Pregnant by ivf
In vitro fertilisation (IVF) | Pregnancy Birth and Baby
In vitro fertilisation (IVF) | Pregnancy Birth and Baby beginning of content12-minute read
Listen
Key facts
- In vitro fertilisation, known as IVF, is a procedure used to help you get pregnant.
- In IVF, a human egg is fertilised with sperm in a laboratory then implanted into a uterus. If the fertilised egg (embryo) successfully implants in the uterus, this will result in pregnancy.
- IVF may be used to treat infertility, to prevent certain genetic problems or to help people who are single or in the sexually- and gender-diverse (LGBTIAQ+) community start a family.
- IVF success rates vary — your doctor can help you understand your chances of becoming pregnant with IVF.
- IVF can be expensive, so it's a good idea to discuss the pros and cons of fertility treatment with your treatment provider and your partner (if you have one) before you start.
What is IVF?
IVF or in vitro fertilisation is a series of procedures to assist you with conception. It is when a human egg is fertilised with sperm in a laboratory. If the fertilised egg (embryo) successfully implants in the uterus, this will result in pregnancy.
What happens during the IVF process?
IVF is a process, with each IVF cycle occurring with one menstrual cycle.
- Blood test: On day one of your menstrual cycle, you will have a blood test with your fertility clinic.
- Hormone stimulation: On day 2 or 3 of your menstrual cycle, your hormone stimulation treatment will start. You will start taking medicine to stimulate your follicles so they produce several eggs.
- Trigger shot: Once your eggs have reached a certain size, you will give yourself an injection containing hormones that trigger your ovary to mature and release an egg.

- Egg retrieval: About 34 to 36 hours after the trigger shot, your eggs will be retrieved (collected). Your fertility specialist will use a thin needle inserted in your vagina wall into the follicles to retrieve the eggs.
- Semen sample: If you are using your partner's fresh sperm, they will provide a semen sample on the same day of the egg collection. If this is not possible, a surgical procedure can help extract sperm directly from the testicles. You may also use frozen donor sperm.
- Fertilisation: Healthy sperm and eggs are brought together on a dish and incubated overnight. In some situations, you may need Intra Cytoplasmic Sperm Injection (ICSI), which is a procedure where a single healthy sperm is injected into a mature egg. This may be helpful when the sperm quality is low.
- Embryo transfer: Around 3 to 5 days after egg retrieval, your fertility specialist will transfer an embryo into your uterus. Usually one embryo is transferred, but sometimes more.
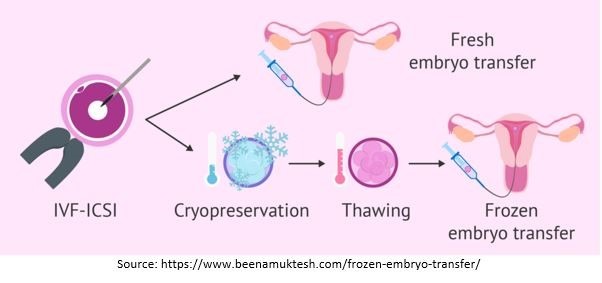
 In some cases your fertility specialist will wait to transfer an embryo. Any good quality embryos that are not transferred might be frozen and used in the future, depending on your individual circumstances.
In some cases your fertility specialist will wait to transfer an embryo. Any good quality embryos that are not transferred might be frozen and used in the future, depending on your individual circumstances. - Pregnancy test: After the embryo is transferred, you will need to wait 2 weeks before you can test for pregnancy. Blood tests are more reliable than a home pregnancy test, so it's best to do this at your fertility clinic or through your GP.
What are the reasons for using IVF?
IVF is used to treat infertility and some genetic problems. It may also help people in the sexually- and gender-diverse (LGBTIAQ+) community start a family, as well as single people who would like to become parents.
You may think about using IVF for a number of reasons, including if you or your partner has:
- low sperm count
- problems with ovulation due to conditions such as polycystic ovary syndrome
- problems with the fallopian tubes
- if either of you have been sterilised
- problems with endometriosis
- a wish to avoid passing on inherited genetic disorders to your children
Some people may choose to use donor sperm or eggs. For example, if a couple is at risk of passing on a serious genetic disorder to their children, they may be advised to use donor sperm or donor eggs.
For example, if a couple is at risk of passing on a serious genetic disorder to their children, they may be advised to use donor sperm or donor eggs.
People who have cancer can sometimes have their healthy eggs or sperm frozen before starting cancer treatment, which can harm their fertility. These eggs or sperm can be thawed later and used in IVF once the cancer treatment is over.
Sexually and gender-diverse people (LGBTIQA+) and single people may also choose to use IVF to build a family.
Should I try other fertility treatments first?
For some people, IVF is the preferred treatment right from the start. Others choose to try other fertility treatments such as fertility drugs, surgery or artificial insemination first. Your doctor can give you more information about the treatment options recommended for you.
What is the success rate of IVF?
Your chance of success with IVF depends on many factors. Some important factors are your age, your partner or donor's age and the cause of infertility. You should ask your doctor or fertility clinic about your own chances of a successful pregnancy and birth.
You should ask your doctor or fertility clinic about your own chances of a successful pregnancy and birth.
That chance is higher if you are younger than 35 years old, and decreases as you get older. By age 44, the chance of success is about 1 in 100.
Some women need 5 cycles of treatment or more to be successful, while others never become pregnant.
Can single or sexually- and gender-diverse people (LGBTIQA+) people use IVF?
Any Australian can use IVF whether they are single or in a partnership.
The situation for LGBTIQA+ people (who may not be infertile) and same-sex couples seeking IVF can vary. For information about IVF that is relevant to your own situation, talk to your doctor or a local fertility clinic.
How much does IVF cost?
IVF is costly and time-consuming. Repeated cycles can take an emotional and physical toll on people going through it, and their family.
