Post partum depression psychosis
SAMHSA’s National Helpline | SAMHSA
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).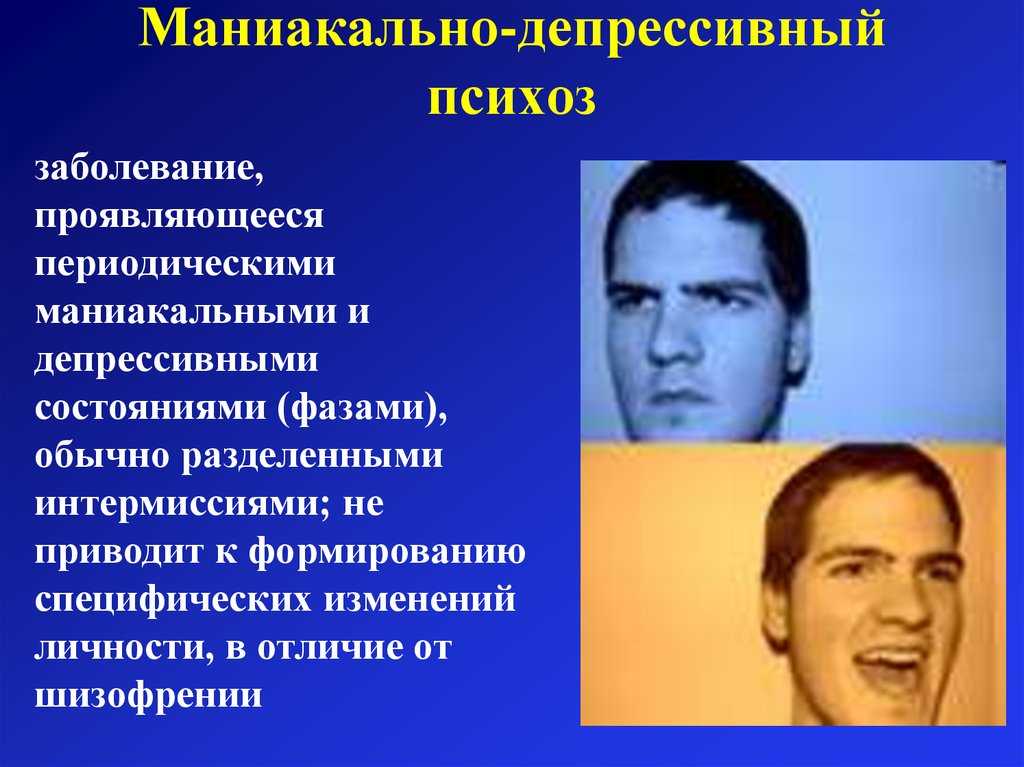
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated
Last Updated: 03/22/2023
Postpartum psychosis. What is postpartum psychosis?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
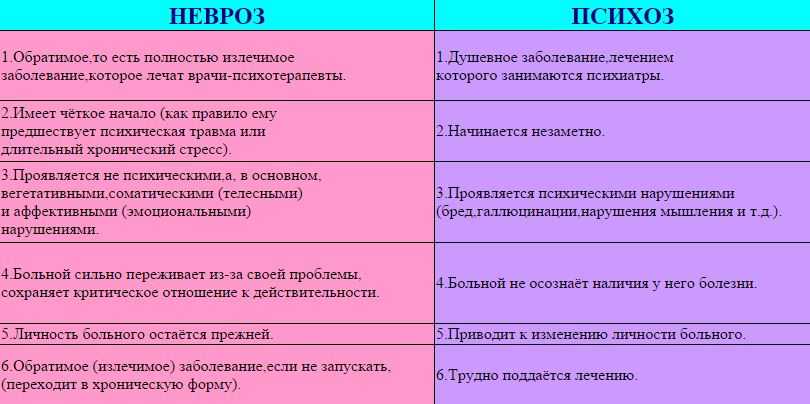
Postpartum psychosis is an acute mental disorder that develops in the first weeks after childbirth.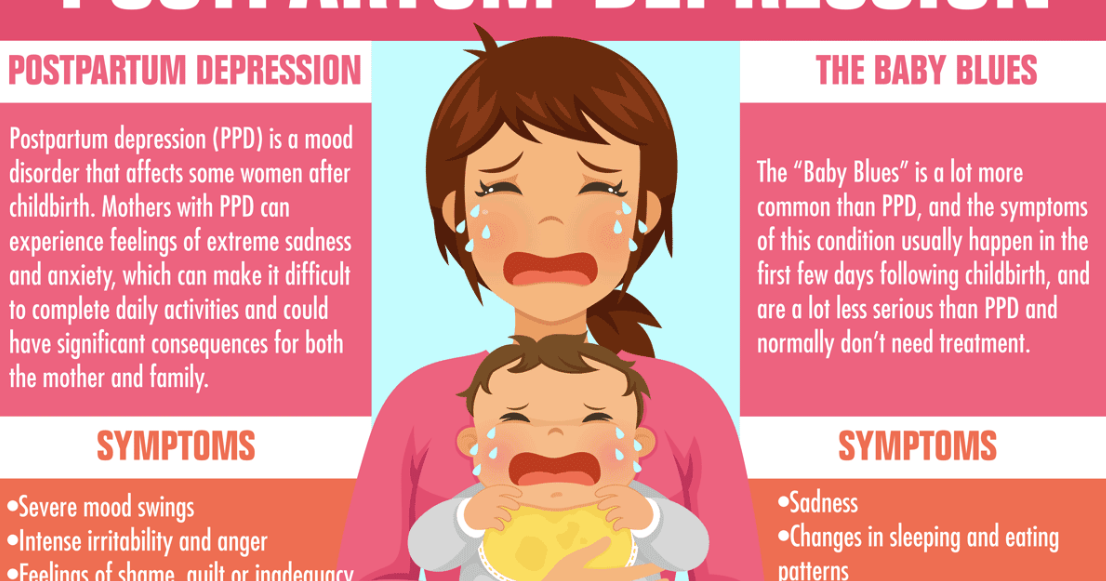 Manifested by depression, insomnia, confusion, delusional ideas about the incurable illness of the child, delusions of persecution, hallucinations. The behavior of the patients becomes inadequate: they refuse to care for the newborn, harm him, and attempt suicide. Diagnosis is carried out by a psychiatrist, the main methods are clinical conversation and observation. Medical treatment, antipsychotics, antidepressants, tranquilizers are used. When the condition improves, sessions of psychotherapy and family counseling are introduced.
Manifested by depression, insomnia, confusion, delusional ideas about the incurable illness of the child, delusions of persecution, hallucinations. The behavior of the patients becomes inadequate: they refuse to care for the newborn, harm him, and attempt suicide. Diagnosis is carried out by a psychiatrist, the main methods are clinical conversation and observation. Medical treatment, antipsychotics, antidepressants, tranquilizers are used. When the condition improves, sessions of psychotherapy and family counseling are introduced.
