Pregnant with rh negative blood
Rh factor blood test - Mayo Clinic
Overview
Rh factor is an inherited protein found on the surface of red blood cells. If your blood has the protein, you're Rh positive. If your blood doesn't have the protein, you're Rh negative. The "+" or "–" you might see after your blood type refers to Rh positive or Rh negative.
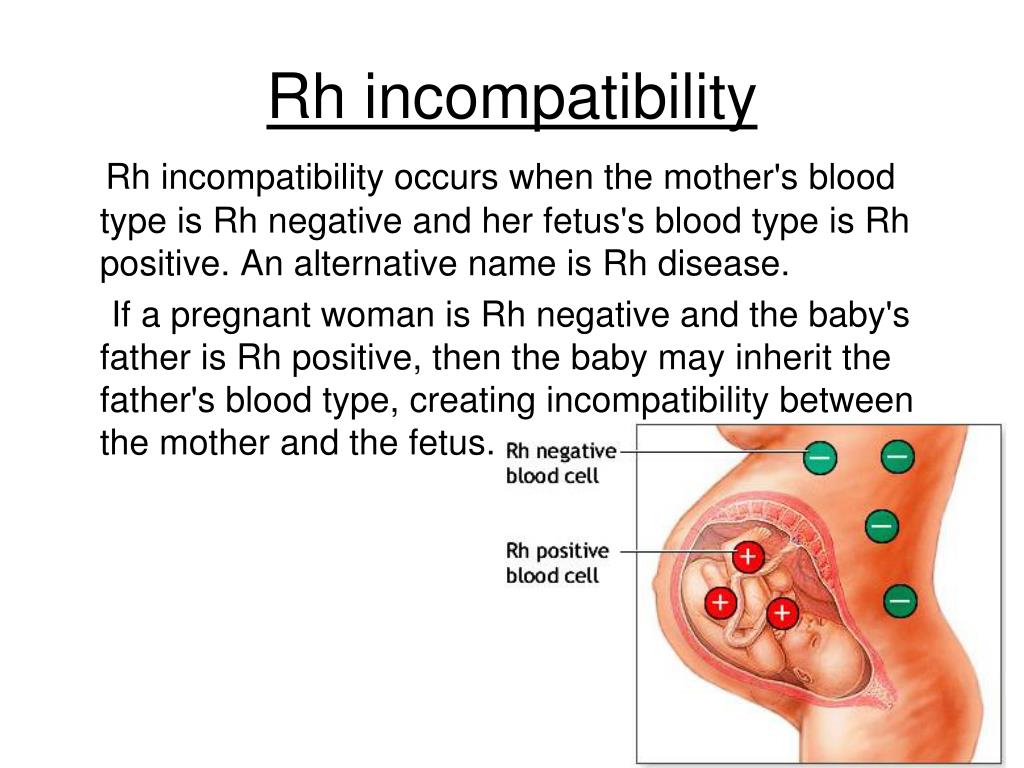
Rh positive is much more common than Rh negative. Having an Rh negative blood type is not an illness, and it usually does not affect your health. But it can affect pregnancy. Your pregnancy needs special care if you're Rh negative and your baby is Rh positive. That's called Rh incompatibility. A baby can inherit the Rh factor from either parent.
