- Chairs
- Divisions nine0022
- Primary trade union organization of workers
- University publications
- University Pride nine0019 Graduate-2021
- Primary organization "Belarusian Union of Women"
- Single window
- GomGMU in international rankings nine0022
- University structure
- Admission Committee
- University Biology Olympiad nine0022
- Targeted training
- Conclusion, termination of the "target" contract
- Benefits for young professionals nine0019 Passing score archive
- Freshman
- Schedule
- Exam Schedule nine0019 Information for students
- Internship and clinical residency nine0022
- Doctorate
- Postgraduate
- Master
- Distribution nine0022
- Professorial Advisory Center
- Faculty of advanced training and retraining nine0061
- Faculty of Foreign Students
- Tuition fees
- Registration and visas nine0022
- Useful information
- Admission rules
- Information on admission opportunities and conditions in 2022 nine0019 Official representatives of GomGMU for enrollment of students
- Home
Prediction of vaginal delivery in pregnant women with a scar on the uterus
Currently, the frequency of caesarean section in Russia ranges from 16 to 27%, reaching 40-50% in large perinatal centers [1].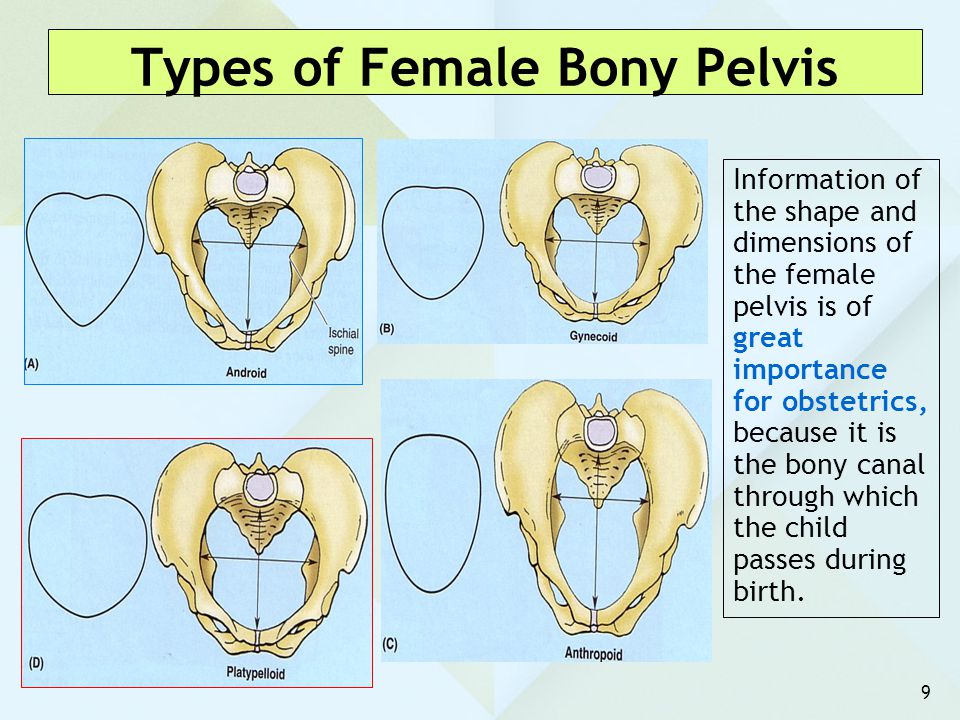 An increase in the frequency of abdominal delivery creates a new problem - the management of pregnancy and childbirth in women with a uterine scar [2-11]. To manage such labor, it is usually necessary to wait for the onset of spontaneous regular labor [1, 3, 7, 12, 13]. However, in the context of an increase in the cost of a pregnant woman's stay in a hospital and an increase in perinatal risk in patients of this category during pregnancy, such tactics are not always possible [14, 15]. To conduct a programmed birth, it is necessary to assess the readiness of the mother's body for childbirth [1, 2, 16, 17]. nine0003
