Rash on vulva during pregnancy
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women.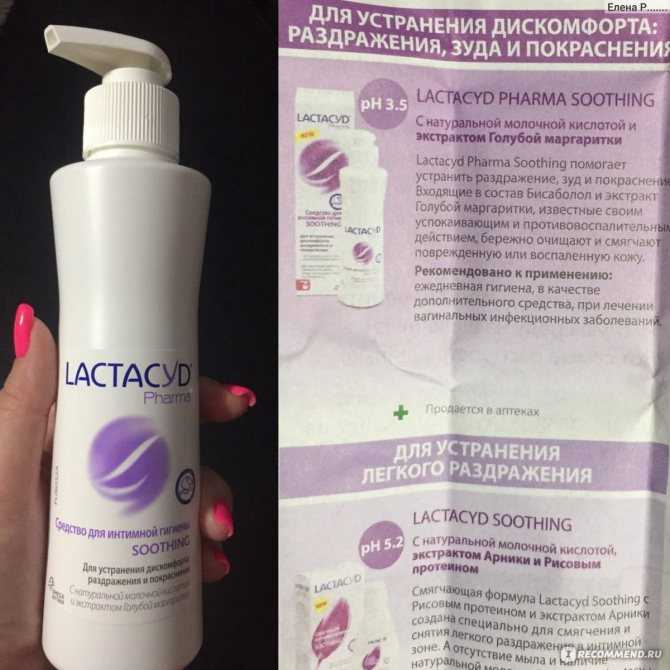 Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
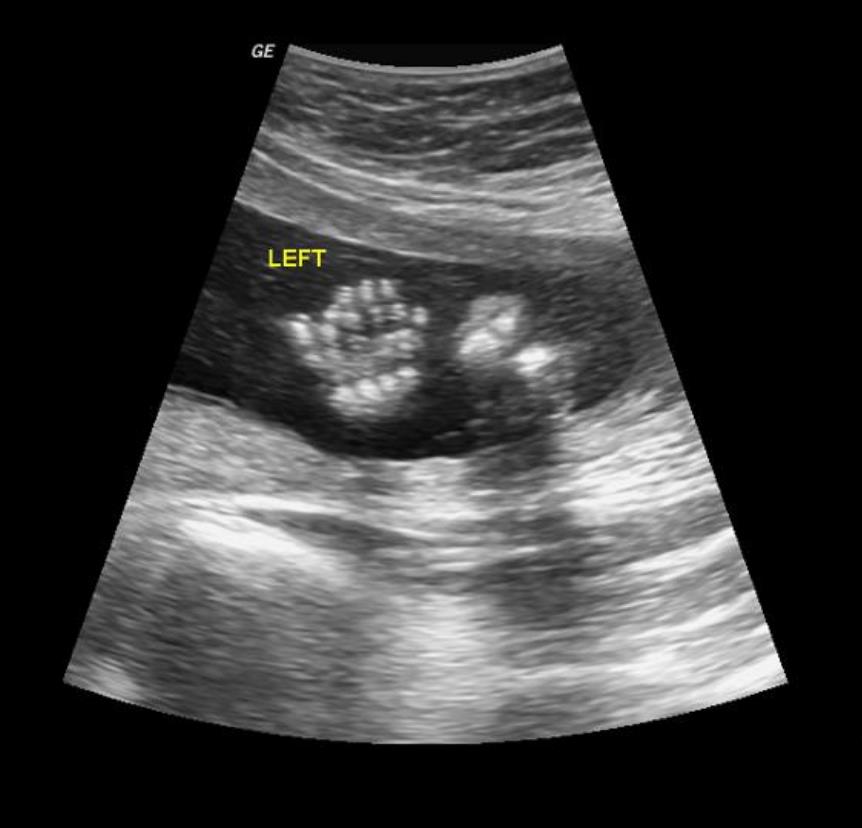
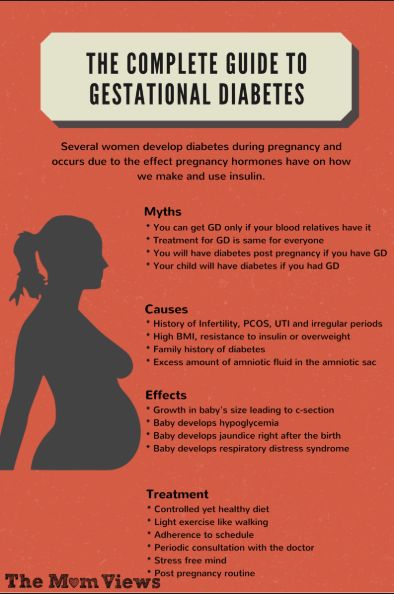
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
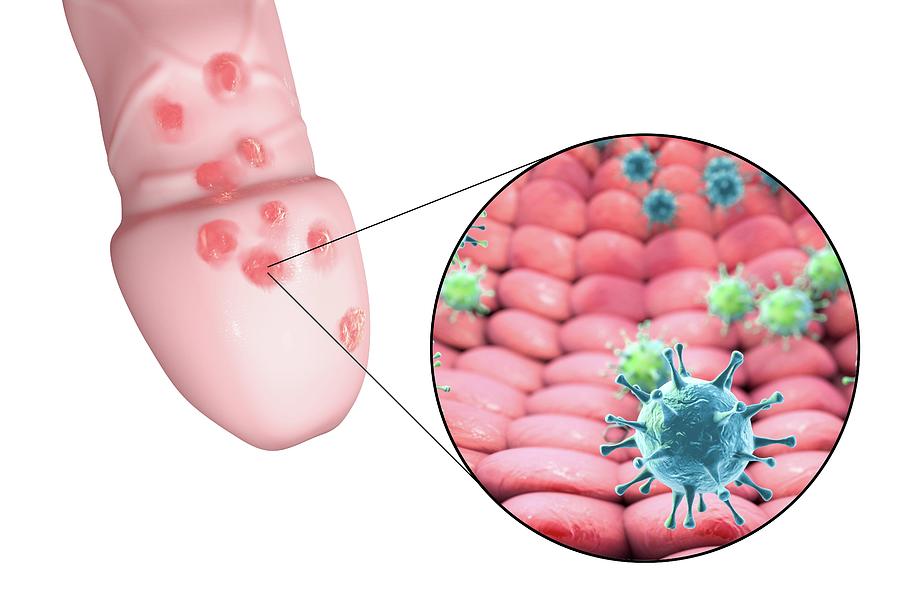
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.
- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.
- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast.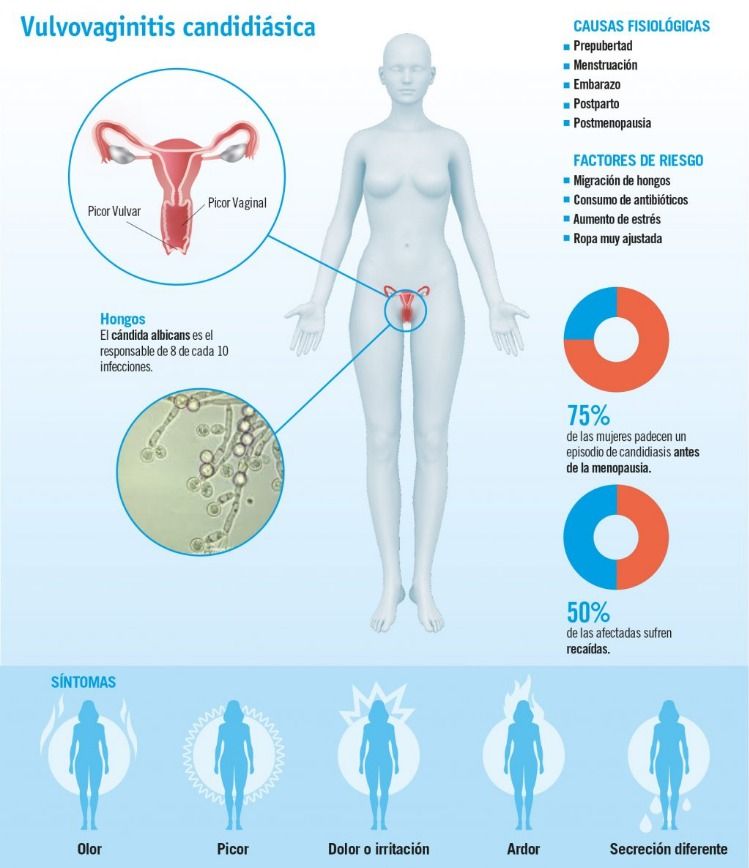 The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women. Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.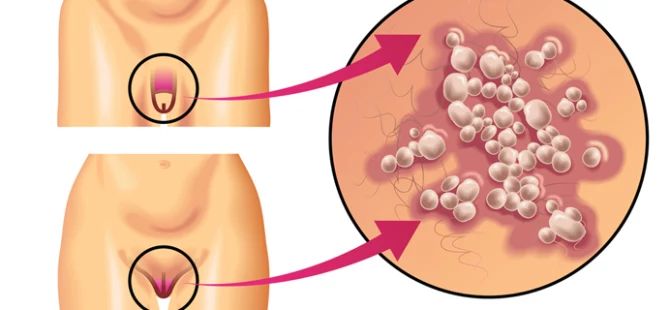
