Week estimator pregnancy
Pregnancy Due Date Calculator – How Many Weeks Am I?
Tell us a bit more:
1st day of my last period*
//
1st day of my last period*
Please select a date
Select your cycle length
Conception Date
//
Conception Date
Please select a date
Few things can compare to the rush and excitement of when you take a pregnancy test and read out the positive result! Once you’ve processed the news that you’re going to be a mom, your thoughts will naturally turn to planning and one of your first questions will no doubt be: when is my due date?
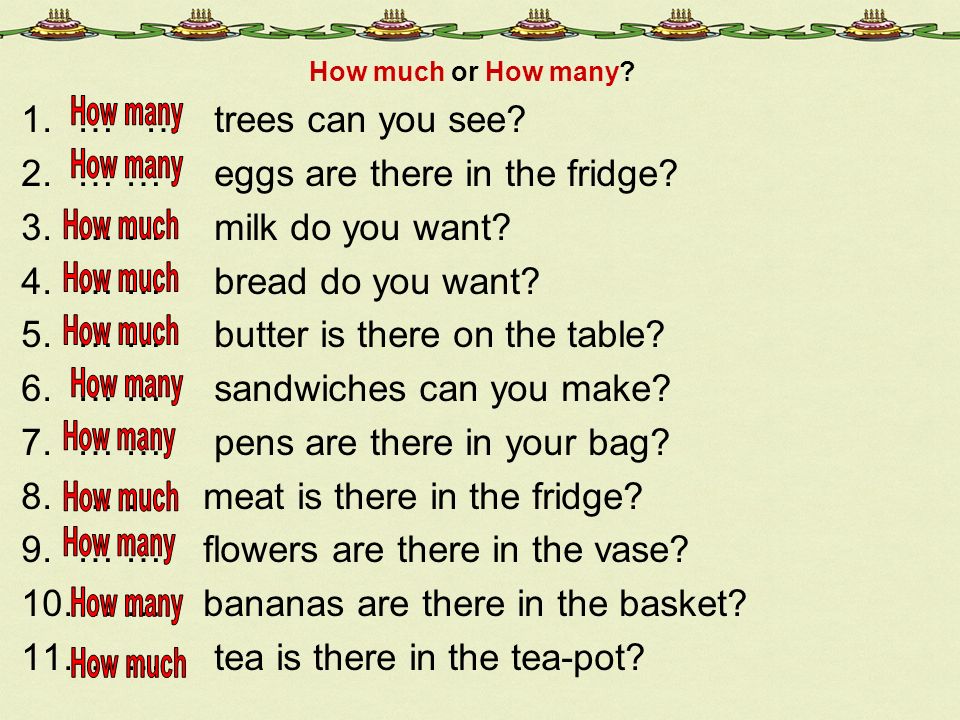
Use these three simple steps to find out how far along you are in your pregnancy:
- Figure out when was the first day of your last period or the exact day you conceived.
- Enter the relevant dates into the pregnancy week calculator.
- Then hit Find out now! to find out how far along you are.
Keep in mind every pregnancy is unique and the result will be an estimation rather than a fixed date.
While it’s true that most pregnancies last 40 weeks, there are other factors at play which will determine your due date. Most expectant mothers don’t realize that both menstrual and ovulation periods count as the first two weeks of pregnancy. Many won’t be aware of their pregnancy until their first missed period, and by that time they could be up to five weeks in. That means that simply estimating nine months from the day you take a pregnancy test isn’t going to calculate your due date, and, even so, factoring in a few weeks here and there for ovulation won’t either.
Unless you can pinpoint exactly what point of your ovulation cycle you were in at the time of fertilization, it’s difficult to know how far along you are and what date you’ll meet your baby.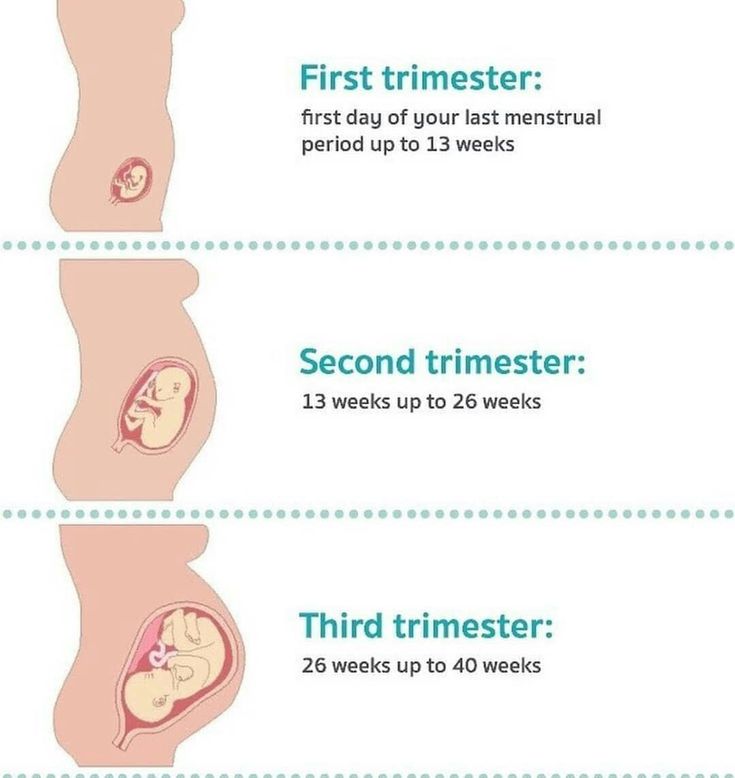 Luckily, our Due Date Calculator can help.