Financial costs vary, but each cycle of IVF may cost several thousand dollars. You can get a rebate on some IVF items from Medicare, if they are medically necessary for you to get pregnant. Your private health fund may pay for other aspects of treatment. There are also the costs of medicines, tests and day surgery. You may also need to take time off work while you have treatment.
You can get a rebate on some IVF items from Medicare, if they are medically necessary for you to get pregnant. Your private health fund may pay for other aspects of treatment. There are also the costs of medicines, tests and day surgery. You may also need to take time off work while you have treatment.
If you are considering IVF, it is important to talk to your doctor, the IVF clinic and your private health fund (if you have one) to understand what is covered and any out-of-pocket costs.
How long does IVF take?
IVF takes time. When you are first considering it, you will need to talk to your doctor and get a referral to an IVF clinic or fertility specialist.
You (and your partner) will need to have a number of physical examinations and tests such as ultrasounds, sperm analysis and blood tests before starting any treatment. Even once you start IVF, you will go through a lot of steps involving visits to clinics and laboratories.
If the first cycle is successful, you are on your way. But if not, you may decide to try again with one or more additional cycles. You may be advised to wait a while between cycles, so speak with your fertility specialist and discuss what is best in your circumstances.
But if not, you may decide to try again with one or more additional cycles. You may be advised to wait a while between cycles, so speak with your fertility specialist and discuss what is best in your circumstances.
What are the risks of IVF?
It's important to remember that with IVF there is a risk of not getting pregnant, which can be upsetting and emotionally painful.
Medical risks include that the ovaries may be stimulated too much, which can be serious. This is known as ‘ovarian hyperstimulation syndrome' or OHSS.
Does an IVF pregnancy have more or different risks?All pregnancies carry a risk of complications. There are many factors that may increase the risk of having a pregnancy complication, including older age (over age 38), obesity and smoking.
Females who become pregnant through IVF are more likely to experience these complications during their pregnancy:
- vaginal bleeding
- blood clots in early pregnancy
- high blood pressure
- premature birth
- birth by caesarean section
- having a child with a congenital disorder
The risk of complications will depend on your own situation. You should discuss the risks and benefits of having IVF with your doctor and/or fertility clinic before you start treatment.
You should discuss the risks and benefits of having IVF with your doctor and/or fertility clinic before you start treatment.
Stress and emotional support
Many couples are not successful in their first IVF cycle — you may need a few cycles of treatment, and some couples do not become pregnant at all. This can be an emotional process, especially if you have already been trying to have a baby for a few years. You or your partner may also be receiving hormone medications that can affect your mood, potentially impacting on your emotional and sexual relationship.
You will be offered counselling before you begin treatment. You should also consider ongoing counselling to help cope with any emotional or relationship issues that you or your partner may experience.
Joining a fertility support group can also help you cope with any challenges you may experience during IVF treatment.
How can I find an IVF doctor?
Your doctor can refer you to a fertility specialist, IVF clinic or special hospital unit for treatment.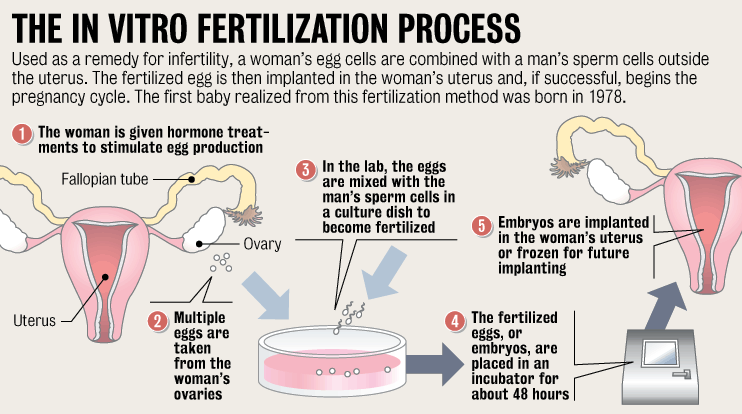 Some public hospital units work in partnership with private clinics.
Some public hospital units work in partnership with private clinics.
The Fertility Society of Australia has a list of accredited assisted reproduction treatment units for different states.
You should discuss treatment options with your doctor or fertility specialist. However, deciding whether to use IVF is a very personal choice. You will need to consider the financial costs as well as the physical and emotional pressures involved.
Questions to ask my IVF doctor
It's a good idea to think about any questions you have about the IVF process and write them down before your appointment.
Here are some questions you might like to ask at your appointment:
- What treatment options are available to me?
- What are the risks and benefits of the treatment plans available?
- Would all IVF procedures be done by my own specialist ?
- What IVF success rate do you have for people of my age and with my condition?
- What tests, treatments and medicines are covered by Medicare or private insurance? Which are not?
- How many cycles of IVF treatment a year are funded by Medicare? Does the practice or clinic manage the claim?
- Do you have a gap agreement with my health fund?
Alternatives to IVF
IVF is a long process that is costly, and a big investment of physical and emotional energy. Some people may find that other options, such as fostering or adopting a child, can help them grow their family. This can be meaningful and rewarding for both the parents and the child.
Some people may find that other options, such as fostering or adopting a child, can help them grow their family. This can be meaningful and rewarding for both the parents and the child.
Where can I get more information and support?
- Visit YourIVFSuccess for information about IVF treatment and success rates in clinics across Australia, and to find an IVF clinic in your area.
- Visit the Victorian Assisted Reproductive Treatment Authority (VARTA) website for helpful information about fertility and fertility treatment including IVF.
- Visit the Fertility Society of Australia and New Zealand (FSANZ) website for information about fertility treatments, and to find accredited IVF clinics in Australia.
- Call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse for advice and support.
