Amniocentesis for down syndrome
Amniocentesis - NHS
Amniocentesis is a test you may be offered during pregnancy to check if your baby has a genetic or chromosomal condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome.
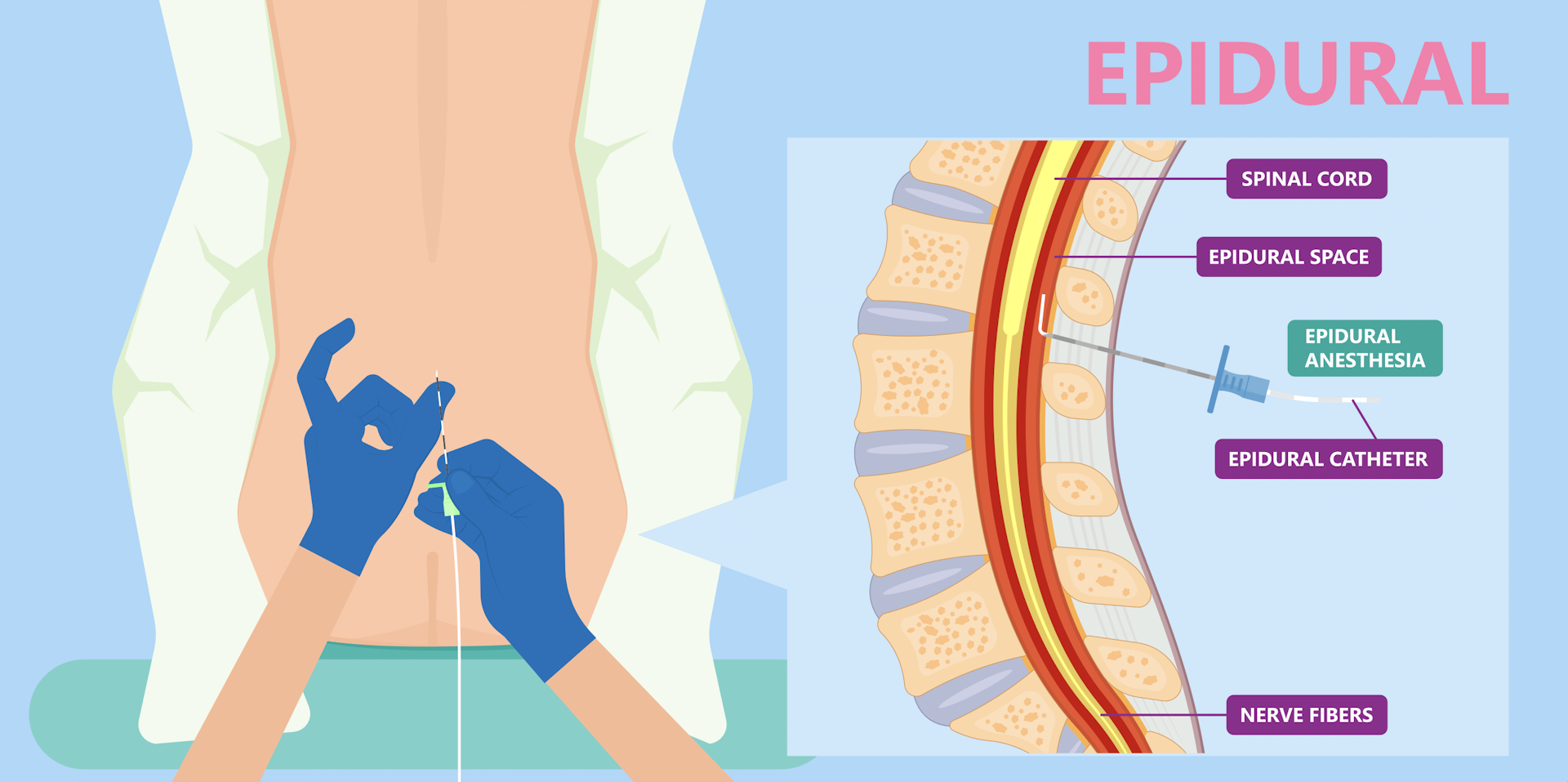
It involves removing and testing a small sample of cells from amniotic fluid, the fluid that surrounds the baby in the womb (uterus).
When amniocentesis is offered
Amniocentesis is not offered to all pregnant women. It's only offered if there's a higher chance your baby could have a genetic condition.
This could be because:
- an antenatal screening test has suggested your baby may be born with a condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome
- you have had a previous pregnancy that was affected by a genetic condition
- you have a family history of a genetic condition, such as sickle cell disease, thalassaemia, cystic fibrosis or muscular dystrophy
It's important to remember that you do not have to have amniocentesis if it's offered. It's up to you to decide whether you want it.
A midwife or doctor will speak to you about what the test involves and let you know what the possible benefits and risks are to help you make a decision.
Find out about why amniocentesis is offered and deciding whether to have it
How amniocentesis is performed
Amniocentesis is usually carried out between the 15th and 20th weeks of pregnancy, but you can have it later if necessary.
It can be performed earlier, but this may increase the risk of complications of amniocentesis and is usually avoided.
During the test, a long, thin needle is inserted through your abdominal wall, guided by an ultrasound image.