Luckily, our Due Date Calculator can help.
Using both the date of your last period and the length of your regular cycle, or exact date of conception, our Due Date Calculator will quickly work out your estimated due date, tailoring it accordingly for longer, shorter, and average cycle lengths.
Once you’ve calculated your due date, you can get a better idea of when to expect your little one – and start to plan accordingly.
If you haven’t done so already, one of the first steps you should take is to schedule an appointment with your doctor, who can confirm that you're pregnant with a blood test and physical exam, and also help you establish a more precise due date.
At each following prenatal care appointment, you'll be examined to determine the size of your uterus, and to monitor your little one's development. Pregnancy milestones such as hearing your baby’s first heartbeat and seeing your baby via ultrasound will be a thrilling part of these checkups. Along the way, depending on what is observed, your pregnancy due date may be adjusted.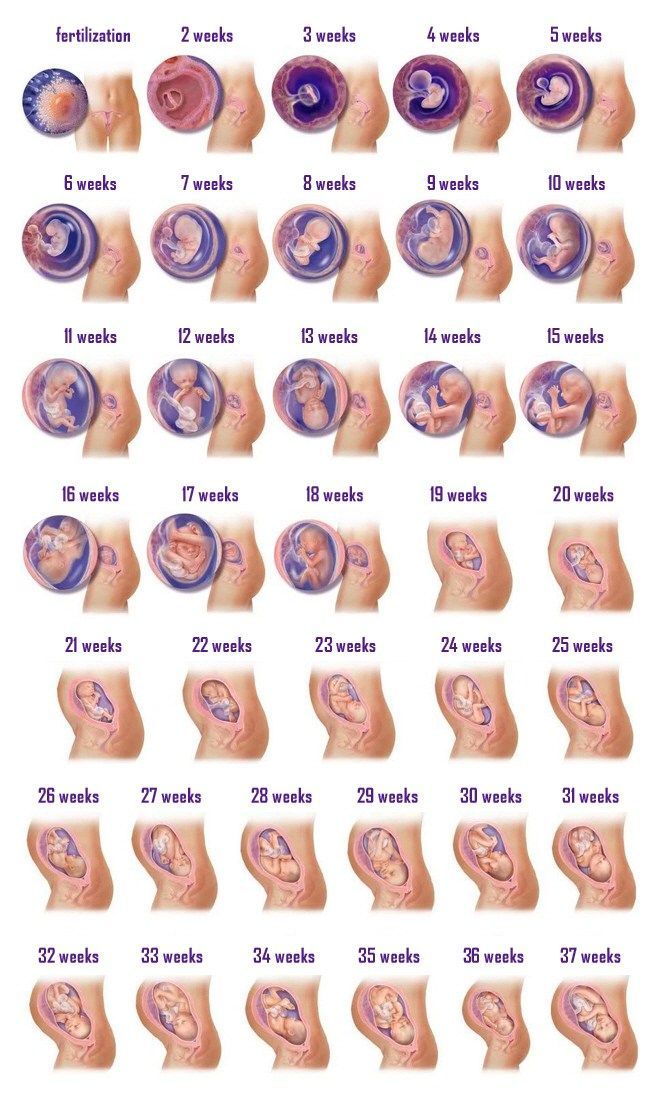
While your doctor will be able to advise you best, there are still plenty of things you can do as soon as you discover you’re pregnant. Explore the rest of our site to find out more.
Pregnancy Due Date Calculator | BabyCenter
BabyCenter's Due Date Calculator
Use our pregnancy due date calculator by plugging in the date of your last period, the date you conceived if you know it, the timing of your IVF transfer, or your first ultrasound date. The tool will do the rest!
How is my due date calculated?
There are several ways your due date is determined. If you happen to know the day you conceived, you can count 38 weeks from that day to find your due date. (Human gestation takes about 38 weeks.)
But very few expectant moms know exactly when they conceived. Even if you only had sex once during your fertile period, you wouldn't conceive on that day unless you happen to be ovulating.
Sperm can live for up to five days inside your fallopian tubes. Meaning it could be up to five days after you have sex that you release an egg (ovulate) and it gets fertilized by a waiting sperm. That's the day you conceive.
Meaning it could be up to five days after you have sex that you release an egg (ovulate) and it gets fertilized by a waiting sperm. That's the day you conceive.
So without knowing the day of conception, how does anyone determine a due date?
First day of your last period
The most common way to calculate your pregnancy due date is by counting 40 weeks from the first day of your last menstrual period (LMP) (or choosing that option from our tool’s menu above). And that's how most healthcare providers do it.
If your menstrual cycle length is the average length (28-day cycle), your period probably started about two weeks before you conceived. This explains why pregnancies are said to last 40 weeks instead of 38 weeks.