ICD-10
F53.1 Severe mental and behavioral disorders associated with the puerperium, not elsewhere classified
- Causes
- Pathogenesis
- Symptoms of postpartum psychosis
- Complications
- Diagnostics
- Treatment of postpartum psychosis
- Prognosis and prevention
- Prices for treatment
General
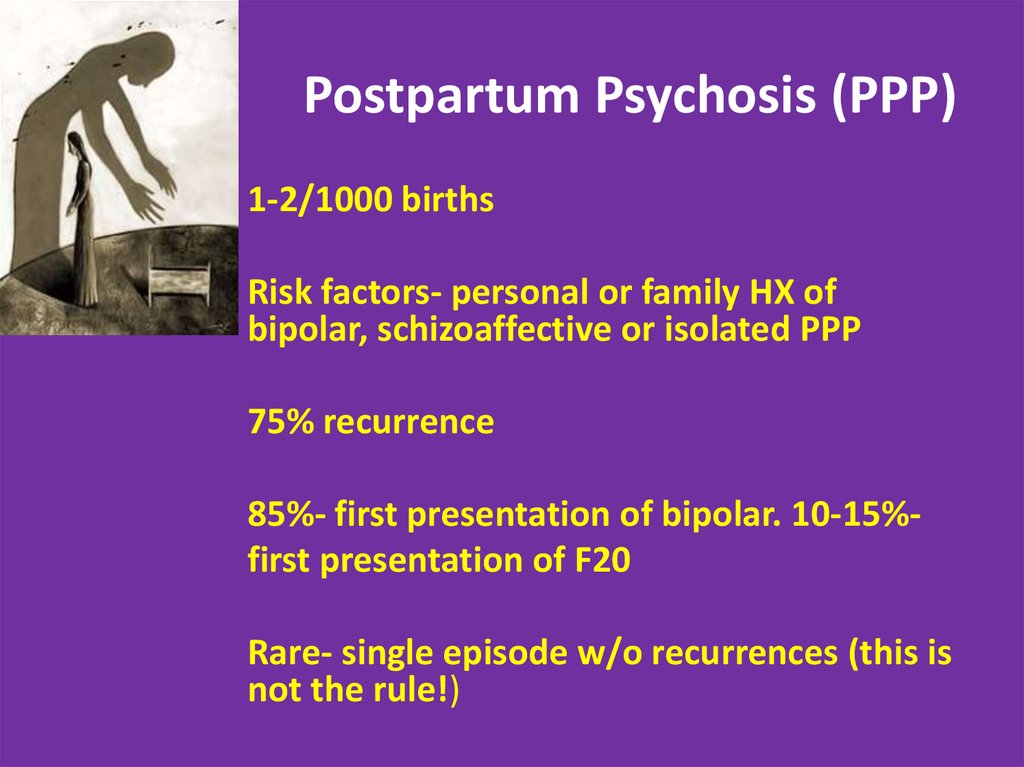
Postpartum psychosis is also called postnatal. This disorder was first described by Hippocrates in 460 BC. e. Its origin was explained by large blood loss during childbirth. More accurate studies date back to the middle of the 19th century. French psychiatrists J.-E. Esquirol and L.-V. Marse described the psychoses of young mothers as the consequences of severe somatic complications of childbirth. Currently, the prevalence of psychotic disorders has significantly decreased. In economically developed countries, their frequency is 1-1.2 cases per 1,000 women who gave birth no more than 3 months ago. The peak incidence is observed within the first 30 days after the birth of a child.
This disorder was first described by Hippocrates in 460 BC. e. Its origin was explained by large blood loss during childbirth. More accurate studies date back to the middle of the 19th century. French psychiatrists J.-E. Esquirol and L.-V. Marse described the psychoses of young mothers as the consequences of severe somatic complications of childbirth. Currently, the prevalence of psychotic disorders has significantly decreased. In economically developed countries, their frequency is 1-1.2 cases per 1,000 women who gave birth no more than 3 months ago. The peak incidence is observed within the first 30 days after the birth of a child.
postpartum psychosis
Causes
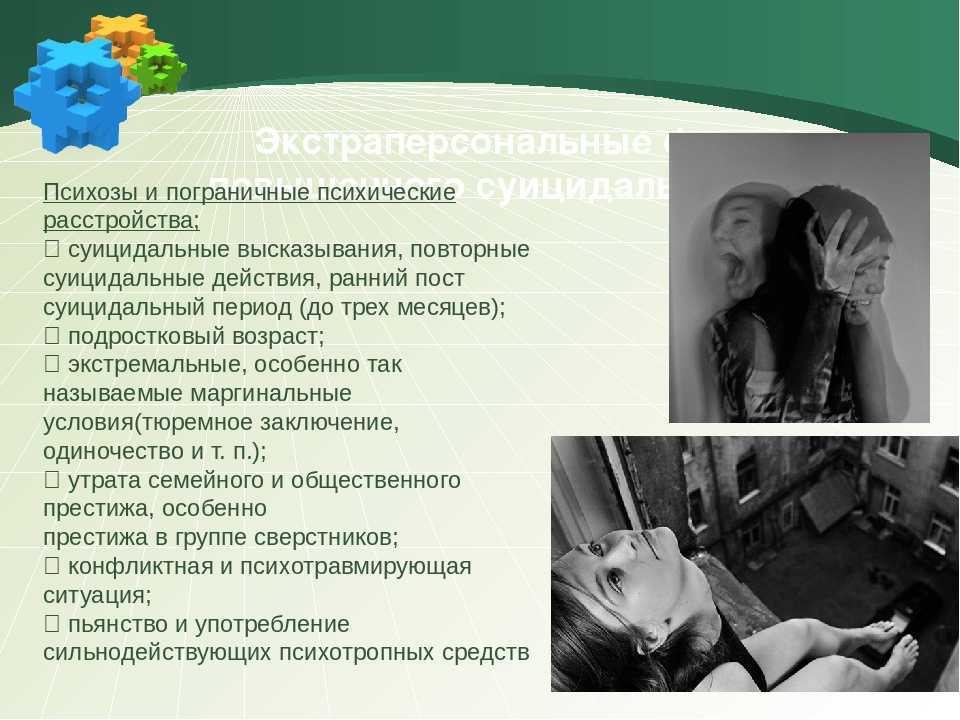
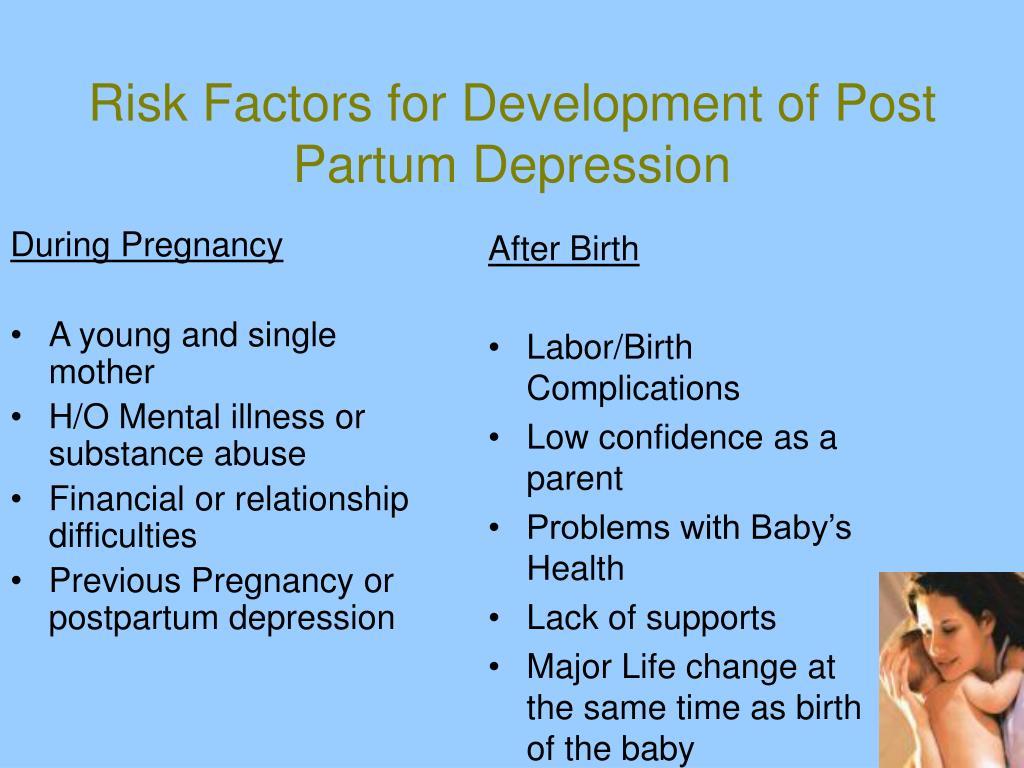
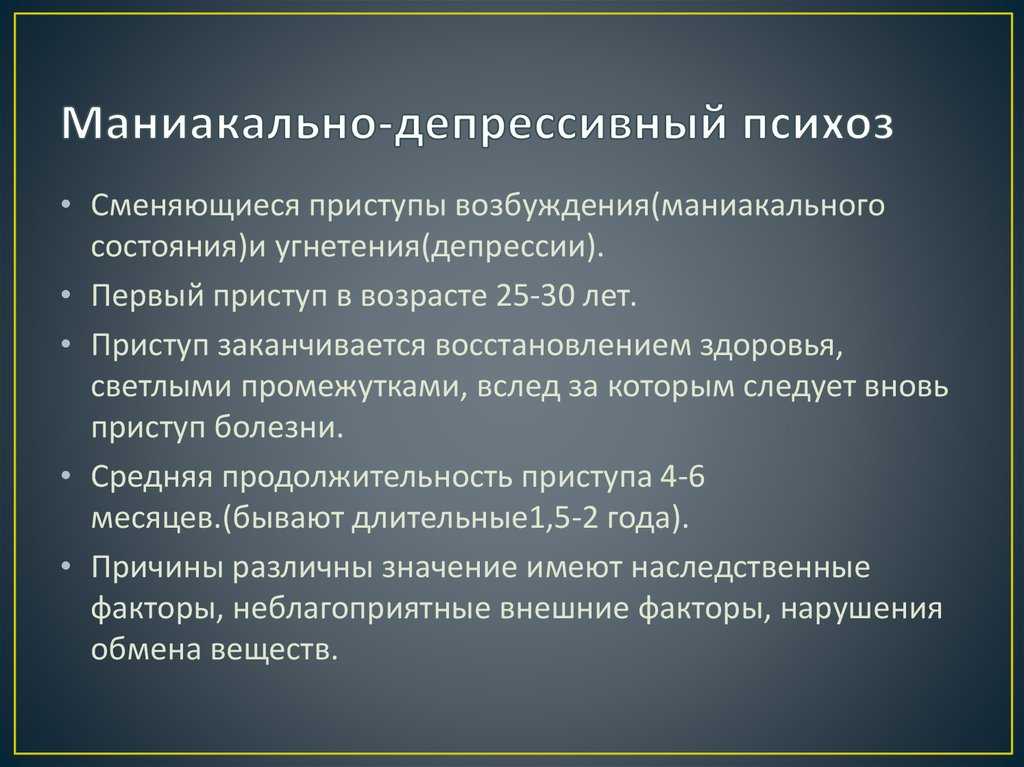
Official data confirm that more than half of women with postnatal psychosis have mental disorders (schizophrenia, depression, MDP) or a hereditary predisposition to them. The exact causes of the pathology are unknown, but several groups of triggers have been identified - factors contributing to its debut:
- Complications of pregnancy, childbirth.
 An acute psychotic state is often caused by the death of a newborn, premature birth, threatened miscarriage. The association of the disorder with massive blood loss and sepsis, identified in ancient times, is confirmed.
