When to test for group b strep
Strep B Test: MedlinePlus Medical Test
What is a group B strep test?
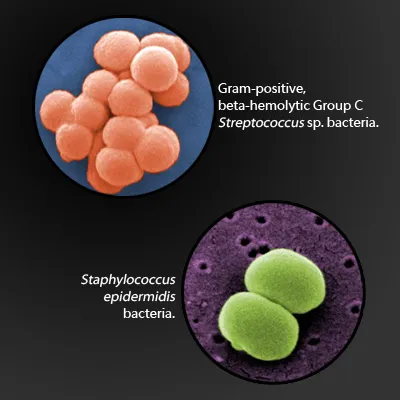
Strep B, also known as group B strep (GBS), is a type of bacteria commonly found in the digestive tract, urinary tract, and genital area. It rarely causes symptoms or problems in adults but can be deadly to newborns.
In women, GBS is mostly found in the vagina and rectum. So a pregnant woman who is infected can pass the bacteria to her baby during labor and delivery. GBS can cause pneumonia, meningitis, and other serious illnesses in a baby. GBS infections are the leading cause of death and disability in newborns.
A group B strep test checks for GBS bacteria. If the test shows that a pregnant woman has GBS, she can take antibiotics during labor to protect her baby from infection.
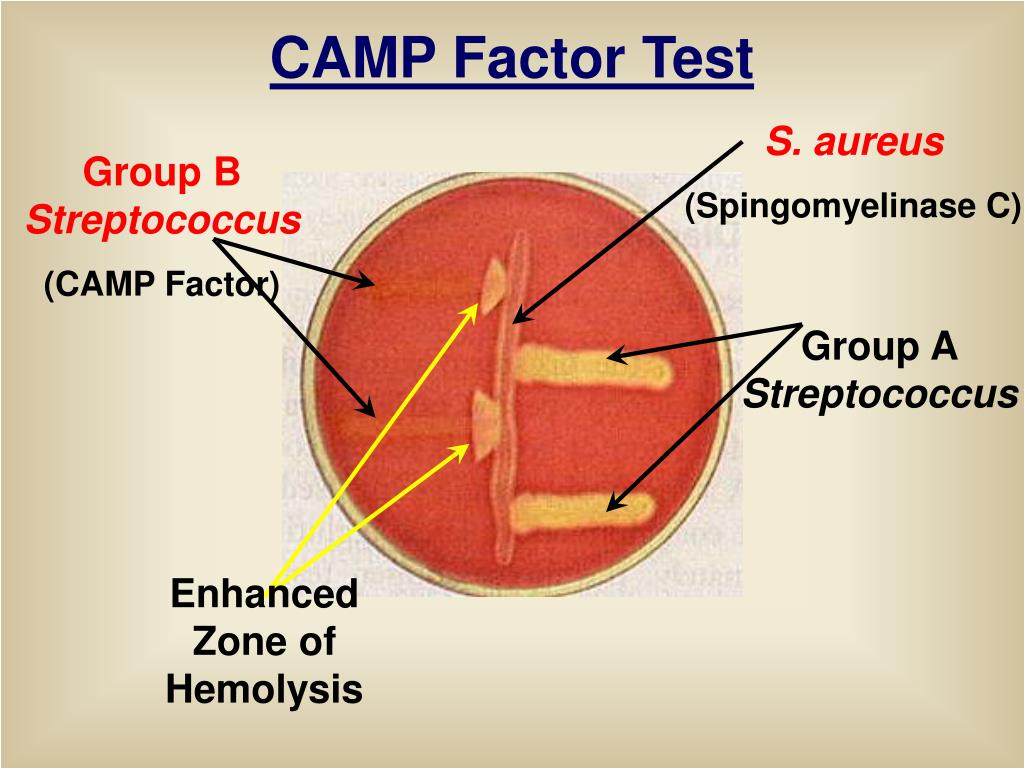
Other names: group B streptococcus, group B beta-hemolytic streptococcus, streptococcus agalactiae, beta-hemolytic strep culture
What is it used for?
A group B strep test is most often used to look for GBS bacteria in pregnant women. Most pregnant women are tested as part of routine prenatal screening. It may also be used to test infants who show signs of infection.
Why do I need a group B strep test?
You may need a strep B test if you are pregnant. The American College of Obstetricians and Gynecologists recommends GBS testing for all pregnant women. Testing is usually done in the 36th or 37th week of pregnancy. If you go into labor earlier than 36 weeks, you may be tested at that time.