An increase in the frequency of abdominal delivery creates a new problem - the management of pregnancy and childbirth in women with a uterine scar [2-11]. To manage such labor, it is usually necessary to wait for the onset of spontaneous regular labor [1, 3, 7, 12, 13]. However, in the context of an increase in the cost of a pregnant woman's stay in a hospital and an increase in perinatal risk in patients of this category during pregnancy, such tactics are not always possible [14, 15]. To conduct a programmed birth, it is necessary to assess the readiness of the mother's body for childbirth [1, 2, 16, 17]. nine0003
Changes in the levels of hormones such as progesterone and estrogen in pregnant women are known [18]. However, there is a lack of information about changes in the level of endogenous oxytocin in the blood of a pregnant woman. Oxytocin is a neuropeptide that is synthesized in the center of the paraventricular and supraoptic nuclei of the hypothalamus and released into the bloodstream through the posterior pituitary gland.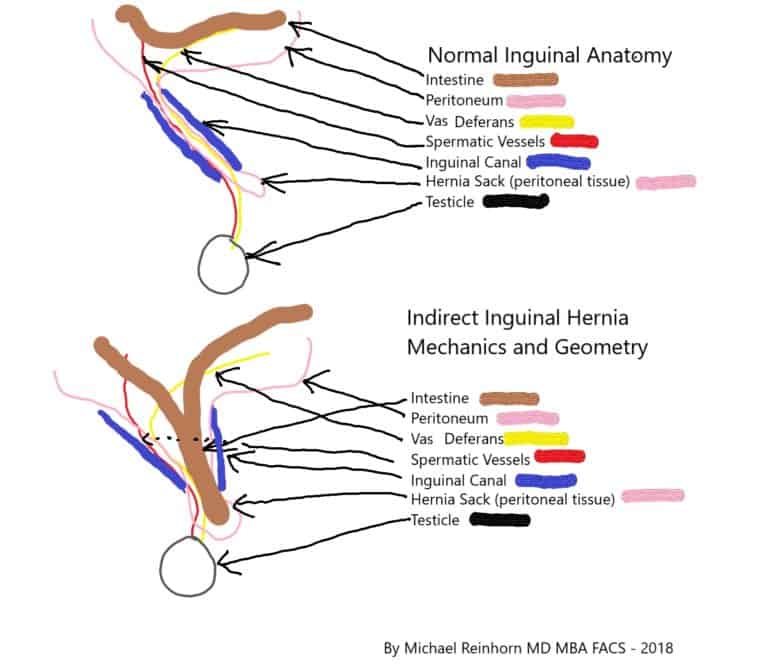 For its measurement, radioimmunoassay and enzyme immunoassay are used. At the same time, literature data regarding the measurement of endogenous oxytocin levels during pregnancy are contradictory. This is due to the fact that oxytocin has a short half-life (several minutes) and is found in blood plasma at low concentrations compared to other hormones. Most authors report an increase in the levels of endogenous oxytocin during pregnancy and the achievement of its maximum concentration by the time of delivery [12, 18, 19, 20].
For its measurement, radioimmunoassay and enzyme immunoassay are used. At the same time, literature data regarding the measurement of endogenous oxytocin levels during pregnancy are contradictory. This is due to the fact that oxytocin has a short half-life (several minutes) and is found in blood plasma at low concentrations compared to other hormones. Most authors report an increase in the levels of endogenous oxytocin during pregnancy and the achievement of its maximum concentration by the time of delivery [12, 18, 19, 20].
This indicator was used to predict the onset of labor, to assess the possibility of preparing patients with a uterine scar for programmed childbirth.
