2 month old eye discharge
Is it normal and how to treat it?
Eye discharge is common in newborns and typically occurs due to a blocked tear duct. However, parents and caregivers can often treat this at home.
Eye discharge is typically harmless and self-resolving. However, discharge that occurs alongside other symptoms in the eye area, such as swelling or tenderness, could indicate an infection or another eye problem. A parent or caregiver of a newborn with these symptoms will need to consult a doctor.
This article discusses how common eye discharge is and explains how to treat it at home. We also cover medical treatment, other causes, complications, and when to contact a doctor.
Eye discharge in newborns is common and rarely a cause for concern. A common cause of eye discharge is a blocked tear duct.
According to the American Academy of Ophthalmology, almost 20% of newborns have a blocked tear duct. This condition can occur because the end of the tear duct does not open properly when the baby is born.
Tears form in the lacrimal gland, which sits just above the eye. Tear fluid helps clean and lubricate the surface of the eye. When a person blinks, the eyelids sweep the tear fluid into these ducts, which drain it into the nose.
If something blocks a tear duct, fluid may no longer be able to drain away from the eye’s surface. Blockages can cause very watery eyes, and sticky discharge may form in the corners.
Learn more about blocked tear ducts.
Blocked tear ducts are a common cause of eye discharge in infants. However, other conditions and factors can also cause discharge.
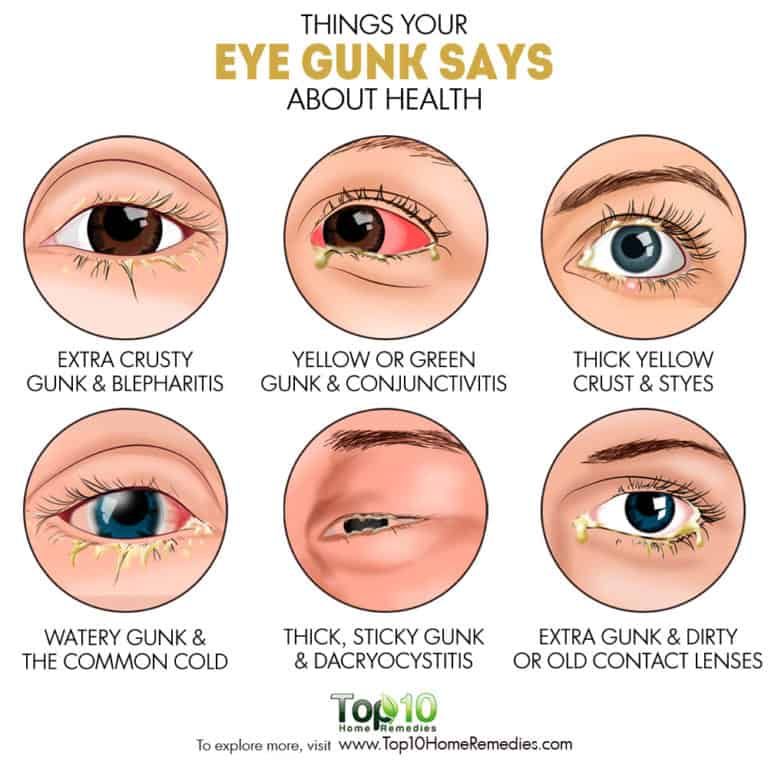
Conjunctivitis
Eye discharge in newborns can also be a sign of conjunctivitis or pinkeye. Conjunctivitis is an inflammation of the conjunctiva, a thin membrane that protects the front of the eye. Unlike a blocked tear duct, conjunctivitis often causes the white part of the eye to appear red.
Symptoms of conjunctivitis in newborns can include:
- drainage or discharge that develops between 5 and 12 days after birth
- puffy or tender eyelids, often with skin discoloration
- red, irritated eyes
Conjunctivitis in newborns can sometimes occur alongside a blocked tear duct. However, a pregnant person can also pass on a bacterial or viral infection to their baby when giving birth, leading to conjunctivitis.
However, a pregnant person can also pass on a bacterial or viral infection to their baby when giving birth, leading to conjunctivitis.
Learn more about the symptoms of eye infections.
Chemical irritation
Chemical irritation can also cause conjunctivitis in newborns. Healthcare professionals often give antibacterial eye drops to newborns to prevent infections. These eye drops can sometimes cause irritation that can result in conjunctivitis symptoms.
Learn more about eye irritation.
If the eye discharge is due to a blocked tear duct, it will usually resolve without treatment within 4–6 months.
However, wind, cold weather, and strong sunlight can also worsen symptoms, so a parent or caregiver should aim to protect a newborn’s eyes from these elements.
Clearing discharge
A parent or caregiver can often treat a newborn with a blocked tear duct at home. Before touching the area close to the child’s eyes, it is essential to wash the hands with soap and warm water to prevent infections. A person should also take care to rinse the hands thoroughly after cleaning them to avoid getting soap in the baby’s eye.
A person should also take care to rinse the hands thoroughly after cleaning them to avoid getting soap in the baby’s eye.
To clear away discharge, dip a clean piece of gauze or soft cloth in some lukewarm water, then gently wipe the corner of the eye. If a blocked tear duct affects both eyes, always use a new area of the cloth or gauze to clean the other eye.
Tearduct massage
A doctor may also recommend gently massaging the blocked tear duct to help it open, and they will demonstrate how to do this safely.
To massage the tear duct:
- Lightly press the tip of the index finger against the inside bridge of the newborn’s nose, on the side of the blocked tear duct.
- Make 2 or 3 short downward strokes with the finger along the side of the nose. These should be gentle but firm.
- Perform the massage twice a day — once in the morning and once in the evening.
If the side of the newborn’s nose becomes red or swollen, stop the massage immediately and contact a doctor.
In newborns, blocked tear ducts tend to open up within several months of birth. However, medical intervention may be necessary in some cases.
Surgery
If the blockage has not gone away by the baby is 1 year of age, a doctor may recommend a medical treatment called a nasolacrimal duct probing.
This procedure involves inserting a small probe into the infant’s tear duct. By using probes that gradually increase in size, a doctor will be able to open up the tear duct. They will then use a saline solution to flush out any remaining debris.
Sometimes, the doctor may also insert a small tube, or stent, into the duct to keep it open.
Probing is usually successful in opening the tear duct. For children with a severe blockage, a doctor may recommend a more complicated surgical procedure called a dacryocystorhinostomy to clear out and open the tear duct.
Antibiotics
If an infection is causing eye discharge, the newborn will need prompt medical attention. To treat cases of infectious discharge, a doctor may prescribe topical, oral, or intravenous antibiotics.
To treat cases of infectious discharge, a doctor may prescribe topical, oral, or intravenous antibiotics.
Blocked tear ducts can sometimes lead to an infection called dacryocystitis. Symptoms of this condition may include:
- excessive thick discharge from the eye
- redness in the corner of the eye
- a tender bump or swelling at the side of the nose
- fever
If a newborn has any of these symptoms, a parent or caregiver should consult a doctor.
Newborns with eye discharge or very watery eyes should speak with a pediatrician or an eye doctor specializing in children, called a pediatric ophthalmologist. These healthcare professionals can diagnose the cause of the discharge and check for signs of infection.
Parents or caregivers should seek medical attention if an infant’s eye discharge persists for more than 6 months.
Newborns with signs of an eye infection require immediate medical attention. Signs of an eye infection can include:
- sore or puffy eyes
- swollen eyelids
- yellow or green pus or discharge
- a bump or swelling on the inside corner of the eye
If a parent or caregiver notices any of these symptoms, they should contact a doctor immediately.
Eye discharge in newborns is common and often results from a blocked tear duct. The blockage will usually clear up by itself within 4 to 6 months.
However, newborns with eye redness, eye discharge, or excessive watering of the eyes should speak with a doctor to diagnose the cause and rule out an eye infection.
Parents and caregivers can treat a baby with a blocked tear duct at home by wiping away any discharge and gently massaging the area twice a day. A doctor can demonstrate how to do this.
Discoloration, swelling, or soreness in the eye can indicate an eye infection. Speak with a doctor immediately if an infant has these signs.
Is My Baby’s Eye Discharge Normal?
Written by Nicole Blades
In this Article
- What’s Normal?
- When It’s Conjunctivitis
- When Treatment Is Needed
As the parent of a newborn, nothing beats staring lovingly into your sweet little bundle’s eyes. (Well, watching your baby sleeping soundly comes pretty close!) But what if when you look into your child’s eyes, you see that they have goopy, sticky discharge? Is it something to be concerned about?
What’s Normal?
First of all, take a breath, because sticky eye discharge in newborns is very common. If the white part of your baby’s eye -- the sclera -- is clear and there is no redness, but there is discharge, it’s most likely a blocked tear duct.
If the white part of your baby’s eye -- the sclera -- is clear and there is no redness, but there is discharge, it’s most likely a blocked tear duct.
About 1 in 5 babies are born with tear ducts that haven’t fully developed. The blockage is usually in one eye but can be in both. It often clears up on its own. A warm compress can help, but if it lasts a long time, it might need surgery.
When It’s Conjunctivitis
Since a newborn hasn’t been around that long -- under 2 months -- it’s not common for them to get a lot of viral infections. But sometimes their clogged tear duct can lead to an infection such as conjunctivitis.
This happens when there is inflammation of the thin layer of tissue (conjunctiva) that covers the sclera. Symptoms are similar to the sticky, watery eyes that come with a blocked tear duct. But with conjunctivitis, there is more swelling, tenderness, and redness of the eye area, and the whites of the eye will be pink or red. Your baby’s eyelid might be red, sticky, and itchy, and the discharge takes on a yellowish color. Also, their eyes might be more watery than usual. The infection often starts in one eye and spreads to the other.
Also, their eyes might be more watery than usual. The infection often starts in one eye and spreads to the other.
Chemical conjunctivitis can happen when eye drops and ointments, typically used on newborns at birth to help prevent infection, actually cause the irritation. It can show up as mildly red eyes and some puffiness in the eyelids.
It’s rare, but red, angry, itchy eyes with swollen eyelids and discharging pus could mean ophthalmia neonatorum (ON).This is a bacterial infection that can happen during childbirth if the baby passes through a birth canal infected with chlamydia. The symptoms usually show up 5-12 days after birth. Among newborns with ON, half also have the infection other areas of their bodies.
Call the doctor if the baby has a fever and:
- Your baby cannot open their eyes or you cannot see the eye
- The area is tender to touch and the skin around the eye is red
- There is a lot of eye discharge
These may be signs of a bacterial infection of the sclera.
When Treatment Is Needed
Doctors usually recommend a wait-and-see approach, as this issue often clears up on its own. You can also apply a warm compress to the bothered eye.
If the tear duct is still blocked and the eye discharge continues up to the baby’s first birthday, you should see your child’s doctor. They may refer you to a pediatric eye specialist, as it may need surgery.
To treat conjunctivitis caused by the blocked tear duct, try a gentle warm massage with your clean hand between your baby’s eye and nasal area. For chemical conjunctivitis, the symptoms usually only last for 1-3 days after birth, so no treatment is needed. And if it’s ON, doctors usually treat that with oral antibiotics.
Why eye discharge appears and what to do about it
You can listen to the short version of the article. If it's more convenient for you, turn on the podcast.
When to see a doctor
Schedule a visit to a general practitioner or see an optometrist if:
- there is a lot of discharge from the eyes and they have a pronounced greenish-yellow or white color;
- you have washed away everything superfluous, but the discharge appears again and again - and there are so many of them that it can be difficult for you to open your eyes;
- vision has become blurred;
- you become sensitive to light: it hurts to look at it;
- an eye that has discharge, is very red or swollen;
- you feel pain in your eyes.

Any of these signs can be a symptom of a serious infection.
Why eye discharge occurs and what to do about it
Eye discharge can also have more harmless causes.
1. This is normal eye mucus
The best-known secretions are ordinary mucus produced by the conjunctiva. Together with it, in the corners of the eyes, and sometimes along the eyelash growth line, fat, dead skin cells and dust can accumulate and solidify. This cocktail is constantly formed on the surface of the eyes, but during the day, when we actively blink, tear fluid washes it away without a trace. At night, tears are produced less and we blink much less frequently.
What to do
Sleepy mucus looks unpleasant, but it is completely harmless and can be easily removed by simply washing with warm water.
2. Reaction to contact lenses
For some people, contact lenses - even when worn exactly as directed - can cause irritation or inflammation of the eyes. The risk is increased if you forget to remove your lenses before bed.
The risk is increased if you forget to remove your lenses before bed.
What to do
Do not go to bed with contact lenses on. If for some reason this is not possible, ask the optometrist to choose a gas-permeable option suitable for night wear. Another option is to try disposable contact lenses.
If you are using your lenses exactly as instructed, and there is more discharge from your eyes, also contact your optometrist as soon as possible. This is to rule out an eye infection or other disease.
2. Chronic dry eyes
There are many reasons why the mucous membrane of the eyes can dry out. For example, this happens if you do not tear yourself away from gadgets for a long time or are in a room with low air humidity.
Be that as it may, dryness leads to the fact that the lacrimal fluid becomes small and does not have time to wash out the accumulated dust, fat, dead skin cells from the eyes. Therefore, the number of allocations increases.
What to do
Pay attention to symptoms.![]() When the mucosa dries out, they are obvious: fatigue, burning, the appearance of broken capillaries, blurred vision, a regular feeling that something has got into the eye. If there are such signs, consult with an ophthalmologist how you can restore healthy moisture to your eyes.
When the mucosa dries out, they are obvious: fatigue, burning, the appearance of broken capillaries, blurred vision, a regular feeling that something has got into the eye. If there are such signs, consult with an ophthalmologist how you can restore healthy moisture to your eyes.
Your doctor will most likely advise you to use over-the-counter artificial tear eye drops as a first aid. But other appointments may be required.
3. Injury or damage to the eye
Any foreign substance, from the occasional sharp speck of dust to cosmetics and perfumes, if it gets into the eyes, can damage their mucous membrane. Lachrymation and copious discharge is one of the most striking signs that the eye is injured.
What to do
If the damage does not look significant (say, you accidentally splashed deodorant on your face), try rinsing the eye with clear, warm water.
However, if you notice bleeding or pus after an injury, contact your optometrist immediately.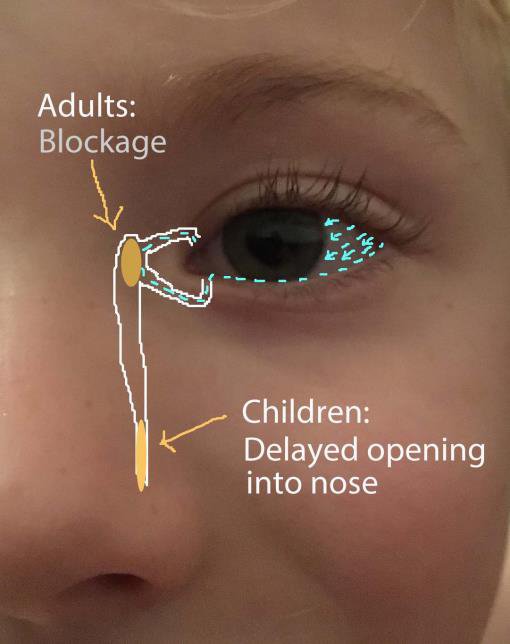
4. Allergic conjunctivitis
This is the name given to the reaction of the conjunctiva to allergen substances — plant pollen, pet dander, house dust. You can recognize allergic conjunctivitis by watery, reddened, swollen and itchy eyes. Sometimes discharges are added to these signs.
What to do
Allergic conjunctivitis is treated in the same way as allergic reactions in general, by taking antihistamines. For the eyes, such funds are available in the form of drops. Ideally, if a doctor helps you choose them.
5. Conjunctivitis
The conjunctiva becomes inflamed not only because of allergies. The cause of redness, itching, cramps, pain and other manifestations of conjunctivitis can be viral and bacterial infections, as well as irritants that have entered the eye.
What to do
Be sure to consult an ophthalmologist. Left untreated, the infection can spread and cause more serious eye damage. The doctor will make an accurate diagnosis and prescribe the necessary medications. For example, prescription eye drops.
For example, prescription eye drops.
6. Blepharitis
This is the term for inflammation of the margins of the eyelids. Blepharitis causes swelling, pain, peeling around the roots of the eyelashes, and increased secretion of sebum around the follicles.
Sometimes the discharge is so profuse that the eyelashes stick together and the person cannot open his eyes.
What to do
Soak a cotton pad or gauze in warm clean water and apply to the eye for 10 minutes. Then, using a disc, gently massage the secretions.
If blepharitis persists, and even more so if additional symptoms occur, such as pain in the eyes and watery eyes, consult an ophthalmologist. The doctor will select the most suitable treatment for you. May recommend antibiotic creams or drops.
7. Keratitis
Keratitis is an inflammation of the cornea. It can be caused by various reasons: a bacterial or herpes infection, a fungus, an amoeba, or, for example, an ultraviolet burn if you forgot to put on your sunglasses on a hot and clear summer afternoon.
Symptoms of keratitis are similar to signs of conjunctivitis or mechanical damage: the eye turns red, watery, sore, vision may be reduced.
What to do
If left untreated, keratitis can lead to corneal scarring and temporary or even permanent loss of vision. Therefore, contact an ophthalmologist as soon as possible.
The doctor will clarify the diagnosis and prescribe treatment. In mild cases, if keratitis is not caused by an infection, you can get by with drops like “artificial tear”. In the case of infectious inflammation, you will need antiviral, antifungal agents or antibiotics, depending on the cause of the infection.
8. Trachoma
Trachoma is a bacterial eye infection caused by a specific bacterium: Chlamydia trachomatis. In the early stages, trachoma resembles the symptoms of conjunctivitis: the eyes swell, itch, and discharge may appear on them.
As the disease progresses, pain and blurred vision appear. Scars form inside the eyelid, and this leads to the fact that the eyelashes seem to be wrapped inside the eye. This condition is called trichiasis and is one of the most characteristic signs of trachoma.
This condition is called trichiasis and is one of the most characteristic signs of trachoma.
What to do
Trachoma is the leading cause of infectious blindness in the world. Therefore, at the slightest suspicion of an infection, you should contact an ophthalmologist as soon as possible.
9. Styes
Styes is an inflammation that can appear on the outer or inner side of the eyelid. In the first case, it is caused by infection of the eyelash follicle (the sac from which it grows). In the second - a blockage of the meibomian gland, which is located on the inside of the eyelid and secretes a secret that protects the mucous membrane from drying out.
A stye usually looks like a hard, round pimple at the edge of the eyelid. The eye may become red, sore and increase the amount of discharge.
What to do
Most often, stye goes away on its own in 7-10 days. Compresses can be used to speed up and facilitate its maturation and removal. Soak a cotton pad or piece of gauze in warm water and place on the affected eye. Change the compress to a new warm one as it cools down.
Change the compress to a new warm one as it cools down.
Be sure to consult a general practitioner or ophthalmologist if, after a week and a half, the barley does not disappear and does not decrease in size. In this case, you may be prescribed antibiotics: in the form of eye drops or a special cream. The doctor may also make a tiny incision in the barley to drain the pus. In no case do not try to do this operation yourself: this often leads to the fact that the infection spreads to the entire eye.
10. Dacryocystitis
Dacryocystitis is a condition where a blocked lacrimal sac becomes infected and inflamed. The result usually looks like a swollen, reddened bump under the lower eyelid on the inside of the eye.
Lachrymation, eye pain, sticky discharge, blurred vision are all associated symptoms of dacryocystitis.
What to do
Often things go away on their own. To speed up and facilitate this process, you can apply a warm compress to the inflammation for 10-15 minutes. For example, gauze soaked in warm water.
For example, gauze soaked in warm water.
However, dacryocystitis can have dangerous complications, up to the spread of infection to the brain. Therefore, it is best to contact an optometrist as soon as possible.
The doctor will examine the eye, ask you about your symptoms, clarify the diagnosis and prescribe the appropriate treatment. These are usually antibiotics in the form of ointments or tablets, as well as over-the-counter pain relievers that help reduce discomfort.
11. Corneal ulcer
A corneal ulcer is an infection that causes an open sore on the cornea. Associated symptoms: pain, tearing, sensitivity to light, difficulty opening the eye, profuse sticky discharge.
What to do
Contact an ophthalmologist as soon as possible. The cornea must be treated, otherwise the ulcers may spread over its entire surface or penetrate deeper. Usually treated with antibiotics.
12. Endofalmitis
Endofalmitis is an infection of the tissues or fluids inside the eyeball.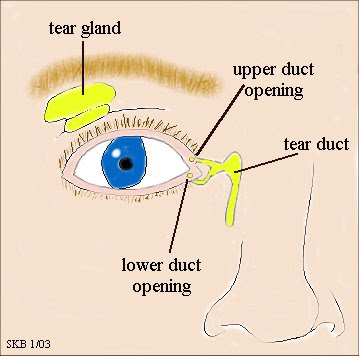
Bacteria or fungi are most commonly introduced into the eye after a poorly performed operation, injection into the eye, or injury. But sometimes endofalmitis is a complication of an infectious process in another part of the body. For example, this can happen with a urinary tract infection or blood poisoning.
This condition has very pronounced symptoms: increased pain in the eyes, distinct redness and swelling, a sharp decrease or loss of vision. And white or yellow (purulent) discharge from the eyes.
What to do
Endofalmitis is a medical emergency. If you do not quickly stop the inflammation, you can be left without vision. Therefore, if you suspect such an infection, you should immediately go to the emergency room or to an ophthalmologist.
13. Shingles
It is also herpes zoster (lat. Herpes zoster). This disease, as a rule, is a complication of chickenpox transferred many years ago.
Usually, shingles is a painful red rash that most often appears in the lower back, hence the name. But if the herpes virus has affected the optic nerves, a painful rash can also appear in the eye area - mainly on the upper and lower eyelids. Among other things, herpes causes swelling of the eyes, decreased vision and the appearance of discharge.
But if the herpes virus has affected the optic nerves, a painful rash can also appear in the eye area - mainly on the upper and lower eyelids. Among other things, herpes causes swelling of the eyes, decreased vision and the appearance of discharge.
What to do
Shingles must be treated urgently or it can lead to corneal scarring, glaucoma or cataracts. Therefore, you need to see an ophthalmologist as soon as possible: the doctor will assess the degree of eye damage and prescribe the most effective treatment.
14. Covid
In some cases, coronavirus infection affects the eyes and can cause symptoms similar to those of allergic conjunctivitis.
To distinguish between these conditions, check with your state of health. If signs of conjunctivitis arose against the background of high fever, cough, severe weakness and other manifestations of covid, it is most likely that the inflammation of the eyes has a coronavirus nature.
What to do
To relieve the condition, apply compresses to the eyes. For example, a clean cotton sponge soaked in warm water. You can also apply a cool, damp towel to your eyes.
For example, a clean cotton sponge soaked in warm water. You can also apply a cool, damp towel to your eyes.
Over-the-counter pain relievers such as ibuprofen and eye drops such as antihistamines or artificial tears are acceptable.
If signs of conjunctivitis persist, consult your physician or ophthalmologist. With confirmed covid - by phone.
What to do so that the discharge does not appear
Surely you will not be able to protect yourself from infections and injuries. But you can reduce the risks.
- Wash your hands regularly. Often we unconsciously touch our eyes, so it is more than possible to bring an infection from dirty hands.
- Watch your movements and avoid touching your face and especially your eyes with your hands.
- If you spend a lot of time in front of the computer or just feel dry eyes, use "artificial tear" drops.
- Carefully remove morning secretions. It is best to do this with a cotton pad or gauze dipped in warm water.

- If you wear contact lenses, pay close attention to how your eyes feel. At the first hint of discomfort or discharge, consult an ophthalmologist.
- If you have had an eye infection before, discard any eye makeup you were wearing during that period. Buy a new one.
- Avoid exposure to allergens whenever possible. For example, do not go outside during the flowering period of those plants whose pollen you are allergic to.
Read also 🧐
- Why you shouldn’t touch cow parsnip and what to do if you did touch it
- How to recognize carbon monoxide poisoning and what to do next
- Why platelets are low and what to do
- What is the normal heart rate and what to do if yours does not match it
- How makeup can harm the eyes and what to do to reduce the risk
Why is there mucus in the eyes. How to treat eye discharge in a child.
From All About Vision
Eye discharge is a combination of mucus, fat, skin cells, and other particles that accumulate in the corners of the eyes during sleep.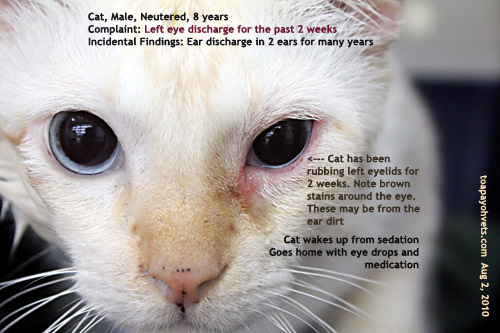 " They may be wet and sticky or dried out, depending on how much fluid is present.
" They may be wet and sticky or dried out, depending on how much fluid is present.
Mucous secretions have a protective function, flushing waste products and potentially harmful particles from the tear film and the anterior surface of the eye.0006
Throughout the day, the eyes secrete mucus, but the ever-present tear film bathes your eyes with every blink, removing the secretions before they can harden.
When you sleep and do not blink, the discharge accumulates and dries up in the corners of the eyes, and sometimes along the lash line. accompanied by blurry vision, sensitivity to light or eye pain may indicate a serious eye infection or eye disease. Therefore, you should immediately contact an optometrist.
FIND AN OCULIST OR OPTICS SHOP NEAR YOU : Whether you need an eye exam or are ready to buy eyeglasses or contact lenses, our locator will help you find a safe place nearby.
Where does eye discharge come from?
The discharge from the eyes consists mainly of a watery mucous secretion (mucin) produced by the conjunctiva and the secretion of the meibomian glands, an oily substance that helps to moisten the eyes between blinks.
Those impurities that are not washed away by tears accumulate in the inner corners of the eye and along the lash line. ""
Causes of discharge from the eyes the consistency, color, or amount of discharge, this may indicate an infection or eye disease.
Common eye conditions with abnormal eye discharge include:
Conjunctivitis. Discharge from the eyes is a common symptom of conjunctivitis - inflammation of the thin membrane that lines the "alkaline" of the eye (the sclera) and the inner surface of the eyelids.
In addition to itching, stinging, eye irritation and redness , conjunctivitis is usually accompanied by white, yellow, or green mucus that may form a crust along the eyelash line during sleep. In some cases, the crust formed on the eyelid can be so dense that it does not allow you to open your eyes.
There are three types of conjunctivitis:
Viral conjunctivitis
Viral conjunctivitis is highly contagious and is caused by the common cold or herpes simplex virus. Eye discharge from viral conjunctivitis is usually clear and watery, and may include white or yellowish mucus.
Eye discharge from viral conjunctivitis is usually clear and watery, and may include white or yellowish mucus.
Bacterial conjunctivitis
Bacterial conjunctivitis, as the name suggests, is caused by a bacterial infection. If not promptly treated, it can pose a threat to vision. Eye discharge from bacterial conjunctivitis is usually thicker and purulent (like pus) than from viral conjunctivitis, and is usually yellow, green, or even gray in color. In the morning after sleep, patients often cannot open their eyelids, which are completely stuck together with secretions.
Allergic conjunctivitis
Allergic conjunctivitis is triggered by allergens - pollen, dandruff, dust and other common irritants that cause eye allergy . It can also be caused by an allergic reaction to chemical pollutants, cosmetics, contact lens solutions, and eye drops. In allergic conjunctivitis, the discharge from the eyes is usually watery. Allergic conjunctivitis is not contagious and always affects both eyes.
Other eye infections
In addition to conjunctivitis, there are many eye infections that cause abnormal eye discharge. For example:
-
Herpes ocularis (recurrent viral eye infection)
-
Fungal keratitis (a rare but serious inflammation of the cornea)
-
while wearing contact lenses).
The discharge from an eye infection varies greatly - it can be clear and watery or thick, green and sticky, so you should see an eye doctor as soon as possible for diagnosis and treatment.
Blepharitis
Chronic eyelid disease, blepharitis, is either an inflammation of the eyelash hair follicles or an abnormal secretion of the meibomian glands at the inner edge of the eyelids.
Meibomian gland dysfunction
Also called MGD, this sebaceous gland disorder in the eyelid can cause foamy discharge from the eyes, sticky eyelids, yellow or green pus, and irritation and pain.
Barley
Barley is a blockage of the meibomian gland at the base of the eyelid, usually caused by an infected eyelash follicle. Also called hordeolum, it resembles a pimple at the edge of the eyelid and is usually accompanied by redness, swelling of the eyelids, and tenderness at the site of the lesion. Yellow pus, sticking of the eyelids, and discomfort when blinking may also occur.
SEE. ALSO: How to get rid of stye
The tear duct system provides moisture and protection to the eyes.
Dry eye
Inadequate tear production or meibomian gland dysfunction can lead to dry eye syndrome , a frequently chronic condition in which the surface of the eye is not properly lubricated, becoming irritated and inflamed. Symptoms include reddened, bloodshot eyes, a burning sensation, blurred vision, and a foreign body sensation in the eye. "" Sometimes dry eyes can also cause very heavy watering.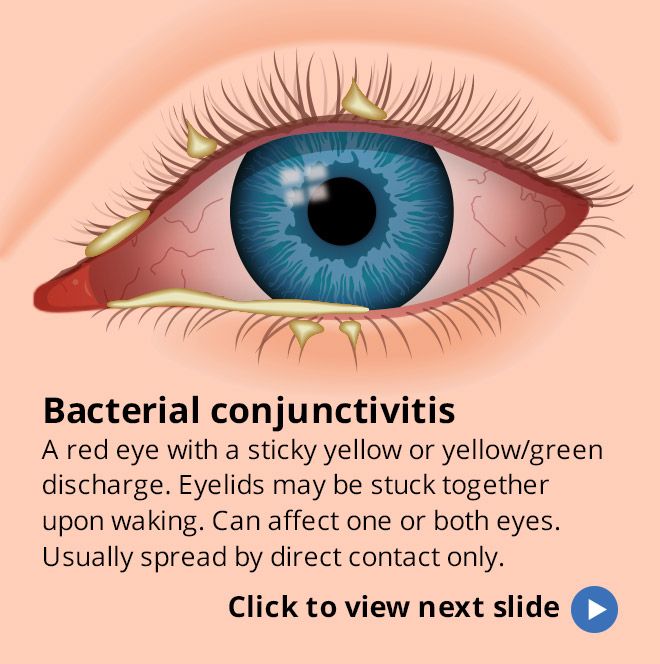
Contact lenses
When wearing contact lenses, there may be more discharge from the eyes than usual. This can be due to a variety of reasons, including eye infection from contact lens wear, contact lens discomfort resulting in dry and irritated eyes, and contact lens wearers rubbing their eyes more frequently. If you notice more discharge due to contact lenses, remove your lenses and see an optometrist to rule out a potentially serious eye disease.
Eye injury
A foreign body in the eye (such as dirt, particles or a chemical) or eye injury may cause watery discharge as a natural defense reaction. If you notice pus or blood in your eye (subconjunctival hemorrhage) after injury to eye , contact your optometrist immediately for treatment. All eye injuries should be treated as an emergency.
Corneal ulcer
A corneal ulcer is a vision-threatening, abscess-like infection of the cornea, usually caused by trauma to the eye or an advanced eye infection. If left untreated, corneal ulcers can lead to permanent vision loss. Corneal ulcers are characterized by pain, redness, swelling of the eyelids, and thick discharge from the eyes. The discharge of pus can be so strong that it causes clouding of the cornea and blurred vision.
If left untreated, corneal ulcers can lead to permanent vision loss. Corneal ulcers are characterized by pain, redness, swelling of the eyelids, and thick discharge from the eyes. The discharge of pus can be so strong that it causes clouding of the cornea and blurred vision.
Dacryocystitis
When the lacrimal duct is blocked, inflammation and infection of the lacrimal sac in the drainage system of the lacrimal apparatus can occur, resulting in a painful and swollen bump under the inner eyelid. In addition to pain and redness, common symptoms of dacryocystitis include watery eyes, sticky discharge from the eyes, and blurry vision.
Eye discharge treatment
A small amount of eye discharge is harmless, but if you notice changes in color, frequency, consistency and amount, contact your optometrist.
If mucus in the eyes is due to an eye infection, the optometrist may prescribe antibiotics or antiviral eye drops and ointments.