Pelvic pain radiating down leg pregnancy
Pelvic pain during pregnancy | BabyCenter
About one in four pregnant women have pelvic pain – sharp pain felt most often in the hips or groin. It may start late in the first trimester and can continue for a few months after giving birth, or longer. Treatments such as physical therapy and modifying how you move can help.
What causes pelvic pain in pregnancy?
Experts believe that pelvic pain, also known as pelvic girdle pain, is caused by a variety of factors related to normal pregnancy changes.
Starting as early as 10 weeks, the developing placenta produces increased levels of a hormone called relaxin. This hormone does just what its name implies: It relaxes your ligaments, including the ones that hold the bones of the pelvis together. This makes it easier for your baby's head to pass through during delivery.
Higher levels of estrogen and progesterone during pregnancy may also contribute to this loosening effect.
Relaxed ligaments can hurt if they stretch too far, or when they allow the bones they hold in place to move too easily. These bones can shift and put pressure on nearby muscles, causing pain.
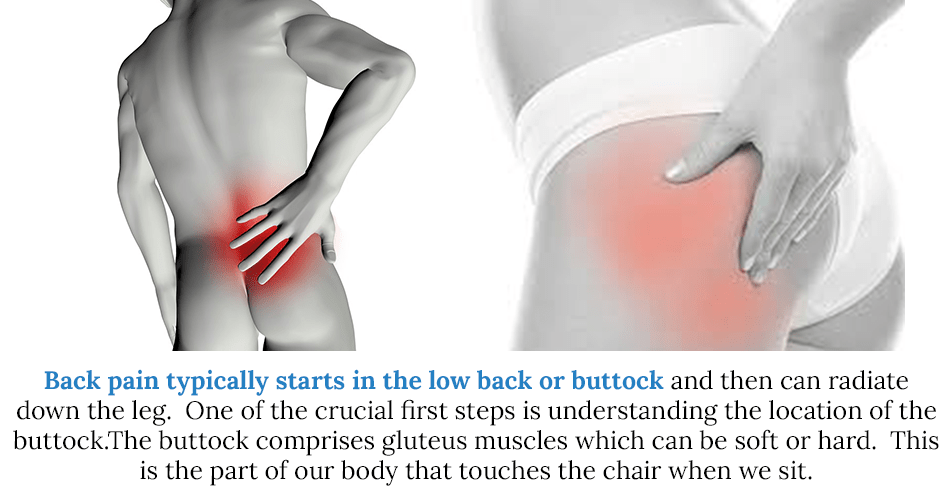
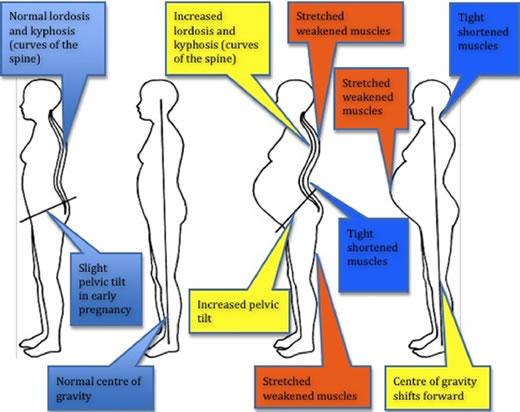
Weight gain and your changing center of gravity can also contribute to pelvic pain. As your belly grows, your pelvis is pushed forward, and the curve of your lower back becomes more pronounced. This can place a lot of strain on the muscles and ligaments in and around the pelvis. In fact, lower back pain and pelvic pain are often related.
What are the symptoms of pelvic pain in pregnancy?
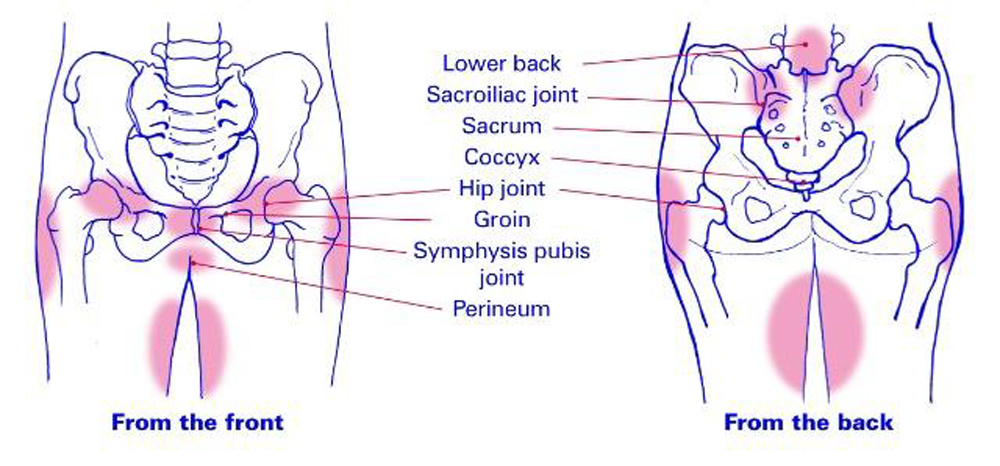
Loosened ligaments in the pelvis can cause soreness, stabbing, stinging, or burning sensations that can occur anywhere from the top of your hip bones down to the fold of your buttocks, either in the front or back.
Some women feel it when lifting, bending, or walking. Going up and down stairs, getting up from a sitting position, and turning over in bed may be especially painful. Some women find the pain is worse at night, especially after a very active day. Some find that their pelvis feels unstable.
What are the different types of pelvic pain in pregnancy?
Symphysis Pubis Dysfunction (SPD) The pubic symphysis is the joint where the two sides of the pelvis meet in the front, right underneath where your pubic hair grows. It's supported by a network of ligaments, and when these ligaments relax, the joint moves too much and causes pain ranging from mild to excruciating.
It's supported by a network of ligaments, and when these ligaments relax, the joint moves too much and causes pain ranging from mild to excruciating.
Diastasis Symphysis Pubis (DSP) This condition occurs when the gap in the pubic symphysis widens too far. The joint normally widens about 2 to 3 millimeters during pregnancy to help your baby pass through your pelvis. In some women, the pubic symphysis widens so much that it becomes unstable.
