Can toddlers become lactose intolerant
Lactose Intolerance in Children
What is lactose intolerance in children?
Lactose intolerance is when the body can’t easily break down or digest lactose. Lactose is a sugar found in milk and milk products.
If your child is lactose intolerant, your child may have unpleasant symptoms after eating or drinking milk products. These symptoms include bloating, diarrhea, and gas.
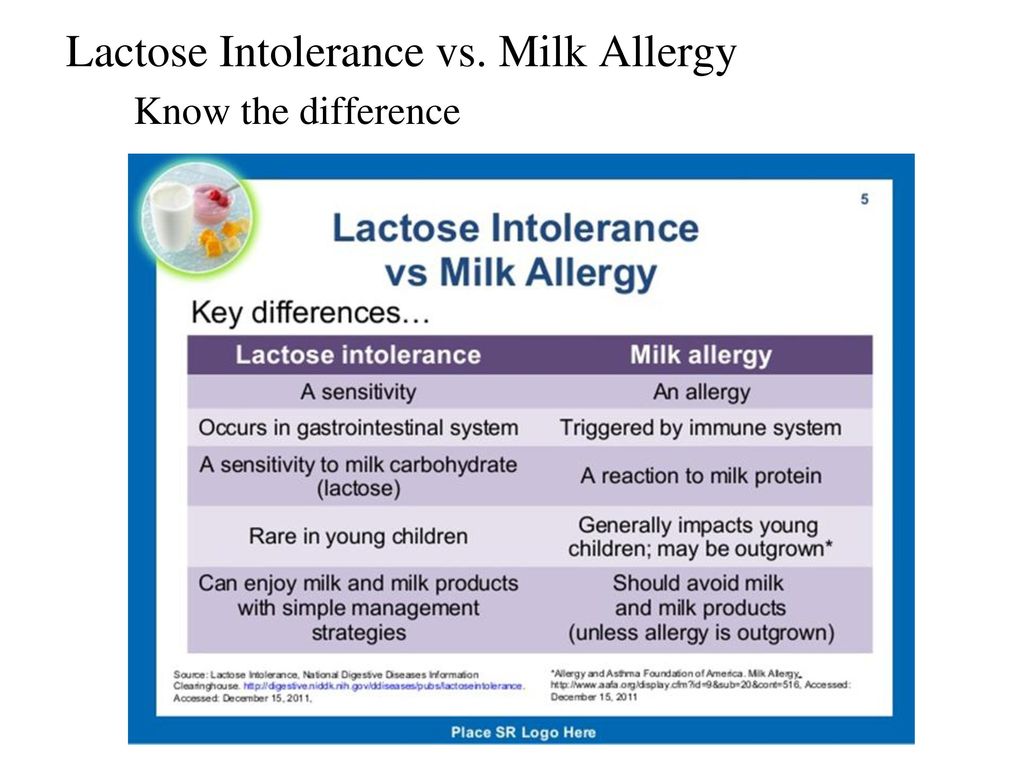
Lactose intolerance is different from having a food allergy to milk.
What causes lactose intolerance in a child?
Lactose intolerance happens when the small intestine doesn’t make enough of a digestive juice, or enzyme, called lactase. Without enough lactase, the body can’t break down or digest lactose.
Lactose intolerance can happen to both children and adults. Some common causes include:
-
Digestive diseases or infection
-
Injury to the small intestine
-
Family history of lactose intolerance.
In these cases, over time the body may make less of the lactase enzyme. Symptoms may occur during the teen or adult years.
-
A baby being born too early, also called a premature baby. This type of lactose intolerance is often a short-term problem that goes away.
In very rare cases, some newborns can’t make any lactase from birth.
Which children are at risk for lactose intolerance?
Lactose intolerance can happen to anyone. But your child is more at risk for lactose intolerance if your child:
-
Is a baby who was born too early (premature). This type of lactose intolerance is often a short-term problem that goes away.
-
Is African American, Jewish, Mexican American, American Indian, or Asian American
-
Has a family history of lactose intolerance. Symptoms may occur during the teen or adult years.

What are the symptoms of lactose intolerance in a child?
Symptoms often begin to appear in white children after age 5. They appear in African-American children as young as 2 years old.
Symptoms begin about 30 minutes to 2 hours after having foods or drinks containing lactose. Each child’s symptoms may vary. Symptoms may include:
-
Upset stomach or nausea
-
Cramps
-
Bloating
-
Belly (abdominal) pain
-
Gas
-
Loose stool or diarrhea
-
Vomiting, happens more often to teens
How severe your child’s symptoms are will depend on how much lactose your child has had. It will also depend on how much lactase your child’s body makes.
The symptoms of lactose intolerance may look like other health conditions. Always see your child's healthcare provider for a diagnosis.
How is lactose intolerance diagnosed in a child?
Your child’s healthcare provider will give your child a physical exam and take a health history.
Your child may need to be tested. The most common tests used to check how lactose is absorbed in the digestive system include:
-
Lactose tolerance test. This test checks how lactose is absorbed by your child’s digestive system. After fasting, your child drinks a liquid that has lactose. The loose stools are then tested for lactose for the next 24 hours.
-
Hydrogen breath test. Your child drinks a liquid that has a lot of lactose. The breath is then checked at regular times to measure the amount of hydrogen. High levels of hydrogen mean your child is lactose intolerant.
-
Stool acidity test. This test is used for babies and young children. It checks how much acid is in the stool. If your child is not digesting lactose, the stool will have lactic acid, glucose, and other fatty acids.
How is lactose intolerance treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
No treatment will help your child’s body make more lactase. But you can manage your child’s symptoms with a diet that limits lactose. Your child may not have to stop eating all foods with lactose. Your child's healthcare provider may also suggest your child take lactase enzymes. They are sold over the counter.
Here are some tips for managing lactose in your child’s diet:
-
Start slowly. After a week of limiting foods with lactose, try adding small amounts of milk or milk products back to your child’s diet.
 Watch to see if your child has any symptoms. Note which foods your child can handle and which foods your child should not eat.