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.

- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.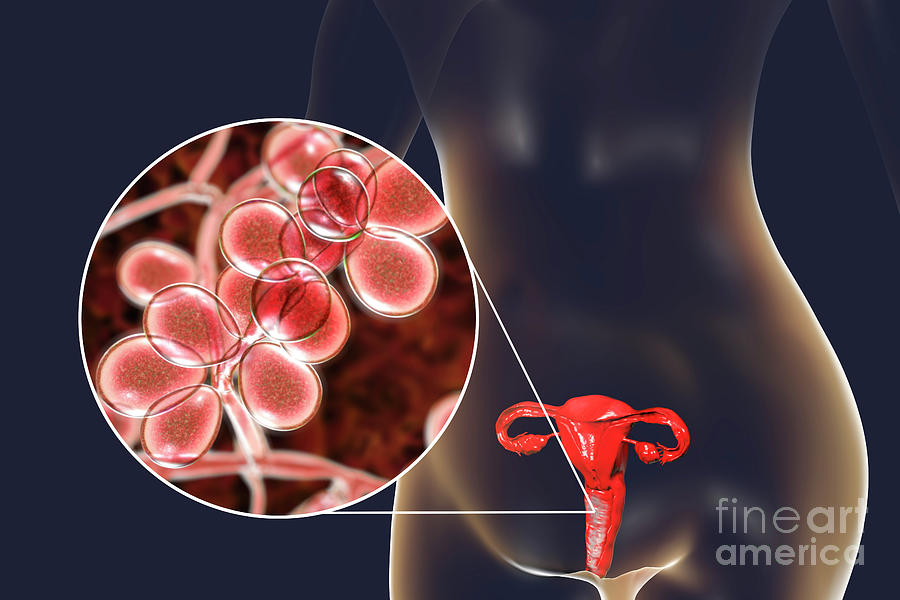
Dermatoses of pregnancy
Cost: from 1500 rubles
Sign up
Pregnancy is a wonderful time for any woman, especially when it is a planned and desired event in the life of a couple. Unfortunately, due to various circumstances, pregnancy does not always occur naturally - in such cases, modern medicine offers various procedures for assisted reproductive technologies. This makes the woman's attitude to such a natural process even more reverent. And here, often, our skin can present surprises. A number of skin conditions can worsen during pregnancy. However, traditionally prescribed drugs have limitations for use in such a situation. And here it is important that the specialist has experience in treating such situations. nine0006
Our Clinic is unique in some way, since many years of experience in managing women with skin diseases during pregnancy is not only the head doctor, who has been a consultant at the D. O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
Now let's try to explain the causes and identify the most common skin diseases during pregnancy. nine0006
During pregnancy, the main cause of skin lesions is considered to be changes in the immune system of the pregnant woman. Pathological processes can be manifested by an exacerbation of chronic skin diseases or the appearance of specific pregnancy-associated dermatosis, the so-called "pregnancy dermatosis".