A baby may need a group B strep test if he or she has symptoms of infection. These include:
- High fever
- Trouble with feeding
- Trouble breathing
- Lack of energy (hard to wake up)
What happens during a group B strep test?
If you are pregnant, your health care provider may order a swab test or a urine test.
For a swab test, you will lie on your back on an exam table. Your health care provider will use a small cotton swab to take a sample of cells and fluids from your vagina and rectum.
For a urine test, you will most likely be told to use the "clean catch method" to ensure your sample is sterile. It includes the following steps.
- Wash your hands.
- Clean your genital area with a cleansing pad given to you by your provider. To clean, open your labia and wipe from front to back.
- Start to urinate into the toilet.
- Move the collection container under your urine stream.
- Collect at least an ounce or two of urine into the container, which should have markings to indicate the amounts.
- Finish urinating into the toilet.
- Return the sample container as instructed by your health care provider.
If your baby needs testing, a provider may do a blood test or a spinal tap.
For a blood test, a health care professional will use a small needle to take a blood sample from your baby's heel. After the needle is inserted, a small amount of blood will be collected into a test tube or vial.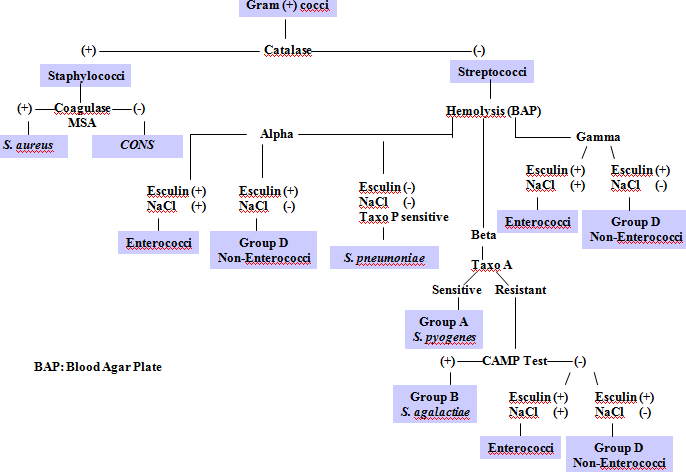 Your baby may feel a little sting when the needle goes in or out.
Your baby may feel a little sting when the needle goes in or out.
A spinal tap, also known as a lumbar puncture, is a test that collects and looks at spinal fluid, the clear liquid that surrounds the brain and spinal cord. During the procedure:
- A nurse or other health care provider will hold your baby in a curled-up position.
- A health care provider will clean your baby's back and inject an anesthetic into the skin, so your baby won't feel pain during the procedure. The provider may put a numbing cream on your baby's back before this injection.
- The provider may also give your baby a sedative and/or pain reliever to help him or her better tolerate the procedure.
- Once the area on the back is completely numb, your provider will insert a thin, hollow needle between two vertebrae in the lower spine. Vertebrae are the small backbones that make up the spine.
- The provider will withdraw a small amount of cerebrospinal fluid for testing.
 This will take about five minutes.
This will take about five minutes.
Will I need to do anything to prepare for the test?
You don't any special preparations for group B strep tests.
Are there any risks to the test?
There is no risk to you from a swab or urine test. Your baby may have slight pain or bruising after a blood test, but that should go away quickly. Your baby will likely feel some pain after a spinal tap, but that shouldn't last too long. There is also a small risk of infection or bleeding after a spinal tap.
What do the results mean?
