Pregnancy and lead exposure
Lead Screening During Pregnancy and Lactation
Number 533 (Reaffirmed 2019)
Committee on Obstetric Practice
This document reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed.
Abstract: Prenatal lead exposure has known adverse effects on maternal health and infant outcomes across a wide range of maternal blood lead levels. Adverse effects of lead exposure are being identified at lower levels of exposure than previously recognized in both children and adults. In 2010, the Centers for Disease Control and Prevention issued the first guidelines regarding the screening and management of pregnant and lactating women who have been exposed to lead.
Prenatal lead exposure has known adverse effects on maternal health and infant outcomes across a wide range of maternal blood lead levels 1. Adverse effects of lead exposure are being identified at lower levels of exposure than previously recognized in both children and adults 2 3 4 5 6 7. In 2010, the Centers for Disease Control and Prevention issued the first guidelines regarding the screening and management of pregnant and lactating women who have been exposed to lead 8.
Background
Environmental policies and public health education programs have led to significant reductions in cases of lead exposure in the United States 9. Despite these improvements, approximately 1% of women of childbearing age (15–49 years) have blood lead levels greater than or equal to 5 micrograms/dL 8.
Although no threshold has been found to trigger the adverse health effects of lead 8, in nonpregnant adults blood lead levels less than 5 micrograms/dL are considered normal, blood lead levels between 5 micrograms/dL and 10 micrograms/dL require follow-up, and blood lead levels greater than 10 micrograms/dL are managed with environmental assessment and abatement of exposures. Chelation therapy is considered at blood lead levels greater than 40 micrograms/dL for symptomatic individuals, and levels greater than 70 micrograms/dL are considered a medical emergency. In children, treatment is recommended at blood lead levels of 45 micrograms/dL or greater.
Chelation therapy is considered at blood lead levels greater than 40 micrograms/dL for symptomatic individuals, and levels greater than 70 micrograms/dL are considered a medical emergency. In children, treatment is recommended at blood lead levels of 45 micrograms/dL or greater.
The main target for lead toxicity is the nervous system, both in adults and children 10. High levels of exposure can result in delirium, seizures, stupor, coma, or even death. Other overt signs and symptoms of lead toxicity may include hypertension, peripheral neuropathy, ataxia, tremor, headache, loss of appetite, weight loss, fatigue, muscle and joint aches, changes in behavior and concentration, gout, nephropathy, lead colic, and anemia. Health effects of chronic low-level exposure in adults include cognitive decline, hypertension and other cardiovascular effects, decrements in renal function, and adverse reproductive outcome. The developing nervous systems in children make them more susceptible to the neurologic effects of lead toxicity.
Adverse Health Effects of Prenatal Exposure
Lead readily crosses the placenta by passive diffusion and has been detected in the fetal brain as early as the end of the first trimester 8. Elevated lead levels in pregnancy have been associated with several adverse outcomes, including gestational hypertension, spontaneous abortion, low birth weight, and impaired neurodevelopment 11 12 13 14.
Lead exposure has been associated with an increased risk of gestational hypertension, but the magnitude of the effect, the exposure level at which risk begins to increase, and whether risk is most associated with acute or cumulative exposure remain uncertain. Also, it is unclear whether lead-induced increases in blood pressure during pregnancy lead to severe hypertension or preeclampsia 11 15 16 17 18.
Evidence shows that maternal exposure to high levels of lead increases the risk of spontaneous abortion 19. However, data for an association between low or moderate lead levels and spontaneous abortion are inconsistent. The strongest available evidence comes from a prospective study of 668 pregnant women in Mexico City that demonstrated a statistically significant dose–response relationship between low-to-moderate maternal blood lead levels and the risk of spontaneous abortion 12. Yet, another longitudinal study of 351 women in Japan showed no difference in blood lead levels between spontaneous abortion cases (n=15) and ongoing pregnancies 20. Larger prospective studies are needed to further clarify the effects of low and moderate levels of lead on spontaneous abortion risk.
The strongest available evidence comes from a prospective study of 668 pregnant women in Mexico City that demonstrated a statistically significant dose–response relationship between low-to-moderate maternal blood lead levels and the risk of spontaneous abortion 12. Yet, another longitudinal study of 351 women in Japan showed no difference in blood lead levels between spontaneous abortion cases (n=15) and ongoing pregnancies 20. Larger prospective studies are needed to further clarify the effects of low and moderate levels of lead on spontaneous abortion risk.