This method doesn't take into account how long your cycle actually is or when you think you might have conceived. But generally speaking, women typically ovulate about two weeks after their menstrual cycle starts. And women are more likely to know when their last period started than the day they ovulated.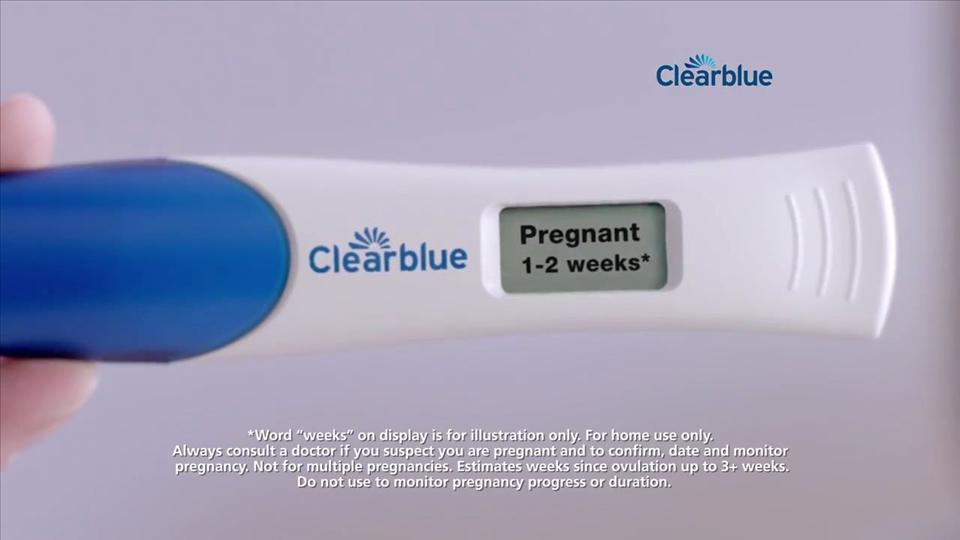
Conception date
If you do happen to know precisely when you conceived – say, if you were using an ovulation predictor kit or tracking your ovulation symptoms – you can calculate your pregnancy due date based on your conception date. Just choose that calculation method from the pulldown above and put in your date.
Remember, you don't necessarily conceive on the day you have sex.
IVF transfer date
If you conceived through IVF, you can calculate your due date using your IVF transfer date. If you had a Day 5 embryo transfer, count 261 days from your transfer date. If you had a Day 3 embryo transfer, count 263 days. Or select "IVF" from our Due Date Calculator method choices.
Ultrasound scan
If you want to try a different method for calculating your due date and are among those who have at least one early, first trimester ultrasound, that scan in your doctor’s or midwife’s office can help you and your practitioner pinpoint when your baby is expected to arrive.
The timing of an early ultrasound can sometimes more accurately date the pregnancy than your last menstrual period, conception date, and other methods. Just choose "ultrasound" from our Due Date Calculator dropdown menu.
Remember, however, that not all pregnant women will have an ultrasound at their first prenatal appointment or another early check-up. Some practitioners perform them for all expectant patients, while others only do them if your due date can’t be calculated by the usual methods or determined via a physical exam.
They might also do early ultrasounds if you have risk factors including previous pregnancy complications, a history of miscarriages or other pregnancy losses, irregular periods or trouble conceiving, various chronic health conditions, or are 35 or older.
Can my due date change?
Your healthcare provider might revise your due date if your baby is measured during a first trimester ultrasound scan and found to be much bigger or smaller than expected for gestational age. This is more likely to happen if you have an irregular menstrual cycle length that makes it hard to pinpoint the date of conception.
This is more likely to happen if you have an irregular menstrual cycle length that makes it hard to pinpoint the date of conception.
Your healthcare provider will measure your baby during that ultrasound exam to figure out how far along your baby is and then provide you with a new due date.
What if I already know my due date?
If you already know your due date, you can use this calculator to see your pregnancy timeline. It will tell you when you'll hit various milestones, and when you may be due for prenatal tests and prenatal visits.
You'll also find out what your baby's sign and birthstone will probably be and a few famous people who were born on your due date.
How likely am I to give birth on my due date?
Of course, a due date calculation is always approximate, whether it's from our tool or from your doctor or midwife. Only 1 in 20 women delivers on her due date. You're just as likely to go into labor any day during the two weeks before or after.
Want more information about how the weeks, months, and trimesters of pregnancy are counted? See our pregnancy timing chart.
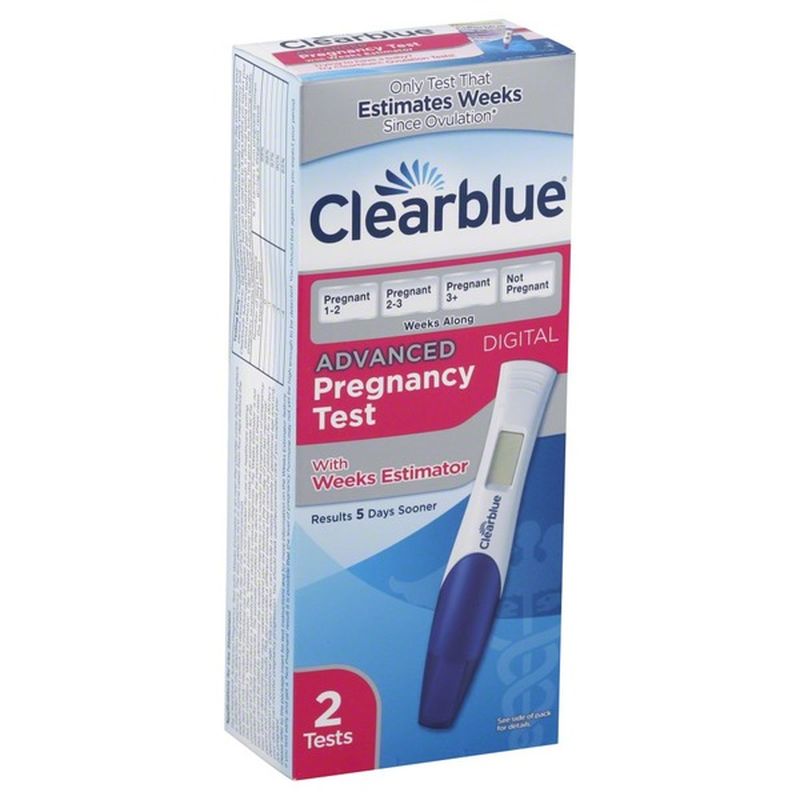
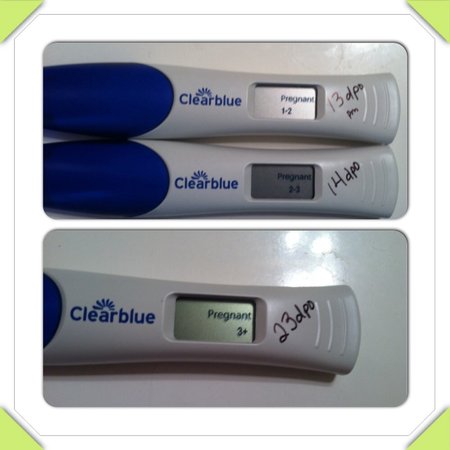
How soon can I take a pregnancy test?
