Pelvic floor dysfunction before pregnancy
What you should know about your pelvic floor: pre-pregnancy, during pregnancy and after giving birth
Squeezes, Kegels, zip-ups – whatever you call them, pelvic floor exercises are important for women at all stages of life.
Pregnancy and birth (both vaginal and caesarean) can put stress on and damage the pelvic floor. So, if you are planning to have a baby, you’re pregnant or you’ve had a baby (or a few), now is an especially important time to pay attention to those muscles downtown.
We spoke with Women’s Health Physiotherapist Marian Donnelly and the pelvic floor team from the RBWH Women’s Health Physiotherapy Department about what you should be paying attention to when you think pelvic floor.
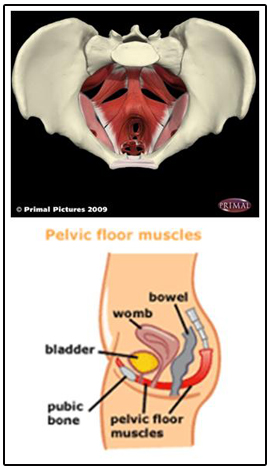
What is my pelvic floor?
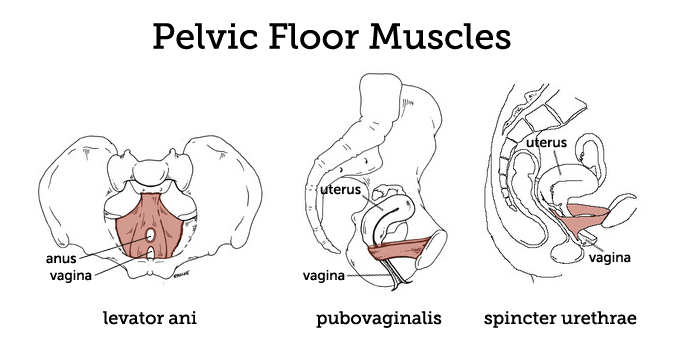
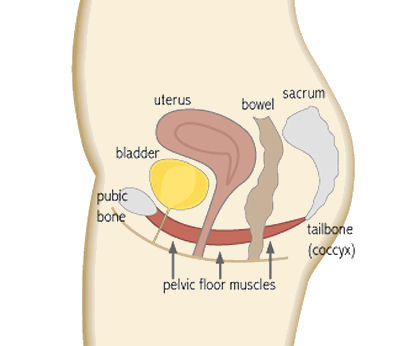
Your pelvic floor is the band of muscles that stretches across the bottom of your abdomen, from your tailbone to your pubic bone. These muscles support your pelvic organs, which include your uterus, bladder and bowel. Think of your pelvic floor like a hammock on which these organs rest. The pelvic floor muscles also help stabilise your spine.
Your pelvic floor includes your sphincters, which are the muscles that surround your urethra and anus. These are the muscles that you use to stop yourself from peeing, pooing or passing wind when you don’t want to, including when you do things like exercise or sneeze. Your vaginal muscles are an important part of your pelvic floor too. These muscles are used during sex and giving birth vaginally.
Marian says there are signs women can look out for that might indicate an issue with their pelvic floor.
“Leakage of urine and vaginal heaviness are two obvious signs of pelvic floor problems. Less obvious signs could be pelvic girdle pain, lower back pain, constipation and pain during intercourse.”
Why should I exercise my pelvic floor?
The benefits of a healthy pelvic floor are numerous. Exercising these muscles before falling pregnant and during pregnancy can decrease the damage done to the muscles by the strain of carrying a growing baby, decrease the risk of injury during a vaginal birth and speed up recovery afterwards. A strong pelvic floor can also make sex more enjoyable.
A strong pelvic floor can also make sex more enjoyable.
And if you don’t pay your pelvic floor some attention?
Marian says, “A weak or damaged pelvic floor can lead to urinary and faecal incontinence, urgency and frequency, as well as pelvic organ prolapse (which happens when the pelvic organs bulge into the walls of the vagina). A weak pelvic floor can also contribute to pelvic girdle pain and lower back pain.”
Marian adds, “After having a child, many women also wish to return to sports and recreational activities that require good pelvic floor strength.”
So, if you’re planning to hit the gym or run around the backyard with the kids, or if you’re prone to the occasional sneeze, pelvic floor strength is going to be your friend.
What happens to the pelvic floor during pregnancy and birth?
Marian explains that as your baby and belly are growing, your pelvic floor is changing, too.
“Pelvic floor muscles work harder than normal during pregnancy: they are required to support the weight of the growing baby. They are also softened by the effects of pregnancy hormones.”
Whether your give birth vaginally or by caesarean, you’re pelvic floor muscles will be impacted.
“During a vaginal birth, the pelvic floor muscles undergo considerable stretching and strain. During a caesarean, surgery through multiple muscle layers can lead to a slower recovery generally and a weakened abdominal wall.”
While pregnant, women can still exercise their pelvic floor, but might need to change their routine. Marian recommends talking to a physiotherapist about your pelvic floor during pregnancy.
“During pregnancy, pelvic floor exercises become more difficult. A pelvic floor physiotherapist can modify an individual program of safe pelvic floor exercises as the pregnancy progresses.”
The pelvic floor after giving birth
Things change again after giving birth, and it can be a good idea to talk to an expert about what you should be doing to help your pelvic floor recover and regain strength.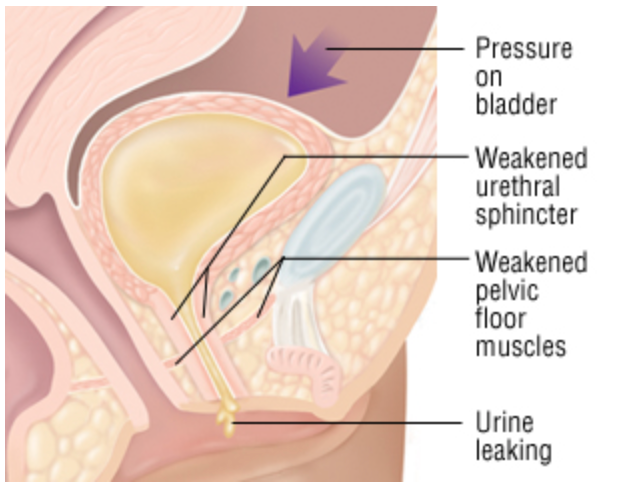
Marian says, “Pelvic floor exercises done post birth are very different from those done before the birth. The state of the perineum and the length of the second stage of labour are just two of many factors a physiotherapist considers when prescribing an individual pelvic floor exercise program after a woman has given birth.
In the first six weeks the pelvic floor focus is on recovery. Research indicates the benefit of strengthening from 6 weeks, especially if there has been any perineal trauma.”
I’m not pregnant yet, should I start pelvic floor exercises now?
Yes – when it comes to strengthening your pelvic floor it’s a case of the earlier, the better.
Marian says, “The earlier you start your pelvic floor exercises, if taught correctly, the better the likelihood of success with pelvic floor strength.
Research shows that correct training in pelvic floor technique is essential, as many women completing pelvic floor exercises under group direction are not doing their pelvic floor exercises correctly. ”
”
How to exercise your pelvic floor properly
Just like you might hire a PT to show you how to use gym equipment properly, you can work with your GP or ask for a referral to see a pelvic floor physiotherapist to learn how to exercise your pelvic floor in the right way.
Continence Australia has a general guide to pelvic floor exercises for all women on their website. Keep in mind that as your body changes during pregnancy and as you get older, or if you don’t know if you’re doing the exercises correctly, a pelvic floor physiotherapist will be able to help you work on a program suited to your individual needs.
During pregnancy, download the Pregnancy Pelvic Floor Plan app for tips on looking after your pelvic floor during pregnancy and reminders on when to do your pelvic floor exercises.
Getting it right
It turns out many women aren’t doing their pelvic floor exercises in the right way, and unfortunately, this can do more harm than good.
Marian says some of the common mistakes women make when exercising their pelvic floor include holding their breath and using accessory muscles incorrectly while doing the exercises. Some women also find that they ‘bear down’ with the muscles instead of ‘pulling up’.
Some women also find that they ‘bear down’ with the muscles instead of ‘pulling up’.
Marian also discourages women from overdoing it after they’ve had a baby.
“Don’t join boot camp before your pelvic floor has fully recovered!
Many women assume that once the baby is born they can return to full pre-pregnancy exercise. This is not the case, as hormonal changes continue in the long-term and are related to how long a women breast feeds and when periods return.
There is also a time lag beyond pregnancy for return to pre-pregnancy hormone levels. These hormones serve to soften the support structures in the pelvic floor.”
I’m busy. Do I really,
really have to?Women have a lot on their plate, and kids only make the schedule busier. Is it really that important to work your pelvic floor?
Marian says, “Yes! In most cases, pelvic floor exercises usually take less than five minutes and can be completed sitting down, at the traffic lights, watching TV or eating dinner – mums can multitask while doing their pelvic floor exercises!”
Your pelvic floor is going to play a role in your overall health for the rest of your life. It’s never too early or late to learn about and strengthen your pelvic floor.
It’s never too early or late to learn about and strengthen your pelvic floor.
Why Pelvic Floor Health Is Important to Your Pregnancy: Kelly Morales, MD, FACOG: Obstetrics & Gynecology
Why Pelvic Floor Health Is Important to Your Pregnancy: Kelly Morales, MD, FACOG: Obstetrics & GynecologyMost women don’t think about their pelvic floor until after they’ve had a baby or two and are having trouble with urine leaking. But waiting until after your baby is born isn’t the right time to start thinking about the health of your pelvic floor.
At Kelly Morales OB/GYN, we’re committed to helping women have the best pregnancies and healthiest babies possible. Dr. Morales and our entire care team understand that a healthy baby starts with a healthy mom. We offer comprehensive pregnancy services to women in and around San Antonio, Texas.
We help you prepare for a healthy pregnancy, delivery, and recovery at home as you care for your baby. Our team has put together this information on pelvic floor health and why it’s imperative for the health of you and your baby.
Our team has put together this information on pelvic floor health and why it’s imperative for the health of you and your baby.
What is the pelvic floor?
Your pelvic floor is made up of layers of muscles, ligaments, and connective tissue that surround your vagina and rectum. The muscles stretch from your pubic bone to your tailbone and support the organs in your pelvis, including your bladder, uterus, and bowel.
You use your pelvic floor muscles during urination and vaginal intercourse. You also use these muscles during childbirth. The pelvic floor is designed to stretch under pressure and bounce back to provide continued support.
How does pregnancy affect my pelvic floor?
During pregnancy, the pelvic floor stretches to make room for the growing baby. Over time, the muscles become weak from being weighed down. Instead of bouncing back to provide support, the weakened muscles may not return to their optimal location.
You may notice it becomes harder to control your bladder, especially as your pregnancy progresses into the second and third trimesters. This is because a weakened pelvic floor makes it difficult to squeeze the muscles necessary to prevent urine from escaping your bladder.
This is because a weakened pelvic floor makes it difficult to squeeze the muscles necessary to prevent urine from escaping your bladder.
Why is pelvic floor health important for my health and my baby’s health?
It’s important to keep your pelvic floor as healthy as possible before, during, and after pregnancy. Starting out your pregnancy with strong pelvic floor muscles helps decrease the damage these muscles experience under the strain of carrying a growing child. A healthy pelvic floor also makes labor and delivery less risky, as you’ll be better equipped for labor, which means less stress for your baby.
And whether you give birth vaginally or through a C-section, the muscles of the pelvic floor undergo quite a bit of stretching and strain. Having a healthy pelvic floor means faster recovery after childbirth.
What’s more? A weakened pelvic floor can lead to pelvic organ prolapse, a condition where your pelvic organs moving out of place and into your vagina, making sex and normal activities uncomfortable and even painful.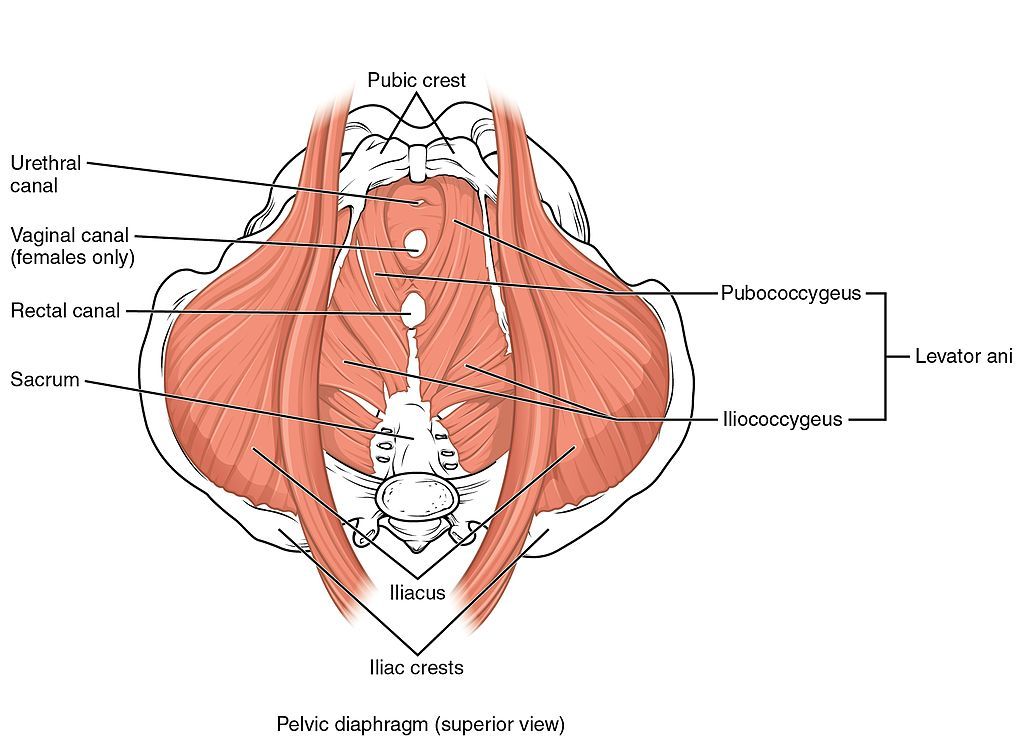
What can I do to improve the health of my pelvic floor?
Pregnancy and childbirth put an enormous amount of strain on your body, but there are steps you can take to improve the health of your pelvic floor, whether you’re pregnant now, thinking about becoming pregnant, or already have children.
Here are some of the ways you can protect your pelvic floor health:
- Maintain a healthy body weight and healthy weight gain during your pregnancy
- Avoid exercises and activities that exert excess pressure on your abdomen — especially during the second and third trimesters
- Give yourself time to rest and recover after exercise or exertion
- Engage in safe pelvic floor exercises to strengthen your muscles, such as pelvic tilts, bridges, and Kegel exercises
Don’t hesitate to ask for guidance when it comes to pelvic floor exercises. It can be tricky to know which muscles to squeeze and when, and some women make the common mistake of holding their breath during the exercises or using additional muscles incorrectly.
Depending on your needs, Dr. Morales and our team can suggest additional exercises to help you based on the current health of your pelvic floor, your pregnancy, and your health history. Some women may benefit from pelvic floor therapy, which you can discuss with Dr. Morales.
Ready to improve your pelvic floor health? Our team at Kelly Morales OB/GYN can help. Contact our office in San Antonio, Texas, to schedule an appointment.
You Might Also Enjoy...
How to Plan for Your Pregnancy After 40
Over 100,000 American women in their 40s give birth each year. While conceiving and carrying a baby is more challenging after 40, you can have a healthy pregnancy and baby with a little planning. Here’s what you need to know.
4 Signs You're a Candidate for Tubal Ligation
If having a baby isn’t part of your future, you may want a permanent form of birth control.
 Getting your tubes tied (tubal ligation) is a safe and effective way to prevent pregnancies. Here’s a look at the signs it could be right for you.
Getting your tubes tied (tubal ligation) is a safe and effective way to prevent pregnancies. Here’s a look at the signs it could be right for you. Skipping Your Periods? It Could Be a Hormonal Imbalance
Have you noticed a change in your menstrual cycle? Symptoms like skipping a period, or short or long cycles could be a sign of a hormonal imbalance. Here’s what you need to know.
Are Prenatal Vitamins Really Necessary?
As an expecting mom, you want the best for your growing baby. That means giving your baby the minerals and vitamins needed for healthy development. Learn how prenatal vitamins help you do just that.
Tips for a Less Painful Delivery
If you’re preparing for labor and delivery, chances are you’re looking for ways to make the process less painful.
 Keep reading to learn our top tips for making labor and delivery a better experience.
Keep reading to learn our top tips for making labor and delivery a better experience. How To Help Your Teen Manage Endometriosis
Does your teen daughter struggle with the painful symptoms of endometriosis? While there’s no cure for this degenerative condition, therapies exist to make managing it easier. Here’s what you and your teen need to know.
Pelvic floor dysfunction before and after childbirth and preventive strategies in obstetric practice » Doctor's Library
1FGAOU HE Peoples' Friendship University of Russia, Moscow
2CJSC Pentcroft Pharma, Moscow, Russia
Research objective. To determine the frequency of pelvic floor dysfunction (FDD) in women during pregnancy, in the postpartum period and in the long term.
Material and methods. Data from 50 foreign and domestic sources found in international databases on this topic were analyzed.
Results. DTD (urinary incontinence and pelvic organ prolapse) occurs already during pregnancy in 40% of women and persists for 6–8 weeks postpartum in most of them. After 1 year, the frequency of DTD increases by 7-10%, after 10 years - by 25% and reaches 50-77%. The frequency of sexual disorders correlates with the manifestations of DTD, increasing from 20% in the postpartum period to 50–80% in the long term. On the contrary, the frequency of fecal incontinence decreases, but not in women who have suffered grade III-IV perineal tears.
DTD (urinary incontinence and pelvic organ prolapse) occurs already during pregnancy in 40% of women and persists for 6–8 weeks postpartum in most of them. After 1 year, the frequency of DTD increases by 7-10%, after 10 years - by 25% and reaches 50-77%. The frequency of sexual disorders correlates with the manifestations of DTD, increasing from 20% in the postpartum period to 50–80% in the long term. On the contrary, the frequency of fecal incontinence decreases, but not in women who have suffered grade III-IV perineal tears.
Conclusion. The data obtained indicate the need for screening to identify women in need of treatment, starting from the postpartum period.
The term Pelvic Floor Dysfunction (FDD) is an umbrella term for urinary incontinence (UI), pelvic organ prolapse (POP), fecal incontinence and sexual dysfunction [1].
In the population, the prevalence of UI among women is 32-64% [2], POP - 48-77% [2-5], fecal incontinence - 0.5-28% [6-8]. The prevalence of female sexual disorders varies: orgasm disorder occurs with a frequency of 4-24%, insufficient lubrication - 6-21%, decreased libido - 10-46%, dyspareunia - 3-41% [9].
However, most women do not seek medical help [10]. The problem is aggravated by the fact that there are no recommendations in the country for the early detection of DTD and timely conservative treatment, while domestic medicine is focused exclusively on the surgical treatment of already advanced forms of the disease.
Given that the main cause of DTD is pregnancy and childbirth, its manifestations are already present in this period and progress over time [10, 11]. Early detection of DTD and conservative measures can prevent the progression of the process and preserve the quality of life of women for many years [12].
Therefore, let us turn to the literature data indicating the frequency of the disease during pregnancy, in the postpartum period, and also in the long term.
DTD during pregnancy and the postpartum period
An analysis of 28 randomized clinical trials showed that stress UI during pregnancy occurs in 40% (18.6–75%) of women [13–15].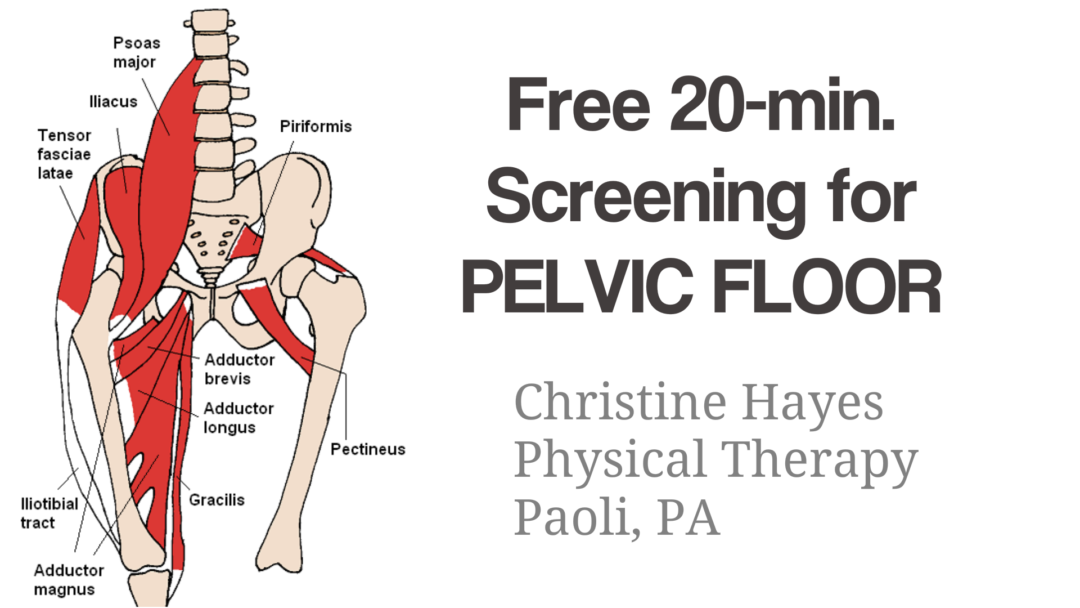 Hormonal changes associated with pregnancy, increasing pressure of the uterus and fetal weight on the pelvic floor muscles lead to a decrease in their strength and supporting function, incompetence of the urethral sphincter. With an increase in the duration of pregnancy, the frequency and severity of UI increase (from 19.2% in the II trimester to 37.9% in III) [16], which reduces the quality of life of pregnant women. The strength of the pelvic floor muscles decreases by 22–35% starting at 20 weeks of gestation and continuing until 6 weeks postpartum [17]. 6–8 weeks after delivery, UI is observed in 14–38% of women [14, 15].
Hormonal changes associated with pregnancy, increasing pressure of the uterus and fetal weight on the pelvic floor muscles lead to a decrease in their strength and supporting function, incompetence of the urethral sphincter. With an increase in the duration of pregnancy, the frequency and severity of UI increase (from 19.2% in the II trimester to 37.9% in III) [16], which reduces the quality of life of pregnant women. The strength of the pelvic floor muscles decreases by 22–35% starting at 20 weeks of gestation and continuing until 6 weeks postpartum [17]. 6–8 weeks after delivery, UI is observed in 14–38% of women [14, 15].
Pregnancy-related UI is an increased risk factor for incontinence in the postpartum period and later in life compared with those who did not have UI during pregnancy [13].
Uterine prolapse during pregnancy, according to A. Ammari et al. [17], is a rare disease that can occur during pregnancy or against the background of pre-pregnancy prolapse with a frequency of 1 in 10 000–15 000. There are descriptions of severe prolapses in pregnant women and their correction using pessaries in the literature [17–19].
There are descriptions of severe prolapses in pregnant women and their correction using pessaries in the literature [17–19].
At the same time, according to Y. Chen et al. stage II POP is present in 36% of pregnant women at 36–38 weeks of gestation [20].
After 6 weeks, 32% of women after vaginal delivery and 35% after caesarean section have prolapse (p=0.805) [1].
When assessing the stage of prolapse 3 months after birth, 39% of women with prolapse in stage I were identified, another 17% - in stage II (56% in total) and none with prolapse of stage III or higher. Stage II is more common in anterior prolapse, stage I - both in the central and other departments [21].
C. Brincat [22] indicates a low incidence of fecal incontinence among pregnant women. However, according to a large cross-sectional study, its prevalence, on the contrary, was high - 40.8% (presence of episodes within 4 weeks before the survey). There were no specific signs during pregnancy that could indicate the risk of fecal incontinence during this period of life - age (p=0. 090), BMI (p=0.094), previous birth (p=0.492), trimester of pregnancy (p= 0.361) and stool features according to the Bristol Scale (p=0.388) did not matter [23, 24].
090), BMI (p=0.094), previous birth (p=0.492), trimester of pregnancy (p= 0.361) and stool features according to the Bristol Scale (p=0.388) did not matter [23, 24].
49.3% of women resume sexual intercourse in the postpartum period [25], while 22.2% have sexual problems, which include pain in the vagina (62.5%), discharge (18.8%), bleeding (15.6%). Injuries of the perineum during childbirth...
Pelvic floor muscle dysfunction | FPA
Author - Natalia Reznik.
Pelvic floor muscle dysfunction is a common problem faced by approximately one fifth of the world's population. It is not life-threatening, but it significantly complicates it. In this case, you need to contact the experts. They provide potential clients information sufficient to independently make a primary diagnosis and take the necessary measures.
How does it work?
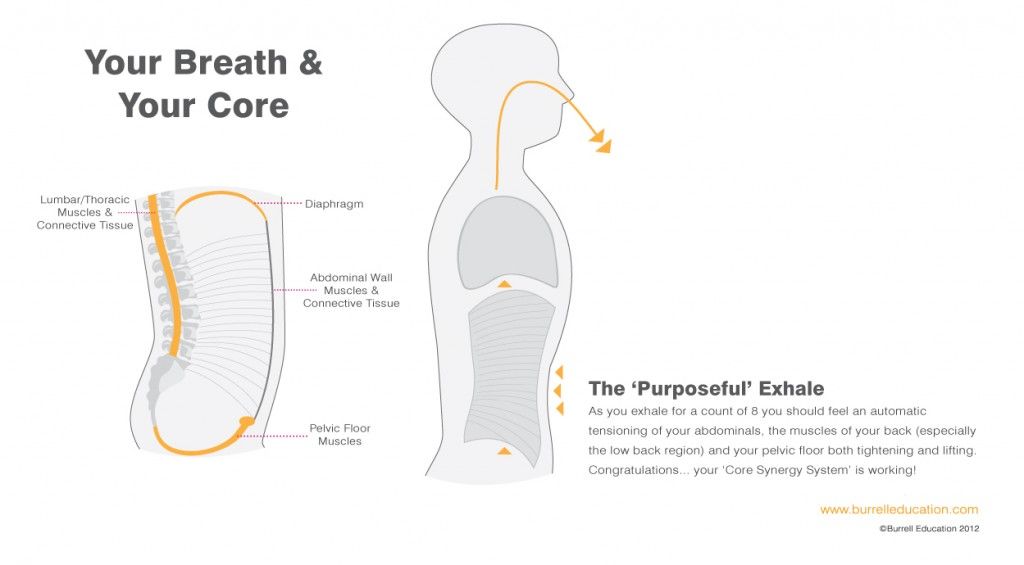
The position of our body is supported by a cylinder-like muscular frame (core).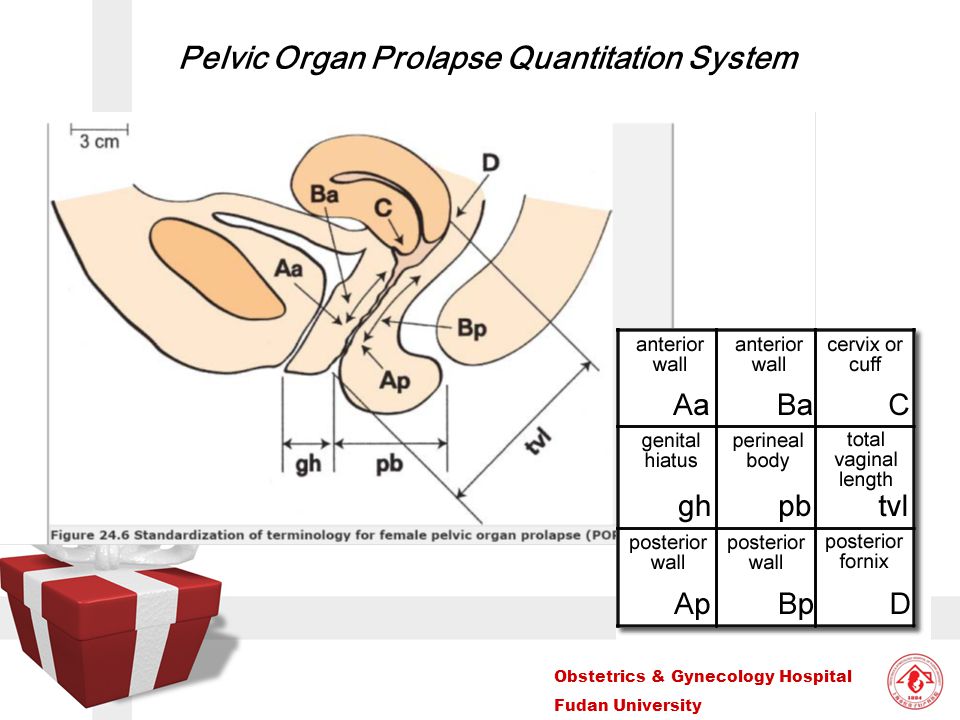 Its walls are made up of transverse, oblique and rectus abdominis muscles, multifidus muscles (deep back muscles) and muscles that straighten the spine. From above, the cylinder is closed by the diaphragm, and from below - by the muscles of the pelvic floor. It is a three-layer muscular plate stretched like a hammock from the pubic bone in front to the coccyx in the back. The thickness of the plate is about 1 cm. If all the pelvic floor muscles contracted separately, they would pull in different directions. However, they work together to support the bladder and intestines, the prostate in men, and the uterus in women, and therefore partly control the functioning of these organs. In addition, the pelvic floor muscles strengthen the rectal sphincter and urethra (Figure 1).
Its walls are made up of transverse, oblique and rectus abdominis muscles, multifidus muscles (deep back muscles) and muscles that straighten the spine. From above, the cylinder is closed by the diaphragm, and from below - by the muscles of the pelvic floor. It is a three-layer muscular plate stretched like a hammock from the pubic bone in front to the coccyx in the back. The thickness of the plate is about 1 cm. If all the pelvic floor muscles contracted separately, they would pull in different directions. However, they work together to support the bladder and intestines, the prostate in men, and the uterus in women, and therefore partly control the functioning of these organs. In addition, the pelvic floor muscles strengthen the rectal sphincter and urethra (Figure 1).
The contractions of the pelvic floor muscles can be controlled by volition, but usually they contract unconsciously, coordinated with the work of the deep muscles of the abdomen and back and the diaphragm, and help control abdominal pressure during exercise. In an ideal situation, intra-abdominal pressure is automatically regulated. For example, when lifting weights, the core muscles work in ensemble: the pelvic floor muscles rise, the abdominal and back muscles retract to support the spine, and breathing is not difficult. If any of the core muscles, including the pelvic floor muscles, are weakened or damaged, automatic coordination is disrupted. Then, in situations that increase intra-abdominal pressure, there is a possibility of overloading the pelvic floor, it weakens and the pressure decreases. If this happens repeatedly, the stress on the pelvic organs increases over time, which can lead to loss of bladder or bowel control, or pelvic organ prolapse.
In an ideal situation, intra-abdominal pressure is automatically regulated. For example, when lifting weights, the core muscles work in ensemble: the pelvic floor muscles rise, the abdominal and back muscles retract to support the spine, and breathing is not difficult. If any of the core muscles, including the pelvic floor muscles, are weakened or damaged, automatic coordination is disrupted. Then, in situations that increase intra-abdominal pressure, there is a possibility of overloading the pelvic floor, it weakens and the pressure decreases. If this happens repeatedly, the stress on the pelvic organs increases over time, which can lead to loss of bladder or bowel control, or pelvic organ prolapse.
To work as part of the core, the pelvic floor muscles must be flexible, that is, able to not only contract and hold tension, but also to relax. Constant tension can cause muscles to lose flexibility and become very stiff, and stiffness of the pelvic floor muscles usually accompanies weakness, which can lead to urinary incontinence, pelvic pain, pain during intercourse, and difficulty urinating.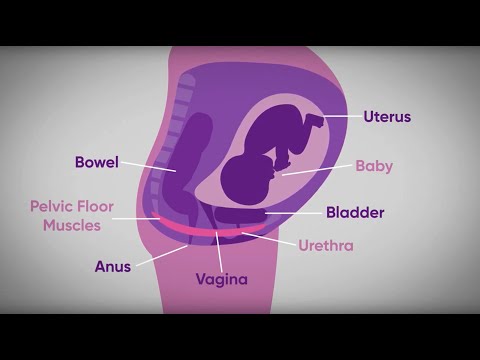
Symptoms of pelvic floor muscle dysfunction
-
Uncontrolled leakage of urine during exercise, laughing, coughing or sneezing (stress incontinence).
-
The need to go to the toilet frequently or urgently (urge incontinence).
-
Incontinence of gas and intestinal contents.
-
Difficulty emptying the bladder or bowels.
-
Prolapse of internal organs. In women, it is felt as a bulge in the vagina or a feeling of discomfort or heaviness. In men, there is a bulge in the rectum or a desire to empty the bladder, although there is no objective need for this.
-
Pain in the bladder, bowel, or back near the pelvic floor when doing pelvic floor exercises or during intercourse.
Experts emphasize that the above problems are not necessarily associated with weakness of the pelvic floor muscles, so their cause should definitely be found out. Diagnosis is by electromyography, ultrasound, or MRI.
Diagnosis is by electromyography, ultrasound, or MRI.
Who is at risk?
Dysfunction of the pelvic floor muscles occurs when they are stretched, weakened, or too tight. Some people have weak pelvic floor muscles since childhood, but more often problems develop with age. The risk group is
-
pregnant women and women who have already given birth,
-
women who are going through or have gone through menopause,
-
women who have undergone gynecological surgery, such as removal of the uterus,
-
men who had their prostate removed
-
high-class athletes such as gymnasts, runners or trampoline jumpers.
Additional risk factors include:
-
back pain,
-
pelvic trauma or radiation therapy,
-
constant constipation (you have to strain to empty your bowels),
-
chronic coughing or sneezing (asthma, smoking or hay fever),
-
being overweight or obese,
-
regularly lifting weights at work or in the gym.
Let's analyze these cases in more detail.
Pregnancy and childbirth affect the physical fitness of the pelvic floor muscles. The growing fetus puts pressure on the pelvic floor muscles. During pregnancy, the hormone relaxin is released, which makes tissues more elastic, allowing the muscles and ligaments of the pelvic floor to stretch during childbirth. Sometimes they remain stretched for a long time. The action of relaxin and fetal pressure prevents the muscles from holding the pelvic organs in the correct position.
Women at greatest risk during pregnancy and childbirth are those who:
-
gave birth multiple times
-
gave birth with the help of instruments: forceps or a vacuum extractor,
-
the second stage of labor lasted more than an hour,
-
during childbirth, there was a rupture of the perineum,
-
the baby weighed more than 4 kg.
During menopause the female body undergoes significant changes. All muscles weaken, including the muscles of the pelvic floor. Because they support the pelvic organs, problems can arise in this area, such as difficulty with bladder or bowel control.
Menopause is often accompanied by weight gain, which also weakens the pelvic floor muscles.
The situation is also exacerbated by:
-
less elastic bladder
-
anal trauma due to childbirth,
-
chronic diseases (diabetes or asthma).
Gynecological or pelvic surgery such as hysterectomy or radiation therapy may deform the pelvic floor muscles and cause incontinence.
Incontinence is also common after prostate surgery . Most men regain full bladder control within 6 to 12 months, and exercise makes a big difference.
Professional athletes and just great fitness enthusiasts often experience constant strong pressure on the pelvic floor.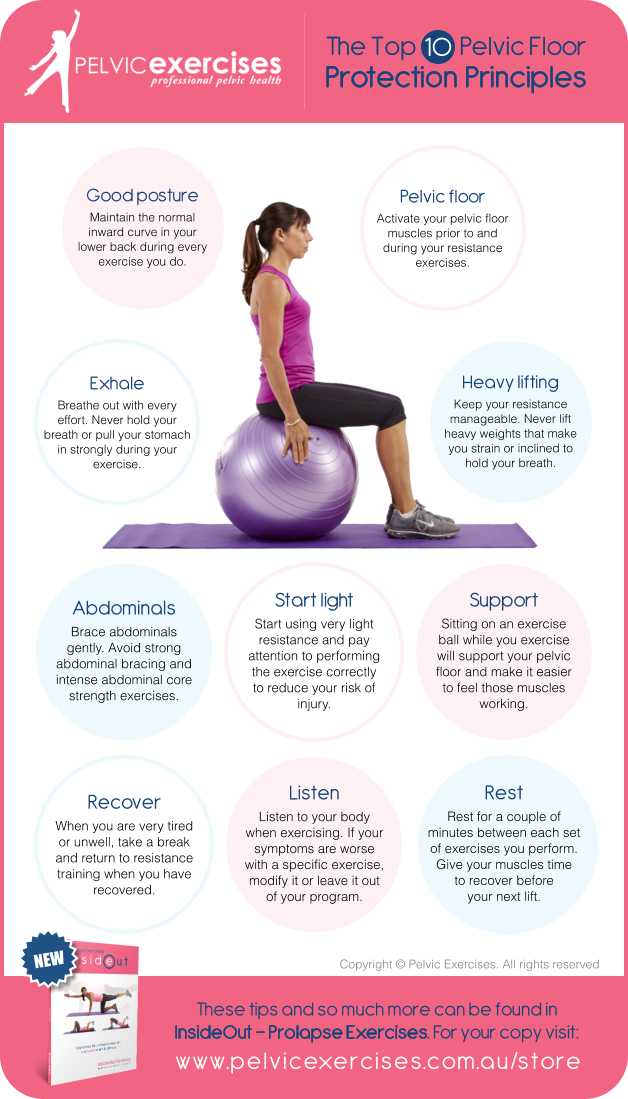 As a rule, these are gymnasts, trampoline jumpers and runners, fans of games in which you often have to “knock” on the ground, such as basketball or netball. Athletes who lift weights or do high-intensity interval training also fall into the risk group.
As a rule, these are gymnasts, trampoline jumpers and runners, fans of games in which you often have to “knock” on the ground, such as basketball or netball. Athletes who lift weights or do high-intensity interval training also fall into the risk group.
Urinary incontinence may be common during these exercises, but it is not normal.
What to do?
Pelvic floor muscle dysfunction treat. There are surgical methods, but we will not discuss them. There is electrical stimulation, in which an electrode is placed on the vagina or rectum. However, the ability of electrical stimulation to increase skeletal muscle strength is questionable, and side effects are common with this procedure. In most cases, patients complain of soreness, local irritation, pain and psychological discomfort.
Drug therapy does not strengthen the muscles, but it can reduce pressure in the urethra at rest by increasing the tone of its smooth or striated muscles. Usually alpha-adrenergic agonists are used: ephedrine, norepinephrine or phenylpropanolamine; imipramine, clebuterol, duloxetine, estrogen. Clinical studies confirming the effect of these drugs are few.
Clinical studies confirming the effect of these drugs are few.
The urethra is sensitive to the action of estrogen, data on its effectiveness are conflicting, and the use is fraught with side effects, such as an increased risk of coronary heart disease and cancer.
For incontinence, experts recommend bladder training - scheduled urination. Their essence is that the patient urinates according to an individual plan, at certain intervals, and restrains untimely urges by reducing the sphincter. Gradually, the intervals between urination increase. It is believed that such restraint will increase the activity of the pelvic floor muscles. This method has been practiced since the 1960s, mainly for urge incontinence, but its effectiveness is questionable.
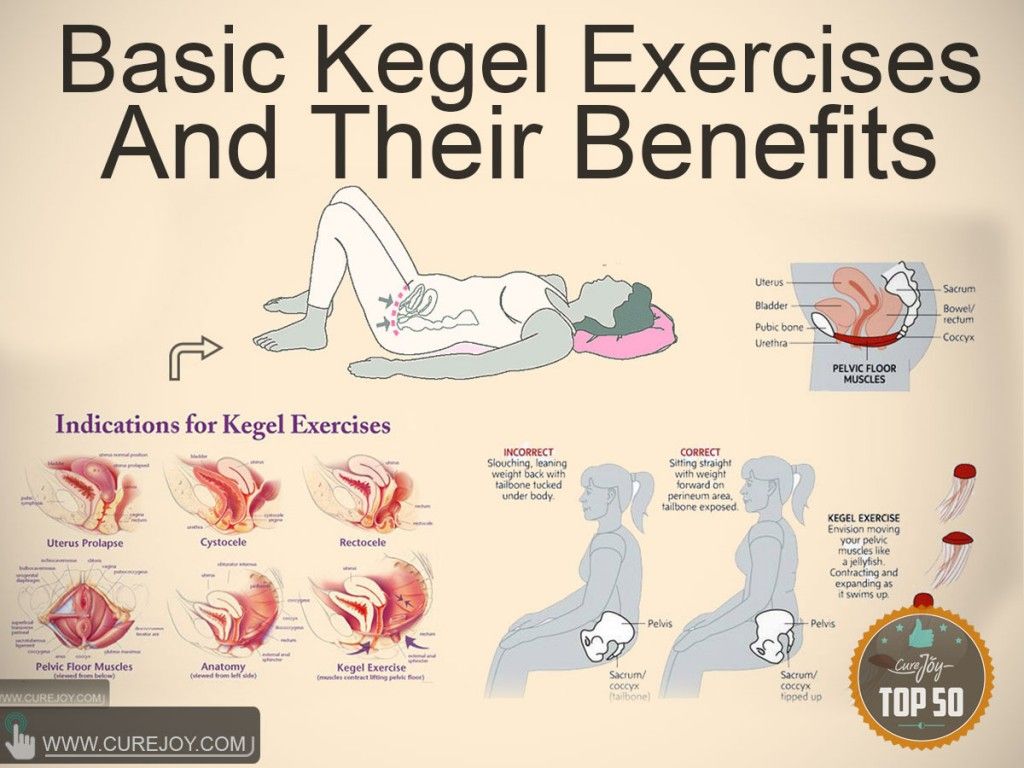
The method of first choice is exercises to strengthen the pelvic floor muscles.
How to train the pelvic floor muscles?
If the muscles are weak, they need to be strengthened. Muscles compress with an effort of will and try to keep it in this position for some time.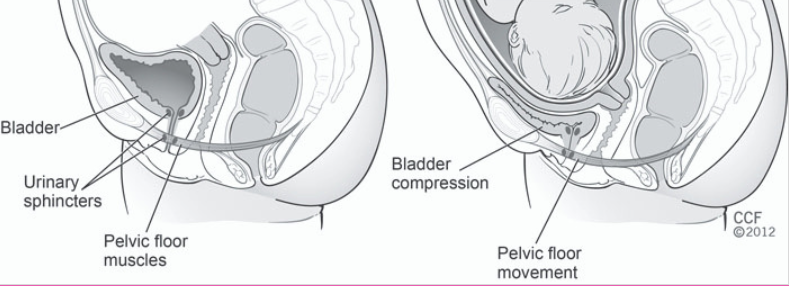 The purpose of the exercises is to increase the tone and cross-sectional area of the pelvic floor muscles and the stiffness of the connective tissue and thus raise the pelvic floor. Exercises were first proposed in 1948 by the American gynecologist Arnold Kegel. By According to some reports, they are quite effective, and patients who perform them very rarely feel pain or discomfort. The frequency, intensity, and duration of exercise can vary, and there is no standard protocol.
The purpose of the exercises is to increase the tone and cross-sectional area of the pelvic floor muscles and the stiffness of the connective tissue and thus raise the pelvic floor. Exercises were first proposed in 1948 by the American gynecologist Arnold Kegel. By According to some reports, they are quite effective, and patients who perform them very rarely feel pain or discomfort. The frequency, intensity, and duration of exercise can vary, and there is no standard protocol.
The key to success is to train exactly the muscles that you need. You cannot see them, but you can feel them. There are several ways to do this.
Feel the muscles - stop the flow
You need to try to stop or slow down the flow of urine in the toilet. This is not an exercise, but just a way to feel the muscles of the pelvic floor, to determine which muscles control the bladder.
Feel the muscles: visualization for women
Another method is to mentally stop urination and keep it in the body at the same time. This can be done lying down, sitting or standing with your feet shoulder-width apart.
This can be done lying down, sitting or standing with your feet shoulder-width apart.
-
Relax the muscles of the thighs, bottom and abdomen.
-
Squeeze the muscles around the anus as if trying to stop the flow of urine.
-
Contract the muscles around the vagina and pull it up into the pelvis.
-
Squeeze the muscles around the anus, as if trying to hold back gases.
-
The muscles around the anterior and anus should contract and retract into the pelvis.
-
Feel the muscles that contract during this complex, then relax them.
Feel the muscles: visualization for men
Men are invited to stand in front of a mirror without clothes and tighten the muscles of the pelvic floor. If done correctly, they will see the base of the penis retract and the scrotum rise. The anus will also retract, but that is not the purpose of the exercise. After relaxing the muscles, you should feel that you have let go.
After relaxing the muscles, you should feel that you have let go.
Contracting muscles correctly
During exercise, only the muscles of the pelvic floor should work. The lower part of the abdominal wall will stretch and flatten, this is not a problem, since this part of the abdomen works together with the muscles of the pelvic floor. The muscles above the navel should be completely relaxed, including the diaphragm.
Try to gently tighten only the pelvic floor muscles so that they rise and contract while breathing freely. See if you can do it. After muscle contraction, it is important to relax. This will allow them to recover and prepare for the next cut.
Often people from zeal also strain the external muscles, as a rule, the muscles of the abdomen, buttocks and adductors of the thigh. However, the joint contraction of these muscles along with the muscles of the pelvic floor does not support the internal organs. Only the internal muscles need to be strained.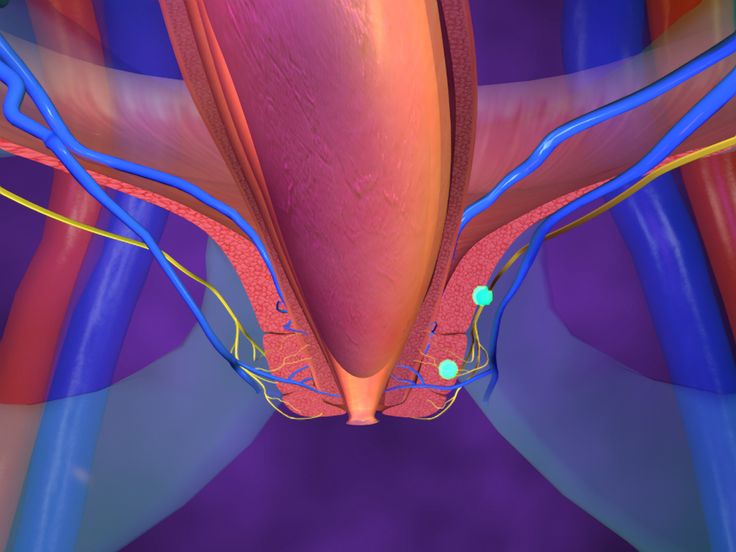 Improper exercise can be harmful (Fig. 2).
Improper exercise can be harmful (Fig. 2).
If you don't feel your pelvic muscles contract, change position and try again. For example, if you are sitting, try lying down or standing up. If this does not help, contact the experts. Studies show that more than 30% of women cannot properly contract the muscles even after they are explained in detail how to do it.
Training mode
Having learned how to properly contract the muscles of the pelvic floor, you can start training. Try to hold the muscles tight for up to 10 seconds before relaxing. Don't forget to breathe while doing this. Repeat the exercise up to 10 times, but only as long as you can perform it correctly. Exercises can be repeated several times during the day. They can be done lying down, sitting or standing with legs apart, but the muscles of the thighs, buttocks and abdomen should be relaxed.
Typically, to achieve long-term effect of the exercise should be performed for at least 6-8 weeks, and preferably 6 months. On their own, they may be not particularly efficient. good Complementing this daily independent activity is a weekly instructor-led session. Exercises are performed standing, sitting, lying or kneeling. The muscles of the pelvic floor contract as much as possible and hold in this position for 6 to 8 seconds. After each long contraction, 3-4 quick ones are made. In each pose, 8-12 long contractions and a corresponding number of fast ones are performed. In this case, all contractions must be performed with the same intensity.
On their own, they may be not particularly efficient. good Complementing this daily independent activity is a weekly instructor-led session. Exercises are performed standing, sitting, lying or kneeling. The muscles of the pelvic floor contract as much as possible and hold in this position for 6 to 8 seconds. After each long contraction, 3-4 quick ones are made. In each pose, 8-12 long contractions and a corresponding number of fast ones are performed. In this case, all contractions must be performed with the same intensity.
Sometimes people forget to do pelvic floor exercises, so it's best to associate them with some regular activity like eating or brushing your teeth. This is a great way to build exercise into a familiar set of routine tasks.
Women who have recently given birth are advised to reduce the load on the pelvic floor muscles in the first few months to allow them to recover.
Men who have had prostate surgery should start exercising as soon as their urinary catheter is removed (during exercise, it can irritate the bladder and cause discomfort).
Pelvic floor exercises and other physical activities
No matter how strong and strong a person is, if his pelvic floor function is impaired, it is necessary to restore it. Regular sports activities do not need to be abandoned, however, for all types of training - cardio, endurance training or strength training - the number of repetitions, sets and frequency of training should depend on the reaction of the pelvic floor. If necessary, you need to reduce the intensity, impact, load, number of repetitions or duration of the workout, and then, as the functions of the pelvic floor improve, gradually return to the previous regimen.
It is better to coordinate the training program with specialists, because people are different, and what suits one may not be suitable for another. But there are some general rules:
-
Avoid high-impact or high-intensity exercise that reduces pressure on the pelvic floor.
-
Don't lift heavy things unless absolutely necessary.
-
Tighten your pelvic floor muscles before lifting weights.
There are two ways to assess pelvic floor loading. It is great if during the exercise there is a feeling of heaviness or urine leaks, and if, while doing the exercise, you cannot tighten the muscles of the pelvic floor.
Constantly thinking about the pelvic floor muscles during an hour-long workout is unrealistic, but it is useful to pay attention to them regularly. If you can't pull in and compress your muscles while doing a squat, bicep curl, or mountain biking, cut back on your workout or opt for something lighter. If your pelvic floor is not ready for running, you can take a walk in the hills. If five squats are exhausting, do three. Over time, you will progress.
How to avoid pelvic floor dysfunction?
Alas, no one knows for sure. Theoretically, you need to strengthen the muscles of the pelvic floor with the help of special exercises.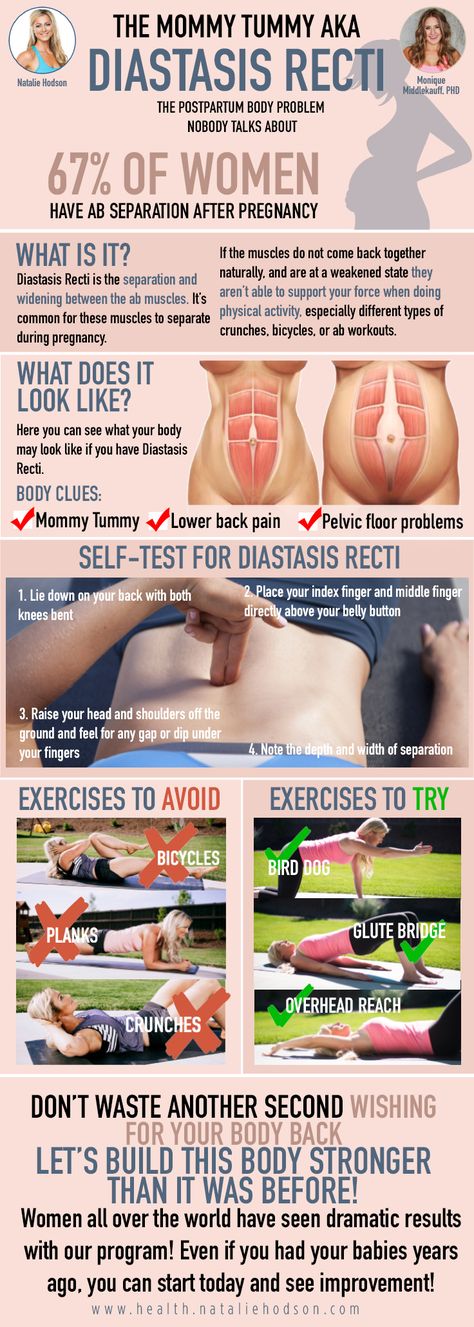 Athletes recommend including these exercises in your regular workouts: 3 sets of 8-12 maximum compressions, 3-4 times a week. Unfortunately, there is no certainty that athletes perform these exercises more correctly than ordinary people.
Athletes recommend including these exercises in your regular workouts: 3 sets of 8-12 maximum compressions, 3-4 times a week. Unfortunately, there is no certainty that athletes perform these exercises more correctly than ordinary people.
Conclusion
-
With dysfunction of the pelvic floor muscles, their training should be part of everyday life. Three times a day, do as many exercises (simply by pulling the muscles in or holding them in this position) as you can do well. Gradually increase the number of repetitions, but do not chase the number.
-
While doing other exercises, constantly listen to the state of the pelvic floor. Replace any exercise with an easier option if it causes a feeling of tension, heaviness, or vulnerability in the pelvic floor.
-
Before lifting heavy weights or intense exercise, strengthen your pelvic floor and deep abdominal muscles and frequently check how your pelvic floor muscles work during exercise.