When do braxton hicks start in second pregnancy
Braxton Hicks contractions | Pregnancy Birth and Baby
Braxton Hicks contractions | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you feel tightening or cramping in your abdomen during your pregnancy, you may be having Braxton Hicks contractions. This is normal and not a sign that you’re ready to give birth.
Braxton Hicks contractions are sometimes called ‘false’ or ‘practice’ contractions.
What are Braxton Hicks contractions?
Braxton Hicks contractions are a tightening in your abdomen that comes and goes. They are contractions of your uterus in preparation for giving birth. They tone the muscles in your uterus and may also help prepare the cervix for birth.
Braxton Hicks contractions don’t cause labour and aren’t a sign that labour is beginning.
If you’re not sure whether what you’re experiencing is Braxton Hicks contractions or actual labour, contact your doctor or midwife. They will be able to tell by doing a vaginal examination — if there are no signs that your cervix is changing, it is not labour.
What do they feel like?
Braxton Hicks contractions feel like muscles tightening across your belly, and if you put your hands on your belly when the contractions happen, you can probably feel your uterus becoming hard.
The contractions come irregularly and usually last for about 30 seconds. While they can be uncomfortable, they usually aren’t painful.
If the pain or discomfort of your contractions eases off, they’re probably Braxton Hicks contractions.
When do you get them?
Braxton Hicks contractions occur from early in your pregnancy but you may not feel them until the second trimester. If this is your first pregnancy, you might start to feel them from about 16 weeks. In later pregnancies, you may feel Braxton Hicks contractions more often, or earlier. Some women won’t feel them at all.
Some women won’t feel them at all.
In late pregnancy, you may experience Braxton Hicks contractions more often — perhaps as much as every 10 to 20 minutes. This is a sign that you are preparing for labour — known as prelabour.
How are Braxton Hicks contractions different from labour pain?
There are some differences between Braxton Hicks contractions and true labour contractions that will help your doctor or midwife decide whether you are in labour:
Braxton Hicks contractions:
- don’t result in your cervix thinning and opening
- usually last for about 30 seconds
- can be uncomfortable, but usually aren’t painful
- come and go at irregular times
- usually occur no more than once or twice an hour (until late in the pregnancy), a few times a day
- usually stop if you change position or activity or go for a walk
- usually go if you have a warm bath or shower
Real labour contractions:
- result in your cervix thinning and opening
- last 30 to 70 seconds
- become very regular
- get closer together
- last longer as time goes by
- get stronger or come more often when you walk
- get stronger over time
Should I call my doctor or midwife?
If you are less than 37 weeks pregnant, contractions can be a sign of premature labour. Contact your doctor or midwife immediately if:
Contact your doctor or midwife immediately if:
- you feel pain, pressure or discomfort in your pelvis, abdomen or lower back
- the contractions become stronger, closer together and more regular
- there is fluid leaking or gushing from your vagina
If you are full-term, you may choose to wait until a bit later in your labour, depending on what you have arranged with your doctor or midwife. If your waters break, or your contractions are strong and 5 minutes apart, it’s time to go to the hospital.
As any stage of pregnancy, you should contact your doctor or midwife immediately if you:
- you have persistent pain in your abdomen
- you have vaginal bleeding
- you notice your baby’s movements have slowed or stopped
- you feel very unwell
If you are in doubt, don’t hesitate to call your doctor or midwife for advice.
How can I ease the discomfort?
Braxton Hicks contractions are normal and don’t need treatment. But if you feel uncomfortable, you can try:
But if you feel uncomfortable, you can try:
- lying down
- taking a walk
- relaxing in a warm bath
- having a massage
It may help to practise your breathing exercises during your Braxton Hicks contractions.
Sources:
Raising Children Network (23 weeks pregnant), RANZCOG (Labour and birth), Elsevier Patient Education (Braxton Hicks Contractions)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Giving birth - stages of labour
- Health professionals involved in your pregnancy
- Signs of premature labour
Need more information?
Pregnancy at week 22
By week 22, some parts of your baby’s body are fully formed, while some women experience Braxton Hicks contractions about now.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Giving birth - contractions
Contractions are when the muscles in your uterus tighten and then relax. They occur throughout the later stages of your pregnancy.
Read more on Pregnancy, Birth & Baby website
What happens to your body in childbirth
During childbirth, your body's hormones, ligaments and muscles, as well as the shape of your pelvis, all work together to bring your baby safely into the world.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - uterus
The uterus is your growing baby’s home during pregnancy. Learn how the uterus works, nurtures your baby and how it changes while you are pregnant.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
38 weeks pregnant | Raising Children Network
38 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
26 weeks pregnant | Raising Children Network
26 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Giving birth - early signs of labour
You can know the early signs of labour, even if you cannot predict when your labour will begin. Find out also what to do if something appears to be wrong.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth
From conception to giving birth, a woman's body goes through many physical changes. Learn what happens to your body during pregnancy and labour.