Changes on the skin are very diverse both in manifestations and in the mechanisms of development. Conventionally, they can be divided into 3 groups:
I. Pregnancy stigmas:
Chloasma is the most famous of them. As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots. nine0006
Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots. nine0006
Pregnancy melanosis - skin changes in the form of hyperpigmentation in the nipples, genitals, white line of the abdomen, also without subjective sensations or inflammation. After childbirth, these disorders disappear. Chloasma and melanosis usually do not require special treatment and spontaneously regress after delivery.
II. Skin diseases that are relatively often registered during pregnancy:
This group includes a variety of skin changes and diseases that often accompany pregnancy, as well as some common dermatoses, the course of which usually worsens during gestation. The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc. nine0006
nine0006
This group includes: hyperhidrosis
- hypertrichosis
- palmoplantar telangiectasias
- erythema of the palms
- alopecia - hair loss
- onychodystrophy - changes in the nail plates
Most of these and other conditions, as a rule, disappear after childbirth. Their treatment, if necessary, is symptomatic.
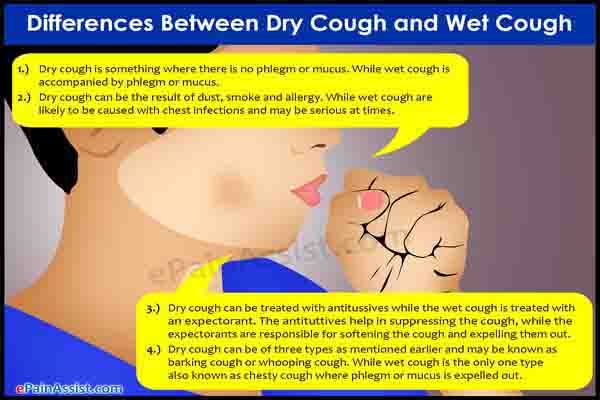
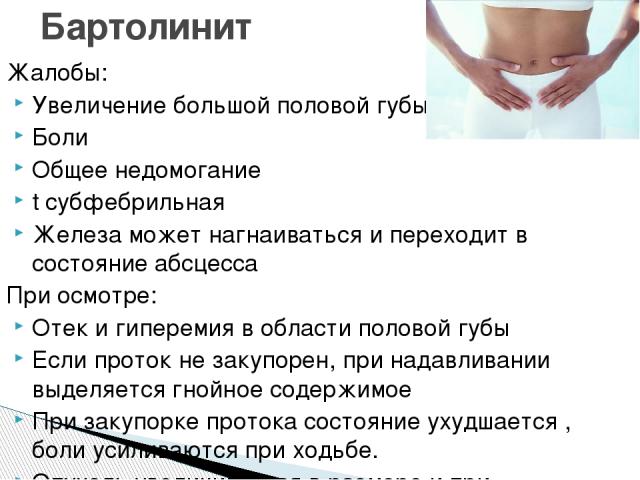
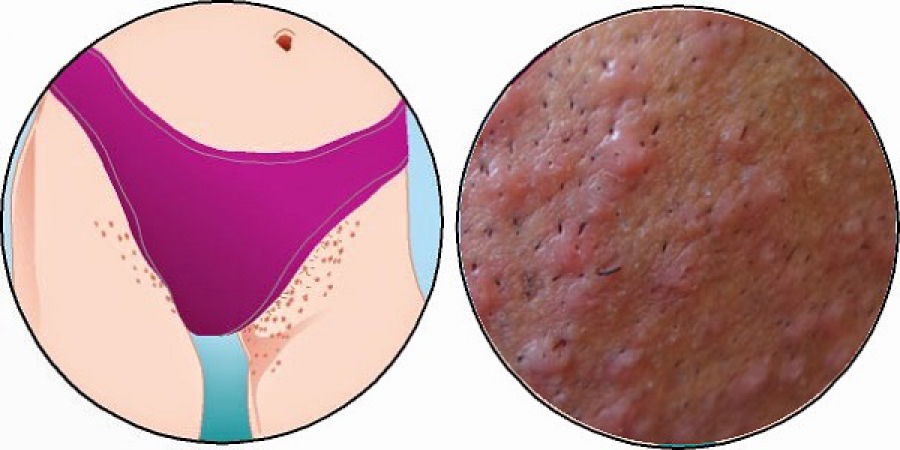
The course and severity of symptoms of other skin diseases also change during pregnancy. nine0013 These primarily include eczema, atopic dermatitis, psoriasis, lichen planus, acne, Dühring's herpetiformis. During pregnancy, they often worsen, and exacerbations are usually more pronounced, more severe than before gestation. Sometimes, on the contrary, during pregnancy, a remission occurs, which continues until childbirth, after which another exacerbation occurs. Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. The four skin diseases characteristic of pregnancy, gestational pemphigoid, polymorphic dermatosis of pregnancy, atopic dermatitis of pregnancy, and cholestasis of pregnancy can be distinguished by clinical presentation, histopathology, risk of fetal complications. Only gestational pemphigoid and intrahepatic cholestasis of pregnancy are associated with significant risk to the fetus. Because all of these dermatoses are characterized by pruritus, careful evaluation of any pruritic pregnancies is necessary. nine0006 Pregnancy pemphigoid , formerly known as herpes gestationis, is the rarest of the skin disorders of pregnancy and is an autoimmune disease. Clinically, it manifests itself in the form of papules and plaques, transforming into vesiculobullous elements, localized in the umbilical region with spread to the chest, back and limbs. Polymorphic dermatosis of pregnancy (PEP) is a benign, pruritic inflammatory disease. It usually occurs at the end of the third trimester or immediately after delivery in the first pregnancy. Urticarial papules and plaques appear first on the abdomen and, unlike gestational pemphigoid, do not affect the umbilical region. The rash usually spreads to the thighs and buttocks, and can rarely be widespread. Eruptions with clear boundaries regress spontaneously within 4-6 weeks without treatment. Treatment for PEP is based on symptomatic relief with topical corticosteroids and antihistamines. Atopic dermatitis of pregnancy (AEP) is the most common skin disorder in pregnancy. AEP is a benign disease characterized by an pruritic eczematous or papular rash. Two-thirds of AEP cases are characterized by eczematous skin changes localized to atopic areas of the body such as the neck and flexor surfaces of the extremities. The remaining cases are characterized by a papular rash in the abdomen and extremities. Lesions usually respond well to treatment and resolve spontaneously after delivery. However, AEP is more likely to recur in subsequent pregnancies. Dermatosis does not significantly affect the fetus, but there is an increased risk of developing atopic dermatitis in an infant. nine0006 Intrahepatic cholestasis of pregnancy (ICP) - characterized by acute itching that often begins on the palms and soles and then generalizes. The skin has mostly secondary lesions such as excoriations but may also have papules. Treatment is aimed at normalizing the level of bile acids in