Your health care provider will advise that you have a blood type and Rh factor screening test during your first prenatal visit. This will show whether you are Rh positive or Rh negative.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
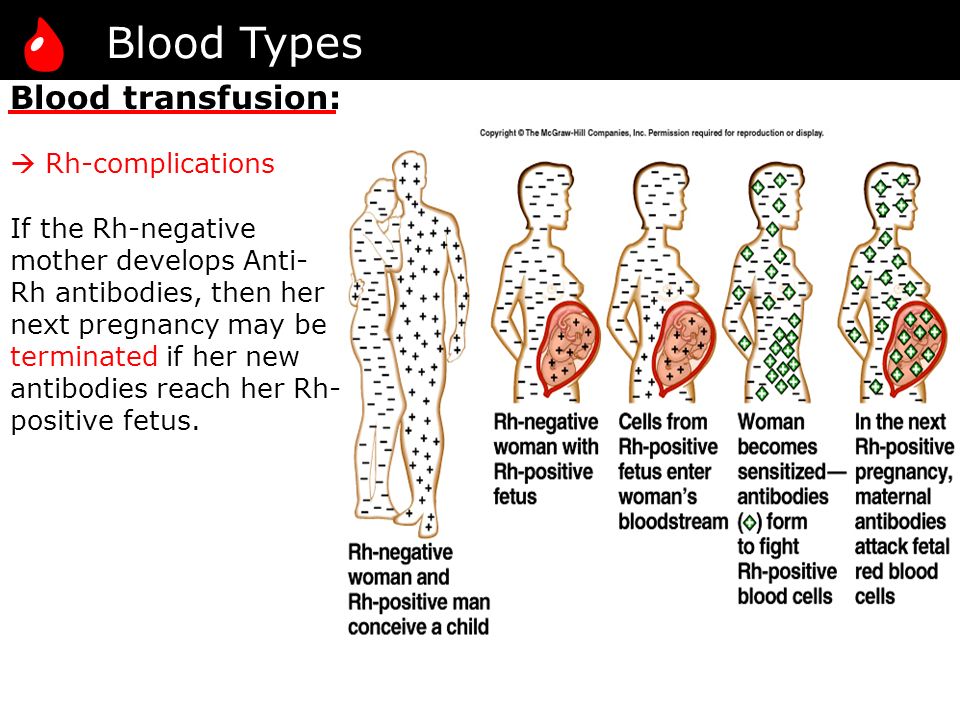
During pregnancy, problems can happen if you're Rh negative and your baby is Rh positive. Usually, your blood doesn't mix with your baby's blood during pregnancy. However, a small amount of your baby's blood could come in contact with your blood when the baby is born. It can also happen if you have bleeding or trauma to your abdomen during pregnancy.
If you're Rh negative and your baby is Rh positive, your body might produce proteins called Rh antibodies if your blood and the baby's blood mix. Those antibodies aren't a problem during the first pregnancy. But problems can happen if you become pregnant again.
If your next baby is Rh positive, the Rh antibodies can cross the placenta and damage the baby's red blood cells. This could lead to life-threatening anemia, a condition in which red blood cells are destroyed faster than the baby's body can replace them. Red blood cells are needed to carry oxygen throughout the body.
If you're Rh negative, you might need to have another blood test — called an antibody screen — several times: during your first trimester, during week 28 of pregnancy and when your baby is born. Some people need the test more often.
Some people need the test more often.
That test is used to detect antibodies to Rh positive blood. If you haven't started to produce Rh antibodies, you'll likely need a shot (injection) of a blood product called Rh immune globulin. This prevents your body from producing Rh antibodies during your pregnancy.
If your baby is born Rh negative, you don't need any other treatment. If your baby is born Rh positive, you'll need another injection shortly after delivery.
If you're Rh negative and your baby might be or is Rh positive, your health care provider may recommend an Rh immune globulin injection after situations in which your blood could come into contact with the baby's blood, including:
- Miscarriage
- Ectopic pregnancy — when a fertilized eggs implants somewhere outside the uterus, usually in a fallopian tube
- Abortion
- Removal of a molar pregnancy — a noncancerous (benign) tumor that develops in the uterus
- Amniocentesis — a prenatal test in which a sample of the fluid that surrounds and protects a baby in the uterus (amniotic fluid) is removed for testing or treatment
- Chorionic villus sampling — a prenatal test in which a sample of the wispy projections that make up most of the placenta (chorionic villi) is removed for testing
- Cordocentesis — a prenatal test in which a sample of the baby's blood is removed from the umbilical cord for testing
- Bleeding during pregnancy
- Injury or other trauma to your abdomen during pregnancy
- The external manual rotation of a baby in a breech position — such as buttocks first — before labor
- Delivery
If the antibody screen shows that you're already producing antibodies, an injection of Rh immune globulin won't help.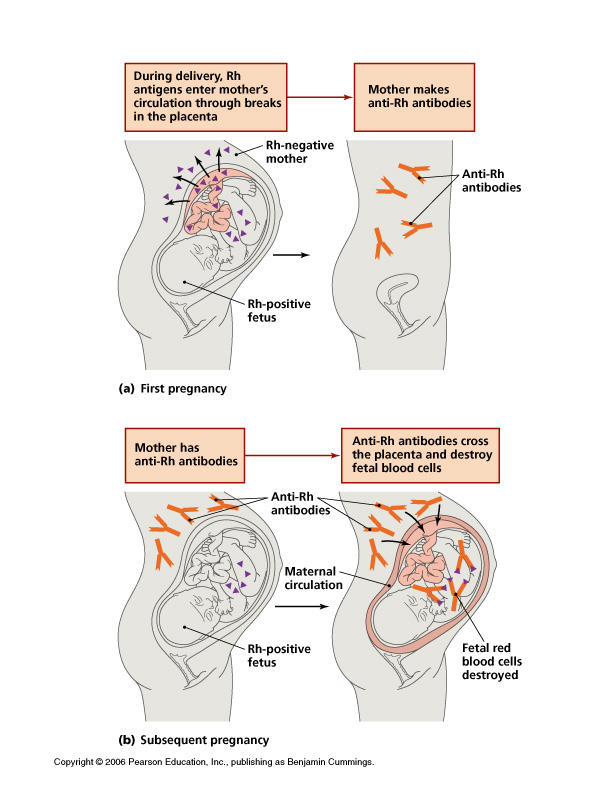 Your baby will be carefully monitored during your pregnancy. The baby might be given a blood transfusion through the umbilical cord during pregnancy or immediately after delivery if necessary.
