Babies skull bones
Cranial sutures Information | Mount Sinai
Fontanelles; Sutures - cranial
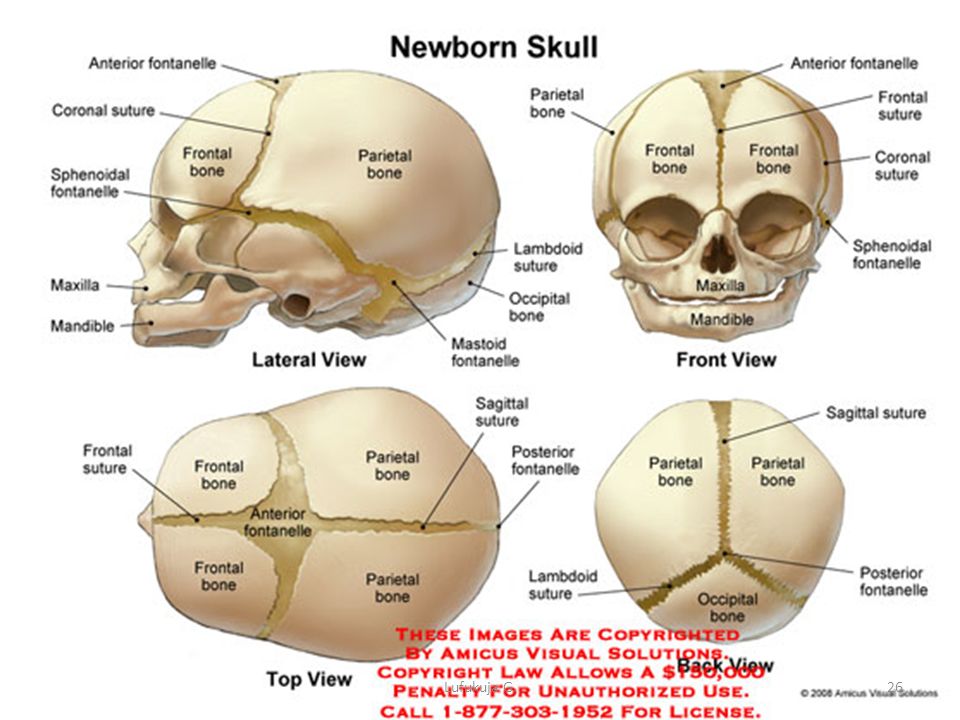
Cranial sutures are fibrous bands of tissue that connect the bones of the skull.
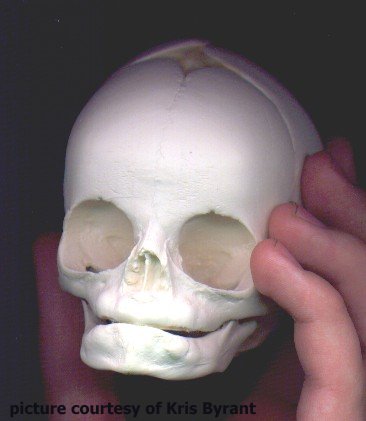
The sutures or anatomical lines where the bony plates of the skull join together can be easily felt in the newborn infant. The diamond shaped space on the top of the skull and the smaller space further to the back are often referred to as the soft spot in young infants.
Fontanelles are the soft spots on an infant's head where the bony plates that make up the skull have not yet come together. It is normal for infants to have these soft spots, which can be seen and felt on the top and back of the head. Fontanelles that are abnormally large may indicate a medical condition.
Information
An infant's skull is made up of 6 separate cranial (skull) bones:
- Frontal bone
- Occipital bone
- Two parietal bones
- Two temporal bones
These bones are held together by strong, fibrous, elastic tissues called sutures.
The spaces between the bones that remain open in babies and young children are called fontanelles. Sometimes, they are called soft spots. These spaces are a part of normal development. The cranial bones remain separate for about 12 to 18 months. They then grow together as part of normal growth. They stay connected throughout adulthood.
Two fontanelles usually are present on a newborn's skull:
- On the top of the middle head, just forward of center (anterior fontanelle)
- In the back of the middle of the head (posterior fontanelle)
The posterior fontanelle usually closes by age 1 or 2 months.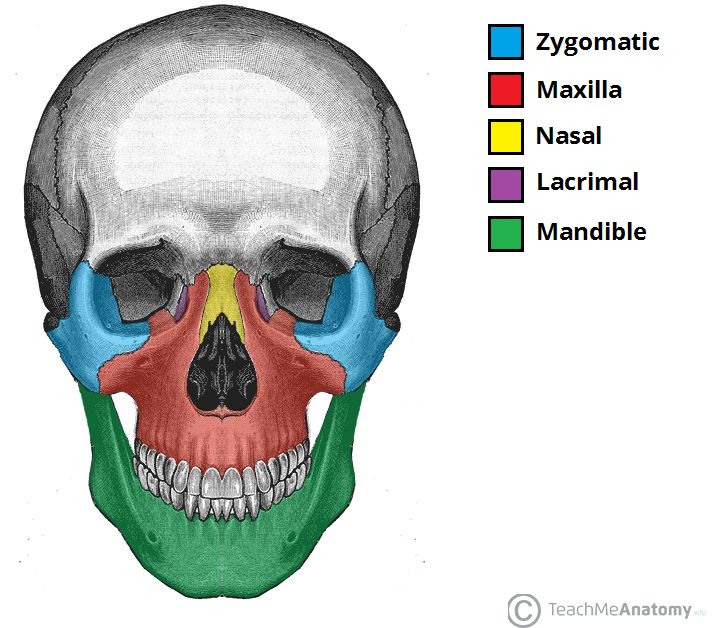 It may already be closed at birth.
It may already be closed at birth.
The anterior fontanelle usually closes sometime between 9 months and 18 months.
The sutures and fontanelles are needed for the infant's brain growth and development. During childbirth, the flexibility of the sutures allows the bones to overlap so the baby's head can pass through the birth canal without pressing on and damaging their brain.
During infancy and childhood, the sutures are flexible. This allows the brain to grow quickly and protects the brain from minor impacts to the head (such as when the infant is learning to hold his head up, roll over, and sit up). Without flexible sutures and fontanelles, the child's brain could not grow enough. The child would develop brain damage.
Feeling the cranial sutures and fontanelles is one way that health care providers follow the child's growth and development. They are able to assess the pressure inside the brain by feeling the tension of the fontanelles. The fontanelles should feel flat and firm. Bulging fontanelles may be a sign of increased pressure within the brain. In this case, providers may need to use imaging techniques to see the brain structure, such as CT scan or MRI scan. Surgery may be needed to relieve the increased pressure.
Bulging fontanelles may be a sign of increased pressure within the brain. In this case, providers may need to use imaging techniques to see the brain structure, such as CT scan or MRI scan. Surgery may be needed to relieve the increased pressure.