An acute psychotic state is often caused by the death of a newborn, premature birth, threatened miscarriage. The association of the disorder with massive blood loss and sepsis, identified in ancient times, is confirmed. - Hormonal disorders. The end of pregnancy is always associated with a change in the level of hormones in a woman's body. Mental disorders develop on the basis of a sharp decrease in the synthesis of progesterone, estrogen, thyroxine.
- CNS lesion. Psychosis often occurs with neurological diseases, after brain injuries, neuroinfections, intoxications. Sometimes the disorder is provoked by the use of scopolamine in combination with lidol for pain relief in childbirth.
- Anxious and suspicious personality traits. Women with high emotional tension, low adaptive abilities, and a tendency to predict failures are more prone to depression and the formation of delusional ideas. The process of childbirth becomes a stressful situation for them, triggering a mental disorder.
- Unfavorable psychosocial environment. Risk factors are unwanted pregnancy, rejection of the child by the mother, financial difficulties, unsettled life, divorce from a spouse. Psychoses are often diagnosed in parturient women leading an asocial lifestyle (drug addiction, alcoholism, prostitution).
Pathogenesis
According to the mechanism of origin, postpartum psychosis is reactive. It develops in response to a traumatic event - childbirth. It is based on the experience of fear of death, violation of the integrity of one's own personality, restriction of freedom, lack of love of others (shift of attention from a woman to a child). An unfavorable background for the onset of psychosis is psychophysiological asthenization - depletion of energy, a decrease in resistance to stress factors. There comes a state of decompensation of nervous adaptive mechanisms.
At the neurophysiological level, there is a violation of reciprocal inhibitory interactions between the cortex and subcortical brain structures, between the anterior and posterior hypothalamus - the highest centers of regulation of autonomic functions and emotions. The balance of activation of the sympathetic and parasympathetic nervous system, the ratio of the main neurotransmitters (serotonin, norepinephrine, dopamine, GABA) change. According to psychodynamic theory, postpartum psychosis results from a conflict between the mother's real desires and the situation of motherhood.
The balance of activation of the sympathetic and parasympathetic nervous system, the ratio of the main neurotransmitters (serotonin, norepinephrine, dopamine, GABA) change. According to psychodynamic theory, postpartum psychosis results from a conflict between the mother's real desires and the situation of motherhood.
Symptoms of postpartum psychosis
Psychosis begins to manifest 2-3 days after the completion of childbirth, when a woman is aware of the changes that have occurred in her life. Symptoms may develop gradually or rapidly. Initially, there is insomnia, anxiety, restlessness, fatigue, fatigue. The emotional background is stably reduced. Then suspicion and alertness begin to grow. Overvalued ideas are formed about the state of the child's health, about the presence of diseases in him or in himself. Consciousness becomes confused, speech - abrupt, illogical.
Suspicion is constantly increasing. Often, mothers closely observe the newborn during sleep and feeding, examining him, listening to his breathing and heartbeat, revealing imaginary incurable, fatal diseases. Patients begin to accuse doctors and close relatives of being indifferent to the condition of the baby, of deliberate unwillingness to treat him. Secretly from those around them, they give him various medicines, carry out “procedures” that can cause real harm (dip in cold water, leave him without clothes and diapers).
In another version of the course of psychosis, mothers lose interest in babies, do not show care and love. Overprotection turns into a feeling of hatred. Delusional thoughts are expressed about the substitution of the child, the infusion of evil spirits, demons into him, about the imminent inevitable death. In severe cases, auditory hallucinations are noted. Voices urge women to kill a newborn, attempts are often made to strangle him. Throughout the disease, the criticism of patients to their condition is disturbed - delusions and hallucinations are not recognized, they are not regarded as pathological.
Complications
Without timely diagnosis and treatment, postpartum psychosis is a danger to the life, health of the baby and mother.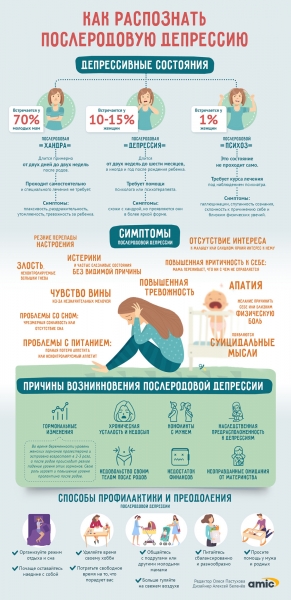 On the basis of hallucinations and delusions, inappropriate behavior is formed - patients try to commit suicide, having previously killed the baby. There are known cases of strangulation, falling from a height of a woman and a newborn. With a sluggish psychotic process, when indifference and detachment gradually increase, the child does not receive sufficient emotional and sensory stimulation, lags behind in physical and mental development, and suffers from neurotic disorders (enuresis, nightmares, phobias) from an early age.
On the basis of hallucinations and delusions, inappropriate behavior is formed - patients try to commit suicide, having previously killed the baby. There are known cases of strangulation, falling from a height of a woman and a newborn. With a sluggish psychotic process, when indifference and detachment gradually increase, the child does not receive sufficient emotional and sensory stimulation, lags behind in physical and mental development, and suffers from neurotic disorders (enuresis, nightmares, phobias) from an early age.
Diagnostics
Postpartum psychosis presents with classic signs of acute psychopathology, so making an accurate diagnosis can be difficult. An important role in the process of identifying the disease is played by the patient's relatives, it is they who most often pay attention to changes in the behavior and emotional reactions of a young mother. Professional diagnostics is performed by a psychiatrist, in addition, pathopsychological, gynecological and neurological examinations may be required to differentiate postnatal psychosis from schizophrenia, bipolar affective disorder, depression, hypothyroidism, Cushing's syndrome.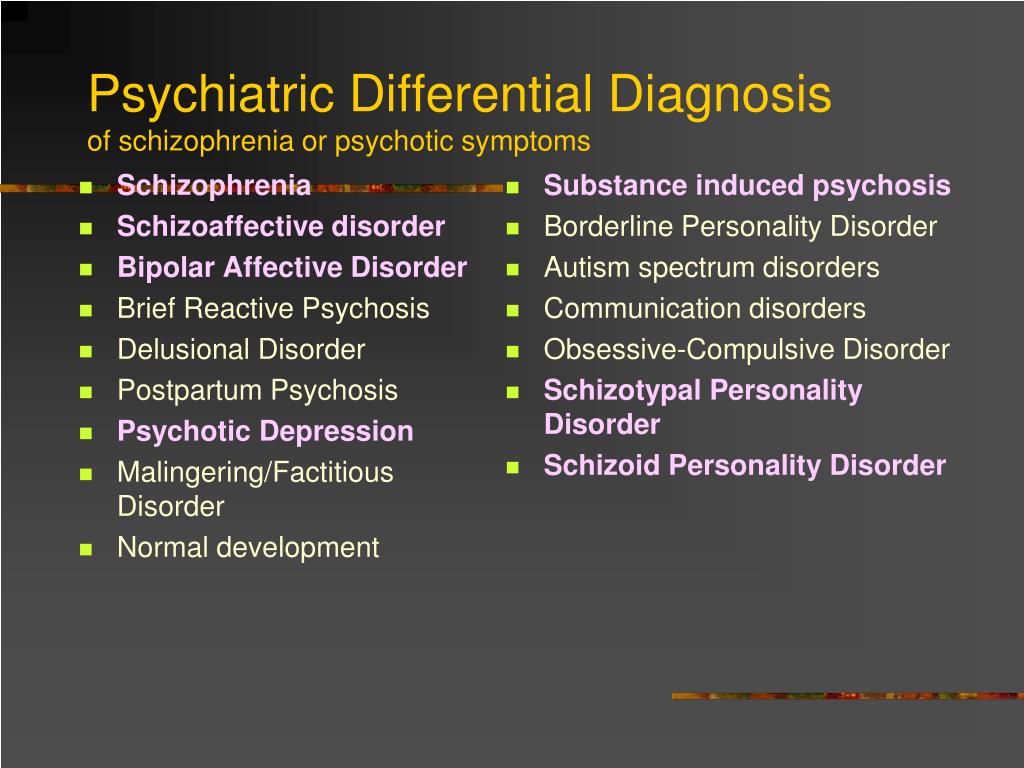 Specific diagnostic methods include:
Specific diagnostic methods include:
- History taking. The doctor examines the medical documentation about the course of childbirth and pregnancy, finds out the presence of a hereditary burden for mental disorders, the patient's existing psychiatric diagnoses, postpartum depression, psychosis after previous pregnancies. The material and living conditions of life, the presence of a spouse, the patient's attitude to conception, pregnancy, and the birth of a child are taken into account.
- Clinical conversation. In direct contact with the patient, the psychiatrist evaluates the productivity of contact, the purposefulness of thinking and speech, and the logic of reasoning. With a psychotic disorder, women express delusional ideas in detail, are concentrated on their own experiences, and do not always answer in accordance with the questions of a specialist.
- Surveillance. During the conversation, the doctor observes the behavior and emotions, determines their adequacy, the safety of arbitrary control, motivation.
 Psychosis is characterized by alertness and distrust, inconsistency of reactions to the examination situation, the predominance of dysphoric and / or depressive affect, and the absence of a critical attitude towards one's behavior.
Psychosis is characterized by alertness and distrust, inconsistency of reactions to the examination situation, the predominance of dysphoric and / or depressive affect, and the absence of a critical attitude towards one's behavior.
Treatment of postpartum psychosis
Therapy of an acute condition is carried out in a hospital setting. Quite often, women are sent to psychiatric departments and neuropsychiatric dispensaries from the maternity hospital. At the time of intensive treatment, the child is separated from the mother, entrusting care to close relatives. Comprehensive assistance includes the following areas:
- Pharmacotherapy. At the acute stage of the disorder, the main task is to relieve psychotic symptoms. Neuroleptics, normotimics, tranquilizers, antidepressants are prescribed. For the period of taking medications, it is necessary to exclude breastfeeding by choosing artificial mixtures for feeding the child.
- Psychotherapy.
 After the elimination of the symptoms of psychosis, a period of awareness of the patient of her actions, feelings, and the presence of the disease begins. This provokes depression, guilt and self-hatred. To stabilize the emotional state and correct negative attitudes, techniques of the cognitive-behavioral direction, psychoanalysis are used.
After the elimination of the symptoms of psychosis, a period of awareness of the patient of her actions, feelings, and the presence of the disease begins. This provokes depression, guilt and self-hatred. To stabilize the emotional state and correct negative attitudes, techniques of the cognitive-behavioral direction, psychoanalysis are used. - Family assistance and rehabilitation. The support of loved ones and the correct organization of the daily routine are important. Relatives organize round-the-clock monitoring of the patient, perform baby care procedures together with the mother. It is important to spend time with a young mother, talk, distract from painful thoughts, control the regular intake of drugs prescribed by a psychiatrist.
Prognosis and prevention
Postpartum psychosis has a favorable outcome, subject to successful recovery from depression, support from loved ones, and the absence of mental illness. Prevention is based on the correct physical and psychological preparation of a woman for pregnancy and the process of childbirth. Expectant mothers need to pay attention to planning to minimize the risk of complications. It is recommended to attend courses in childcare skills, master breathing and relaxation techniques in childbirth, share your experiences with your husband, parents, close friends, and if you have severe anxiety, seek help from a psychologist.
Expectant mothers need to pay attention to planning to minimize the risk of complications. It is recommended to attend courses in childcare skills, master breathing and relaxation techniques in childbirth, share your experiences with your husband, parents, close friends, and if you have severe anxiety, seek help from a psychologist.
You can share your medical history, what helped you in the treatment of postpartum psychosis.
Sources
- Features of clinical manifestations and treatment of postpartum psychosis/ Zhuk TP, Dudal LV// Medicine and ecology. – 2014.
- Postpartum psychosis - a significant problem of modern medicine / Mishchenko AN, Mishchenko MM// Modern scientific research and development. - 2017 - No. 8 (16).
- Pregnancy, childbirth and the postpartum period: physiology, psychopathology, psychotherapy and psychoprophylactic preparation / Stanko E.P., Liskovich V.A. and others - 2005.
- This article was prepared based on the materials of the site: https://www.
 krasotaimedicina.ru/
krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
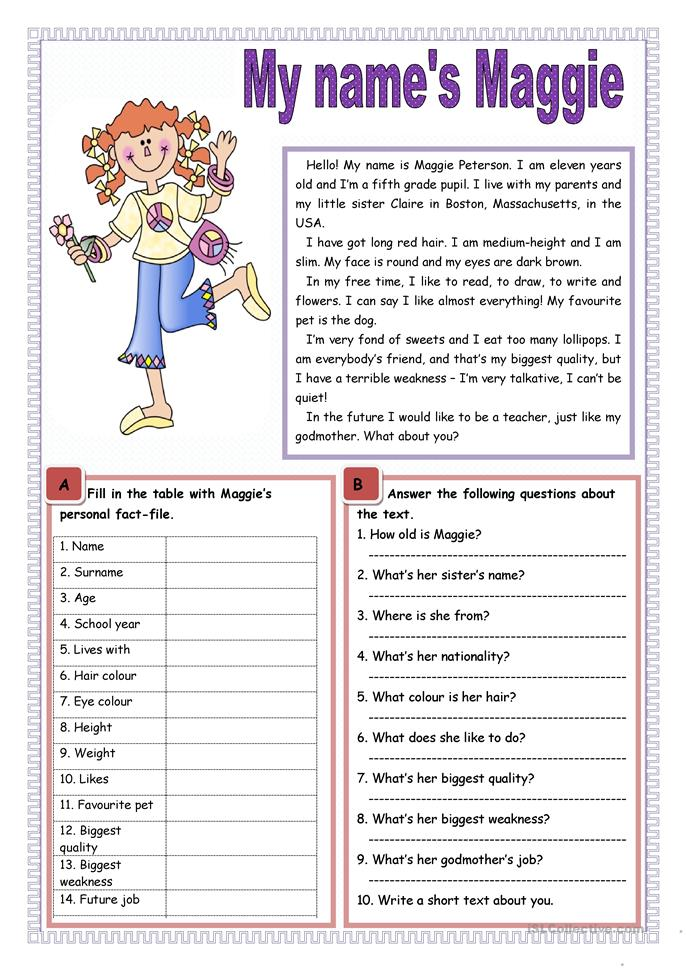
Postpartum depression | The CALDA Clinic
Treatment options: postpartum depression
A child is happiness! Everyone is happy, but you, as a mother, should be the happiest of all? But it's just the opposite: you're sad, you lack energy, you're exhausted, and the situation terrifies you. You feel guilty because you can't give your child as much love as you would like. Maybe you even feel like a “bad” mother? Are you ashamed and do not understand what is happening to you? These are all signs of postpartum depression. This disease responds well to treatment and will not require you to be alone.
What is postpartum depression?
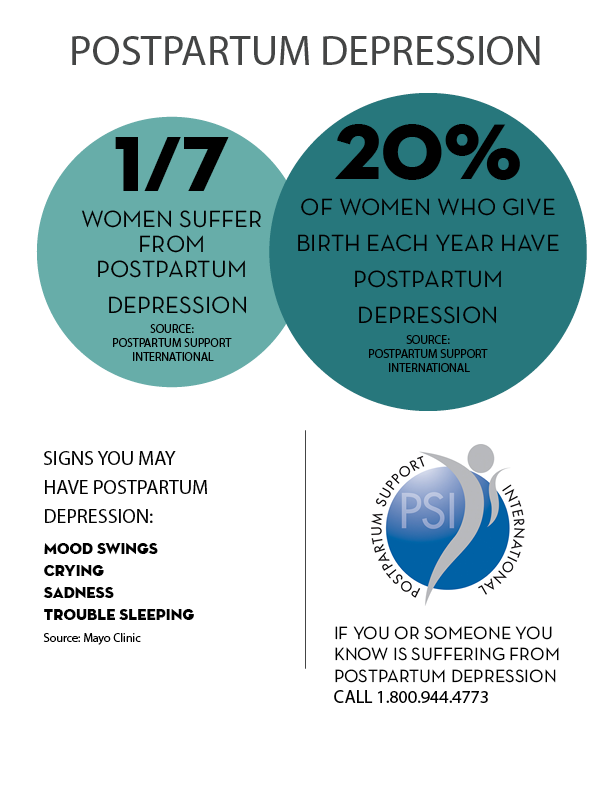
Postpartum or postnatal depression is the most common mental illness that occurs in women after childbirth. Approximately every seventh or tenth woman suffers from it. During the first two years after the birth of a child, prolonged depressive episodes are observed, characterized by sadness, apathy and guilt. The immediate environment often does not understand anything. A mother who is unable to show love for her child is considered taboo. Therefore, many sick people silently suffer from shame. They neglect themselves and the child or take care of him only mechanically. This threatens the violation of attachment and behavioral problems in the child. Lack of treatment is fraught with an increase in the suffering of the patient and the child. In the worst cases, this can lead to conventional or extended suicide, when the mother sees no way out of the current situation and kills herself and the child.
Approximately every seventh or tenth woman suffers from it. During the first two years after the birth of a child, prolonged depressive episodes are observed, characterized by sadness, apathy and guilt. The immediate environment often does not understand anything. A mother who is unable to show love for her child is considered taboo. Therefore, many sick people silently suffer from shame. They neglect themselves and the child or take care of him only mechanically. This threatens the violation of attachment and behavioral problems in the child. Lack of treatment is fraught with an increase in the suffering of the patient and the child. In the worst cases, this can lead to conventional or extended suicide, when the mother sees no way out of the current situation and kills herself and the child.
Postpartum depression: important signs
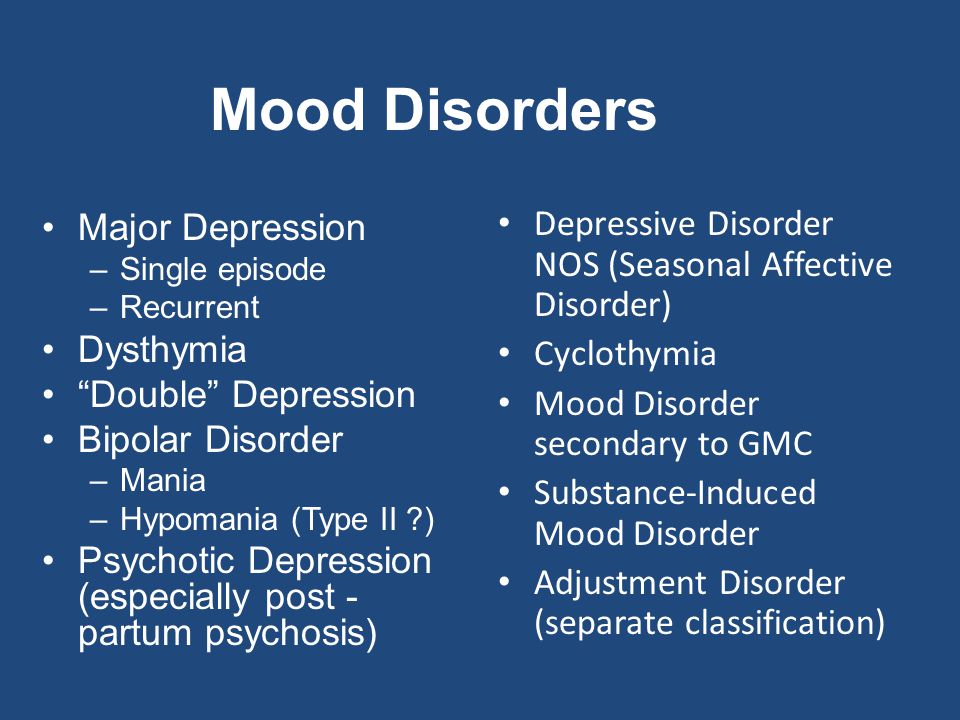
Postpartum or postnatal depression is a mental illness that must be taken very seriously. As a rule, it is sluggish and is closely associated with the birth of a child.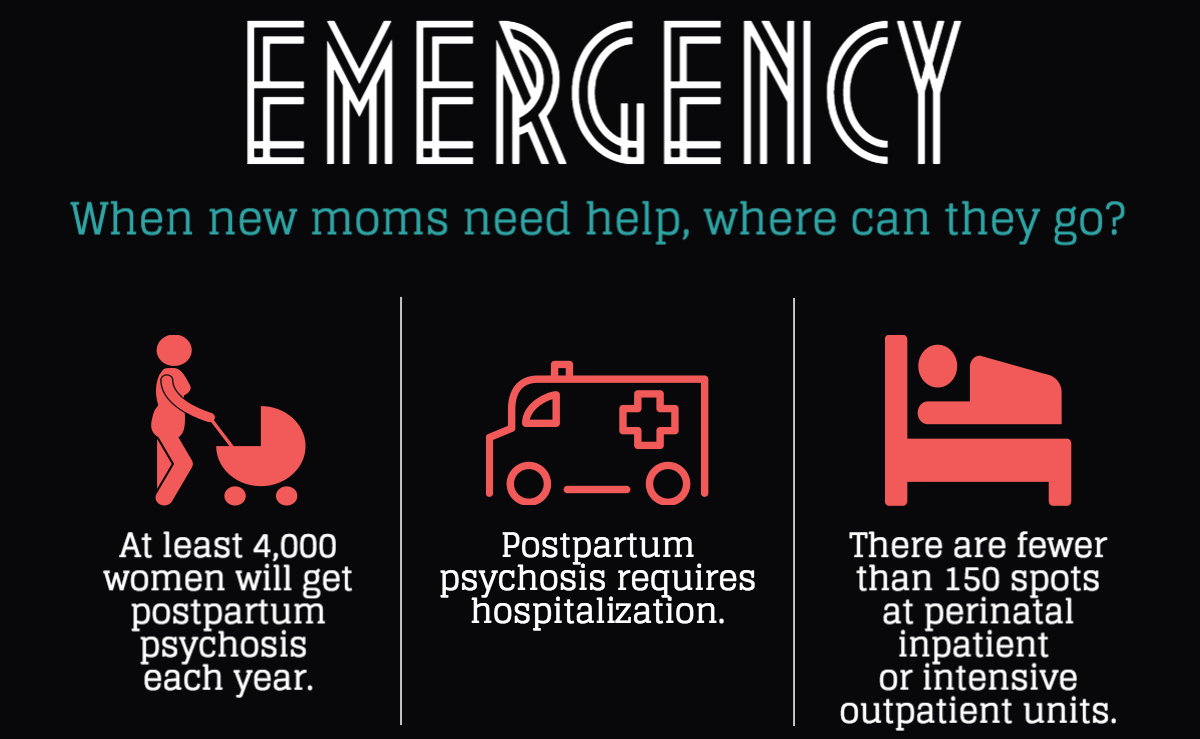 Depending on the severity and severity of the symptoms, three forms of the disease are distinguished:
Depending on the severity and severity of the symptoms, three forms of the disease are distinguished:
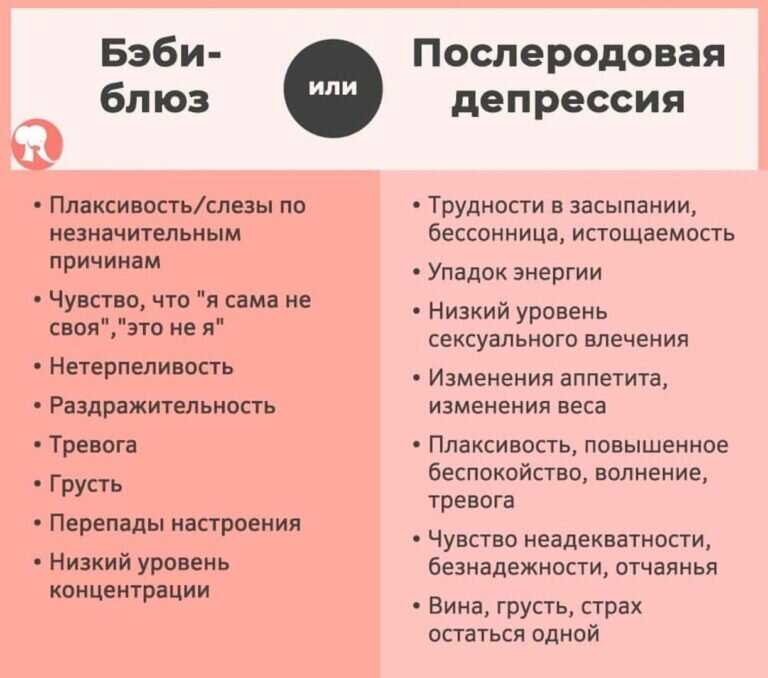
- postpartum blues or "weeping days";
- postpartum depression;
- postpartum psychosis.
Postpartum blues: what are “weeping days”?
A few days after giving birth - around the time milk comes in - 50-80 percent of all mothers experience a bad mood - the so-called postpartum blues. It is characterized by mild psychological distress and hypersensitivity, accompanied by depression, fear of failure, frequent crying, sleep problems, and exhaustion. "Days of crying" tend to pass fairly quickly. They are considered the mildest form of postpartum depression. The main reason for the occurrence is a sharp drop in the hormones estrogen and progesterone immediately after childbirth. Estrogen, in particular, has an improving and stabilizing effect on the brain. There are also many changes in daily life and in the relationship of the couple that the child brings with it, including lack of sleep. When hormone levels in the body level off again after a few hours or a few days, and daily life with a child becomes more routine, the symptoms of the disease in most women quickly disappear on their own. Treatment in such cases is usually not required. At this stage, it is very important to provide the woman with advice and advice from her doctor or midwife, as well as help and support from a partner and other close relatives.
When hormone levels in the body level off again after a few hours or a few days, and daily life with a child becomes more routine, the symptoms of the disease in most women quickly disappear on their own. Treatment in such cases is usually not required. At this stage, it is very important to provide the woman with advice and advice from her doctor or midwife, as well as help and support from a partner and other close relatives.
What is postpartum depression?
However, if symptoms persist for more than two weeks, increase and become fixed, or similar symptoms recur and persist during the first two years after childbirth, this may be a sign of the onset of postpartum depression. Postpartum depression develops in 10-15 percent of all women in labor. Postpartum or postnatal depression is a very serious mental illness. It usually develops in a sluggish manner. The first signs usually appear about 4-6 weeks after birth. However, they can also occur later, up to two years after childbirth.
Because of illness, such women are unable to develop positive feelings for the child and to care for him lovingly, they often feel a strong sense of guilt. They are very ashamed, they feel like bad mothers and hide their feelings from others. Often, patients completely withdraw into themselves and isolate themselves from the outside world. Only a few find the courage to trust other people. As a result, postpartum depression is often recognized too late, and sometimes not detected at all.
Unlike the postpartum blues, postpartum depression does not go away on its own. This can have serious consequences for the health of the mother and child. Therefore, these cases require mandatory treatment by a specialist.
What are the symptoms of postpartum depression?
Typical signs of postpartum depression:
- constant sadness;
- frequent crying;
- sleep disorders;
- feeling of emptiness;
- anxiety;
- mental overload;
- self-doubt;
- trouble concentrating;
- psychosomatic effects such as headaches, dizziness, heart problems, etc.
 ;
; - loss of appetite;
- aversion to sex;
- indifference;
- self-neglect;
- lack of empathy for the child;
- feelings of shame and guilt;
- self-isolation and loneliness.
Postpartum psychosis: what is it?
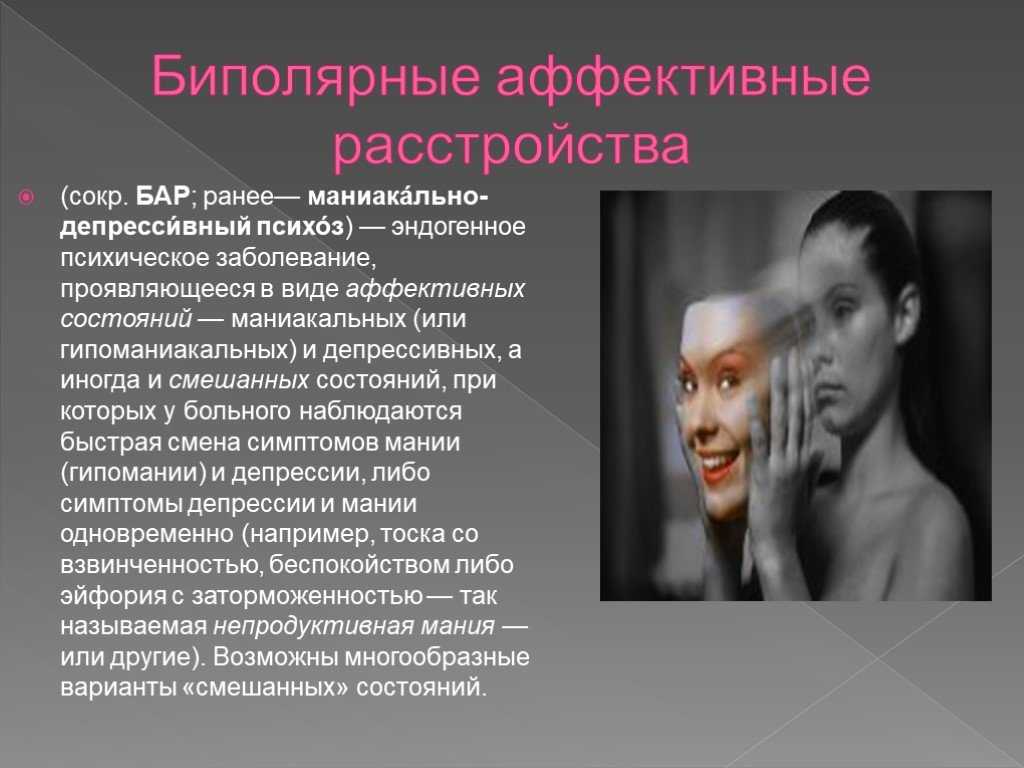
Postpartum psychosis is the most severe form of postpartum depression. Occurs very rarely. Only 0.1–0.3 percent of women in labor suffer from this disease, i.e. 1-3 out of a thousand. This is a severe depression in which, in addition to the symptoms of postpartum depression, there are also signs of psychosis. These include personality and behavioral changes that can pose a serious risk to mother and baby. Therefore, postpartum psychosis always requires emergency medical care with treatment in a hospital.
What are the symptoms of postpartum psychosis?
The first signs of postpartum psychosis usually appear within the first six weeks after delivery. In addition to the typical signs of postpartum depression, such as deep sadness, indifference, apathy, anxiety, etc., there are also symptoms of psychosis. These include:
In addition to the typical signs of postpartum depression, such as deep sadness, indifference, apathy, anxiety, etc., there are also symptoms of psychosis. These include:
- crazy ideas;
- hallucinations;
- severe anxiety;
- anxiety;
- confusion;
- disorientation;
- obsessive thoughts about hurting yourself or a child;
- thoughts of suicide.
Causes of postpartum depression
The causes of postpartum depression, or postnatal psychosis, are still not fully understood. What is certain, however, is that there are many causes of the disease, and the development of postpartum depression requires a combination of various factors. These include:
Biological risk factors
- Hormonal changes
Strong hormonal changes after childbirth are an important factor in the development of postpartum depression. Among other things, the concentration of female sex hormones progestogen and estrogen drops sharply. But because estrogen, in particular, has a stabilizing and mood-enhancing effect on the brain, a sharp drop in hormone levels often manifests itself in a depressive mood. Most women are already familiar with these mood swings in a much milder form - hormonal changes during the menstrual cycle. Women who are particularly sensitive to hormonal changes, such as those who suffer from premenstrual dysphoric disorder or who react to mood swings to the use of hormonal contraceptives, are at increased risk of postpartum depression.
Among other things, the concentration of female sex hormones progestogen and estrogen drops sharply. But because estrogen, in particular, has a stabilizing and mood-enhancing effect on the brain, a sharp drop in hormone levels often manifests itself in a depressive mood. Most women are already familiar with these mood swings in a much milder form - hormonal changes during the menstrual cycle. Women who are particularly sensitive to hormonal changes, such as those who suffer from premenstrual dysphoric disorder or who react to mood swings to the use of hormonal contraceptives, are at increased risk of postpartum depression.
- Lack of sleep
Childbirth and aftercare is extremely tiring. Many women suffer from severe sleep deprivation, which can lead to physical and mental exhaustion, as well as metabolic imbalance. In addition, uncertainty and excessive demands often arise due to a new situation, a new role, changing partnerships and constant concern about the correctness of one's actions.
Risk factor - previous illnesses
Past mental illness and depression, psychosis and anxiety disorders during pregnancy are also significant risk factors. According to a 2006 study 1) , women with untreated depression are 7 times more likely to develop postpartum depression after giving birth.
1) Ross LE, McLean LM Anxiety disorders during pregnancy and the postpartum period: a systematic review. Depression 2006; 6:1-14
Social risk factors
Risk factors for postpartum depression also include: lack of support from partners and the social environment or even domestic violence, previous breakup or divorce, unwanted pregnancy, twins or multiple pregnancy, and problems with the health of the child or "crying" children.
Risk factor - trauma
Traumatic childbirth experiences, traumatic experiences and neglect in one's own childhood, the death of a loved one during pregnancy, and other hardships and critical life events can contribute to the development of postpartum depression.
Postpartum depression: consequences for mother and child
A mother who is unable to enjoy motherhood is still considered taboo in society. Therefore, sick mothers are often hesitant to talk about their problems. As a result, the clinical picture of postpartum depression is often detected late, and, accordingly, the disease is treated at a late stage. This creates a consistently high level of distress for the mother, which in the worst case can lead to suicide or even extended suicide (killing the child). The child may have sleep disturbances, developmental delays, problems with breastfeeding, behavioral problems, and attachment disorders. In the long term, emotional and cognitive impairments can also occur, which can manifest themselves in adulthood.
Common comorbidities of postpartum depression
Other psychiatric comorbidities may occur in addition to or in conjunction with postpartum depression. These primarily include:
—Anxiety disorders
In addition to general fears, there are often exaggerated fears about the well-being of the child, as well as strong fears and insecurity about proper care for him. In addition, it can also lead to panic attacks.
In addition, it can also lead to panic attacks.
—Obsessive Compulsive Disorders
Obsessive compulsive disorders often occur in connection with postpartum depression, associated with constant bathing and disinfection with accompanying frightening obsessive thoughts about harming yourself and the baby.
Treatment: how to treat postpartum depression?
Thus, the clinical picture of postpartum depression is extremely complex, because on the one hand it is necessary to find out the causes and severity of the disease, and on the other hand, symptoms and concomitant diseases. Treatment complicates the fact that it is necessary to treat not only the sick mother, but above all to improve and normalize her relationship with the child. Traditional medicine involves the use of psychotherapy, assistance and relief in daily life, as well as the use of psychotropic drugs.
However, the use of drugs can be problematic for breastfeeding mothers, since most of the active ingredients can pass into breast milk.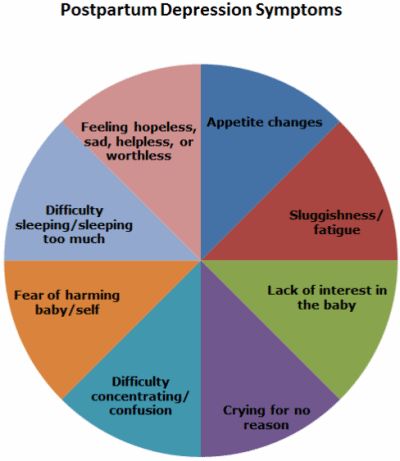
We offer an alternative!
The CALDA Postpartum Depression Treatment Program is a therapy program specifically designed for women with postpartum depression that does not use psychoactive drugs whenever possible!
The CALDA concept: we will give you back the enjoyment of every moment of life with your baby!
As a CALDA client, you have every right to take your child with you at any time. It's even recommended! Our luxurious residences are optimally prepared for the special needs of mothers with children. Throughout your stay in the clinic, your baby will be lovingly looked after and cared for around the clock by a specially trained pediatric nurse, and you will receive individually tailored 1:1 therapy in accordance with the CALDA Postpartum Depression Treatment Program.
This is a personalized, highly effective, holistically oriented ultra-precise therapy: scientifically based methods of classical medicine are combined with specially approved methods of complementary, traditional Chinese (TCM) and orthomolecular medicine.
Your baby is always with you!
Of course, whenever possible, we always include the child in your treatment program or adjust it accordingly for you. This allows you to maximize the long-term relationship between you and your child, filled with love and tenderness.
Your benefit: Treatment with the CALDA concept works very effectively at different levels of the body and is problem oriented. As a result, amazing results can be achieved in a short time - and often without the use of psychotropic drugs!
The CALDA concept
Our motto and guarantee:
we treat the causes, not the symptoms!
If possible, we work without psychotropic drugs!
Our time and all our know-how is an exclusive service for a specific client.
The CALDA concept: every therapy is based on a correct diagnosis
A comprehensive and detailed diagnosis is the basis of every treatment according to the CALDA concept.