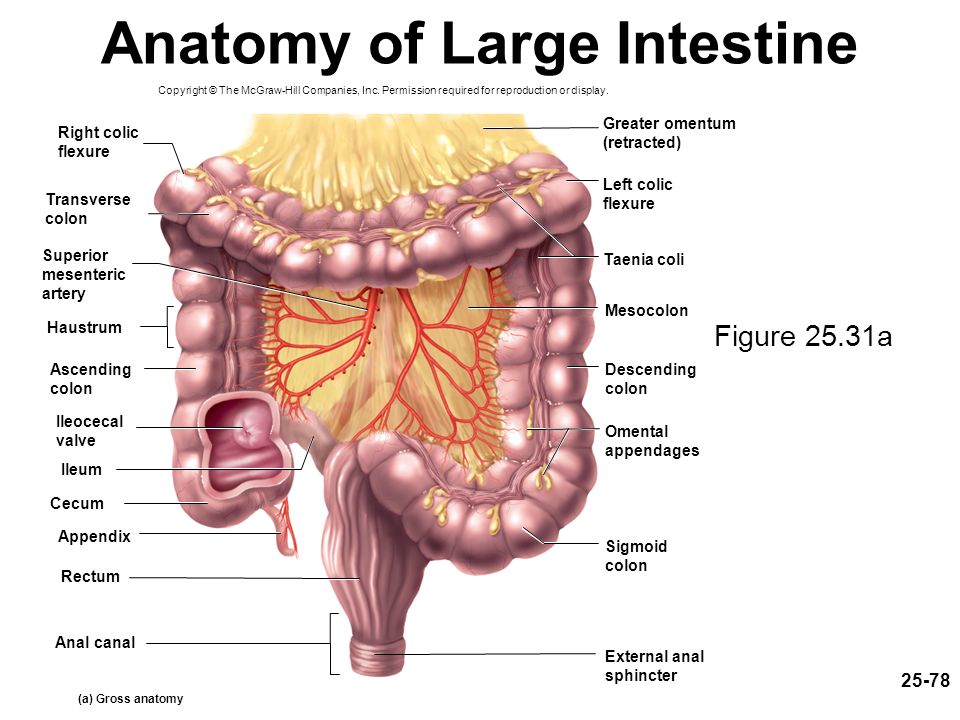
Sacroiliac joint pain. The sacroiliac joints contain ligaments that connect the sacrum – the structure composed of the last five vertebrae of your spine – to the "wings" of the pelvis on either side. If these ligaments relax too much, it can cause the bones in this area to move, putting pressure on nearby nerves and muscles. With sacroiliac joint pain, one side of your pelvis may hurt more than the other. The pain may radiate down your legs, into the back or front of your thighs. Or you may have a combination of very low back pain and feeling like the bones of your pelvis are unstable.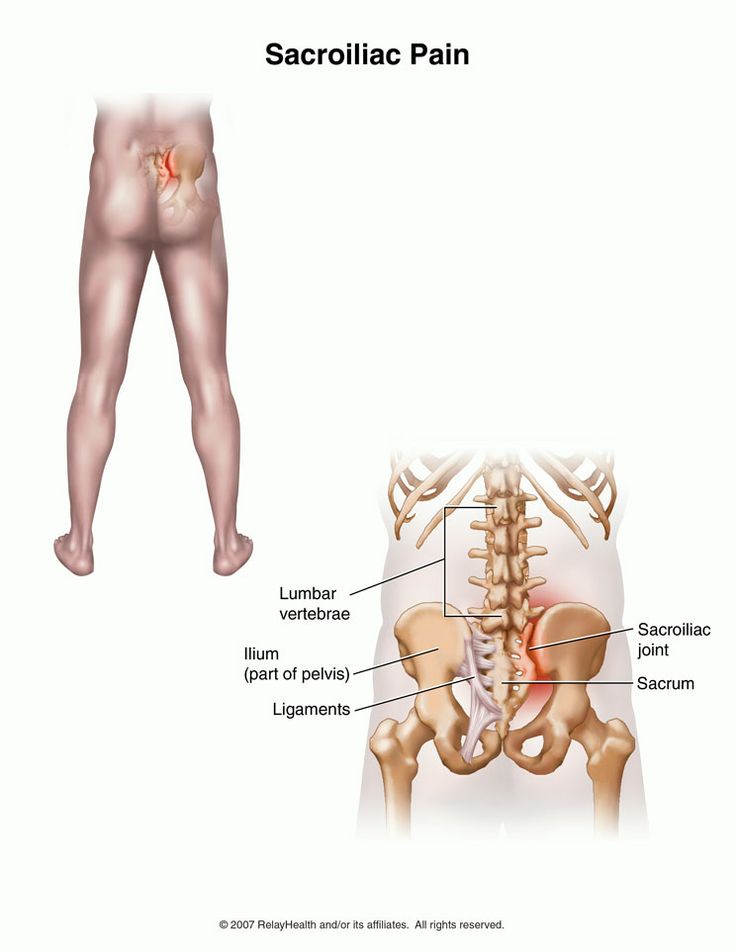
Round ligament pain. There are two round ligaments that attach your uterus to your pelvis. As your uterus grows up out of the pelvis, the ligaments pull, stretch, and thicken to accommodate and support it. These changes can cause pain which typically lasts just a few seconds as you change position. This pain is concentrated in your groin where your abdomen meets your legs, although occasionally it can shoot down the inside of your thigh.
Who's at risk for pelvic pain in pregnancy?
You may be more likely to develop pelvic pain if you:
• Had pelvic pain in a prior pregnancy.
• Have had multiple pregnancies.
• Have a history of pelvic trauma, like a back injury or pelvic fracture.
• Perform strenuous activities such as lifting, twisting, and bending.
Being overweight or carrying a very large baby (a condition called macrosomia) may also raise your risk for pelvic pain, but evidence is conflicting.
How is pelvic pain diagnosed in pregnancy?
If you're experiencing pain anywhere during pregnancy, it's important to tell your doctor or midwife. They'll want to make sure your pain isn't due to any other health problems, and they'll offer options for relief.
They'll want to make sure your pain isn't due to any other health problems, and they'll offer options for relief.
Your healthcare provider will examine you and may have you do certain movement tests to help pinpoint where the pain is coming from. In some cases, you may need to have an ultrasound or magnetic resonance imaging (MRI), which provides pictures of the soft tissue and bones.
How is pelvic pain in pregnancy treated?
There are many treatments available. While you may not get complete relief from pelvic pain during your pregnancy, you can take steps to prevent it from getting worse. Many women use more than one of these techniques to maximize their relief.
Pregnancy girdles, bands, and belts. These work by applying gentle pressure to the pelvis to give you more stability. They can be effective when combined with gentle exercise.