Sunken, depressed fontanelles are sometimes a sign of dehydration.
Goyal NK. The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Varma R, Williams SD. Neurology. In: Zitelli BJ, McIntire SC, Nowalk AJ, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 16.
Last reviewed on: 2/2/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA.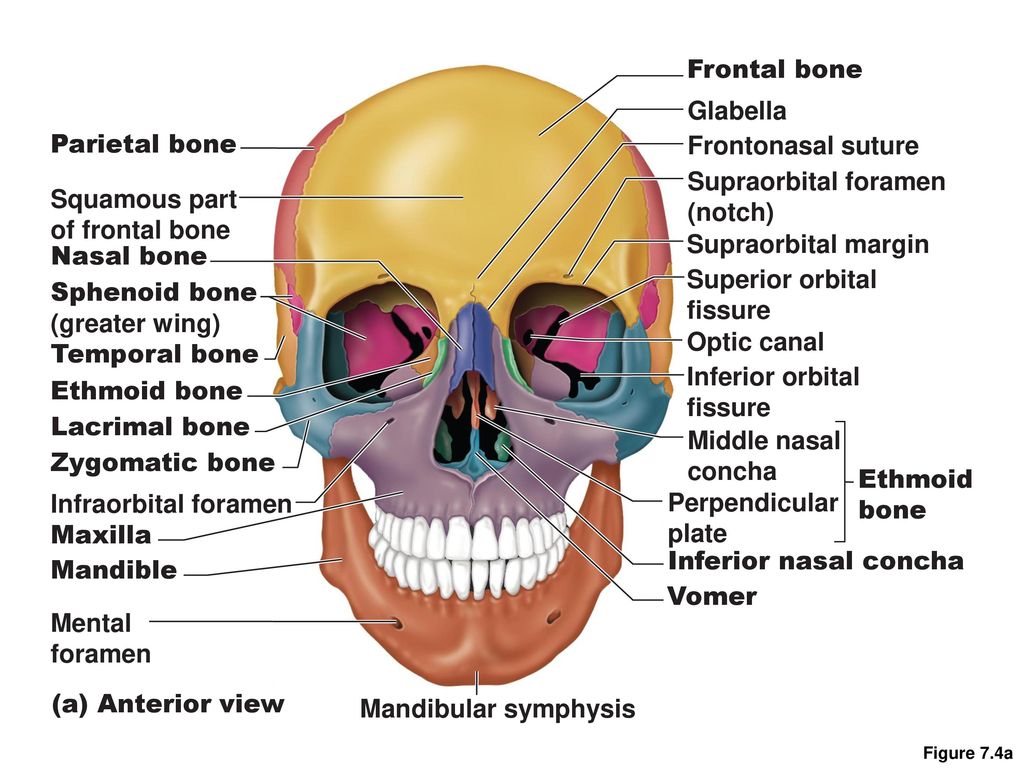 Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Facts about Craniosynostosis | CDC
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen.
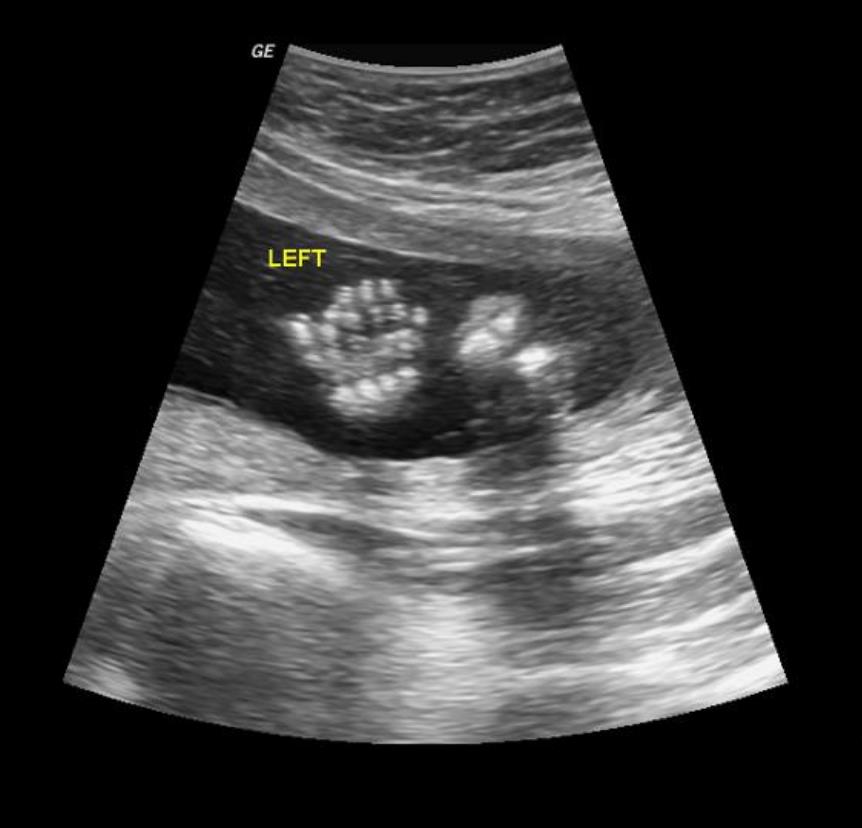
Click here to view a larger image
Click here to view a larger image
What is Craniosynostosis?
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen. The spaces between a typical baby’s skull bones are filled with flexible material and called sutures. These sutures allow the skull to grow as the baby’s brain grows. Around two years of age, a child’s skull bones begin to join together because the sutures become bone. When this occurs, the suture is said to “close.” In a baby with craniosynostosis, one or more of the sutures closes too early. This can limit or slow the growth of the baby’s brain.
When this occurs, the suture is said to “close.” In a baby with craniosynostosis, one or more of the sutures closes too early. This can limit or slow the growth of the baby’s brain.
When a suture closes and the skull bones join together too soon, the baby’s head will stop growing in only that part of the skull. In the other parts of the skull where the sutures have not joined together, the baby’s head will continue to grow. When that happens, the skull will have an abnormal shape, although the brain inside the skull has grown to its usual size. Sometimes, though, more than one suture closes too early. In these instances, the brain might not have enough room to grow to its usual size. This can lead to a build-up of pressure inside the skull.
Types of Craniosynostosis
The types of craniosynostosis depend on what sutures join together early.
- Sagittal synostosis– The sagittal suture runs along the top of the head, from the baby’s soft spot near the front of the head to the back of the head.
 When this suture closes too early, the baby’s head will grow long and narrow (scaphocephaly). It is the most common type of craniosynostosis.