the blood serum in order to reduce the risk to the fetus and to control symptoms in the mother. Treatment with ursodeoxycholic acid (UDCA) is recommended. Other drugs that reduce itching may be used, such as antihistamines, dexamethasone. Treatment of pregnant women with dermatoses is very difficult, especially in the first trimester of pregnancy. If dermatosis is detected in a pregnant woman, it is necessary to jointly manage it by a dermatologist, an obstetrician-gynecologist. Treatment of dermatoses in pregnant women requires a differentiated approach to therapy, taking into account the duration of pregnancy, exacerbation of the disease and the prevalence of the process. The clinic has sufficient laboratory facilities and all the necessary equipment for the diagnosis and treatment of conditions such as pregnancy dermatosis. During pregnancy, a woman, as a rule, takes special care of her health and reacts anxiously to every unusual symptom. Unusual discharge and discomfort in the genital area are often the cause of the expectant mother's panic. Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman. nine0006 Vaginitis during pregnancy is a good reason to immediately contact a gynecologist and start treating this dangerous pathology. Diagnose the disease and determine how to treat colpitis during pregnancy without harming the mother and baby, qualified gynecologists will prompt. Symptoms of colpitis during pregnancy First of all, it should be determined that vaginitis or colpitis is an inflammatory disease that involves the mucous membranes of the vagina. The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia. In this case, inflammation can be seen with the naked eye. nine0006 The characteristic signs of colpitis during pregnancy do not differ from the symptoms of a non-pregnant woman: - itching and burning in the vaginal area - the inflammatory process irritates the delicate mucous membranes, which causes discomfort and sometimes pain in the vaginal walls; - pain in the lower abdomen - this symptom is especially frightening for pregnant women, but it is not associated with the tone of the uterus, as many assume, but with inflammation of the