If you are pregnant and results show you have GBS bacteria, you will be given antibiotics intravenously (directly to your veins) during labor, at least four hours before delivery. This will prevent you from passing the bacteria to your baby. Taking antibiotics earlier in your pregnancy is not effective, because the bacteria can grow back very quickly. It's also more effective to take antibiotics through your vein, rather than by mouth.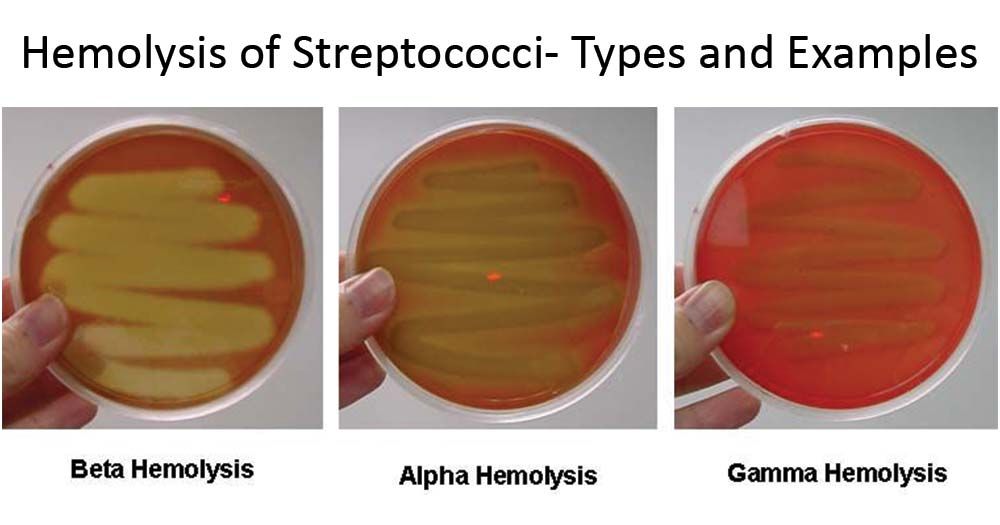
You may not need antibiotics if you are having a planned delivery by Cesarean section (C-section). During a C-section, a baby is delivered through the mother's abdomen rather than vaginally. But you still should be tested during pregnancy because you may go into labor before your scheduled C-section.
If your baby's results show a GBS infection, he or she will be treated with antibiotics. If your provider suspects a GBS infection, he or she may treat your baby before test results are available. This is because GBS can cause serious illness or death.
If you have questions about your results or your baby's results, talk to your health care provider.
Learn more about laboratory tests, reference ranges, and understanding results.
Is there anything else I need to know about a group B strep test?
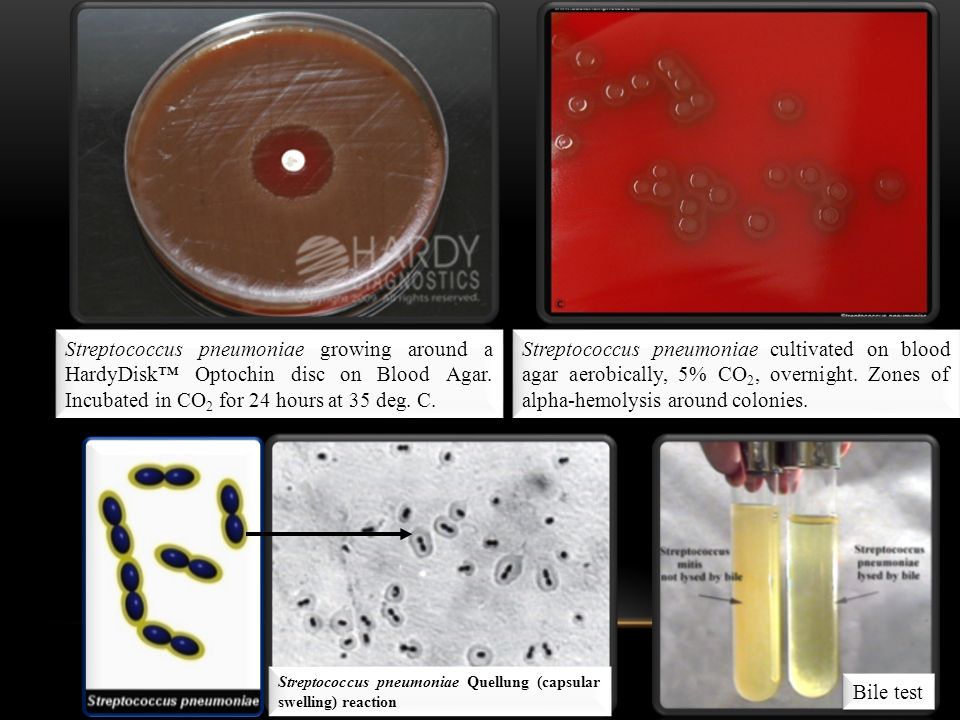
Strep B is one type of strep bacteria. Other forms of strep cause different types of infections. These include strep A, which causes strep throat, and streptococcus pneumoniae, which causes the most common type of pneumonia. Streptococcus pneumonia bacteria can also cause infections of the ear, sinuses, and bloodstream.