Sources:
Australian Institute of Family Studies (AIFS) (Families, policy and the law: Gay and lesbian parenting: the legislative response), Centre of Perinatal Excellence (COPE) (When becoming pregnant isn't easy), Centre of Perinatal Excellence (COPE) (Emotions when going through IVF), Choice (IVF Clinics and Costs), Family Planning NSW (Infertility), Fertility Society of Australia and New Zealand (IVF treatment in Australia and NZ), Fertility Society of Australia and New Zealand (The IVF journey explained), Jean Hailes for Women's Health (Infertility treatment), Victorian Assisted Reproductive Treatment Authority (VARTA) (Fertility treatment explained), Victorian Assisted Reproductive Treatment Authority (VARTA) (Possible health effects of IVF and ICSI), Victorian Assisted Reproductive Treatment Authority (VARTA) (Costs of IVF), Victorian Assisted Reproductive Treatment Authority (VARTA) (Understanding IVF success rates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2022
Back To Top
Related pages
- When to consider IVF
- What to expect from IVF
- Infertility
- Fertility tests and treatments
- Fertility treatments
- Understanding fertility
Need more information?
Storing your sperm (Sperm preservation) | Healthy Male
Semen can be frozen and stored long-term for future use. If you want to father a child at a later stage, the frozen semen is thawed and used in fertility treatments such as in vitro fertilisation (IVF).
Read more on Healthy Male - Andrology Australia website
A male perspective on IVF treatment | VARTA
Ben talks about the effects of IVF and coping strategies
Read more on Victorian Assisted Reproductive Treatment Authority website
A man's guide to going through IVF | Healthy Male
IVF is one of the more widely known forms of assisted reproductive technology — used to overcome a range of fertility issues.
Read more on Healthy Male - Andrology Australia website
IVF can increase the rates of depression, anxiety and stress
COPE's purpose is to prevent and improve the quality of life of those living with emotional and mental health problems that occur prior to and within the perinatal period.
Read more on COPE - Centre of Perinatal Excellence website
How pathology helps IVF parents get pregnant | Know Pathology Know Healthcare
For IVF parents, pathology testing is vital from fertility tests before conception to ensuring a healthy pregnancy
Read more on Know Pathology Know Healthcare website
Fertility treatment explained | VARTA
Understanding fertility treatment There are many types of fertility treatments available, ranging from simple interventions such as medication to help a woman ovulate, through to more complicated procedures known as assisted reproductive treatment (ART). ART, also known as assisted reproductive technology, refers to medical and scientific methods used to help people conceive. Fertility treatments are used: to treat infertility for people who can’t become pregnant, carry a pregnancy or give birth to reduce the chance of a baby inheriting a genetic disease or abnormality to preserve fertility. Types of treatment Depending on the cause of infertility, the following types of treatment may be recommended by your fertility specialist. This information provides a general overview of techniques available. Speak to your fertility clinic for more information. Ovulation induction (OI) Ovulation induction (OI) can be used if a woman is not ovulating or not ovulating regularly. It involves taking a hormone medication (tablets or injections) to stimulate ovulation. The response to the hormones is monitored with ultrasound and when the time is right, an injection is given to trigger ovulation (the release of the egg). Timing intercourse to coincide with ovulation offers the chance of pregnancy.
ART, also known as assisted reproductive technology, refers to medical and scientific methods used to help people conceive. Fertility treatments are used: to treat infertility for people who can’t become pregnant, carry a pregnancy or give birth to reduce the chance of a baby inheriting a genetic disease or abnormality to preserve fertility. Types of treatment Depending on the cause of infertility, the following types of treatment may be recommended by your fertility specialist. This information provides a general overview of techniques available. Speak to your fertility clinic for more information. Ovulation induction (OI) Ovulation induction (OI) can be used if a woman is not ovulating or not ovulating regularly. It involves taking a hormone medication (tablets or injections) to stimulate ovulation. The response to the hormones is monitored with ultrasound and when the time is right, an injection is given to trigger ovulation (the release of the egg). Timing intercourse to coincide with ovulation offers the chance of pregnancy. Artificial insemination or IUI Artificial insemination, which is sometimes called intrauterine insemination (IUI), involves insertion of the male partner’s (or a donor’s) sperm into a woman’s uterus at or just before the time of ovulation. IUI can help couples with so called unexplained infertility or couples where the male partner has minor sperm abnormalities. You can use the Unexplained infertility - exploring your options guide to better understand if IUI is a suitable option for you. IUI can be performed during a natural menstrual cycle, or in combination with ovulation induction (OI) if the woman has irregular menstrual cycles. If a pregnancy is not achieved after a few IUI attempts, IVF or intracytoplasmic sperm injection (ICSI) may be needed. In-vitro fertilisation (IVF) During IVF, the woman has hormone injections to stimulate her ovaries to produce multiple eggs. When the eggs are mature, they are retrieved in an ultrasound-guided procedure under light anaesthetic. The eggs and sperm from the male partner or a donor are placed in a culture dish in the laboratory to allow the eggs to hopefully fertilise, so embryos can develop.
Artificial insemination or IUI Artificial insemination, which is sometimes called intrauterine insemination (IUI), involves insertion of the male partner’s (or a donor’s) sperm into a woman’s uterus at or just before the time of ovulation. IUI can help couples with so called unexplained infertility or couples where the male partner has minor sperm abnormalities. You can use the Unexplained infertility - exploring your options guide to better understand if IUI is a suitable option for you. IUI can be performed during a natural menstrual cycle, or in combination with ovulation induction (OI) if the woman has irregular menstrual cycles. If a pregnancy is not achieved after a few IUI attempts, IVF or intracytoplasmic sperm injection (ICSI) may be needed. In-vitro fertilisation (IVF) During IVF, the woman has hormone injections to stimulate her ovaries to produce multiple eggs. When the eggs are mature, they are retrieved in an ultrasound-guided procedure under light anaesthetic. The eggs and sperm from the male partner or a donor are placed in a culture dish in the laboratory to allow the eggs to hopefully fertilise, so embryos can develop. Three to five days later, if embryos have formed, one is placed into the woman's uterus in a procedure called embryo transfer. If there is more than one embryo, they can be frozen and used later. The IVF process: Is IVF safe? IVF is a safe procedure and medical complications are rare. But as with all medical procedures, there are some possible health effects for women and men undergoing treatment and for children born as a result of treatment. Read more about the possible health effects of IVF here. Understanding IVF success rates Clinics report success rates in different ways, so when comparing clinics’ success rates make sure you compare like with like or ’apples with apples’. Most importantly, you need to consider your own personal circumstances and medical history when you estimate your chance of having a baby with IVF. You can read more about interpreting success rates here. The chance of a live birth following IVF depends on many factors including the woman’s age, the man’s age and the cause of infertility.