The needle is passed into the amniotic sac that surrounds your baby and a small sample of amniotic fluid is removed for analysis.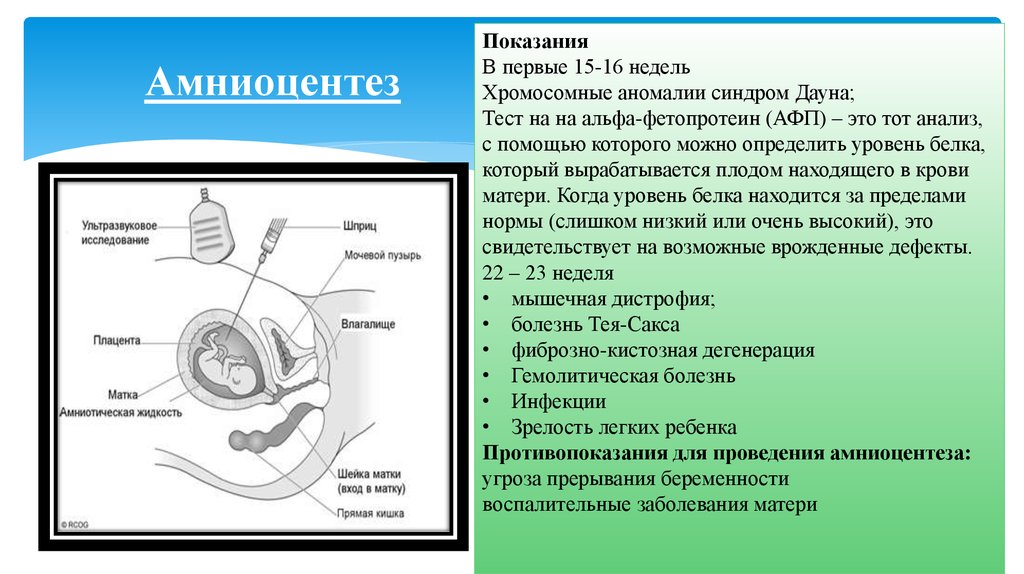
The test itself usually takes about 10 minutes, although the whole consultation may take about 30 minutes.
Amniocentesis is usually described as being uncomfortable rather than painful.
Some women describe experiencing a pain similar to period pain or feeling pressure when the needle is taken out.
Find out more about what happens during amniocentesis
Getting your results
The first results of the test should be available within 3 working days and will tell you whether Down's syndrome, Edwards' syndrome or Patau's syndrome has been discovered.
If rarer conditions are also being tested for, it can take 3 weeks or more for the results to come back.
If your test shows that your baby has a genetic or chromosomal condition, the implications will be fully discussed with you.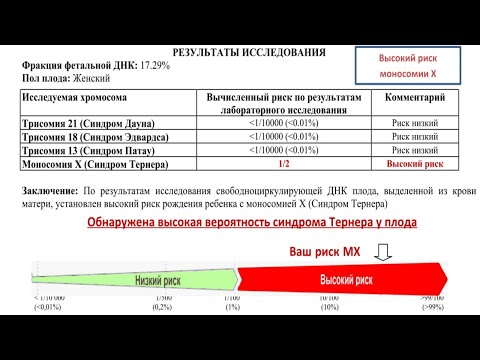
There's no cure for most of the conditions amniocentesis finds, so you'll need to consider your options carefully.
You may choose to continue with your pregnancy, while gathering information about the condition so you're fully prepared.
Find out more about having a baby that might be born with a condition
Or you may consider ending your pregnancy (having a termination).
Find out more about the results of amniocentesis
What are the risks of amniocentesis?
Before you decide to have amniocentesis, the risks and possible complications will be discussed with you.
One of the main risks associated with amniocentesis is miscarriage, which is the loss of the pregnancy in the first 23 weeks.
This is estimated to occur in up to 1 out of every 200 women who have amniocentesis.
There are also some other risks, such as infection or needing to have the procedure again because it was not possible to accurately test the first sample.
The risk of amniocentesis causing complications is higher if it's carried out before the 15th week of pregnancy, which is why the test is only done after this point.
Find out more about the possible complications of amniocentesis
What are the alternatives?
An alternative to amniocentesis is a test called chorionic villus sampling (CVS).
This is where a small sample of cells from the placenta, the organ that links the mother's blood supply with her baby's, is removed for testing.
It's usually carried out between the 11th and 14th weeks of pregnancy, although it can be performed later than this if necessary.
With CVS, the risk of miscarriage is similar to the risk of miscarriage for amniocentesis (up to 1 out of every 200).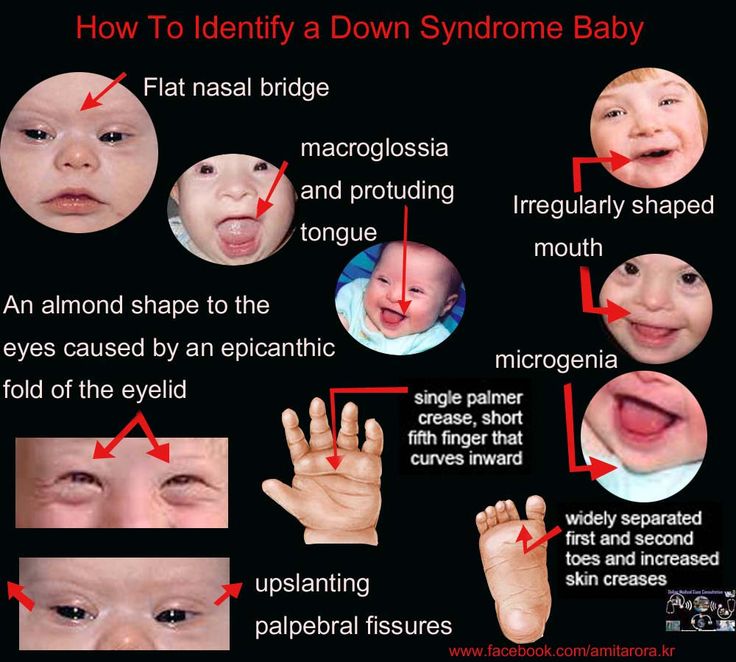
As the test can be carried out earlier, you'll have more time to consider the results.
If you're offered tests to look for a genetic or chromosomal condition in your baby, a specialist involved in carrying out the test will be able to discuss the different options with you and help you make a decision.