Learn what happens to your body during pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Understanding and Identifying Braxton Hicks Contractions
- Home
- OB/GYN Knowledge Center
- Understanding and Identifying Braxton Hicks Contractions
The doctors and midwives at All About Women of Gainesville and Lake City, FL discuss how you can distinguish between Braxton Hicks vs.
 real labor contractions
real labor contractionsWhether you're 22 or 35 weeks along, pregnant with your first baby or your third, Braxton Hicks contractions can take you by surprise and even trick you into thinking you're entering labor. Also called "warm- up" or "toning" contractions, Braxton Hicks contractions are your body's way of preparing the uterus for labor. And they can send even the most seasoned mother to the hospital – only for her to find out that her Braxton Hicks are causing "false labor."
Many women report having more of these contractions later in the day when they are tired or haven't had enough to drink. If you're having lots of Braxton Hicks contractions, don't stop your normal activities, but do make sure you stay well hydrated and take some time to get off your feet during the day.
Understanding Braxton Hicks contractions during pregnancy - when they occur, what they're like, and how to relieve them, as well as how your true labor contractions will differ - can help you interpret what is occurring in your body, and when it's really time to go to the hospital or call your OB doctor.
When Do Braxton Hicks Contractions Start During Pregnancy?
As with most all pregnancy matters, Braxton Hicks contractions are different for every woman. All pregnant women experience these contractions but not all expecting mothers are aware they occur. Some women don't feel any kind of contraction until delivery day, and that is completely normal. You don't need to worry if you haven't felt any warm-up contractions.
Many women, however, do feel their Braxton Hicks contractions, usually any time after the 20- week marker of pregnancy. While some women feel them this early, others may not experience any until the later weeks of pregnancy. In second and third pregnancies, some mothers say they're Braxton Hicks contractions start earlier.
What Do Braxton Hicks Contractions Feel Like?
Braxton Hicks contractions often begin very mildly, feeling like a tightening sensation across the uterus. They may become stronger in the later weeks of pregnancy. Their strength and recurrence is how expecting mothers confuse them with true labor contractions.
Their strength and recurrence is how expecting mothers confuse them with true labor contractions.
The job of a true labor contraction is to dilate the cervix. Braxton Hicks contractions, you may remember, work only to tone the uterus and do not cause the cervix to dilate. Of course, you can't tell if your cervix is dilated unless you go in and have your obstetrician or midwife check you, but Braxton Hicks contractions have other distinct characteristics like:
- Their intensity doesn't change. Braxton Hicks contractions usually remain fairly weak, while true labor contractions grow increasingly intense.
- They go away with a change in activity. If you're sitting down and having Braxton-Hicks contractions, they will usually go away if you get up and walk around. If you've been moving around, the opposite is true – try resting for a while and the contractions should go away. True contractions, on the other hand, do not go away with changes in activity.

- They feel like a tightening across the front of the uterus. True labor contractions, on the other hand, wrap from the top of the abdomen down, and wrap across the front of the abdomen and around the back.
- They are irregular. The length and frequency of Braxton Hicks contraction varies. True labor contractions occur at regular intervals and last at least thirty seconds. Real contractions will also grow longer and closer together.
What Causes Braxton Hicks Contractions?
While they may occur without reason, there are some known life factors that cause women to have Braxton Hicks contractions:
- Strenuous exercise or activity
- Dehydration
- Sex, particularly orgasm
- Someone touching the mother's belly
Many women report having more of these contractions later in the day when they are tired or haven't had enough to drink. If you're having lots of Braxton Hicks contractions, don't stop your normal activities, but do make sure that you stay well hydrated and take some time to get off your feet during the day. A warm bath or a cup of tea can also help to relieve your contractions.
If you're having lots of Braxton Hicks contractions, don't stop your normal activities, but do make sure that you stay well hydrated and take some time to get off your feet during the day. A warm bath or a cup of tea can also help to relieve your contractions.