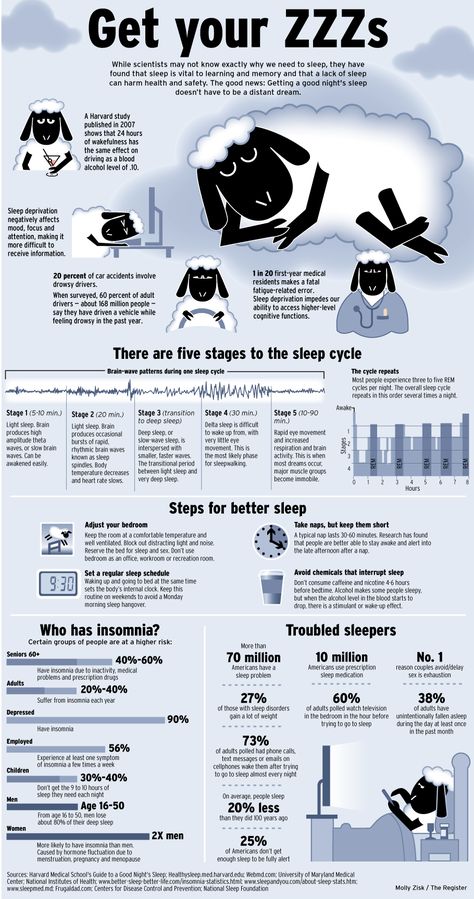
Sleep positioning. Pregnancy pillows that support your belly and hips can ease the strain on your pelvic ligaments and allow you to get a good night's sleep. You may need to experiment to find one that's right for you. Women's hips are wider than their knees, especially in pregnancy. Sleep with a pillow between your knees to keep your hips in a neutral position and avoid extra stress on your hips and lower back. Read more about how to be comfortable in bed during pregnancy.
You may need to experiment to find one that's right for you. Women's hips are wider than their knees, especially in pregnancy. Sleep with a pillow between your knees to keep your hips in a neutral position and avoid extra stress on your hips and lower back. Read more about how to be comfortable in bed during pregnancy.
Physical therapy. Studies show that certain exercises – especially in water – can be helpful in reducing pelvic pain. Ask your doctor or midwife for a referral to a physical therapist who specializes in pregnancy. (Your insurance may pay for part or all of the cost.) You'll learn stretches to relieve your pain and exercises to strengthen your core, pelvic floor, and back to provide your pelvis with more stability. A physical therapist can also teach you how to avoid pain when getting out of bed and doing daily tasks.
Acupuncture. Some women find that acupuncture helps with pelvic pain. When performed by a licensed practitioner, acupuncture is considered safe for expecting moms.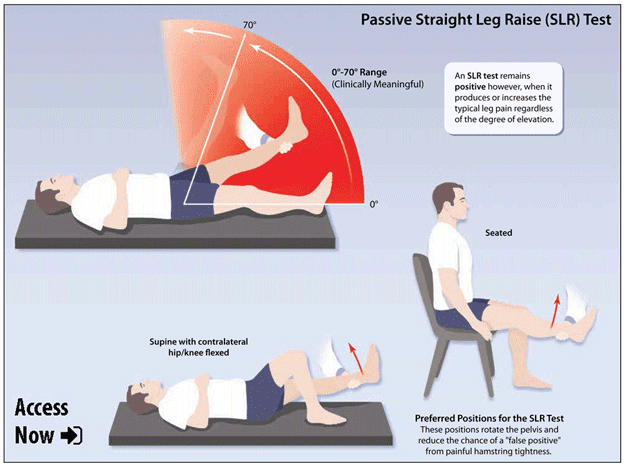
Pain relievers. Acetaminophen (such as Tylenol) is an over-the-counter medication that has a long history of safety during pregnancy. Avoid ibuprofen (Advil, Motrin) and other nonsteroidal anti-inflammatory drugs, like Aleve and aspirin.
What else can I do to ease my pelvic pain during pregnancy?
In addition to the treatments that your doctor or midwife recommends, there are ways you can reduce pain as you go through your day:
Avoid painful activities. Limit activities that cause discomfort, such as heavy lifting and carrying, standing or walking for long periods, and strenuous exercise. Find new ways to do the things that cause you pain. For instance, instead of getting out of bed by sitting straight up, try rolling to your side first and pushing up from that position.
Take frequent breaks. Try to rest a few minutes in a comfortable position as often, and as regularly, as possible.
Exercise gently. Try mild to moderate exercise, such as gentle abdominal strengthening exercises, Kegels, prenatal yoga, and walking. Don't overdo it, and avoid exercises that require squatting or spreading your legs, which can aggravate hip pain.
Try mild to moderate exercise, such as gentle abdominal strengthening exercises, Kegels, prenatal yoga, and walking. Don't overdo it, and avoid exercises that require squatting or spreading your legs, which can aggravate hip pain.
Practice good posture. Keep your back straight and aligned. Try not to slump, especially when seated.
Apply ice or heat. Try using an ice pack or rubbing an ice cube on the areas where it hurts. (For low back pain, get one of those flat ice packs that go in lunch bags and tuck it into your waist band.) Ice helps tame inflammation. If you're also experiencing low back pain, a heating pad can be soothing – but use it only on your back (for about 20 minutes at a time), not in the front where your uterus and baby are.
Will pelvic pain affect my labor and delivery?
Here are a few things you may need to consider:
• As you approach your due date, make sure your healthcare provider has reevaluated your condition and tested your pain level and range of motion, especially if you plan to get an epidural.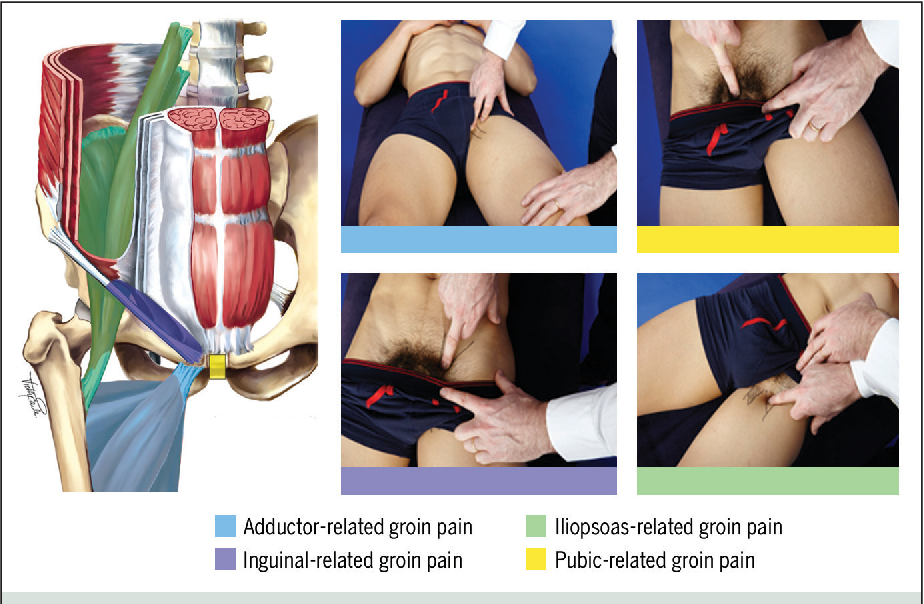 This information helps determine if any special accommodations need to be made for you during labor and delivery.
This information helps determine if any special accommodations need to be made for you during labor and delivery.