Material and methods
The study was conducted on the basis of the Perinatal Center of the Regional Clinical Hospital of the Omsk Region. The study included 284 pregnant women with a scar on the uterus in the period from June 2012 to May 2015. The main group consisted of 143 pregnant women with one scar on the uterus, delivered through the natural birth canal at full-term pregnancy. The comparison group included 141 pregnant women with an inferior scar on the uterus, delivered by caesarean section. All patients gave informed voluntary consent to the study. In 42 patients of the main group, the level of endogenous oxytocin in venous blood plasma was measured. nine0003
The comparison group included 141 pregnant women with an inferior scar on the uterus, delivered by caesarean section. All patients gave informed voluntary consent to the study. In 42 patients of the main group, the level of endogenous oxytocin in venous blood plasma was measured. nine0003
An analysis of the obstetric history, indications for a previous caesarean section, and the course of the postoperative period was carried out. The condition of the scar was assessed using ultrasound diagnostics with Doppler in the area of the scar on the uterus (ultrasound device Aloka SSD-3500, SonoScape SSI-800 Pro). Determination of the concentration of endogenous oxytocin in blood plasma was carried out by enzyme immunoassay (ELISA) using the Human oxytocin test system from ELISA Kit at the Central Research Laboratory of Omsk State Medical University. Statistical processing of the results obtained was carried out using standard methods of descriptive statistics (calculation of indicators, calculation of the mean, standard deviation).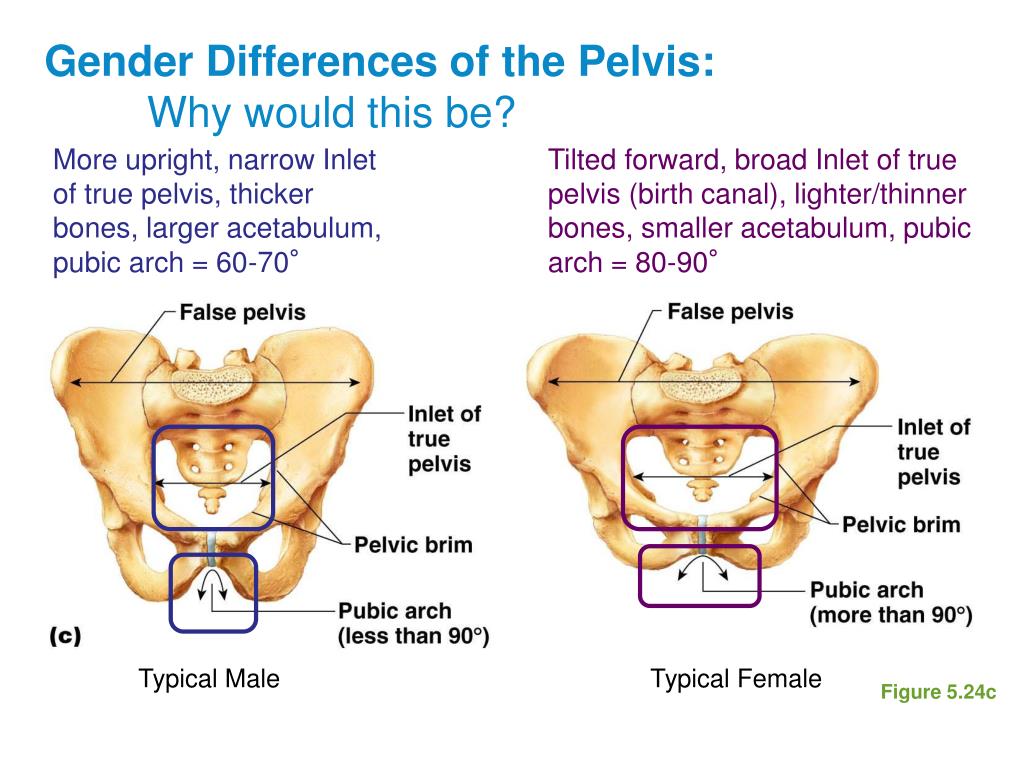 ROC 9 was used to compile prognostic models and identify possible prognostic factors for vaginal delivery.0237 * - analysis. The regression equation for determining the predictive model of the mode of delivery is as follows:
ROC 9 was used to compile prognostic models and identify possible prognostic factors for vaginal delivery.0237 * - analysis. The regression equation for determining the predictive model of the mode of delivery is as follows:
p=1/(1+e -582.96+1.216E3IR-44.07TCMP ),
where p is the desired value; e is a mathematical constant equal to 2.718; IR - resistance index; TSMR is the thickness of the uterine wall in the area of the scar. The regression equation for determining the predictive model for the term of delivery is as follows:
nine0002 term of delivery = 14.88–0.023 oxytocin level–0.64 Bishop score.Statistical analysis was performed using Microsoft Excel (2010), Statistica 6.0 (StatSoft, USA) and SSPS 16 (statistical package for the social science 16).