More recent and well-designed studies suggest that maternal lead exposure during pregnancy is inversely related to fetal growth, as reflected by duration of pregnancy and infant size. One study that used a registry-based approach found that offspring of mothers occupationally exposed to lead had an increased risk of low birth weight (relative risk [RR], 1.34; confidence interval [CI], 1.12–1.6) compared with infants of women not exposed to lead 13. A case–control study in Mexico City found umbilical cord blood lead levels to be higher in preterm infants (mean value, 9.8 micrograms/dL) compared with term infants (mean value, 8.4 micrograms/dL) 21. A birth cohort study, also conducted in Mexico City, found maternal bone lead burden to be inversely related to offspring weight 22, length, and head circumference at birth 23.
A case–control study in Mexico City found umbilical cord blood lead levels to be higher in preterm infants (mean value, 9.8 micrograms/dL) compared with term infants (mean value, 8.4 micrograms/dL) 21. A birth cohort study, also conducted in Mexico City, found maternal bone lead burden to be inversely related to offspring weight 22, length, and head circumference at birth 23.
A large number of studies provide evidence that prenatal lead exposure impairs children’s neurodevelopment. Some prospective studies have included children with low levels of prenatal lead exposure and continue to detect inverse associations with neurodevelopment, although these data are less consistent than those related to the high levels of lead exposure. In one study, each 1 microgram/dL increase in umbilical cord blood lead was found to be associated with a reduction of 0.6 points in the mental development index scores of the Bayley Scales of Infant Development at age 3 months, with similar results at age 6 months 14 24. However, another prospective cohort study found that the relationship between prenatal blood lead levels and early childhood IQ is not linear, with the strongest postnatal effects noted at low levels of prenatal exposure 25. The available data are inadequate to establish the presence or absence of an association between maternal lead exposure and major congenital anomalies in the fetus.
However, another prospective cohort study found that the relationship between prenatal blood lead levels and early childhood IQ is not linear, with the strongest postnatal effects noted at low levels of prenatal exposure 25. The available data are inadequate to establish the presence or absence of an association between maternal lead exposure and major congenital anomalies in the fetus.
Lead Exposure During Breastfeeding
Although the benefits of breastfeeding generally outweigh the risks of environmental exposure, the effects of breastfeeding on infant lead levels have been studied. Lead has been detected in the breast milk of women in population-based studies; however, the availability of high-quality data to assess the risk for toxicity to the breastfeeding infant is limited 8. Although infant blood lead levels have been correlated with the duration of breastfeeding 26, the ratio of breast milk lead levels to blood lead levels has been found to be less than 3% 27. According to the American Academy of Pediatrics, because of the contribution of lead levels found in infant formula and other infant foods, breastfed infants of mothers with normal blood lead levels are actually exposed to slightly less lead than if they were not breastfed 28.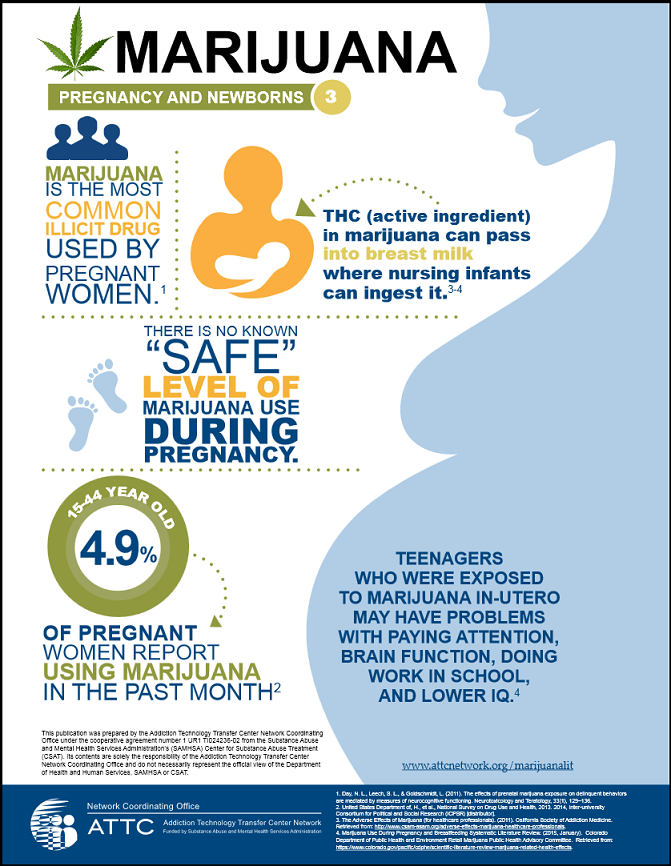
Screening and Management
Pregnancy
The Centers for Disease Control and Prevention (CDC) and the American College of Obstetricians and Gynecologists do not recommend blood lead testing of all pregnant women in the United States. Obstetric health care providers should consider the possibility of lead exposure in individual pregnant women by evaluating risk factors for exposure as part of a comprehensive health risk assessment and perform blood lead testing if a single risk factor is identified. Assessment of lead exposure should take place at the earliest contact with the pregnant patient.