Three to five days later, if embryos have formed, one is placed into the woman's uterus in a procedure called embryo transfer. If there is more than one embryo, they can be frozen and used later. The IVF process: Is IVF safe? IVF is a safe procedure and medical complications are rare. But as with all medical procedures, there are some possible health effects for women and men undergoing treatment and for children born as a result of treatment. Read more about the possible health effects of IVF here. Understanding IVF success rates Clinics report success rates in different ways, so when comparing clinics’ success rates make sure you compare like with like or ’apples with apples’. Most importantly, you need to consider your own personal circumstances and medical history when you estimate your chance of having a baby with IVF. You can read more about interpreting success rates here. The chance of a live birth following IVF depends on many factors including the woman’s age, the man’s age and the cause of infertility. Research using the Australian and New Zealand Assisted Reproduction Database calculated the chance of a woman having a baby from her first cycle of IVF according to her age. The results below apply to women who used their own eggs, and it includes the use of frozen embryos produced by one cycle of IVF: Under 34: 44 per cent chance of a live birth 35-39: 31 per cent chance of a live birth 40-44: 11 per cent chance of a live birth 44 and above: one per cent chance of a live birth. Costs of IVF In Australia, Medicare and private health insurers cover some of the costs associated with IVF and ICSI but there are also substantial out-of-pocket costs. The difference between the Medicare contribution and the amount charged by the clinic is the ‘out-of-pocket cost’. These costs vary, depending on the treatment, the fertility clinic and whether a patient has reached the Medicare Safety Net threshold. You can read more about costs here. Intracytoplasmic sperm injection (ICSI) ICSI (intracytoplasmic sperm injection) is used for the same reasons as IVF, but especially to overcome sperm problems.
Research using the Australian and New Zealand Assisted Reproduction Database calculated the chance of a woman having a baby from her first cycle of IVF according to her age. The results below apply to women who used their own eggs, and it includes the use of frozen embryos produced by one cycle of IVF: Under 34: 44 per cent chance of a live birth 35-39: 31 per cent chance of a live birth 40-44: 11 per cent chance of a live birth 44 and above: one per cent chance of a live birth. Costs of IVF In Australia, Medicare and private health insurers cover some of the costs associated with IVF and ICSI but there are also substantial out-of-pocket costs. The difference between the Medicare contribution and the amount charged by the clinic is the ‘out-of-pocket cost’. These costs vary, depending on the treatment, the fertility clinic and whether a patient has reached the Medicare Safety Net threshold. You can read more about costs here. Intracytoplasmic sperm injection (ICSI) ICSI (intracytoplasmic sperm injection) is used for the same reasons as IVF, but especially to overcome sperm problems. ICSI follows the same process as IVF, except ICSI involves the direct injection of a single sperm into each egg to hopefully achieve fertilisation. Because it requires technically advanced equipment, there are additional costs for ICSI. For couples with male factor infertility, ICSI is needed to fertilise the eggs and give them a chance of having a baby. But for couples who don’t have male factor infertility, ICSI offers no advantage over IVF in terms of the chance of having a baby. You can read more about what’s involved in
ICSI follows the same process as IVF, except ICSI involves the direct injection of a single sperm into each egg to hopefully achieve fertilisation. Because it requires technically advanced equipment, there are additional costs for ICSI. For couples with male factor infertility, ICSI is needed to fertilise the eggs and give them a chance of having a baby. But for couples who don’t have male factor infertility, ICSI offers no advantage over IVF in terms of the chance of having a baby. You can read more about what’s involved in
Read more on Victorian Assisted Reproductive Treatment Authority website
The Pink Elephants Support Network - Male Fertility Issues - Pink Elephants
Many people are surprised to learn that men actually account for 30% of infertility in couples
Read more on Pink Elephants Support Network website
Fertility treatment journey | VARTA
Things to consider Possible emotional effects of fertility treatments Fertility treatments are psychologically and emotionally demanding
Read more on Victorian Assisted Reproductive Treatment Authority website
The Pink Elephants Support Network - Letting Go and Moving Forward After Miscarriage
For some couples, the quest for a baby, or another baby, can be a very long, very challenging road
Read more on Pink Elephants Support Network website
How pregnancy happens - Body Talk
For a woman to become pregnant an egg must be fertilised by a sperm
Read more on Body Talk website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
In vitro fertilization (IVF) - Mayo Clinic
Overview
In vitro fertilization
In vitro fertilization
During in vitro fertilization, eggs are removed from mature follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg (embryo) is transferred into the uterus (C).
The fertilized egg (embryo) is transferred into the uterus (C).
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using a couple's own eggs and sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. In addition, IVF can be time-consuming, expensive and invasive. If more than one embryo is transferred to the uterus, IVF can result in a pregnancy with more than one fetus (multiple pregnancy).
Your doctor can help you understand how IVF works, the potential risks and whether this method of treating infertility is right for you.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Fertility and Conception
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
In vitro fertilization (IVF) is a treatment for infertility or genetic problems. If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in the uterus near the time of ovulation.
If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in the uterus near the time of ovulation.
Sometimes, IVF is offered as a primary treatment for infertility in women over age 40. IVF can also be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.

- Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy. If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
- Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg.
 If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns. - Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found. Embryos that don't contain identified problems can be transferred to the uterus.
-
Fertility preservation for cancer or other health conditions. If you're about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option.
 Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman's eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier's uterus.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
Risks of IVF include:
- Multiple births. IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.

- Premature delivery and low birth weight. Research suggests that IVF slightly increases the risk that the baby will be born early or with a low birth weight.