Results and discussion
All patients of the comparison group underwent a caesarean section in the lower uterine segment with a transverse incision.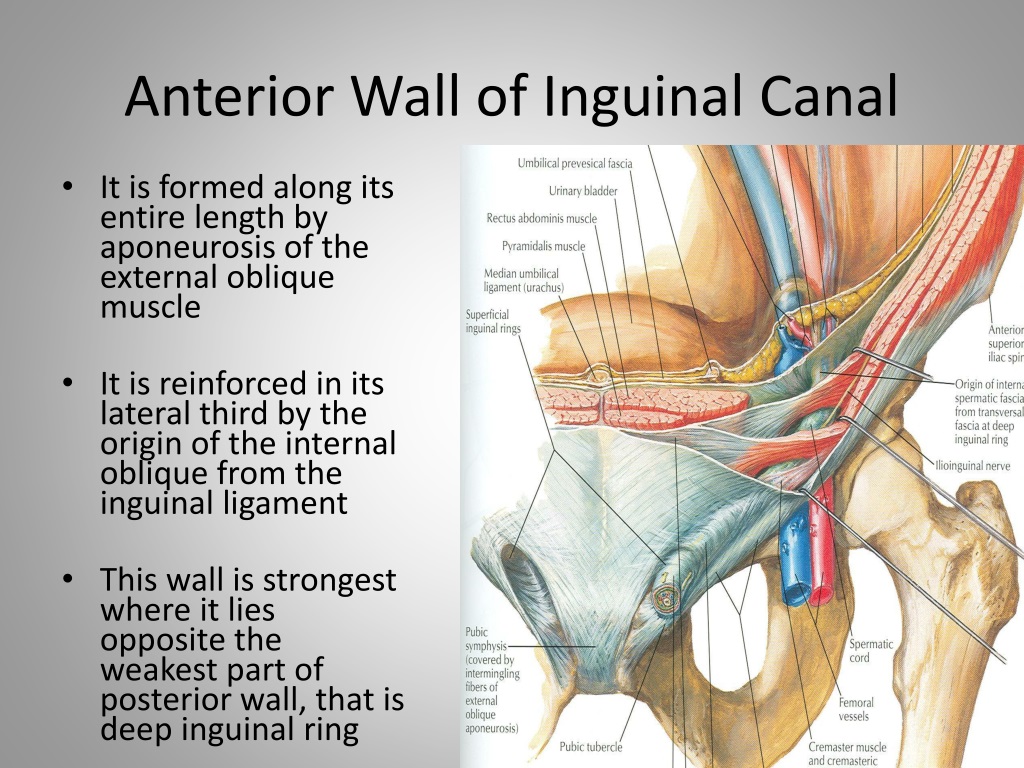
Among the complications of previous births in the main group, endometritis was noted - in 2.8% of patients and hypotonic bleeding - in 2.8% during operative delivery. In the comparison group, the following complications were most common: endometritis - in 4.3% of patients, hypotonic bleeding - in 3.6%, suppuration of the postoperative suture - in 1.4%, hematoma of the postoperative suture - in 0.7%; bladder injury - in 0.7%. nine0003
In the main group, there were no patients with a thickness of the uterine wall in the area of the scar from 1 to 2 mm. The thickness of the myometrium in the area of the scar 2-3 mm was observed in 8.4% of women, according to ultrasound, 3-6 mm in the area of the scar - in 70.6% of pregnant women. In the rest of the patients of the main group, ultrasound was not performed due to admission to the maternity hospital in the active phase of labor. At the same time, in the comparison group, the thickness of the myometrium in the scar area was less than 1 mm in 1. 4% of pregnant women, 1-2 mm in 46.8%, 2-3 mm in 28.4% of women, 3-6 mm with a discontinuous contour of the scar shadow - in 19,1%.
