Pin prick rash on face
Red Pin Prick Rashes and Spots
If spots are accompanied by any of the following symptoms and your child appears to be more unwell then seek urgent medical attention.
- Drowsiness
- Unresolving high temperature/fever
- Floppy body tone (your child looks and feels like a rag doll when you pick them up)
- Confusion/difficulty awakening
- Severe/worsening headaches
- Very pale skin
- Seizures, fits (convulsions)
- Shortness of breath
- A sharp chest pain that feels worse with breathing
- Coughing up blood.
Go to your nearest accident and emergency department or call 999 for an ambulance if you or your child develops any of these symptoms.
Here Jackie lists some of the most common spots and rashes to watch out for:
1. Meningitis
This is the scary one every parent dreads. Remember though, a rash is often one of the last signs of meningitis or septicaemia, so do see a doctor if you are concerned about any of these symptoms:
What to look for
“A child with meningitis would normally be very unwell with reddish/purple spots which look a little like tiny fresh bruises on the skin – the key is that these do not blanch in colour when you press on them. The glass test is a very useful way to check,” explains Jackie. “This is if you press the side of a clear glass firmly against the skin and the rash doesn’t fade, it’s a sign of blood poisoning (septicaemia) and you should seek medical attention immediately. The rash may be harder to see on darker skin so check for spots on the paler areas, such as the palms of the hands, soles of the feet or the abdomen.”
How to treat it
If meningitis is suspected then the child must go immediately to an Accident and Emergency Department.
Is it contagious?
Bacterial meningitis can be contagious and you will be advised by the professionals looking after your child of actions that need to be taken.
2. Slapped cheek syndrome
What to look for
This is caused by parvovirus and causes a bright red rash on the cheeks. It is accompanied by slight fever and the child will feel mild/moderately unwell but get better after a few days.
How to treat it
Slapped cheek syndrome is usually mild and should clear up without specific treatment. If you or your child is feeling unwell, you can try the following to ease the symptoms:
If you or your child is feeling unwell, you can try the following to ease the symptoms:
- Rest and drink plenty of fluids - babies should continue their normal feeds. Dehydration poses the greater risk, particularly in the young.
- For a fever, headaches or joint pain you can take painkillers, such as paracetamol or ibuprofen. Aspirin should not be given to children under 16 years old.
- To reduce itchiness, oral antihistamines can be taken and/or emollients used – some antihistamines are not suitable for young children, so check with your pharmacist first.
- Those who should contact a GP include: pregnant women exposed to anyone with slapped cheek syndrome or who have symptoms of the infection, those who have a blood disorder, a weakened immune system or those with symptoms of severe anaemia, such as very pale skin, shortness of breath, extreme tiredness or fainting.
Is it contagious?
The virus is spread by inhaling droplets that are sneezed or coughed out by someone infected or by touching a contaminated surface or object and then touching your mouth or nose. It’s very difficult to prevent slapped cheek syndrome because people who have the infection are most contagious before they develop any obvious symptoms. However, making sure that everyone in the household washes their hands frequently may help stop the infection from spreading.
It’s very difficult to prevent slapped cheek syndrome because people who have the infection are most contagious before they develop any obvious symptoms. However, making sure that everyone in the household washes their hands frequently may help stop the infection from spreading.
Someone with slap cheek syndrome is infectious during the period before the rash develops. Once the rash appears, the condition can no longer be passed on. Unless you or your child is feeling unwell, there’s no need to stay away from school or work once the rash has developed. It is however a good idea to notify your child’s school about the infection, so children who develop early symptoms can be spotted quickly and vulnerable people can be made aware that they may need to get medical advice.
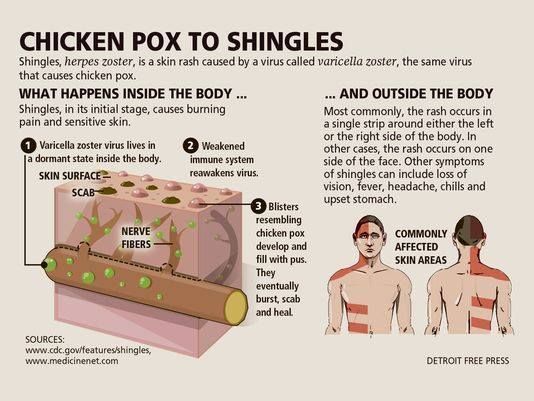
3. Chicken pox
What to look for
At first your child will seem a bit off-colour, they may be off their food and quite lethargic for a few days. Then a few, itchy, red, raised spots on the neck, face, chest or back or other body parts will start to appear. These turn into little fluid-filled blisters, which can be itchy and painful. The child can be infectious for several days before spots appear and for 5 days or more after spots become visible. forming .
These turn into little fluid-filled blisters, which can be itchy and painful. The child can be infectious for several days before spots appear and for 5 days or more after spots become visible. forming .
How to treat it
Chickenpox is usually mild and can be self-managed from home. Most people feel better within a week or so. But some people can become more seriously ill and need to see a doctor. There’s no cure but the treatment below can help relieve the symptoms while the body fights the infection.
- Rest and drink plenty of fluids to avoid dehydration.
- For a fever, painkillers can help, such as paracetamol. Ibuprofen shouldn’t be given to children with chickenpox as it can make them very ill and do not give aspirin to children under 16.
IMPORTANT: Always read the packet or leaflet that comes with the medicine to check it’s suitable and how much to take. Speak to a pharmacist or your GP if you’re unsure.