Accompanying Signs of Early Labor
If you are getting close to your due date and are experiencing contractions, you should be aware of the signs of early labor that accompany true labor contractions:
- Lower back ache, or pain in your abdomen or pelvis
- Loose stools
- Brown-tinged mucous
- Watery discharge
- Increased urination
If you experience any of these signs along with regularly occurring contractions, you are probably in labor. You may not need to go to the hospital right away, but you should contact your OB doctor or midwife to let them know what symptoms you are experiencing and how far apart your contractions are.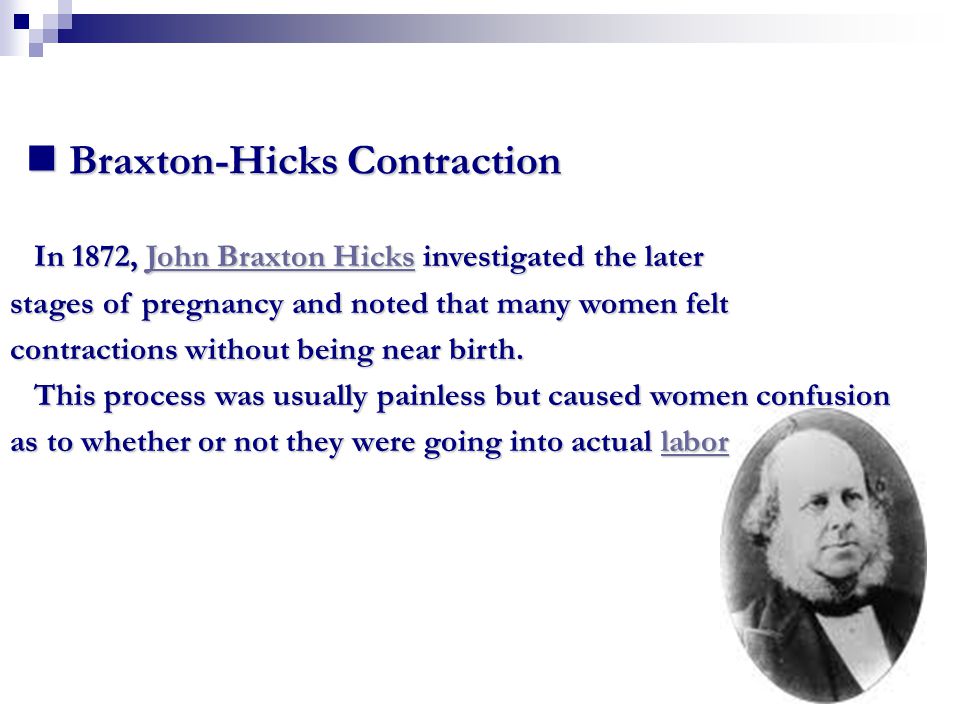
Braxton Hicks contractions present themselves so differently in successive pregnancies that even the most seasoned mothers can be confused , not to mention first-time mothers. The best way to have peace of mind about these contractions, besides educating yourself, is to stay in close contact with your OB doctor and midwife.
Florida's obstetricians and midwives at All About Women want you to feel confident with every step of your pregnancy. If you're concerned about contractions, or think you a re pregnant and need to ensure you and your baby are healthy, contact our Gainesville or Lake City office to schedule an appointment today.
Related KC and Blog Articles
Contact Us Knowledge Center
Braxton Hicks contractions for how long - 25 recommendations on Babyblog.ru
For fifteen years now we have been living not just in the new century, but in the new millennium. For twenty years we have been using computers and the Internet everywhere. It would seem that with the progress of technology, people have enormous opportunities for the exchange of progressive information, knowledge and best practices. But the real picture is almost the opposite: false, untruthful information, often presented under the “sauce” of intimidation and deceit, is spread and accepted by people faster and easier than truthful and useful information. nine0003
It would seem that with the progress of technology, people have enormous opportunities for the exchange of progressive information, knowledge and best practices. But the real picture is almost the opposite: false, untruthful information, often presented under the “sauce” of intimidation and deceit, is spread and accepted by people faster and easier than truthful and useful information. nine0003
The worst thing that is now observed in medicine is the filing of many conditions, including quite normal ones, and some diagnoses as something terrible and dangerous, threatening a person’s life, requiring aggressive and extensive treatment immediately. Obstetrics is no exception. On the contrary, in recent years this branch of medicine has grown in a number of countries into a kind of machine of deliberate harm to a pregnant woman and her unborn child.
The concept of "commercial diagnosis", introduced by me ten years ago, is no longer denied by many people and is even used by them in everyday life, conversations and discussions of the situation in the healthcare system. Both doctors and people of other specialties began to talk and write about obstetric aggression. Nevertheless, the number of fictitious diagnoses that do not exist in most countries of the world is striking not only by their backwardness, but also by the lack of a logical analysis of the situation, signs, and examination results when they are made (more precisely, invented). nine0003
Both doctors and people of other specialties began to talk and write about obstetric aggression. Nevertheless, the number of fictitious diagnoses that do not exist in most countries of the world is striking not only by their backwardness, but also by the lack of a logical analysis of the situation, signs, and examination results when they are made (more precisely, invented). nine0003
INCOMPATIBILITY OF THE SPOUSES
Usually such a diagnosis sounds when:
- unsuccessful planning of pregnancy and infertility;
- loss of pregnancy, even the first or one;
- spontaneous habitual miscarriages;
- in exceptionally "striking cases" in the presence of one child or several healthy children.
If we talk about some kind of “spousal incompatibility”, then we can only talk about psychological incompatibility or sexual temperaments, but there is no other “incompatibility”. nine0003
Allergic reaction to semen is extremely rare in humans, but the diagnosis would be allergy, not incompatibility.
If a married couple cannot conceive, it may be infertility, which requires proper diagnosis. There are different types of infertility or infertility factors, which means that there will be a different approach to the examination of a married couple and treatment.