• Depending on your mobility, here are some alternative positions for giving birth: kneeling while someone supports you from behind, lying on your side with someone holding your leg, or delivering your baby on all fours.
• If you choose epidural or spinal anesthesia, you could overstretch your already sensitive ligaments while you're numb. Discuss this possibility with your practitioner so you can plan to avoid this problem.
Will I still have pelvic pain after my baby is born?
Most women feel complete relief within about 3 months of giving birth. A small number have residual pain, which may need further treatment, such as pain-relievers or immobilization devices like belts or girdles. Many women benefit from physical therapy to strengthen the muscles of the abdomen and lower back and rebuild strength and coordination in the pelvic floor.
In very rare cases in which the pubic symphysis has separated, surgery may be needed to stabilize the pelvis.
Learn more about pelvic organ prolapse.
advertisement | page continues below
Pelvic girdle pain in pregnancy
Pelvic girdle pain in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- Pelvic girdle pain refers to pain or discomfort in your lower back, pelvis, hips, or thighs during pregnancy.
- This pain can be mild or severe, and you may find you have difficulty sitting, standing and walking.
- • Pelvic pain is common in pregnancy, but you are more likely to have it if you had back or pelvic pain before you were pregnant, had an injury to the area, your work is physically demanding, you are overweight or you smoke.
- Your GP, obstetrician and physiotherapist can help you to manage your pelvic pain in pregnancy.

- Depending on your circumstances, your health team may recommend that you modify your daily activities, wear a pelvic support garment, or they may refer you to physiotherapy and exercise programs.
What is pelvic girdle pain?
Pelvic girdle pain (PGP) refers to pain or discomfort in the lower back or pelvis during pregnancy. The pain may also extend to your upper thighs and perineum. During pregnancy your pelvic ligaments relax, and other joints become more mobile. This can result in pain in the pelvic area. Pelvic girdle pain usually goes away without treatment after birth, though symptoms may return in future pregnancies.
What are the symptoms of pelvic girdle pain in pregnancy?
If you have PGP, you may only have mild discomfort in your pelvis or back. Alternatively, you may have severe pain making it difficult for you to sit, stand, walk and move around. Each person has a different levels of pain or discomfort.
Who gets pelvic pain in pregnancy?
Some people are more likely to have PGP than others.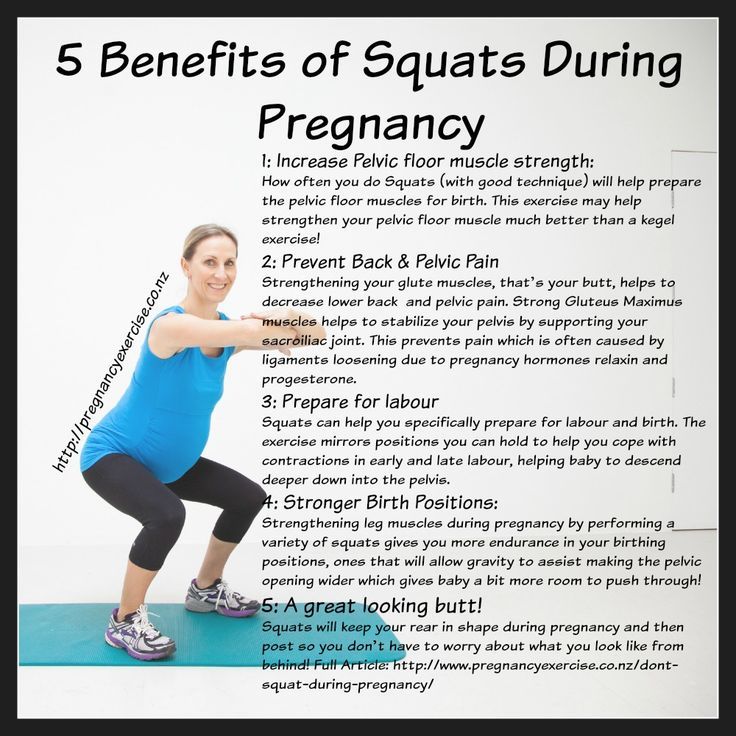 If you had back or pelvic pain before your pregnancy or had PGP in a previous pregnancy, you are more likely to have PGP in your current pregnancy. If you have had a back or pelvic injury, you are also more likely to develop PGP. Other risk factors for PGP include the number of times you’ve been pregnant, physically demanding work, being overweight, emotional distress, or smoking.
If you had back or pelvic pain before your pregnancy or had PGP in a previous pregnancy, you are more likely to have PGP in your current pregnancy. If you have had a back or pelvic injury, you are also more likely to develop PGP. Other risk factors for PGP include the number of times you’ve been pregnant, physically demanding work, being overweight, emotional distress, or smoking.
Who can help with pelvic pain?
If you are experiencing back, pelvic, or hip pain during pregnancy, you should see your doctor. Your doctor will ask you about your medical history and do a physical examination. It is important to see a doctor so you can be sure that your pain is because of PGP.
Your doctor may suggest that you see a physiotherapist. A physiotherapist can teach you exercises to help you to manage your pain.
If your pain is severe and you are not improving with standard care, you may be referred to a specialist pain service.
How is pelvic girdle pain treated?
There are several strategies that you can use to help you manage and control pelvic girdle pain. First, you can try and identify what daily activities cause you pain and try to adjust or avoid those activities. For example, you can avoid wearing high heeled shoes and standing on one leg. You can also reduce weight-bearing activities like climbing stairs or walking and standing for long periods of time. You can also try to avoid activities that involve straining your hip, like getting in and out of a car or bath, or squatting.
First, you can try and identify what daily activities cause you pain and try to adjust or avoid those activities. For example, you can avoid wearing high heeled shoes and standing on one leg. You can also reduce weight-bearing activities like climbing stairs or walking and standing for long periods of time. You can also try to avoid activities that involve straining your hip, like getting in and out of a car or bath, or squatting.
Wearing a pelvic support garment can also help to reduce pain. Pelvic support garments can help to stabilise your pelvic girdle and improve symptoms if the garment is fitted correctly and used for short periods of time. Ask your physiotherapist for more information about pelvic support garments.
You can also ask your doctor or pharmacist about medicines that can help you to manage your pain so you can continue with your daily activities. This may include taking medicines like paracetamol.
Physiotherapy and exercise programs can help to reduce pain too.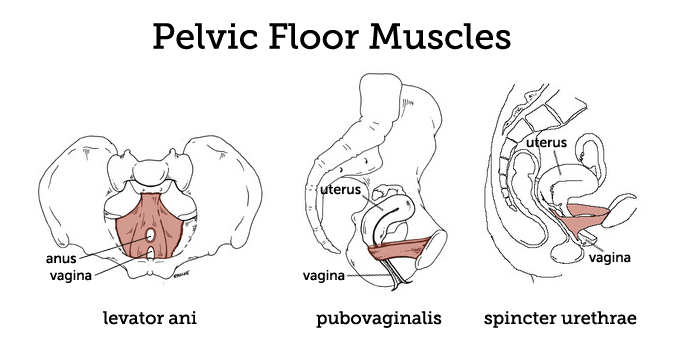 They may also help to correct the problem causing the pain.