When this suture closes too early, the baby’s head will grow long and narrow (scaphocephaly). It is the most common type of craniosynostosis. - Coronal synostosis – The right and left coronal sutures run from each ear to the sagittal suture at the top of the head. When one of these sutures closes too early, the baby may have a flattened forehead on the side of the skull that closed early (anterior plagiocephaly). The baby’s eye socket on that side might also be raised up and his or her nose could be pulled toward that side. This is the second most common type of craniosynostosis.
- Bicoronal synostosis – This type of craniosynostosis occurs when the coronal sutures on both sides of the baby’s head close too early. In this case, the baby’s head will grow broad and short (brachycephaly).
- Lambdoid synostosis – The lambdoid suture runs along the backside of the head. If this suture closes too early, the baby’s head may be flattened on the back side (posterior plagiocephaly).
 This is one of the rarest types of craniosynostosis.
This is one of the rarest types of craniosynostosis. - Metopic synostosis – The metopic suture runs from the baby’s nose to the sagittal suture at the top of the head. If this suture closes too early, the top of the baby’s head shape may look triangular, meaning narrow in the front and broad in the back (trigonocephaly). This is one of the rarest types of craniosynostosis.
Other Problems
Many of the problems a baby can have depend on:
- Which sutures closed early
- When the sutures closed (was it before or after birth and at what age)
- Whether or not the brain has room to grow
Sometimes, if the condition is not treated, the build-up of pressure in the baby’s skull can lead to problems, such as blindness, seizures, or brain damage.
How Many Babies are Born with Craniosynostosis?
Researchers estimate that about 1 in every 2,500 babies is born with craniosynostosis in the United States.1
Causes and Risk Factors
The causes of craniosynostosis in most infants are unknown. Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
CDC, like the many families of children with birth defects, wants to find out what causes these conditions. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011), to understand the causes of and risks for birth defects, such as craniosynostosis.
Recently, CDC reported on important findings from research studies about some factors that increase the chance of having a baby with craniosynostosis:
- Maternal thyroid disease ― Women with thyroid disease or who are treated for thyroid disease while they are pregnant have a higher chance of having an infant with craniosynostosis, compared to women who don’t have thyroid disease.
 2
2 - Certain medications ― Women who report using clomiphene citrate (a fertility medication) just before or early in pregnancy are more likely to have a baby with craniosynostosis, compared to women who didn’t take this medicine.3
CDC continues to study birth defects, such as craniosynostosis, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Craniosynostosis usually is diagnosed soon after a baby is born. Sometimes, it is diagnosed later in life.
Usually, the first sign of craniosynostosis is an abnormally shaped skull. Other signs may include:
- No “soft spot” on the baby’s skull
- A raised firm edge where the sutures closed early
- Slow growth or no growth in the baby’s head size over time
Doctors can identify craniosynostosis during a physical exam. A doctor will feel the baby’s head for hard edges along the sutures and unusual soft spots.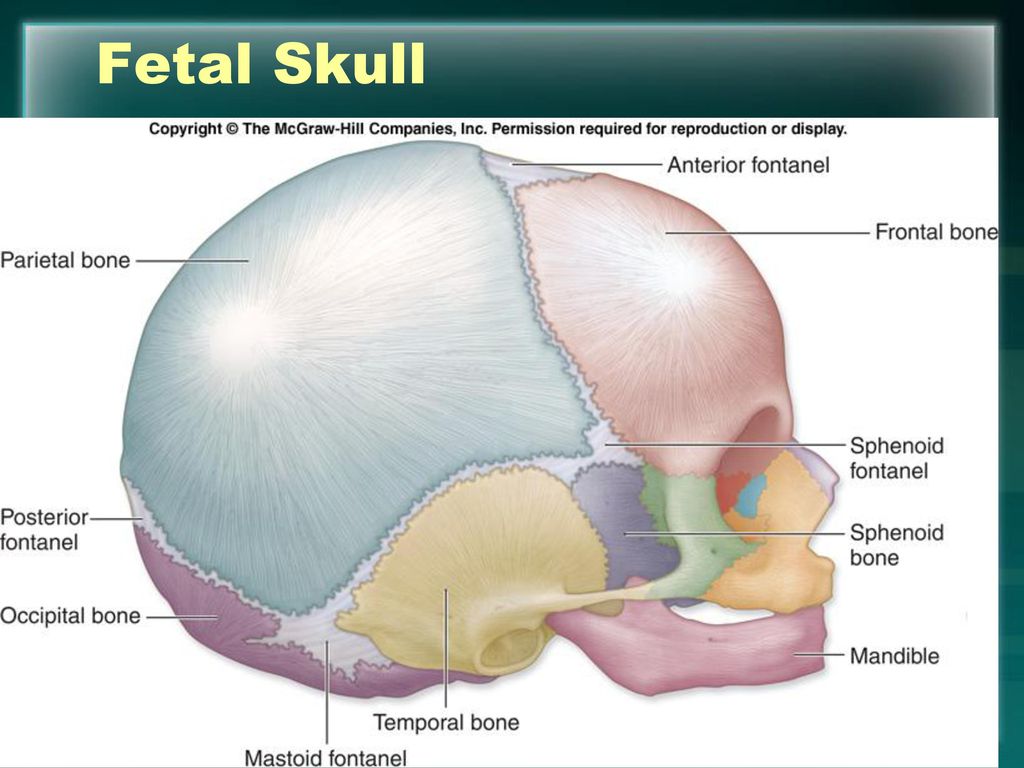 The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
Treatments
Many types of craniosynostosis require surgery. The surgical procedure is meant to relieve pressure on the brain, correct the craniosynostosis, and allow the brain to grow properly. When needed, a surgical procedure is usually performed during the first year of life. But, the timing of surgery depends on which sutures are closed and whether the baby has one of the genetic syndromes that can cause craniosynostosis.
Babies with very mild craniosynostosis might not need surgery. As the baby gets older and grows hair, the shape of the skull can become less noticeable. Sometimes, special medical helmets can be used to help mold the baby’s skull into a more regular shape.
Each baby born with craniosynostosis is different, and the condition can range from mild to severe. Most babies with craniosynostosis are otherwise healthy. Some children, however, have developmental delays or intellectual disabilities, because either the craniosynostosis has kept the baby’s brain from growing and working normally, or because the baby has a genetic syndrome that caused both craniosynostosis and problems with how the brain works. A baby with craniosynostosis will need to see a healthcare provider regularly to make sure that the brain and skull are developing properly. Babies with craniosynostosis can often benefit from early intervention services to help with any developmental delays or intellectual problems. Some children with craniosynostosis may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups also can be useful for new families of babies with birth defects of the head and face, including craniosynostosis.
Other Resources
The views of these organizations are their own and do not reflect the official position of CDC.
- Children’s Craniofacial Association (CCA)
CCA addresses the medical, financial, psychosocial, emotional, and educational concerns relating to craniofacial conditions. - The National Craniofacial Association (FACES)
FACES is dedicated to assisting children and adults who have craniofacial disorders resulting from disease, accident, or birth.