4% of pregnant women, 1-2 mm in 46.8%, 2-3 mm in 28.4% of women, 3-6 mm with a discontinuous contour of the scar shadow - in 19,1%.
The resistance index of the radial arteries in the area of the lower uterine segment was measured. The resistance index in the main group was 0.51±0.08, in the comparison group - 0.68±0.12. Thus, the resistance index in the comparison group was 1.3 times higher compared to those in the main group.
ROC analysis confirmed the existence of the possibility of predicting the method of delivery according to ultrasound data, however, it was found that the most valuable prognostic factors are the vascular resistance index and scar thickness, and the least significant are the vascularization index and fetal weight (Table 1). nine0003
Table 1. Results of ROC-analysis for the identified factors predicting the mode of delivery Note. AUC (area under ROC curve) - a statistical indicator - the area bounded by a certain curve and the abscissa axis (area under the ROC curve).
Based on the data in Table. 1, it can be argued that with a scar thickness of more than 3 mm, an index of vascular resistance of less than 0.555, satisfactory vascularization and a fetal weight of up to 3027 g, preference should be given to delivery through the natural birth canal. nine0003
Considering two possible modes of delivery (binary), binary logistic regression was used to make a prediction.
Based on the results of logistic regression of continuous and binary features, a predictive model was built for the possibility of choosing a method of delivery based on ultrasound data (Table 2).
Table 2. Model for predicting the mode of delivery based on the vascular resistance index and the thickness of the uterine wall in the scar area according to ultrasound data in pregnant women with a uterine scar Note. Wald (Wald test) a statistical test used to test the limitation of the parameters of statistical models estimated on the basis of selected data; df - number of degrees of freedom, used as an indicator of confidence based on test results; Exp - exponent, a number indicating the degree, which is written in the form of a superscript to the right of the number or symbol. nine0003
nine0003
This model explains 100% of the variance. Adding another parameter to the model - the vascularization index - does not have a significant impact on the prognostic ability, since this indicator has a low sensitivity - 37.7%. Thus, the model presented in Table. 2 can predict the choice of delivery method with a probability of up to 100%. Subsequently, the concentration of endogenous oxytocin in the blood was measured by ELISA and the "maturity" of the cervix was assessed according to the Bishop scale in 42 patients of the main group. nine0003
When conducting a correlation analysis with the calculation of the Spearman ® correlation coefficient, a statistically significant negative correlation of a strong degree was found between the number of days before delivery and the concentration of oxytocin (R = -0.95; p \u003d 0.000001) and the assessment of the cervix according to the Bishop scale (R=-0.95; p =0.000001). The higher the oxytocin concentration and the Bishop score, the closer the due date (see figure).
The results of correlation analysis in 42 patients of the main group. nine0003
A linear multiple regression model was used to generate the forecast. The results of the analysis confirmed that the relationship between the parameters is strong — R 2 = 0.93; p \u003d 0.00001 (R 2 - coefficient of determination).
To determine the cut-off threshold for the selected indicators, ROC analysis was used (Table 3). The readiness of the woman's body for childbirth was indicated by an oxytocin concentration of more than 349.55 μIU / ml and the degree of "maturity" of the cervix of 8 points on the Bishop scale. The model for predicting the term of labor based on the concentration of endogenous oxytocin and assessing the degree of "maturity" of the cervix in the examined pregnant women is presented in Table. 4.