Your baby will be carefully monitored during your pregnancy. The baby might be given a blood transfusion through the umbilical cord during pregnancy or immediately after delivery if necessary.
| Mother's Rh factor | Father's Rh factor | Baby's Rh factor | Precautions |
|---|---|---|---|
| Rh positive | Rh positive | Rh positive | None |
| Rh negative | Rh negative | Rh negative | None |
| Rh positive | Rh negative | Could be Rh positive or Rh negative | None |
| Rh negative | Rh positive | Could be Rh positive or Rh negative | Rh immune globulin injections |
What you can expect
An Rh factor test is a basic blood test. The blood sample usually is taken during the first prenatal visit and sent to a lab for testing. No special preparation is necessary.
The blood sample usually is taken during the first prenatal visit and sent to a lab for testing. No special preparation is necessary.
Results
If you're Rh positive, you don't need to do anything.
If you're Rh negative and your baby is Rh positive, your body could make antibodies that might be harmful during another pregnancy. Take these steps:
- If you have vaginal bleeding any time during pregnancy, contact your health care provider right away.
- Talk with your health care provider about scheduling an Rh immune globulin injection during your pregnancy.
- Remind your health care team during labor that you're Rh negative.
By Mayo Clinic Staff
Related
Products & Services
The Rh Factor: How It Can Affect Your Pregnancy
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Breech Presentation: A position in which the feet or buttocks of the fetus would appear first during birth.
Cells: The smallest units of a structure in the body. Cells are the building blocks for all parts of the body.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Ectopic Pregnancy: A pregnancy in a place other than the uterus, usually in one of the fallopian tubes.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Genes: Segments of DNA that contain instructions for the development of a person's physical traits and control of the processes in the body.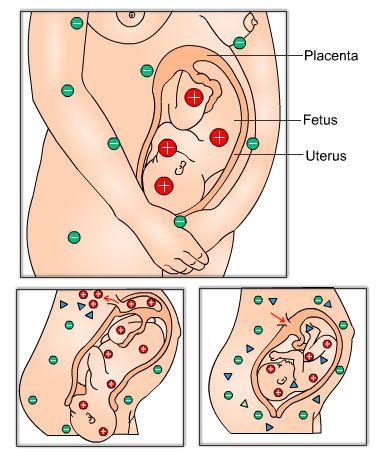 They are the basic units of heredity and can be passed from parent to child.
They are the basic units of heredity and can be passed from parent to child.
Induced Abortion: An intervention to end a pregnancy so that it does not result in a live birth.
Jaundice: A buildup of bilirubin (a brownish yellow substance formed from the breakdown of red cells in the blood) that causes the skin to have a yellowish appearance.
Miscarriage: Loss of a pregnancy that is in the uterus.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women's health.
Oxygen: An element that we breathe in to sustain life.