Very fashionable commercial HLA (human leukocyte antigen) testing in the world of progressive medicine is used in organ and tissue transplantation, to diagnose a number of autoimmune diseases, confirm paternity and monitor the effectiveness of the treatment of a number of diseases, but has nothing to do with conceiving children, carrying a pregnancy , and even more so with the "incompatibility of the spouses." "Genetic incompatibility of partners" is another invention for imposing an expensive examination and treatment. nine0003
If one of the partners has affected genes, that is, there are changes in the form of mutations, then such changes may be associated with problems in conceiving and bearing offspring, but this is not incompatibility. This may be a specific diagnosis (disease, syndrome) on the part of one or both partners. And the recommendations of some doctors to carry out IVF in such cases using the same sexual material, or to find a sexual partner outside of marital relations in order to conceive a child, do not always sound professional. nine0003
This may be a specific diagnosis (disease, syndrome) on the part of one or both partners. And the recommendations of some doctors to carry out IVF in such cases using the same sexual material, or to find a sexual partner outside of marital relations in order to conceive a child, do not always sound professional. nine0003
TOXICOSIS
The concept of "toxicosis" appeared in Soviet obstetrics in the early 1990s, when everyone in the world of progressive medicine had already completely abandoned this concept. Toxicosis means “a state of poisoning” (toxins are poison), and the logical conclusion is that this is pregnancy poisoning, that is, the embryo / fetus poisons the body, and therefore the life of the expectant mother. But doesn’t a mother poison her unborn child with poor-quality food, water, medication, smoking, and even drinking alcohol? nine0003
In the West, they quickly realized the absurdity of such a “diagnosis” and tried to switch to the concept of “preeclampsia”, that is, a condition associated with gestation (pregnancy). However, this definition was also abandoned very quickly, because the more science and medicine developed, the faster the exchange of advanced information and experience, the faster doctors began to understand that many “strange” phenomena during pregnancy are not diseases, but variants of the norm. and vice versa - all complications of pregnancy have specific specific names, which should appear as diagnoses. nine0003
However, this definition was also abandoned very quickly, because the more science and medicine developed, the faster the exchange of advanced information and experience, the faster doctors began to understand that many “strange” phenomena during pregnancy are not diseases, but variants of the norm. and vice versa - all complications of pregnancy have specific specific names, which should appear as diagnoses. nine0003
In post-Soviet medicine, a completely normal phenomenon - nausea and vomiting at the beginning of pregnancy - is still called early toxicosis (in the rest of the world these are just unpleasant symptoms of this condition), and edema, which for the vast majority of women are normal, hypertension in pregnancy, preeclampsia, eclampsia, and about ten other complications of pregnancy, which are independent diagnoses, and not a comprehensive mythical toxicosis. nine0011 Remember: there is no such diagnosis - toxicosis!
UTERINE TONE / HYPERTONE
For the first time, normal uterine contractions from the beginning of pregnancy to the end of childbirth were described by the English physician John Braxton Hicks in 1872. Mistakenly, such contractions are called "training bouts", which is not true. In the publication of this doctor, it was about normal uterine contractions throughout pregnancy, and not before childbirth.
Mistakenly, such contractions are called "training bouts", which is not true. In the publication of this doctor, it was about normal uterine contractions throughout pregnancy, and not before childbirth.
The uterus is a muscular organ, therefore, just like any muscle, it has its own mode of contraction, which depends on many factors and can be observed both outside of pregnancy and during pregnancy. nine0011 The diagnosis of "tonus" or "hypertonicity" was invented by post-Soviet ultrasound doctors and the rest of the world does not exist in obstetrics, therefore it does not require treatment, and even more so inpatient, with the use of a large number of drugs that have also not been used in modern obstetrics for a long time ("Papaverine" , "No-shpa", "Viburkol", vitamin E, magnesia, etc.)
THREAT OF LOSS OF PREGNANCY
I have already raised the topic of "threat of abortion" more than once, especially since it is consonant with the topic of "preservation of pregnancy". In reality, the threat to a pregnant woman comes more from the medical staff than really from someone else or something (nature), because it is people who intimidate, put pressure on the psyche with negative scenarios, escalate the situation, harm with unsafe treatment. nine0003
In reality, the threat to a pregnant woman comes more from the medical staff than really from someone else or something (nature), because it is people who intimidate, put pressure on the psyche with negative scenarios, escalate the situation, harm with unsafe treatment. nine0003
The only diagnosis in obstetrics that has a word root consonant with “threat” is “threatened abortion”. This diagnosis is made according to strict criteria, and not because of "tonus / hypertonicity of the uterus", it does not require treatment, because there is no cure.
All other types of threats are fictitious diagnoses. In obstetrics, it is customary to talk about risk factors and determine the group or degree of risk for the development of one or another pregnancy complication (low risk, high risk). Against the background of the presence of various risk factors, pregnancy can proceed quite normally and end safely. nine0003
RH AND GROUP CONFLICT
In modern obstetrics there is no such concept or diagnosis as "Rh conflict" or "group conflict". The worst thing is that such a “diagnosis” intimidates a married couple to such an extent that she refuses to conceive children: since it is absolutely impossible to get pregnant, then we are not trying. The presence of different blood types, as well as different Rh factors, is a normal phenomenon in human life and is not considered any conflict.
The worst thing is that such a “diagnosis” intimidates a married couple to such an extent that she refuses to conceive children: since it is absolutely impossible to get pregnant, then we are not trying. The presence of different blood types, as well as different Rh factors, is a normal phenomenon in human life and is not considered any conflict.