Important risk factors for lead exposure in pregnant women are listed in Box 1. Lead-based paint is less likely to be an important exposure source for pregnant women than it is for children, except during renovation or remodeling in older homes. Women should take precautions when repainting surfaces with deteriorated paint or performing any remodeling or renovation work that disturbs painted surfaces, such as scraping off paint or tearing out walls 8.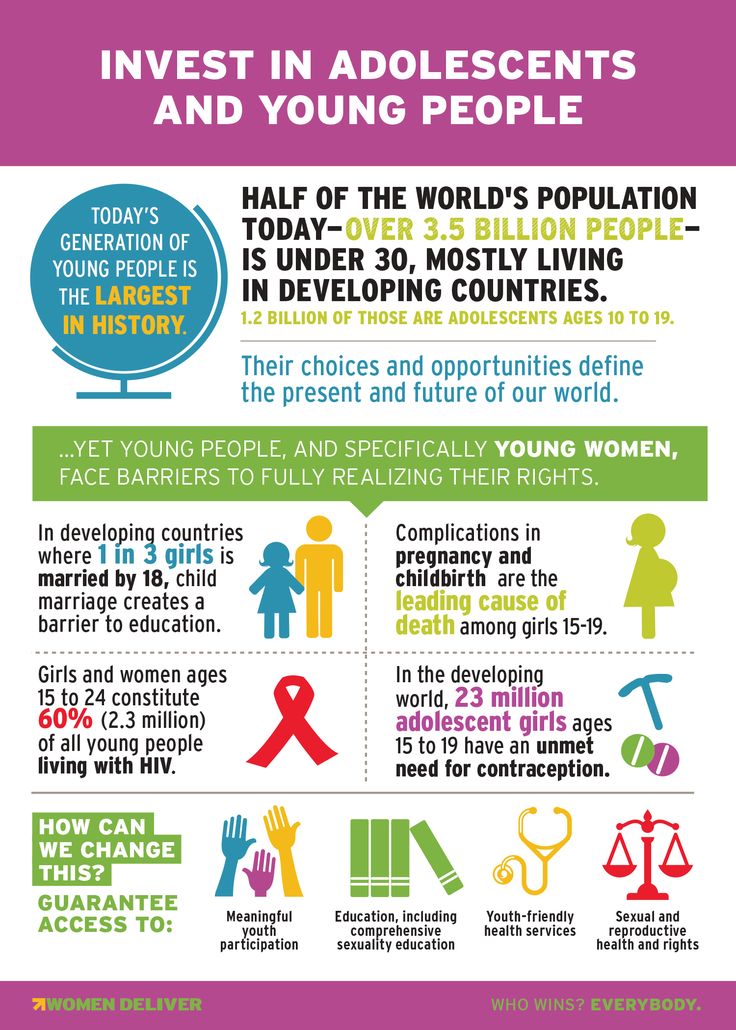
For pregnant women with blood lead levels of 5 micrograms/dL or higher, sources of lead exposure should be identified and women should receive counseling regarding avoidance of further exposure. Confirmatory and follow-up blood lead testing should be performed in accordance with the CDC’s recommended schedules Table 1 and maternal or umbilical cord blood lead levels should be measured at delivery 8. Women with confirmed blood lead levels of 45 micrograms/dL or more should be treated in consultation with clinicians experienced in the management of lead toxicity and high-risk pregnancy. Once the source of lead exposure is identified and eliminated, the initial decrease in blood lead level occurs relatively rapidly because of lead’s short (35-day) initial half-life in blood 29. This initial rapid decrease is followed by a slow, continuous decrease over several months to several years because of mobilization of lead from stores in the bone 8. Recommendations for the frequency of blood lead follow-up tests are included in Table 1.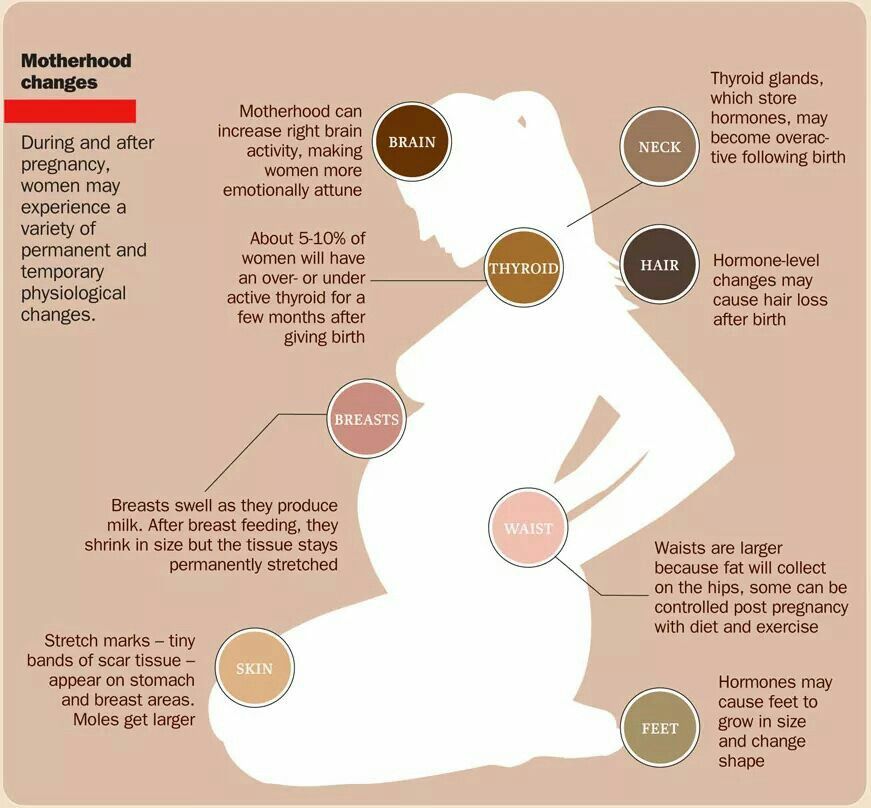
Adequate dietary intake of calcium, iron, zinc, vitamin C, vitamin D, and vitamin E is known to decrease lead absorption 30 31. Iron-deficiency anemia is associated with elevated blood lead levels and may increase lead absorption. During pregnancy and lactation, lead from prior exposures can be mobilized from bones because of the increased bone turnover. Pregnant and lactating women with a current or past blood lead level of 5 micrograms/dL or higher should receive specific nutritional recommendations regarding calcium and iron supplementation. A balanced diet that contains 2,000 mg of calcium and 60–120 mg of iron daily is recommended 8. This can be achieved through either food intake or supplementation. Supplements should be divided into doses of 500 mg of calcium and 60 mg of iron to improve absorption.
Risk Factors for Lead Exposure in Pregnant and Lactating Women