tissues; nine0006 - the appearance of specific discharge - the discharge during colpitis during pregnancy is very abundant and may have a different color and consistency. - swelling and redness of the genitals - patients often notice hyperemia and swelling of the labia and clitoris, which become more sensitive and cause discomfort to the woman. Acute vaginitis during pregnancy is accompanied by severe symptoms, which should make the patient seek professional help. This will help protect the child from possible negative consequences. Causes and types of vaginitis during pregnancy Inflammation of the mucous membranes of the vagina is usually of an infectious nature. This becomes possible due to vaginal dysbacteriosis, which often accompanies the period of pregnancy. Hormonal changes and high loads on all organs of the expectant mother cause a decrease in the body's defenses, which provokes an infectious and inflammatory process. Interestingly, depending on the cause of the development of disease, its symptoms and manifestations may differ: - candidal colpitis - accompanied by profuse curdled discharge and severe itching of the genital organs, which manifests itself even at rest; - emphysematous colpitis - a very common type of vaginitis in pregnant women. Pathology is accompanied by the formation of small watery vesicles on the surface of the mucous membranes of the genital organs. This form of colpitis resolves on its own in 2-3 weeks after childbirth; nine0006 - Trichomonas colpitis - a very dangerous form of pathology that develops when Trichomonas enter the vaginal environment. Concomitant conditions for the development of colpitis in a pregnant woman, in addition to a decrease in immunity, can be allergic reactions, microtrauma of the vagina, non-observance of personal hygiene, the presence of chronic diseases. nine0006 Colpitis during pregnancy: consequences for the child Inflammation of the mucous membranes of the vagina poses a threat not only to the health of the expectant mother, but also to the baby. The ascending route of infection can lead to pregnancy abnormalities such as polyhydramnios, premature birth, and infection of the amniotic