In modern obstetrics, there are more than 50 blood markers (antigens) for which antibodies (immunoglobulins) can be produced, and this condition is called alloimmunization, or sensitization. nine0003
During pregnancy, antibodies can be produced in the mother's body against fetal antigens, cross the placenta and destroy the fetal red blood cells, leading to anemia and fetal hemolytic disease. If hemolytic disease of the fetus occurs, then it will end either with the death of the fetus, or the birth of a child with hemolytic disease of the newborn. Unfortunately, many doctors do not understand the types of jaundice, do not know the current norm of bilirubin levels, so the diagnosis of "hemolytic disease of the newborn" in most cases turns out to be false, which means that aggressive treatment of such children is absolutely inappropriate. nine0003
nine0003
If we talk about really rare "blood conflicts", then they arise not between a man and a woman, but between a mother and a fetus. Therefore, the enthusiasm of some doctors for the search for antibodies in the blood of a man is so surprising. Also depressing is the fact of searching for antibodies in the mother's blood after childbirth in order to make a diagnosis of "hemolytic disease of the newborn." And the use of such a dangerous procedure as plasmapheresis, supposedly to “cleanse the blood” of antibodies, is shocking. This procedure has passed into the category of commercial ones, because it is expensive and brings considerable income to those who carry it out. nine0003
For the prevention of Rh sensitization in the mother, vaccination with immunoglobulins (D-antibodies) has long been used, which is carried out in the absence of a woman's own antibodies during pregnancy, after childbirth, abortion, and a number of procedures. This prophylaxis does not protect the current pregnancy, but it does prevent hemolytic disease of the fetus and newborn in subsequent pregnancies.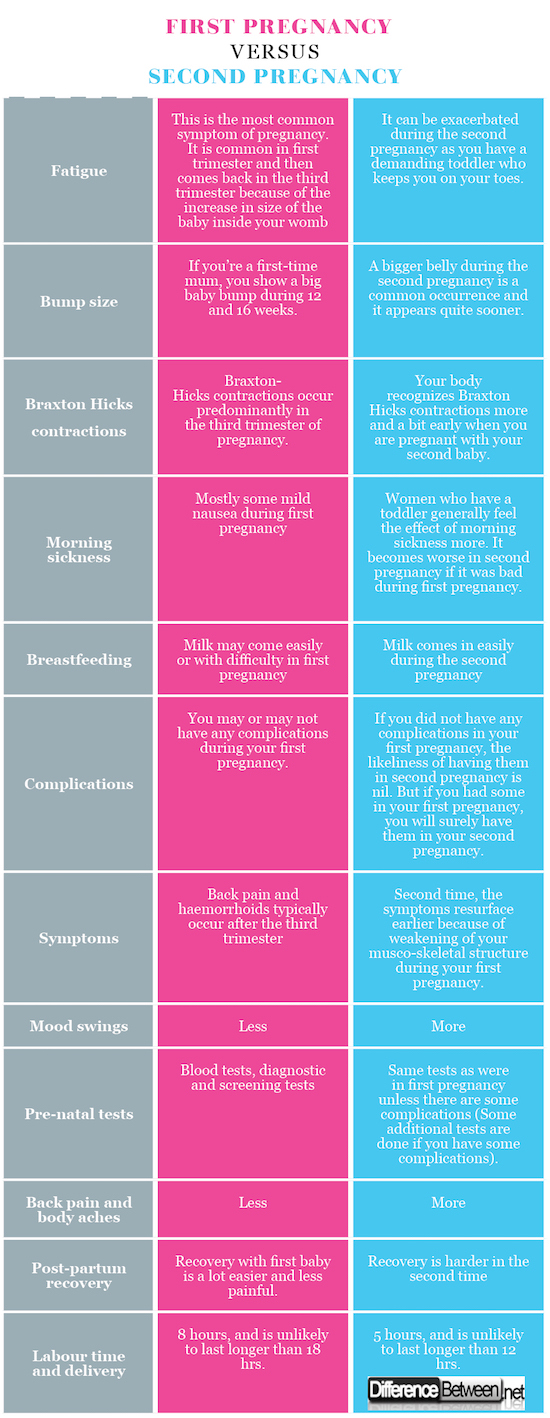 However, it is ineffective in preventing sensitization for all other blood markers.
However, it is ineffective in preventing sensitization for all other blood markers.
HEREDITARY (GENETIC) THROMBOPHILIA
In post-Soviet obstetrics, over the past decade, there have been an extremely large number of positions of geneticists who do not understand prenatal genetic screenings and genetics in general, and hematologists (they are fashionably called hemostesiologists, hemastesologists), who do not understand blood and know absolutely nothing about normal changes in the composition of the blood, especially the blood coagulation system in pregnant women.
During pregnancy, blood viscosity increases despite an increase in blood (plasma) volume and a decrease in the concentration of many substances. Therefore, from the very first weeks, pregnancy is accompanied by a hypercoagulable state. It can persist for several weeks, not only after childbirth, but also after abortions and missed pregnancies. This is not a pathological condition, but normal physiological changes. nine0003
nine0003
D-dimer, according to the level of which heparin is prescribed to all pregnant women in a row, is a derivative of fibrinogen. Both of these indicators increase from the first weeks of pregnancy, which is absolutely normal.