-
Ovarian hyperstimulation syndrome. Use of injectable fertility drugs, such as human chorionic gonadotropin (HCG), to induce ovulation can cause ovarian hyperstimulation syndrome, in which your ovaries become swollen and painful.
Symptoms typically last a week and include mild abdominal pain, bloating, nausea, vomiting and diarrhea. If you become pregnant, however, your symptoms might last several weeks. Rarely, it's possible to develop a more severe form of ovarian hyperstimulation syndrome that can also cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15% to 25% — but the rate increases with maternal age.

- Egg-retrieval procedure complications. Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also associated with sedation and general anesthesia, if used.
- Ectopic pregnancy. About 2% to 5% of women who use IVF will have an ectopic pregnancy — when the fertilized egg implants outside the uterus, usually in a fallopian tube. The fertilized egg can't survive outside the uterus, and there's no way to continue the pregnancy.
- Birth defects. The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived. More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects.
- Cancer. Although some early studies suggested there may be a link between certain medications used to stimulate egg growth and the development of a specific type of ovarian tumor, more-recent studies do not support these findings.
 There does not appear to be a significantly increased risk of breast, endometrial, cervical or ovarian cancer after IVF.
There does not appear to be a significantly increased risk of breast, endometrial, cervical or ovarian cancer after IVF. - Stress. Use of IVF can be financially, physically and emotionally draining. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
How you prepare
The Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about U.S. clinics' individual pregnancy and live birth rates.
A clinic's success rate depends on many factors. These include patients' ages and medical issues, as well as the clinic's treatment population and treatment approaches. Ask for detailed information about the costs associated with each step of the procedure.
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
- Ovarian reserve testing.
 To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen) and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results, often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication.
To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen) and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results, often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication. - Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.

- Uterine exam. Your doctor will examine the inside lining of the uterus before you start IVF. This might involve a sonohysterography — in which fluid is injected through the cervix into your uterus — and an ultrasound to create images of your uterine cavity. Or it might include a hysteroscopy — in which a thin, flexible, lighted telescope (hysteroscope) is inserted through your vagina and cervix into your uterus.
Before beginning a cycle of IVF, consider important questions, including:
-
How many embryos will be transferred? The number of embryos transferred is typically based on age and number of eggs retrieved. Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.
Most doctors follow specific guidelines to prevent a higher order multiple pregnancy, such as triplets or more.
 In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your doctor agree on the number of embryos that will be transferred before the transfer procedure.
In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your doctor agree on the number of embryos that will be transferred before the transfer procedure. -
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for several years. Not all embryos will survive the freezing and thawing process, although most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or, you might be able to donate unused frozen embryos to another couple or a research facility. You might also choose to discard unused embryos.
- How will you handle a multiple pregnancy? If more than one embryo is transferred to your uterus, IVF can result in a multiple pregnancy — which poses health risks for you and your babies.
 In some cases, fetal reduction can be used to help a woman deliver fewer babies with lower health risks. Pursuing fetal reduction, however, is a major decision with ethical, emotional and psychological consequences.
In some cases, fetal reduction can be used to help a woman deliver fewer babies with lower health risks. Pursuing fetal reduction, however, is a major decision with ethical, emotional and psychological consequences. - Have you considered the potential complications associated with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You may also need an attorney to file court papers to help you become legal parents of an implanted embryo.
What you can expect
IVF involves several steps — ovarian stimulation, egg retrieval, sperm retrieval, fertilization and embryo transfer. One cycle of IVF can take about two to three weeks. More than one cycle may be needed.
Ovulation induction
The start of an IVF cycle begins by using synthetic hormones to stimulate the ovaries to produce multiple eggs — rather than the single egg that typically develops each month. Multiple eggs are needed because some eggs won't fertilize or develop normally after fertilization.
Multiple eggs are needed because some eggs won't fertilize or develop normally after fertilization.
Several different medications may be used, such as:
- Medications for ovarian stimulation. To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both. These medications stimulate more than one egg to develop at a time.
- Medications for oocyte maturation. When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.
- Medications to prevent premature ovulation. These medications prevent your body from releasing the developing eggs too soon.
- Medications to prepare the lining of your uterus. On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation.

Your doctor will work with you to determine which medications to use and when to use them.
Typically, you'll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, you may have:
- Vaginal ultrasound, an imaging exam of your ovaries to monitor the development of follicles — fluid-filled ovarian sacs where eggs mature
- Blood tests, to measure your response to ovarian stimulation medications — estrogen levels typically increase as follicles develop, and progesterone levels remain low until after ovulation
Sometimes IVF cycles need to be canceled before egg retrieval for one of these reasons:
- Inadequate number of follicles developing
- Premature ovulation
- Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome
- Other medical issues
If your cycle is canceled, your doctor might recommend changing medications or their doses to promote a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Or you may be advised that you need an egg donor.
Egg retrieval
Egg retrieval can be done in your doctor's office or a clinic 34 to 36 hours after the final injection and before ovulation.
- During egg retrieval, you'll be sedated and given pain medication.
- Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs.
- If your ovaries aren't accessible through transvaginal ultrasound, an abdominal ultrasound may be used to guide the needle.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After egg retrieval, you may experience cramping and feelings of fullness or pressure.
- Mature eggs are placed in a nutritive liquid (culture medium) and incubated.
 Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be provided at your doctor's office or clinic the morning of egg retrieval. Typically, the semen sample is collected through masturbation. Other methods, such as testicular aspiration — the use of a needle or surgical procedure to extract sperm directly from the testicle — are sometimes required. Donor sperm also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Fertilization can be attempted using two common methods:
- Conventional insemination. During conventional insemination, healthy sperm and mature eggs are mixed and incubated overnight.
- Intracytoplasmic sperm injection (ICSI). In ICSI, a single healthy sperm is injected directly into each mature egg.
 ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
In certain situations, your doctor may recommend other procedures before embryo transfer.
- Assisted hatching. About five to six days after fertilization, an embryo "hatches" from its surrounding membrane (zona pellucida), allowing it to implant into the lining of the uterus. If you're an older woman, or if you have had multiple failed IVF attempts, your doctor might recommend assisted hatching — a technique in which a hole is made in the zona pellucida just before transfer to help the embryo hatch and implant. Assisted hatching is also useful for eggs or embryos that have been previously frozen as the process can harden the zona pellucida.
- Preimplantation genetic testing.
 Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryo transfer
Egg-retrieval technique
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into your vagina to identify follicles, and a needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
ICSI
ICSI
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
Blastocyst
Blastocyst
Three days after fertilization, a normally developing embryo will contain about six to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
Embryo transfer is done at your doctor's office or a clinic and usually takes place two to five days after egg retrieval.
- You might be given a mild sedative. The procedure is usually painless, although you might experience mild cramping.
- The doctor will insert a long, thin, flexible tube called a catheter into your vagina, through your cervix and into your uterus.
- A syringe containing one or more embryos suspended in a small amount of fluid is attached to the end of the catheter.

- Using the syringe, the doctor places the embryo or embryos into your uterus.
If successful, an embryo will implant in the lining of your uterus about six to 10 days after egg retrieval.
After the procedure
After the embryo transfer, you can resume your usual daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity, which could cause discomfort.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure — due to the swabbing of the cervix before the embryo transfer
- Breast tenderness due to high estrogen levels
- Mild bloating
- Mild cramping
- Constipation
If you develop moderate or severe pain after the embryo transfer, contact your doctor. He or she will evaluate you for complications such as infection, twisting of an ovary (ovarian torsion) and severe ovarian hyperstimulation syndrome.
Results
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you're pregnant.
- If you're pregnant, your doctor will refer you to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. If you don't get your period or you have unusual bleeding, contact your doctor. If you're interested in attempting another cycle of in vitro fertilization (IVF), your doctor might suggest steps you can take to improve your chances of getting pregnant through IVF.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF.
 Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success.
Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success. - Embryo status. Transfer of embryos that are more developed is associated with higher pregnancy rates compared with less-developed embryos (day two or three). However, not all embryos survive the development process. Talk with your doctor or other care provider about your specific situation.
- Reproductive history. Women who've previously given birth are more likely to be able to get pregnant using IVF than are women who've never given birth. Success rates are lower for women who've previously used IVF multiple times but didn't get pregnant.
- Cause of infertility. Having a normal supply of eggs increases your chances of being able to get pregnant using IVF.
 Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility.
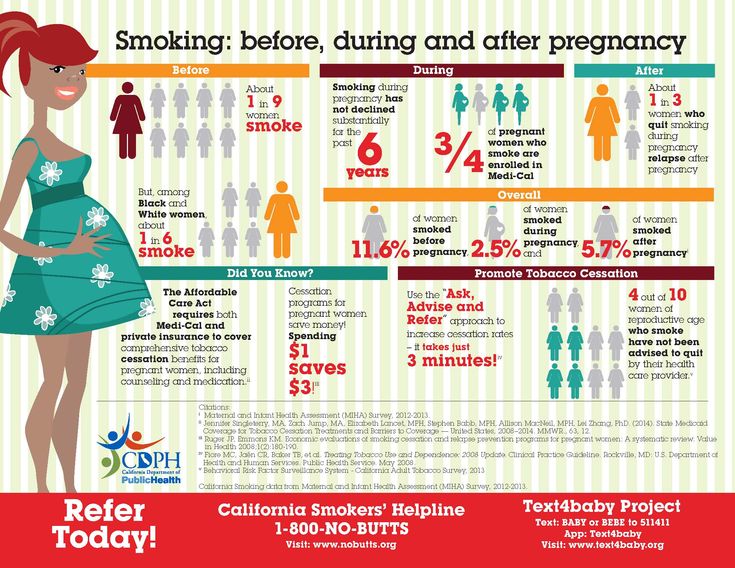
Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility. - Lifestyle factors. Women who smoke typically have fewer eggs retrieved during IVF and may miscarry more often. Smoking can lower a woman's chance of success using IVF by 50%. Obesity can decrease your chances of getting pregnant and having a baby. Use of alcohol, recreational drugs, excessive caffeine and certain medications also can be harmful.
Talk with your doctor about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
How to maintain a pregnancy after IVF - recommendations from leading reproductologists at the Liniya Zhizni clinic in Moscow
home
/ Articles
/ How to keep pregnant after IVF
Pregnancy after IVF often comes with complications..jpg) This is because women who have diseases of the endocrine system and the genital area resort to in vitro fertilization. They often experience miscarriage, toxicosis and other problems that put pregnancy at risk. To prevent this and keep the pregnancy after IVF, you need to be observed in a clinic that has the necessary equipment and qualified specialists working with IVF mothers. nine0003
This is because women who have diseases of the endocrine system and the genital area resort to in vitro fertilization. They often experience miscarriage, toxicosis and other problems that put pregnancy at risk. To prevent this and keep the pregnancy after IVF, you need to be observed in a clinic that has the necessary equipment and qualified specialists working with IVF mothers. nine0003
Hormonal disorders during pregnancy after IVF
These problems are caused by the introduction of large doses of hormones in the preparation for IVF, if hormonal ovarian stimulation was performed. For many women, hormone therapy for IVF is a necessity and the only way to get pregnant, since stimulation of the ovaries leads to the maturation of several follicles at once. This sharply increases the concentration of estrogen in the blood. Hormonal failure can cause impaired vascular permeability and fluid accumulation in the lungs and abdominal cavity. Excess moisture prevents a woman from breathing, causes nausea, vomiting and loss of appetite.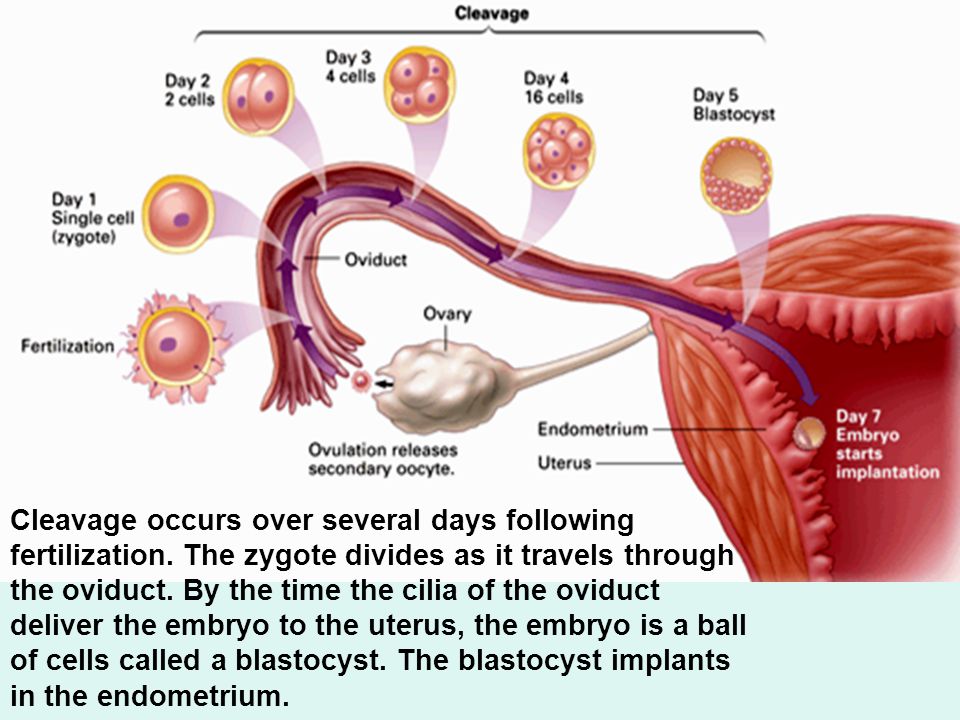 nine0003