With all this talk about pregnancy due dates, you may be wondering when you can take a pregnancy test. To ensure you get the most accurate reading, it's best to wait a few days after your missed period to take a pregnancy test.
At-home urine tests measure the amount of hCG (human chorionic gonadotropin) present in your body. If you take a pregnancy test before you miss your period, you may not get an accurate result, despite what some tests advertise.
If you're getting a blood test in your provider's office, you may get results sooner. These tests also measure the amount of hCG in your bloodstream, but they're more sensitive than at-home urine tests. Blood tests may be able to detect pregnancy six to eight days after ovulation.
Read more:
- Your pregnancy, week by week
- Your first trimester pregnancy checklist
- Pregnancy Weight Gain Calculator
- Ovulation Calculator
- See all tools
Advertisement | page continues below
Pregnancy calendar
Telephone information
City Clinical Hospital No. 15 named after O.M. Filatov Department of Health of the City of Moscow
15 named after O.M. Filatov Department of Health of the City of Moscow
"Your health is our daily work"
GKB No. 15
- Clinic
- News
- Our news
- Interesting medical case
- Important announcements
- media about us
- Food
- Filatovsky Bulletin
- About us
- City Clinical Hospital No. 15 - 40 years old
- Manual
- Photo gallery
- Feedback and thanks
- Q&A
- Vacancies
- Regulatory framework
- Scientific base
- Parent organizations
- Youth Council
- News
- Branches
- Inpatient departments
- Blood Service
- Maternity Hospital on Veshnyakovskaya
- Maternity hospital on Samarkand Boulevard
- Women's consultation
- Consultative and diagnostic center
- Laboratories, paraclinics
- Interdistrict Department of Multiple Sclerosis (IDMS)
- Pathology department
- Specialists
- Internal labor regulations and Regulation on the protection of personal data
- Short stay hospitals
- For visitors
- Helpful information
- Healthy nutrition information
- Baby supplies gift sets
- Pregnancy calendar
- Drug supply