Watch to see if your child has any symptoms. Note which foods your child can handle and which foods your child should not eat. -
Have milk and milk products with other foods. You may find your child has fewer symptoms if your child has milk or milk products with meals. Have your child try eating cheese with crackers. Or let your child have milk with cereal.
-
Choose dairy products with naturally lower levels of lactose. These include hard cheeses and yogurt.
-
Look for lactose-free and lactose-reduced milk and milk products. These can be found at many food stores. They are the same as regular milk and milk products. But they have the lactase enzyme added to them.
-
Ask about lactase products.
 Ask your child’s healthcare provider if your child should take a lactase pill or lactase drops when having milk products.
Ask your child’s healthcare provider if your child should take a lactase pill or lactase drops when having milk products.
Talk with your child’s provider about what products or diet changes may help your child. You may also find it helpful to see a registered dietitian.
Calcium
Children and teens who are lactose intolerant may have little or no milk in their diet. But milk and dairy products are a major source of calcium. If your child is lactose intolerant, be sure that your child gets enough calcium. Calcium is needed for growing and repairing bones throughout life. Calcium may also help prevent some diseases.
The amount of calcium your child needs will vary by age:
|
Child's age |
Recommended dietary amount of calcium (mg per day) |
|
0 to 6 months |
200 mg |
|
6 months to 1 year |
260 mg |
|
1 to 3 years |
700 mg |
|
4 to 8 years |
1,000 mg |
|
9 to 18 years |
1,300 mg |
Many nondairy foods are high in calcium, including:
-
Green vegetables, such as collard greens, turnip greens, broccoli, and kale
-
Fish with soft, edible bones, such as salmon and sardines
Other nondairy foods that are good sources of calcium include:
-
Tofu
-
Orange juice with added calcium
-
Soy milk with added calcium
-
Breakfast cereals with added calcium
Always talk with your child’s healthcare provider. Your child's provider may prescribe a calcium supplement if your child can’t get enough calcium from diet alone.
Your child's provider may prescribe a calcium supplement if your child can’t get enough calcium from diet alone.
Vitamin D
Vitamin D is needed for the body to absorb calcium. It’s important that your child’s diet has enough vitamin D. Sources of vitamin D include eggs and liver.
Children under 1 year old should have a vitamin D supplement of 400 IU a day. Children over 1 year old should have 600 IU of vitamin D a day.
What are possible complications of lactose intolerance in a child?
Lactose intolerance won’t hurt your child’s body. The symptoms are unpleasant, but they are not serious.
How can I help my child live with lactose intolerance?
Lactose intolerance can cause unpleasant symptoms. But in most cases, you don’t need to remove all foods with lactose from your child's diet. By watching your child's symptoms, you can find out which foods he or she can handle. You can also tell which foods your child should stay away from.
When foods are removed from your child's diet, you must replace them with other foods that offer needed nutrients. Also make sure that your child has enough calcium and vitamin D. Read nutrition labels on foods. The bottom section of the label contains information on calcium and vitamin D.
Talk with your child’s provider about what products or diet changes may help your child. You may also find it helpful to see a registered dietitian.
When should I call my child's healthcare provider?
The symptoms of lactose intolerance may look like symptoms of other disorders. Have your child checked by a healthcare provider if your child has:
-
Loose stool or diarrhea
-
Swelling or bloating
-
Belly pain
-
Other GI (gastrointestinal) symptoms
Key points about lactose intolerance in children
-
Lactose intolerance is when your child’s body can’t easily break down, or digest, lactose.
 Lactose is a sugar found in milk and milk products.
Lactose is a sugar found in milk and milk products. -
It happens when the small intestine doesn’t make enough of a digestive juice, or enzyme, called lactase.
-
Your child may have uncomfortable symptoms such as bloating, gas, and an upset stomach after eating or drinking milk or milk products.
-
Have your child see a healthcare provider for a diagnosis.
-
You can manage your child’s symptoms by limiting foods that have lactose.
-
Children and teens need calcium and vitamin D for bone growth and health. Read food labels so you can check that your child gets the right amount of these nutrients.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
-
Know the reason for the visit and what you want to happen.

-
Before your visit, write down questions you want answered.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
-
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
-
Ask if your child’s condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if your child does not take the medicine or have the test or procedure.
-
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Lactose Intolerance in Infants & Children: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP
It can be difficult to know whether your infant or child is having symptoms of lactose intolerance or whether he or she may have a milk allergy.
The following frequently asked questions from parents will help you learn more about the common symptoms of lactose intolerance, diagnosis, and treatment options.
Is lactose intolerance the same thing as a milk allergy?
No. Many parents confuse the terms lactose intolerance and milk allergy. While they may share similar symptoms, they are entirely different conditions. Lactose intolerance is a digestive problem, while milk allergy involves the immune system. So, while lactose intolerance can cause a great deal of discomfort, it will not produce a life-threatening reaction such as anaphylaxis.
So, while lactose intolerance can cause a great deal of discomfort, it will not produce a life-threatening reaction such as anaphylaxis.
Milk allergies tend to appear within the first year of life, while an infant's digestive system is still quite immature. Lactose intolerance can start in childhood into adolescence and can become more noticeable into adulthood.
What is lactose?
Lactose is a sugar found in foods that many children love—milk and dairy products, such as frozen yogurt and cheeses. The list of other foods containing lactose is long and includes some breads, cereals, and frozen or canned foods.
Lactose is broken down by the lactase enzyme located in the small intestine—the organ where most food digestion and nutrient absorption takes place. When we eat lactose, lactase breaks lactose down into two simple sugars: glucose and galactose. The body then absorbs these simple sugars into our intestines. When there is a decrease or loss of the lactase enzyme, we cannot break down or absorb lactose. The unabsorbed lactose can lead to symptoms, which is called an intolerance.
The unabsorbed lactose can lead to symptoms, which is called an intolerance.
In addition to milk, what other food products contain lactose?
Lactose is present in many food products and in some medications. Manufacturers also often add milk and milk products to boxed, canned, frozen, packaged, and prepared foods. People who have digestive symptoms after consuming a small quantity of lactose should be aware of the many food products that may contain even small amounts of lactose.