nine0003
Another possible consequence of HS is a slow rise in hCG (human chorionic gonadotropin), which is called the “pregnancy hormone”. This hormone must:
- preserve the corpus luteum;
- prepare a woman's immune system for an upcoming pregnancy;
- stimulate fetal development
With a lack of hCG, the growth of the fetus slows down, which leads to miscarriage and fading of pregnancy.
Pregnancy support after IVF is simply necessary in this case. When observed in a specialized clinic, doctors will be able to correct the hormonal background in time, remove puffiness and eliminate the threat of miscarriage.
Infectious and inflammatory processes
Women who become pregnant through IVF often suffer from chronic inflammation of the genital organs, which lead to the impossibility of natural conception. Although women are treated as much as possible during the period of preparation for pregnancy, the diseases often become aggravated again. All this affects the functioning of the immune system and a decrease in the production of hormones responsible for the normal course of pregnancy. nine0003
All this affects the functioning of the immune system and a decrease in the production of hormones responsible for the normal course of pregnancy. nine0003
A woman develops a bloody "daub" indicating a threatened interruption. It is not easy for the fetus to stay in the uterus under these conditions, so medical support for pregnancy after IVF is required. Medical supervision helps to eliminate dangerous inflammatory processes, keeping the pregnancy after IVF.
Maternal problems
IVF is mainly used by women aged 30 and older. A large percentage of them have various diseases of internal organs (kidneys, heart, liver, gallbladder) and metabolic disorders. All these "sores" are prone to exacerbations during pregnancy, which negatively affects the intrauterine development of the child. nine0003
Women with pre-existing health problems may develop gestational diabetes due to a malfunctioning pancreas. The level of glucose in the blood rises, which causes oxygen starvation of the fetus. This complication often occurs if a woman is carrying twins, which often happens after artificial insemination. If the violations that have arisen are not treated in time, the pregnancy can be lost. To do this, women, being observed in the clinic after IVF, regularly donate blood for biochemistry and sugar. nine0003
This complication often occurs if a woman is carrying twins, which often happens after artificial insemination. If the violations that have arisen are not treated in time, the pregnancy can be lost. To do this, women, being observed in the clinic after IVF, regularly donate blood for biochemistry and sugar. nine0003
Fetoplacental insufficiency
This condition results from abnormal formation and/or insufficiency of the placenta. Since women who become pregnant after IVF often have problems in the genital area, fetoplacental disorders are not uncommon for them.
As a result, the fetus suffers, which gets little nutrition and oxygen, which can lead to miscarriage or the birth of a sick child. To help with this condition, the periodic appointment of dopplerometry, showing the state of the fetal-placental blood flow, can help. If a pathology is suspected, pregnancy support after IVF involves the appointment of drugs that improve blood circulation in the placenta and help the pregnancy to proceed properly. nine0003
nine0003
Multiple pregnancy
During IVF, a woman often receives several embryos at once. If all of them take root, a multiple pregnancy occurs. Sometimes twins develop from one egg, as in a normal pregnancy, a woman gives birth to identical twins. Many consider twins or triplets to be a great result after IVF, forgetting that multiple babies are harder to bear and easier to lose.
Sometimes nature itself regulates the process, and extra embryos stop developing, but often all implanted eggs grow the same way. It is possible, of course, to carry out a reduction (removal) of superplanned embryos, but parents rarely agree to this. nine0003
In women pregnant with twins, toxicosis occurs more often and is more severe. The uterus, growing much faster, puts pressure on the legs, causing them to swell. The pressure on the diaphragm in recent months interferes with the full breathing of the mother. In the later stages of pregnancy with twins or triplets, an increase in pressure is more often observed, which can lead to convulsive syndrome (eclampsia) and premature birth. Since twins are already born with a small weight, this can lead to deep prematurity and death of newborns. nine0003
Since twins are already born with a small weight, this can lead to deep prematurity and death of newborns. nine0003
Overdistension of the uterus and increased stress on the body cause:
- bleeding;
- fetal anoxia;
- anemia caused by a high load on the hematopoietic system of the mother;
- feto-fetal transfusion syndrome, when one fetus takes more nutrients, inhibiting the development of the second;
- thrombosis of placental vessels. With multiple pregnancies, one or both "children's places" are located incorrectly, which causes premature placental detachment; nine0018
- oblique, transverse or pelvic position in the uterus of one or all babies
A woman who has a multiple pregnancy as a result of IVF needs special supervision and strict control, so she is more likely to have an ultrasound scan to find out how the babies are developing.