References
- Boulet SL, Rasmussen SA, Honein MA. A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet Part A. 2008;146A:984–991.
- Rasmussen SA, Yazdy MM, Carmichael SL, Jamieson DJ, Canfield MA, Honein MA. Maternal thyroid disease as a risk factor for craniosynostosis. Obstet Gynecol. 2007;110:369-377.
- Reefhuis J, Honein MA, Schieve LA, Rasmussen SA, and the National Birth Defects Prevention Study. Use of clomiphene citrate and birth defects, National Birth Defects Prevention Study, 1997–2005.
 Hum Reprod. 2011;26:451–457.
Hum Reprod. 2011;26:451–457.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
Skull of a newborn and age features of the structure of the skull : Farmf
Skull of a newborn and age features of the structure of the skull
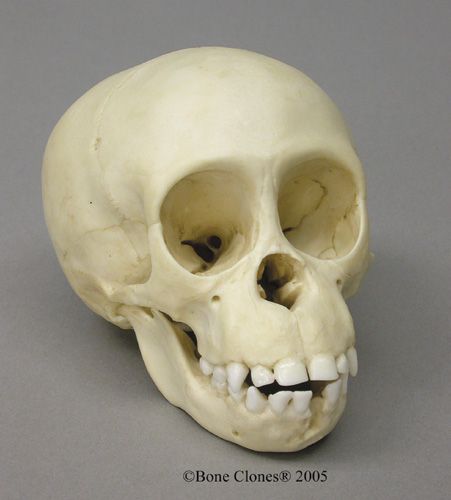
Chapter 2. Musculoskeletal system , two lateral and scales. Their fusion begins in the second year of life. Fusion of the basilar part with the lateral parts begins at 3–4 years and ends at 6–10 years. Sphenoid bone at the time of birth consists of the body and small wings, large wings, lateral and medial plates of the pterygoid process, which grow together during the 3rd–8th years of life. In a newborn, the sphenoid sinus is a small cavity in the body of the sphenoid bone, which reaches the size of an adult sinus at 11–15 years of age. The temporal bone of a newborn child consists of three parts: squamous, tympanic and stony. The fusion of parts of the temporal bone ends by the age of 13–14. The mandibular fossa in a newborn child is smoothed out, it is finally formed only at the age of 6 years. The articular tubercle appears at the age of 7-8 months. nine0005 The frontal bone of a newborn consists of two halves connected by a frontal suture (metopic). This seam overgrows at the age of 7-8. The frontal sinus by the end of the fourth year becomes the size of a pea, at 12-14 years old it reaches its final size. The lower jaw at the time of birth consists of two halves connected by fibrous tissue. Their fusion begins in the third month after birth and ends at 2 years of age. In newborns of the first year of life, the angle of the lower jaw is obtuse (140–150°). In adulthood, the dimensions of the angle approach a straight line. In the elderly and senile age, the angle increases. Fusion of parts of the hyoid bone into a single bone occurs at the age of 25–30 years. nine0005 In a newborn, there are no seams between the bones, the spaces are filled with connective tissue. In areas where several bones converge, there are six fontanelles covered with connective tissue plates: two unpaired (anterior and posterior) and two paired (sphenoid and mastoid). The largest - the anterior, or frontal, fontanel has a diamond shape (Fig. 82). It is located between the frontal scales and the parietal bones. Fig. 82. Skull of a newborn, side view (A) and top (B): 1 - anterior fontanel; 2 - wedge-shaped fontanel; 3 - a large wing of the sphenoid bone; 4 - frontal tubercle; 5 - nasal bone; 6 - lacrimal bone; 7 - zygomatic bone; 8 - maxillary bone; 9 - lower jaw; 10 - tympanic ring of the temporal bone; 11 - scaly part of the temporal bone; 12 - lateral part of the occipital bone; 13 - mastoid fontanel; 14 - occipital scales; 15 - posterior fontanelle; 16 - parietal tubercle; 17 - frontal seam The volume of the brain cavity of a newborn is on average 350–375 cm 3 . After birth, the growth of the skull is uneven. In postnatal ontogenesis, three periods of growth and development of the skull are distinguished. 1. Period of vigorous active growth – from birth to seven years. During the first year of life, the skull grows more or less evenly. From one to three years, the skull grows especially actively at the back, this is due to the transition of the child to upright posture. At the 2nd or 3rd year of life, due to the eruption of milk teeth and the strengthening of the function of the masticatory muscles, the growth of the facial part of the skull increases. From three to seven years, the growth of the entire skull continues, especially its base. By the age of seven, the base of the skull is almost as long as that of an adult. nine0005 2. Period of slow growth - from 7 to 12-13 years (beginning of puberty). 3. In the third period - after 13 years - both the brain and facial parts of the skull actively grow. Sexual features of the skull are manifested. If, before puberty, the faces of boys and girls are rounded, then after the onset of puberty, in men, the face, as a rule, is extended in length, in women, roundness remains. The male skull, due to the large overall body size, is larger than the female one. The male skull is distinguished by a more pronounced relief due to the stronger development of the muscles attached to it; in women, the relief of the skull is smoothed. nine0005 Overgrowth of the sutures in the skull begins at the age of 20-30 years, and in men somewhat earlier than in women. The scaly seam, as a rule, does not overgrow. We continue the series of publications on neurosurgical diseases. The first written references to the deformation of the skull are found in ancient authors. In the V-IV centuries. BC e. Hippocrates in the text "On Air, Waters and Localities" described the people of the long-headed, or macrocephalians, living on the eastern coast of the Black Sea. Their heads stretched upwards were a sign of their belonging to the elite. However, from the text it becomes clear that the macrocephals themselves voluntarily deformed the skulls of their babies. “They consider the most noble those who have the longest heads. . However, modern parents often face congenital, unintentional deformity of the skull. And she, unfortunately, does not make their children a sign of belonging to the elite, rather the opposite... The word "craniostenosis" comes from the Greek. cranio - "skull" and stenosis - "bone fusion". As the Association of Neurosurgeons of Russia has recognized, craniosynostosis (or craniostenosis) is “a disease manifested by congenital absence or premature closure of the sutures of the skull. Premature synostosis in the area of the sutures of the skull leads to a limitation of the growth of the skull in the area of the closed suture, resulting in the development of cranio-cerebral disproportion. The clinical manifestation of cranio-cerebral disproportion is the syndrome of intracranial hypertension. The skull of a newborn consists of five main bones: a pair of frontals, a pair of parietals and one occipital. These bones are connected by fibrous sutures, which allow the bones to move relative to each other, which facilitates the process of childbirth and brain growth. Normally, the coronal (coronary) suture separates the two frontal bones from the parietal bones. The metopic suture separates the frontal bones. The sagittal suture separates the two parietal bones. The lambdoid suture separates the occipital bone from the two parietal bones. nine0005 But sometimes things go wrong... Genetic mutations, which can be localized in one area or have a systemic, widespread lesion, cause sutures to close prematurely. If the closure of one or another suture is accompanied by other anomalies, such craniostenosis is called "syndromic". Syndromes characterized by premature closure of the cranial sutures: Crouzon Syndrome, Apert Syndrome, Pfeiffer Syndrome, Satpre-Hotzen Syndrome, Carpenter Syndrome and others. Craniostenosis can be part of various hereditary syndromes. But in most cases, the hereditary nature of the disease is not confirmed, and craniostenosis does not appear in the next generations. An unusually strong degree of craniostenosis (a type of scaphocephaly) was present in the so-called "Stettin weaver" (Bonnet-Bonnet, 1904). He was a worker in one of the weaving mills in Stettin. His skull was so long and narrow that the back of his head rested on his back when the unfortunate man tried to raise his head. It was said about the "Stettin weaver" that he never saw the sky and always looked gloomily at the ground. Persecuted for his deformity by ridicule, he died of pleurisy in the 38th year of his sad life ... Sometimes not one, but several seams are exposed to early overgrowth. It also leads to skull deformity. In those cases when such sutures as the coronal and sagittal sutures are prematurely closed, the small dimensions of the upper part of the child's skull seem to be fixed and their increase stops. Hydrocephalus is not a sentence! It is quite difficult to detect craniostenosis in utero. But there is a chance that a standard fetal ultrasound (third trimester) of pregnancy may reveal a head deformity, especially if a 3D ultrasound scan is performed. The deformation of the skull in the fetus and the suspicion of craniostenosis may be an indication for a caesarean section in order to avoid injury to the birth canal of the mother and child. After all, with craniostenosis, the bones will not be able to form in the right way during childbirth. nine0005 How to detect craniostenosis in a newborn? Alexander Vladimirovich Sakharov, a neurosurgeon at the National Medical Research Center for Neurosurgery named after academician N. – First of all, you need to pay attention to any changes in the shape of the skull. An elongated skull, a sloping forehead or occiput, a ridge in the forehead, flattening of the child's head in the anterior-posterior direction, the presence of a bone ridge behind a large fontanel over a fused sagittal suture, close or vice versa, wide-set or asymmetrically located eyes, protrusion of the eye from the orbits, symmetry of the ears. Also, a large fontanel may close early, or vice versa, remaining open at an older age (with syndromic forms). Normally, a large fontanel in an infant closes up to a year, even up to a year and a half. If the fontanel closed much earlier, or, moreover, the baby was born with a closed fontanel, contact a neurosurgeon for advice. nine0005 – Is craniostenosis always associated with an abnormal development of the brain itself? - Not at all necessary. Yes, it happens that we meet with microcephaly - a primary anomaly of the brain, in which the skull does not grow, since the brain does not develop. – At what age are such surgeries performed? - It depends on the type of craniostenosis. For scaphocephaly, the optimal age for surgery is up to 6 months. In this case, endoscopic surgery can be performed. If the parents turned to us later than this period, then it is no longer an endoscopic, but a conventional reconstructive surgery. It is usually carried out before the age of 1 year 2 months - 1 year 5 months. At an older age, the operation is performed only if clinical symptoms of hypertension (high blood pressure) appear: headaches, nausea, vomiting. If a child was not diagnosed with craniostenosis in time, but a deformity was discovered, for example, at the age of 3 years, operations are usually not performed. The brain has already formed in adverse conditions, and it is more difficult to get a good cosmetic result of a change in the shape of the skull. – What does a neurosurgeon do during an operation? – In scaphocephaly, for example, the surgeon endoscopically cuts the bone in the area of the synostotic sagittal suture and makes “notches” on the sides of the parietal bones so that the parietal bones can diverge. If the child wears a special helmet after the operation, then the normal skull will form earlier. The anteroposterior size of the skull will be limited in growth by the helmet, and the parietal bones will be able to diverge to the sides. In other forms of craniostenosis, a different tactic is used. For example, in trigonocephaly (a ridge in the forehead, a triangular shape of the skull), the frontal bone is reconstructed, the distance between the eyes increases (with trigonocephaly it is narrowed), and the frontal region is advanced. – Are surgical interventions indicated in all cases of early diagnosis? – Craniostenosis is a rather rare pathology. Much more often we meet with positional deformity of the skull. This is the scourge of our times. Parents now have many car seat-type restraints at their disposal. And they often and for a long time leave the child lying in one position in them. Or, say, a child lies in a crib and looks all the time towards a working TV. This is convenient for mom, he requires less of her attention. But the longer he lies, the more the back of his head flattens on one side. This problem does not require surgery. But it is important to diagnose it in time and start changing the position of the child. Or apply the same cranial orthosis (helmet) to avoid negative consequences. nine0005 – If we rule out a brain anomaly and perform an operation for craniostenosis in time, can we hope that the child will develop fully? - Yes. – How old are your first patients with craniostenosis that you operated on? – 20 years… Elena from Yaroslavl is the mother of eleven children, Varya is the eighth daughter. When Varyukha was born, the doctors told her parents that she would live for a maximum of six months. And it will live like a plant. Microcephaly. Severe brain pathology. Parents could not accept this test and refused it. Three months later, Lena and Vadim Burov saw Varya's photo in the Federal Base. “In custody, they told us that we were crazy. At that time, in addition to our three own children, we had four adopted children. The repeated commission questioned my husband and me for forty minutes, trying to understand our motives. I will say more. When we arrived at the orphanage, and saw her not in the photograph, but in reality, I myself was frightened. Will we make it? Varyusha had a triangular head. She herself was in a very strong tension, did not allow herself to be hugged or pressed. Bound, she held her hands in front of her, her eyes were bulging, frightened, like those of a wolf cub. “She's like this all the time: in a high tone, she doesn't smile, she doesn't coo... There are no emotions, nothing,” the employees told us. Well, we think we’ll figure it out ... On the second day of our acquaintance, she was already smiling at us from the top of her head, her hands lowered, as if she realized that we were taking her. At home, after a week and a half, she began to hum ... Development began. nine0005 At the age of 9 months, Varia's pictures, thanks to the charitable foundations "Road of Life" and "He Needs You", came to Moscow, to the Scientific Research Clinical Institute of Pediatrics named after academician Yu. And we went to the first operation to Dmitry Yuryevich Zinenko. It turned out that despite microcephaly, Varya's brain continued to grow. He is still growing. And the seams on the skull overgrown ahead of time. Craniostenosis was confirmed. That kind of it, in which the sagittal suture overgrows. Scaphocephaly. nine0005 Varya had an incision from her forehead to the back of her head, and an artificial fontanel was made. A day later, she began to stand and took her first steps. No support. The brain was nourished - and there was a powerful leap in development. She began to crawl, in the same place, in the department. All the staff gathered to look at this miracle. Started to babble. But three months passed, and a keel formed on her forehead. Like a rooster's comb. We went back to the Institute named after Yu. The condition began to deteriorate. Varya stood all the time, resting her head on the pillow, sleeping only in the fetal position. I cried constantly at night. It was evident that her head was very worried. So the brain has grown. A few months later she underwent a second operation. Cut from ear to ear. As Dmitry Yuryevich Zinenko, who again performed the operation on Varya, later said, the brain straightened out during the operation literally before our eyes. Varya began to sleep peacefully, learned to speak in short words. It was obvious that she felt better. Despite predictions and microcephaly, her head continues to grow. From the moment of birth to the present day, Varina's head has grown by 13 cm. This is a very good result. In a healthy child, the head grows by 10 cm during the first year of life. But for some reason, the bones do not allow the brain to grow, they quickly grow together. A year and a half later, Varya began to deteriorate again. She became lethargic, refused to eat ... They did a CT scan, sent her to the Veltishchev Institute, and received the answer: “The brain is compressed. Surgery will be required." Dmitry Zinenko operated again for the third time. He said: “If I hadn’t operated on myself last time, I wouldn’t have believed it ...” I must say that Dmitry Yuryevich is the only doctor who did not refuse us. He just saves Varka. Every time. We were denied in all known clinics. The brain is growing, and no one believes that it is growing. nine0005 A month after the operation, Varya experienced a developmental leap again - she began to pronounce many words at once. The brain receives nourishment - oxygen, and the child develops. Now she is going to kindergarten. At this point, of course, she has developmental delay. But if you remember that she was given half a year of her life at the most… Cysts in the head: real and imaginary She is very mobile, loves to dance, says “hello!” to everyone! and “bye!”, and her funniest word is “pomikaka”. Of course we have sleepless nights at times. Sometimes Varya is tormented by bouts of headache. And if nothing hurts, she just wakes up my husband and me, “Dad! Mum!" - and satisfied, she lies down next to us to sleep. I am sure that any child should be given a chance to cope with the disease and stand on their own feet. You can't give up on a child. None." Download the leaflet, it contains a lot of useful information: contacts of doctors, information on treatment, care and rehabilitation. Bystrov A.P. Past, present, future of man. Medgiz, Leningrad branch, 1957, Vorobyeva E A Gubar A V Safyannikova E B – Anatomy and Physiology: Textbook, 1988 Article "Craniosynostosis or premature fusion of the bones of the skull" Article "Craniostenosis" Site materials.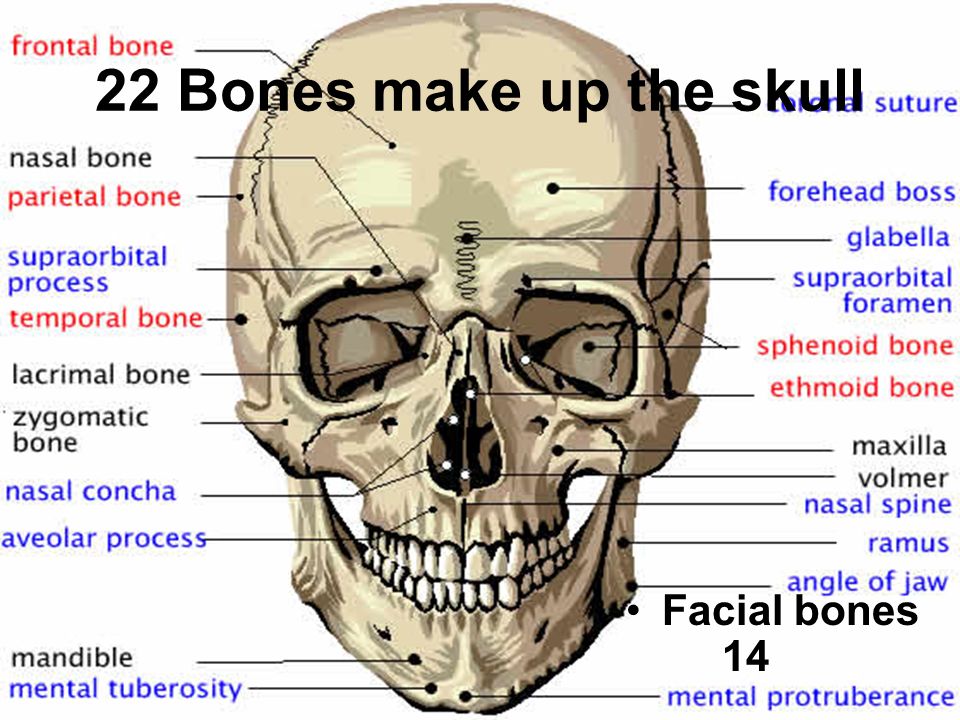 At 16–17 years of age, the occipital bone fuses with the sphenoid bone lying in front of it. nine0005
At 16–17 years of age, the occipital bone fuses with the sphenoid bone lying in front of it. nine0005 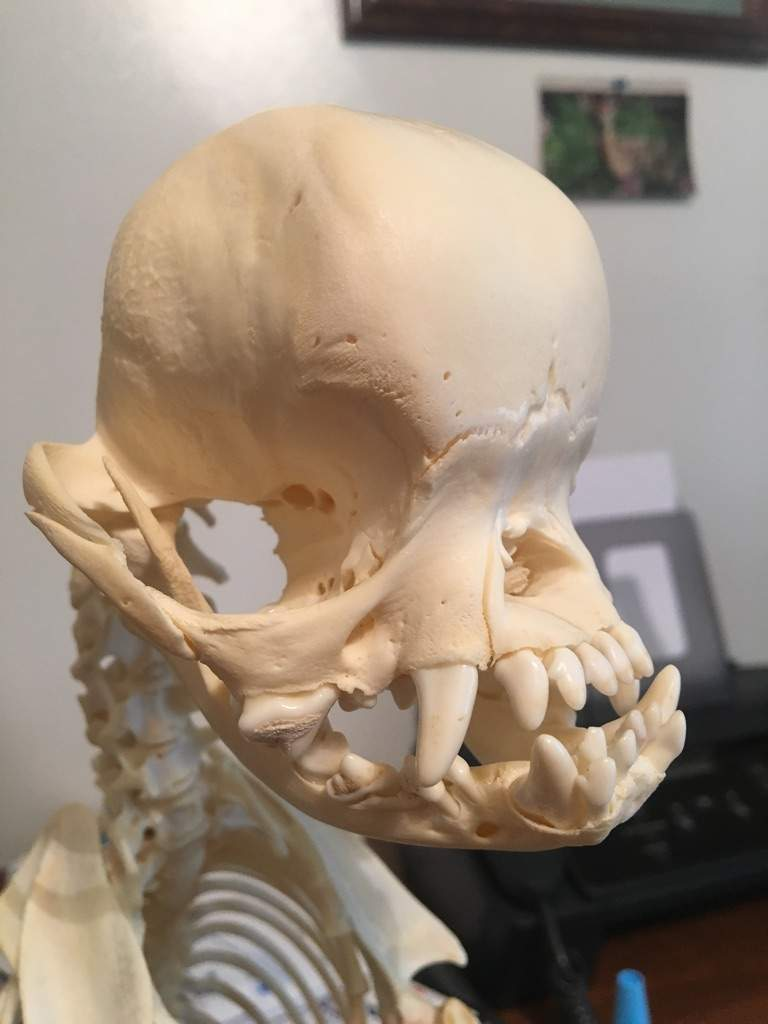 The maxillary sinus in the same bone in a newborn child is poorly developed. Its final irregular rounded shape is formed at the age of 7 years.
The maxillary sinus in the same bone in a newborn child is poorly developed. Its final irregular rounded shape is formed at the age of 7 years.  The posterior, or occipital, fontanelle is located between the posterior edge of the parietal bones and the occipital bone. The sphenoid fontanel is located laterally, between the frontal and parietal bones and the greater wing of the sphenoid bone. The mastoid fontanel is located at the point where the occipital, parietal bones and mastoid process of the temporal bone converge. Due to the presence of fontanelles, the skull of a newborn is very elastic, its shape can change during the passage of the fetal head through the birth canal during childbirth. At the 2-3rd month after birth, the posterior (occipital) and mastoid fontanelles close, by 1.5 years - the anterior one, only by the 3rd year the wedge-shaped fontanel completely disappears. The formation of sutures ends mainly at the 3–5th year of life. nine0005
The posterior, or occipital, fontanelle is located between the posterior edge of the parietal bones and the occipital bone. The sphenoid fontanel is located laterally, between the frontal and parietal bones and the greater wing of the sphenoid bone. The mastoid fontanel is located at the point where the occipital, parietal bones and mastoid process of the temporal bone converge. Due to the presence of fontanelles, the skull of a newborn is very elastic, its shape can change during the passage of the fetal head through the birth canal during childbirth. At the 2-3rd month after birth, the posterior (occipital) and mastoid fontanelles close, by 1.5 years - the anterior one, only by the 3rd year the wedge-shaped fontanel completely disappears. The formation of sutures ends mainly at the 3–5th year of life. nine0005 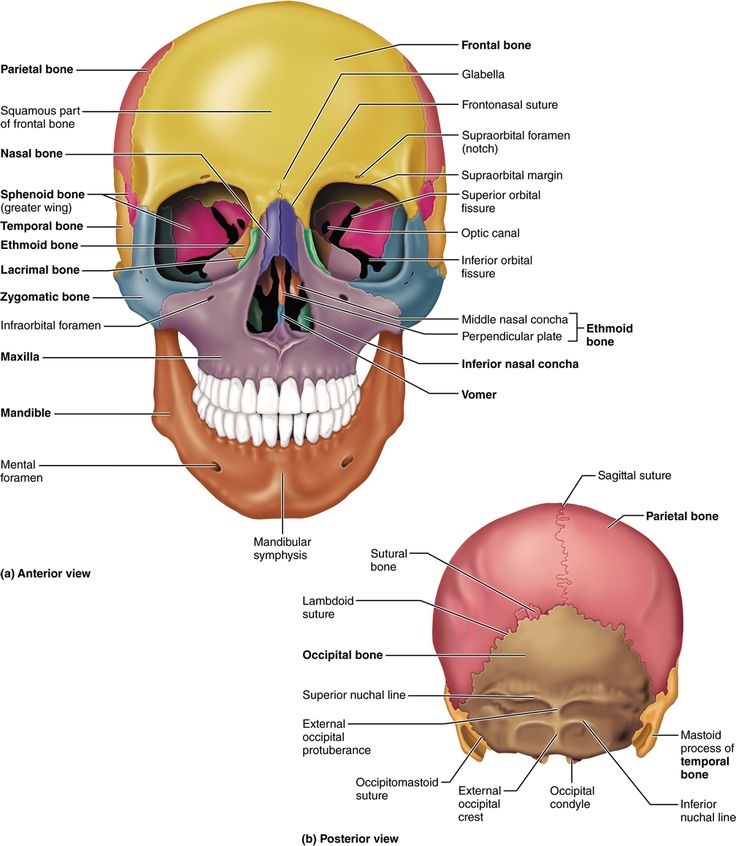 In the first 6 months of a child's life, it doubles, triples by two years, in an adult it is four times more than in a newborn.
In the first 6 months of a child's life, it doubles, triples by two years, in an adult it is four times more than in a newborn.  At this time, mainly the brain part of the skull grows, the volume of its cavity reaches 1200–1300 cm 3 .
At this time, mainly the brain part of the skull grows, the volume of its cavity reaches 1200–1300 cm 3 . Craniostenosis: the skull can be corrected - Mercy.ru
 The project was prepared jointly with the ICPA for helping children with neurosurgical diseases "He needs you." We want these “terrible” diagnoses not to put pressure on parents and take away their hope. In our publications, the best specialists and experienced parents will talk about ways to cure and overcome, give recommendations and show that life can go on with any, even such complex, diseases. nine0005
The project was prepared jointly with the ICPA for helping children with neurosurgical diseases "He needs you." We want these “terrible” diagnoses not to put pressure on parents and take away their hope. In our publications, the best specialists and experienced parents will talk about ways to cure and overcome, give recommendations and show that life can go on with any, even such complex, diseases. nine0005 Others involuntarily
 .. as soon as a child is born, while his bones are still soft, his unhardened head is straightened by hand and forced to grow in length by means of bandages and other suitable devices, as a result of which the spherical shape of the head deteriorates, and its length increases. nine0005
.. as soon as a child is born, while his bones are still soft, his unhardened head is straightened by hand and forced to grow in length by means of bandages and other suitable devices, as a result of which the spherical shape of the head deteriorates, and its length increases. nine0005  nine0005
nine0005 Stitches that allow movement
 nine0005
nine0005  Since the growth of bones in the preserved sutures of the skull continues, the so-called "tower" head appears in an adult. The skull becomes elongated upward and slightly back.
Since the growth of bones in the preserved sutures of the skull continues, the so-called "tower" head appears in an adult. The skull becomes elongated upward and slightly back.