Commercially profitable genetic testing leads to the diagnosis of thrombophilia being overused, although several dozen diseases are known to be associated with disorders of the blood clotting process. There are several types of hereditary thrombophilia that have a clear name, and not just "genetic thrombophilia". There are also acquired thrombophilias, which often turn out to be not a separate diagnosis, but a laboratory and clinical symptom of other diseases. nine0003
The presence of genes and their combinations does not mean that a person has thrombophilia (and many other diseases). This may indicate a hereditary predisposition, but without clinical and laboratory confirmation, and even more so outside the state of pregnancy, such diagnoses are not made and blood thinning drugs are not prescribed.
Bed rest in hospitals, where pregnant women are kept for weeks and even months, is recognized as the most dangerous factor in the formation of blood clots. It is also surprising that before pregnancy, many women had no idea about their "genetic disease", they took hormonal contraceptives that are incompatible with thrombophilia, and then after giving birth they continue to take them, forgetting about the terrible diagnosis. However, doctors quickly forget about him too. nine0003
OLD PLACENTA
The diagnosis of "old placenta", which often sounds in conjunction with the diagnosis of "uteroplacental insufficiency", was born by the same ultrasound specialists.
The placenta is a dynamic organ that undergoes regular changes as pregnancy progresses. Therefore, we can safely say that not only the placenta is aging, but also the fetus itself. The woman also gets older by 9 months!
Placenta insufficiency can be spoken of only when it does not fulfill its function.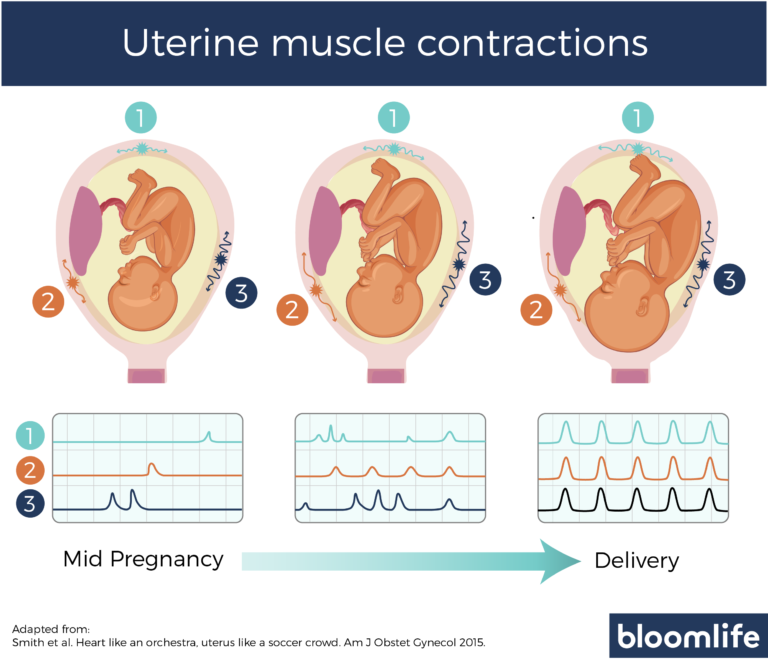 Just as there is heart or liver failure, placental failure can also exist. But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about? nine0011 But what is depressing in all these stories with placentas is that a woman is offered different schemes for "rejuvenation" of the placenta, which necessarily include two fuflomycins - "Kurantil" and "Actovegin". Remember: the placenta cannot be rejuvenated!
Just as there is heart or liver failure, placental failure can also exist. But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about? nine0011 But what is depressing in all these stories with placentas is that a woman is offered different schemes for "rejuvenation" of the placenta, which necessarily include two fuflomycins - "Kurantil" and "Actovegin". Remember: the placenta cannot be rejuvenated!
In addition, the diagnosis "placentitis" suddenly became fashionable, which was indeed used in veterinary medicine for a very long time, but never in obstetrics! Turning pregnant women into female animals?
oligohydramnios/polyhydramnios tendencies
When I hear or read about the diagnosis of oligohydramnios/polyhydramnios tendency, I want to respond with a great sense of humor: “You know, we all have a lot of tendencies. For example, there is a real tendency with age to get senile dementia. You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby. nine0003
For example, there is a real tendency with age to get senile dementia. You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby. nine0003
The extremely common diagnosis of "trends" is often the product of ultrasound specialists who somehow do not use the logical thinking of obstetrician-gynecologists to ask a simple question: what kind of nonsense is this?
The state of amniotic fluid is only in the form of a norm, polyhydramnios and oligohydramnios, but there are no trends. These conditions are determined by measuring one pocket (column) of amniotic fluid in centimeters, but most often by the sum of four (namely four, not two or three) pockets, that is, by determining the amniotic index of amniotic fluid (AIF). After 20 weeks, the normal AIH ranges from 8 to 24 cm, of course, adjusted for the condition of the fetus and other ultrasound findings. nine0003
nine0003
Oligohydramnios and polyhydramnios are practically not treated, therefore, volumetric regimens of antibiotics and fuflomycins, the same "Kurantil", "Actovegin", "Khofitol", "Viferon", "Tivorin" and other similar drugs, and with the obligatory presence of a pregnant woman in a hospital , is a manifestation of medical illiteracy.
fetal asphyxia
Most often, the diagnosis of fetal asphyxia appears in the conclusions of pathologists after pregnancy loss, as well as in stillbirth. Surprisingly, it is specialists who do not see the difference between hypoxia and asphyxia, who are just obliged to find out the cause of abortion and fetal death. nine0003
The baby is not breathing inside the uterus. His lungs don't work. Everything he receives from his mother in the form of nutrients and oxygen comes through the umbilical cord. The concept of hypoxia implies a violation of blood flow in the vessels of the fetus (impaired hemodynamics) due to the presence of usually two parallel conditions - anemia (anemia) and acidosis (increased acidity) due to oxygen starvation of tissues.