Page last reviewed: 12 October 2022
Next review due: 12 October 2025
Prenatal Testing for Down Syndrome | Patient Education
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age. Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them. The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome.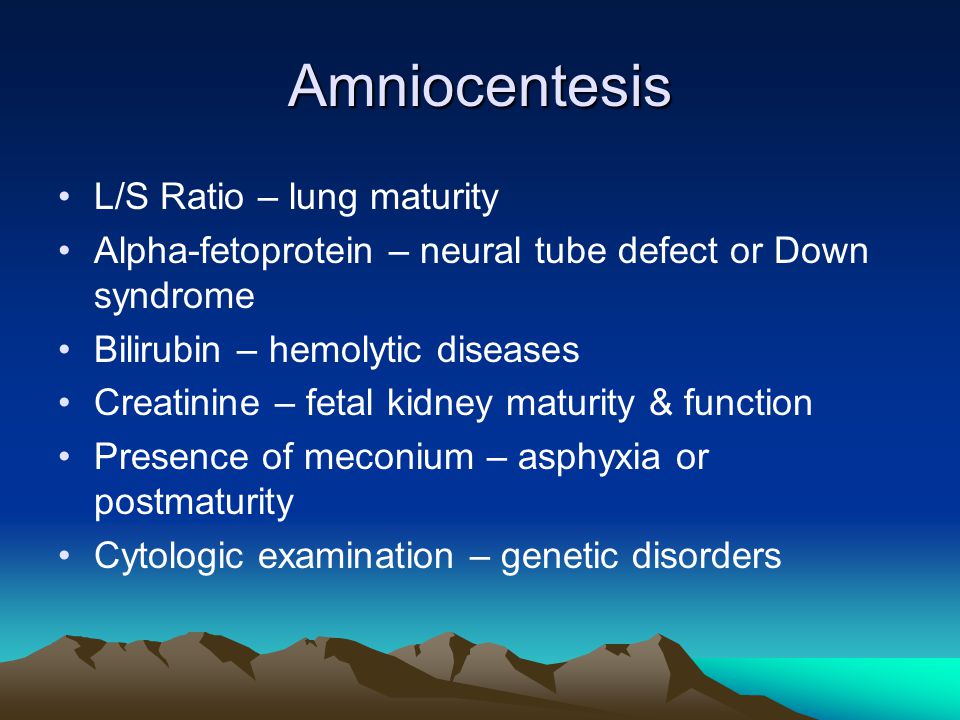 These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.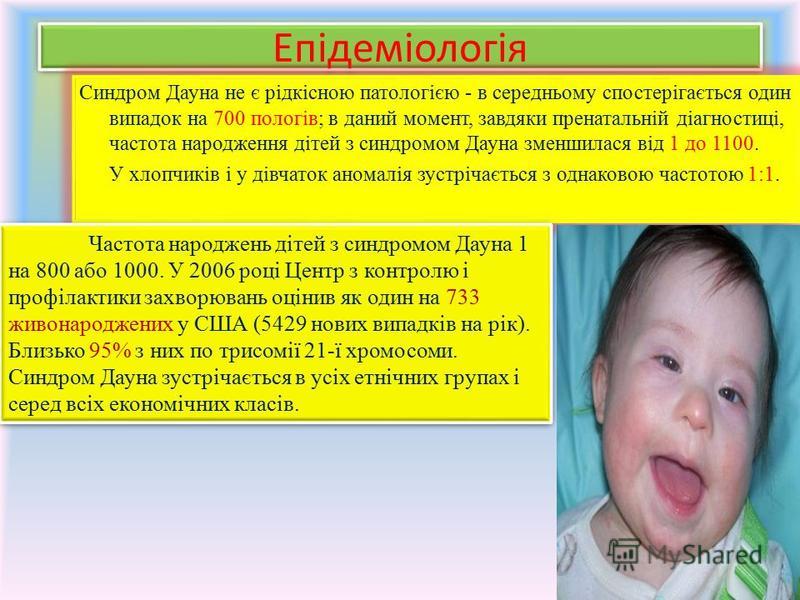
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid. The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month. A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Related clinic
Prenatal Diagnostic Center
1825 Fourth St., Third Floor
San Francisco, CA 94158
(415) 476-4080
M-F, 8 a.m. - 5 p.m.
Diagnostics of blood trisomy - DW - 02.02.2012
Photo: Fotolia/Sven Bähren
February 3, 2012
Until now, for road diagnostics of Downencenta syndrome, pregnant women had to be subjected a procedure that is fraught with complications. Now they have an alternative.
https://p.dw.com/p/13wNH
Advertising
The disease known as Down's syndrome was described as early as the middle of the 19th century, but scientists did not find out the cause of this congenital pathology until a whole century later. It turned out that Down syndrome occurs as a result of a genetic anomaly - the presence of an extra chromosome. If in the nucleus of each cell of a healthy person there is a set of 23 pairs of chromosomes, then in the cells of patients suffering from Down syndrome, the 21st chromosome is represented not by two, but by three copies. nine0005
It turned out that Down syndrome occurs as a result of a genetic anomaly - the presence of an extra chromosome. If in the nucleus of each cell of a healthy person there is a set of 23 pairs of chromosomes, then in the cells of patients suffering from Down syndrome, the 21st chromosome is represented not by two, but by three copies. nine0005
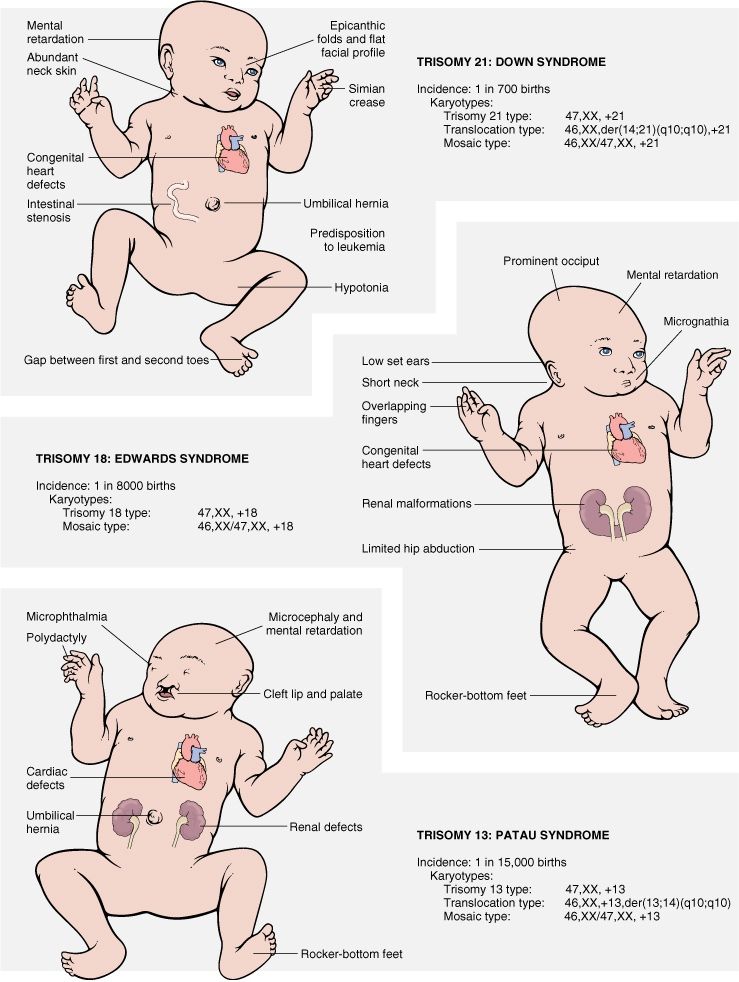
This anomaly, called trisomy 21, manifests itself in a number of specific external features (short stature, hypotension, underdeveloped ears, flat face with slanted eyes, thickened cervical skin fold, wide hands with short fingers and a single crease along the palm) and often accompanied by congenital heart disease, underdevelopment of the intestine, deafness, strabismus. In addition, many of these patients show signs of mental retardation.
nine0021 Amniocentesis - risky procedure
The probability of giving birth to a child with Down syndrome, and so not so small, increases with the age of the parents, especially the mother. In Germany, for example, one such baby accounts for an average of 800 births. Pregnant women who want to make sure in advance that this fate will pass for them, until recently, had only one reliable method at their disposal - prenatal (that is, prenatal) diagnosis. Specifically, amniocentesis. This is an invasive procedure, during which the doctor uses a special needle through the anterior abdominal wall of the pregnant woman to puncture the embryonic membrane in order to obtain a sample of amniotic fluid for their subsequent laboratory examination. After all, amniotic fluid also contains embryonic cells, and their analysis reveals genetic and chromosomal defects. nine0005
In Germany, for example, one such baby accounts for an average of 800 births. Pregnant women who want to make sure in advance that this fate will pass for them, until recently, had only one reliable method at their disposal - prenatal (that is, prenatal) diagnosis. Specifically, amniocentesis. This is an invasive procedure, during which the doctor uses a special needle through the anterior abdominal wall of the pregnant woman to puncture the embryonic membrane in order to obtain a sample of amniotic fluid for their subsequent laboratory examination. After all, amniotic fluid also contains embryonic cells, and their analysis reveals genetic and chromosomal defects. nine0005
One trouble: a puncture of the embryonic membrane is fraught with complications. Michael Entezami, gynecologist at the Center for Prenatal Diagnosis and Human Genetics in Berlin, explains: “There is a 0.3 to 1.0 percent chance that amniotic fluid sampling alone will lead to miscarriage. or even weeks after the procedure, either the fetal heart suddenly stops beating, or there is a rupture of the membranes, premature outflow of amniotic fluid, contractions begin, the temperature rises, and as a result, a miscarriage. nine0005
nine0005
New test - real breakthrough
So far, in Germany alone, about 70,000 pregnant women have had amniocentesis every year. But now the vast majority of expectant mothers will be able to do without this unpleasant and risky procedure: soon doctors will be able to diagnose trisomy in the fetus based on a pregnant woman's blood test. Michael Entezami says: "This test is a real breakthrough in an area where 20 years of research has been carried out to develop a method that allows you to make conclusions about the chromosomes of the fetus without compromising the course of pregnancy. And now they have been crowned with success." nine0005
All that is required for analysis is a sample of the mother's blood. The gynecologist explains: "Maternal blood always contains the mother's hereditary material from the decayed cells of her body and directly from blood cells, but about five percent is the hereditary material of the embryo from placental cells"
Not only trisomy 21, but also 13 and 18
Placental cells are usually genetically identical to fetal cells.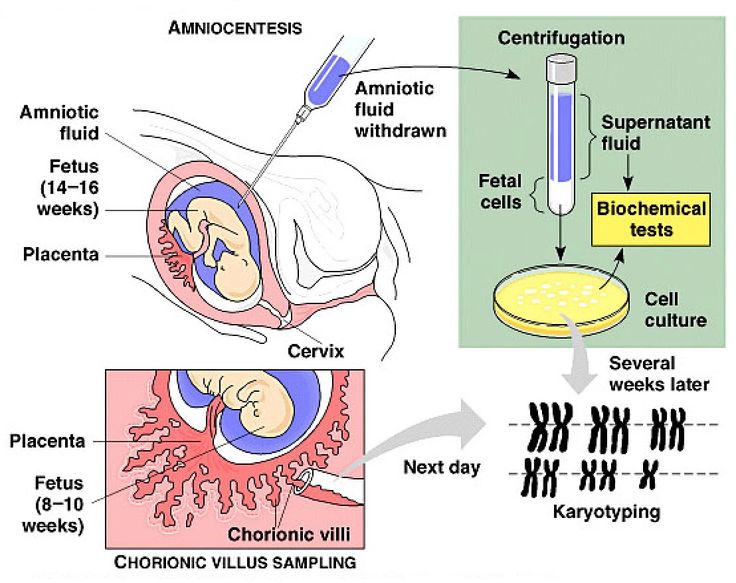 Using special methods adopted in molecular biology, researchers increase the concentration of the hereditary material of the embryo in a maternal blood sample, and then determine how many copies of the 21st chromosome are present in it. And not only the 21st. The same analysis at the same time allows you to identify such less common genetic anomalies as trisomy on the 13th and 18th chromosomes. nine0005
Using special methods adopted in molecular biology, researchers increase the concentration of the hereditary material of the embryo in a maternal blood sample, and then determine how many copies of the 21st chromosome are present in it. And not only the 21st. The same analysis at the same time allows you to identify such less common genetic anomalies as trisomy on the 13th and 18th chromosomes. nine0005
Michael Entezami is one of the first in Germany to use the new test - so far as part of an experiment, in order to test its reliability and validity. Today, only those patients of Berlin physicians who, in any case, are also recommended to study amniotic fluid, donate blood for such an analysis. But if it’s too early to sum up here, then in the USA, where the test was introduced into clinical practice in October last year, the numbers are already there, says Michael Entezami: “The error rate is low, the reliability of detecting trisomy 21 is about 98 percent, and cases of "false alarms" are practically not registered.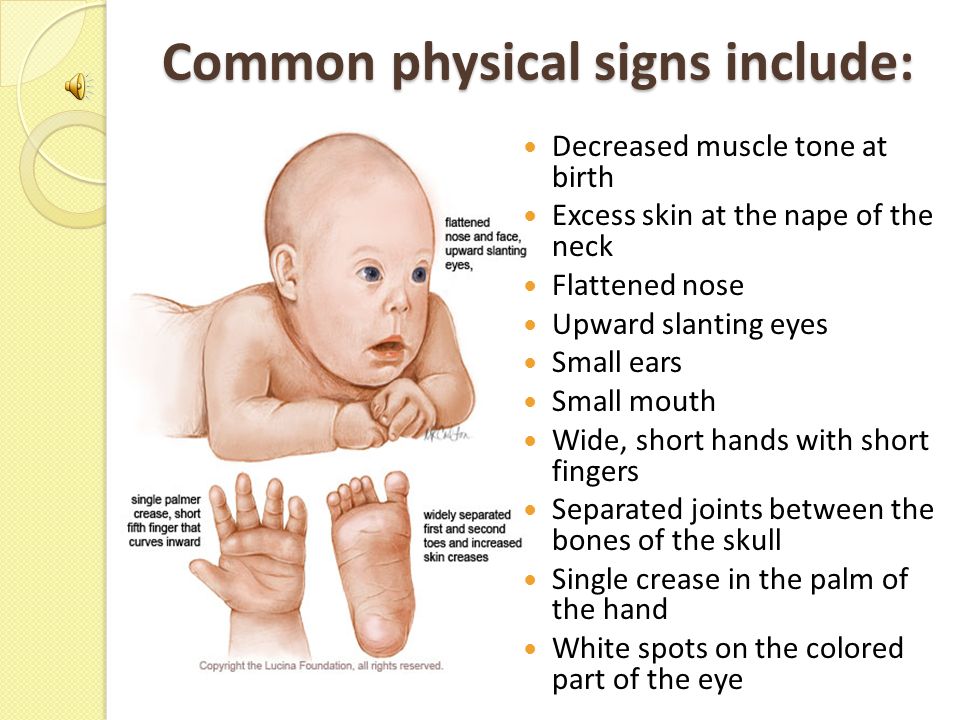 However, it should be borne in mind that, in principle, errors are possible."
However, it should be borne in mind that, in principle, errors are possible."
Not a panacea, but a serious alternative
Therefore, the gynecologist does not recommend expectant mothers to rely solely on a blood test. First of all, at the 11th week of pregnancy, they should undergo an ultrasound examination, during which, in particular, the thickness of the nuchal space in the fetus is measured. And only if this screening gives cause for alarm, it makes sense to turn to a new test instead of an amniocentesis. nine0005
Michael Entezami believes that such a test will relieve 80 - 90 percent of pregnant women from the need to study amniotic fluid, especially if it is dictated only by age. But if a blood test indicates trisomy and the question arises of artificial termination of pregnancy, here, the gynecologist believes, one cannot do without amniocentesis: “An inner feeling tells me that, at least in the coming years, hardly anyone will take responsibility decide on an abortion only on the basis of such a blood test.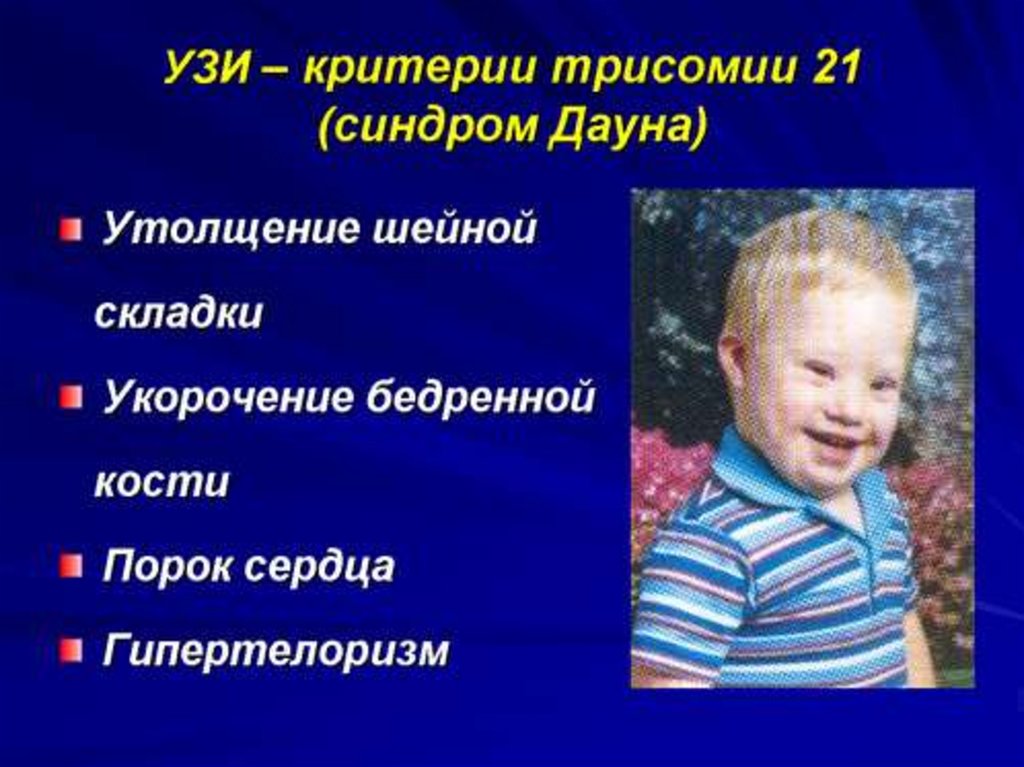 nine0005
nine0005
And yet, although the new test is not a panacea, it will greatly simplify the prenatal diagnosis of Down syndrome and become a worthy alternative for thousands and thousands of pregnant women, saving them from the unpleasant and risky procedure of puncture of the germinal membrane. In Germany, the new test should be on the market in the middle of this year.
Author: Vladimir Fradkin
Editor: Daria Bryantseva
Advertising
Skip section More related topicsEven on the topic
, show another
Smat the section of the top-theme1 p. Out of 3
, Skip the section Other publications DWto the main page
What is amniocentesis, indications and conduct of the procedure
what is it amniocentesis?
Amniocentesis is a specific amniotic fluid test. A study is carried out by puncturing the abdomen, the embryonic membrane in order to obtain a sample of the amniotic fluid containing fetal cells. According to the results of studies of the amniotic fluid, the doctor can determine the presence or absence of genetic diseases in the unborn child. Amniocentesis in Kyiv is successfully performed at the IPF Family Planning Institute. nine0005
A study is carried out by puncturing the abdomen, the embryonic membrane in order to obtain a sample of the amniotic fluid containing fetal cells. According to the results of studies of the amniotic fluid, the doctor can determine the presence or absence of genetic diseases in the unborn child. Amniocentesis in Kyiv is successfully performed at the IPF Family Planning Institute. nine0005
Depending on the indications, several types of amniotic fluid tests are carried out:
- hormonal analysis, determines the composition and amount of available hormones;
- cytological - studies the cells and particles of the fetus contained in the amniotic fluid in order to detect chromosomal abnormalities;
- immunological - "will tell" about possible violations of the emerging immunity;
- biochemical analysis will show the composition and properties of amniotic fluid; nine0087
- analysis for general indicators will determine the color, transparency of the liquid, its amount.
The amniocentesis procedure can be performed at the IPF clinic. Sign up for a consultation by going to at the link in contacts.
At what stage of pregnancy can amniocentesis be done?
The study of amniotic fluid is carried out not earlier than the 14th week of pregnancy. Why? Until this time, there are not enough cells in the amniotic fluid to obtain reliable analysis results. nine0005
14 weeks of pregnancy is the earliest period at which doctors can perform amniocentesis: at this time, it is already possible to study the chromosome set of the embryo and make sure that there are no/presence of anomalies, the most common of which is Down syndrome.
The terms of the research procedure are from 16 to 22 weeks, and since the results of the analysis do not come immediately, they are ready in a few weeks, it is better to do it at 16-17 weeks, in case of disappointing results, it is possible to terminate the pregnancy before 20 -and a weekly period.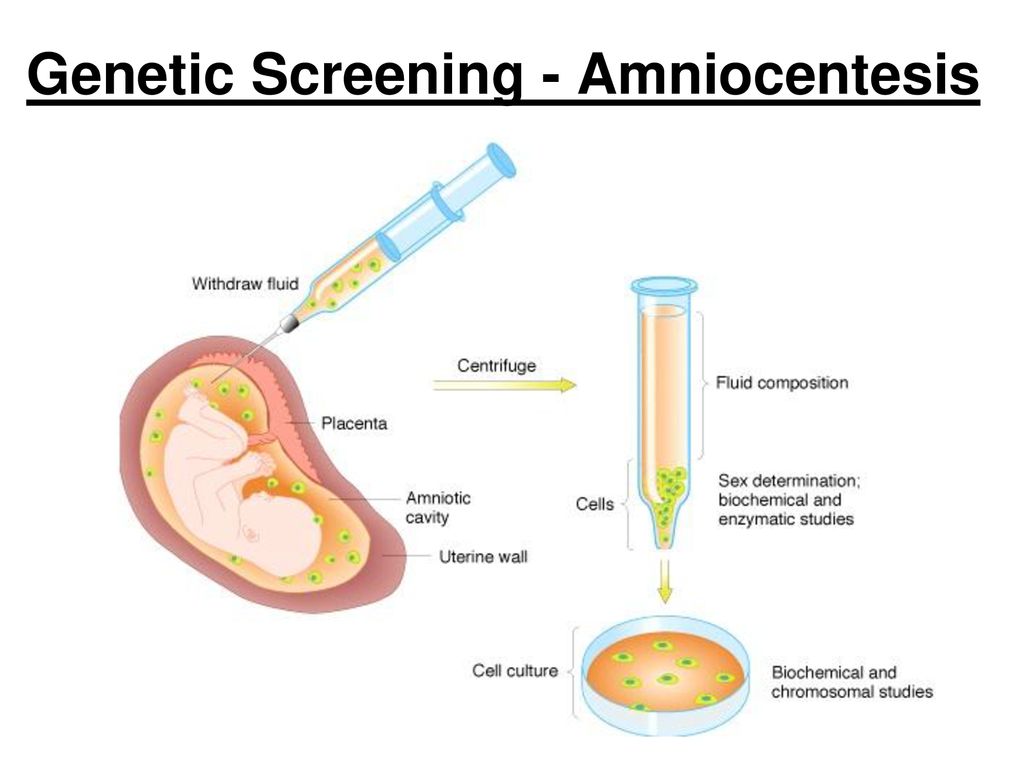 nine0005
nine0005
Indications and contraindications for analysis
Indications for analysis
When a woman finds out she is pregnant, she goes to an obstetrician-gynecologist. At the appointment, the doctor collects an anamnesis, prescribes a list of tests, taking into account the duration of pregnancy.
If at the time of data collection or the results of the tests done, the gynecologist doubts the normal course of pregnancy, the health of the fetus and its healthy development, he may suggest an amniocentesis to the pregnant woman. nine0005
What factors may warrant a procedure?
- Age. A doctor may suggest an amniocentesis procedure for a pregnant woman over 35 years of age.
- Burdened heredity. If during the collection of anamnesis it was found that there are genetic diseases in the family of the pregnant woman and her husband, as well as from relatives.
- A woman had a child with a chromosome abnormality in a previous pregnancy.
- Ultrasound examination raised suspicions regarding the absence of anomalies.
 nine0087
nine0087 - The results of screening tests showed possible disorders that require invasive intervention to clarify. Invasive intervention is also used in case of necessary surgical treatment of the fetus, as well as in the presence of medical indications for abortion.
Contraindications for amniocentesis
The main contraindication for amniocentesis is the risk of miscarriage.
Do not perform the procedure under the following circumstances:
- placental abruption;
- the presence of urogenital infections;
- the presence of acute inflammatory processes in the body of a woman;
- tumor-like neoplasms of the muscular layers of the uterus of large sizes;
- exacerbations of chronic diseases.
An obstacle to the analysis may be poor blood clotting, abnormal development of the uterus, the location of the placenta on the anterior wall of the uterus.
If a woman fears complications, she may refuse the procedure, but she must clearly understand what the consequences of such a decision may be. nine0005
nine0005
Amniocentesis Methods and Process
Two methods of amniocentesis are known to physicians today:
- The first method is called the Free Hand Method.
The procedure is carried out under ultrasound control, it is with the help of an ultrasound probe that the insertion site of the puncture needle is specified.
To avoid the risk of possible complications and the threat of miscarriage, the needle injection site is chosen where the placenta is absent or, if this is not possible, in the place where the placental wall is as thin as possible. nine0005
- The second method is the Puncture Adapter Method.
The second method differs from the first one in that the puncture needle is fixed on an ultrasound probe, and then a trajectory is drawn along which the needle will go.
The main plus of this method is the possibility of visual visibility of the needle and its trajectory during the entire course of the procedure.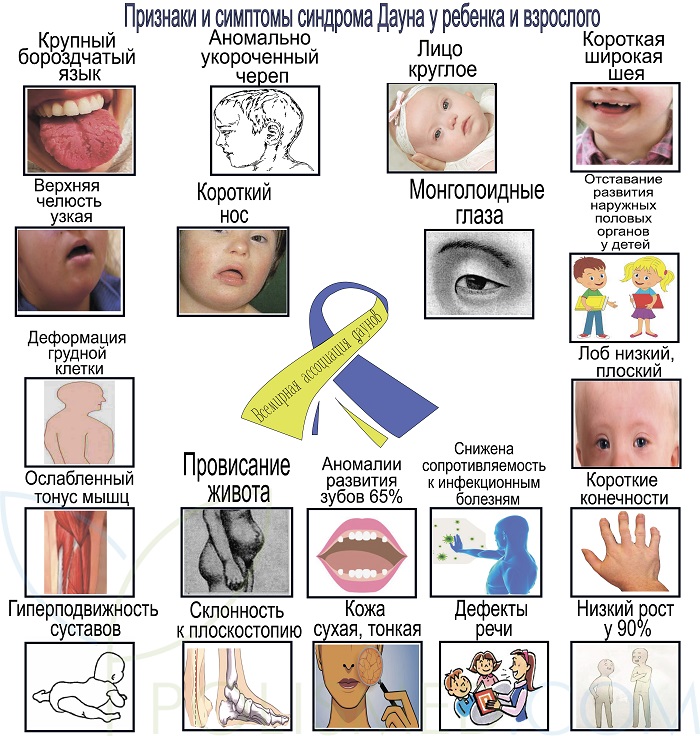
However, this method requires experience and certain professional skills from the doctor.
How long does an amniocentesis procedure take and how painful is it? nine0080
In terms of time, the procedure will take, together with preparation, about 5 minutes. Puncture of the abdomen with a puncture needle - 1 minute. The next step in amniocentesis is amniotic fluid sampling. The next 2 hours after the operation, the pregnant woman should be in the hospital under the supervision of doctors.
Patients do not feel any severe pain during amniocentesis, the procedure is similar to a regular injection. A slight movement in the lower abdomen can be felt at the time of amniotic fluid sampling.
Many pregnant women, driven by a sense of fear, ask for pain relief. Yes, local anesthesia can be used, but doctors have noticed that anesthetic injections cause more discomfort than the amniocentesis procedure itself, and therefore gynecologists recommend women not to do anesthesia. nine0005
nine0005
Most women agree, because it is better to endure one injection instead of two.
How is the amniocentesis procedure performed?
The procedure takes place in an office equipped with an ultrasound machine. The gynecologist invites the pregnant woman to lie down and expose her belly. The puncture site on the abdomen is treated with an antiseptic - iodine or alcohol. The next step - the doctor, using an ultrasound machine, determines the most successful place for a puncture: the point of insertion of the needle should be away from the baby and from the placenta. nine0005
When looking for a good point, the gynecologist may ask the pregnant woman to turn on one side, then on the other - it all depends on the position of the fetus in the uterus and the location of the placenta.
That's it, a good point has been found: the doctor inserts a thin puncture needle, pierces the skin of the abdomen and enters the membrane surrounding the amniotic fluid. The sampling of amniotic fluid is carried out under ultrasound control - about 2 tablespoons are taken for analysis.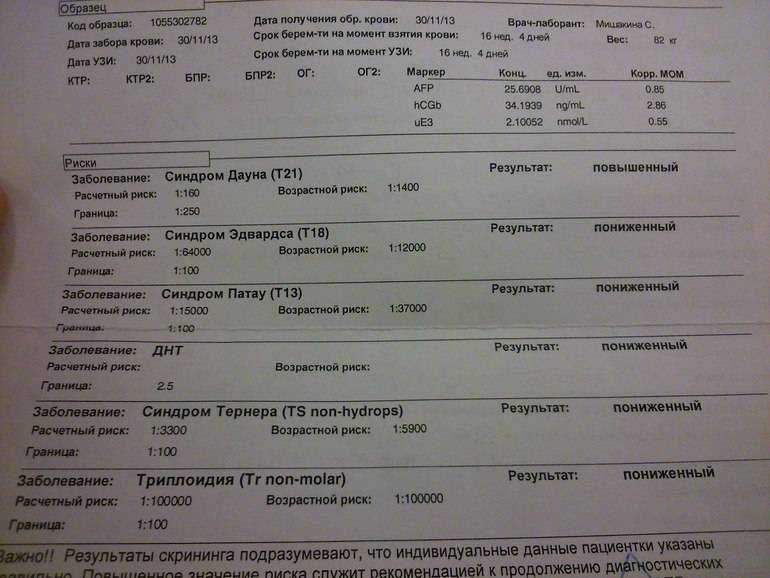 Future babies do not feel a lack of amniotic fluid, and soon its amount is replenished. nine0005
Future babies do not feel a lack of amniotic fluid, and soon its amount is replenished. nine0005
What if I am Rh negative and the baby's father is Rh positive?
If a pregnant woman has a negative Rh factor, and the father of the child has a positive Rh factor, then after the amniocentesis procedure, the pregnant woman is given a special drug that prevents the immune conflict between the body of the mother and the unborn child.
What happens after the amniocentesis?
After the amniotic fluid collection procedure, the specialist will show the baby on the screen of the ultrasound machine, and the woman herself will be able to make sure that nothing happened to the baby. nine0005
A few hours after the procedure, the doctor observes the patient, then the pregnant woman can go home. The rest of the day is recommended to be spent in peace, it is advisable for a working woman to take a day off. 2-3 days after the procedure, gynecologists advise not to lift weights, refrain from sex, air travel is not recommended in the next few days.
One to two days after the amniocentesis, the woman may experience mild abdominal cramps. There is no cause for concern - this is normal after the procedure. nine0005
An urgent need to consult a gynecologist if:
- spasms become pronounced, intensify and become frequent;
- bleeding from the vagina;
- profuse watery discharge began to stand out.
Amniocentesis - how to take the test results?
The test results are within the normal range, they say that your baby is all right - the chromosome set of the unborn child is formed normally, there are no signs of a neural tube defect. The test is quite accurate and informative, but, nevertheless, it should be remembered that no one will give a 100% guarantee about the birth of an absolutely healthy child. nine0005
If the test showed that the fetus has congenital malformations, development takes place with pathologies - a pregnant woman and her husband will have to make a very difficult decision. In some cases, the decision depends on various facts - on the type of defect, the partner's reaction to unpleasant news, the woman's personal reaction to what happened.
In some cases, the decision depends on various facts - on the type of defect, the partner's reaction to unpleasant news, the woman's personal reaction to what happened.
Naturally, many women have questions:
- Should I continue this pregnancy?
If a fetus is found to have a serious defect, some women go for a medical abortion. Others decide to have a baby with a defect. nine0005
- Where is the best place to give birth?
If the fetus has a defect that requires surgical intervention at birth, childbirth should only be in specialized clinics where doctors know how to act, where to provide such services - not new.
For a baby with a disability, is it better to have a natural birth or a caesarean section?
The results of the amniocentesis will show if a caesarean section is needed and if the baby is ready for delivery.
Amniocentesis - is there a similar test? nine0080
Chorionic villus sampling may be an alternative to amniocentesis in the first trimester of pregnancy. With the help of this test, the presence / absence of Down syndrome and other genetic diseases in the future baby can be detected in early pregnancy. But, this test does not detect neural tube defects.
With the help of this test, the presence / absence of Down syndrome and other genetic diseases in the future baby can be detected in early pregnancy. But, this test does not detect neural tube defects.
Modern research has confirmed that both amniocentesis and chorionic villus sampling cause the same percentage of miscarriages.
Even if the procedures are carried out by experienced graduates, spontaneous abortions occur in 400 cases - 1.
Other studies show an increased risk of 2 or even 4 miscarriages per 400 cases. These statistics are in medical centers where specialists are less professional, where such procedures are not often performed, especially chorionic villus biopsy.
IPF specialists are highly qualified, and therefore the risk of spontaneous miscarriage after procedures in our clinic is minimal.
Amniocentesis - possible risk during test
In most cases, the amniocentesis procedure is quite safe. The reaction of women to the results of a test, which can show that the fetus has a congenital pathology, an inherited disease, or Down's syndrome, is more unpredictable than the possible risks of the procedure. But, nevertheless, certain risks exist:
But, nevertheless, certain risks exist:
- If an inexperienced specialist undertakes the procedure, he can prick the mother or fetus with a needle. To reduce this risk, ultrasound is used to accurately guide the puncture needle. It happens that during the procedure the placenta is pierced, but it is quickly restored. nine0087
- There is a risk of infection in the amniotic sac - this happens 1 in 1000 cases.
- Miscarriages. According to statistics, when amniocentesis is performed by experienced specialists, the risk of spontaneous abortion is 1 in 400 cases. Sometimes miscarriages after the procedure are not related to the procedure itself, the problem may lie in the course of pregnancy or in the fetus itself.
- If the procedure is performed before the 15th week, there is a risk that the unborn child will develop clubfoot.
- There is a risk that maternal and fetal blood will mix during amniocentesis. This fact can cause concern only when the mother and fetus have different Rh factors (the mother has a negative Rh factor) and there is a possibility of Rh sensitization, that is, an increased sensitivity of the body to the effects of various factors.