Table 3. Results of ROC-analysis for the identified factors predicting the term of delivery
Table 4. Model for predicting the term of delivery based on determining the concentration of endogenous oxytocin and assessing the degree of "maturity" of the cervix according to the Bishop scale in pregnant women with a scar on the uterus
Model for predicting the term of delivery based on determining the concentration of endogenous oxytocin and assessing the degree of "maturity" of the cervix according to the Bishop scale in pregnant women with a scar on the uterus
The general model for predicting the delivery of pregnant women with a scar on the uterus can be presented in the form of the following table (Table 5).
Table 5. Results of ROC-analysis for the identified factors predicting the term of delivery
According to the data in Table. 5, prognostic criteria for vaginal delivery in pregnant women with a scar on the uterus are the thickness of the uterine wall in the scar area of more than 3.01 mm, but less than 7 mm; the resistance index is less than 0.55 and the concentration of endogenous oxytocin in venous blood plasma is more than 349.55 µIU/ml.
The data obtained served as prognostic factors in deciding the issue of conducting childbirth through the birth canal in the main group. nine0003
nine0003
After admission to the hospital 1 day before the scheduled birth, the pregnant women of the main group held a consultation at which the ultrasound data were discussed, the "maturity" of the birth canal was assessed, and the results of the study of the concentration of endogenous oxytocin. In 51% of patients, the condition of the cervix on the Bishop scale was estimated at 7-8 points, in 25.9% of women - at 5-6 points, and in 23.1% of pregnant women - less than 5 points. In 23.1% of patients, the cervix was prepared with mifepristone. 25.9% of patients were admitted to the hospital in the active phase of labor, the remaining 74.1% of pregnant women underwent programmed delivery. Amniotomy was performed at 6 am. Childbirth was carried out with constant monitoring of the cardiotocogram and control of the scar condition using ultrasound. Of all the patients, in 2.8%, with weakness of labor activity, labor intensification was carried out with oxytocin 2.5 IU intravenously. After delivery, in 50.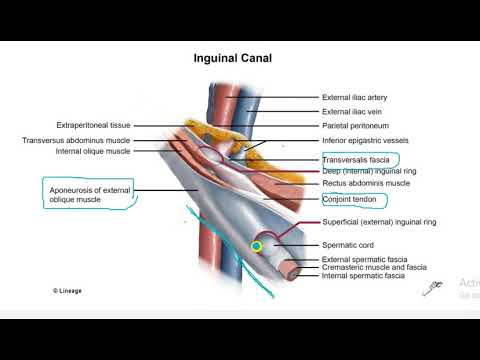 3% of puerperas, a control manual examination of the walls of the uterine cavity was carried out to assess the condition of the scar, and in 49.7% - ultrasound after the end of the third stage of labor. Blood loss during childbirth in the main group was 179.11±5.9 ml. Blood loss during childbirth in the comparison group was 584.04±30.25.
3% of puerperas, a control manual examination of the walls of the uterine cavity was carried out to assess the condition of the scar, and in 49.7% - ultrasound after the end of the third stage of labor. Blood loss during childbirth in the main group was 179.11±5.9 ml. Blood loss during childbirth in the comparison group was 584.04±30.25.
Terminals
1. For delivery through the natural birth canal of pregnant women with a scar on the uterus, the thickness of the uterine wall in the area of the scar (3.01 mm) and the resistance index in the radial arteries of the lower uterine segment (0.55) were significant.
2. The concentration of endogenous oxytocin in the blood (more than 34955 µIU/ml) and the evaluation of the "maturity" of the cervix on the Bishop scale (7-8 points) indicate the readiness of the pregnant woman's body for delivery.
3. The created model for predicting childbirth allows you to select a group of pregnant women with a scar on the uterus for their delivery through the natural birth canal and exclude complications of the birth act.