Recent emigration from or residency in areas where ambient lead contamination is high—women from countries where leaded gasoline is still being used (or was recently phased out) or where industrial emissions are not well controlled.
Living near a point source of lead—examples include lead mines, smelters, or battery recycling plants (even if the establishment is closed).
Working with lead or living with someone who does—women who work in or who have family members who work in an industry that uses lead (eg, lead production, battery manufacturing, paint manufacturing, ship building, ammunition production, or plastic manufacturing).
Using lead-glazed ceramic pottery—women who cook, store, or serve food in lead-glazed ceramic pottery made in a traditional process and usually imported by individuals outside the normal commercial channels.
Eating nonfood substances (pica) —women who eat or mouth nonfood items that may be contaminated with lead, such as soil or lead-glazed ceramic pottery.
Using alternative or complementary substances, herbs, or therapies—women who use imported home remedies or certain therapeutic herbs traditionally used by East Indian, Indian, Middle Eastern, West Asian, and Hispanic cultures that may be contaminated with lead.
Using imported cosmetics or certain food products—women who use imported cosmetics, such as kohl or surma or certain imported foods or spices that may be contaminated with lead.
Engaging in certain high-risk hobbies or recreational activities—women who engage in high-risk activities (eg, stained glass production or pottery making with certain leaded glazes and paints) or have family members who do.
Renovating or remodeling older homes without lead hazard controls in place—women who have been disturbing lead paint, creating lead dust, or both or have been spending time in such a home environment.
Consumption of lead-contaminated drinking water—women whose homes have leaded pipes or source lines with lead.
Having a history of previous lead exposure or evidence of elevated body burden of lead—women who may have high body burdens of lead from past exposure, particularly those who have deficiencies in certain key nutrients (calcium or iron).

Living with someone identified with an elevated lead level—women who may have exposure in common with a child, close friend, or other relative living in the same environment.
Modified from Centers for Disease Control and Prevention. Guidelines for the identification and management of lead exposure in pregnant and lactating women. Atlanta (GA): CDC; 2010. Available at: http://www.cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf. Retrieved March 7, 2012.