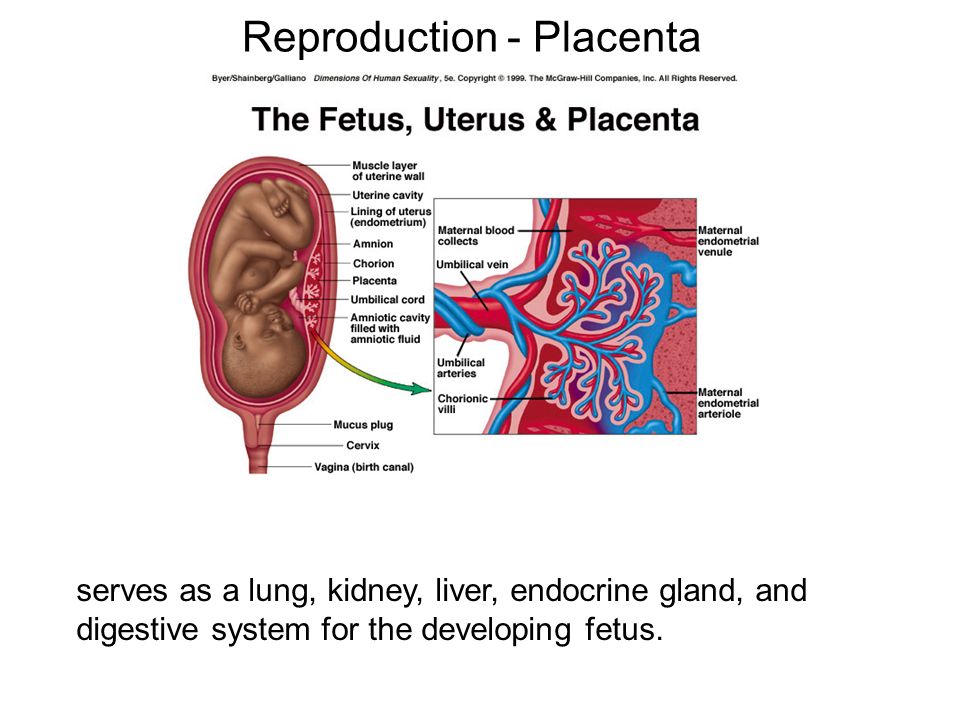
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rh Immunoglobulin (RhIg): A substance given to prevent an Rh-negative person's antibody response to Rh-positive blood cells.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord: A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus: A muscular organ in the female pelvis. During pregnancy, this organ contains and nourishes the fetus.
Pregnancy in women with Rh-negative blood
The issue of Rhesus conflict during pregnancy is one of the few in medicine, in which all the i's are dotted and not only diagnostic and treatment methods have been developed, but, most importantly, effective prevention.
The history of immunoprophylaxis of Rhesus conflict is a rare example of unconditional success in medicine. Indeed, after the introduction of a set of preventive measures, infant mortality from complications of the Rhesus conflict decreased from 46 to 1.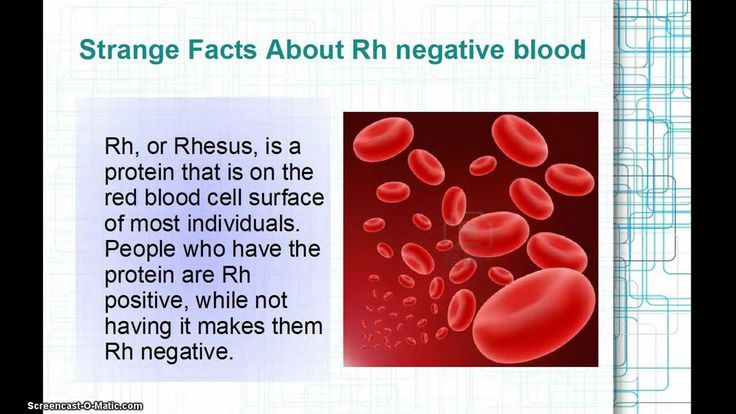 6 per 100 thousand children - that is, almost 30 times.
6 per 100 thousand children - that is, almost 30 times.
What is Rh conflict, why does it occur and what can be done to minimize the risk of its occurrence?
The entire population of the planet, depending on the presence or absence on erythrocytes (red blood cells) of the protein, denoted by the letter "D", is divided respectively into Rh-positive and Rh-negative people. According to approximate data, about 15% of Europeans are Rh-negative. When pregnancy occurs in an Rh-negative woman from an Rh-positive man, the probability of having an Rh-positive child is 60%.
In this case, when fetal erythrocytes enter the mother's bloodstream, an immune reaction occurs, as a result of which fetal erythrocytes are damaged, anemia and a number of other serious complications occur.
During physiological pregnancy, fetal erythrocytes cross the placenta in the first trimester in 3% of women, in the second - in 15%, in the third - in 48%. In addition, massive casting occurs in childbirth, after termination of pregnancy (abortion, miscarriage, ectopic pregnancy, hydatidiform mole), invasive procedures (chorionic villus biopsy, amniocentesis), prenatal bleeding with a threat of termination of pregnancy.
The total risk of developing an Rh conflict in Rh-negative women pregnant with an Rh-positive fetus in the absence of prophylaxis is about 16%. In women who have undergone prophylaxis, this risk is reduced to 0.2%.
And now the most interesting - what is this very prevention and what needs to be done to keep the situation under control.
All women who applied to a medical institution for pregnancy registration, as well as those who applied to terminate an unwanted pregnancy, are assigned an analysis to determine the blood type and Rh factor. Sexual partners of women who have a negative Rh are also recommended to undergo an examination to establish Rh-affiliation. If, by a happy coincidence, a man also has a negative Rh factor, then there is no risk of an Rh conflict and there is no point in conducting immunoprophylaxis.
Women with Rh-negative blood and Rh-positive partner's blood who wish to terminate an unwanted pregnancy are advised to give an injection of anti-Rh immunoglobulin within 72 hours after the termination. The mechanism of action of this drug is based on the fact that the injected antibodies bind the fetal erythrocytes that have entered the maternal bloodstream and prevent the development of an immune response.
The mechanism of action of this drug is based on the fact that the injected antibodies bind the fetal erythrocytes that have entered the maternal bloodstream and prevent the development of an immune response.
Rh-negative women registered for pregnancy are prescribed a monthly blood test for anti-Rh antibodies. Thus, it is determined whether there was contact between the blood of the mother and the fetus, and whether the woman's immune system reacted to a foreign protein.
If by the 28th week there are no anti-Rh antibodies in the woman's blood, she is sent for prophylactic administration of anti-Rh immunoglobulin. This prophylaxis is carried out from 28 to 30 weeks of pregnancy. After that, the determination of anti-Rhesus antibodies in the mother's blood is not carried out.
If, according to the results of the examination, anti-Rhesus antibodies are detected in a woman before 28 weeks of pregnancy, she is sent for an in-depth examination to determine the severity of the Rh conflict, timely treatment and, if necessary, emergency delivery.
After the birth of an Rh-negative woman, the Rh factor is determined. And, if the baby is Rh-positive, within 72 hours after birth, the woman is also injected with anti-Rh immunoglobulin.
Other situations requiring prophylactic administration of anti-Rhesus immunoglobulin:
- miscarriage or non-progressive pregnancy;
- ectopic pregnancy;
- hydatidiform mole;
- prenatal bleeding with threatened miscarriage;
- invasive intrauterine interventions during pregnancy.
The only controversial issue at the moment is the determination of the Rh factor of the fetus during pregnancy. To do this, starting from the 10th week of pregnancy, a woman’s blood is taken, the genetic material of the fetus is isolated from it, and on the basis of a genetic study, the Rh affiliation of the unborn child is determined.
On the one hand, this study would allow 40% of Rh-negative women carrying an Rh-negative fetus to avoid monthly testing of anti-Rh antibodies and the introduction of anti-Rh immunoglobulin.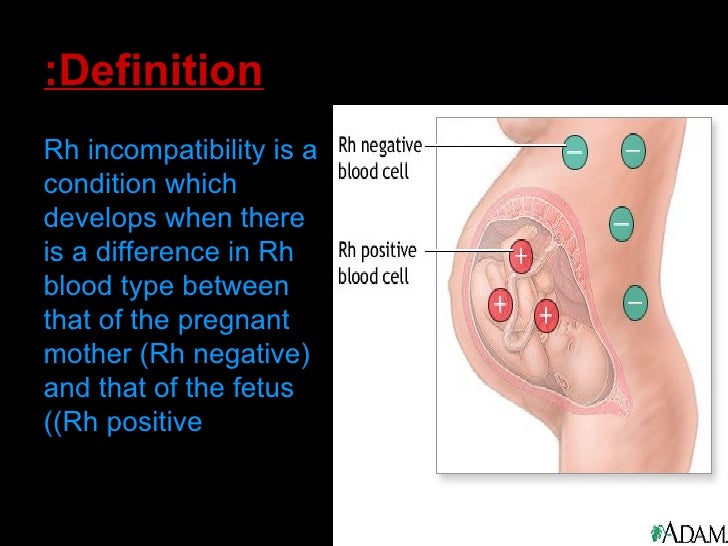
On the other hand, this research does not appear in the official order of the Ministry of Health, is not included in the CHI system and is carried out only on a paid basis.
Thus, at the moment, a clear algorithm has been developed for the management of pregnant women with Rh-negative blood. And following this simple algorithm will allow a woman to give birth to one, two or more healthy babies.
Obstetrician-gynecologist
antenatal clinic No. 14
Khivrich E.B.
Pregnancy and Rh
All parents dream of having a healthy baby. Many risks associated with the health of the baby are now manageable. This means that some, even very serious and dangerous diseases are preventable, the main thing is not to waste time. For example, the situation associated with the development of hemolytic disease in the fetus and newborn. Many have heard that in the presence of Rh-negative blood in the mother, it is possible to develop an immunological conflict between the mother and the fetus in the Rh system, which later causes a severe hemolytic disease, from which the baby may already suffer in utero, but few can explain in detail what is it, and what to do if it directly concerns you.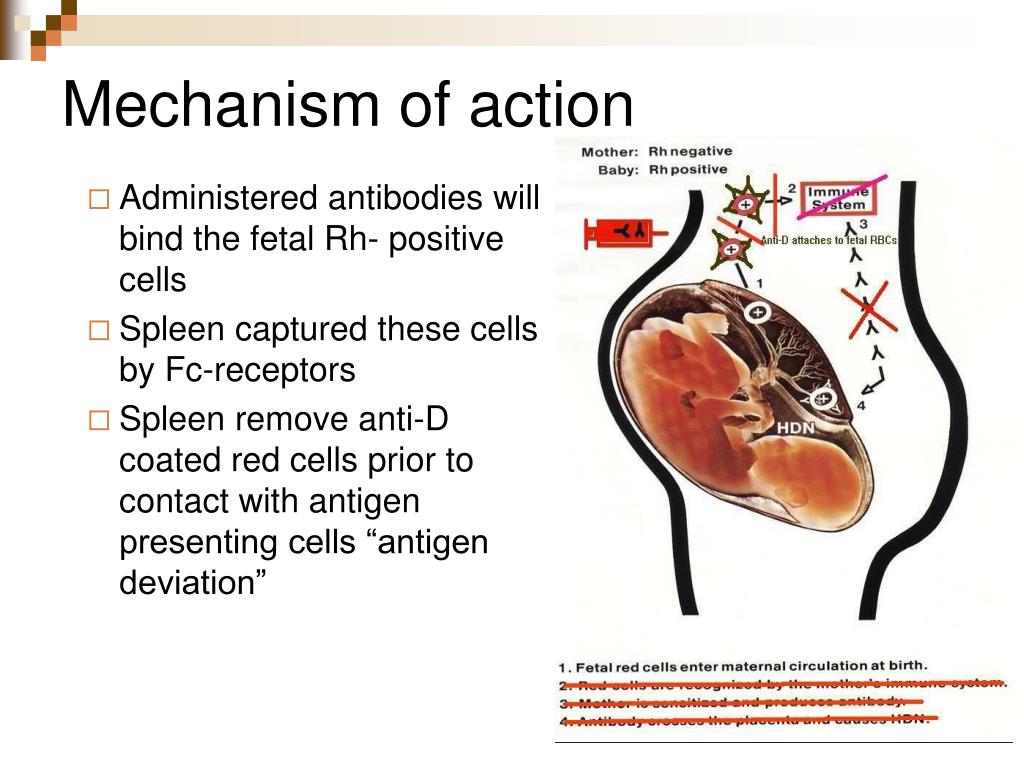
First, let's figure out what the Rh factor is.
Rh factor is a special complex of proteins (also called D-antigen) that is located on the surface of red blood cells. It can be determined by laboratory methods (blood test). Most people in the population have the D antigen. Such people are said to be Rh-positive. A minority of the population (about 15-18%) do not have D antigen in their blood cells; such people are called Rh-negative.
Rh factor is inherited, and a child can inherit it from both mother and father. If the mother is Rh-negative and the father is Rh-positive, there is a high chance that the child will inherit the father's Rh-positive father. Then it turns out that the mother does not have the D-antigen in the blood, but the fetus has it. The mother's immune system can perceive the fetal erythrocytes penetrating into her blood as foreign, and begin to fight them by synthesizing antibodies. These antibodies have a very low molecular weight, are able to cross the placenta into the fetal circulation and destroy fetal red blood cells, causing hemolytic disease in the fetus. Such a pathological condition in which the synthesis of antibodies occurs is called Rh immunization.
Such a pathological condition in which the synthesis of antibodies occurs is called Rh immunization.
Why is Rh immunization dangerous?
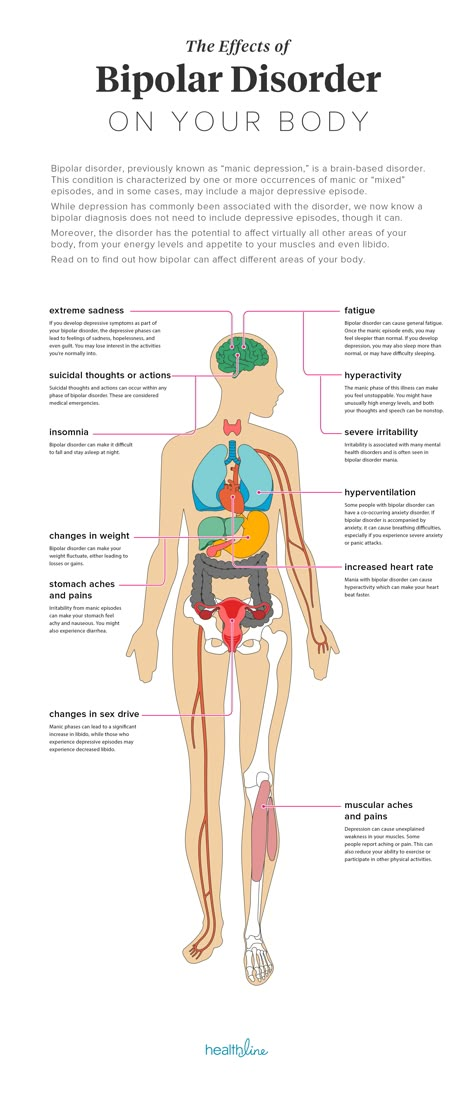
The main role of erythrocytes is the transport of oxygen to the organs and tissues of the body. With the massive destruction of these cells, the organs of the fetus begin to experience oxygen starvation. But that's not all. With the breakdown of red blood cells, a special substance is released - bilirubin, which has a toxic effect on the heart, liver, nervous system of the fetus. Bilirubin turns the baby's skin yellow (“jaundice”). In severe cases, bilirubin, exerting its toxic effect on brain cells, causes irreversible consequences, up to severe disability and death of the baby.
The level of danger increases with each successive pregnancy. The mother’s immune system has the ability to “remember” foreign proteins (Rhesus antigen of the fetus) and, during repeated pregnancy, responds with an even faster and more massive release of antibodies that can very quickly penetrate the placenta into the baby’s bloodstream and lead to severe intrauterine suffering and even death of the baby even before birth.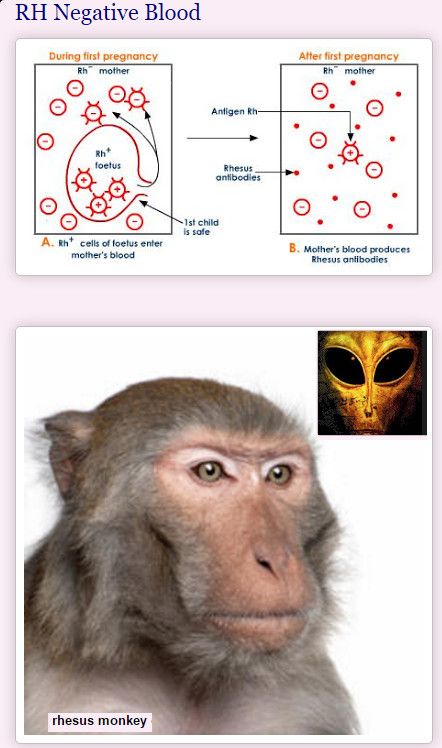
The risk factors for an Rh negative woman are therefore:
- Previous birth of an Rh-positive child (unless a special anti-Rhesus immunoglobulin was administered after the birth)
- Past fetal deaths
- Ectopic pregnancy
- Miscarriages and abortions
- Transfusion of Rh-incompatible blood before pregnancy
The first pregnancy in an Rh-negative woman is usually uneventful. Therefore, there is a tendency to keep the first pregnancy, in no case interrupting it, unless there are serious medical indications for this.
What to do?
Fortunately, it should be noted that worldwide the incidence of hemolytic disease of the fetus in newborns due to Rh conflict is decreasing. And this happens because the methods of Rh prophylaxis are widely introduced into practice, which is carried out for Rh-negative women during pregnancy and after the birth of a Rh-positive baby. Yes, as in the case of all diseases without exception, it is easier to prevent a problem than to treat the consequences of an already developed severe Rh conflict.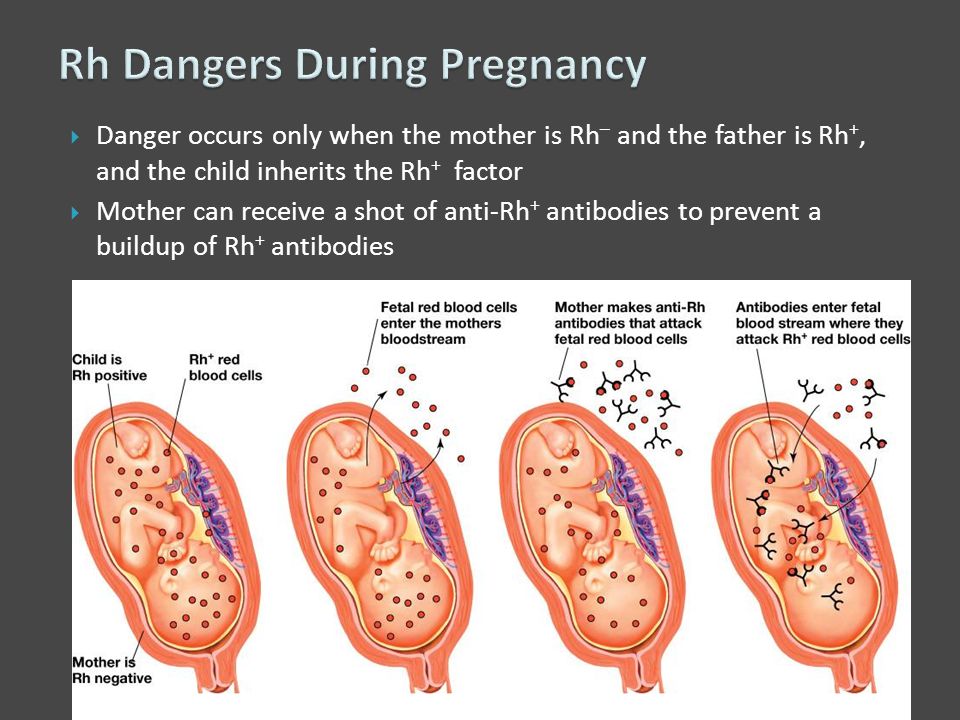
To date, the only (and effective) preventive method to prevent this pathology is the introduction of a special drug - anti-D-immunoglobulin.
Preventive vaccination is carried out twice - during pregnancy (prenatal prophylaxis) and immediately after childbirth (postnatal prophylaxis).
Let's dwell on this in more detail.
The antenatal prophylaxis step aims to protect an existing pregnancy.
If the pregnancy proceeds without complications (“everything goes according to plan”), the woman is given prophylactic administration of anti-D-immunoglobulin at 28-32 weeks of pregnancy. A specially set dose is introduced, which provides protection for the baby until the end of pregnancy. This is planned prenatal prophylaxis.
In the event of dangerous situations that greatly increase the risk of developing a Rh conflict, emergency prenatal prophylaxis is carried out . These situations include:
- Complications of pregnancy: miscarriage; threatened miscarriage with bloody discharge
- Abdominal injury during pregnancy (e.
 g. after a fall or car accident)
g. after a fall or car accident) - Therapeutic and diagnostic interventions during pregnancy: amniocentesis, chorionic biopsy, cordocentesis
In these cases, additional administration of the drug may be required to protect the fetus.
Stage postpartum prophylaxis aims to protect your future pregnancy.
If the baby is found to be Rh-positive after delivery, the mother is given another injection of anti-D-immunoglobulin. The drug should be administered as soon as possible, no later than 72 hours after delivery. If the vaccination is given later, its effectiveness is reduced and you cannot be sure that you did everything that was necessary to protect your next baby.
Attention! Women should receive the same prophylaxis with anti-D-immunoglobulin if:
- a miscarriage occurred at 5-6 weeks of gestation or more
- an abortion was performed at 5-6 weeks of gestation or more
- an operation was performed for an ectopic pregnancy
pregnancy and your unborn child.