The condition of babies born by IVF mothers is monitored using ultrasound and dopplerometry. Competent doctors working at the Liniya Zhizni clinic will provide full support for pregnancy after IVF and will help you successfully endure multiple pregnancies and give birth to healthy babies. The conscious attitude of a woman and the supervision of experienced specialists allows saving the majority of pregnancies that occur after IVF. nine0075
Competent doctors working at the Liniya Zhizni clinic will provide full support for pregnancy after IVF and will help you successfully endure multiple pregnancies and give birth to healthy babies. The conscious attitude of a woman and the supervision of experienced specialists allows saving the majority of pregnancies that occur after IVF. nine0075
03/14/2021
Author of the article
Expert Council of the Life Line Reproduction Center
You may also be interested in
Pregnancy management programs
We have 3 pregnancy management programs, which are selected taking into account the health of the expectant mother and in accordance with the recommendations of the Ministry of Health. nine0003
Pregnancy management after IVF
Pregnancy after IVF, as well as that which occurred by natural conception, needs careful monitoring by doctors
Pregnancy management at the Life Line reproduction center
nine0002 Regular visits to an experienced obstetrician-gynecologist, which are accompanied by a complex of diagnostic and control studies, help to minimize the anxieties, fears and risks associated with pregnancy I want to express my deep gratitude to the most sensitive, attentive doctor Falaleeva Larisa Nikolaevna, this is our fairy who works miracles, thanks to her we became parents for the second time on December 30, 2022, our second boy was born). Before meeting Larisa Nikolaevna, we no longer believed that maybe something will turn out, 5 protocols and no dynamics, but after meeting with her everything changed, I am a mother of two with ...
Before meeting Larisa Nikolaevna, we no longer believed that maybe something will turn out, 5 protocols and no dynamics, but after meeting with her everything changed, I am a mother of two with ...
January 12, 2023
January 12, 2023
Specialist
Falaleeva Larisa Nikolaevna
Many thanks to Kalinina Natalya Gennadievna, embryologists and all the specialists of the clinic! Continued success to all! In April 2022, the cryotransfer of my only past PGD embryo took place. The chances at my age were low, especially since the first transfer. But a miracle happened and the pregnancy came! And on December 21, 2022, my son was born!
December 30, 2022
Specialist
Kalinina Natalya Gennadievna
I came to Diana Malkhazovna after 3 unsuccessful IVFs under compulsory medical insurance and after 5 years of planning. I started treatment with her back in St. Petersburg, then I continued to go to the doctor in Moscow. We had a plan and after each stage we corrected something.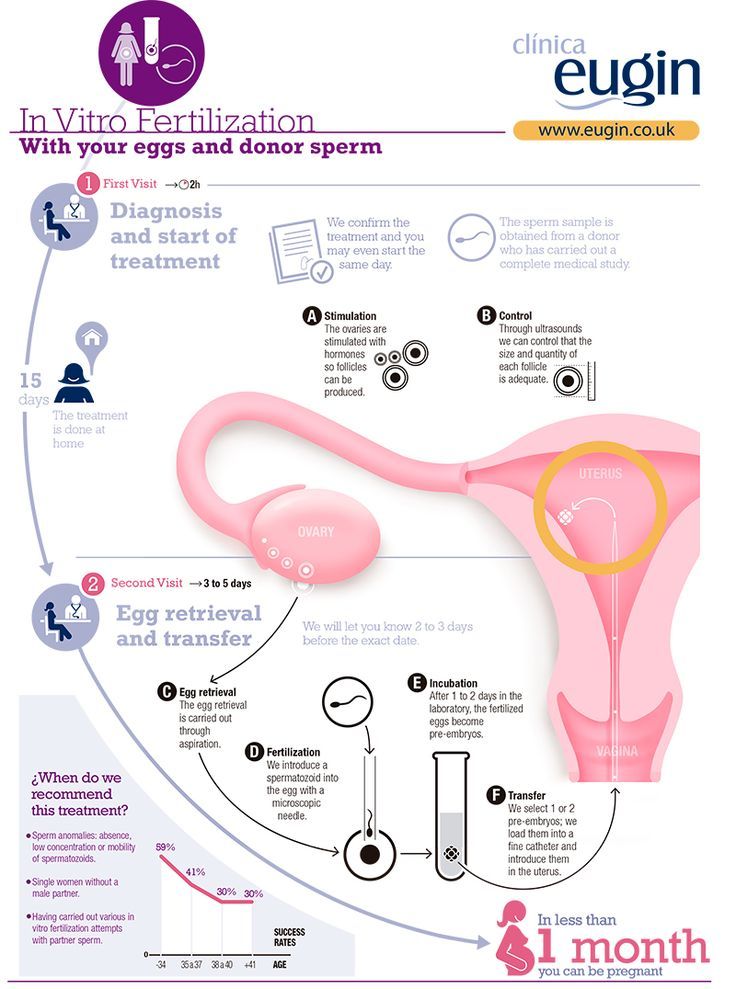 There was a moment when I stopped believing in success, but Diana Malkhazovna did not for a minute let me doubt my ability to get pregnant on my own ...
There was a moment when I stopped believing in success, but Diana Malkhazovna did not for a minute let me doubt my ability to get pregnant on my own ...
December 30, 2022
December 30, 2022
Specialist
Diana Malkhazovna Obidnyak
Make an appointment
Name *
Telephone *
Message
By clicking on the button, you consent to the processing of your personal data. This site is protected by reCaptcha, to which the Google Privacy Policy and Terms of Service apply. nine0003
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and Child" Lefortovo
All directionsEco DepartmentEco services
01.