Lactation
Women with risk factors for elevated lead levels Box 1 who have not been screened during pregnancy should be screened postpartum if they plan to breastfeed. Initiation of breastfeeding should be encouraged postpartum in a woman with a blood lead level less than 40 micrograms/dL. A woman with a confirmed blood lead level of 40 micrograms/dL or higher should not initiate breastfeeding and should be advised to pump and discard her breast milk until her blood lead level has decreased to less than 40 micrograms/dL. Blood lead measurements should be repeated every 1–2 weeks after the source of exposure has been identified and removed. At maternal blood lead levels of 5–39 micrograms/dL, breastfeeding should be initiated and accompanied by sequential testing of infant blood lead levels to monitor trends. If the infant’s blood lead level is greater than 5 micrograms/dL, breastfeeding should be discontinued until the maternal blood lead level decreases. If no external source is identified, and the maternal blood lead level is greater than 20 micrograms/dL and the infant blood lead level is 5 micrograms/dL or more, breast milk should be suspected as the source and temporary interruption of breastfeeding until the maternal blood lead level decreases should be considered.
Blood lead measurements should be repeated every 1–2 weeks after the source of exposure has been identified and removed. At maternal blood lead levels of 5–39 micrograms/dL, breastfeeding should be initiated and accompanied by sequential testing of infant blood lead levels to monitor trends. If the infant’s blood lead level is greater than 5 micrograms/dL, breastfeeding should be discontinued until the maternal blood lead level decreases. If no external source is identified, and the maternal blood lead level is greater than 20 micrograms/dL and the infant blood lead level is 5 micrograms/dL or more, breast milk should be suspected as the source and temporary interruption of breastfeeding until the maternal blood lead level decreases should be considered.
In addition to removing the source of lead exposure for the mother and infant, several nutritional interventions have been studied. Calcium supplementation (1,200 mg daily) has been associated with a 5–10% decrease in breast milk lead levels among women over the course of lactation 31 32 33 34, suggesting that calcium supplementation also may be an intervention strategy to reduce lead in breast milk from both current and previously accumulated sources. Among women in the postpartum period, increased intakes of vitamin C also have been associated with decreased levels of lead in breast milk.
Among women in the postpartum period, increased intakes of vitamin C also have been associated with decreased levels of lead in breast milk.
Conclusions and Recommendations
Routine blood lead testing of all pregnant women is not recommended.
Risk assessment of lead exposure should take place at the earliest contact with pregnant or lactating women, and blood lead testing should be performed if a single risk factor is identified Box 1.
Elevated lead levels in pregnancy have been associated with gestational hypertension, spontaneous abortion, low birth weight, and impaired neurodevelopment.
Prenatal lead exposure has known adverse effects on maternal health and infant outcomes across a wide range of maternal blood lead levels.
Pregnant women with blood lead levels of 5 micrograms/dL or higher should be treated as follows:
Sources of lead exposure should be identified.

Women should receive counseling regarding avoidance of further exposure and receive specific nutritional recommendations regarding calcium and iron supplementation because these strategies can decrease their lead levels.
Confirmatory and follow-up blood lead testing should be performed in accordance with the CDC’s recommended schedules Table 1.
Women with confirmed blood lead levels of 45 micrograms/dL or more should be treated in consultation with clinicians experienced in the management of lead toxicity and high-risk pregnancy.
Initiation of breastfeeding should be encouraged postpartum in a woman with a blood lead level less than 40 micrograms/dL.
A breastfeeding woman with a confirmed blood lead level of 40 micrograms/dL or higher should be advised to pump and discard her breast milk until her blood lead level has decreased to less than 40 micrograms/dL.
If no external source is identified, and the maternal blood lead level is greater than 20 micrograms/dL and the infant blood lead level is 5 micrograms/dL or more, breast milk should be suspected as the source and temporary interruption of breastfeeding until the maternal blood lead level decreases should be considered.

Copyright August 2012 by the American College of Obstetricians and Gynecologists, 409 12th Street, SW, PO Box 96920, Washington, DC 20090-6920. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, posted on the Internet, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission from the publisher. Requests for authorization to make photocopies should be directed to: Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923, (978) 750-8400.
ISSN 1074-861X
Lead screening during pregnancy and lactation. Committee Opinion No. 533. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:416–20.
Lead Exposure During Pregnancy and Breastfeeding
Download a PDF version of this information in English, Hmong, Karen, or Spanish
- English: Lead Exposure During Pregnancy and Breastfeeding (PDF)
- Hmong: Raug Lead thaum Cev Xeeb Me Nyuam los yog Pub Niam Mis (PDF)
- Karen: Lead Exposure During Pregnancy and Breastfeeding (PDF)
- Spanish: Exposición al plomo durante el embarazo y la lactancia materna (PDF)
On this page:
What is lead
Why be concerned about lead
How can you become lead poisoned
How can your baby be exposed to lead
How do you know if you or your baby have been exposed to lead
Is there financial assistance for home remodeling
What can you do to prevent lead poisoning
What is lead?