Asphyxia is suffocation, which is associated with a decrease and even cessation of oxygen supply through the respiratory system. At the same time, the oxygen content in the blood drops sharply, which leads to brain death and death. Since the fetus is not breathing, it cannot have asphyxia. nine0011 Asphyxia of a newborn is said when a foreign body (amniotic fluid, mucus, meconium, blood, etc.) enters the child's respiratory tract after birth with the first or subsequent breaths. Therefore, the diagnosis of "fetal asphyxia" simply does not exist, and if it is present in the conclusions of the pathoanatomical examination (autopsy), this indicates the unprofessionalism of the doctor.
21st week of pregnancy - pregnancy calendar on the site Mamovediya | Mamovedia
The 21st week begins the 6th month of pregnancy. You have passed the equator and are now on your way to that desired day that serves as a guide for you - the probable date of delivery. nine0003
However, remember that this is only a guide, and labor can begin normally between 37 and 42 weeks
The time period is quite long and depends on various factors: the first or subsequent pregnancies, the way of life of the pregnant woman, physical activity, the regularity of the menstrual cycle and etc. If the pregnancy proceeds without complications, then the baby begins childbirth - just when he is ready to appear in this world. So, mothers, prepare everything you need for childbirth in advance ! Then, with peace of mind, you can expect a signal from the baby and enjoy the last weeks of your pregnancy. Remember that there is no template of normality, each woman and her baby is individual and will have their own happy story of birth...
If the pregnancy proceeds without complications, then the baby begins childbirth - just when he is ready to appear in this world. So, mothers, prepare everything you need for childbirth in advance ! Then, with peace of mind, you can expect a signal from the baby and enjoy the last weeks of your pregnancy. Remember that there is no template of normality, each woman and her baby is individual and will have their own happy story of birth...
What is going on?
Starting from the 21st week of pregnancy, the baby rapidly begins to gain weight - 10 g per day . At 19 weeks old, he weighs 370 - 390 g , has a height from head to tailbone 18 cm , full height is 27 cm . Your baby is about the size of a long head of corn.
The development and growth of the baby, its organs and systems continues
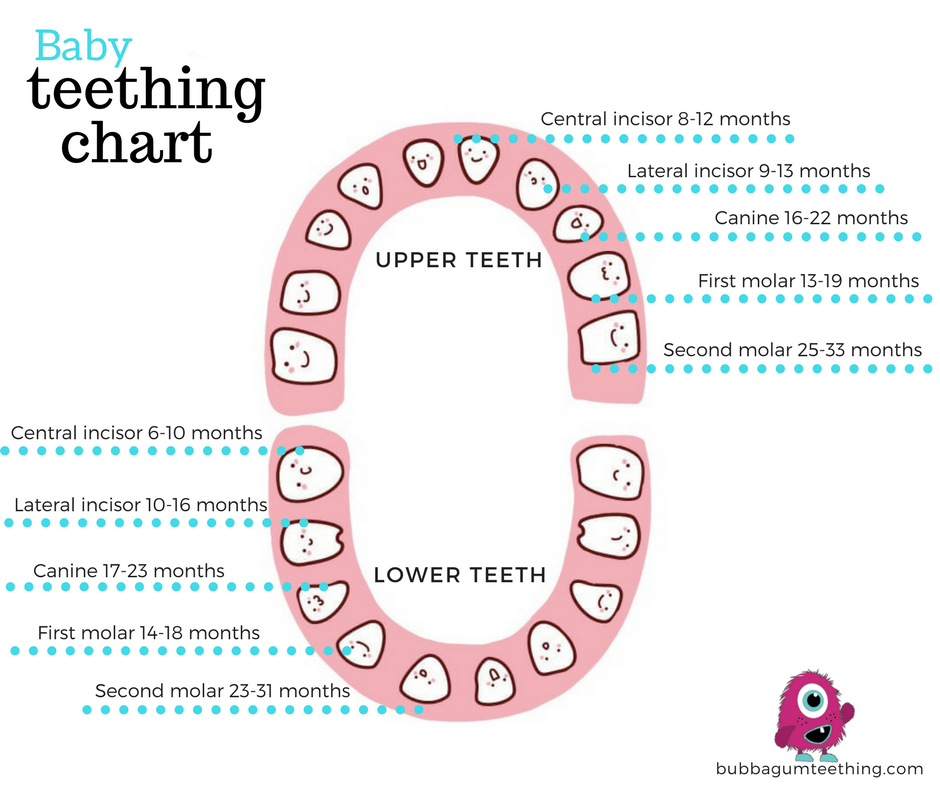
The baby's blood is rich in red blood cells, white blood cells also begin to form. The digestive system is already working hard - the baby swallows amniotic fluid, from which water is drawn out in the small intestine, and the rest goes into the large intestine. However, the enzymes and hydrochloric acid inherent in the digestive system of an adult are still present in a fairly small amount in a baby. Ultrasound can be used to observe the process of swallowing amniotic fluid at different stages of pregnancy. Development of the bone marrow  They will be responsible for fighting infections. Taste papillae are already forming on the tongue of . With the help of ultrasound, it is already possible to distinguish between the rudiments of milk and permanent teeth. There is still lanugo above the lip, above the eyes and eyebrows. The eyes are still closed for centuries. nine0003
They will be responsible for fighting infections. Taste papillae are already forming on the tongue of . With the help of ultrasound, it is already possible to distinguish between the rudiments of milk and permanent teeth. There is still lanugo above the lip, above the eyes and eyebrows. The eyes are still closed for centuries. nine0003 The placenta remains the main source of nutrition for the baby, but the skill of swallowing amniotic fluid is such a preparatory stage for life outside the mother's tummy

The baby still has enough space for free rotation around its own axis. He can change his location several times a day : across the abdomen, up or down the head. Growing up, the baby chooses the position in which he will expect his appearance. As a rule, this is upside down, but other options for the location of the child in the womb are possible. Sometimes the baby turns around and takes the right position almost before the very birth. nine0003
What does it feel like?