You can check the ingredients on food labels and the nutrition facts to find possible sources of lactose in food products. If a food label includes any of the following words, the product contains lactose:
What are some key symptoms of lactose intolerance?
The symptoms of lactose intolerance depend on the amount of lactose that's consumed. The more lactose your child consumes, the more symptoms he or she will experience. Symptoms of lactose intolerance can occur within minutes to hours after drinking milk or eating dairy products and range from mild to severe based on the amount consumed and the amount tolerated.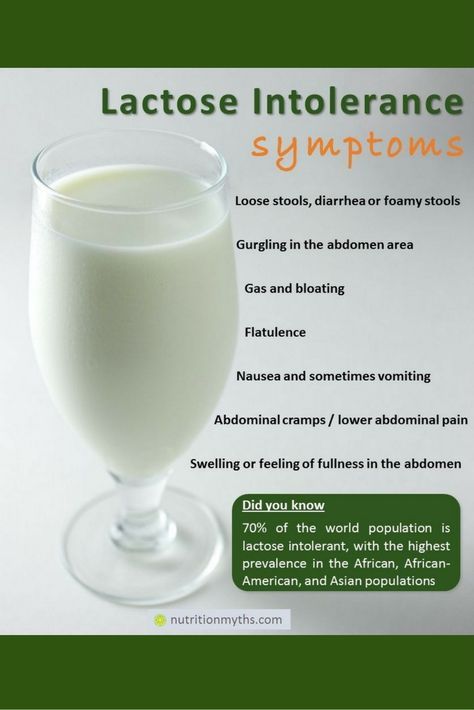 Here are symptoms you should look out for:
Here are symptoms you should look out for:
Nausea
Abdominal pain, cramping, and bloating
Loose stools and gas
Watery diarrhea with gas
If I think my child might be lactose intolerant. How can I tell?
One way to check if your child has trouble digesting lactose is to take all the milk products out of your child's diet for two weeks and to then see if his or her symptoms improve. After two weeks, slowly reintroduce the products in small amounts each day to see if symptoms return. Your pediatrician can also test your child for lactose intolerance with a hydrogen breath test.
I've heard lactose intolerance can sometimes be a temporary side effect when kids are sick. Is that true?
Yes. Lactose intolerance can occur temporarily in children after a viral infection (that is why you may be told to avoid milk with lactose in it during a stomach bug) or it may be seen with conditions that lead to inflammation of the intestines, such as celiac disease.
Can infants be lactose intolerant?
Lactose intolerance is actually not very common in infants and typically only starts showing up after age three in children who were born full-term. All babies are born with lactase in their intestines. As they grow older, the lactase enzyme decreases.
Babies who were born premature are more likely to have a type of lactose intolerance called developmental lactase deficiency. This condition usually lasts only for a short time after birth. However, the majority of premature infants will be able to consume lactose-containing formula and breast milk.
Congenital lactase deficiency is a very rare disorder in which babies can't break down the lactose in breast milk or formula. Genes inherited from parents cause this disorder. This type of intolerance results in severe diarrhea, and if not fed a lactose-free infant formula, those babies could develop severe dehydration and weight loss.
If a mother is lactose intolerant, is it safe for her to breastfeed her baby?
It's perfectly safe to breastfeed your child if you're lactose intolerant. Breastfeeding does not put your baby at greater risk of becoming lactose intolerant, and it has important health benefits for your baby.
How can my child get enough calcium in her diet if milk or lactose are reduced?
If your child has lactose intolerance, he or she can still eat lactose-free dairy products including lactose-free milk, cheese, and yogurts—all are good sources of calcium. In addition, your child can get calcium from dark green leafy vegetables such as spinach, broccoli and kale, nuts (almonds), beans (white beans), fish (sardines, salmon) and calcium-fortified orange juice. If you feel your child is not getting enough calcium, talk with your pediatrician about starting a calcium supplement.
Are soy or almond milks adequate substitutes for children who are lactose intolerant?
There are many milk substitutes that a child with lactose intolerance can drink, including soy, almond, rice, hemp, and oat milk. Soy milk is a popular milk alternative, because it is a good source of calcium and protein. Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
Soy milk is a popular milk alternative, because it is a good source of calcium and protein. Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
How is lactose intolerance diagnosed?
Your pediatrician will take a medical, family, and diet history to help diagnose lactose intolerance in your infant or child. During this discussion, he or she will review your child's symptoms with you.
In some cases, a hydrogen breath test is done to test for lactose intolerance. For the test, your child breathes into a container that measures breath hydrogen level before and after he or she drinks a beverage that contains a known amount of lactose.
 Normally, only a small amount of hydrogen is detectable in the breath when a person eats or drinks and digests lactose. An increase in hydrogen levels is considered a positive test for lactose intolerance.
Normally, only a small amount of hydrogen is detectable in the breath when a person eats or drinks and digests lactose. An increase in hydrogen levels is considered a positive test for lactose intolerance.Pediatricians check acidity in the stools of infants and young children who may be unable to properly do the hydrogen breath test. Acidic stool (low pH) may indicate lactose malabsorption. Another stool test (reducing substances) looks for the presence of glucose in the stool, which signifies undigested lactose.
If your child's symptoms persist, he or she may be referred to a pediatric gastroenterologist (GI) for further evaluation. Depending on the severity of your child's symptoms, the GI may perform an endoscopy to measure lactase levels directly from the intestine. This is done with a biopsy.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age.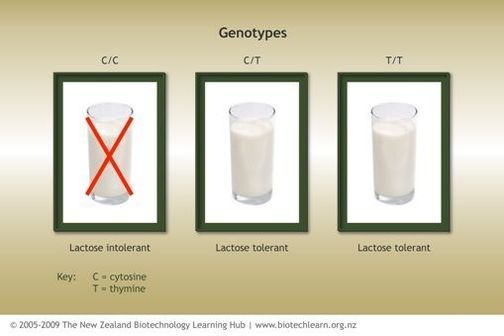 Here is a breakdown of the Recommended Dietary Allowances (RDA) for calcium and vitamin D.
Here is a breakdown of the Recommended Dietary Allowances (RDA) for calcium and vitamin D.
How is lactose intolerance treated?
How lactose intolerance is treated depends on the extent of your child's symptoms. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
To help alleviate symptoms if/when your child consumes lactose-containing food, your pediatrician may recommend an over-the-counter lactase enzyme supplement.
If your child's symptoms are severe and warrant removing all lactose from his or her diet, your pediatrician may refer your child to a registered dietitian. Since dairy is a good source of calcium and vitamin D—which all kids need—a registered dietitian can suggest other foods to provide those nutrients and may suggest vitamin supplements.
Is lactose intolerance a lifelong condition?
In some cases, lactose intolerance is temporary—if lactose intolerance develops after a viral illness or if it is associated with other conditions, like celiac disease. For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
Additional Information & Resources:
Vitamin D: On the Double
Milk Allergy
Infant Allergies and Food Sensitivities
Lactose Intolerance in Infants, Children and Adolescents (AAP Clinical Report)
About Dr. Porto:
Anthony Porto, MD, MPH, FAAP is a board certified pediatrician and board certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr.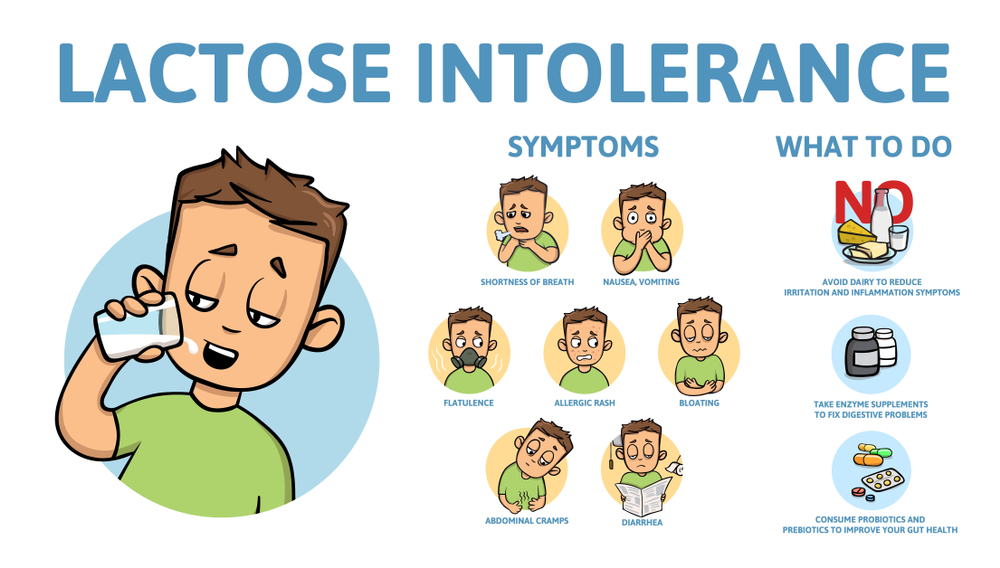 Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Causes and Solutions
When Should You See a Doctor?, Symptoms and Treatment
Many people do not tolerate one or another food, and sometimes even several. One of the most common types of these nutritional problems is lactose intolerance in children. This pathology occurs as a result of the fact that lactose (milk sugar) is not able to break down. Meanwhile, this nutrient is very important for babies under 3 years old. It is necessary for the absorption of trace elements and provides energy needs. In addition, it has a depressing effect on the development of pathogenic microorganisms, is a life-giving environment for the vital activity of lacto- and bifidobacteria.
This pathology occurs as a result of the fact that lactose (milk sugar) is not able to break down. Meanwhile, this nutrient is very important for babies under 3 years old. It is necessary for the absorption of trace elements and provides energy needs. In addition, it has a depressing effect on the development of pathogenic microorganisms, is a life-giving environment for the vital activity of lacto- and bifidobacteria.
Author : Ph.D. Zoryana Tomkiv
Lactose intolerance (lactase deficiency) is a pathological process in which dairy products are no longer digested. The problem arises in the first months of life, since the main product that the baby eats at this time is breast milk. With an increase in its consumed amount, the severity of clinical manifestations increases. This problem also occurs in adults.
Speaking about the inability to digest dairy products, it should be noted that the body may not tolerate cow's milk protein. However, in this case, we are no longer talking about lactose intolerance, but about an allergy to cow's milk protein.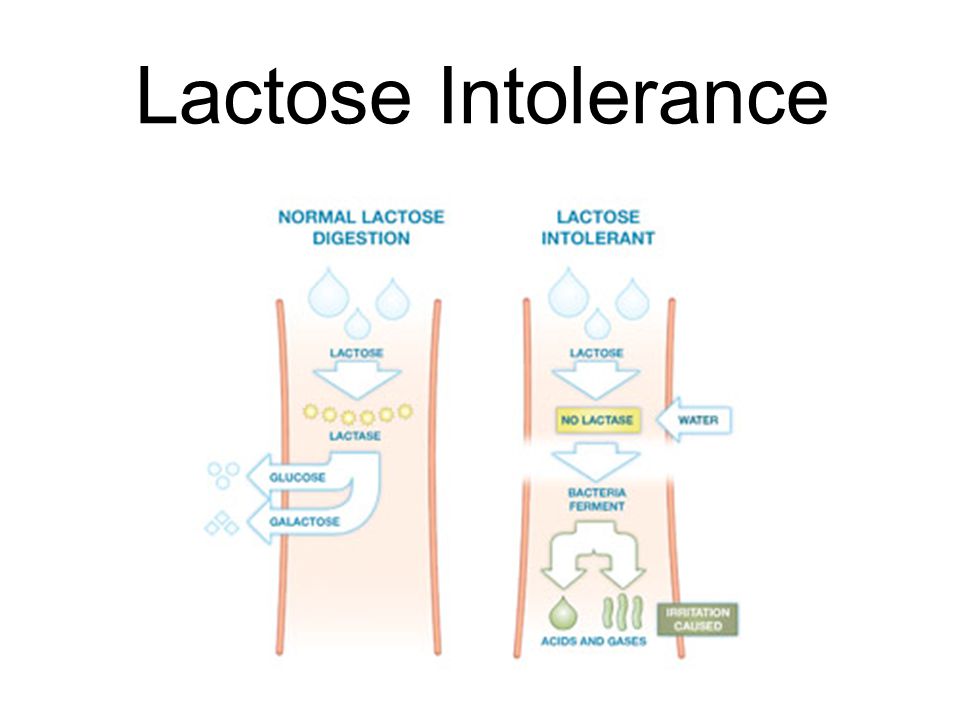
Why babies develop lactose intolerance
Our ability to digest milk sugar is directly dependent on the activity of the enzyme that is involved in this process ¾ lactase. It is he who breaks down lactose (milk sugar) in our small intestine into simpler carbohydrates, which are then absorbed into the bloodstream and used by the body.
Lactase first begins to form in the baby's body at 3-4 months of fetal development, and from 6 months it begins to become more active. Before childbirth, the activity of this enzyme increases dramatically, and its level at the birth of a baby becomes higher than in adults. Lactase remains highly active during the entire period of breastfeeding. A gradual decrease in its activity is observed already when the child switches to adult food, on average, at the age of 3-5 years and is a natural consequence of a change in the baby's diet.
If a baby is diagnosed with lactase deficiency, then it can be of two types: primary or secondary.
In turn, primary lactose intolerance, depending on the mechanisms of development, can be:
- congenital;
- constitutional;
- temporary (transient).
Congenital alactasia (lack of lactase) is characterized by the fact that there is no enzyme that breaks down lactose in the body at all, but such cases are very rare and have a genetic nature.
With constitutional lactase deficiency, a sufficient amount of lactase is secreted in the intestine, but its activity is reduced. As a rule, the activity of the enzyme begins to decrease after complementary foods are introduced, that is, it directly depends on the type of nutrition characteristic of the child during life. This type of lactose intolerance is common in older children as well as adults. It is associated with genetic predisposition and belonging to a particular ethnic group.
Insufficiently mature newborns, as well as in babies born prematurely, transient or temporary lactase deficiency may occur.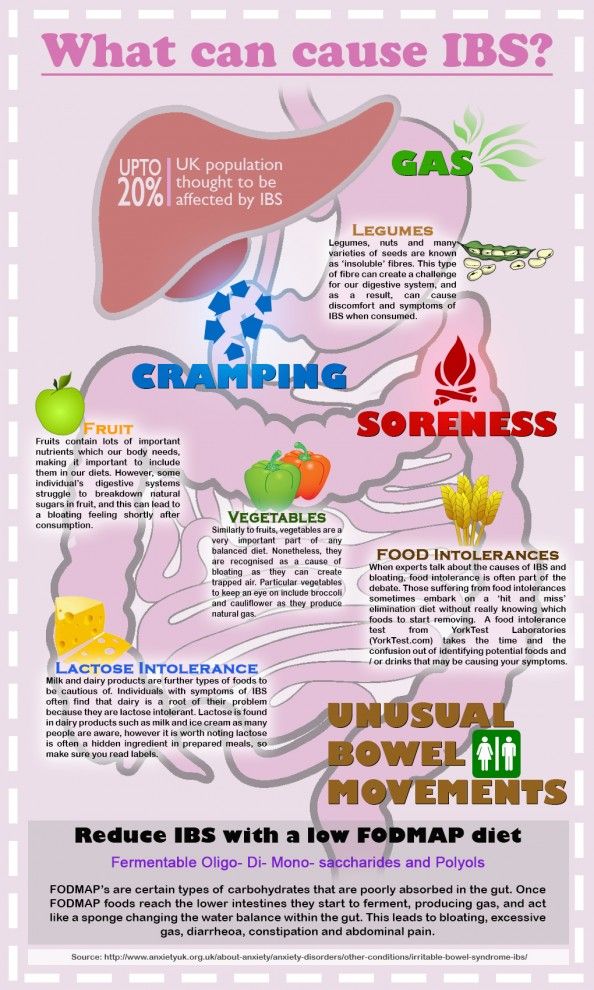 The reason for this phenomenon is that lactase has not yet become active enough by the time of birth to break down all the milk sugar that enters the baby's body with food.
The reason for this phenomenon is that lactase has not yet become active enough by the time of birth to break down all the milk sugar that enters the baby's body with food.
Secondary lactose intolerance in a child occurs against the background of some other pathology in which enterocytes (epithelial cells of the small intestine) are damaged. Often the functioning of these cells is disturbed by intestinal infections, allergies and other inflammatory diseases, as well as pathological processes in which atrophic changes occur in the small intestine. In this case, the secretion of lactase is disturbed, which provokes the development of insufficiency.
In any case, both with insufficient production of the lactase enzyme and with its low activity, undigested lactose from the small intestine passes into the large intestine, where it plays the role of a nutrient medium for intestinal flora microorganisms. The result of this is increased fermentation, gas formation and acidification of the intestinal contents.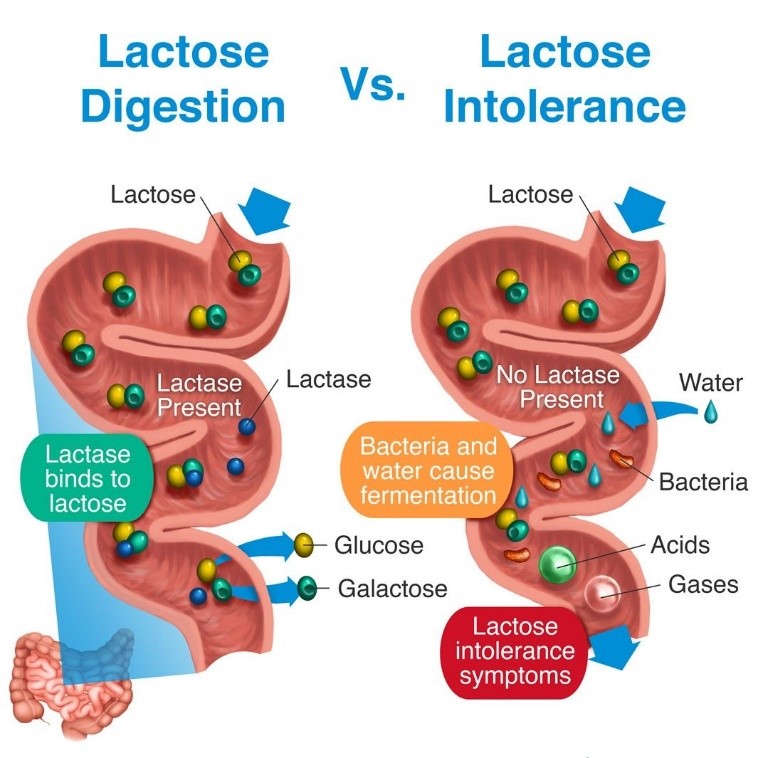
Symptoms
In order to understand that an infant is lactose intolerant, one must first pay attention to the specific manifestations of the disease.
Symptoms of lactase deficiency in infants are as follows:
- Stools are thin, frothy, yellow. The chair can be frequent (8-10 times a day) and rare. Feces have a sour smell and look like yeast dough. When settling in a glass container, after some time it separates into 2 fractions - dense and liquid. This is important to consider when using diapers: the liquid part is absorbed, so you can miss this violation.
- Intestinal motility is enhanced.
- Baby is restless during and after feeding.
- There is bloating, intestinal colic, flatulence.
- Regurgitation occurs, vomiting is possible.
- The baby is not gaining weight well and may even lose it.
A child with this pathology does not suffer from appetite. Often he sucks greedily, but after a while he pulls his legs up to his stomach, starts crying and throws his breast.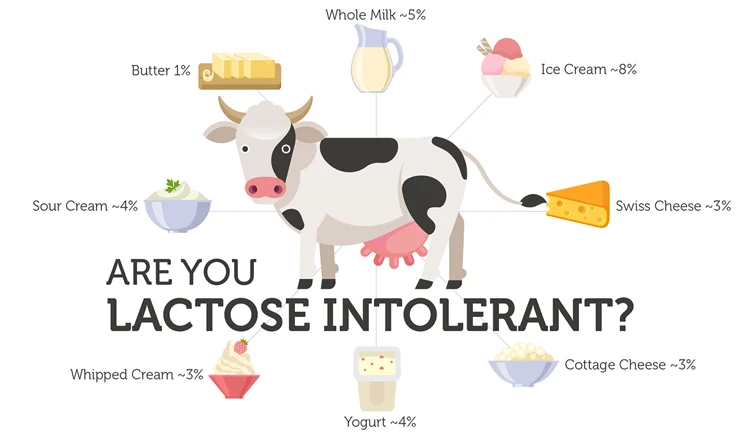 In the first weeks of life, the disease may be asymptomatic. Its manifestations intensify with an increase in the consumption of milk.
In the first weeks of life, the disease may be asymptomatic. Its manifestations intensify with an increase in the consumption of milk.
In older children, often after 5 years, the signs of lactose intolerance are less pronounced, since milk is no longer the dominant food in their diet. The intestinal microflora of the child gradually adapts to the intake of lactose, due to which the symptoms also decrease and can only appear after taking a large amount of milk.
How does lactose intolerance manifest itself in an infant if it has developed a secondary type? Clinical manifestations are supplemented by regurgitation, the presence of greens in the feces, mucus in large quantities, undigested lumps of food, and expressed anxiety. After feeding, rumbling is felt along the intestines.
Diagnosis of lactase deficiency in the newborn
The diagnosis of lactase deficiency is made after examination and observation of clinical signs in the infant and is confirmed by additional tests, which may include: The presence of carbohydrates in the stool is determined, as well as the pH of the feces (as a rule, with this pathology it is less than 5. 5). The test is carried out without delay on a fresh portion of stool with sufficient lactose intake.
5). The test is carried out without delay on a fresh portion of stool with sufficient lactose intake.
In certain cases, additional tests may be ordered to make a correct diagnosis.
In addition, the so-called elimination diet effect is important in diagnosing lactase deficiency in infants: that is, if the child is transferred to a lactose-free diet, the symptoms of the disease will decrease, and eventually disappear altogether.
Treatment of lactose intolerance in children
Lactose intolerance is tested before treatment is started in infants. With its positive result, the amount of lactose in the diet is reduced or, if possible, eliminated altogether. At the same time, other symptoms are corrected. This tactic works with primary lactase deficiency.
If secondary lactose intolerance is diagnosed in children, the disease that caused the condition must first be treated. The amount of lactose consumed is temporarily reduced. During the period of treatment of the primary disease, the damaged intestinal mucosa is restored, and the secretion of lactase is getting better.
The treatment of lactase deficiency is difficult in that the most effective method is the elimination of milk from the diet. As soon as this product is not in the diet, the condition returns to normal. This is a good option for older children, but not for babies who need it, because proper feeding helps the baby develop normally. When we talk about lactose intolerance, proper nutrition of the child is, literally, the key to successful treatment.
When we talk about lactose intolerance, proper nutrition of the child is, literally, the key to successful treatment.
For those babies who are fed mother's milk, reducing its amount is undesirable, so the missing enzyme is added directly to it. To do this, the doctor individually calculates the dose of lactase, before feeding it is preliminarily diluted in expressed breast milk, left for the fermentation process for 5-10 minutes and then given to drink to the baby. After that, feeding is carried out according to age needs. Sometimes a problem can arise if a baby who is accustomed to breastfeeding refuses to take the bottle.
If lactase deficiency occurs in an infant who is bottle-fed, the problem is solved by using low-lactose and lactose-free mixtures. The attending physician will help you choose an infant formula with the maximum amount of lactose that does not cause negative symptoms in the newborn. If the signs of the disease are severe, the baby is transferred to a lactose-free mixture, which does not contain lactose at all.
For secondary lactose intolerance due to food allergy, food intolerance or malabsorption, your doctor may prescribe formulas based on complete protein hydrolysis to combat the underlying disorder. After that, the diet is gradually expanded by adding lactose to the diet of the baby.
Symptomatic therapy may also be needed, in which multivitamin complexes, pancreatic enzymes, drugs for the correction of dysbacteriosis and water and electrolyte balance are prescribed.
A special analysis will help to control the correctness of therapy, in which the level of carbohydrates in the feces is determined. With any form of lactose intolerance, such control is carried out regularly, and in accordance with its results, the baby's diet is adjusted.
With the right choice of treatment, the child's ability to absorb lactose from food gradually increases. Therefore, most infants with temporary lactase deficiency can return to milk nutrition by 3-4 months.
Diet for lactose intolerance
Lactose intolerance in a child requires a special lactose-free or low-lactose diet. Older children can eat vegetables, fish, meat, eggs, fats, fruits, sugar. To date, there are special lactose-free products. A wide range of such products will allow you to organize a complete diet for the child, if the baby needs to introduce complementary foods. Therefore, it is worth stopping your choice on them.
Older children can eat vegetables, fish, meat, eggs, fats, fruits, sugar. To date, there are special lactose-free products. A wide range of such products will allow you to organize a complete diet for the child, if the baby needs to introduce complementary foods. Therefore, it is worth stopping your choice on them.
Older children with this pathology completely exclude milk (not only whole, but also condensed), as well as various confectionery products that contain milk fillers.
Small amounts of fermented milk products, especially yoghurts, whey-free cottage cheese, butter, hard cheeses (<1% lactose), can be consumed in small amounts in older children if they do not cause signs of lactase deficiency. However, in any case, the tolerance of the child's body to certain products is determined individually, as well as the duration of such a diet.
- When to see a doctor?, Symptoms and treatment Functional dyspepsia in children: symptoms and treatment
- When to see a doctor?, Symptoms and treatment Dysentery in children: symptoms and treatment
- When to see a doctor see a doctor?, Symptoms and treatment Gastritis in children: symptoms and treatment
- When to see a doctor?, Symptoms and treatment Early signs of appendicitis in children
- When to see a doctor?, Digestive problems, Symptoms and treatment Intestinal infection in children: symptoms, treatment, menu and diet
- When to see a doctor?, Symptoms and treatment Intestinal obstruction in children: symptoms and treatment
- When to see a doctor?, Symptoms and treatment Lactose intolerance in children: symptoms and treatment
- All when to see a doctor?
Lactase deficiency in infants: symptoms and diagnosis
Signs of lactase deficiency in infants should be known to parents, because this will allow them to suspect this condition in a timely manner, identify its cause and improve the condition of the baby.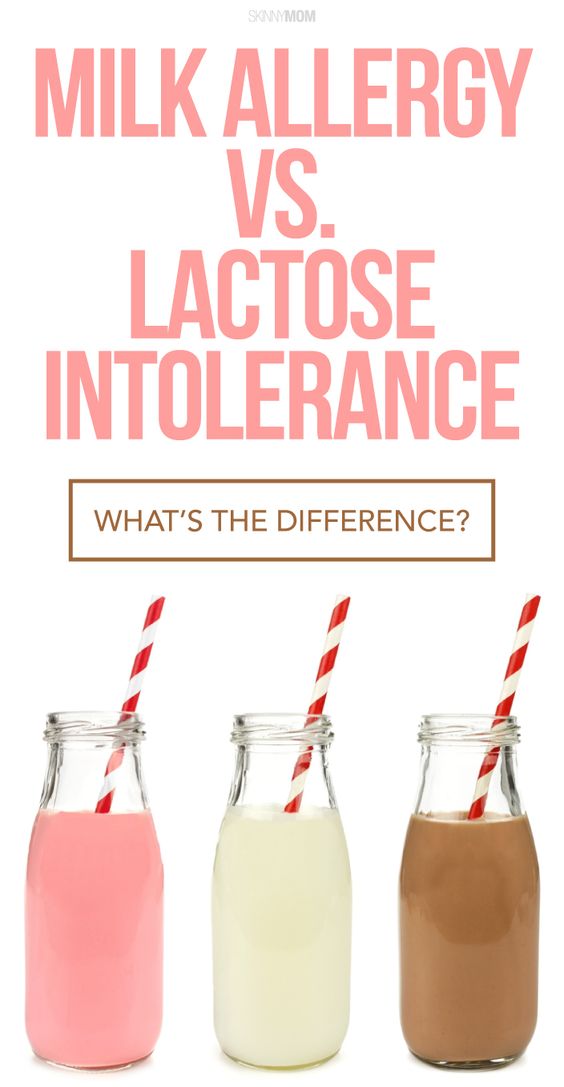
Signs of lactose intolerance
Signs of lactase deficiency in a child are diverse. This is a stool with a large water spot and a sour smell, bloating, rumbling, abdominal pain (colic). One of the most common symptoms that worries parents is frequent loose stools in a baby. It is watery, frothy and has a sour smell. It should be remembered that the younger the child, the more frequent his stool, and this is completely normal. So if the baby is developing well and feels good, and his feces are normal, you should not think that these are signs of lactose intolerance in newborns.
Sometimes lactase deficiency in newborns is accompanied by poor weight gain and growth. This is due to the fact that the carbohydrates necessary for the child do not enter the body, and the baby may lack nutrients.
If the baby quickly grew out of the recently purchased sliders and sleepsuits, and his cheeks and handles are round and plump, you should not suspect lactase deficiency in the child.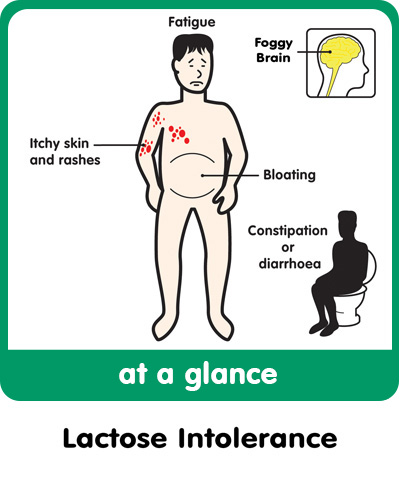
Intestinal colic may be present in children with lactose intolerance. After eating, the child will experience bloating, anxiety, crying. These signs usually appear on the 3-6th week of a baby's life. This is probably due to an increase in milk consumption by an older baby.
The mechanism of such manifestations of lactose intolerance as intestinal colic, bloating and rumbling is as follows. Carbohydrates that are not digested due to the absence or lack of the lactase enzyme continue their movement through the intestines. In the colon, they are exposed to intestinal microflora, resulting in the formation of an excess of gases (hydrogen, methane, carbon dioxide). Gas stretches the walls of the intestines, causing bloating, pain and increased intestinal peristalsis. Violation of the normal chemical composition of intestinal contents can lead to disturbances in the composition of the intestinal microflora.
When should you not think about lactase deficiency?
Quite often in recent years, when there are problems with digestion, children are diagnosed with lactose intolerance.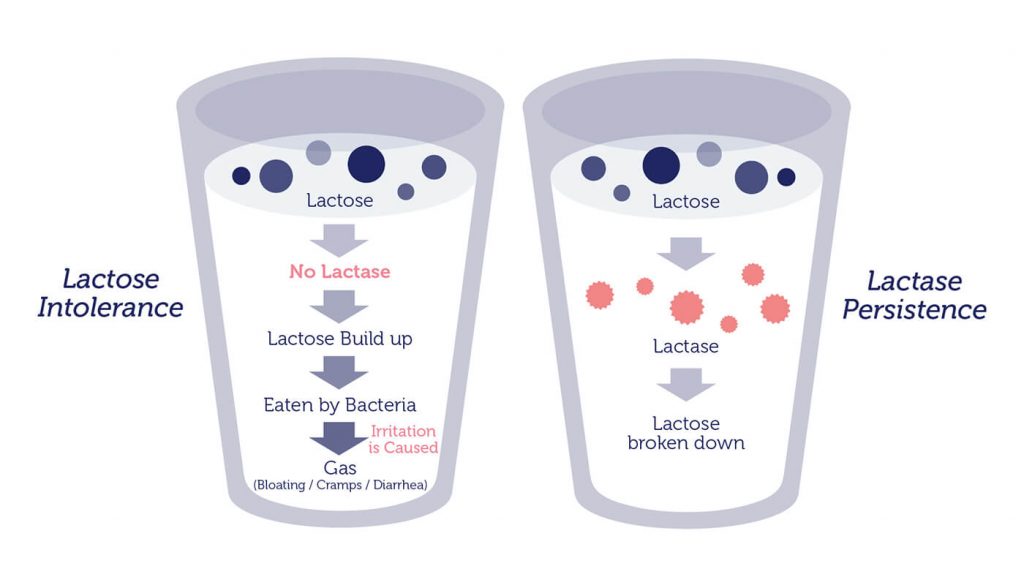 However, this is not always true. As mentioned above, the frequency of stool in infants is individual. Frequent or rare stools are not in themselves a sign of lactase deficiency in a child. The symptoms of this pathology are multiple.
However, this is not always true. As mentioned above, the frequency of stool in infants is individual. Frequent or rare stools are not in themselves a sign of lactase deficiency in a child. The symptoms of this pathology are multiple.
Important!
Sometimes regurgitation is mistaken for signs of lactose intolerance by parents. But even if regurgitation is frequent and plentiful, it is unlikely that this is lactase deficiency - the symptoms in children with this pathology are associated with the work of the intestines, and not the esophagus or stomach.
How to identify lactose intolerance
The diagnosis of lactose intolerance usually begins with an organoleptic evaluation of feces. Unformed, watery, frothy yellow or green feces with a sour smell testify in favor of this pathology. In a chemical study, the reaction of feces is acidic (pH less than 5.5).
Another test method is to determine the content of carbohydrates in feces. Exceeding their value by 0.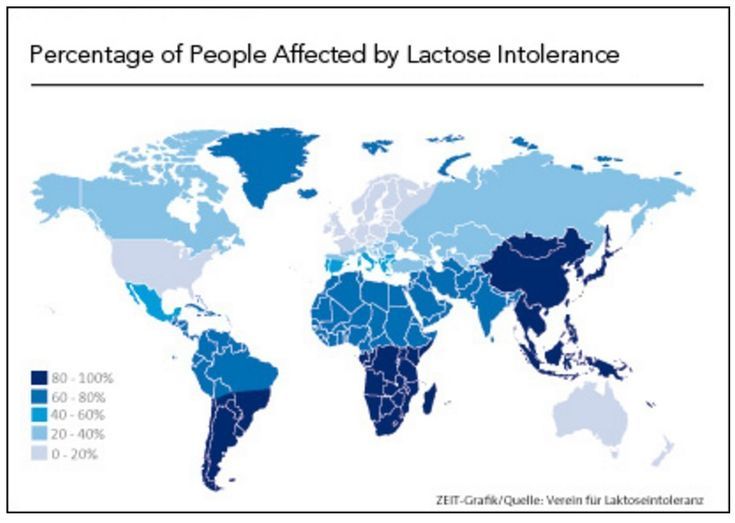 25% is typical for lactase deficiency. Despite the widespread use, this method is not the most accurate, since it does not allow you to determine which carbohydrates are present in the feces.
25% is typical for lactase deficiency. Despite the widespread use, this method is not the most accurate, since it does not allow you to determine which carbohydrates are present in the feces.
Important!
Whenever lactose intolerance is suspected, a specialist should be consulted. He will prescribe examinations that will allow you to say if the child has lactose intolerance, or if the symptoms are not associated with this condition.
Other methods are used in difficult cases. For example, a specific breath test based on determining the concentration of hydrogen in exhaled air after a load of lactose. The advantage of this method is its simplicity, the disadvantage is the possibility of false positive results and the impossibility of determining the degree of lactase deficiency.
Lactose curve is another test for lactose intolerance. Normally, lactose, under the action of the lactase enzyme, breaks down into simpler sugars, in particular, glucose. Subsequently, glucose is absorbed through the intestinal wall and enters the bloodstream.