- Guidelines for new parents
- Fire Patient Aid
- Risk factors for noncommunicable diseases
- Hospitalization regulations
- Project "Moscow - the capital of health"
- Procedure for preparing for diagnostic tests
- Procedure for the provision of high-tech medical care
- Program of state guarantees within the framework of CHI
- Cooperation with insurance organizations on CHI and VHI
- Internal regulations
- Memo for visitors to intensive care units and anesthesiology
- Independent assessment of the quality of services provided
- Entry and Parking Regulations
- Anti-corruption
- Helpful information
- Employees
- International medical tourism
- Contacts
- Paid services
- About branch
- Consultative and diagnostic center
- Stationary
- Women's clinics
- Maternity hospital
- Voluntary medical insurance
- Price list
© GKB No.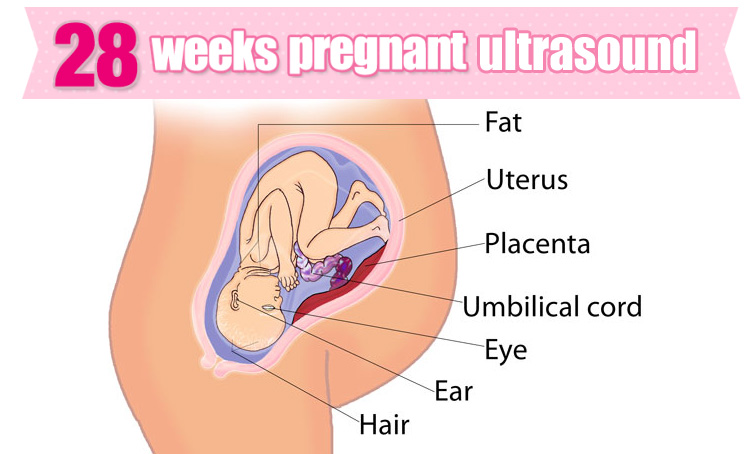 15 im. O. M. Filatova
15 im. O. M. Filatova
All rights reserved
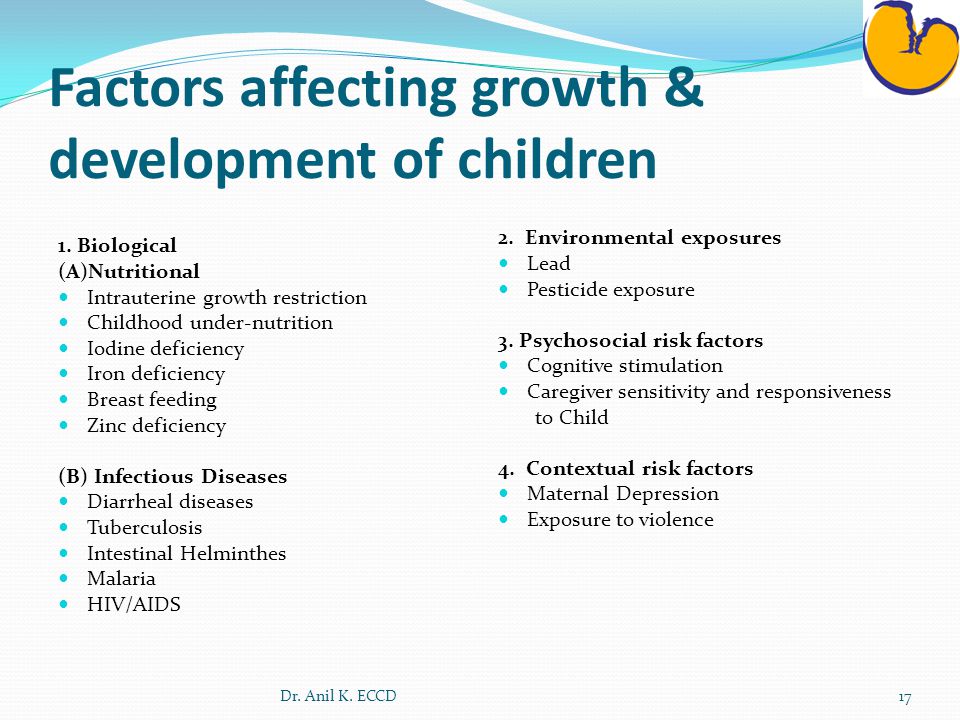
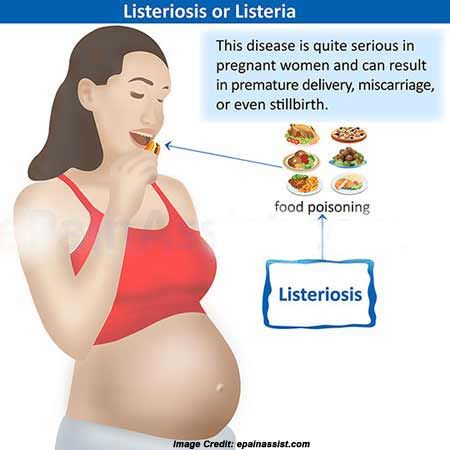
Here are some basic steps you need to take during pregnancy. We labeled them as the "Calendar of physiological (normal) pregnancy":
- When planning pregnancy - Folic acid intake 3 months before the expected date of conception.
- 7 days delayed period => pregnancy test. With a positive test → the first visit to the obstetrician-gynecologist of the antenatal clinic (approximate gestational age is 5-7 weeks): a doctor's examination, ultrasound of the pelvic organs, a blood test for hCG to determine the gestational age, exclude ectopic pregnancy. Continue taking Folic Acid for another 12 weeks, i.e. the entire first trimester.
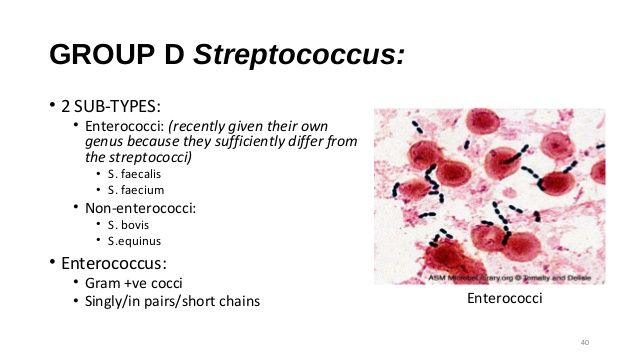
- 7-8 weeks pregnant - pregnancy registration. Complete clinical and laboratory examination: clinical and biochemical blood tests, hemostasiogram, blood test for RW (syphilis), HIV, HbsAg (hepatitis B and C), TORCH, TSH (thyroid-stimulating hormone), clinical urinalysis.
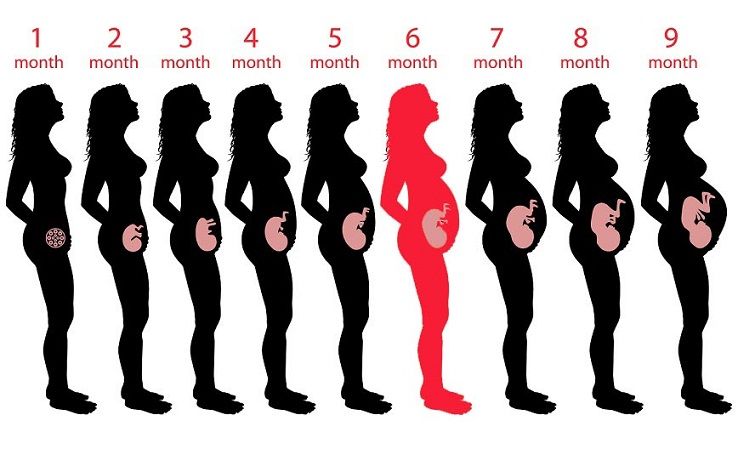 Primary consultation of specialists: therapist, ENT, ophthalmologist, dentist.