The feeling of absolute happiness fills your heart, the joy of future motherhood illuminates your face with a radiant smile.
The uterus grows in response to your baby's growth. Now its tip is already 1.25 cm above the navel. Due to the increase in the size of the uterus, other organs and systems of your body are "crowded" and can cause you certain inconveniences , such as slight shortness of breath or heartburn. nine0003
nine0003
A period of visual changes to your body begins - the next 10 weeks the rate of weight gain begins to increase . This is due to the fact that the baby begins to accumulate fat, which means your body will require additional calories. Accordingly, you will experience an increasing appetite and a constant need to snack.
Your baby's movements become clearer , and sometimes you can not only feel them, but you can also watch them, following the vibrations on your tummy. nine0003
Your pretty, already well-rounded tummy changes your figure and posture , the appropriate size.
Nutrition for the expectant mother!
Because of your increased appetite, you need to be more careful about your daily diet so that you don't put on extra pounds and still get all the vitamins, minerals and nutrients you need. try avoid fatty foods and foods that are poor in nutrients .
The best food during this period will be dairy products, lean meat, fish, wholemeal products, various cereals, vegetables or vegetable salads seasoned with vegetable oil, and of course seasonal fruits.
Some women may be surprised by new food preferences - something completely unusual, rare or in general - chalk or earth.
Remember that it is better to eat more often and in small portions, avoid late dinner. Women who have problems with swelling of the legs and arms, at the 21st week of pregnancy, should reconsider the amount of daily fluid intake. nine0003
Risk factors for mother and child!
Pregnancy is a great joy, but it is worth remembering that this is a colossal burden on your body. As a result, there may be some complications. They do not need to be afraid, just need to be "aware" of everything that can cause certain inconveniences, as well as know how to prevent, avoid, get rid of or alleviate their condition.
One of the possible complications at 21 weeks is thrombosis . Thrombosis manifests itself in the form of swelling in the legs and redness in places where the veins are clogged. Usually all this is accompanied by pain. Women who had such a problem before pregnancy should be especially attentive to themselves. In this case, you should definitely notify your doctor so that he can monitor your condition and prescribe the necessary treatment or prevention in a timely manner.
Women who had such a problem before pregnancy should be especially attentive to themselves. In this case, you should definitely notify your doctor so that he can monitor your condition and prescribe the necessary treatment or prevention in a timely manner.
Varicose veins, edema and cramps are common complications during pregnancy. The best prevention in this case is a balanced diet, constant control of weight gain and an active mobile lifestyle. nine0003
At this stage of pregnancy Braxton-Hicks contractions may occur . These are short-term cramping pains in the abdomen. This phenomenon is in the nature of preparing the body for the upcoming birth and does not pose a threat. Such fights are also called training or false. However, if you are confused by their duration, severe pain or their intensity, do not put off a visit to the doctor. To reduce discomfort from false contractions, take a horizontal position - rest, you can drink a cup of your favorite tea or warm milk, a warm shower can also help. nine0003
nine0003
Important!
You are still agile and nimble - although the tummy is already quite rounded. It's time to open the list of necessary purchases compiled in advance and start or continue their implementation. In addition, you apparently have a list of cases that must be resolved before childbirth - confidently take on their implementation: you can do something yourself, and delegate something to your husband, future grandparents, aunts or uncles))) - Distribute small tasks to everyone on time and monitor their timely completion. nine0003
Don't forget about the renovation and furnishing of the children's room ! In no case should you breathe paint or rearrange furniture. Your main function is to convey your wishes to the performers and, of course, exercise control)))
Have plenty of rest and exercise, for example, walking in the evening park with your favorite drink in accordance with the season - fragrant tea in cool weather or a milkshake on a hot summer evening.