fluid. Vaginitis is especially dangerous during childbirth, when the baby passes through an infected maternal birth canal. In at this moment there is a high probability of infection newborn. Interestingly, colpitis after pregnancy can go away on its own, but this happens relatively rarely. The development of colpitis after childbirth is most often provoked by trauma to the vaginal membranes during delivery. In connection with this fact, doctors recommend abstaining from sexual activity for the first weeks after childbirth. Violating this prohibition, a woman increases the risk of developing colpitis after childbirth. Treatment of colpitis during pregnancy Diagnosis of the disease involves a standard gynecological examination and colposcopy. This research method makes it possible to visualize the surface of the mucous membrane of the walls of the vagina and assess their condition. During the examination, the doctor takes a smear for analysis. The study of biological material is carried out by bacterioscopic and bacteriological methods. Treatment of colpitis in pregnant women requires a rational approach to prescribing antibiotics. Therefore, external symptomatic therapy becomes the leading method. nine0006
Therefore, external symptomatic therapy becomes the leading method. nine0006 III. Actually dermatoses of pregnant women
 Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids. nine0006
Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids. nine0006 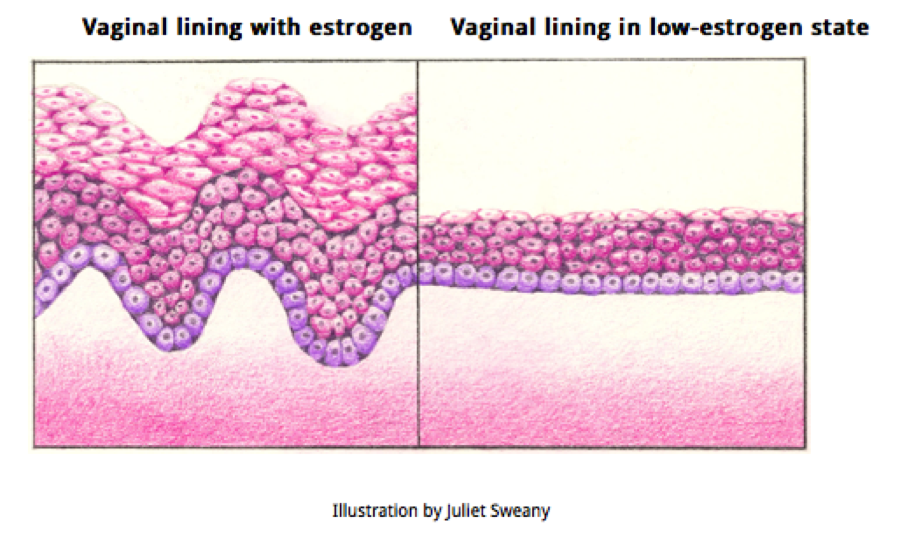 If the rash becomes generalized, a short course of systemic corticosteroids may be used. nine0006
If the rash becomes generalized, a short course of systemic corticosteroids may be used. nine0006  In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus. nine0006
In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus. nine0006 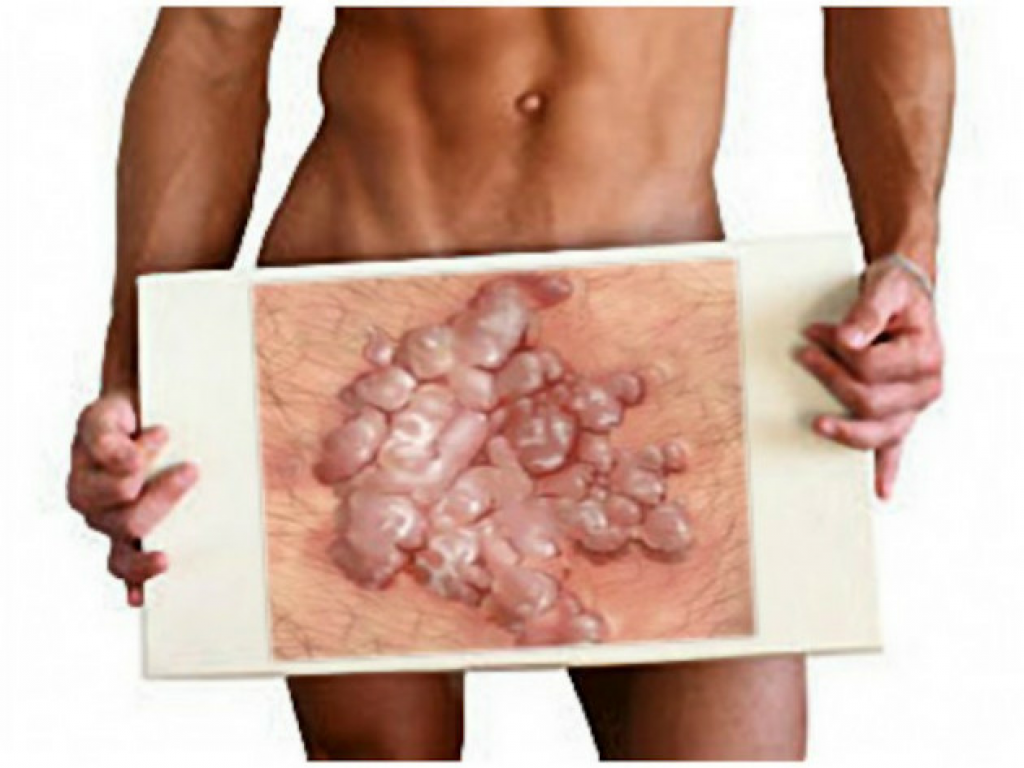 nine0006
nine0006 COLPITIS IN PREGNANCY

 Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice; 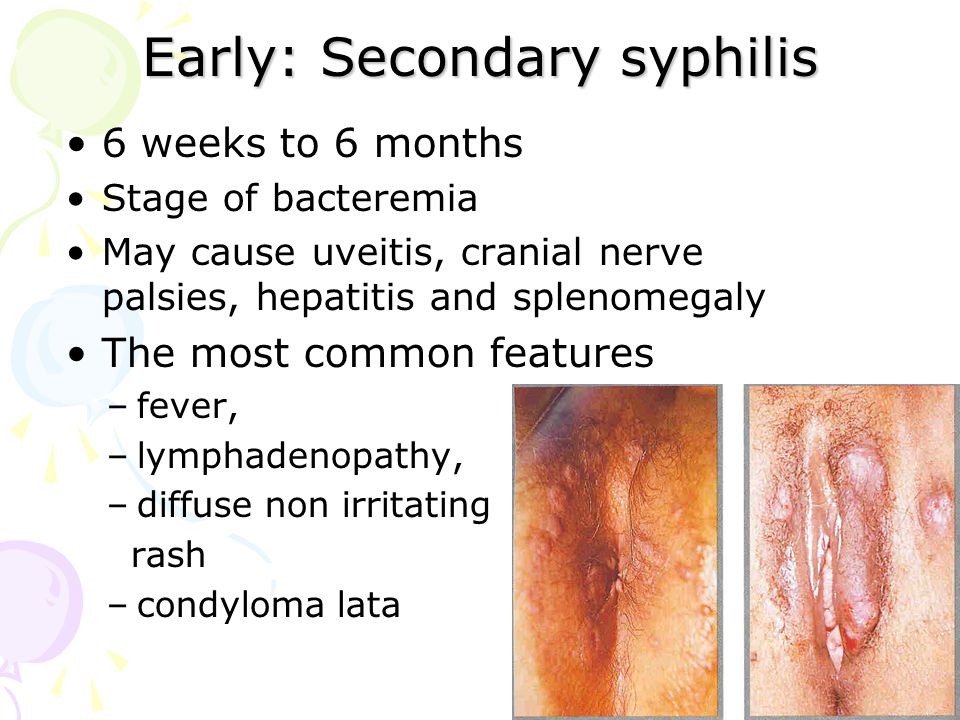 In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc. 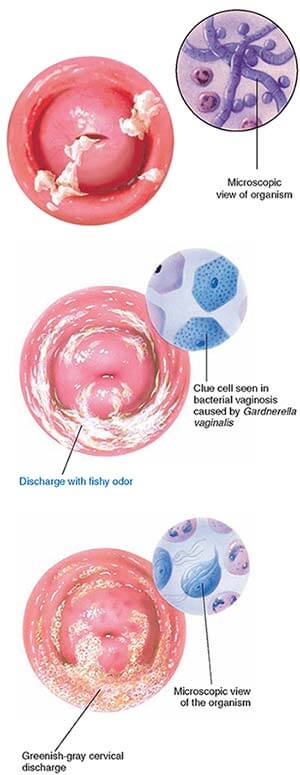 Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.