Streptococcus pneumonia bacteria can also cause infections of the ear, sinuses, and bloodstream.
References
- ACOG: The American College of Obstetricians and Gynecologists [Internet]. Washington D.C.: American College of Obstetricians and Gynecologists; c2019. Group B Strep and Pregnancy; 2019 Jul [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.acog.org/Patients/FAQs/Group-B-Strep-and-Pregnancy
- Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Group B Strep (GBS): Prevention; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://www.cdc.gov/groupbstrep/about/prevention.html
- Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Group B Strep (GBS): Signs and Symptoms; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://www.cdc.gov/groupbstrep/about/symptoms.html
- Centers for Disease Control and Prevention [Internet].
 Atlanta: U.S. Department of Health and Human Services; Streptococcus Laboratory: Streptococcus pneumoniae; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.cdc.gov/streplab/pneumococcus/index.html
Atlanta: U.S. Department of Health and Human Services; Streptococcus Laboratory: Streptococcus pneumoniae; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.cdc.gov/streplab/pneumococcus/index.html - Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Travelers' Health: Pneumococcal Disease; [updated 2014 Aug 5; cited 2019 Nov 15]; [about 3 screens]. Available from: https://wwwnc.cdc.gov/travel/diseases/pneumococcal-disease-streptococcus-pneumoniae
- Intermountain Healthcare: Primary Children's Hospital [Internet]. Salt Lake City: Intermountain Healthcare; c2019. Lumbar Puncture in a Newborn; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://intermountainhealthcare.org/ext/Dcmnt?ncid=520190573
- Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Blood Culture; [updated 2019 Sep 23; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.
 org/tests/blood-culture
org/tests/blood-culture - Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Prenatal Group B Strep (GBS) Screening; [updated 2019 May 6; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.org/tests/prenatal-group-b-strep-gbs-screening
- Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Urine Culture; [updated 2019 Sep 18; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.org/tests/urine-culture
- Michigan Medicine: University of Michigan [Internet]. Ann Arbor (MI): Regents of the University of Michigan; c1995–2021. Group B Streptococcal Infections in Newborns[cited 2021 Aug 6]; [about 3 screens]. Available from: https://www.uofmhealth.org/health-library/zp3014spec
- University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; c2019. Health Encyclopedia: Group B Streptococcus Infection in Babies; [cited 2019 Nov 15]; [about 2 screens].
 Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02363
Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02363 - University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; c2019. Health Encyclopedia: Pneumonia; [cited 2019 Nov 15]; [about 2 screens]. Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P01321
- WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy [Internet]. Geneva (SUI): World Health Organization; c2010. 6. Paediatric and neonatal blood sampling; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138647
Group B strep test | Pregnancy Birth and Baby
Group B strep test | Pregnancy Birth and Baby beginning of content8-minute read
Listen
If your baby suddenly develops very high fever with vomiting, call triple zero (000) and ask for an ambulance or go to the nearest hospital emergency department.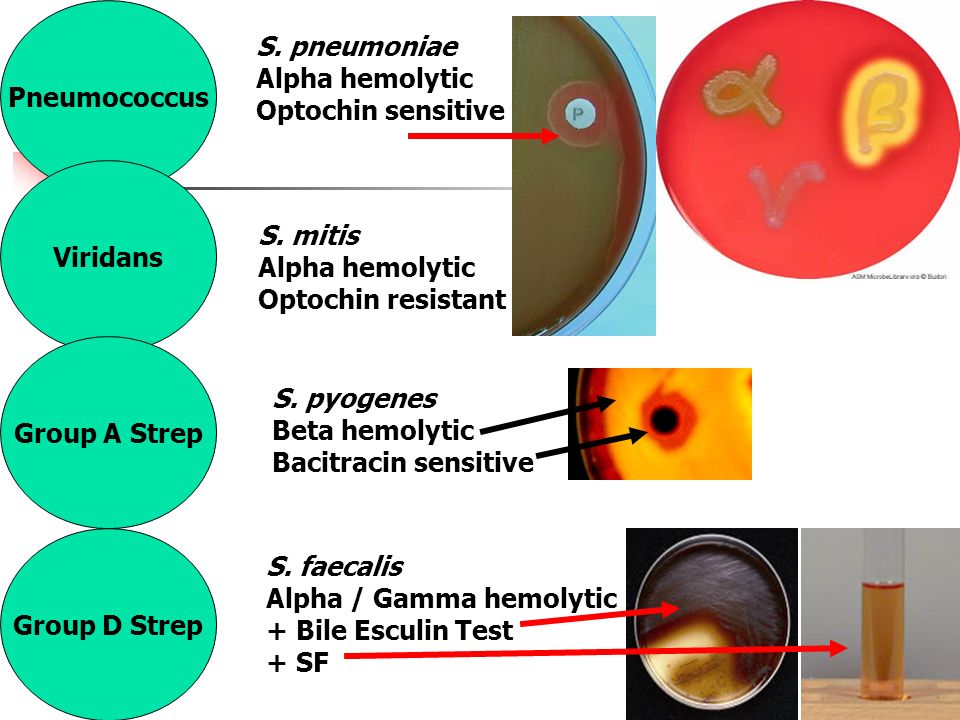
Key facts
- Group B streptococcus (GBS) is part of the normal bacteria that lives in our body. It is most commonly found in the intestines, rectum, urethra or vagina.