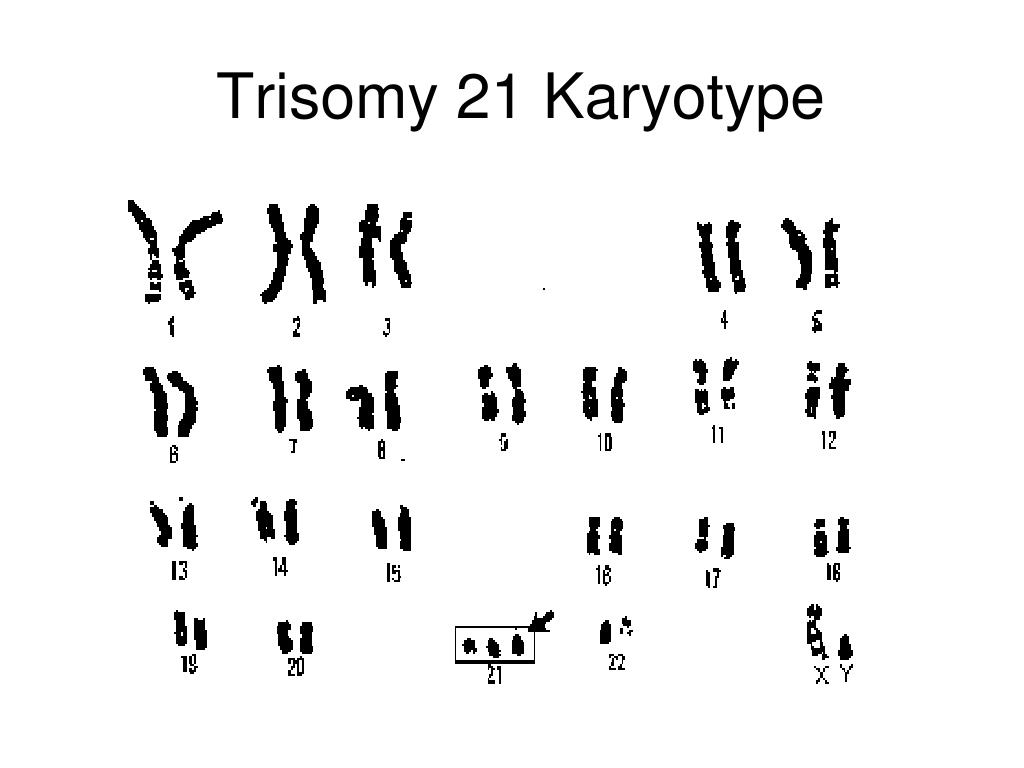
Primary consultation of specialists: therapist, ENT, ophthalmologist, dentist. - 11-13 weeks of pregnancy - I (first) screening: ultrasound of the fetus + biochemical blood test to detect chromosomal diseases in the fetus.
- 19-21 weeks of pregnancy - visit to the obstetrician-gynecologist of the antenatal clinic. Carrying out the II (second) screening.
- 23-24 weeks of pregnancy - visit to the obstetrician-gynecologist of the antenatal clinic. Conducting a glucose tolerance test to detect latent diabetes mellitus.
- 30 weeks of pregnancy - visit to the obstetrician-gynecologist of the antenatal clinic. Registration of maternity leave (issuance of a disability certificate for pregnancy and childbirth) + receipt of a birth certificate. Repeated full clinical and laboratory examination. Repeated consultation of specialists (therapist + ophthalmologist). Carrying out III (third) screening (fetal ultrasound + vascular Doppler).

- 32 weeks pregnant - CTG (fetal cardiotocography).
- 36 weeks pregnant - taking a bacteriological culture of the cervical canal.
- 38 weeks pregnant - CTG (fetal cardiotocography).
- 40-41 weeks of pregnancy - hospitalization in the maternity hospital for childbirth.
Please note that if there are indications for a caesarean section, the terms of hospitalization in the maternity hospital depend on the specific somatic pathology, and the date of hospitalization will be assigned to you by the obstetrician-gynecologist of the antenatal clinic or the obstetrician-gynecologist of the maternity hospital.
We are always ready to provide you with the necessary medical assistance!
Be healthy and happy!
Screening for the detection of congenital fetal diseases during pregnancy
Category: Reminders for the population .
Screening during pregnancy is a whole range of studies that allows parents and doctors to get the most complete information about the health of an unborn baby. Screening reveals many congenital and physical characteristics. How and when is pregnancy screening done
What is pregnancy screening and why is it done
Screening during pregnancy is a complex of examinations, which includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to start treating genetic diseases as early as possible and, if not completely cure them, then at least stop the symptoms as much as possible. If the doctor notices any abnormalities during the examination, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth.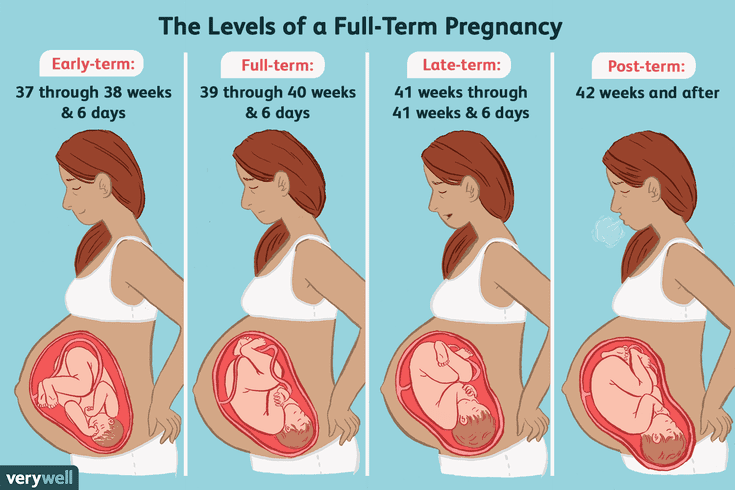 If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
Pregnancy screening is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not give a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman's compliance with the rules for preparing for the examination, and other factors.
First pregnancy screening
The first screening during pregnancy is carried out between the 11th and 13th weeks. It makes no sense to undergo this examination earlier - before the 11th week of pregnancy, many indicators are practically indeterminate.
The study includes two medical tests - an ultrasound and a blood test.
ultrasound
With the help of ultrasound, the doctor determines the exact gestational age, evaluates the baby's physique, its dimensions (head circumference, limb length, height), the work of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus. For each of these parameters, there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy, these rates are:
- KTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the tailbone) is 43–65 mm. If this figure is more than normal, then the child will be large. A downward deviation indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case, the heart will not be auscultated). However, this may also be due to a banal mistake in determining the timing of pregnancy.
- BDP (biparietal size, that is, the distance from the temple to the temple) - 17-24 mm. A high BDP means a large fetus, but only on the condition that all other indicators say the same. Otherwise, we can talk about a herniated brain or hydrocephalus. Low BDP indicates slow brain development.
- TVP (collar space thickness) - 1.
 6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research.
6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research.
The length of the nasal bone is 2–4.2 mm. Too small a nose bone can indicate pathology or simply that the baby's nose will be snub-nosed. HR (heart rate) - 140-160 beats per minute. A small (up to 40 beats per minute) deviation in one direction or another is considered a variant of the norm.
The size of the chorion, amnion and yolk sac. The chorion is the outer shell of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion previa. This is a potentially dangerous situation, fraught with miscarriage, and in this case, bed rest is recommended for the pregnant woman.
The amnion is the inner membrane that holds the amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of a fetus's life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies.
Cervix. Normally, its length by the time of the first screening is 35–40 mm. A shorter cervix means a risk of preterm labor.
Ultrasound is performed in two ways - transabdominal, in which the sensor of the ultrasound machine is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but it is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdomen does not allow the fetus and uterus to be examined in detail.
It is necessary to properly prepare for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that the bladder is full at the time of the examination - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With transvaginal ultrasound, the degree of fullness of the bladder does not matter, however, before the examination, it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is carried out. Therefore, expectant mothers suffering from flatulence are advised the day before the examination to take remedies for flatulence and not eat anything that produces gas.
Blood test
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.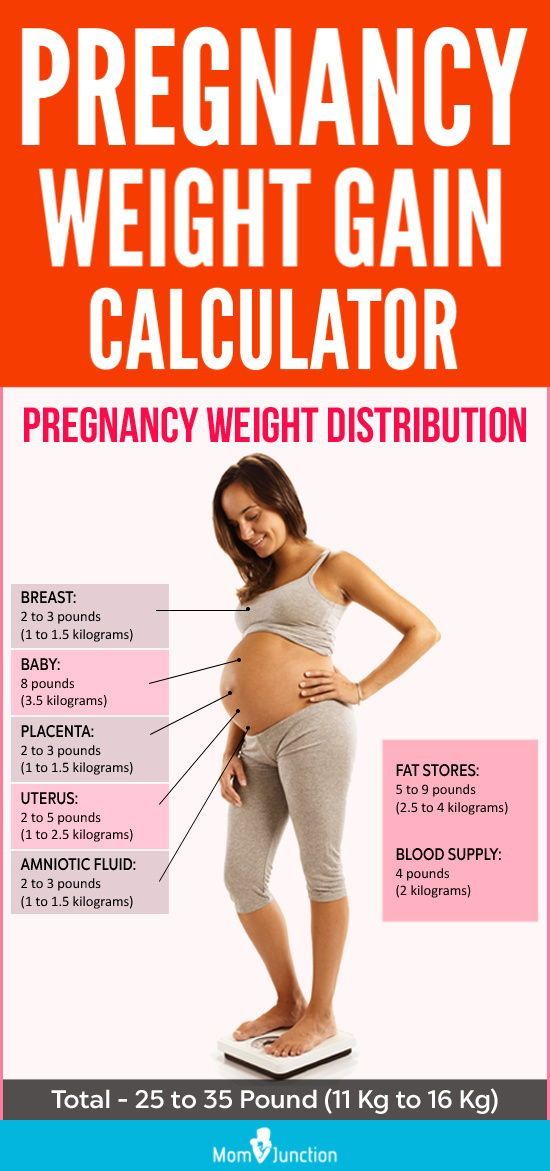
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU / ml is considered the norm. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes in the mother. Reduced hCG is typical of miscarriage, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome).
- PAPP-A is an A-plasma protein. The content rate for a period of 11–13 weeks is 0.79–6.01 mU / l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- A high PAPP-A is a sign of multiple pregnancies, large fetuses, or a low placenta.
In order for the blood test to give the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal.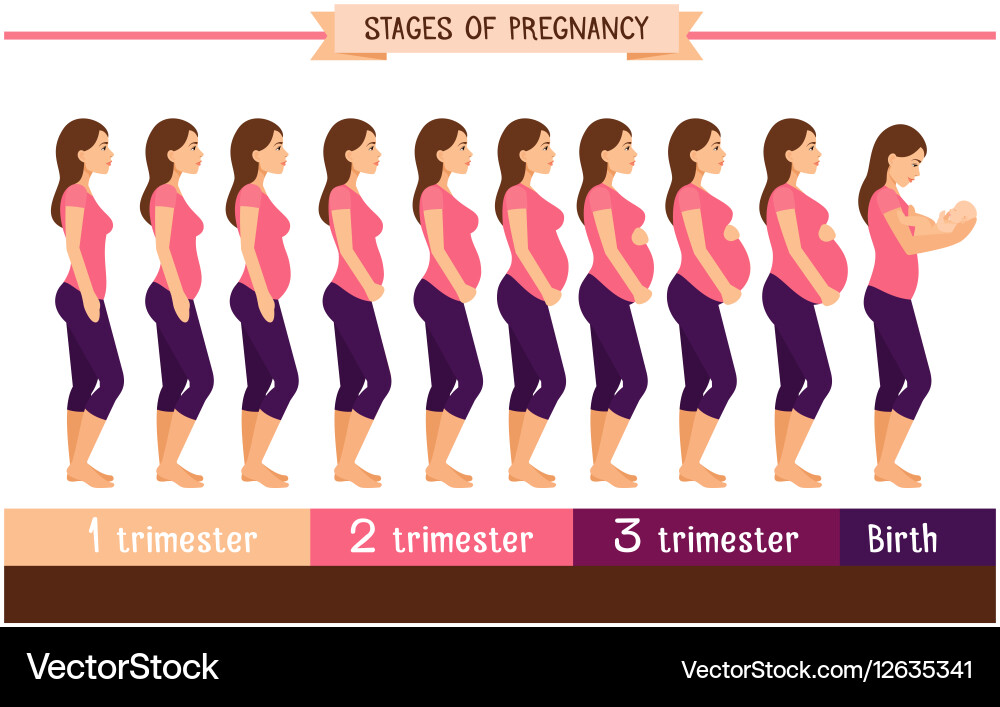 2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
Second pregnancy screening
The second screening during pregnancy is carried out at 16-20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood test.
ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate main indicators of the norm for a period of 16-20 weeks:
- BPR - 26–56 mm.
- DBK (length of the femur) - 13-38 mm.
- DPC (length of the humerus) - 13-36 mm.
- OG (head circumference) - 112-186 mm.
IAF (amniotic fluid index, that is, the volume of amniotic fluid) - 73-230 mm. Oligohydramnios can adversely affect the condition of the child's bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such localization, detachment of the placenta is possible.
Umbilical cord. One of the most important parameters is the place of attachment of the umbilical cord. Marginal, split or sheath attachment is fraught with fetal hypoxia and difficulties during childbirth, often it becomes an indication for caesarean section. The umbilical cord is fed through 2 arteries and 1 vein, although sometimes only one artery is available. This can cause fetal hypoxia, heart disease, disorders in the child’s cardiovascular system, and cause a baby’s low body weight. However, if all other analyzes and examinations do not show deviations from the norm, you should not worry.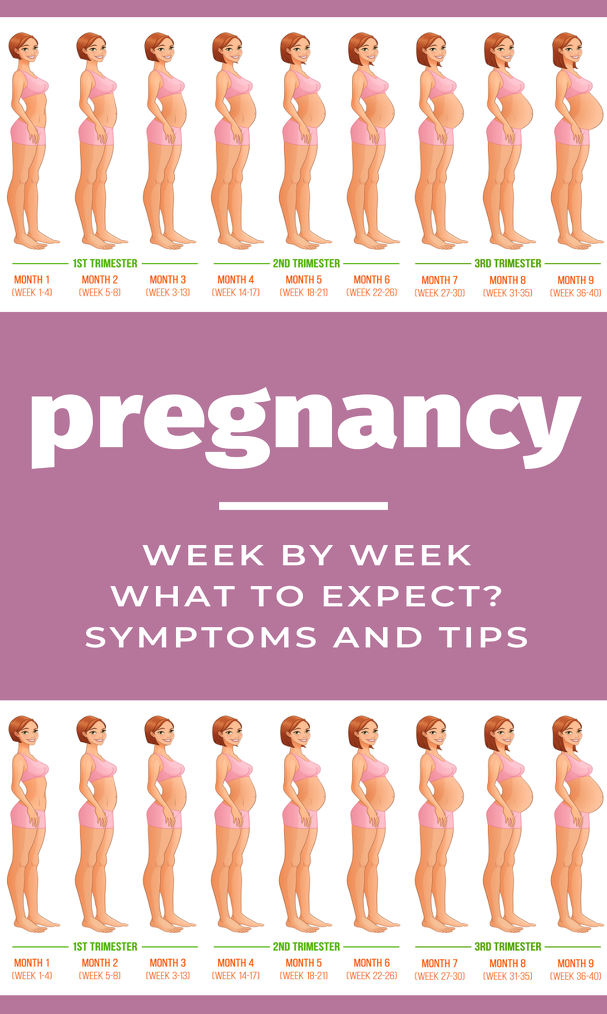
Cervix. The length of the cervix at this time should be 40–45 mm. A short cervix means a threatened miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the peculiarities of the position of the fetus or the excess weight of the expectant mother, and by edema or hypertonicity of the uterus.
Blood test
As during the first screening, during the second, a blood test for b-hCG is taken, the level of free estriol and AFP is also checked. Here are the norms for their content at the 16th-20th weeks of pregnancy:
- b-hCG - 4.67-5-27 ng / ml.
- Free estriol is a hormone whose level can be used to judge the state of the placenta. The norm is 1.17–3.8 ng / ml. Elevated estriol is characteristic of multiple pregnancy or a large fetus. Reduced - for threatened miscarriage, placental insufficiency, anencephaly and Down's syndrome.
- AFP is a protein that is produced in the gastrointestinal tract of the fetus.
 Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Third pregnancy screening
The third screening during pregnancy is carried out at the 30th-43rd week. Based on the results of this screening, the doctor decides on the need for a caesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes dopplerography is prescribed - a study of the work of blood vessels. Here are the approximate norms for a given gestational age:
ultrasound
- BPR — 67–91 mm
- DBK - 47-71 mm
- WPC - 44-63 mm
- Exhaust gas - 238-336 mm
- IAG — 82- 278 mm
The thickness of the placenta is 23.