You can buy topical preparations to apply directly onto the rash or administer an oral antihistamine to help reduce itching and soothe the skin– some antihistamines are not suitable for young children, so check with your pharmacist first.
An antiviral medicine called Aciclovir may be recommended if there is a risk of severe chickenpox and you already have symptoms. It ideally needs to be started within 24 hours of the rash appearing.
Is it contagious?
Chickenpox is highly contagious and can make some people very ill, so it’s important to try and avoid spreading it to others. If you or your child has chickenpox, stay away from nursery, school or work until all of the blisters have dried up and scabbed over. This usually happens five or six days after the rash first appears. You may continue to have spots on your skin for another week or two, but you’re no longer contagious if the spots are dry and scabby.
Certain people are at a higher risk of becoming seriously ill if they become infected with chickenpox. These include:
- Pregnant women
- Newborn babies
- People with weakened immune systems
- People in these groups should avoid contact with people with chickenpox and consult their GP if there is a risk that they have become infected.
Chicken pox can be spread through contact with objects that have been contaminated with the virus, such as toys, bedding or clothing. You can prevent it spreading by cleaning any objects or surfaces with a disinfectant and wash any infected clothing or bedding regularly.
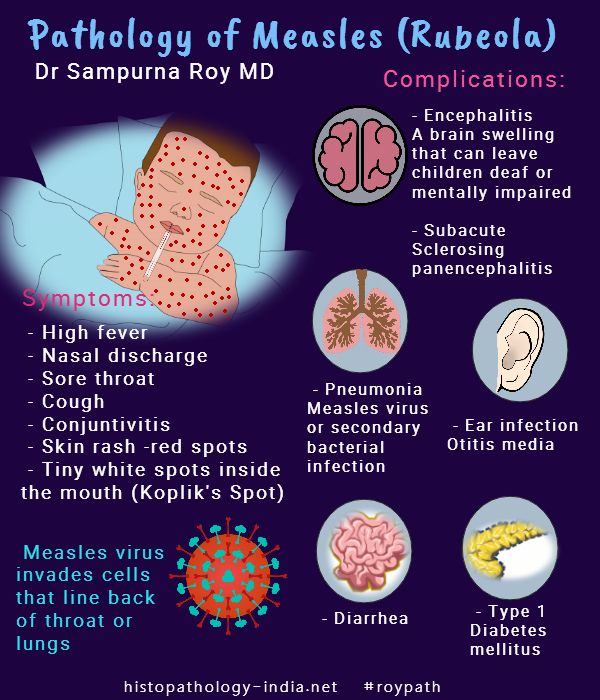
4. Measles
Measles is a highly infectious, unpleasant viral illness that has some characteristic features to distinguish it from other viruses. Furthermore, it has the potential to cause serious complications.
What to look for
A mass of red spots break out around the neck, behind the ears and face but can appear elsewhere too, including the inside of the mouth. Measles can result in serious complications but, thanks to vaccination programmes, the incidence of outbreaks is low.
Initial symptoms of measles can include:
- A runny or blocked nose
- Sneezing
- Watery eyes
- Swollen eyelids
- Sore, red eyes that may be sensitive to light
- A fever
- Small greyish white spots in the mouth
- Aches and pains
- Cough
- Loss of appetite
- Tiredness, irritability and a general lack of energy.

How to treat it
You should contact your GP as soon as possible if you suspect that you or your child has measles. Its best to phone before your visit as your GP surgery may need to make some arrangements to reduce the risk of spreading the infection to others. There’s no specific treatment for measles, but the condition usually improves within 7 to 10 days. If the symptoms of measles are causing discomfort for you or your child, there are some things you can do to treat these while you wait for your body to fight off the virus.
- Rest and drink plenty of fluids to avoid dehydration.
- Paracetamol or ibuprofen can be used to reduce a fever and relieve any aches or pains if you or your child is uncomfortable. (Aspirin should not be given to children under 16). Speak to your pharmacist if you are not sure which medications are suitable for you child.
Stay away from work or school for at least four days from when the measles rash first appears to reduce the risk of spreading the infection. It’s important to avoid contact with people who are more vulnerable to the infection, such as young children and pregnant women.
It’s important to avoid contact with people who are more vulnerable to the infection, such as young children and pregnant women.
You can avoid catching measles by having the measles, mumps and rubella (MMR) vaccine. Measles is unlikely in people who are fully immunised or who have previously contracted the infection. Vaccination with one dose of the combined measles, mumps, and rubella (MMR) vaccine should provide about 90% immunity. However, vaccination with two doses of the MMR vaccine, as indicated by the UK Childhood Immunisation Programme, is thought to provide close to 100% lifelong immunity.
Data suggests that the people most likely to present with measles are younger people who have not received the MMR vaccine and who have not been previously exposed to the virus. In the past, there has been measles endemic, but since the introduction of the MMR vaccination, this has become relatively rare. However, in recent years, the infection has become more prevalent due to a failure of uptake of vaccination.
5. German measles (rubella)
What to look for
This is usually a mild illness with small red spots appearing on the face at first and then spreading to other parts of the body. Other symptoms include swollen glands and a cold-like illness. It’s rarely seen nowadays in the UK, thanks to routine vaccination. It is, however, of serious concern if a pregnant woman catches the virus in the first 16 weeks of pregnancy because it can cause birth defects in her baby.
Both measles and rubella are viral, however, the infection with rubella is usually mild by comparison, (symptoms include a rash and swollen lymph glands) but the likelihood of developing complications is rare. The main risk is contracting rubella in pregnancy.
How to treat it
You should always contact your GP if you suspect rubella. It’s best to phone before your visit as your GP surgery may need to make some arrangements to reduce the risk of spreading the infection to others. There’s no specific treatment for rubella. The condition is usually mild and improves without treatment within 7 to 10 days. If the symptoms of rubella are causing discomfort for you or your child, there are some things you can do while you wait for the infection to pass.
The condition is usually mild and improves without treatment within 7 to 10 days. If the symptoms of rubella are causing discomfort for you or your child, there are some things you can do while you wait for the infection to pass.
- Rest and drink plenty of fluids to avoid dehydration.
- Paracetamol or ibuprofen can be used to reduce a fever and relieve any aches or pain. (Aspirin should not be given to children under 16). Speak to your pharmacist if you are not sure which medications are suitable for you child.
Is it contagious?
While you have rubella, it’s important to reduce the risk of spreading the infection to others. If you or your child has the condition, you should avoid work or school for four days from when you first develop the rubella rash.
In rare cases, rubella can cause serious problems in an unborn baby, so you should also try to avoid contact with pregnant women for four days from the start of the rash. If your pregnant and develop a rash or have been in contact with someone who has a rash, contact you GP or midwife immediately.
6. Impetigo
What to look for
This often begins as a red patch of skin often around the nose or mouth but can occur anywhere on the body. The red patches then become a crusty/brownish colour after a few days.
It is caused by overgrowth of skin bacteria and can easily be cleared by antibiotics, although spreads easily if left untreated.
Speak to your GP if you think you or your child may have symptoms of impetigo. Impetigo isn’t usually serious, but it can sometimes have similar symptoms to more serious conditions such as cellulitis so it’s important to get the correct diagnosis.
How to treat it
Impetigo usually gets better without treatment in a few weeks. However, treatment is often recommended because it can reduce the length of the illness to around 7 to 10 days and can reduce the risk of spreading the infection to others.
Hygiene measures alone even for small, localised lesions are not recommended. The main treatments prescribed are antibiotic creams or oral antibiotics and duration of treatment is usually one week.
Is it contagious?
During treatment it’s important to take precautions to minimise the risk of impetigo spreading to other people or to other areas of the body. Most people are no longer contagious after 48 hours of treatment or once their sores have dried and healed. It’s important to stay away from school or work until then.
To help prevent the risk of infection spreading:
- Don’t share flannels, bedding or towels with anyone who has impetigo.
- Wash and loosely cover the sores.
- Avoid touching or scratching the sores.
- Avoid contact with new born babies, preparing food, playing contact sports, or going to the gym – until the risk of infection has passed.
- Wash your hands frequently
- Washable toys should be washed – thoroughly wipe no washable toys.
7. Eczema
What to look for
Dry /inflamed patches of skin typically form on creases of elbows and behind knees, but can occur anywhere on the body.
How to treat it
Treating eczema fundamentally involves breaking the scratch-itch cycle and replenishing the moisture content of the skin. It will normally respond well to the regular use of emollients/moisturisers and topical steroid preparations for flare ups. It is not possible to “overdose” on moisturisers and what may work for one person, may not for another. Steroid preparations are useful in managing flare-ups but should be used as prescribed. There are also specific bath additives/shower gels/soaps that are targeted to help manage eczema.
Is it contagious?
Eczema is not contagious. It is a chronic skin condition, most prevalent in childhood.
8. Molluscum
What to look for
Little crops of raised, fluid-filled blisters can occur anywhere on the body or limbs. These spots are harmless and the child will not be unwell but they are contagious and spread by person to person contact.
How to treat it
It can take up to 18 months for these to clear. Usually no treatment is needed as they clear on their own.
Usually no treatment is needed as they clear on their own.
Is it contagious?
Resolution is spontaneous but it is contagious. It can be spread through close direct contact. If you become infected by the virus and spots appear on your skin, the virus can also spread to other areas. It is not known how long someone with molluscum is contagious for, but it is thought the contagious period may last up until the last spot has completely healed.
9. Allergic wheals
What to look for
These are blistery, reddish, raised blotches to the skin which can appear rapidly on different parts of the body. They tend to be itchy and are usually due to exposure to an allergen e.g. animal hair/dander, grasses or foods/additives.
How to treat it
Antihistamines such as Piriton can be helpful in reducing symptoms and progression. Most often the rash settles quickly over 24 hours but if there is associated swelling of the face, lips or any breathing problems, call 999.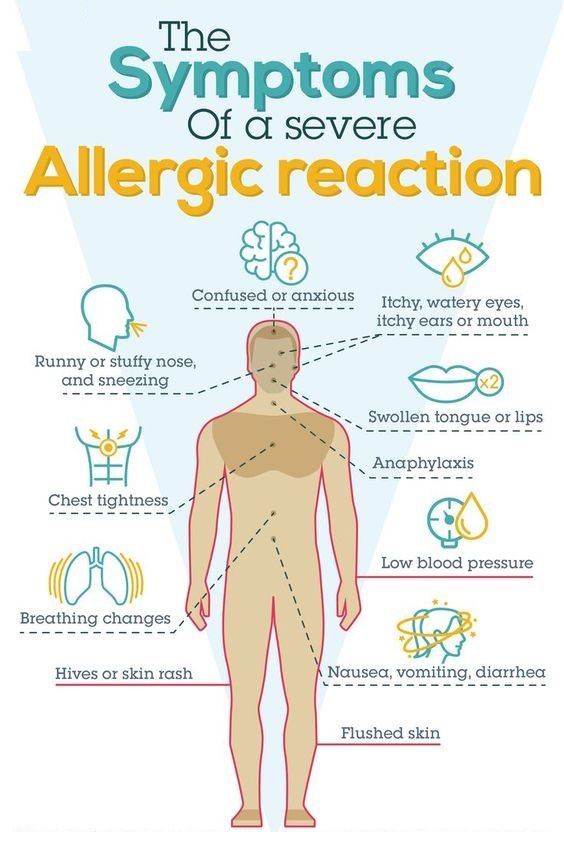
Is it contagious?
Allergic wheals are not contagious. This is because allergic reactions are a result of the unique response of each individual's immune system to certain triggers. Substances that cause a reaction in one person may not cause a reaction in someone else.
10. Neonatal heat spots
What to look for
These small red spots with a tiny white pimple on top appear on the face, neck and upper chest. They are the result of immature sweat glands becoming blocked when the baby gets hot. They are very common and usually of no concern and will disappear after a few months.
Find out more about the child health care options available to your family. You can also discover more information in our pregnancy and childcare centres or if you have a specific question, you can ask our experts.
Further reading
Meningitis
Skin rashes in babies
Allergies
Pinprick Red Dots on Skin That Aren't Itchy: Causes, Next Steps
Red or purple spots on your skin may be hives or acne. But they can also indicate a health condition, including an infection or autoimmune disease.
But they can also indicate a health condition, including an infection or autoimmune disease.
Your skin’s health and appearance shifts all the time depending on your environment, lifestyle, and health conditions, among other factors.
Sometimes skin problems have an obvious cause, like sunburn or a mosquito bite. But other times rashes or dots appear on your skin that are harder to identify.
Petechiae are red, purple, or brown dots on the skin that are generally painless and itch-free. These dots form when your tiniest blood vessels, called capillaries, break and leak blood under the skin. This blood pools under the surface, creating the appearance of spots.
Petechiae aren’t considered a medical condition on their own. They’re often a symptom of another underlying health problem, such as infection, allergic reaction, or autoimmune disease.
In this article, we will explore some common potential causes of petechiae, symptoms to watch out for, and when to see a doctor.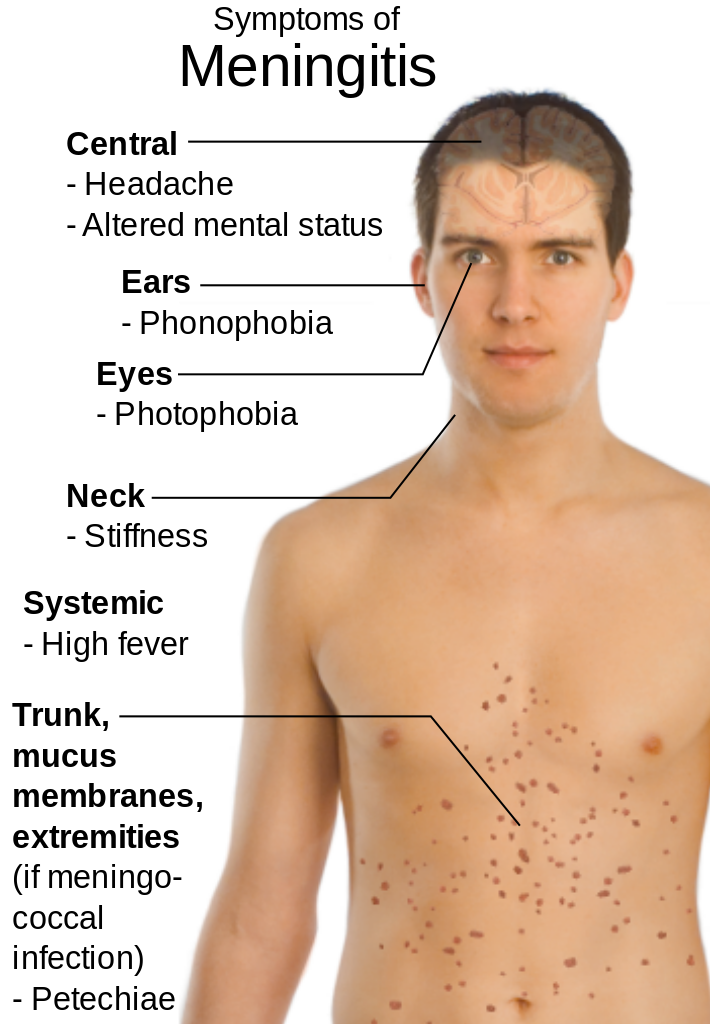
You can develop petechiae for a number of different reasons, including injuries and infection. In many of these cases, petechiae are a symptom of an underlying health issue.
Here’s an overview of common causes of petechiae:
Medication
An allergic reaction to certain medications may cause clusters of red dots to appear on your skin. This could be petechiae or hives. Hives are often itchy, raised welts that are generally larger than petechiae. Medications known to cause petechiae in rare cases include:
- antiplatelet medications
- aspirin
- steroids
Infections
Both viral and bacterial infections can cause red dots or other rashes to appear on your skin. Common infections linked to petechiae include:
- enterovirus infection
- parvovirus B19 infection
- dengue virus infection
- meningococcal infection (meningitis)
- scarlet fever
- infective endocarditis
- Rocky Mountain spotted fever
- septicemia/sepsis
- congenital TORCH syndrome (concurrent infection with toxoplasma gondii, other agents, rubella, cytomegalovirus, and herpes simplex virus)
Blood-related disorders
These include blood cancers, chronic conditions, and blood-related congenital disorders.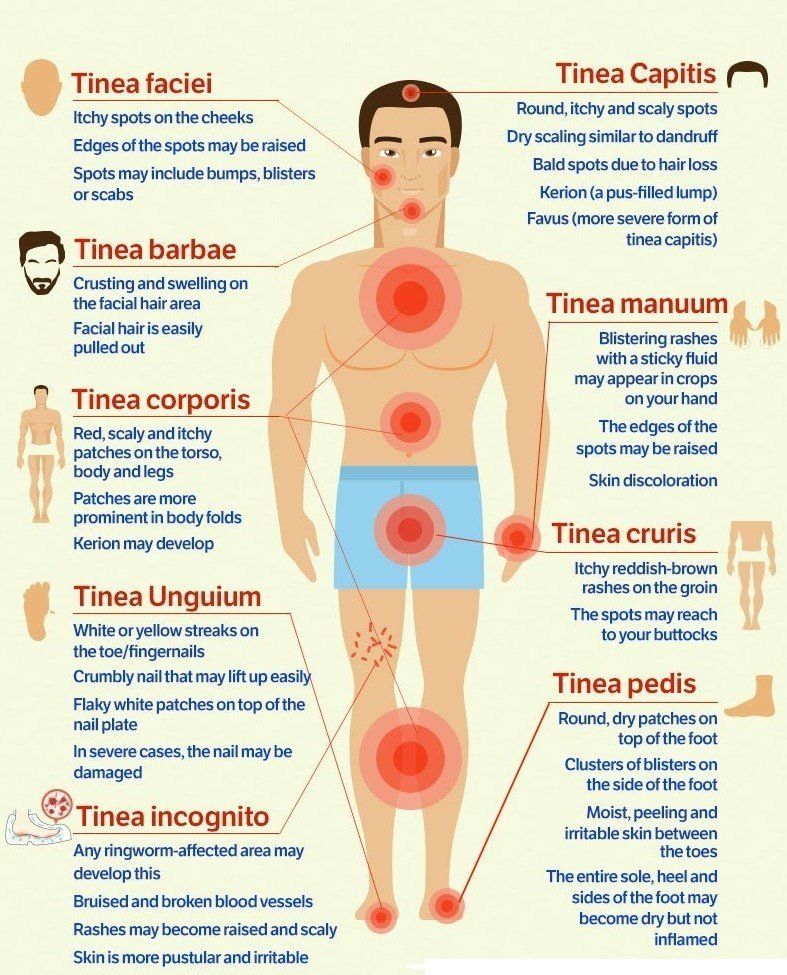
- thrombocytopenia
- leukemia
- types of anemia
- platelet dysfunction
- coagulation disorders
- vascular diseases
- Bernard-Soulier syndrome
- Glanzmann thrombasthenia
Other chronic conditions
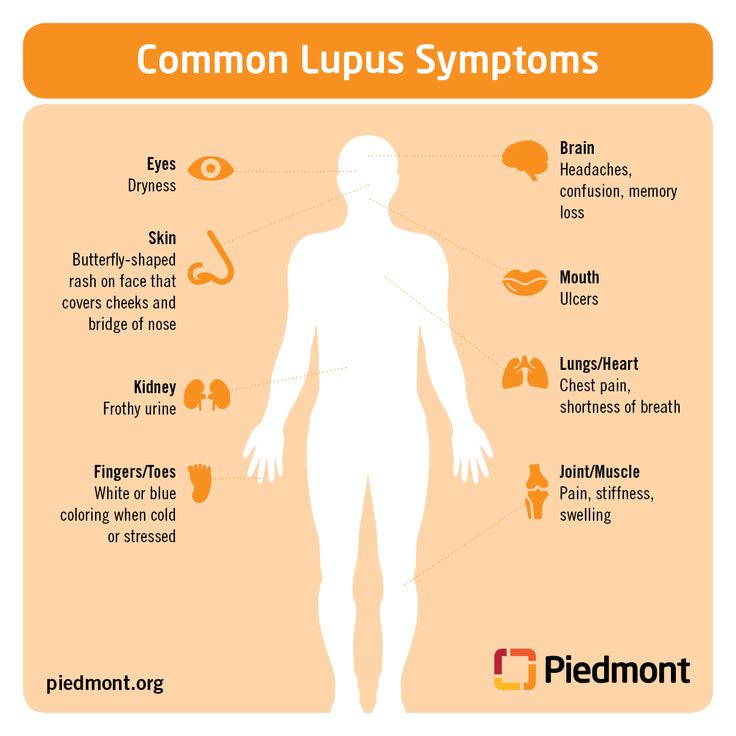
Petechiae may come and go as a result of a chronic disease or illness. This includes autoimmune conditions, and certain congenital and connective tissue disorders. For example:
- Ehlers-Danlos syndromes (EDS)
- lupus
- chronic liver disease
- Wiskott-Aldrich syndrome
Acute injuries, allergic reactions, and a vitamin K deficiency are also associated with the symptom of petechiae.
Does COVID-19 cause petechiae?
Each new variant of SARS-CoV-2, the virus that causes COVID-19, seems to appear with new symptoms. Different variants of the virus have caused some level of skin symptoms, including petechiae. This is believed to be related to bleeding and coagulation changes brought on by COVID-19.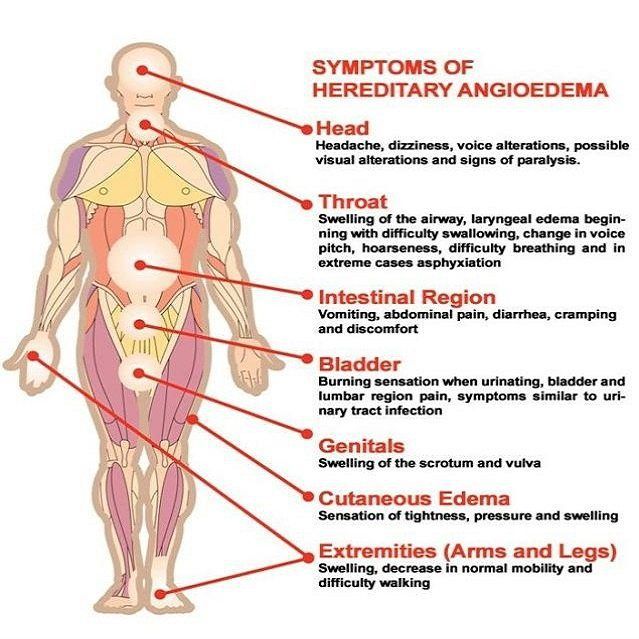
Although petechiae has been observed in people with COVID-19, it’s not the most common skin manifestation. One study estimated that only about 3% of people with COVID-19 develop this symptom.
Was this helpful?
Petechiae may not always appear alongside other noticeable symptoms. These tiny dots are usually flat, red, brown, or purple in color, and measure less than 2 millimeters (mm).
A hallmark of petechiae is that they’re nonblanching. This means they don’t fade away or disappear when you apply pressure to your skin.
Size is what differentiates petechiae from purpura. Purpura are also caused by broken capillaries leading blood to pool under your skin, but they’re larger than petechiae (over 2 mm).
Although you may itch, be sore, or have a fever alongside petechiae, these symptoms are usually related more to the issue that caused your petechiae than these spots themselves.
Treatment for petechiae depends on the underlying cause, since the dots are usually a symptom of another condition.
Petechiae that appear from an injury or infection usually resolve on its own in 2 to 3 days. You’ll likely need to rest and take antibiotics for a bacterial infection. Treatment for most viral infections includes rest and over-the-counter pain medication (OTC NSAIDs).
If you have a blood-clotting disorder, your doctor will design an individualized treatment plan. This could include taking reversal agents to counter anticoagulation medications.
Steroids, chemotherapy, and immunosuppressant drugs may also be used to control a variety of autoimmune or inflammatory disorders that could be causing you to develop petechiae.
Immunosuppressant drugs work by suppressing or modifying your immune system so it doesn’t cause inflammation to joints, tissues, and organs.
Learn about ways to prevent petechiae.
If your petechiae (or your child’s) develops alongside other symptoms like fever, talk with your doctor.
Febrile (feverish) conditions that appear with petechiae are especially common in children, accounting for about 2. 5% of visits to the pediatric emergency department each year.
5% of visits to the pediatric emergency department each year.
In these children, doctors will usually evaluate for a meningococcal infection first.
In a 2018 study, between 7% and 11% of cases of petechiae and fever in children were caused by meningococcal disease, and about 10% were caused by Group A staphylococcus infection. Overall, about 60% of these cases were linked to viral illnesses.
Learn more about when to see a doctor for petechiae.
There are many conditions that can cause red dots on your skin. You may need your doctor to help you differentiate between these conditions and petechiae.
Other conditions that can produce dots or skin irritation similar to petechiae include:
- hives
- acne
- bug bites
- eczema
- heat rash
- rosacea
Petechiae are usually a symptom of another health issue. These spots form after blood leaks from your capillaries. They don’t itch and won’t disappear if pressed.
Common causes for petechiae include infections, certain chronic diseases, and even injuries.
Your doctor may have to run several tests to identify what’s causing the dots to appear on your skin. Treatment depends entirely on the underlying cause.
Most of the time, these red, purple, or brown dots will resolve in a few days, especially if the condition causing them has been addressed and managed.
diagnosis of skin rash in the clinic, prices for dermatologist services in Moscow
Prices Appointment with a dermatologist Call a dermatologist at home Pimples
Skin rash is the general name for a huge group of external skin changes that can be caused by a wide range of different diseases. Traditionally, it is believed that any skin rash is exclusively infectious, but experts are diligently fighting this erroneous point of view. In fact, a skin rash can appear for several reasons:
- presence of infectious and parasitic diseases;
- allergic reactions of various etiologies;
- presence of diseases of the blood and blood vessels;
- non-compliance with the rules of personal hygiene.
Depending on the cause, a skin rash can take completely different forms, which sometimes makes it difficult to diagnose the disease. Only conducting a whole range of examinations allows you to accurately determine the disease and prescribe a qualified treatment.
Skin rash and its varieties
1. Stains. They are areas of the skin that have a different color from the rest of the skin. Their peculiarity lies in the fact that they do not rise above the skin.
2. Blisters. Skin rash slightly rises above healthy areas of the skin, differs from them in color. There is also a slight roughness of the surface of such a blister, which is sometimes accompanied by itching.
3. Papules. Such a skin rash is a small seal inside the skin, a tiny nodule, the size of which does not exceed the head of a pin.
4. Bubbles. Cavities in the skin that are filled with fluid. They can vary greatly in size and other characteristics.
5. Erosions and ulcers. Severe skin lesions, accompanied by a violation of its integrity, in which fluid separation is observed.
Severe skin lesions, accompanied by a violation of its integrity, in which fluid separation is observed.
6. Crusts. Small seals on the skin that appear at the site of ulcers and erosions. Often the appearance of crusts is associated with the healing process.
Sometimes a skin rash can take on a variety of forms, and in some diseases there are several varieties at once on the body of one patient.
Diseases and skin rashes
- Secondary syphilis is often accompanied by skin rashes that come in a wide variety of forms. The only feature is the symmetrical location of the skin rash, which is quite rare in other diseases. At the beginning of the second period, the skin rash is characterized by a bright color, which becomes pale in the second wave of rashes. Such a skin rash passes without a trace, which some patients regard as a sign of recovery.
- Scabies is accompanied by the appearance of papules or blisters that form at the site of introduction of the pathogen.
 Near the skin rash, small gray stripes appear, which are the passages of the parasite. Scabies is a contagious disease that needs urgent treatment.
Near the skin rash, small gray stripes appear, which are the passages of the parasite. Scabies is a contagious disease that needs urgent treatment. - Candidiasis is a disease that is manifested by a small skin rash localized in the skin folds. First, small bubbles appear, which gradually burst. Then, in their place, ulcers and erosion appear, which cause severe discomfort to the patient.
- Urticaria are rather large itchy blisters that appear after contact with an allergen. Such a skin rash is similar to a nettle burn, while the blisters are characterized by rapid spread. After taking antihistamines, hives usually go away. However, in difficult cases, it is better to consult a specialist, because edema can go to the respiratory tract, which will lead to the death of a person.
In general, the list of diseases in which a skin rash appears is much larger, so you should definitely contact a dermatologist or therapist for an accurate diagnosis.
How is a skin rash treated?
- Determine the cause of the skin rash.
- Preparations are selected for the treatment of the underlying disease.
- External drugs are used.
Traditionally, many people believe that skin rashes are treated with brilliant green, iodine, and other similar drugs. In fact, the treatment depends on the disease against which skin rashes appear.
If the skin rash was the result of a meeting with an allergen, it must be calculated and removed, and antihistamines are also prescribed. In infectious diseases, the patient is isolated and antifungal and anti-inflammatory drugs are prescribed. If a skin rash is caused by improper hygiene, the patient, along with drug treatment, is selected with a whole range of hygiene measures to prevent relapses.
In general, a skin rash can accompany completely different diseases, each of which requires its own treatment. A timely appeal to a specialist will allow you to achieve a quick and complete cure, and will also become the best prevention of complications and exacerbations.
A timely appeal to a specialist will allow you to achieve a quick and complete cure, and will also become the best prevention of complications and exacerbations.
Related articles:
- Child rash
- Rash on hands
- Rash on body
- Rash on the face
- Treatment of rashes
- Syphilitic rash
This article is not medical advice and should not be used as a substitute for consultation with a physician.
Acne: symptoms, causes and treatment
Acne is an inflammation of the skin characterized by blackheads, whiteheads and pimples. Such rashes most often appear on the face, as well as on the chest, back and shoulders.
Acne affects approximately 90% of teenagers and 20% to 30% of people in their 20s and 40s. This is the most common dermatological problem.
call me back
Acne occurs when hair follicles become blocked by dead skin cells mixed with sebum. Sebum is an oily substance produced by glands attached to hair follicles called sebaceous glands.
Sebum is an oily substance produced by glands attached to hair follicles called sebaceous glands.
In people with acne, these glands produce excess sebum, which mixes with dead skin cells and forms a plug that clogs the follicles. This creates a favorable environment for the growth of Cutibacterium acnes bacteria, which are normally found under the skin, and cause inflammation.
The sebaceous glands are extremely sensitive to hormonal changes. For example, puberty hormones stimulate the growth and production of sebum. The most noticeable effect on the sebaceous glands is the so-called androgenic male hormones. They are secreted by men and women, but their level is higher in the male body.
These hormones can also cause breakouts during a woman's menstrual cycle, which is why it's common for women to have breakouts in adulthood.
However, oily hair and skin do not cause acne, but are often a sign of overactive sebaceous glands, the true cause of acne. In addition, the predisposition to acne can be hereditary.
In addition, the predisposition to acne can be hereditary.
Anything that irritates the skin can also cause acne, including:
-
friction of clothes;
-
licking an overly affectionate dog;
-
contact with certain sports equipment;
-
applying some cosmetics;
-
skin exposure to extreme temperatures.
Other factors that can cause acne include:
-
Sun. Sun exposure can cause a special type of acne called summer acne. This is especially true for women aged 25 to 40 who suffer from acne during puberty.
-
Smoking. Due to its effects on the skin (clotting of pores), smoking may be actively involved in the spread of acne.
-
Food. Until now, no serious scientific study has been able to prove the connection between food and acne. On the other hand, some studies have shown that a significant intake of dairy products, sweets, cakes and fish oil is responsible for the activity of the sebaceous glands.

Symptoms of acne vary, they can manifest themselves as follows:
-
Black dots (the size of a pinhead) that open up on the surface of your skin and don't leave a scar.
-
Whiteheads or pustules, which are the most common type of acne and form the first lesions - they do not turn into blackheads because they are not exposed to air.
-
Inflamed deep pustules and cysts. They are usually red, swollen, and clearly contain pus.
-
Deep acne, which can be more severe - These lesions are usually red, inflamed, pus-filled, and painful to the touch.
Deep pimples often appear on the back and chest. It is usually the most difficult form of acne to treat and is prone to scarring. Deep acne has pustules and cysts that appear mainly on the surface of the skin and sometimes in the deeper layers of the skin. If they are damaged, the released pus will cause the formation of new lesions.
All acne starts with clogged pores, but variations in this blockage and the body's response to it lead to different types of breakouts.
The four main manifestations of acne, in order of severity, are comedones, pimples, cysts, and nodules. They differ in appearance, progression, and treatment required.
-
Comedones. They are the most common type of acne and can lead to the development of other forms. Comedones occur when pores become clogged with debris and bacteria begin to accumulate.
-
Black dots. This is the main form of acne, and it can appear when sebum builds up underneath. Blackheads are usually easy to prevent and treat with over-the-counter cleansers and exfoliators.
-
Whiteheads. In cases where the skin grows out of the blockage and blocks it from air, a closed comedone, commonly referred to as white head, forms. This closed comedone is a sealed skin pocket containing bacteria; if it bursts, these bacteria can spread to the surrounding pores, exacerbating acne.
As with blackheads, whiteheads can be treated and prevented with over-the-counter topical products.
-
Acne. Usually formed as a result of excessive activity of the sebaceous glands located at the base of the hair follicles - most often on the face, chest, shoulders or back.
-
Papules. These are inflamed pimples that appear on the skin as red or pink bumps. These pimples are not necessarily painful, but can be sensitive to touch. Papules should never be touched or squeezed as this can cause scarring.
-
Pustules. They are similar in appearance to whiteheads, except that the bumps are surrounded by a red ring of inflammation. The pustules are filled with pus. Like papules, pustules should not be plucked or squeezed as this can lead to scarring.
-
Cysts. This is a large, pus-filled mass that may resemble a boil. Cysts form when pores become clogged deep within the hair follicle and an infection occurs that damages the deeper layers of the skin.
 Fat that is normally secreted gets under the skin and turns into a sac known as a cyst.
Fat that is normally secreted gets under the skin and turns into a sac known as a cyst. Cysts are often painful and are a severe form of acne requiring treatment by a dermatologist.
-
Nodules. These are large, inflamed bumps that are hard to the touch. They form when bacteria enter the pores and cause an infection that reaches deeper layers of the skin. This infection causes hard and painful nodules to appear under the skin.
Like cysts, nodules require treatment by a dermatologist.
Sign up for a consultation
There are many ways to treat acne, and in some cases more than one option may be needed.
Therapy depends on the severity, location and type of acne. In many cases, it is necessary to wait 2 to 3 months before evaluating the effectiveness of treatments, because it takes about 2 months for acne to mature. At the beginning of treatment, acne may even worsen before there are signs of improvement.
The most common treatments for acne include:
-
Local treatments. OTC acne treatments include benzoyl peroxide, salicylic acid, and glycolic acid. When used individually, these treatments are effective for moderate acne. These are exfoliators that unclog clogged pores and help the skin get rid of dead skin cells. Benzoyl peroxide also has an antibacterial effect.
-
Antibiotics (tetracycline, minocycline, doxycycline). They can be used to treat bacteria that cause inflammatory acne, but strictly on prescription.
-
retinoids are often used to treat non-inflammatory acne, but they are also useful for treating inflammatory breakouts. They speed up skin renewal and may cause skin irritation at the start of treatment (which usually resolves as the skin adjusts).
Isotretinoin, a strong oral retinoid, is very effective in treating severe acne. However, due to potential side effects, it is usually only used when many other treatments have failed, especially in women of childbearing age.

-
Treatment procedures. In some cases, acne may require inpatient treatment by a dermatologist. It may include laser or light therapy and chemical peels, depending on the type and severity of acne.
Cysts and nodules may need to be drained and removed if topical treatments don't work. During these procedures, a dermatologist makes a surgical incision in the affected area to drain fluid and pus from the cyst or nodule.
A dermatologist may also inject a dilute corticosteroid into the cyst or nodule. The anti-inflammatory properties of corticosteroids can help reduce the inflammation associated with these types of acne in as little as 24 hours.
-
Additional treatments include oral contraceptives, which may be effective in reducing acne in some women; one of the ingredients of such drugs is spironolactone, which targets the overproduction of the androgen hormone.
Many of these methods can increase your skin's sensitivity to the sun.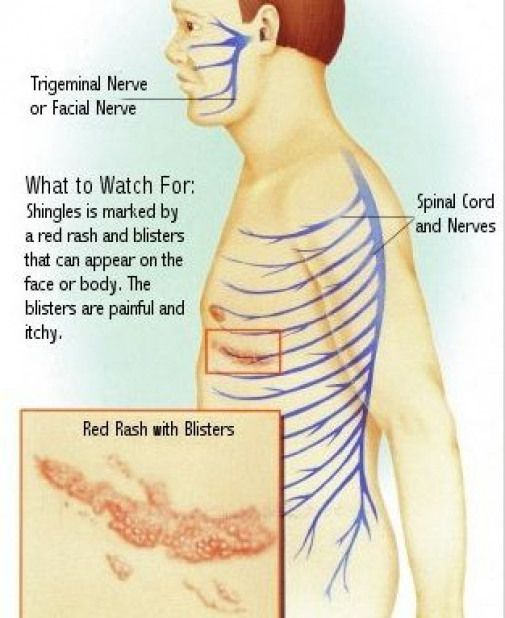 Therefore, they should be used together with appropriate sun protection.
Therefore, they should be used together with appropriate sun protection.
Certain foods can make skin problems worse. For example, these:
-
Processed foods. Highly processed and cooked foods often contain compounds that promote oxidative stress and inflammation. Again, oxidative stress and inflammation almost always contribute to chronic diseases, including dermatological ones.
-
Dairy products. Dairy products cause a strong insulin response, increase hormone levels in the body and increase inflammation - all of which lead to the onset and exacerbation of acne.
-
Alcohol. Many studies have linked alcohol consumption to acne.
Also, a link between wheat gluten and acne (as well as between gluten and other skin conditions) cannot be ruled out. Try eliminating all sources of wheat and gluten from your diet for a month and see if that helps.