Lead is a heavy metal that has been used for thousands of years to make a variety of products and is still in use today. Too much lead exposure can cause serious health problems, and young children and developing fetuses are most at risk.
Too much lead exposure can cause serious health problems, and young children and developing fetuses are most at risk.
Why be concerned about lead?
Lead poisoning can cause serious harm to your baby’s health. Side effects of lead poisoning include:
- Lowered intelligence
- Decreased coordination
- Shortened attention span
- Aggressive behavior
- Reading problems and other disabilities
How can you get lead poisoning?
Lead enters your body each time you swallow or breathe in something that has lead in it, such as fumes, dust or paint chips. Many pregnant women have cravings for non-food items, which can cause exposure to lead. For adults, exposure normally happens at work, during repair or remodeling of an older home, or while doing a hobby where lead is used (such as making stained glass or jewelry with lead solder and target shooting). If someone you live with is exposed to lead and does not shower and change clothing before coming home, you may be exposed to the lead on their clothing or in their hair.
How can your baby become exposed to lead?
Pregnant women with high blood lead levels can transfer lead to their baby through the placenta or through breast milk. Breastfeeding is still recommended unless the mother’s blood lead level is so high that it would put the baby at risk.
How do you know if you or your baby have been exposed to lead?
There are no signs or symptoms of lead poisoning until you are very sick. The only way to know if you have been exposed to lead is to get a blood lead test by:
- Visiting your medical clinic (as part of your prenatal exam)
- Contacting the local public health office nearest you for information on services in your area
If you live in a home built before 1978 and any remodeling is being done, you and your home should be tested to make sure that you and your baby are not being exposed to lead.
Is there financial assistance for home remodeling?
Contact your local housing agency for financial assistance with home remodeling needs. Some counties have loans and grants available for controlling lead hazards.
Some counties have loans and grants available for controlling lead hazards.
What can you do to prevent lead poisoning?
The best way to prevent lead exposure during pregnancy and breastfeeding is to:
- Talk about possible risks with your doctor if your job includes working with or around lead. You will need to decide if you should get a job transfer.
- Stay away from work areas during repair or remodeling of a house built before 1978.
- Never sand or scrape lead-based paint (all repair or remodeling needs to be done using lead-safe work practices).
- Have all household members who are exposed to lead through a hobby or job do the following:
-shower after working with lead
-wash their clothes separately from other household clothing - Avoid eating non-food items (such as soil, clay, plaster, paint chips, pottery), using herbal medicines, and traditional remedies or cosmetics that may contain lead.
- Test your home and water for lead.
Paint chips, water and soil can be tested for lead. (Call MDH or your local health department for more information.)
- Avoid using imported pottery and leaded crystal for preparing or eating food.
Download a PDF version of this information here:
- English: Lead Exposure During Pregnancy and Breastfeeding (PDF)
- Spanish: Exposición al plomo durante el embarazo y la lactancia materna (PDF)
Lead poisoning
lead poisoning- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 O
- M
- R
- S
- T
- Y
- F
- X
- C
- W 0005
- B
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find country »
- A
- B
- in
- g
- d
- E
- С
- and
- K
- m
- N 9000
- t
- in
- x
- h
- Sh
- 9000 WHO in countries » nine0003
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Lead poisoning
EPA/L. Koula
A man melts lead metallic wastes use in the production of cooking pots, at a recycling warehouse in Koumassi, Abidjan, Ivory Coast
© Photo
Key Facts
- Lead is a poisonous substance whose accumulation affects a number of body systems and is especially harmful to young children.
- In the body, lead enters the brain, liver, kidneys and bones. Over time, lead accumulates in teeth and bones. The dose of lead received by the human body, as a rule, is estimated by determining the content of lead in the blood. nine0005
- Lead accumulated in bones enters the bloodstream during pregnancy and becomes a source of exposure to the developing fetus.
- There is no standard intake of lead at which, according to available data, no harmful effects occur.
- Lead exposure is preventable.
General information
Lead is a natural toxic metal found in the earth's crust. Its widespread use has resulted in widespread environmental pollution, lead ingestion and significant public health problems in many parts of the world. nine0286
nine0286
Lead mining, smelting, industrial use, recycling, and the use of lead in a wide range of products are important sources of environmental pollution. More than three-quarters of global lead consumption comes from the production of lead-acid batteries for motor vehicles. However, lead is also used in many other products, such as pigments, paints, solder, stained glass, lead crystal utensils, ammunition, ceramic glazes, jewelry, toys, as well as some cosmetics (such as kayal and sindur) and traditional medicine in India, Mexico, Vietnam and other countries. Lead can be found in drinking water supplied through lead pipes or pipes connected with lead solder. Currently, a significant part of the lead for the needs of the world economy is obtained as a result of recycling. nine0286
Young children are particularly vulnerable to the toxic effects of lead, and their health may be subject to profound and irreversible negative changes, primarily affecting the development of the brain and nervous system. Lead also causes long-term effects in adults, including an increased risk of high blood pressure and kidney damage. Exposure to high levels of lead in pregnant women can cause miscarriages, stillbirths, premature births and low birth weight newborns. nine0286
Lead also causes long-term effects in adults, including an increased risk of high blood pressure and kidney damage. Exposure to high levels of lead in pregnant women can cause miscarriages, stillbirths, premature births and low birth weight newborns. nine0286
Sources and routes of exposure
People may be exposed to lead through work or contact with environmental objects. It is mainly caused by:
- inhalation of lead particles from the combustion of materials containing lead, such as smelting, recycling, removing lead paint and using leaded aviation gasoline; and
- ingestion of lead-contaminated dust, water (from lead pipes), and food (from containers made with lead glaze or lead solder). nine0005
Young children are especially vulnerable to lead poisoning because they absorb 4 to 5 times more lead from any source than adults. Because of children's inherent curiosity and age-specific desire to put their hands in their mouths, children put lead-containing or lead-coated objects into their mouths and swallow, such as contaminated soil or dust and peeling lead paint. This route of exposure is especially dangerous for children who suffer from a psychological disorder called pica (constant and obsessive cravings for inedible things), who can pick and eat lead paint from walls, door frames, and furniture. Exposure to lead-contaminated soil and dust from battery recycling and mining has been responsible for massive lead poisoning and many deaths among young children in Nigeria, Senegal and elsewhere. nine0286
This route of exposure is especially dangerous for children who suffer from a psychological disorder called pica (constant and obsessive cravings for inedible things), who can pick and eat lead paint from walls, door frames, and furniture. Exposure to lead-contaminated soil and dust from battery recycling and mining has been responsible for massive lead poisoning and many deaths among young children in Nigeria, Senegal and elsewhere. nine0286
When lead enters the body, it is distributed to organs such as the brain, kidneys, liver and bones. Lead is deposited in teeth and bones, where it accumulates over time. Lead deposited in bone tissue can return to the blood during pregnancy, exposing the fetus to its effects. Malnourished children are more susceptible to lead exposure because their bodies absorb more lead when other nutrients, such as calcium or iron, are deficient. The most at risk are very young children (including fetuses in utero) and children living in poor families. nine0286
Children's health effects
Lead exposure can have serious health effects on children.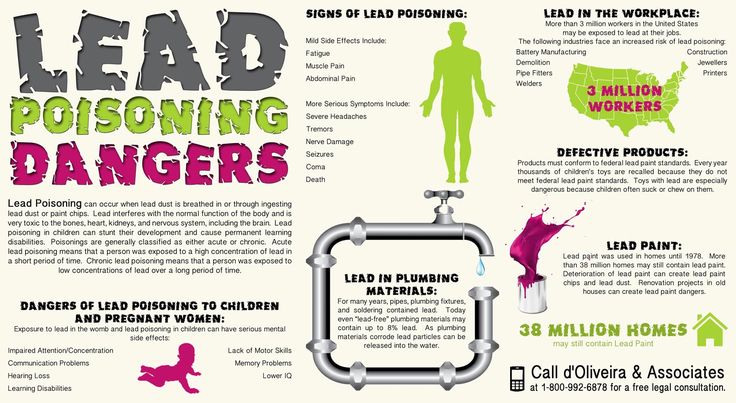 At high levels, lead disrupts the functioning of the brain and central nervous system, causing coma, seizures, and even death. Children who survive severe lead poisoning may experience mental retardation and behavioral problems. At lower levels of exposure, which do not cause any overt symptoms, lead causes a range of damage to various body systems. In particular, lead can affect children's brain development and lead to a decrease in intelligence quotient (IQ), behavioral changes such as reduced attention spans and increased antisocial behavior, and poor learning outcomes. Lead exposure also causes anemia, hypertension, kidney failure, immune toxicosis, and toxic damage to the reproductive organs. The neurological and behavioral effects of lead exposure are considered irreversible. nine0286
At high levels, lead disrupts the functioning of the brain and central nervous system, causing coma, seizures, and even death. Children who survive severe lead poisoning may experience mental retardation and behavioral problems. At lower levels of exposure, which do not cause any overt symptoms, lead causes a range of damage to various body systems. In particular, lead can affect children's brain development and lead to a decrease in intelligence quotient (IQ), behavioral changes such as reduced attention spans and increased antisocial behavior, and poor learning outcomes. Lead exposure also causes anemia, hypertension, kidney failure, immune toxicosis, and toxic damage to the reproductive organs. The neurological and behavioral effects of lead exposure are considered irreversible. nine0286
There is no “safe” concentration of lead in blood; even as low as 3.5 mcg/dl of lead in the blood can cause intellectual decline, behavioral problems and learning difficulties in children (1). As blood lead levels increase, the spectrum and severity of symptoms and sequelae increase.
Fortunately, the elimination and use of leaded gasoline in most countries, as well as other restrictive measures against the use of this metal, have led to a significant decrease in blood lead concentrations at the population level. As of July 2021, leaded fuel for cars and trucks is not sold in any country in the world (2). However, more efforts are needed to eliminate the use of lead paint: to date, only 45% of countries have legal restrictions on the use of lead paint (3). nine0286
Burden of disease due to lead exposure
The World Health Organization’s 2021 update of Public Health Exposure to Chemicals: Known and Unknown Factors estimates that in 2019 almost half of the 2 million deaths in as a result of established exposure to chemicals was caused by the intake of lead in the body. Globally, long-term health effects from lead exposure are estimated to result in 21.7 million life years lost due to disability and death (disability-adjusted life years, DALYs), causing 30% of the global burden of idiopathic intellectual disability, 4 6% of the global burden of cardiovascular disease and 3% of the burden of chronic kidney disease. nine0286
nine0286
WHO activities
WHO has identified lead as one of the 10 chemicals of major public health concern requiring action by Member States to protect workers, children and women of childbearing age. WHO has published a wide range of information materials on lead on its website, including information for policy makers, technical guidance and campaign materials. WHO has developed guidelines for the clinical management of people exposed to lead and is developing and is preparing guidelines for the prevention of lead exposure that will provide policy makers, health authorities and healthcare professionals with evidence-based advice on measures they can take to protect the health of children and adults from lead exposure. nine0286
As lead paint continues to be a source of exposure in many countries, WHO, together with the United Nations Environment Programme, has formed the Global Alliance to Eliminate Lead Paint. In addition, WHO is a partner in a project funded by the Global Environment Facility to help at least 40 countries put in place legislation to limit the use of lead paint (3) . The phase-out of lead paint by 2020 is one of the priority government actions included in the WHO Roadmap to Empower the Health Sector in the Strategic Approach to International Chemicals Management to help us reach the 2020 target and beyond. nine0286
The phase-out of lead paint by 2020 is one of the priority government actions included in the WHO Roadmap to Empower the Health Sector in the Strategic Approach to International Chemicals Management to help us reach the 2020 target and beyond. nine0286
1) US CDC Advisory Committee on Childhood Lead Poisoning Prevention. CDC updates blood lead reference value to 3.5µg/dL. Atlanta: US Centers for Disease Control and Prevention; 2021 (https://www.cdc.gov/nceh/lead/news/cdc-updates-blood-lead-reference-value.html).
(2) End of leaded fuel use a “milestone for multilateralism” press release https://news.un.org/en/story/2021/08/1098792, 2021.
(3) SAICM GEF Project - Lead in Paint Component
International Lead Poisoning Prevention Week
Childhood lead exposure can make a person a criminal
https://ria.ru/20080528/108695506.html
Childhood lead exposure can make a person a criminal
Childhood lead exposure can make a person a criminal - RIA Novosti, 28. 07. 2008
07. 2008
Childhood lead exposure can make a person a criminal
The authors of an article from the University of Cincinnati, USA investigated the relationship between lead intoxication of children or fetuses during pregnancy and felony arrests in adulthood. nine0286
The authors of the article, Dr. Kim Dietrich and her colleagues from the University of Cincinnati, US, investigated the relationship between lead intoxication in children or fetuses during pregnancy and felony arrests in adulthood.
"A large amount of experimental data clearly indicates that lead can lead to neurological disorders in animals. However ... the observed association between lead exposure and neurological diseases in humans, especially in children, has remained controversial," the article says. nine0286
Previously, there was evidence that lead exposure in childhood increases the risk of antisocial behavior in adults. These data have not been supported by accurate measurements of lead exposure levels in the same people during childhood and adulthood. The new study provides accurate data on these parameters for the first time.
The new study provides accurate data on these parameters for the first time.
Between 1979 and 1984, scientists conducted a survey of pregnant women living in poor areas of Cincinnati. They were exposed to lead due to its high concentration in the building materials from which their homes were built. nine0286
The 376 infants born thereafter continued to be examined, 250 of whom participated in the final stage of the study in 2005.
Their mothers had their blood lead levels measured during pregnancy, and these measurements were taken regularly in their children until they were six and a half years old. The levels of lead exposure were found to be consistent with how often these children were arrested for various offenses from when they were 18 until the end of October 2005. nine0286
Researchers have found that elevated blood lead levels before birth and in early childhood are associated with high rates of arrests for various offenses, as well as for violence.