Pain in lower abdomen and pelvic area during pregnancy
Pelvic pain in pregnancy - NHS
Some women may develop pelvic pain in pregnancy. This is sometimes called pregnancy-related pelvic girdle pain (PGP) or symphysis pubis dysfunction (SPD).
PGP is a collection of uncomfortable symptoms caused by a stiffness of your pelvic joints or the joints moving unevenly at either the back or front of your pelvis.
Symptoms of PGP
PGP is not harmful to your baby, but it can be painful and make it hard to get around.
Women with PGP may feel pain:
- over the pubic bone at the front in the centre, roughly level with your hips
- across 1 or both sides of your lower back
- in the area between your vagina and anus (perineum)
- spreading to your thighs
Some women may feel or hear a clicking or grinding in the pelvic area.
The pain can be worse when you're:
- walking
- going up or down stairs
- standing on 1 leg (for example, when you're getting dressed)
- turning over in bed
- moving your legs apart (for example, when you get out of a car)
Most women with PGP can have a vaginal birth.
Non-urgent advice: Call your midwife or GP if you have pelvic pain and:
- it's hard for you to move around
- it hurts to get out of a car or turn over in bed
- it's painful going up or down stairs
These can be signs of pregnancy-related pelvic girdle pain.
Treatments for PGP
Getting diagnosed as early as possible can help keep pain to a minimum and avoid long-term discomfort.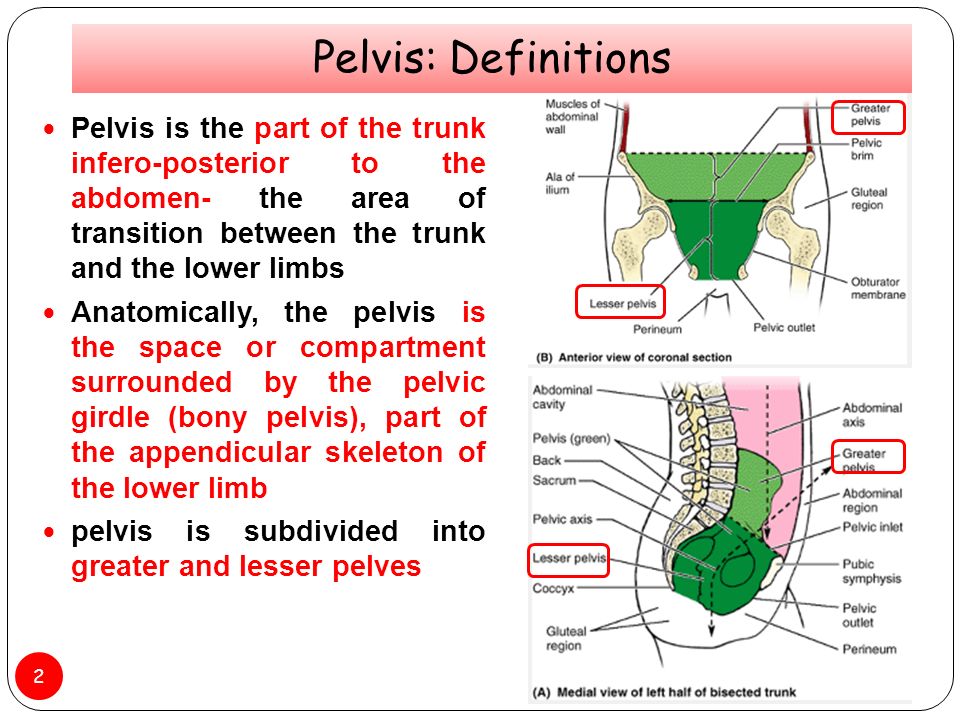
You can ask your midwife for a referral to a physiotherapist who specialises in obstetric pelvic joint problems.
Physiotherapy aims to relieve or ease pain, improve muscle function, and improve your pelvic joint position and stability.
This may include:
- manual therapy to make sure the joints of your pelvis, hip and spine move normally
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice and suggestions, including positions for labour and birth, looking after your baby and positions for sex
- pain relief, such as TENS
- equipment, if necessary, such as crutches or pelvic support belts
These problems tend not to get completely better until the baby is born, but treatment from an experienced practitioner can improve the symptoms during pregnancy.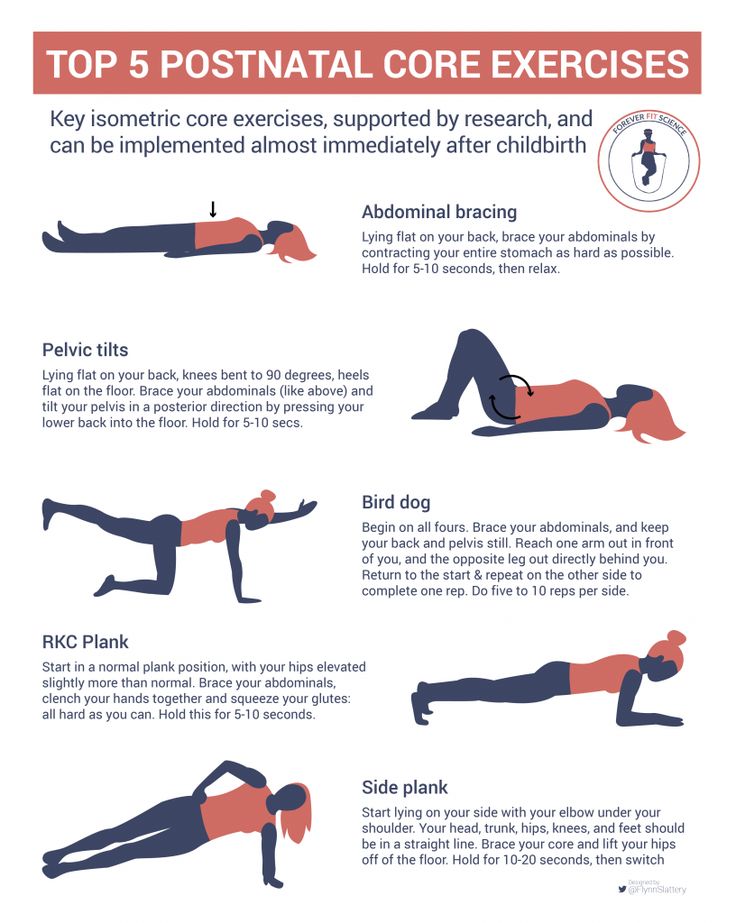
You can contact the Pelvic Partnership for information and support.
Coping with pelvic pain in pregnancy
Your physiotherapist may recommend a pelvic support belt to help ease your pain, or crutches to help you get around.
It can help to plan your day so you avoid activities that cause you pain. For example, do not go up or down stairs more often than you have to.
The Pelvic, Obstetric & Gynaecological Physiotherapy (POGP) network also offers this advice:
- be as active as possible within your pain limits, and avoid activities that make the pain worse
- rest when you can
- ask your family, friends or partner, if you have one, to help with everyday activities
- wear flat, supportive shoes
- sit down to get dressed – for example, do not stand on 1 leg when putting on jeans
- keep your knees together when getting in and out of the car – a plastic bag on the seat can help you swivel
- sleep in a comfortable position – for example, on your side with a pillow between your legs
- try different ways of turning over in bed – for example, turning over with your knees together and squeezing your buttocks
- take the stairs 1 at a time, or go upstairs backwards or on your bottom
- if you're using crutches, have a small backpack to carry things in
- if you want to have sex, consider different positions, such as kneeling on all fours
POGP suggests that you avoid:
- standing on 1 leg
- bending and twisting to lift, or carrying a baby on 1 hip
- crossing your legs
- sitting on the floor, or sitting twisted
- sitting or standing for long periods
- lifting heavy weights, such as shopping bags, wet washing or a toddler
- vacuuming
- pushing heavy objects, such as a supermarket trolley
- carrying anything in only 1 hand (try using a small backpack)
The physiotherapist should be able to provide advice on coping with the emotional impact of living with chronic pain, such as using relaxation techniques. If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
Download the POGP leaflet Pregnancy-related pelvic girdle pain for mothers-to-be and new mothers.
You can get more information on managing everyday activities with PGP from the Pelvic Partnership.
Labour and birth with pelvic pain
Many women with pelvic pain in pregnancy can have a normal vaginal birth.
Plan ahead and talk about your birth plan with your birth partner and midwife.
Write in your birth plan that you have PGP, so the people supporting you during labour and birth will be aware of your condition.
Think about birth positions that are the most comfortable for you, and write them in your birth plan.
Being in water can take the weight off your joints and allow you to move more easily, so you might want to think about having a water birth. You can discuss this with your midwife.
You can discuss this with your midwife.
Your 'pain-free range of movement'
If you have pain when you open your legs, find out your pain-free range of movement.
To do this, lie on your back or sit on the edge of a chair and open your legs as far as you can without pain.
Your partner or midwife can measure the distance between your knees with a tape measure. This is your pain-free range.
To protect your joints, try not to open your legs wider than this during labour and birth.
This is particularly important if you have an epidural for pain relief in labour, as you won't be feeling the pain that warns you that you're separating your legs too far.
If you have an epidural, make sure your midwife and birth partner are aware of your pain-free range of movement of your legs.
When pushing in the second stage of labour, you may find it beneficial to lie on one side.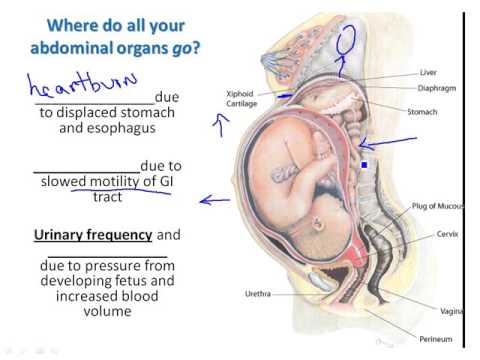
This prevents your legs from being separated too much. You can stay in this position for the birth of your baby, if you wish.
Sometimes it might be necessary to open your legs wider than your pain-free range to deliver your baby safely, particularly if you have an assisted delivery (for example, with the vacuum or ventouse).
Even in this case, it's possible to limit the separation of your legs. Make sure your midwife and doctor are aware that you have PGP.
If you go beyond your pain-free range, your physiotherapist should assess you after the birth.
Take extra care until they have assessed and advised you.
Who gets pelvic pain in pregnancy?
It's estimated that PGP affects up to 1 in 5 pregnant women to some degree.
It's not known exactly why pelvic pain affects some women, but it's thought to be linked to a number of issues, including previous damage to the pelvis, pelvic joints moving unevenly, and the weight or position of the baby.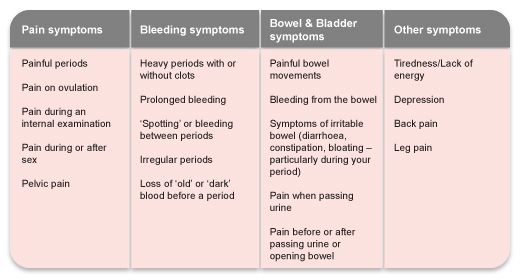
Factors that may make a woman more likely to develop PGP include:
- a history of lower back or pelvic girdle pain
- previous injury to the pelvis (for example, from a fall or accident)
- having PGP in a previous pregnancy
- a physically demanding job
- being overweight
- having a multiple birth pregnancy
healthtalk.org has interviews with women talking about their experiences of pelvic pain in pregnancy.
Read more about coping with common pregnancy problems, including nausea, heartburn, tiredness and constipation.
Find maternity services or physiotherapy services near you.
Community content from HealthUnlockedUterus Pain in Early Pregnancy: Causes and Seeking Help
During early pregnancy, you may experience mild twinges or cramping in the uterus.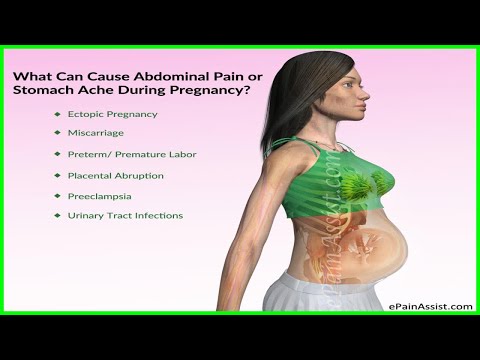 You may also feel aching in your vagina, lower abdomen, pelvic region, or back. It may feel similar to menstrual period cramps.
You may also feel aching in your vagina, lower abdomen, pelvic region, or back. It may feel similar to menstrual period cramps.
These minor pains may be caused by different factors like implantation, constipation or gas, or the womb expanding and your ligaments stretching to make room for your baby.
If the pain is mild and goes away on its own, it’s likely nothing to worry about. But any pain along with spotting or heavy bleeding should be reported to your doctor.
Seek emergency care if you experience sharp or chronic pain along with faintness, nausea, high fever or chills, or dizziness.
Read on to learn more about the causes for uterus pain in early pregnancy and when to seek help.
During the first weeks of pregnancy, you likely won’t notice your uterus growing or expanding. But by the 12th week, your uterus stretches and grows to about the size of a grapefruit. If you’re pregnant with twins or multiples, you may feel your uterus stretching sooner.
Symptoms of your uterus stretching may include twinges, aches, or mild discomfort in your uterine or lower abdominal region. This is a normal part of pregnancy and a sign that everything is progressing normally.
This is a normal part of pregnancy and a sign that everything is progressing normally.
Watch for spotting or painful cramping. Report these symptoms to your doctor.
Gas and constipation are common during the first trimester of pregnancy. Levels of hormones in the body increase during pregnancy, which can slow down digestion and relax muscles in the bowels. You may feel additional pressure in the uterus as a result.
Symptoms also include hard, dry stools, or fewer bowel movements than usual.
Some women also experience bloating or gas in the first trimester. This is considered a normal part of pregnancy.
Drink at least 10 cups of water per day to help relieve gas pain and bloating.
For constipation, eat plenty of fiber-rich foods. You can also talk to your doctor about taking a pregnancy-safe stool softener.
Miscarriage is the loss of pregnancy before 20 weeks.
Possible symptoms include:
- vaginal spotting or bleeding
- uterine or pelvic pain
- low back pain
- abdominal pain
- passing tissue or discharge through the vagina
Let your doctor know if you’re experiencing miscarriage symptoms.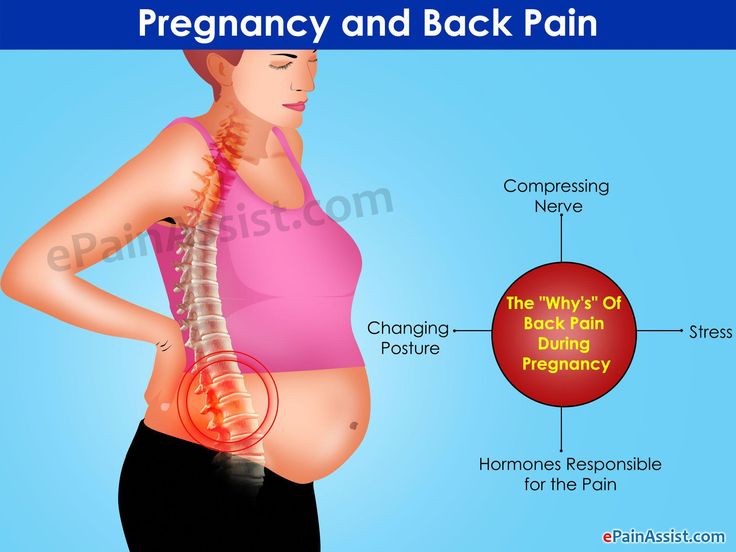 Once a miscarriage has started, there is no treatment for saving the pregnancy, but in some cases medication or surgery is needed.
Once a miscarriage has started, there is no treatment for saving the pregnancy, but in some cases medication or surgery is needed.
Ectopic pregnancy occurs when a fertilized egg attaches itself in a place other than the inside of the uterus, usually in the fallopian tubes. You may feel sharp, stabbing, or chronic pain on one or both sides of the uterus or abdomen.
Other symptoms include:
- vaginal bleeding that’s heavier or lighter than your normal period
- weakness, dizziness, or fainting
- gastrointestinal or stomach discomfort
Ectopic pregnancy is a medical emergency. Seek immediate emergency medical help if you think you’re experiencing an ectopic pregnancy.
Round ligament pain usually starts in the second trimester, so it’s unlikely to be the cause of pain in early pregnancy. The round ligaments are located in the pelvis and hold the uterus in place. As your belly grows, they stretch.
With round ligament pain, you may experience what feels like a spasm on the right side of your abdomen or right hip.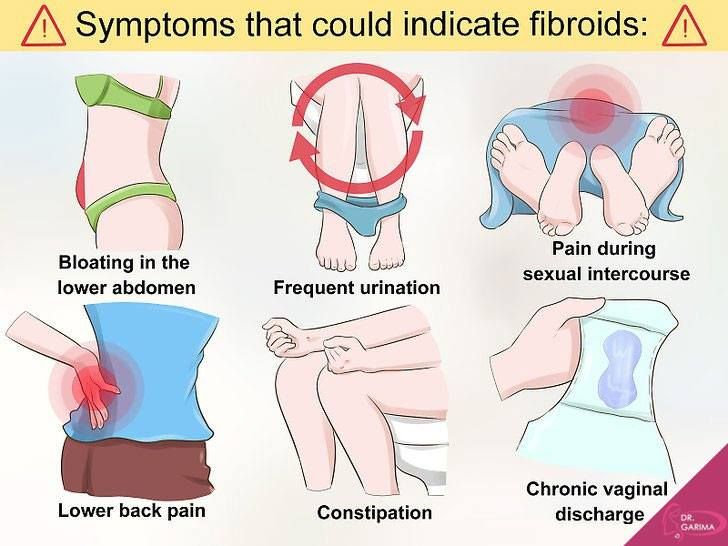 Some pregnant women do feel round ligament pain on both sides, though.
Some pregnant women do feel round ligament pain on both sides, though.
The pain should only last a few seconds or minutes, though it may return when you laugh or do certain movements like standing or bending down.
If you continue to experience round ligament pain, it may be helpful to try light stretching, prenatal yoga, or prenatal massage. Always check with your doctor before trying these treatments, though.
Treatment for uterine pains depends on your symptoms. Mild uterine pain that goes away after a few minutes or hours is likely nothing to worry about.
You can treat mild uterine discomfort at home by taking a warm (not hot) shower or bath, resting, and drinking plenty of water and other fluids. Tell your doctor about your symptoms, as they may recommend another form of treatment that’s safe for your pregnancy.
Sharp, stabbing, or chronic pain along with symptoms like bleeding, shortness of breath, or fever or chills likely requires emergency medical care.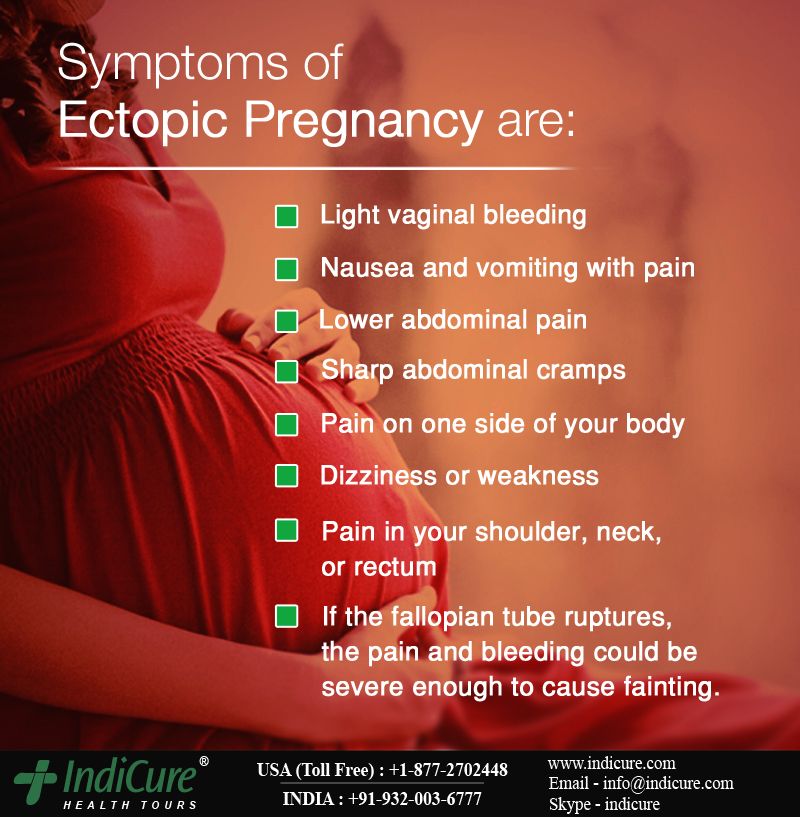
Let medical staff know you’re pregnant and report any symptoms such as dizziness, nausea, or faintness right away. The medical staff will assess your symptoms and may perform an ultrasound.
Seek help if you’re experiencing sharp or chronic uterine pain along with other symptoms like:
- vaginal bleeding
- dizziness
- high fever
- chills
If the pain goes away on its own, it likely isn’t a reason for concern, but you should still let your doctor know.
You should also let your doctor know about any mild uterine pain during pregnancy. They can decide if you need to be seen right away or if you can wait until your next scheduled prenatal appointment.
Also, tell your doctor if you’re experiencing uterine pain along with spotting or bleeding. These may be symptoms of a miscarriage. Your doctor can assess your symptoms and determine next steps.
Mild uterine pain during early pregnancy doesn’t always mean something is wrong with the pregnancy. However, pain accompanied by spotting or bleeding should be reported to your doctor. These may be signs that a miscarriage is starting.
However, pain accompanied by spotting or bleeding should be reported to your doctor. These may be signs that a miscarriage is starting.
Your doctor can assess your symptoms at any point during your pregnancy to determine if you need medical care.
Pelvic pain in early pregnancy | Symptoms
Ectopic pregnancy
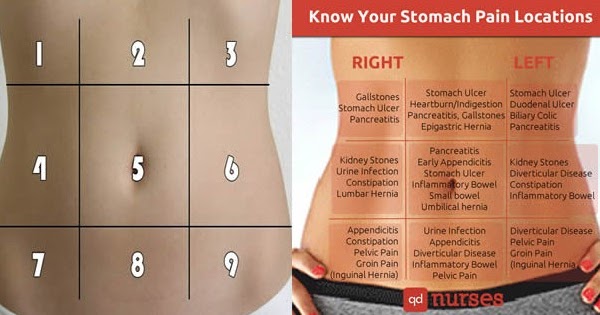
Signs: Abdominal or pelvic pain that is often sudden and persistent (not crampy), localized, and may or may not be accompanied by vaginal bleeding. If an ectopic pregnancy is terminated, fainting, dizziness, or palpitations may occur.
Miscarriage (threatened miscarriage or ongoing spontaneous abortion)
Signs: Spasmodic pain in the pelvic area, often radiating to the abdominal cavity. Often vaginal bleeding, sometimes with the release of fragments of fetal tissue.
Septic abortion (infection of the contents of the uterus before, during or after a miscarriage)
Signs: Usually in women who have already had an abortion (usually performed by an inexperienced doctor or by the women themselves). Fever and chills, persistent abdominal or pelvic pain, and pus-filled vaginal discharge.
Fever and chills, persistent abdominal or pelvic pain, and pus-filled vaginal discharge.
Normal changes during pregnancy (includes distension and growth of the uterus in early pregnancy)
Signs: Cramping or burning sensation in the lower abdomen, pelvis and/or lower back.
Uterine fibroma degeneration
Signs: Pelvic pain that starts suddenly and is usually accompanied by nausea, vomiting, and fever. Sometimes vaginal bleeding.
Torsion (twisting) of the epididymis
Signs: Pain in the pelvic area that starts suddenly, may be with colic, which is often mild if the ovary uncoils on its own, often with nausea or vomiting.
Rupture of the corpus luteum cyst (forms in the ovary from which the egg is released after ovulation)
Signs: Abdominal or pelvic pain that originates in a specific area, sometimes resembling pain due to ovarian torsion;
usually occurs suddenly. Vaginal bleeding.
Pelvic inflammatory disease
Signs: Pain in the pelvic area that lasts a long time, usually develops gradually, as a rule, is felt on both sides.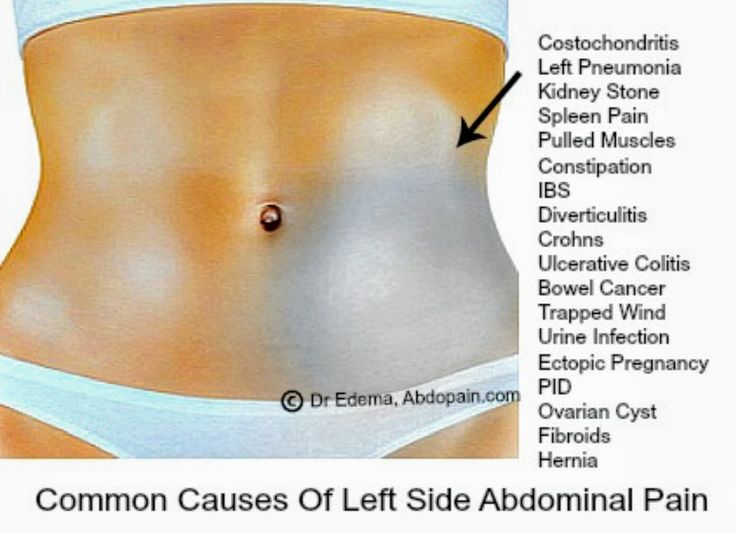
Vaginal discharge containing pus. Sometimes fever or chills. It is more common in women who have sex with new partners and do not use condoms or diaphragms.
Appendicitis
Signs: As a rule, continuous pain and tenderness in the lower abdomen on the right. There may be pain in a different place (higher in the abdomen) or a different nature of pain (weaker and more crampy) compared to non-pregnant women.
Urinary tract infections
Signs: Discomfort that is felt just above the pubic bone. Often burning during urination, frequent urge to urinate, and the need to urinate immediately. Sometimes blood in the urine.
Inflammatory bowel disease (Crohn's disease, ulcerative colitis)
Signs: Pain, which may be spasmodic or continuous, may occur in multiple locations. Often diarrhea, sometimes with mucus or blood. As a rule, in women who have already been diagnosed with this disease.
Intestinal obstruction (intestinal obstruction)
Signs: Spasmodic pain that recurs periodically, vomiting.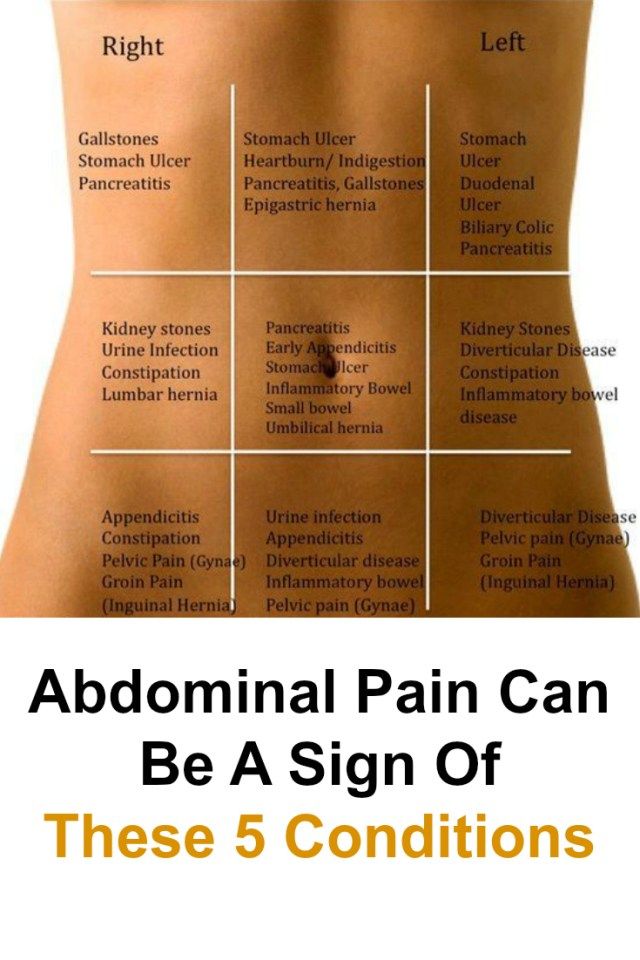 Lack of bowel movements or gas (flatulence), bloating. As a rule, in women who have undergone surgery in the abdominal cavity.
Lack of bowel movements or gas (flatulence), bloating. As a rule, in women who have undergone surgery in the abdominal cavity.
Gastroenteritis
Signs: Usually vomiting and diarrhea.
Why does the stomach pull in the early stages of pregnancy?
Why does the stomach pull in early pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of having an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations, and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor.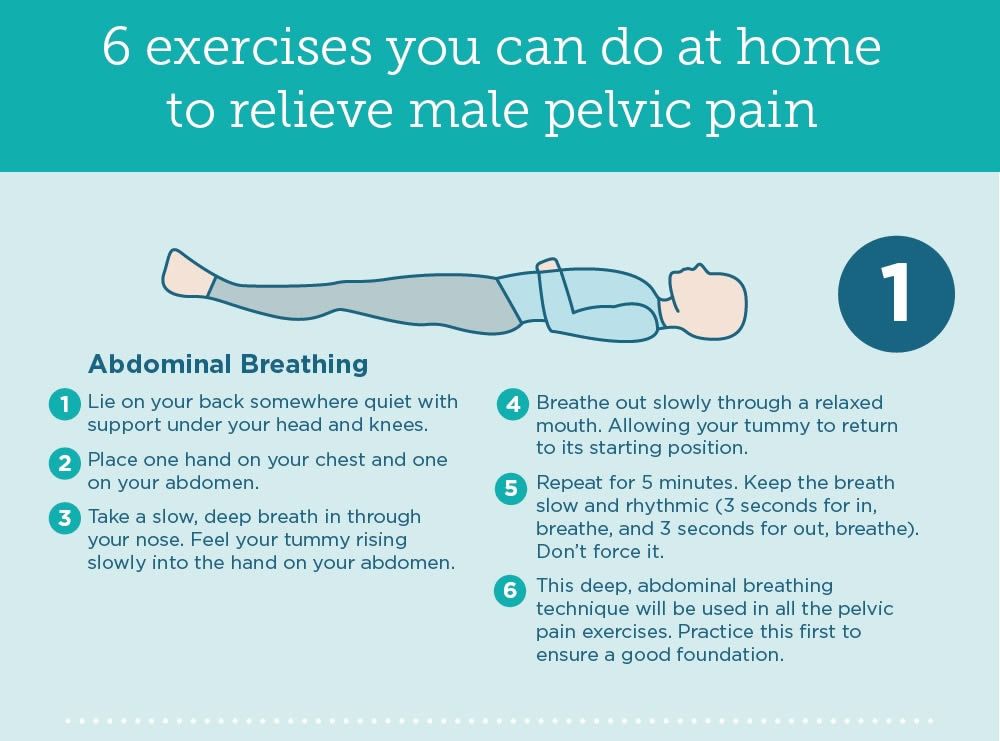 However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy can be:
- "obstetric";
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- miscarriage;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus.
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good if the menstruation is regular and not less than 14 days late. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.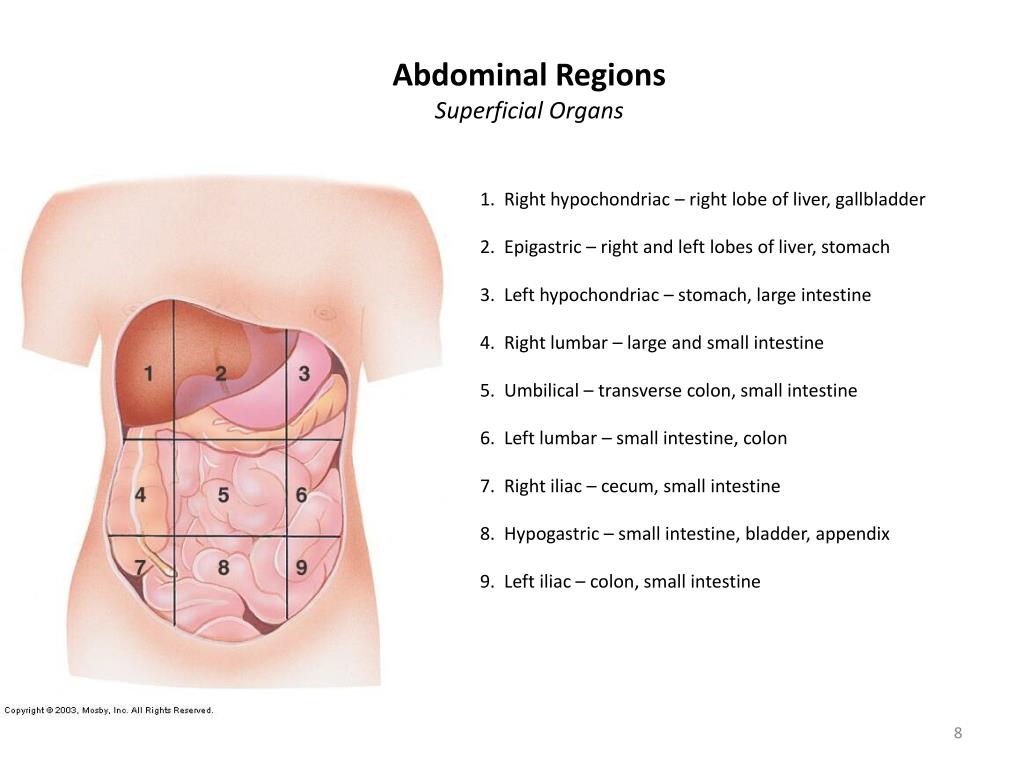
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the influence of the movement of cilia in the fallopian tubes.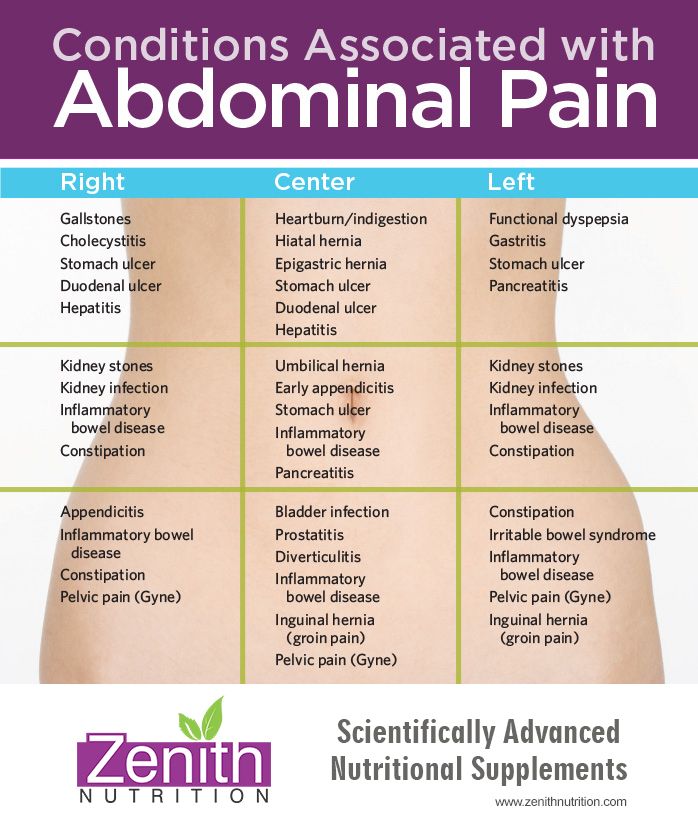 The uterine endometrium is a loose mass where a fertilized egg is implanted.
The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the introduction of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Causes that may cause miscarriage include:
- heavy physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you should consult a doctor, as a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.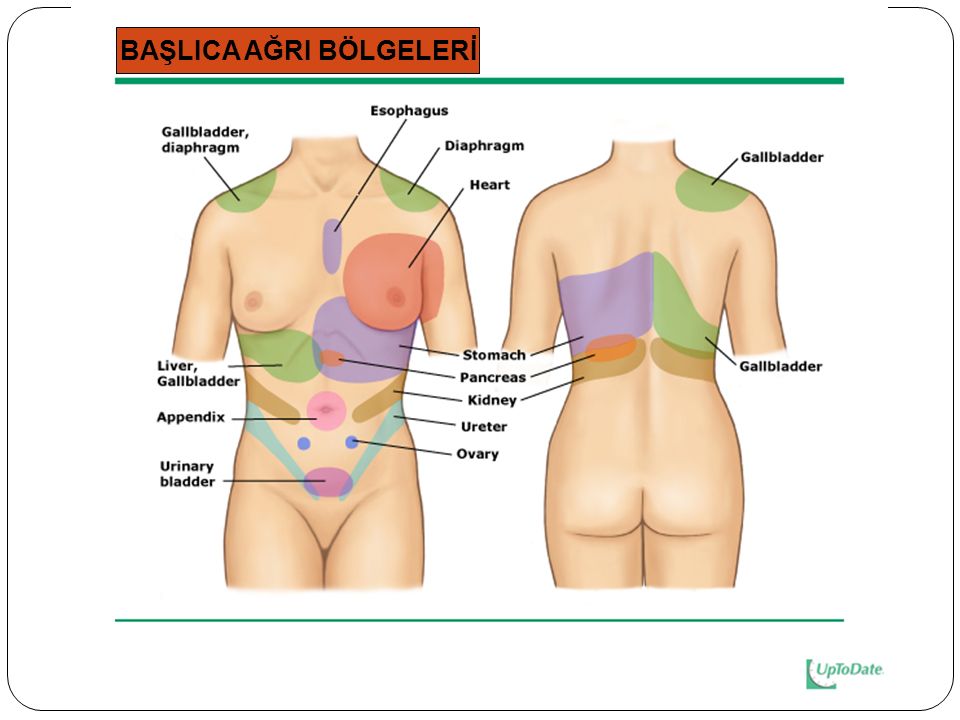
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Missed pregnancy
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, miscarriage occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
Most often, miscarriage occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. In this case, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.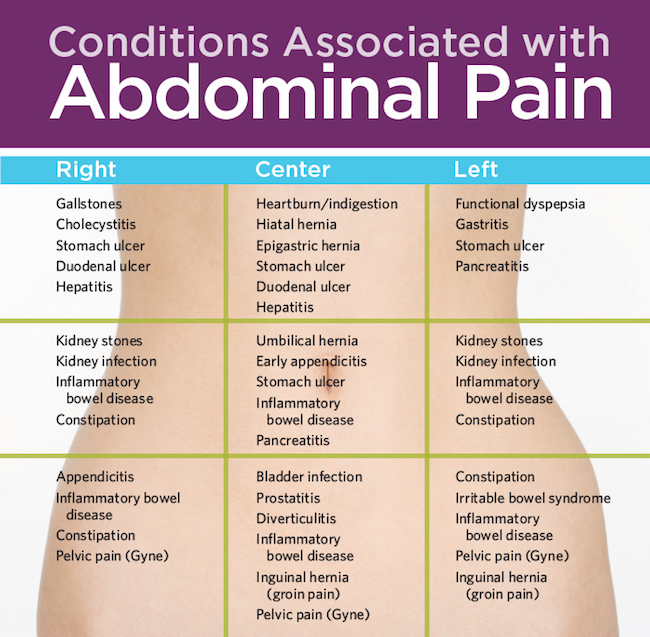
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Cystitis due to the anatomical features of a woman can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.
The bladder, located in the lower third of the abdomen, may give false symptoms of a threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection.