Premature delivery definition
Premature birth - Symptoms and causes
Overview
A premature birth is a birth that takes place more than three weeks before the baby's estimated due date. In other words, a premature birth is one that occurs before the start of the 37th week of pregnancy.
Premature babies, especially those born very early, often have complicated medical problems. Typically, complications of prematurity vary. But the earlier your baby is born, the higher the risk of complications.
Depending on how early a baby is born, he or she may be:
- Late preterm, born between 34 and 36 completed weeks of pregnancy
- Moderately preterm, born between 32 and 34 weeks of pregnancy
- Very preterm, born at less than 32 weeks of pregnancy
- Extremely preterm, born at or before 25 weeks of pregnancy
Most premature births occur in the late preterm stage.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Your Baby's First Years
Symptoms
Your baby may have very mild symptoms of premature birth, or may have more-obvious complications.
Some signs of prematurity include the following:
- Small size, with a disproportionately large head
- Sharper looking, less rounded features than a full-term baby's features, due to a lack of fat stores
- Fine hair (lanugo) covering much of the body
- Low body temperature, especially immediately after birth in the delivery room, due to a lack of stored body fat
- Labored breathing or respiratory distress
- Lack of reflexes for sucking and swallowing, leading to feeding difficulties
The following tables show the median birth weight, length and head circumference of premature babies at different gestational ages for each sex.
| Weight, length and head circumference by gestational age for boys | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs. , 15 oz. , 15 oz.(3.6 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 8 oz. (2.5 kg) | 18.1 in. (46 cm) | 12.6 in. (32 cm) |
| 32 weeks | 3 lbs., 15.5 oz. (1.8 kg) | 16.5 in. (42 cm) | 11.6 in. (29.5 cm) |
| 28 weeks | 2 lbs., 6.8 oz. (1.1 kg) | 14.4 in. (36.5 cm) | 10.2 in. (26 cm) |
| 24 weeks | 1 lb., 6.9 oz. (0.65 kg) | 12.2 in. (31 cm) | 8.7 in. (22 cm) |
| Weight, length and head circumference by gestational age for girls | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs.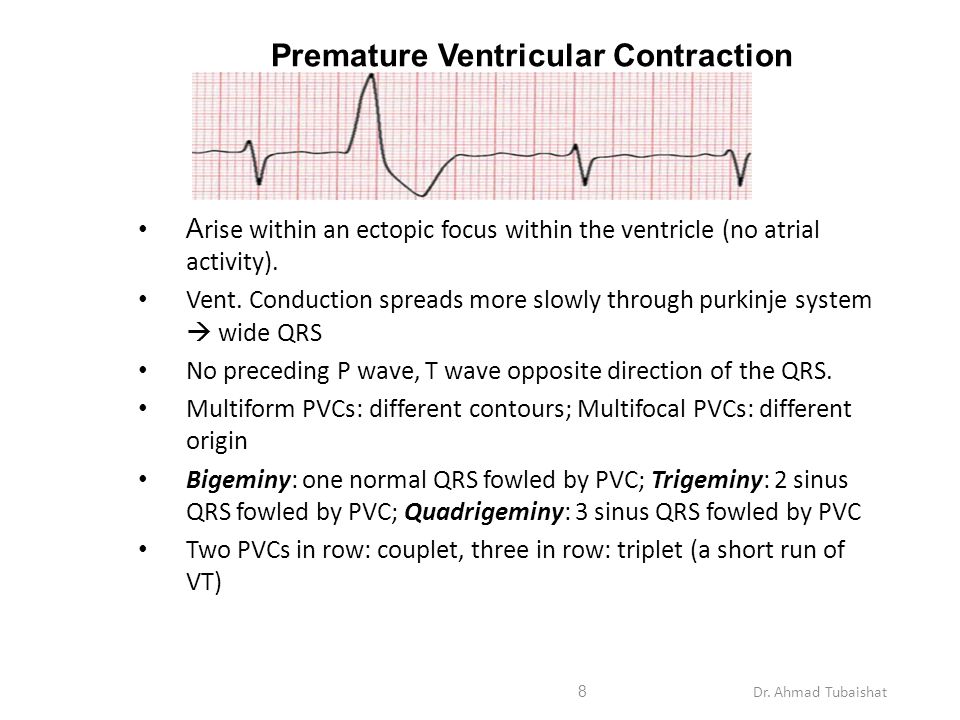 , 7.9 oz. , 7.9 oz.(3.4 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 4.7 oz. (2.4 kg) | 17.7 in. (45 cm) | 12.4 in. (31.5 cm) |
| 32 weeks | 3 lbs., 12 oz. (1.7 kg) | 16.5 in. (42 cm) | 11.4 in. (29 cm) |
| 28 weeks | 2 lbs., 3.3 oz. (1.0 kg) | 14.1 in. (36 cm) | 9.8 in. (25 cm) |
| 24 weeks | 1 lb., 5.2 oz. (0.60 kg) | 12.6 in. (32 cm) | 8.3 in. (21 cm) |
Special care
If you deliver a preterm baby, your baby will likely need a longer hospital stay in a special nursery unit at the hospital. Depending on how much care your baby requires, he or she may be admitted to an intermediate care nursery or the neonatal intensive care unit (NICU). Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Your baby may need extra help feeding, and adapting immediately after delivery. Your health care team can help you understand what is needed and what your baby's care plan will be.
Request an Appointment at Mayo Clinic
Risk factors
Often, the specific cause of premature birth isn't clear. However, there are known risk factors of premature delivery, including:
- Having a previous premature birth
- Pregnancy with twins, triplets or other multiples
- An interval of less than six months between pregnancies
- Conceiving through in vitro fertilization
- Problems with the uterus, cervix or placenta
- Smoking cigarettes or using illicit drugs
- Some infections, particularly of the amniotic fluid and lower genital tract
- Some chronic conditions, such as high blood pressure and diabetes
- Being underweight or overweight before pregnancy
- Stressful life events, such as the death of a loved one or domestic violence
- Multiple miscarriages or abortions
- Physical injury or trauma
For unknown reasons, black women are more likely to experience premature birth than are women of other races. But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
Complications
While not all premature babies experience complications, being born too early can cause short-term and long-term health problems. Generally, the earlier a baby is born, the higher the risk of complications. Birth weight plays an important role, too.
Some problems may be apparent at birth, while others may not develop until later.
Short-term complications
In the first weeks, the complications of premature birth may include:
-
Breathing problems. A premature baby may have trouble breathing due to an immature respiratory system. If the baby's lungs lack surfactant — a substance that allows the lungs to expand — he or she may develop respiratory distress syndrome because the lungs can't expand and contract normally.
Premature babies may also develop a lung disorder known as bronchopulmonary dysplasia.
 In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea.
In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea. - Heart problems. The most common heart problems premature babies experience are patent ductus arteriosus (PDA) and low blood pressure (hypotension). PDA is a persistent opening between the aorta and pulmonary artery. While this heart defect often closes on its own, left untreated it can lead to a heart murmur, heart failure as well as other complications. Low blood pressure may require adjustments in intravenous fluids, medicines and sometimes blood transfusions.
- Brain problems. The earlier a baby is born, the greater the risk of bleeding in the brain, known as an intraventricular hemorrhage. Most hemorrhages are mild and resolve with little short-term impact. But some babies may have larger brain bleeding that causes permanent brain injury.
-
Temperature control problems.
 Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.
Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.Hypothermia in a premature baby can lead to breathing problems and low blood sugar levels. In addition, a premature infant may use up all of the energy gained from feedings just to stay warm. That's why smaller premature infants require additional heat from a warmer or an incubator until they're larger and able to maintain body temperature without assistance.
- Gastrointestinal problems. Premature infants are more likely to have immature gastrointestinal systems, resulting in complications such as necrotizing enterocolitis (NEC). This potentially serious condition, in which the cells lining the bowel wall are injured, can occur in premature babies after they start feeding.
 Premature babies who receive only breast milk have a much lower risk of developing NEC.
Premature babies who receive only breast milk have a much lower risk of developing NEC. -
Blood problems. Premature babies are at risk of blood problems such as anemia and newborn jaundice. Anemia is a common condition in which the body doesn't have enough red blood cells. While all newborns experience a slow drop in red blood cell count during the first months of life, the decrease may be greater in premature babies.
Newborn jaundice is a yellow discoloration in a baby's skin and eyes that occurs because the baby's blood contains excess bilirubin, a yellow-colored substance, from the liver or red blood cells. While there are many causes of jaundice, it is more common in preterm babies.
- Metabolism problems. Premature babies often have problems with their metabolism. Some premature babies may develop an abnormally low level of blood sugar (hypoglycemia). This can happen because premature infants typically have smaller stores of stored glucose than do full-term babies.
 Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose.
Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose. - Immune system problems. An underdeveloped immune system, common in premature babies, can lead to a higher risk of infection. Infection in a premature baby can quickly spread to the bloodstream, causing sepsis, an infection that spreads to the bloodstream.
Long-term complications
In the long term, premature birth may lead to the following complications:
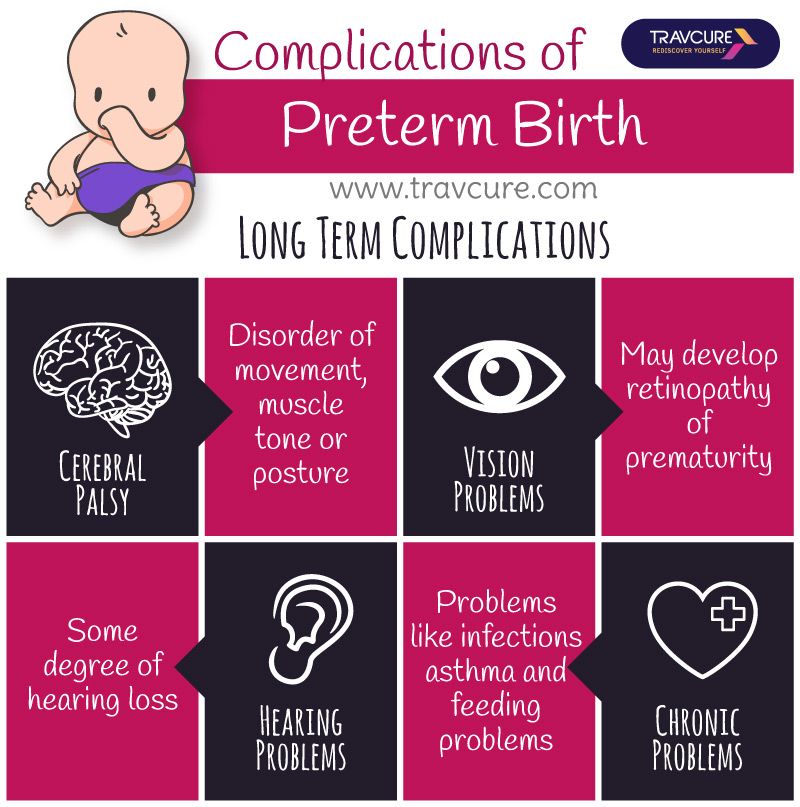
- Cerebral palsy. Cerebral palsy is a disorder of movement, muscle tone or posture that can be caused by infection, inadequate blood flow or injury to a newborn's developing brain either early during pregnancy or while the baby is still young and immature.
- Impaired learning. Premature babies are more likely to lag behind their full-term counterparts on various developmental milestones. Upon school age, a child who was born prematurely might be more likely to have learning disabilities.
- Vision problems. Premature infants may develop retinopathy of prematurity, a disease that occurs when blood vessels swell and overgrow in the light-sensitive layer of nerves at the back of the eye (retina). Sometimes the abnormal retinal vessels gradually scar the retina, pulling it out of position. When the retina is pulled away from the back of the eye, it's called retinal detachment, a condition that, if undetected, can impair vision and cause blindness.
- Hearing problems. Premature babies are at increased risk of some degree of hearing loss. All babies will have their hearing checked before going home.
- Dental problems. Premature infants who have been critically ill are at increased risk of developing dental problems, such as delayed tooth eruption, tooth discoloration and improperly aligned teeth.
- Behavioral and psychological problems. Children who experienced premature birth may be more likely than full-term infants to have certain behavioral or psychological problems, as well as developmental delays.

- Chronic health issues. Premature babies are more likely to have chronic health issues — some of which may require hospital care — than are full-term infants. Infections, asthma and feeding problems are more likely to develop or persist. Premature infants are also at increased risk of sudden infant death syndrome (SIDS).
Prevention
Although the exact cause of preterm birth is often unknown, there are some things that can be done to help women — especially those who have an increased risk — to reduce their risk of preterm birth, including:
- Progesterone supplements. Women who have a history of preterm birth, a short cervix or both factors may be able to reduce the risk of preterm birth with progesterone supplementation.
-
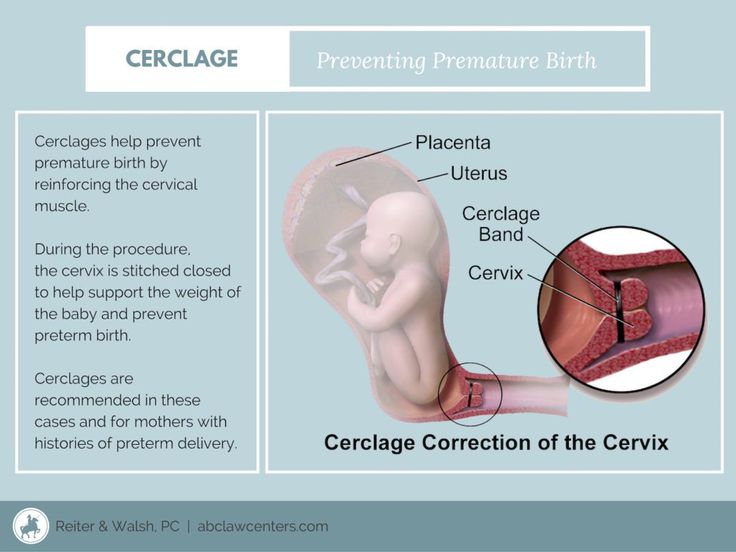
Cervical cerclage. This is a surgical procedure performed during pregnancy in women with a short cervix, or a history of cervical shortening that resulted in a preterm birth.

During this procedure, the cervix is stitched closed with strong sutures that may provide extra support to the uterus. The sutures are removed when it's time to deliver the baby. Ask your doctor if you need to avoid vigorous activity during the remainder of your pregnancy.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Preterm labor and premature birth: Are you at risk?
Preterm labor and premature birth happen too early, before 37 weeks of pregnancy.
Babies born prematurely are more likely to have health problems than babies born on time.
Learn the signs and symptoms of preterm labor so you can get help quickly if they happen to you.
We don’t always know what causes preterm labor and premature birth. We do know certain risk factors may make you more likely to give birth early.
Talk to your provider about what you can do to help reduce your risk for preterm labor and premature birth.

What are preterm labor and premature birth?
Preterm and premature mean the same thing — early. Preterm labor is labor that begins early, before 37 weeks of pregnancy. Labor is the process your body goes through to give birth to your baby. Preterm labor can lead to premature birth. Premature birth is when your baby is born early, before 37 weeks of pregnancy. Your baby needs about 40 weeks in the womb to grow and develop before birth.
Babies born before 37 weeks of pregnancy are called premature. Premature babies can have serious health problems at birth and later in life. About 1 in 10 babies is born prematurely each year in the United States.
What are the signs and symptoms of preterm labor?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Learn the signs and symptoms of preterm labor so you can get help quickly if they happen to you.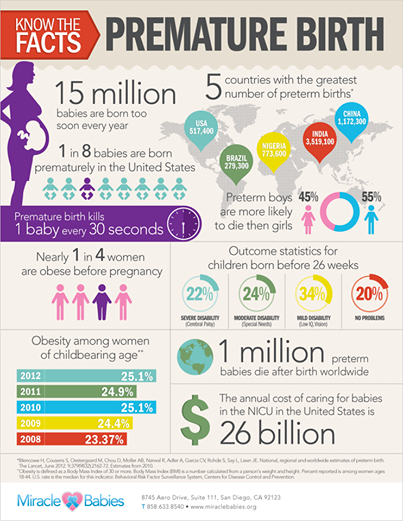
If you have even one of these signs and symptoms of preterm labor, call your provider right away:
- Change in your vaginal discharge (watery, mucus or bloody) or more vaginal discharge than usual
- Pressure in your pelvis or lower belly, like your baby is pushing down
- Constant low, dull backache
- Belly cramps with or without diarrhea
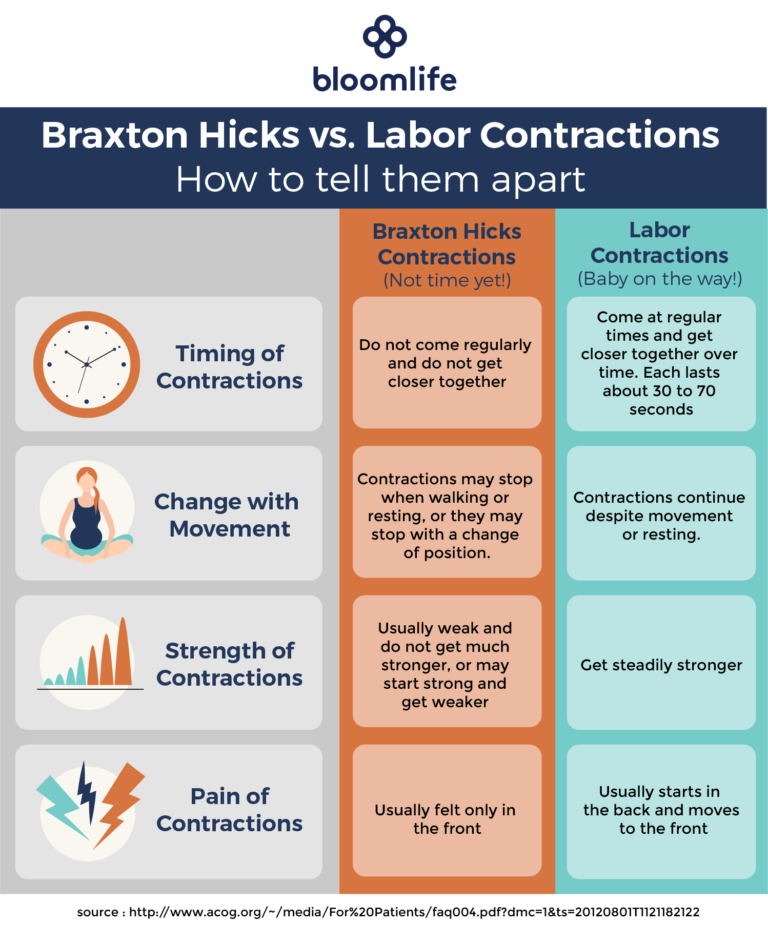
- Regular or frequent contractions that make your belly tighten like a fist. The contractions may or may not be painful.
- Your water breaks
When you see your provider, he may do a pelvic exam or a transvaginal ultrasound to see if your cervix has started to thin out and open for labor. Your cervix is the opening to the uterus (womb) that sits at the top of the vagina (birth canal). A transvaginal ultrasound is done in the vagina instead of on the outside of your belly. Like a regular ultrasound, it uses sound waves and a computer to make a picture of your baby. If you’re having contractions, your provider monitors them to see how strong and far apart they are. You may get other tests to help your provider find out if you really are in labor.
You may get other tests to help your provider find out if you really are in labor.
If you’re having preterm labor, your provider may give you treatment to help stop it. Or you may get treatment to help improve your baby’s health before birth. Talk to your provider about which treatments may be right for you.
Are you at risk for preterm labor and premature birth?
We don’t always know for sure what causes preterm labor and premature birth. Sometimes labor starts on its own without warning. Even if you do everything right during pregnancy, you can still give birth early.
We do know some things may make you more likely than others to have preterm labor and premature birth. These are called risk factors. Having a risk factor doesn’t mean for sure that you’ll have preterm labor or give birth early. But it may increase your chances. Talk to your health care provider about what you can do to help reduce your risk.
Because many premature babies are born with low birthweight, many risk factors for preterm labor and premature birth are the same as for having a low-birthweight baby. Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces.
Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces.
These three risk factors make you most likely to have preterm labor and give birth early:
- You’ve had a premature baby in the past.
- You’re pregnant with multiples (twins, triplets or more).
- You have problems with your uterus or cervix now or you’ve had them in the past. Your uterus (also called the womb) is where your baby grows inside you.
Medical risk factors before pregnancy for preterm labor and premature birth
- Being underweight or overweight before pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Having a family history of premature birth. This means someone in your family (like your mother, grandmother or sister) has had a premature baby. If you were born prematurely, you’re more likely than others to give birth early.
- Getting pregnant again too soon after having a baby.
 For most women it’s best to wait at least 18 months before getting pregnant again. Talk to your provider about the right amount of time for you.
For most women it’s best to wait at least 18 months before getting pregnant again. Talk to your provider about the right amount of time for you.
Medical risk factors during pregnancy for preterm labor and premature birth
Having certain health conditions during pregnancy can increase your risk for preterm labor and premature birth, including:
- Connective tissue disorders, like Ehlers-Danlos syndromes (also called EDS) and vascular Ehlers-Danlos syndrome (also called vEDS). Connective tissue is tissue that surrounds and supports other tissues and organs. EDS can cause joints to be loose and easy to dislocate; skin to be thin and easily stretched and bruised; and blood vessels to be fragile and small. It also can affect your uterus and intestines. vEDS is the most serious kind of EDS because it can cause arteries and organs (like the uterus) to rupture (burst). EDS and vEDS are genetic conditions that can be passed from parent to child through genes.
- Diabetes. Diabetes is when your body has too much sugar (called glucose) in your blood.
- High blood pressure and preeclampsia. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. This can stress your heart and cause problems during pregnancy. Preeclampsia is a kind of high blood pressure some women during or right after pregnancy. If not treated, it can cause serious problems and even death.
- Infections, including sexually transmitted infections (also called STIs) and infections of the uterus, urinary tract or vagina
- Intrahepatic cholestasis of pregnancy (also called ICP). ICP is the most common liver condition that happens during pregnancy.
- Thrombophilias. These are conditions that increase your risk of making abnormal blood clots.
Other medical risk factors during pregnancy include:
- Getting late or no prenatal care. Prenatal care is medical care you get during pregnancy.
- Not gaining enough weight during pregnancy. This can include having an eating disorder, like anorexia or bulimia.
- Bleeding from the vagina in the second or third trimester
- Preterm premature rupture of the membranes (also called PPROM). Premature rupture of membranes (also called PROM) is when the amniotic sac around your baby breaks (your water breaks) before labor starts. PPROM is when this happens before 37 weeks of pregnancy. If you have any fluid leaking from your vagina, call your provider and go to the hospital.
- Being pregnant after in vitro fertilization (also called IVF). IVF is a fertility treatment used to help women get pregnant.
- Being pregnant with a baby who has certain birth defects, like heart defects or spina bifida. Birth defects are health conditions that are present at birth.
 They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. Spina bifida is a birth defect of the spine.
They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. Spina bifida is a birth defect of the spine.
Risk factors in your everyday life for preterm labor and premature birth
- Smoking, drinking alcohol, using street drugs or abusing prescription drugs.
- Having a lot of stress in your life, Low socioeconomic status (also called SES). SES is a combination of things like your education, your job and your income (how much money you make).
- Domestic violence. This is when your partner hurts or abuses you. It includes physical, sexual and emotional abuse.
- Working long hours or having to stand a lot
- Exposure to air pollution, lead, radiation and chemicals in things like paint, plastics and secondhand smoke. Secondhand smoke is smoke from someone else’s cigarette, cigar or pipe.
Age and race as risk factors for preterm labor and premature birth
Being younger than 17 or older than 35 makes you more likely than other women to give birth early. In the United States, black women are more likely to give birth early. Almost 17 percent of black babies are born prematurely each year. Just more than 10 percent of American Indian/Alaska Native and Hispanic babies are born early, and less than 10 percent of white and Asian babies. We don’t know why race plays a role in premature birth; researchers are working to learn more about it.
In the United States, black women are more likely to give birth early. Almost 17 percent of black babies are born prematurely each year. Just more than 10 percent of American Indian/Alaska Native and Hispanic babies are born early, and less than 10 percent of white and Asian babies. We don’t know why race plays a role in premature birth; researchers are working to learn more about it.
Can you reduce your risk for preterm labor and premature birth?
Yes, you may be able to reduce your risk for early labor and birth. Some risk factors are things you can’t change, like having a premature birth in a previous pregnancy. Others are things you can do something about, like quitting smoking.
Here’s what you can do to reduce your risk for preterm labor and premature birth:
- Get to a healthy weight before pregnancy and gain the right amount of weight during pregnancy. Talk to your provider about the right amount of weight for you before and during pregnancy.
- Don’t smoke, drink alcohol use street drugs or abuse prescription drugs. Ask your provider about programs that can help you quit.
- Go to your first prenatal care checkup as soon as you think you’re pregnant. During pregnancy, go to all your prenatal care checkups, even if you’re feeling fine. Prenatal care helps your provider make sure you and your baby are healthy.
- Get treated for chronic health conditions, like high blood pressure, diabetes, depression and thyroid problems. Depression is a medical condition in which strong feelings of sadness last for a long time and interfere with your daily life. It needs treatment to get better. The thyroid is a gland in your neck that makes hormones that help your body store and use energy from food.
- Protect yourself from infections. Talk to your provider about vaccinations that can help protect you from certain infections. Wash your hands with soap and water after using the bathroom or blowing your nose.
 Don’t eat raw meat, fish or eggs. Have safe sex. Don’t touch cat poop.
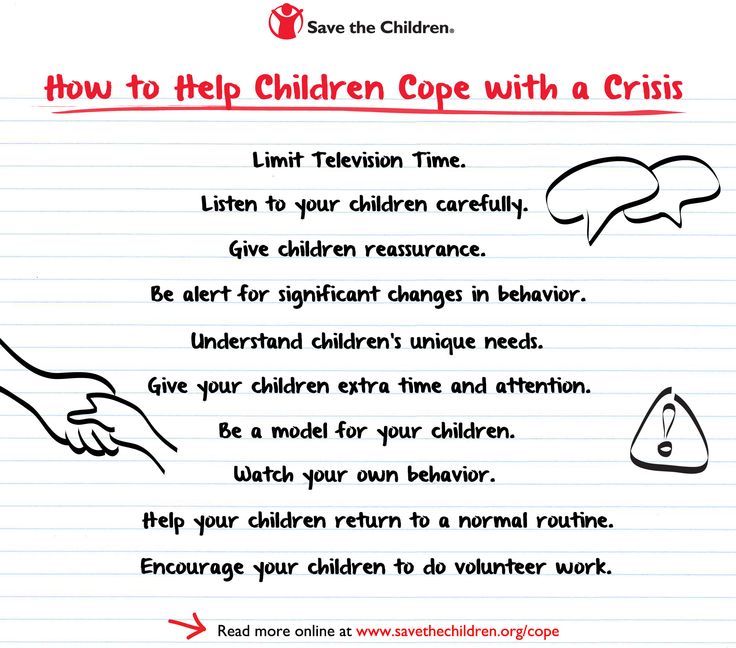
Don’t eat raw meat, fish or eggs. Have safe sex. Don’t touch cat poop. - Reduce your stress. Eat healthy foods and do something active every day. Ask family and friends for help around the house or taking care of other children. Get help if your partner abuses you. Talk to your boss about how to lower your stress at work.
- Wait at least 18 months between giving birth and getting pregnant again. Use birth control until you’re ready to get pregnant again. If you’re older than 35 or you’ve had a miscarriage or stillbirth, talk to your provider about how long to wait between pregnancies. Miscarriage is the death of a baby in the womb before 20 weeks of pregnancy. Stillbirth is the death of a baby in the womb after 20 weeks of pregnancy.
Last reviewed: March, 2018
See also: Signs and symptoms of preterm labor infographic
Premature birth - Juno
Premature birth: content of the article
What is preterm birth
The birth of a baby weighing more than 0. 5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.
At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.
Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different terms
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous. Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
- By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced.
 For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life; - According to symptoms: threatening, incipient and incipient. With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm birth
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis.
 They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth; - Placental bleeding. They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
- Neck weakness. In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
- Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, angina, health status during gestation, genetic factors are all common reasons for early delivery.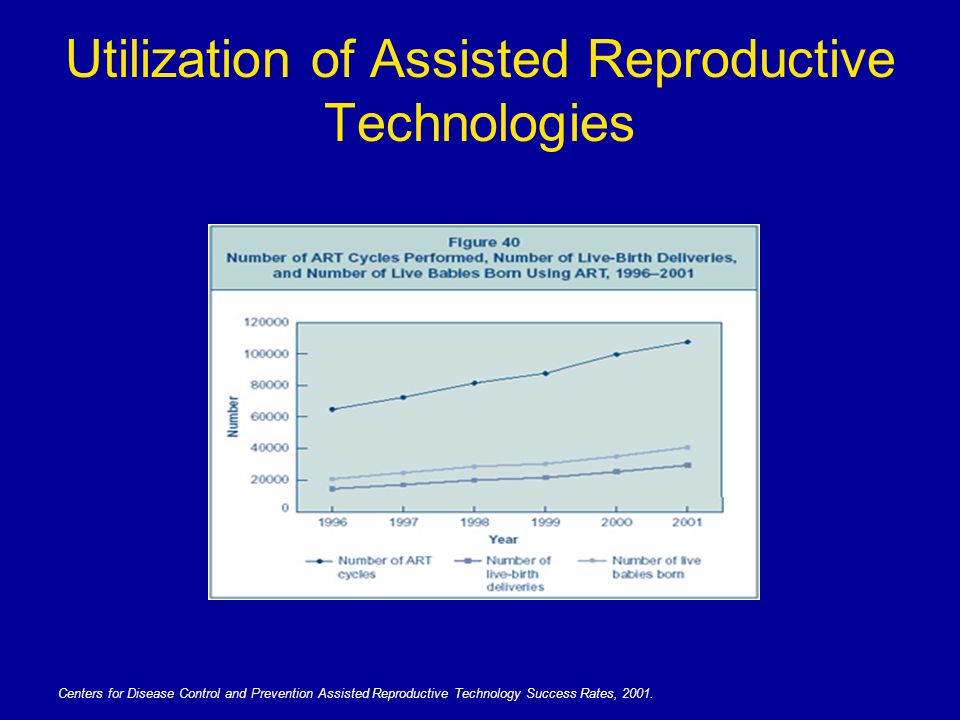 Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.

Differential diagnosis
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck. Determined by the level of PSIFR-1 in the cervical canal.
Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 stages of preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby. A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
- Take care of yourself. Rest, avoid nervous overload. Sleep at least 7 hours;
- Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman.
Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
- Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it. Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
- Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body.
In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
- Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up. This will relax the muscles, eliminate swelling;
- Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck. The expectant mother is out of the risk zone in this situation, stitches may not be applied.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the mortality rate of newborns is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short neck in multiple pregnancies can provoke preterm labor. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibiotic prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Terminals
Premature birth is one of the fears of many expectant mothers. Nobody is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, do not refuse to stay in the perinatal center.
Don't think bad. Modern medicine successfully nurses premature babies, reduces the risks of complications and consequences.
The role of determining biochemical tests and cervicometry in the diagnosis of threatened preterm birth » Obstetrics and Gynecology
Purpose of the study. Evaluation of the use of the PartoSure test for the determination of placental α-microglobulin (PAMG-1) and cervicometry to determine the risk of preterm birth.
Material and methods. The test for the determination of PAMG-1 and cervicometry were performed in 49 patients with threatened preterm labor. In the case of delivery, the interval between the time and date of the test of delivery (TTD) was estimated.
Results. The test was positive in 100% of cases with a length of the cervical canal ≤1.5 cm (6% of patients), while in 75% there was a preterm birth (TTD: 18 and 44 hours). With the length of the cervical canal from 1.5 to 3 (85%), only in 1 case a positive test result was detected, TTD=140 h.
The relationship between the results of the test and cervicometry, diagnostic sensitivity, specificity, predictive value of positive and negative results were determined.
Conclusion. The PartoSure PAMG-1 test, combined with cervicometry, is a method for determining outpatient treatment for threatened preterm labor.
Currently, the frequency of preterm births is 6-10% of all births in the Russian Federation [1]. The clinical picture of threatening preterm labor consists of complaints of a pregnant woman at a period of 220/7–366/7 weeks for pulling pains in the lower abdomen and lower back, contractions, detection of increased uterine tone during an objective examination, as well as changes in the cervix during vaginal examination (and namely, its softening and shortening). In the presence of clinical manifestations of threatening preterm birth, it is customary in the vast majority of cases to hospitalize a pregnant woman in a hospital, prescribe tocolytic drugs, as well as glucocorticosteroids in order to prevent fetal respiratory distress syndrome. Currently, there are no clear criteria for the need for hospitalization in the presence of a threat of preterm birth and, accordingly, the percentage of outpatient treatment of patients with this pathology is decreasing. There is evidence that 30% of cases of threatened preterm birth stop spontaneously, without medical treatment [2].
In clarifying the criteria for diagnosis and the likelihood of spontaneous preterm birth, the possibility of reducing cases of unreasonable inpatient treatment and drug aggression is laid down.
To clarify the likelihood of preterm birth, the following methods are currently used: instrumental (ultrasound assessment of the cervix) and biochemical (tests based on the determination of fibronectin (FFN), placental α-microglobulin (PAMG-1) and phosphorylated protein-I, binding insulin-like growth factor (phIGFBP-I).
The listed biochemical markers are mainly used to diagnose premature rupture of amniotic fluid, however, the concentration of these proteins increases in the vaginal secretion and in the presence of uterine contractions in intact fetal membranes [3-6]. In particular, PAMG-1 is found at very high concentrations in amniotic fluid and at very low concentrations in vaginal secretions. Lee, Romero et al. put forward two reasons for the increase in the concentration of this protein in the vaginal secretion in cases of threatened preterm labor with an intact fetal bladder: 1) PAMG-1 extravasation through the pores of the membranes during uterine contractions and 2) degradation of the extracellular matrix of the membranes due to the inflammatory process, which, in turn, , the root cause of threatening preterm birth [7].
Compared to FFN and phIGFBP-I, the PAMG-1 test has a higher positive predictive value: a positive Partosure test in pregnant women with symptoms of threatened preterm labor is highly likely to indicate the possibility of labor within 7 days; a negative test result indicates a low probability of delivery within 14 days after the test [8].
The length of the cervical canal of 30 mm or more on transvaginal ultrasound (ultrasound) indicates a low probability of preterm birth even in the presence of uterine tone in preterm pregnancy [2]. Whereas, according to R.E. Bittar et al., in the presence of changes in the cervix in the form of its shortening less than 2 cm, the probability of delivery before the 37th week of pregnancy is 69.6% [5].
There is evidence that the combined use of biochemical test (FFN) and cervical ultrasound enhances the diagnostic value of the latter, especially when the length of the cervix is less than 30 mm [2]. According to a study by D. Paternoster, the length of the cervical canal and the result of the phIGFBP-I test are independent predictors of the likelihood of preterm birth; at the same time, the length of the cervical canal is more than 26 mm and a negative test result indicates a low probability of preterm labor in the presence of uterine contractions at a period of less than 37 weeks [9].
Data on the study of the combined use of transvaginal ultrasound assessment of the cervix and a test that determines the presence of PAMG-1 in vaginal secretions in threatened preterm labor was not found in the available literature.
The aim of the study was to evaluate the combined use of the PAMG-1 test in vaginal secretion and transvaginal cervicometry to determine the risk of preterm birth.
Material and research methods
A prospective study was conducted in 50 pregnant women with signs of threatened preterm labor from January to September 2014. One patient was excluded from the study due to refusal to continue inpatient treatment. The inclusion criteria for the study were the following parameters: gestational age 220/7–366/7 weeks, presence of complaints of nagging pain in the lower abdomen and/or contractions, the presence of contractions according to cardiotocography data, the absence of clinical data for premature rupture of amniotic fluid (a whole amniotic bladder with vaginal examination), singleton pregnancy, head presentation of the fetus. All pregnant women underwent clinical and laboratory examination: history taking, general clinical and special obstetric examination, PartoSure time-to-delivery (TTD) test (AmniSure International, Boston, MA, USA) to determine the presence of PAMG-1 in vaginal discharge), vaginal examination with an assessment of the condition of the cervix, namely its length, degree of softening and patency of the cervical canal; Ultrasound with cervicometry, assessment of the functional state of the fetus and the nature of the contractile activity of the uterus (cardiotocography) with obtaining the informed consent of the patients for all of the above procedures. In cases of preterm birth, the time interval of the spontaneous birth prediction test (the interval between the time and date of the test and the time and date of birth) was evaluated.
The PartoSure TTD test was performed according to the following procedure: a sample of vaginal discharge taken with a vaginal swab was placed in a solvent tube. The sample was extracted from the swab with the solvent for 1 minute, after which the test strip was immersed in the test tube. The test result was visually read by the presence of one or two lines: the absence of strips - the test is of poor quality, one strip - a negative result, two strips - a positive result (there is a high probability of preterm labor within the next 7 days).
Transvaginal cervicometry was performed after the PartoSure TTD test using a 5 MHz transvaginal transducer placed in the anterior vaginal fornix. The length of the cervical canal was defined as the distance between the internal and external os of the cervix.
All patients underwent therapy aimed at maintaining pregnancy (β-agonists, calcium antagonists, magnesium sulfate, glucocorticoids).
Statistical analysis of the obtained data was performed using Microsoft Excel 2007 (Microsoft Corporation, USA) and STATISTICA v.8 (Statsoft Inc., Tulsa, USA).
Results of the study
The first stage of our study was a clinical examination of pregnant women with threatened preterm labor (Table 1).
As shown in the table. 1, the mean gestational age of the examined patients was 32 weeks (interquartile range 29–35 weeks). Approximately 15% of women had a history of preterm birth, 30% had spontaneous miscarriages up to 22 weeks. It should be noted that one third of the surveyed pregnant women had ovarian failure before pregnancy and infectious diseases of the urogenital tract (bacterial vaginosis and cervicitis of various etiologies) during this pregnancy, which could be considered as an etiological factor in the threat of abortion. Attention is drawn to the multiple hospitalizations during this pregnancy (this hospitalization was at least repeated in half of the women).
At admission, all pregnant women complained of pulling pains in the lower abdomen and/or contractions. Cardiotocography revealed a satisfactory fetal condition and irregular contractions (from 2 to 20 contractions per hour, median 10, interquartile range 5–13 contractions) in all patients. The PartoSure TTD test was positive in 4 of 49 patients (8%). Vaginal examination revealed changes in the cervix: its shortening (less than 3 cm) and/or softening in 38 (88%) pregnant women. At the same time, the absence of changes in the cervix was found in 11 (22%) women with complaints characteristic of the threat of abortion in the presence of contractions on cardiotocography. When transvaginal cervicometry in 3 (6%) women, the length of the cervical canal was 1.5 cm or less; in 42 (85%) patients - from 1.5 to 3 cm: in 4 (8%) patients, the length of the cervical canal was 3 cm or more. The expansion of the internal os was detected in 2 of 49women (4%). At the same time, in eight patients who did not have changes in the cervix during vaginal examination, a shortening of the cervix of less than 3 cm was detected during transvaginal cervicometry. Thus, in the presence of clinical manifestations of the threat of termination of pregnancy, transvaginal cervicometry can be recommended.
Despite full pregnancy maintenance therapy, 3 out of 49 women (6%) delivered within 7 days of admission; the time interval of the spontaneous birth prediction test (the interval between the time and date of the examination and the time and date of birth) was 18, 44 and 140 hours.
The second step of our study was to determine the relationship between the results of the PartoSure TTD test and ultrasound cervicometry data in assessing the risk of preterm birth. Depending on the length of the cervix during ultrasound cervicometry, pregnant women were divided into 3 groups: 1. 5 cm or less (group 1), from 1.5 to 3 cm (group 2), more than 3 cm (group 3). group) (Table 2).
Among the examined pregnant women with threatened preterm labor, a significantly larger proportion were patients with a shortened neck during ultrasound cervicometry (groups 1 and 2), while group 3 (with an unchanged cervix) made up a significantly smaller part (p< 0.05). The PartoSure TTD test in the 3rd group also showed a negative value in 100% of cases.
These facts confirm the results of other researchers [5] and may indicate, in particular, that patients with complaints characteristic of threatened preterm labor and a preserved cervix during an objective examination (ultrasound cervicometry), as well as a negative test result for the determination PAMG-1 can receive therapy on an outpatient basis.
In the 1st group (cervical length 1.5 cm or less), all women had a positive result of the PartoSure TTD test, while, despite the therapy, 2 out of 3 women gave birth prematurely (at a period of 34 and 35 weeks) , and the third patient gave birth 16 days later at 38 weeks' gestation. Thus, these data confirm the highest risk of preterm birth with a cervical length of less than 1.5 cm and a positive biochemical test result.
Of particular interest for study is the 2nd group, which consisted of patients with a length of the cervical canal from 1.5 to 3 cm according to ultrasonic cervicometry. Out of 42 women in this group (85% of the examined patients), only 1 case showed a positive result of the PartoSure TTD biochemical test. The time interval of the spontaneous birth prediction test in this case was 140 hours. All other patients were discharged home after a maximum of 18 days with progressing pregnancy. Thus, patients in the presence of complaints, as well as such objective data of the threat of termination of pregnancy, as shortening of the cervical canal (from 1.5 to 3 cm with transvaginal cervicometry), undoubtedly, are included in the "risk zone" of preterm labor and require drug therapy, however, the need for hospitalization in this case remains controversial. In this situation, it is the combined use of ultrasound and biochemical methods that can resolve the issue of the need for inpatient treatment. If the cervical canal is longer than 1.5 cm and the result of the PartoSure TTD test is negative, it is possible to discuss the issue of outpatient treatment for the pregnant woman.
We also evaluated the correlation between the results of the test and cervicometry. Spearman's correlation coefficient was -0.47, p<0.05. Thus, the shorter the cervical canal, the more likely a positive PartoSure TTD test result.
Our study found a very low diagnostic specificity (11%) for a cervical canal length of less than 3 cm on transvaginal cervicometry with respect to the likelihood of preterm birth within 14 days. The diagnostic sensitivity of this method was 100%. At the same time, the diagnostic sensitivity of the PartoSure TTD test regarding the likelihood of preterm birth within 14 days after the test, according to our data, was 100%, and the specificity was 9eight%; the predictive value of a positive result is 75%, the predictive value of a negative result is 100%, which confirms the data of other researchers [8].
Conclusion
Thus, for diagnosing threatened preterm labor and determining indications for inpatient treatment, in addition to assessing complaints and an objective examination of patients, instrumental methods (transvaginal ultrasound cervicometry) and biochemical markers of threatened preterm labor are of great importance. Performing transvaginal cervicometry in all patients with complaints characteristic of threatening preterm labor allows to identify patients requiring medical therapy. However, given the low specificity of this method, it should be recommended to use the test for the determination of PAMG-1 in vaginal secretion simultaneously with cervicometry as a method with high specificity and predictive value to determine the possibility of outpatient treatment for this group of patients.
Bolotskikh Vyacheslav Mikhailovich, Doctor of Medical Sciences, Head 2nd Department of Pathology of Pregnancy, Federal State Budgetary Institution Research Institute of Obstetrics and Gynecology named after A.