Diagnosis
 N. Burdenko, tells about this:
N. Burdenko, tells about this:  The brain does not grow - there is no impetus for the development of the bones of the skull, the sutures and the fontanel close ahead of time. In such a situation, unfortunately, surgery will not be able to help. But in most cases, on the contrary, prematurely overgrown (for some genetic reason) sutures do not allow the normally formed brain to grow and develop. The surgical operation eliminates its compression and allows further development without any deviations. nine0005
The brain does not grow - there is no impetus for the development of the bones of the skull, the sutures and the fontanel close ahead of time. In such a situation, unfortunately, surgery will not be able to help. But in most cases, on the contrary, prematurely overgrown (for some genetic reason) sutures do not allow the normally formed brain to grow and develop. The surgical operation eliminates its compression and allows further development without any deviations. nine0005  But this is more typical for syndromic cases (that is, a complex anomaly). nine0005
But this is more typical for syndromic cases (that is, a complex anomaly). nine0005 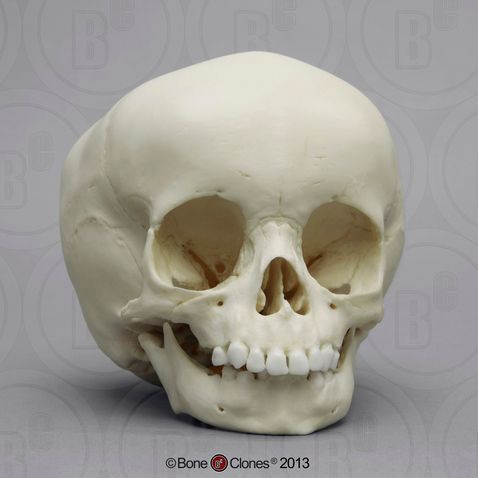 Due to this, the volume of the skull increases, the shape and proportions approach the norm. nine0005
Due to this, the volume of the skull increases, the shape and proportions approach the norm. nine0005 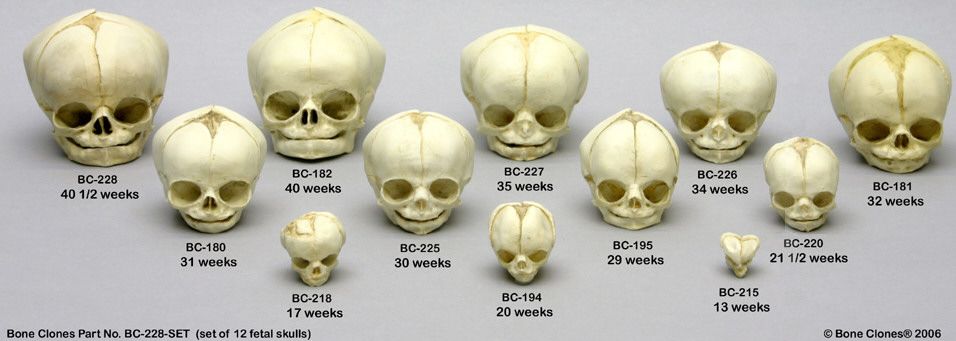 Of course. This is what the operation is for. For craniostenosis, with the exception of syndromic, preventive (preventive) surgery is done to avoid problems that may arise in the future. In the future, we observe such patients for 2-3 years. And then the need just disappears. They don't contact us anymore. nine0005
Of course. This is what the operation is for. For craniostenosis, with the exception of syndromic, preventive (preventive) surgery is done to avoid problems that may arise in the future. In the future, we observe such patients for 2-3 years. And then the need just disappears. They don't contact us anymore. nine0005 Varya and three operations
 Finally, we were allowed to take Varya. Nobody believed in her. Nobody believed we could make it. nine0005
Finally, we were allowed to take Varya. Nobody believed in her. Nobody believed we could make it. nine0005  E. Veltishchev. We got a call from the institute saying: “We looked at your pictures. Varya has severe craniostenosis. Urgently need to go to the operation, the brain is crushed.
E. Veltishchev. We got a call from the institute saying: “We looked at your pictures. Varya has severe craniostenosis. Urgently need to go to the operation, the brain is crushed. 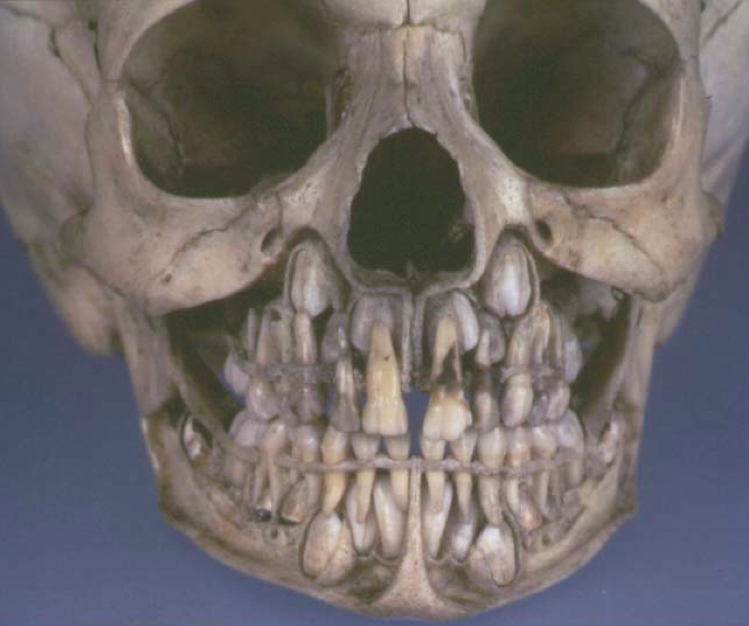 E. Veltishchev, they did a CT scan, it turned out to be trigonocephaly. Another, metopic, suture has grown together. nine0005
E. Veltishchev, they did a CT scan, it turned out to be trigonocephaly. Another, metopic, suture has grown together. nine0005 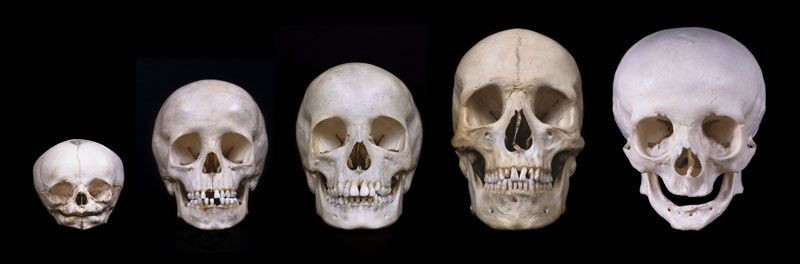 There is probably some genetic reason for this...
There is probably some genetic reason for this...
 It means "tomato". He loves our next adopted daughter, Sonechka with cerebral palsy, very much. He takes pity on her and always gives her hands to help her up. nine0005
It means "tomato". He loves our next adopted daughter, Sonechka with cerebral palsy, very much. He takes pity on her and always gives her hands to help her up. nine0005 Sources: