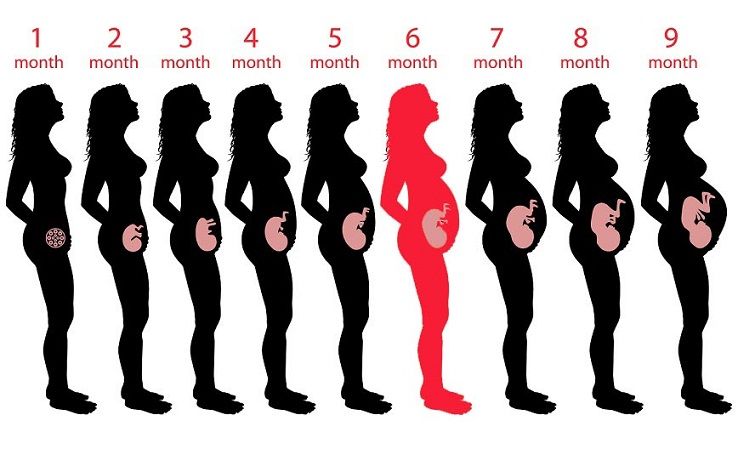
Pain in 7 month pregnancy
7 Months Pregnant: Symptoms and Fetal Development
Now that you’re seven months pregnant, your little one is growing quickly and starting to look more and more like the baby you’ll soon meet. For example, she’s plumping up and her skin is becoming less transparent. Your belly is also growing, and you may face some physical challenges as a result. Try to keep in mind that every day that brings you back pain or tiredness also brings you one day closer to meeting your baby. Read on to find out what kinds of things may be in store this month from symptoms to baby development and more.
Common Pregnancy Symptoms at 7 Months Pregnant
You’re entering the third trimester — the home stretch! Around this time, it’s common to feel the effects of your growing tummy and progressing pregnancy. Symptoms at seven months pregnant can include:
Sciatica. As your uterus grows, it can put pressure on the sciatic nerve, which can then cause hip or lower back pain.
If the pain starts in your lower back or hip and travels down one leg, it could be sciatica, but only your healthcare provider can make a diagnosis. A hot or cold pack can help relieve the pain, and your provider can recommend stretches. If, at any time, you notice numbness in your legs or feet, let your provider know right away. Sciatica is likely to go away after your baby is born.
Pelvic pain. Pregnancy hormones do strange and unexpected things to your body. For example, they help loosen the joints that connect the two sides of your pelvis in preparation for labor and delivery. This can cause pelvic pain. If this strikes, try to stay off your feet as much as possible. Your healthcare provider can also give you stretches to do that may help ease your discomfort.
Constipation. Higher levels of the hormone progesterone and iron (if it’s in your prenatal vitamins) can slow digestion, making you feel blocked up. To help alleviate constipation, keep yourself hydrated (water and prune juice are great) and make sure you’re getting enough fiber in your diet.
 Good sources of fiber include beans, whole grains, fruits, and veggies.
Good sources of fiber include beans, whole grains, fruits, and veggies. Braxton Hicks contractions. Sometimes called practice contractions, Braxton Hicks contractions can begin in the second or third trimester. They sometimes feel like a slight tightening in your abdomen, and they usually go away when you move or change positions. They’re more likely to occur later in the day, and after physical activity like exercising or sex. Read up on Braxton Hicks contractions and speak to your healthcare provider if you’re unsure whether you’re experiencing practice or real contractions.
Fatigue. Some moms-to-be experience a boost of energy during the second trimester, but as you begin the third trimester, you may start to feel a little more tired. One reason for this is that by seven months pregnant your belly has grown quite a bit, and it may be more difficult to get a restful night’s sleep. Try to rest when you can — even if that means taking some time out during the day — and sleep on your side using a pillow to support your growing bump.
 Maintaining a healthy diet and moderate exercise routine can also help you sleep better and keep your energy levels up.
Maintaining a healthy diet and moderate exercise routine can also help you sleep better and keep your energy levels up. Bleeding or spotting. Some light bleeding or spotting can happen around this time. Although it may not be anything serious, check with your healthcare provider, just in case. Bleeding can sometimes be a sign of a problem, so consulting your provider can give you peace of mind.
How Is Your Baby Developing This Month?
When you’re seven months pregnant, your baby is busy developing those organs and systems that will help her survive outside the womb. For example, her lungs are starting to produce a substance called surfactant, which allows her lungs to expand and contract properly.
Other big news: your little one can now open and close his eyes! You’re probably eager to see those little peepers, and it won’t be long now! In the meantime, your baby may be able to sense changes in light and dark, and might respond to bright lights by moving or kicking. She’s also fattening up (becoming even more adorable), and this extra fat helps to smooth out the wrinkles in her skin. Her skin cells, meanwhile, are starting to produce melanin, which is a natural pigment that helps give skin its color.
She’s also fattening up (becoming even more adorable), and this extra fat helps to smooth out the wrinkles in her skin. Her skin cells, meanwhile, are starting to produce melanin, which is a natural pigment that helps give skin its color.
How Big Is Your Baby When You’re 7 Months Pregnant?
So, what’s your baby’s approximate size when you’re seven months pregnant? Your baby could weigh about 2.5 pounds and measure 14 inches at this time.
Related pregnancy tool
Fill out your details:
Pre-pregnancy weight (lbs.)
This is a mandatory field.
Height (ft.)
This is a mandatory field.
Height (in.)
Current week of pregnancy (1 to 40)
This is a mandatory field.
Tick the box
I'm expecting twins
What Does a Fetus Look Like at 7 Months?
Check out these illustrations for a glimpse at what your baby might look like when you’re seven months pregnant:
7 Months Pregnant: Your Body’s Changes
In your third trimester, you could gain as much as a pound a week. Using our Weight Gain Calculator, you can learn how to calculate your pre-pregnancy body mass index, or BMI (if you don't know that value already) and then get a basic overview of the weight gain ranges that might be acceptable for someone of your pre-pregnancy BMI. You can use the information you get to talk to your healthcare provider about the healthy pregnancy weight gain that’s right for you, and how to stay on track.
As your belly grows, and likely some time when you’re seven months pregnant, your healthcare provider will start to measure your fundal height. This is the distance between your pubic bone and the top of your uterus. This distance is measured in centimeters, and often corresponds closely to the week of your pregnancy. So, if you’re 28 weeks pregnant, it’s quite likely that your fundal height measurement will be something like 28 centimeters (11.02 inches), or very close to it. This measurement is just a tool to track your baby’s steady growth, and the measurements may not be exact for all moms-to-be.
This is the distance between your pubic bone and the top of your uterus. This distance is measured in centimeters, and often corresponds closely to the week of your pregnancy. So, if you’re 28 weeks pregnant, it’s quite likely that your fundal height measurement will be something like 28 centimeters (11.02 inches), or very close to it. This measurement is just a tool to track your baby’s steady growth, and the measurements may not be exact for all moms-to-be.
How Far Along Are You at 7 Months Pregnant?
At seven months pregnant, it’s generally accepted that you’re at the very beginning of the third trimester. It's a little trickier to determine how many weeks seven months pregnant is. The weeks of pregnancy don’t fit neatly into months, so seven months can begin between 25 weeks and 27 weeks pregnant and extend up to 28 to 31 weeks.
Checklist for When You’re 7 Months Pregnant
If you have had a cesarean section before and would now like to try for a vaginal delivery, ask your healthcare provider whether you might be a good candidate for a VBAC (a vaginal birth after a cesarean delivery).
Consider whether you’d like to hire a labor support person called a doula and ask your healthcare provider or other moms in your area for recommendations.
Ask your healthcare provider about counting your baby’s movements at seven months pregnant. Download our Fetal Movement Tracker to help.
If you know and would like to share your baby’s gender before her birth, why not hold a gender reveal party this month? See our guide on planning a gender reveal party as well as our creative ideas for how to actually reveal your baby’s gender at the party.
If the search continues for the perfect baby name, try our Baby Name Generator for inspiration.
Download our Pampers Club app to learn how you can earn gifts and discounts on all those baby products you’ll soon be needing!
Put the finishing touches on your baby shower registry by checking our comprehensive list of registry must-haves to make sure you haven’t forgotten something important.
Consider whether you’ll store or donate your baby’s umbilical cord blood. Your provider can give you more information about your options.
If you are thinking of making a birth plan, download our Birth Plan Guide to help organize your thoughts.
If you’re starting to shop for baby gear items or would like more inspiration on what to add to your registry list, check out the best baby products as voted by Pampers Parents. We surveyed thousands of Pampers Parents to find out which specific items they love and recommend, and we reviewed all their favorites so you can make the right choice for you and your little one.
Sign up for even more weekly pregnancy tips here:
8 third trimester pains and how to deal with them | Your Pregnancy Matters
Congratulations! You’ve made it through the early pregnancy morning sickness and fatigue. Now it’s the third trimester and you’re so close to meeting baby. Unfortunately, there may be a few uncomfortable symptoms still in store for you.
Swelling ankles, trouble sleeping, back pain, having to go to the bathroom every 20 minutes – these are all possibilities as you move into the pregnancy homestretch.
Patients often ask me how to make the third trimester a little more comfortable. This topic has been on my mind more in the last few months as my sister, Toral Patel, who is a neurosurgeon at UT Southwestern Medical Center, entered her third trimester and began dealing with some of these discomforts.
Let’s take a look at eight common symptoms during the third trimester of pregnancy: What causes them, how to help relieve them, and when you should call your doctor.
1. Swelling
Why it happens: When you hit 30 weeks of pregnancy, it may not just be your belly that’s swelling. You also may notice swelling (edema) in other parts of your body, especially in your lower extremities, such as your feet and ankles.
During pregnancy, your body produces about 60 percent more blood volume. Meanwhile, your growing uterus is putting pressure on the large veins that return blood to your heart, leaving all the extra fluid to pool in your lower limbs.
This pressure also may cause some veins to become swollen or look purple or blue. These are called varicose veins, and they should go back to normal after the birth of the baby.
What you can do: The best thing you can do to avoid or reduce swelling is to reduce how long you’re on your feet. If you have to stand for a long period of time, take a break every couple hours to sit down and put your feet up for 10 minutes. This helps gravity pull fluids from the legs back into your circulatory system.
One of the best times to put your feet up is after dinner. While you don’t have to have them straight up, get them as high as you can. I often tell patients to prop their feet up on a few pillows on the coffee table. I recommend doing this a few hours before bed because all those fluids that you’re helping return to the heart will be filtered by the kidneys and you’ll have to pee it all out. If you elevate your feet right before bed, you’ll likely have to get up right as you’re falling into a deep sleep to use the bathroom!
When you need to be on your feet for a long time, wear compression stockings, or TED hose.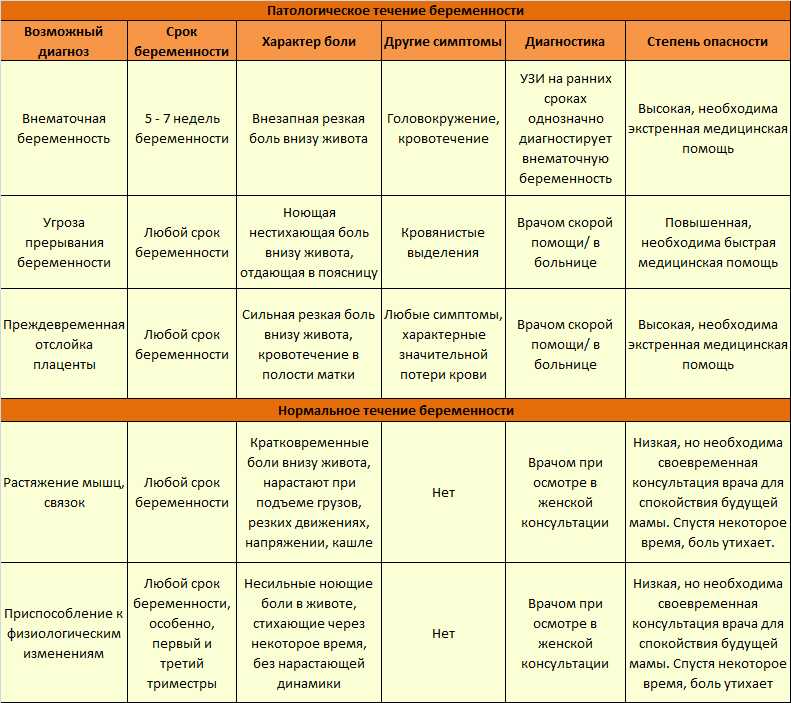 These can go from your feet up to your knees or mid-calves. They help move fluids up to the heart and keep them from pooling in your legs. If you’re picturing your grandma’s stockings, don’t worry. Many manufacturers are making much more stylish versions these days. You wouldn’t even know some of them are compression stockings!
These can go from your feet up to your knees or mid-calves. They help move fluids up to the heart and keep them from pooling in your legs. If you’re picturing your grandma’s stockings, don’t worry. Many manufacturers are making much more stylish versions these days. You wouldn’t even know some of them are compression stockings!
If your shoes are starting to feel tight, wear shoes with straps you can loosen. Or if it’s nice out, throw on some flip flops.
When to be concerned: If you notice sudden swelling, asymmetric swelling – such as one leg being larger than the other – or one calf being warm or tender to the touch, see your physician right away. These could be signs of a blood clot. Swelling in non-dependent parts of your body like hands and fingers may suggest the development of preeclampsia.
2. Insomnia
Why it happens: Insomnia – trouble falling asleep or staying asleep – often occurs in the first and third trimesters, although for different reasons. In the first trimester, it’s a result of hormonal changes, specifically due to a surge of progesterone. However, your progesterone levels off in the second trimester, returning you to peaceful slumber.
In the first trimester, it’s a result of hormonal changes, specifically due to a surge of progesterone. However, your progesterone levels off in the second trimester, returning you to peaceful slumber.
In your third trimester, sleep becomes more elusive because it’s difficult to get comfortable due to your growing belly.
What you can do: Find the position that’s most comfortable for you to sleep in, whether it’s your left or right side. It doesn’t matter which side you pick. Sleeping on your back is likely not comfortable, but if you want to sleep this way, it helps to shift your hips just a little to keep all the weight from being on your back.
There are a variety of body pillows you can try. My sister particularly liked the Snoogle pillow, which is C-shaped and goes up under the neck, around the shoulders, and between the legs.
Practice good sleep hygiene, such as not watching TV or looking at your phone right before you go to sleep. Other things you can try before going to bed are sipping warm milk or tea, taking a warm bath, or using lavender scents in your bath or lotion.
When to be concerned: If you’ve tried all of these things and you still can’t sleep, talk to your physician about which over-the-counter medications may be safe to take.
3. Reflux and feeling full faster
Why it happens: You may find that you can’t eat as much as you used to or that you’re experiencing reflux. As your uterus gets bigger, it begins to push up on your stomach. This means there just isn’t as much space for food. Also, the sphincter between your stomach and esophagus doesn’t work as well during pregnancy.
What you can do: Eat five small meals each day instead of three larger meals. Find foods that make you feel less full without lowering your caloric intake. For example, try a protein shake instead of a big sandwich.
If you’re having problems with reflux, avoid foods that are spicy or acidic. Instead, choose foods that are creamy, such as yogurt. Don’t eat within two hours of going to bed to allow foods time to leave your stomach prior to going to bed. Elevating your head and not lying flat also helps to avoid reflux.
Elevating your head and not lying flat also helps to avoid reflux.
When to be concerned: If you continue to have problems with reflux, talk to your doctor about an over-the-counter medication. If you are having reflux that is not related to something you ate, or you are experiencing heartburn or abdominal pain that doesn’t go away with medications such as Tums or Maalox, see your doctor. This could be an indication of a serious problem, such as preeclampsia.
4. Restless leg syndrome
Why it happens: Restless leg syndrome is a sensation of needing to move your legs. This can manifest in many ways, from a general feeling of discomfort to a burning or throbbing sensation. My sister said it made her feel like she needed someone to pull on her legs.
Restless leg syndrome is more common in the evening, making it impossible to fall asleep. While there are theories out there, we’re not 100 percent sure why restless leg syndrome affects so many pregnant women.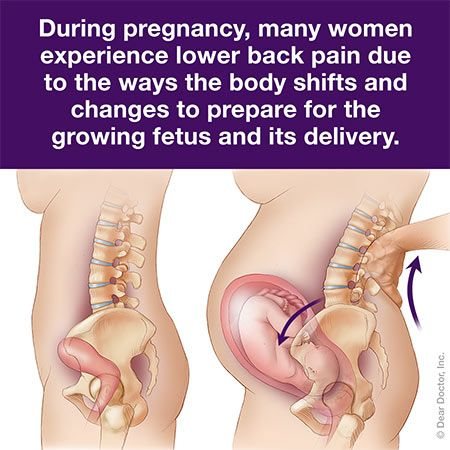
What you can do: There’s no real cure for restless leg syndrome, but there are lifestyle changes you can make to relieve the symptoms, including staying hydrated. We recommend pregnant women drink 80 to 100 ounces of water each day. Calcium and vitamin D supplements also may help.
Take a 20- to 30-minute walk around the time your legs are most restless to relieve the sensation. You also can try massaging the legs or using heat or ice packs.
When to be concerned: If these tricks don’t relieve your symptoms and your sleep is affected, talk to your doctor about medication.
5. Back and hip pain
Why it happens: Increased levels of progesterone during pregnancy relax the joints and muscles to accommodate the growing uterus and enhance flexibility in your pelvis so the baby can pass through the birth canal more easily. However, this also can cause pain.
Your posture may change due to carrying extra weight around. You may find yourself leaning more to one side or another, which can lead to lower back or hip pain.
What you can do: Wear a support belt under and over the belly to take some of the weight off the hips and back. There are a wide variety of types and brands to choose from. This won’t hurt your baby, so tighten it enough to get the support you need.
When you sit down, place pillows under your hips or try sitting on a balance or yoga ball instead of a chair. Take a warm bath or use a heating pad on your hips or back to help relieve the pain.
Remember, thanks to your growing belly, your center of gravity is much different these days. Skip the stilettos until after you give birth.
When to be concerned: If you have unrelenting pain, a deep and sharp pain, or have become unable to walk or get up, see your doctor. Also, if you are experiencing a rhythmic pain in your low back every few minutes, it may be contractions, which sometimes present as low back pain.
6. Breast pain
Why it happens: Sore breasts are common during pregnancy. Hormonal changes are preparing them to feed your baby, and you may find you go up a few cup sizes.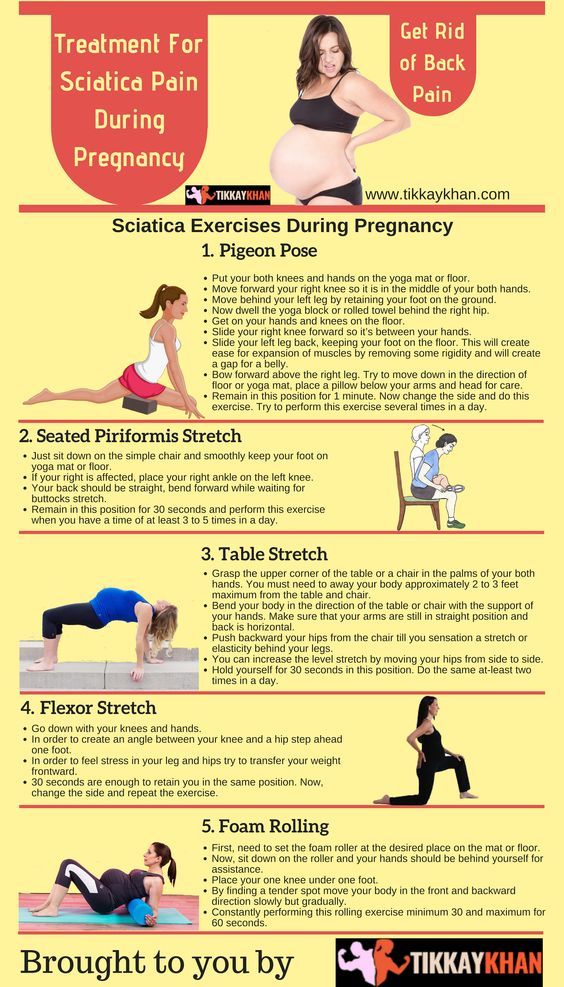 Women with smaller breasts may find they have more pain than women with larger breasts.
Women with smaller breasts may find they have more pain than women with larger breasts.
What you can do: I see too many women in their third trimester try to wear the same bras they did before pregnancy. Plan to buy new bras a couple times as your breasts grow throughout pregnancy – your breasts and back will thank you.
When to be concerned: Sports bras may be comfortable during and right after pregnancy, but if they are too tight, they can inhibit milk production. We advise women who don’t want to breastfeed to wear a sports bra to help dry up their milk. If you plan to breastfeed, make sure your bra has good support, but don’t let it get too tight.
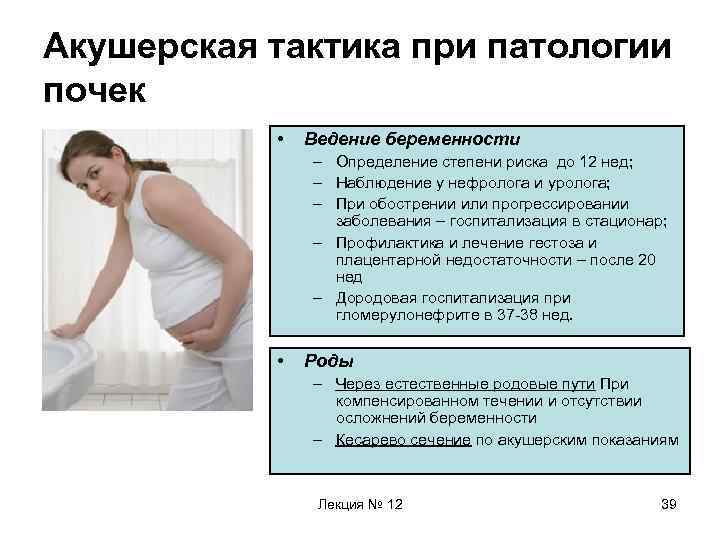
7. Frequent urination
Why it happens: Needing to run to the bathroom frequently may be the most annoying part of the third trimester. The volume of fluids running through your kidneys doubles during pregnancy, meaning you will need to pee twice as much. As your baby grows, he or she also may press on your bladder.
What you can do: Unfortunately, there’s not much you can do about this. Don’t stop drinking liquids in order to avoid frequent urination. You need to stay hydrated. Dehydration can cause contractions, dizziness, and lightheadedness.
Know you’re going to need to pee more often and prepare for it. For example, sit on the aisle or near the exit when at an event.
When to be concerned: Sudden changes in urination may be cause for concern, such as if you’re peeing far more today than you were yesterday. Also, if you experience pain or burning when you urinate, or if there is blood in your urine, see your doctor right away.
8. Lightheadedness and dizziness
Why it happens: Along with swelling, fluid pooling in your legs instead of circulating throughout the body can cause dizziness or lightheadedness. You may notice this more when you have been standing for a prolonged period of time or when you get up too quickly.
What you can do: Again, compression stockings can help by pushing blood out of the legs and to the heart. If you have to stand for a long time, keep moving to increase circulation – shuffle your feet or bend your knees by bringing your lower leg up toward your rear end a few times.
If you have to stand for a long time, keep moving to increase circulation – shuffle your feet or bend your knees by bringing your lower leg up toward your rear end a few times.
Avoid getting up too quickly from sitting and lying positions. When you’re ready to get out of bed in the morning, sit up, put your feet on the floor, and wait a minute before you stand up and go. This will give your body time to adjust. This is another instance in which staying properly hydrated will help.
When to be concerned: If you are constantly feeling lightheaded or dizzy, if it happens even after a short period of standing, or if it’s accompanied by a racing heartbeat, call your doctor.
The upside to dealing with all of these issues? You are getting close to the end of the pregnancy! We understand these problems can make the third trimester feel like it will never end. However, a few simple changes can make it a little more comfortable. And remember, it’s worth it. Just ask my sister, who gave birth May 6, 2016, to a perfect little boy, Elliott.
If you have questions about any third-trimester symptoms you are experiencing, request an appointment online or call 214-645-8300.
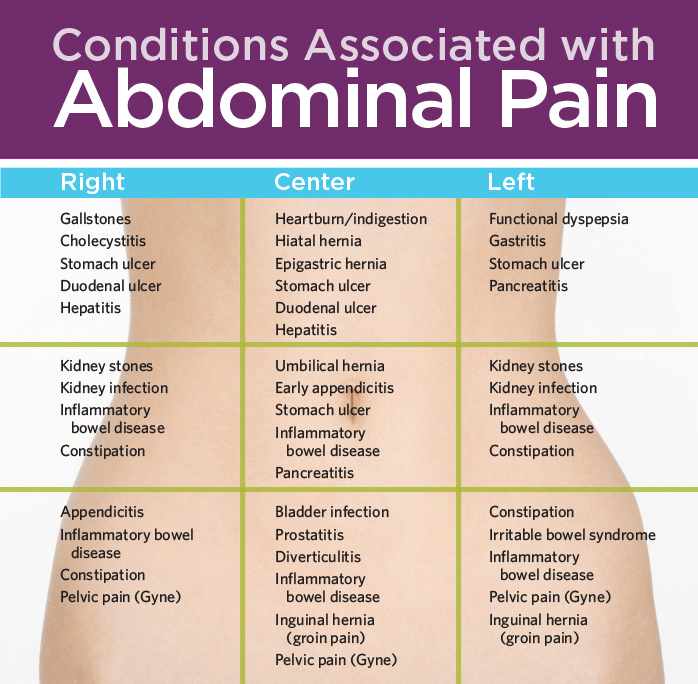
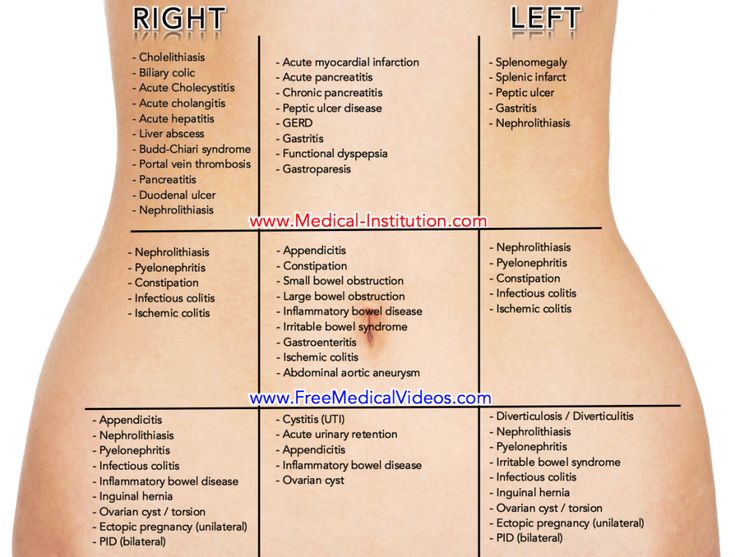
Abdominal pain during pregnancy
Abdominal pain in a pregnant woman can be felt for various reasons. In some cases, this is a natural reaction of the body to changes occurring in the body. In some - an alarming symptom that requires urgent medical intervention.
Consider the most common causes of abdominal pain in pregnant women.
Fatigue
The most obvious cause of pulling pains in the abdomen, especially in the later stages. Due to the weight of a growing belly, the body gets tired faster, and even habitual physical activity can cause fatigue, shortness of breath and pain. Naturally, this pain goes away during rest.
Ectopic pregnancy
If the fetal egg is not fixed in the uterus, but outside it, the pregnancy is called ectopic. After 2-3 weeks, the growing embryo begins to damage the surrounding tissues and organs - for example, a rupture of the fallopian tube often occurs. With this dangerous pathology, a woman's life is in danger, urgent hospitalization and surgical intervention are necessary. Therefore, it is very important to visit the antenatal clinic, where the doctor will determine whether the fetal egg is fixed in the uterus.
With this dangerous pathology, a woman's life is in danger, urgent hospitalization and surgical intervention are necessary. Therefore, it is very important to visit the antenatal clinic, where the doctor will determine whether the fetal egg is fixed in the uterus.
Growing pain
As the baby grows in the uterus, the uterus stretches. Most often, a woman does not notice this. But in some cases, the stretching of the uterus is felt and causes pain. Often this happens when the uterus is in hypertonicity. This reason is natural and practically not dangerous.
Compression of internal organs
A growing baby not only stretches the uterus, but also gains weight. In some positions, the uterus presses on adjacent organs, which also causes pain, especially when the child moves. Sometimes it is enough just to move, change the position of the body, so that the squeezed organ is released and the pain is gone.
Constipation
Due to changes in metabolism, as well as the weight of a growing belly, the intestines may not be active enough to perform their functions, and the pregnant woman suffers from constipation. A mild laxative will help ease the bowel and relieve pain.
A mild laxative will help ease the bowel and relieve pain.
Read in our media center: "What is the luteal phase." Find out why it is so important, what happens to a woman's body during the luteal phase and how it affects the skin.
Appendicitis
Not very often - about 1 in 10,000 pregnancies - the weight of the growing belly leads to inflammation of the appendix. Sometimes this inflammation goes away on its own, the woman does not even have time to understand what is the cause of the pain. But if the inflammation progresses, surgery may be needed. As with any inflammatory process, body temperature rises with appendicitis. In combination with the characteristic pains, the temperature gives a clinical picture that will allow the doctor to make a correct diagnosis.
Training contractions
In the third semester, pregnant women often experience rhythmic uterine contractions, which can be quite painful. As a rule, they are safe. But if the contractions are strong, frequent and do not stop, you should call an ambulance.
As a rule, they are safe. But if the contractions are strong, frequent and do not stop, you should call an ambulance.
Placental abruption
This is an alarming symptom that is fraught with abortion. For various reasons, the placenta begins to exfoliate from the walls of the uterus. This is fraught with metabolic disorders of the fetus and spontaneous abortion. Usually, a woman notices spotting from the vagina. It is recommended to go to the hospital.
Miscarriage
Of all the listed causes of abdominal pain, this is one of the most dangerous. Spontaneous abortion can occur at any time, although in the first half it is called autoabortion, and in the later stages - premature birth. The fact that this is the cause of the pain can be recognized by a combination of several signs: pulling pains in the lower abdomen, spotting, preliminary contractions. Without medical assistance, the life of both the fetus and the mother is at risk.
What to do if you experience lower abdominal pain during pregnancy:
- Change body position: stand up or lie down, find a comfortable position.
- Remember what and when you last ate, when you emptied your bowels.
- Measure the temperature.
- Check for bloody or other discharge from the genitals.
- Determine if there are contractions.
If the pain is severe, accompanied by discharge, contractions and fever, call an ambulance.
If the pain is tolerable, disappears rather quickly, there is no discharge, it is worth telling the doctor about this at the next visit to the antenatal clinic.
Make an appointment with a gynecologist
View prices and services
Why does my stomach pull in early pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are quite physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy can be:
- "obstetric";
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- miscarriage;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus.

Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good if the menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
Each woman is individual.
If each menstruation is preceded by unpleasant painful sensations in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the introduction of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.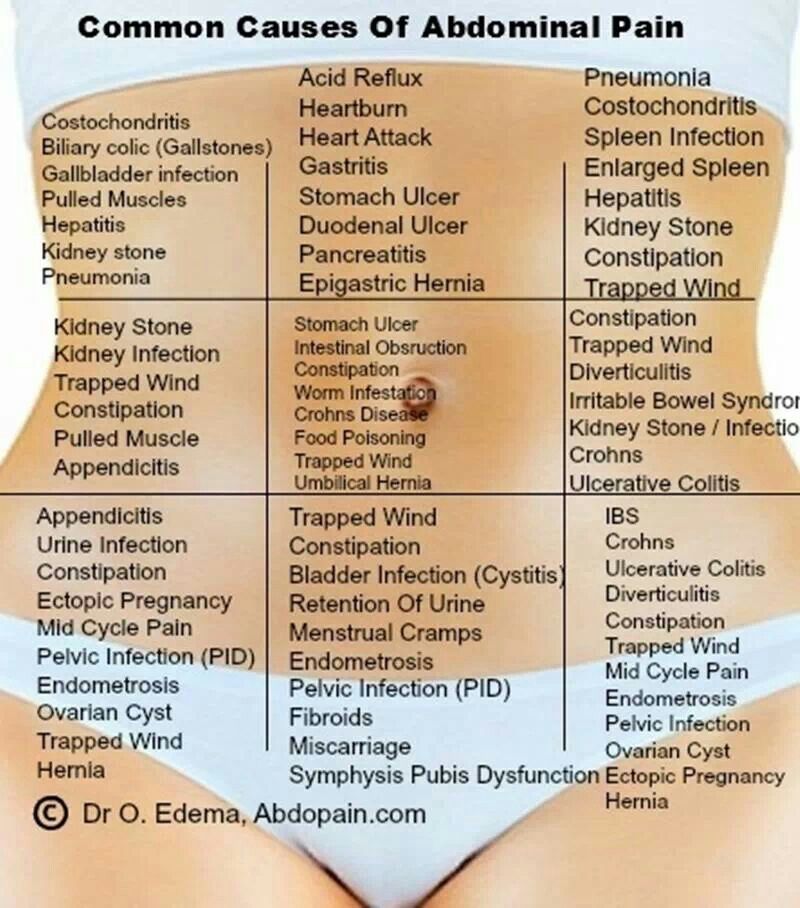
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Causes that may cause miscarriage include:
- heavy physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from threats of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.

- bloody discharge from the genital tract.
If you experience pain in the lower abdomen, you should consult a doctor, as a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance must be called if:
- pain in the lower abdomen increases;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be sparse, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Missed pregnancy
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, miscarriage occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes, due to which there are pulling pains in the lower abdomen, inflammatory processes of the pelvic organs are most common. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Due to the anatomical features of a woman, cystitis can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.