They may also help to correct the problem causing the pain.
How can I relieve pelvic girdle pain at home?
Many of these pain-relieving techniques can be done at home. Ask your physiotherapist to suggest a home exercise program to help you when you first start to feel a pelvic-pain episode. If your pain stops you from doing essential daily activities, you can take a pain-relief medicine like paracetamol. Taking pain relief may mean that you’re better able to do the exercises that your physiotherapist has recommended. If you have a pelvic support garment, you can put that on.
Applying heat to painful areas and sitting or lying down may help you control your pain. Extended bedrest without the guidance of a doctor is not recommended, so speak to your doctor if you feel you need to lie down for extended periods of time while you’re pregnant.
Will pelvic girdle pain affect labour and birth?
In most cases, people with PGP can have a normal vaginal labour and birth. Your doctor may recommend that during labour you position yourself in a way that puts less stress and strain on your pelvis and hips. For example, you might find it less painful to go through labour on your side or in the 'all fours' position. Usually inducing labour early or having a caesarean section are not recommended. These options may occasionally be suggested in severe cases.
Your doctor may recommend that during labour you position yourself in a way that puts less stress and strain on your pelvis and hips. For example, you might find it less painful to go through labour on your side or in the 'all fours' position. Usually inducing labour early or having a caesarean section are not recommended. These options may occasionally be suggested in severe cases.
Will I have pelvic girdle pain in future pregnancies?
Not every person with PGP during pregnancy will have pelvic pain again in future pregnancies. However, recurrence is very common. Nearly 7 out of 10 people with PGP during pregnancy have it again in future pregnancies. Unfortunately, your pain may also be worse during future pregnancies.
If you’ve had PGP in a previous pregnancy, speak with your health team to develop a strategy to manage your pelvic pain early. Managing your pelvic girdle pain early can help to avoid pain from worsening as your pregnancy progresses.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Department of Health (Pelvic girdle pain), AJGP (Pelvic girdle pain in pregnancy), National Center for Biotechnology Information (Pregnancy-related pelvic girdle pain: an update), Royal Women's Hospital Victoria (Pregnancy related girdle pain fact sheet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2022
Back To Top
Related pages
- Pelvic floor exercises
- Exercising during pregnancy
- Yoga and Pilates during pregnancy
- Backache in pregnancy
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.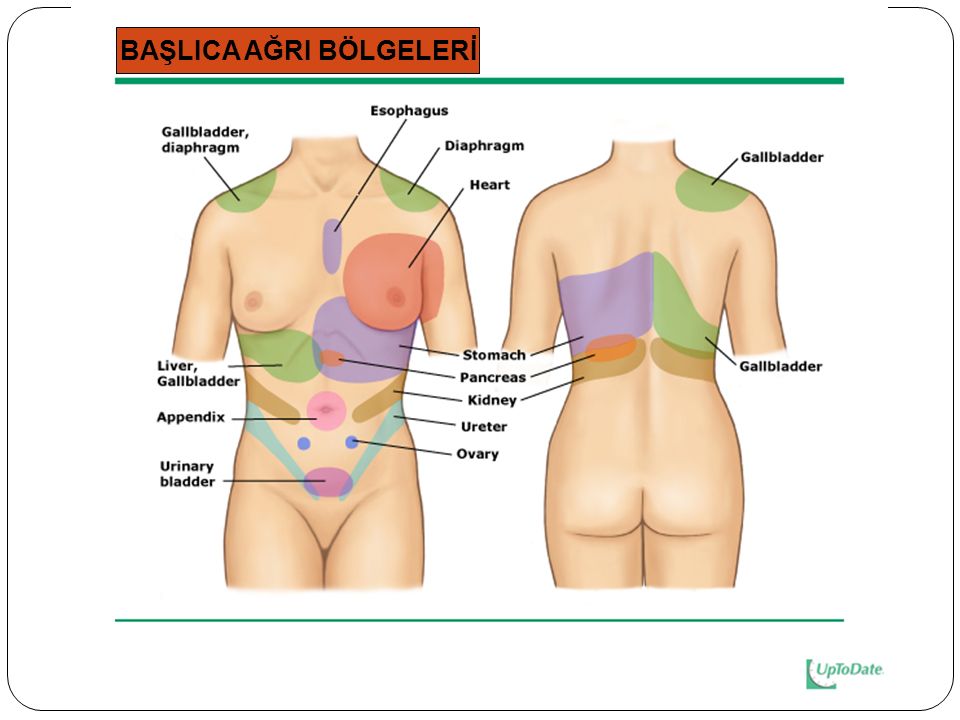
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.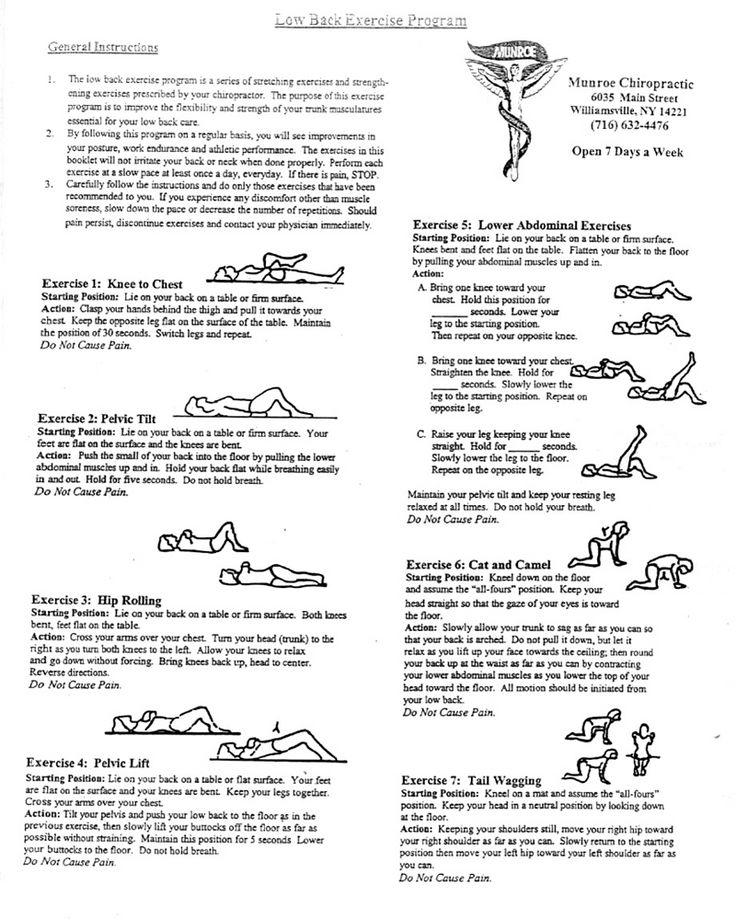 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Lower back pain and pregnancy
As a result, there are changes in the spine, in the muscles of the abdomen and back and the shape of the lumbar curve of the spine (hyperlordosis), and all this becomes relaxed. Poor posture and poor muscle tone can also affect spinal mechanics.
The lumbar curve of the spine begins to slowly increase as the pelvis begins to move back. This posture begins to affect the weakened muscles and leads to the accumulation of fatigue in the muscles of the lower back. A woman may experience moderately painful muscle spasms at first, which may be the first sign of the possibility of persistent low back pain as the pregnancy progresses. The growing uterus shifts the center of gravity and weakens the abdominal muscles, changes posture and puts excessive stress on the back. If the uterus affects the nerves, then this can lead to pain. In addition, being overweight during pregnancy puts more stress on the muscles and joints, and therefore, by the end of the day, a pregnant woman may feel discomfort. nine0003
The growing uterus shifts the center of gravity and weakens the abdominal muscles, changes posture and puts excessive stress on the back. If the uterus affects the nerves, then this can lead to pain. In addition, being overweight during pregnancy puts more stress on the muscles and joints, and therefore, by the end of the day, a pregnant woman may feel discomfort. nine0003
Experts describe the two most common patterns of low back pain during pregnancy: low back pain that occurs in the area of the lumbar vertebrae in the lower back, and posterior pelvic pain, which is felt in the back of the pelvis. Some women have symptoms of both types of low back pain.
Lower back pain is similar to the pain that a woman experienced before pregnancy. Pain is felt in the lower back and around the spine, approximately at waist level. Women may also experience pain that radiates to the legs. Prolonged sitting or standing can aggravate the pain and, as a rule, the pain tends to increase towards the end of the day. Many more women experience back pelvic pain, which is felt less than lower back pain. The pain may be deep inside the buttocks, on one or both buttocks, or in the back of the thighs. Pain can be triggered by activities such as walking, climbing stairs, getting in and out of the bathroom on a low cabinet, turning in bed, or twisting and lifting heavy objects. nine0003
Many more women experience back pelvic pain, which is felt less than lower back pain. The pain may be deep inside the buttocks, on one or both buttocks, or in the back of the thighs. Pain can be triggered by activities such as walking, climbing stairs, getting in and out of the bathroom on a low cabinet, turning in bed, or twisting and lifting heavy objects. nine0003
Positions that involve leaning forward, such as sitting, in a chair, and working at a desk while leaning forward, can exacerbate posterior pelvic pain. Women with posterior pelvic pain are also more likely to experience pain over the pubic bone.
When low back pain radiates to the buttocks and thighs, sciatica is often suspected - although sciatica is not very common in pregnant women. True sciatica, which can be caused by a herniated disc or the presence of a disc protrusion in the lumbar spine, occurs in only 1 percent of pregnant women. nine0003
If there is compression and inflammation of the sciatic nerve (disc herniation), then the pain in the legs is more severe than with normal low back pain. Pain can be felt not only in the thigh, but also below the knee or even radiate to the foot. It is also possible the presence of sensory disturbances, such as numbness or tingling sensations.
Pain can be felt not only in the thigh, but also below the knee or even radiate to the foot. It is also possible the presence of sensory disturbances, such as numbness or tingling sensations.
In severe sciatica, there may be numbness in the groin area, as well as in the genital area. You may also have trouble urinating or defecation. If a pregnant woman has suspicions of sciatica, then she must definitely contact her doctor. If symptoms such as impaired sensation in the legs and weakness in one or both legs or loss of sensation in the groin and impaired urination or defecation appear, then you need to see a doctor urgently! Such symptoms may be evidence of the development of the "cauda equina" syndrome in the presence of a herniated disc in a pregnant woman, and in such cases an emergency operation is necessary. nine0003
Risk factors for low back pain
It is not surprising that, most likely, low back pain in pregnant women is most likely if there were already pains before pregnancy or there were degenerative changes in the lumbar spine (protrusions, herniated discs).
 Also at higher risk are pregnant women who led an inactive lifestyle before pregnancy, as a result of which their back muscles are weak, as well as the abdominal muscles. Pregnancy with multiple fetuses (twins) significantly increases the risk of lower back pain. Obesity may also be a risk factor for developing low back pain during pregnancy. nine0019
Also at higher risk are pregnant women who led an inactive lifestyle before pregnancy, as a result of which their back muscles are weak, as well as the abdominal muscles. Pregnancy with multiple fetuses (twins) significantly increases the risk of lower back pain. Obesity may also be a risk factor for developing low back pain during pregnancy. nine0019 Diagnosis of low back pain.
Examinations such as CT (MSCT) are rarely used to diagnose the causes of low back pain in pregnant women due to possible teratogenic effects on the fetus. MRI is also not recommended, especially in the first trimester of pregnancy. But, if there are clinical indications, then MRI can be performed. Therefore, as a rule, the diagnosis of low back pain in pregnant women is mainly based on physical examination data, symptoms and medical history (for example, the presence of a disc herniation before pregnancy). nine0003
Treatment
The use of any medication during pregnancy is a big risk, as all medication will also be delivered to the fetus. Therefore, the usual prescription of painkillers, muscle relaxants, or steroids (NSAIDs) for back pain is contraindicated in pregnant women. In addition, the use of acupuncture physiotherapy is also not recommended. It is possible to use light massage and very gentle manual therapy techniques.
Therefore, the usual prescription of painkillers, muscle relaxants, or steroids (NSAIDs) for back pain is contraindicated in pregnant women. In addition, the use of acupuncture physiotherapy is also not recommended. It is possible to use light massage and very gentle manual therapy techniques.
At the forefront of the treatment of back pain in pregnant women comes exercise therapy (gymnastics) and certain recommendations for the implementation of daily activities. Gymnastics can be specialized, such as prenatal yoga. Good effect gives swimming and walking. nine0003
Swimming is an excellent choice of exercise for pregnant women because it strengthens the abdominal and lower back muscles, and being in the water relieves stress on joints and ligaments.
Need to maintain proper biomechanics during pregnancy:
- Stand up straight. This becomes more and more difficult to do as the shape of the body changes, but one must try to keep the back straight and the shoulders back.
 Pregnant women tend to drop their shoulders and arch their back as their belly grows, which puts more stress on the spine. nine0039
Pregnant women tend to drop their shoulders and arch their back as their belly grows, which puts more stress on the spine. nine0039 - If it is necessary to sit during the day, then one should sit straight. Leg support (bedside table) can help prevent lower back pain, and you can also put a special pillow under the lower back. Take frequent breaks from sitting. You need to get up and walk for several minutes, at least once an hour.
- It is equally important not to stand too long. If you need to stand all day, then it is advisable to rest while lying on your side during a break, supporting your upper leg and stomach with pillows. nine0039
- Avoid movements that increase pain. If there is posterior pelvic pain, then one should try to limit activities such as climbing stairs. It is also advisable to avoid any activity that requires extreme movement of the hips or spine.
- It is important to wear comfortable shoes and avoid high heels. As the abdomen grows, the center of gravity shifts and when wearing shoes with heels, the risk of falls increases.
 nine0039
nine0039 - Always bend your knees and pick things up from your haunches to minimize stress on your back. Spinal twisting should be avoided and activities such as vacuuming or mopping should be avoided.
- Divide the weight of the items to be carried. For a uniform load, it is necessary to carry the weight in two bags.
With severe pain and weak muscle corset, you can wear a belt.
Particular attention should be paid to pregnant women with herniated discs, as in a certain percentage of cases it is possible to develop cauda equina syndrome during pregnancy, a very serious neurological condition. nine0003
Seek immediate medical attention if any of the following symptoms occur:
- Back pain pain is very severe, persistent, or gradually increases, or if the pain appears after an injury, or if it is accompanied by a rise in temperature.
- Numbness in one or both legs, or feeling that the legs do not obey
- Loss of sensation in the buttocks, groin, perineum, or impaired bladder and bowel function.
 nine0038 Low back pain at the end of the second or third trimester is very suspicious. This may be a sign of preterm labor, especially if the pregnant woman has not had back pain before.
nine0038 Low back pain at the end of the second or third trimester is very suspicious. This may be a sign of preterm labor, especially if the pregnant woman has not had back pain before. - If pregnant you experience pain in your lower back or side just below your ribs, on one or both sides. This may be a sign of a kidney infection, especially if there is fever, nausea, or blood in the urine.
Sciatica in pregnancy: symptoms, treatment and prevention
During pregnancy, various chronic diseases can worsen, as the woman's body experiences increased stress. One such disease is sciatica. It is worth understanding in more detail what it is and how the disease manifests itself.
Sciatica in pregnancy: a description of the disease
The sciatic nerve is one of the largest in the human body. Its branches go to many parts of the body, their full-fledged work depends on it, as well as the normal perception of touch, temperature, etc. Sciatica during pregnancy is nothing more than a pinched sciatic nerve. This condition requires immediate medical attention and manifests itself in many specific signs. nine0003
Sciatica during pregnancy is nothing more than a pinched sciatic nerve. This condition requires immediate medical attention and manifests itself in many specific signs. nine0003
Causes of pinching of the sciatic nerve in pregnant women
During pregnancy, the spinal column of the future mother experiences a significant increase in the load. The sacrum also suffers greatly, which becomes most noticeable by the last third of pregnancy. This is due to the fact that the greatly enlarged uterus begins to put pressure on nearby tissues and organs. It is here that the sciatic nerve is located, which, in the process of such pressure, begins to become inflamed.
The main causes of sciatica include: nine0003
- sudden weight gain;
- multiple pregnancy;
- large amount of amniotic fluid;
- lack of normal physical activity on the body of the expectant mother;
- hypothermia of the lower part of the body, mainly the pelvic region;
- strong physical activity, lifting heavy weights.
In addition, ailments and conditions that were diagnosed even before a woman decided to become a mother often contribute to the occurrence of sciatica during pregnancy. In this position, any disease can worsen in a woman. Sciatica can lead to: nine0003
- Injury to the spinal column.
- Osteochondrosis.
- Protrusions and hernias.
- Diabetes mellitus, as well as other ailments associated with metabolism.
- Infections in the pelvis.
If earlier a woman did not have any problems with the sciatic nerve, and there are no diseases provoking it, it is possible to encounter an ailment only shortly before childbirth. At the same time, age is unimportant - both young mothers and aged ones can note the symptoms of pinching. As a rule, in this case, after the birth of a child, the discomfort from pinching passes. nine0003
Symptoms of sciatica during pregnancy
It is not difficult to recognize the symptoms of sciatica during pregnancy, since they are quite characteristic. Expectant mothers with the appearance of such symptoms strongly complain about their well-being, the opportunity to fully relax and do everyday activities is lost. Pain tends to intensify at night, so women suffer from insomnia. Even getting up is sometimes very difficult, which is why you have to call for help from loved ones.
Expectant mothers with the appearance of such symptoms strongly complain about their well-being, the opportunity to fully relax and do everyday activities is lost. Pain tends to intensify at night, so women suffer from insomnia. Even getting up is sometimes very difficult, which is why you have to call for help from loved ones.
Intermittent or persistent pain in one buttock or leg
Pain appears below the lower back, on the one hand it can be stronger, and the intensity depends on the strength of the infringement and the presence of an inflammatory process.
Pain along the sciatic nerve radiating from the buttocks to the thigh and foot
Painful sensations can occur along the course of the nerve or even the entire nerve bundle. Often, expectant mothers note that even the foot hurts, which causes a lot of inconvenience and does not allow them to move normally. nine0003
Sharp, shooting or burning pain
The nature of the pain is usually throbbing or shooting.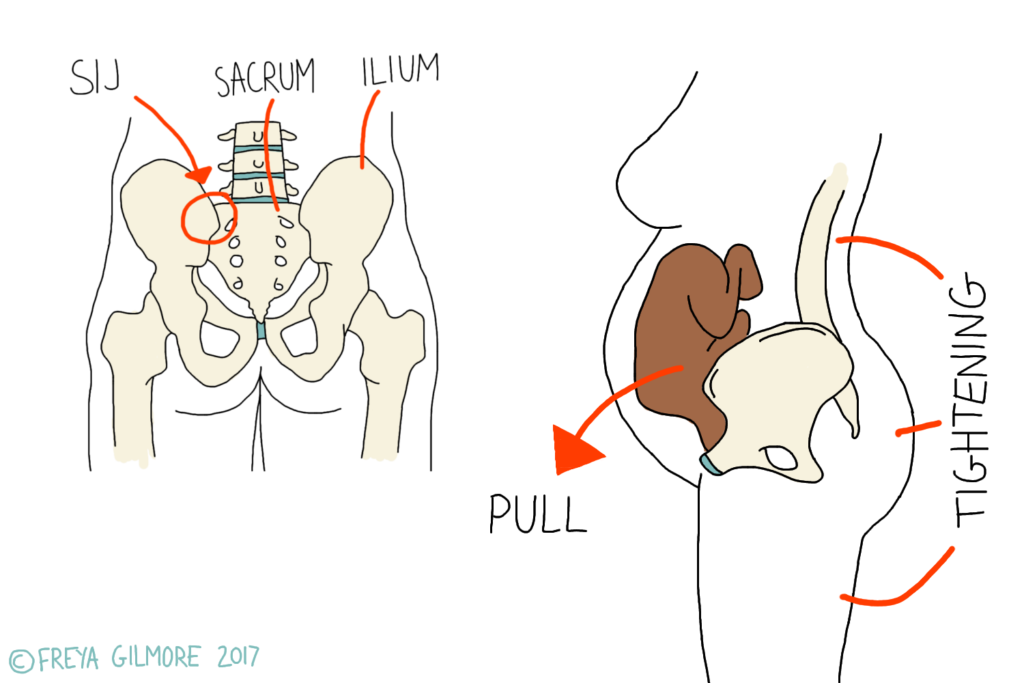 The pain syndrome is pronounced, since the nervous tissue is constantly affected.
The pain syndrome is pronounced, since the nervous tissue is constantly affected.
Numbness, colic, or weakness in the affected leg or foot
The area below the waist suffers from loss of sensitivity, paresthesias appear, as well as a pain syndrome resembling a cramp. Due to the constant impact on the nerve, the functioning of the affected limb may deteriorate, the pregnant woman notes a feeling of weakness in the leg. nine0134
Difficulty walking, standing or sitting
It becomes difficult for a woman to rise, change the position of the body. Incontinence may occur, but this usually occurs in advanced cases.
Treatment
It is important to learn about the symptoms and treatment of sciatica during pregnancy if you have to deal with such a condition. It should be understood that the position of a woman significantly complicates any therapy. However, infringement of the sciatic nerve is not the condition when treatment is postponed for the period after the delivery of the pregnant woman.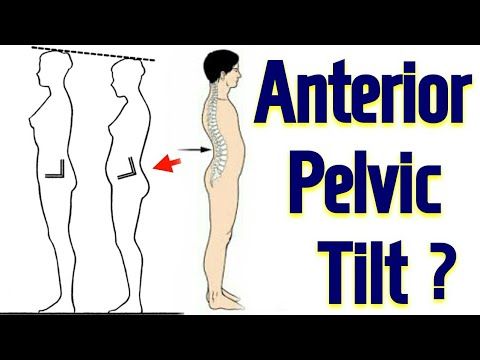 nine0003
nine0003
If, after visiting a gynecologist, a woman has not received clear recommendations for treatment, it will be necessary to visit a neurologist. In such a situation, the doctor prescribes to the pregnant woman:
- taking medicines;
- doing exercises;
- bandaging;
- massages and other therapeutic effects from an experienced manual;
- purchase of an orthopedic mattress.
Doctors also recommend abandoning shoes with heels, choosing more comfortable and practical options. This will reduce the load on the spine and the manifestations of pinching. In the same way, it is worth choosing comfortable clothes according to the weather, which do not restrict movement and do not allow you to overcool or overheat. However, remember that self-medication, especially in this position, is fraught with negative consequences for the body. Therefore, do not take any medication or exercise without consulting your doctor.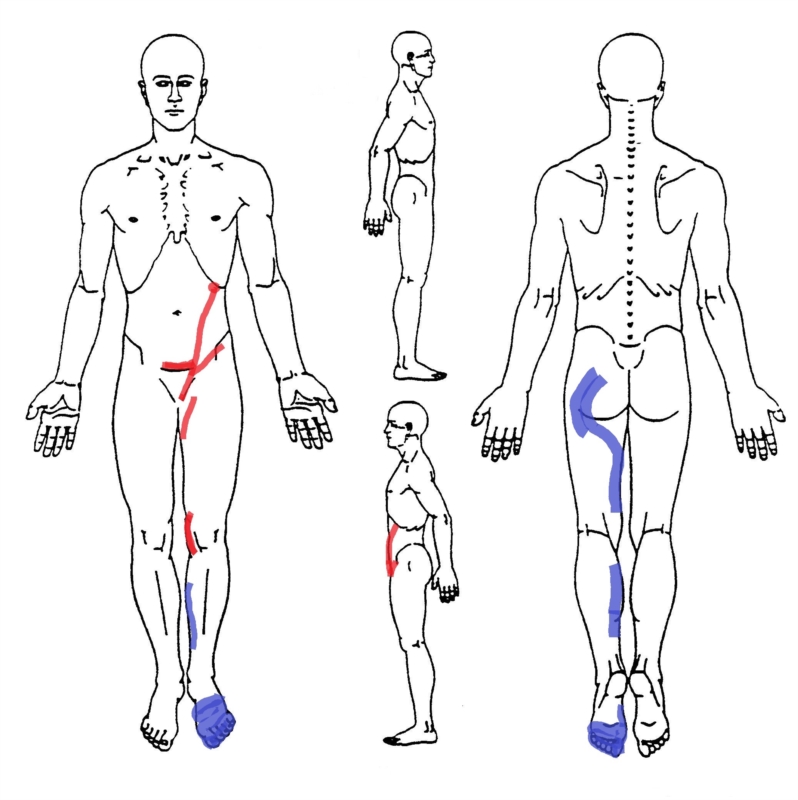 nine0003
nine0003
Physical exercise
If the doctor reveals that the sciatic nerve (pregnancy becomes much more difficult) is impaired and inflammation has occurred, some exercises are prescribed. For example, taking a knee-elbow position for 15 minutes or more can bring great relief to a woman, as a rule, after this time, the pregnant woman's well-being improves significantly.
Also useful will be:
- Yoga.
- Gymnastics for pregnant women.
- Swimming pool visit.
During the period of remission, the pregnant woman is recommended to move more in order to prevent an acute attack, but it is important not to overdo it.
Blockade with pain medications
A pinched sciatic nerve during pregnancy can cause unbearable pain. In this case, massages and exercises alone are not enough. Physicians resort to:
- blockades;
- candles with analgesic effect - often this is the drug "Diclofenac";
- external preparations - ointments and gels with which a pregnant woman should rub the affected area, it can be "Chondroxide", "Finalgon" and some others.
Doctors select drugs that are not capable of harming the baby by penetrating into the general bloodstream. As a result, the mother experiences significant relief, the affected area is better supplied with blood, and the tissues damaged by the pathological process are regenerated. nine0003
Massage
If you do not know how to treat sciatica during pregnancy, you should know that a course of massages is a great way to treat it. However, such a procedure must be authorized by a doctor, and you will also need to find an experienced massage therapist who knows how to handle the body of a pregnant woman. If the massage therapist does not have the proper experience, serious complications can occur, up to the threat of premature delivery. As a rule, 15 sessions with an experienced chiropractor are enough to improve well-being and eliminate unpleasant symptoms. nine0003
Traditional treatments
Also, folk recipes become a good answer to the question of what to do if sciatica occurs during pregnancy.