- It usually causes no health concerns or symptoms.
- If you are pregnant and have GBS, bacteria can pass to your baby before or during a vaginal birth. In a small number of cases, this may make your baby sick.
- You may be offered a test to check if you have GBS, which involves taking a swab of your vagina at around 35 to 37 weeks of pregnancy.
- If you are a GBS carrier or if you develop risk factors for GBS infection, intravenous antibiotics during labour can reduce the risk of GBS colonisation and an early GBS infection in your baby.
- Testing and treatment for GBS is your choice and should be done in consultation with your care provider.
What is GBS?
Group B streptococcus (GBS) is one of many bacteria that normally live in our bodies. GBS is commonly found in the intestines, rectum, urethra, or vagina.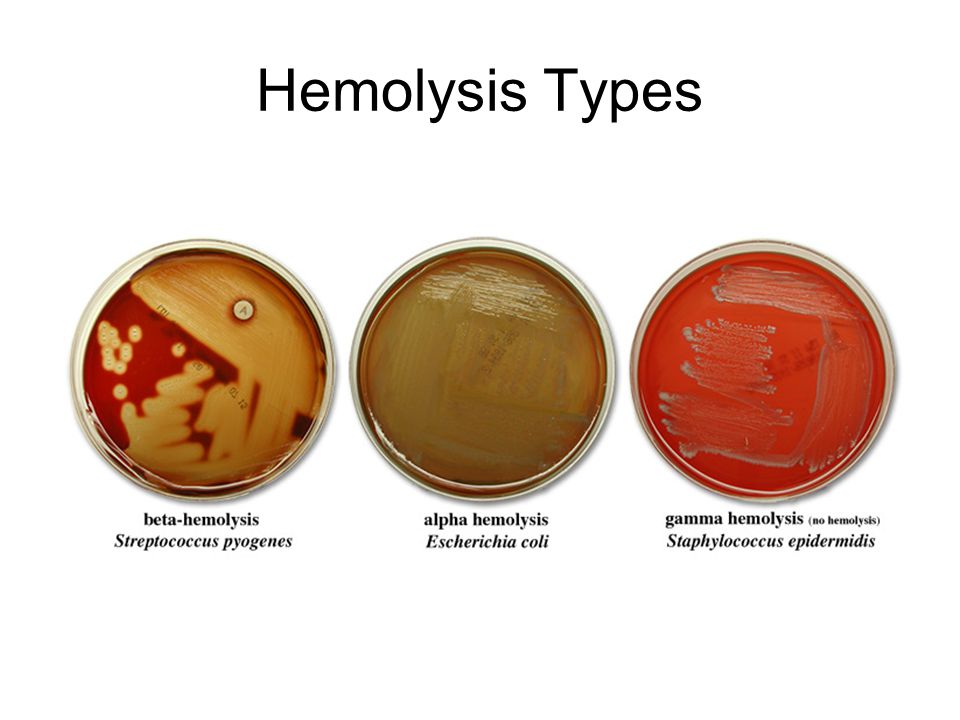 Many people have it, and it usually causes no health concerns or symptoms. This bacterium is transient, meaning that it comes and goes from your body. GBS is not sexually transmitted. Being a carrier of GBS in pregnancy is not usually harmful to you but it can cause infection in some babies.
Many people have it, and it usually causes no health concerns or symptoms. This bacterium is transient, meaning that it comes and goes from your body. GBS is not sexually transmitted. Being a carrier of GBS in pregnancy is not usually harmful to you but it can cause infection in some babies.
Carrying GBS, also known as GBS colonisation is not the same as having a GBS infection.
What could GBS mean for my baby?
Many babies come into contact with GBS during labour or around the time of birth. Most of these babies won’t become unwell. However, if you carry GBS, there is a small chance (about 1 in 1000) that your baby will develop GBS infection in the first week after birth. This is known as ‘early onset GBS infection’.
GBS can cause infections such as pneumonia, blood poisoning (septicaemia), or meningitis (an infection around the brain) in babies. However, with early detection and treatment using intravenous antibiotics, most babies fully recover. A very small number of babies who become infected may have long-term disability and some don’t survive.
Can GBS infection be prevented?
Unfortunately, there is no way to completely prevent GBS infection in babies. However, early detection and treatment with antibiotics can reduce the chance of your baby becoming very unwell.
How is GBS found?
GBS may be found during a routine antenatal test. It can be found in urine or more commonly, when you have a vaginal or rectal swab testing specifically for this bacterium.
There is no standard practice for testing for GBS in Australia, but universal screening for the GBS bacteria is most common. This means that all women will be offered to test for GBS bacteria during pregnancy. Some healthcare providers may only test for GBS if you have risk factors that make GBS infection more likely.
The test can only find GBS if the bacteria is there at the time of testing. Because GBS bacteria comes and goes from your body, routine screening for this bacteria may not detect GBS in everyone who has it during pregnancy.
Testing for GBS involves taking a swab of the inside of the vagina and/or rectum. You can usually do this test yourself, but if you prefer your doctor or midwife can do this for you. The swab is usually taken between 35 to 37 weeks of pregnancy.
You can usually do this test yourself, but if you prefer your doctor or midwife can do this for you. The swab is usually taken between 35 to 37 weeks of pregnancy.
Speak to your doctor or midwife to understand how GBS is tested and managed at your care provider. They can help you to decide if this test is right for you.
Questions you may want to ask your doctor
- What are the risks and benefits to me and my baby if I test for GBS?
- If I have GBS, what does this mean for my pregnancy and birth?
- What is the rate of GBS infection in newborn babies?
- Can my baby become unwell if my test is negative?
What are the risk factors for early onset GBS infection?
Babies are more likely to become infected with GBS if:
- they are born prematurely
- your waters break before 37 weeks of pregnancy
- you give birth more than 18 hours after your waters break
- you have a fever (over 38°C) while in labour
- you've had a previous child with severe GBS infection
- a urine test during pregnancy detected GBS
- a swab taken no more than 5 weeks earlier detected GBS
How is GBS treated?
If your GBS test is positive, or if you have risk factors as listed above, your doctor or midwife will probably recommend that you have intravenous antibiotics when your waters break or when labour starts. If your waters break before your labour starts your healthcare team may recommend inducing labour.
If your waters break before your labour starts your healthcare team may recommend inducing labour.
The antibiotic given is usually penicillin, but other options are available if you are allergic to penicillin. The antibiotics pass through the placenta and into your baby’s blood. This reduces your baby's chances of GBS colonisation and infection.
There is usually no need for screening or treatment with antibiotics for GBS before a planned caesarean, because the baby will not pass through your vagina.
What happens after the birth?
All babies are monitored for the first couple of days for signs of infection. Your baby’s health team will monitor their heart rate, breathing and temperature to check they are well. The chance of your baby being infected with GBS is very low.
Signs that your baby is not well may include:
- abnormal breathing sounds, such as ‘grunting’ with each breath out
- difficulty breathing or breathing too fast or slow
- sleepiness and not interested in feeding
- vomiting
- having trouble keeping their temperature at the right level (being too hot or too cold)
- looking pale or blotchy
- floppy arms and legs
If you notice any of these signs in hospital or at home, it’s important that you contact your healthcare provider straight away.
What is late-onset group B strep?
Rarely, babies can develop GBS infection weeks or months after birth. This is called ‘late onset group B strep'. They become seriously unwell quite quickly with fevers, vomiting and difficulty feeding. Unfortunately, the group B strep test and use of antibiotics during labour doesn’t prevent a baby developing late-onset group B strep infection.
If your baby's condition deteriorates quickly, call triple zero (000) and ask for an ambulance or go to the nearest hospital emergency department.
If you want more information about GBS, or if you have any concerns about your baby, call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse, or talk to your midwife or doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Department of Health (Pregnancy Care Guidelines, Group B streptococcus), RANZCOG (Group B Streptococcus), Mater Mothers Hospital (Group B streptococcus and pregnancy), Safer Care Victoria (Group B streptococcus (GBS) – screening and management), Monash Women's (Group B streptococcus (GBS) screening)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Pregnancy checkups, screenings and scans
- Routine antenatal tests
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.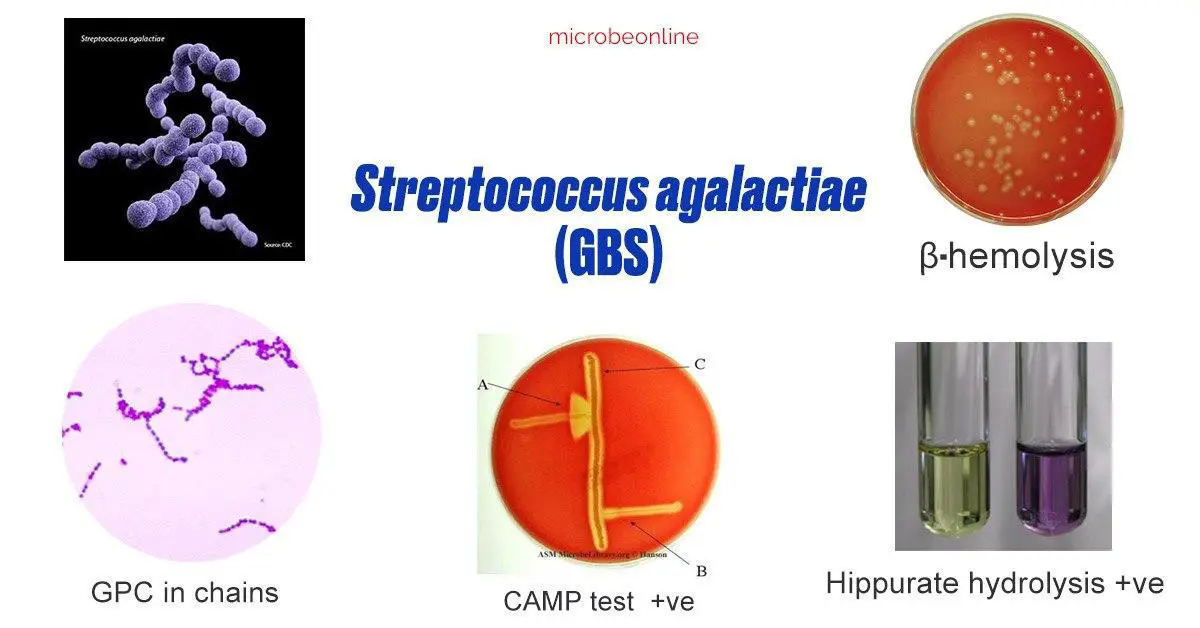
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Culture for group B beta-hemolytic streptococcus (Streptococcus group B, S. agalactiae)
Method of determination The study is carried out by the method of sowing on dense nutrient media. The identification of microorganisms is carried out by mass spectrometry using a Microflex Brucker Daltonik MALDI Biotyper, BRUKER, Germany.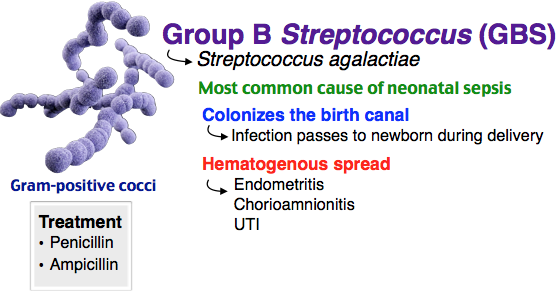
Test material A swab from the entrance to the vagina or anorectal area; vaginal discharge, cervical discharge
Home visit available
Synonyms: Streptococcus group B (S. agalactiae) Culture.
Brief description of the study "Culture for group B beta-hemolytic streptococcus (Streptococcus group B, S. agalactiae)"
Group B streptococcus (GBS, Streptococcus agalactiae) causes severe illness in newborns and is dangerous for certain patients other age groups.
In the vast majority of cases, newborns become infected with GBS during maternal deliveries, with a higher incidence during vaginal delivery. GBS causes early neonatal infections such as sepsis, meningitis, pneumonia, osteomyelitis, arthritis, and pyelonephritis, with rates ranging from 0.2 to 5 or more per 1,000 live births in different countries. In obstetric practice, group B streptococcus is associated with bacteremia, urinary tract infections, chorioamnionitis, premature rupture of amniotic fluid, preterm labor, postpartum endometritis, etc.
GBS in the human body can colonize the oropharynx, anal area of the rectum, vagina (usually vestibule), urogenital tract, skin.
It has been established that GBS in 5-35% of women can be detected in the vagina and often in the urethra of their sexual partners A significant association of carriage of GBS in the vagina has been shown not only with early septicemia of newborns, but also with spontaneous miscarriages, premature birth, premature rupture of amniotic fluid , urinary infection in pregnant women, the birth of children with low body weight, the development of chorioamnionitis in childbirth, endometritis and sepsis in puerperas. The highest level of colonization in women of reproductive age and pregnant women. In pregnant women, GBS is isolated from the listed areas in 7-30% of cases (more often in young people who have high sexual activity or use intrauterine contraceptives). Of these, 60-75% remain GBS carriers until the end of pregnancy.
Vaginal-rectal swabs are collected to detect colonization of the vagina of pregnant women with group B streptococcus.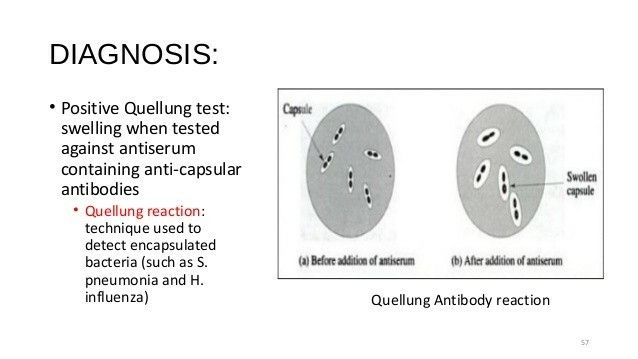 In all other cases, the biomaterial is taken only if there are clinical signs of infection.
In all other cases, the biomaterial is taken only if there are clinical signs of infection.
GBS has a natural sensitivity to beta-lactam antibiotics, including penicillins. Determination of sensitivity is necessary in cases where the patient has an individual intolerance to drugs of this group.
Isolateable microorganisms and pathogens:
- Streptococcus agalactiae.
What is the purpose of culture for group B beta-hemolytic streptococcus (Streptococcus group B, S. agalactiae)? in order to identify bacteriocarrier and determine the need for antibiotic prophylaxis during childbirth, to prevent neonatal complications (septicemia, pneumonia and neonatal meningitis).
What can affect the result of the test "Culture for beta-hemolytic streptococcus group B (Streptococcus group B, S. agalactiae)"
Failure to follow the rules for preparing for the study may affect the result of the test.
What is a streptatest and why should it be done?
Streptatest in the package
Article rating
3. 64 (Votes: 14)
Contents
- Who needs a strepta test?
- How is a strep test performed?
- Benefits of a streptate test:
Streptatest is a fast and informative method for the detection of a pathogenic strain of streptococcus, namely group A b-hemolytic streptococcus, which is a frequent causative agent of upper respiratory tract infections, primarily tonsillitis and scarlet fever. The danger of these diseases is in their complications, with untimely or inadequate antibiotic therapy within a few weeks after the disease, rheumatic joint damage may develop with involvement of the heart and kidneys.
Who needs a strepta test?
If you suffer from tonsillitis, tonsillitis, frequent sore throats accompanied by pain, then you need to have a streptate test.
This will distinguish streptococcal infections that require antibiotics from other sore throats such as viral infections that do not require antibiotics. Thus streptatest will help the doctor to make the correct diagnosis and prescribe the correct treatment.
Accordingly, in case of a positive result, it is necessary to prescribe antibacterial drugs, in case of a negative result, their unreasonable prescription should be avoided.
How is the strep test performed?
The Streptatest is easy to use, results are ready in five minutes, unlike traditional methods of detection and identification of the pathogen, when it takes 24 to 48 hours. A swab is taken from the tonsils, throat and all inflamed areas with a special swab, which is then placed in a test tube with a special reagent, after a certain time the swab is removed from the test tube and a test strip is placed in the test tube.
After 5 minutes the result can be read. If the concentration of the pathogen is high, then a positive result may appear in the first minute, but to verify a negative result, you must wait 5 minutes.
Advantages of the streptate test
- Has no age restrictions.