Varicose vein pain during pregnancy
Bulging, Painful Leg Veins During Pregnancy: Can they be treated?
CONTACT US
Share This Post
Share on facebook
Share on twitter
Share on email
Thursday, 6 October 2016
Some pregnancy symptoms are minor, such as backache and fatigue. Others are more serious, like bleeding, severe nausea/vomiting, preeclampsia or preterm labor. In light of these symptoms, leg vein problems can seem to be the last straw.
Since there are so many pregnancy risks associated with various medical treatments, prescription drugs, surgeries and even certain vitamins and herbs that it may seem like an impossible feat to treat your leg veins during pregnancy. We’re here to tell you that’s not the case.
Why Varicose Veins Develop In Pregnancy
While any vein can become varicose, the veins most commonly affected by this condition are found in the legs and feet. Although pregnancy increases the volume of blood in your body, it also slows the blood flow from the legs to the pelvis. This change in circulation is designed to support the growing fetus and prepare the body for labor and delivery, but it can produce the unfortunate side effect of enlarged veins in your legs.
While some women don’t get enlarged veins until later in pregnancy, other women develop these troublesome veins near the beginning of pregnancy due to hormone fluctuations. Varicose veins that develop during pregnancy often improve without medical treatment within 6 to 12 weeks after delivering the baby. The more babies the more likely some of the varicose veins will persists. This problem also tends to be hereditary; if your mother had them, you will most likely develop them as well.
Treating Leg Veins During Pregnancy: Dos And Don’ts
While varicose veins may not be attractive, they don’t pose a health risk to you or your baby in and of themselves. However, they can lead to considerable pain. In most cases, the veins will disappear after the baby is born and your hormones have dropped to normal levels. Treating leg veins during pregnancy is not an exact science, but there are some things you can do to help.
In most cases, the veins will disappear after the baby is born and your hormones have dropped to normal levels. Treating leg veins during pregnancy is not an exact science, but there are some things you can do to help.
Improve Blood Flow And Circulation
Keep your blood moving by getting off your feet whenever you can. If you have young children requiring care, consider hiring a babysitter to give you a chance to rest for a few hours.
If you need to stand for an extended period of time, put one foot on a low stool. Alternate your legs to give each one a change of position. Flex your ankles occasionally to improve blood flow. If you have a habit of crossing your legs, now is the time to break it. You may lower the risks of spider veins this way as well.
Work Your Muscles
One of the key steps to promote healthy veins, blood flow and preventing varicose veins during pregnancy is exercise. If you can, take at least one walk per day. Better still, take several walks.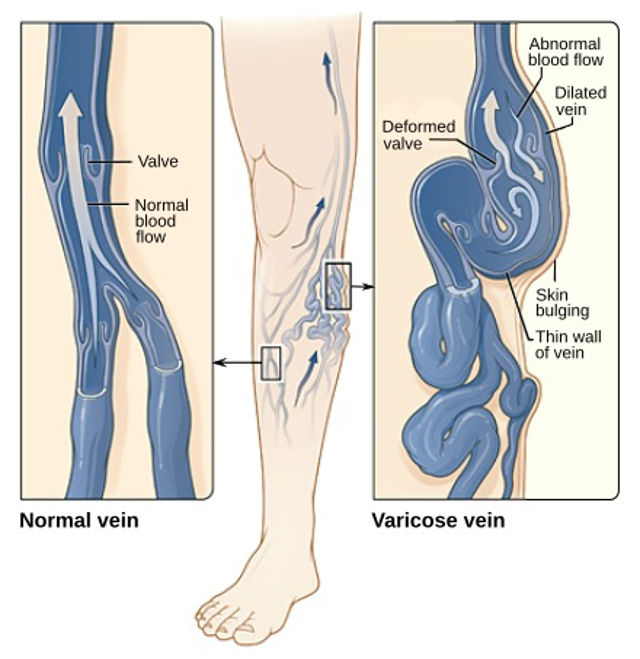 If you don’t want to walk, do some other form of low-impact exercise that increases circulation. Swimming and light stretching are both excellent choices, but be sure to consult with your OB/GYN first.
If you don’t want to walk, do some other form of low-impact exercise that increases circulation. Swimming and light stretching are both excellent choices, but be sure to consult with your OB/GYN first.
Choose Your Wardrobe Wisely
Wear clothing that is loose and comfortable. If your underwear is binding or tight, replace it with something less snug. Avoid tight belts and socks with tight elastic tops. Footwear should be snug to prevent stumbling, but should not be tight in any way. Of course, stay away from stiletto heels until you’ve given birth.
Compression Is Key
A pair of compression stockings is useful when it comes to pregnancy-caused varicose veins. Wearing these socks consistently is one of the most effective ways to provide support. Medical grade graduated compression hosiery provide the strongest pressure at the ankles and gradually decrease in pressure as they rise. You may want to keep wearing them even after pregnancy and until your circulation and hormones have returned to normal. Compression hose can also decrease other pregnancy-related symptoms, such as swollen feet and tired, aching legs.
Compression hose can also decrease other pregnancy-related symptoms, such as swollen feet and tired, aching legs.
Talk To A Vein Specialist
To ensure that you don’t develop any varicose vein complications during or after your pregnancy, be sure to visit a phlebologist. Phlebologists, or vein specialists, treat and diagnosis vein disorders and will be able to spot a complication before it becomes serious.
The most likely vein symptoms during pregnancy include: swelling, pain, bleeding or a superficial blood clot in the varicose vein. Because your baby’s health is a top concern, consult with your OB/GYN before beginning any type of treatment plan for venous disease. It is generally not advisable to receive treatment for varicose veins during pregnancy that involves any incisions or injections; however, notify your OB/GYN or phlebologist immediately if your varicose veins and the surrounding area become warm, red, very painful or begin to bleed.
Managing Discomfort And Pain From Leg Veins In Pregnancy
Along with support hose, there are several other things you can do to help with the discomfort and pain caused by leg veins. During pregnancy, the uterus exerts pressure on the inferior vena cava. This vein is responsible for transporting blood from the legs and feet to the heart. If the vena cava is restricted in some way, blood will pool in the feet and legs, leading to varicose veins. This is why your OB/GYN likely advised you to lie on your left side when resting or sleeping, as it prevents excess pressure on this vein. Drinking plenty of water can also help your body maintain a proper fluid balance.
During pregnancy, the uterus exerts pressure on the inferior vena cava. This vein is responsible for transporting blood from the legs and feet to the heart. If the vena cava is restricted in some way, blood will pool in the feet and legs, leading to varicose veins. This is why your OB/GYN likely advised you to lie on your left side when resting or sleeping, as it prevents excess pressure on this vein. Drinking plenty of water can also help your body maintain a proper fluid balance.
Other options for treating leg veins during pregnancy include maintaining the weight recommended by your OB/GYN and avoiding long periods of sitting or standing. If your veins continue to bother you after you have given birth, you will benefit from a consultation with a vein specialist.
Safe Treatment Options After Pregnancy
Although self-care and compression stockings may work for some people and varicose veins developed during pregnancy often resolve on their own after giving birth, some patients will require treatment. In these cases, we offer treatments for venous disease that are non-surgical and performed right in our practice without ever having to set foot in an operating room.
In these cases, we offer treatments for venous disease that are non-surgical and performed right in our practice without ever having to set foot in an operating room.
Endovenous thermal ablation was the first endovenous minimally invasive alternative to vein stripping. It is the most common method used to treat saphenous reflux at this time. The procedure uses thermal radiofrequency energy to close or collapse the unhealthy saphenous vein reflux. It is performed in an office setting under local anesthesia with ultrasound guidance.
VenaSeal is our newest FDA approved treatment for varicose veins that doesn’t require surgery or heat to treat the affected veins. A small IV catheter is inserted into the unhealthy saphenous vein. Through the catheter, a surgical adhesive is injected to seal the affected vein shut. Patients are able to walk out with just a regular bandaid. It’s that simple and minimally invasive.
Varithena is a non-surgical injectable foam treatment specifically indicated for the great saphenous vein and surrounding veins.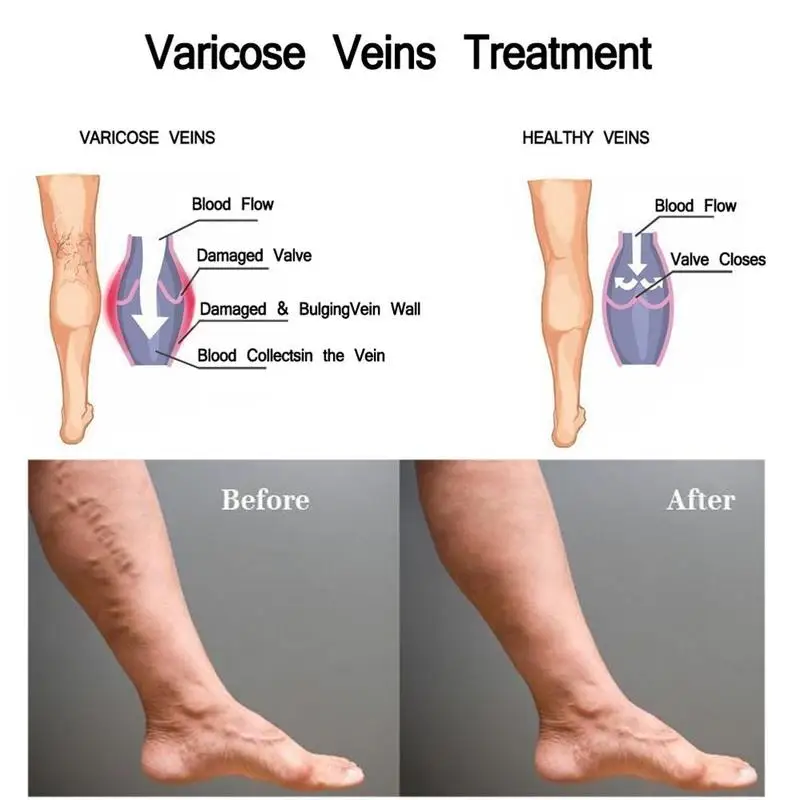 Unlike VenaSeal, which seals the vein shut, Varithena foam channels through the vein, creating a chemical reaction that causes the vein to scar shut. Patients feel no pain and don’t require sedation during this procedure but do need to wear compression after the procedure. Additional sessions may be needed to complete the treatment.
Unlike VenaSeal, which seals the vein shut, Varithena foam channels through the vein, creating a chemical reaction that causes the vein to scar shut. Patients feel no pain and don’t require sedation during this procedure but do need to wear compression after the procedure. Additional sessions may be needed to complete the treatment.
Ambulatory phlebectomy is used to treat large bulging varicose veins on your legs. It is an outpatient procedure using local anesthesia to numb the area, allowing the problem veins to be removed through micro-incisions in the skin that do not require stitches and heal with minimal scarring.
Sclerotherapy uses a liquid chemical injected into the spider vein. The sclerosant chemically scars the wall of the unhealthy vein, causing it to close off. This procedure is commonly used to treat small varicose veins and spider veins.
Treating Leg Veins During Pregnancy And Postpartum In Middle Georgia
For exemplary varicose vein treatment in Middle Georgia, consider Vein Specialists of the South. Dr. Kenneth Harper has evaluated more than 14,000 patients since 2000, and is a leader in comprehensive vein care. We offer a wide variety of treatment options, including sclerotherapy, VenaSeal, Venefit / Radiofrequency Closure and ambulatory phlebectomy. Please schedule a consultation with Dr. Harper and our team of vein specialists and learn which varicose vein treatment is best for you.
Dr. Kenneth Harper has evaluated more than 14,000 patients since 2000, and is a leader in comprehensive vein care. We offer a wide variety of treatment options, including sclerotherapy, VenaSeal, Venefit / Radiofrequency Closure and ambulatory phlebectomy. Please schedule a consultation with Dr. Harper and our team of vein specialists and learn which varicose vein treatment is best for you.
Over 18,000 Procedures Performed
Dr. Kenneth Harper, founder of Vein Specialists of the South, has evaluated more than 22,000 patients and performed over 18,000 procedures since 2000. Dr. Harper is a leader in comprehensive vein care, having focused on diagnosis and treatments for varicose veins, spider veins, venous ulcers, and leg swelling since 1997.
Learn More
BETTER VEINS.
BETTER LIFE.® PLAN
It’s just 3 easy steps…
SCHEDULE A CONSULTATION
HAVE YOUR LEGS EVALUATED
ENJOY BETTER LOOKING BETTER FEELING LEGS
SCHEDULE A CONSULTATION
HAVE YOUR LEGS EVALUATED
ENJOY BETTER LOOKING BETTER FEELING LEGS
REQUEST YOUR CONSULTATION >>
PATIENT REVIEWS
*Individual Results May Vary
★★★★★ 5/5
Everybody was so friendly.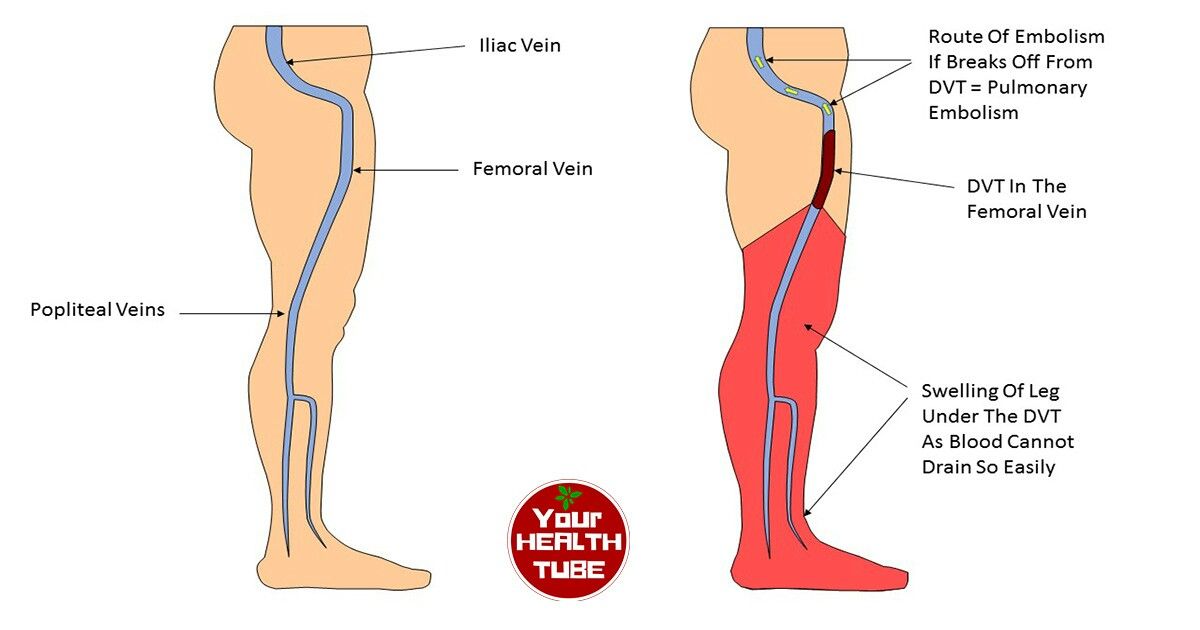 I trust Dr. Harper. I feel like I did the right thing. I have more energy and am feeling better. I do believe that this has helped me. Go to your doctor, get a recommendation and talk with Dr. Harper and staff. Trust their recommendations and follow through with the procedure. I have nothing but good things to say and am so thankful.*
I trust Dr. Harper. I feel like I did the right thing. I have more energy and am feeling better. I do believe that this has helped me. Go to your doctor, get a recommendation and talk with Dr. Harper and staff. Trust their recommendations and follow through with the procedure. I have nothing but good things to say and am so thankful.*
Dr. Harper and the staff are great. They make you feel extremely comfortable and they are very professional. I have had 5 procedures over the previous years and I have been very satisfied and happy with the results. I would recommend anyone who suffers with leg discomfort or varicose veins to go in for a visit.*
Very friendly and knowledgeable staff. Took great lengths to ensure I knew everything that was going on (before and during) and always made me feel extremely comfortable and at ease.*
READ MORE
PrevPreviousAre your fashion choices damaging your vein health?
NextBlondes vs BrunettesNext
More To Explore
Are embarrassing Varicose Veins keeping you from wearing shorts?
- Understand the underlying cause of varicose veins.

- Determine if your unsightly varicose veins could be more than a cosmetic concern.
- Learn what to expect at your vein evaluation.
- Choose the best treatment options to meet your needs.
Ready to learn how we can help you enjoy Better Veins for Life®?
Complete the information below to receive a FREE resource about varicose veins.
By signing up for this content, you will receive a limited series of e-mails on this subject matter and how we can help.
Hemorrhoids and Varicose Veins in Pregnancy
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What are hemorrhoids and varicose veins?
Hemorrhoids and varicose veins might seem to be two different, unrelated problems, but they're actually quite similar. And many women, especially those in the third trimester of pregnancy, have them.
Both hemorrhoids and varicose veins are swollen, twisted veins. These veins are often in the legs, but they also can form in other parts of your body. When they form in the rectum, they're called hemorrhoids.
What causes hemorrhoids and varicose veins in pregnancy?
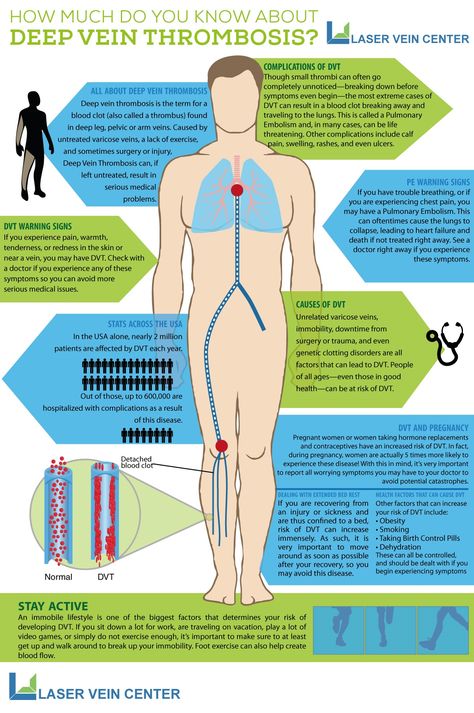
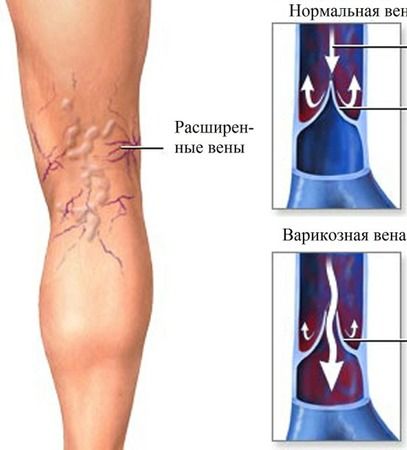
Normally, veins have one-way valves to help keep blood flowing toward the heart. Pressure or weakening of these valves allows blood to back up and pool in the veins. This causes them to enlarge and swell. Hemorrhoids result when rectal veins enlarge. Varicose veins occur when veins of the legs swell.
Many changes in pregnancy can increase the risk of hemorrhoids and varicose veins, such as:
- Increased blood volume, which enlarges the veins
- The heavy weight of the growing baby, which presses on the large blood vessels in the pelvis, altering blood flow
- Hormone changes affecting blood vessels, which can slow the return of blood to the heart and cause the smaller veins in the pelvis and legs to swell
Hemorrhoids can get worse with pushing or straining, especially with constipation.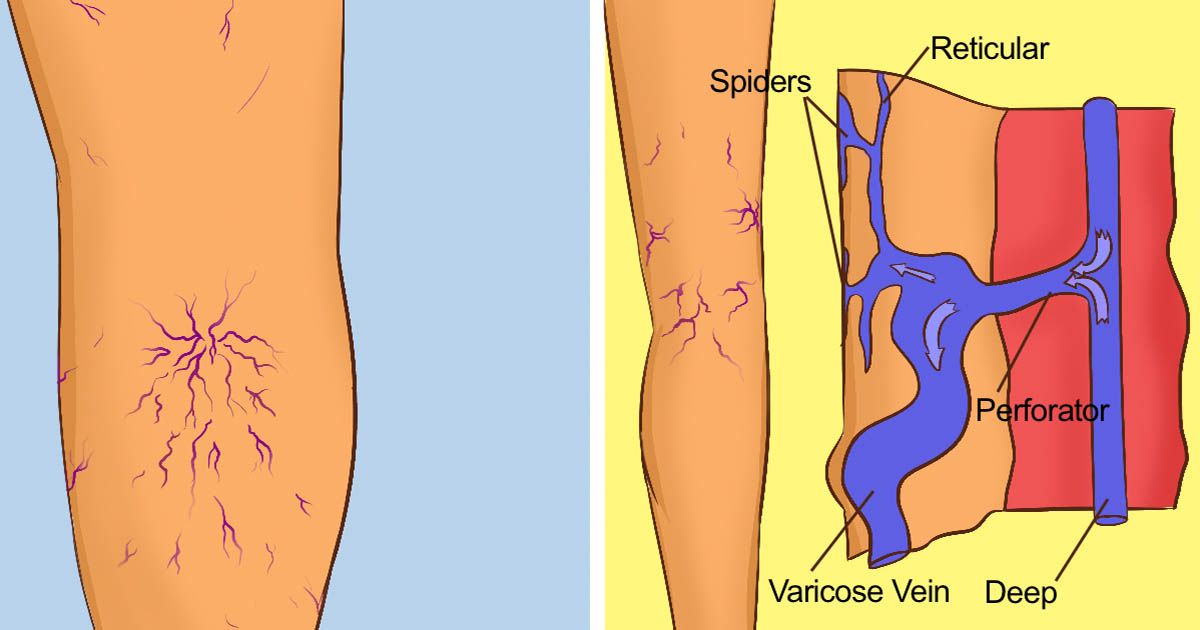 Being overweight and having hemorrhoids before pregnancy can also make them worse. Pushing during delivery tends to worsen hemorrhoids, too.
Being overweight and having hemorrhoids before pregnancy can also make them worse. Pushing during delivery tends to worsen hemorrhoids, too.
Varicose veins tend to run in families. Sitting or standing in one position for a long time may force the veins to work harder to pump blood to the heart. This can result in swollen, varicose veins and can also worsen existing hemorrhoids. Varicose veins can also occur in a woman's genital area.
What are the symptoms of hemorrhoids and varicose veins in pregnancy?
Hemorrhoids can be internal, forming inside the rectum, or external, located on the outside, around the anal opening. Internal hemorrhoids can sometimes bulge out through the anal opening. The most common symptom is bright red blood passed with a bowel movement. External hemorrhoids can be painful or itch and may bleed if irritated by straining or wiping.
Varicose veins often look like large, twisted, raised blue or purple veins on the legs–often on the backs of the calves or inside the legs. They may cause mild swelling in the ankles and feet or aching, heaviness, or throbbing in the legs. They can also cause leg cramps. If varicose veins occur in the genital area, they also appear as large, twisted, raised veins.
How are hemorrhoids and varicose veins in pregnancy diagnosed?
Your healthcare provider will examine your legs or rectal area to check for varicose veins or hemorrhoids.
How are hemorrhoids and varicose veins in pregnancy treated?
Hemorrhoids in pregnancy are a short-term problem, and they get better after your baby is born. Still, there are some things you can do to relieve the discomfort:
- To relieve pain, sit in a tub or sitz bath several times a day in plain, warm water for about 10 minutes each time.
 When you use a tub bath, don’t fill the tub all the way. Just put in enough warm water to sit in. That will direct blood flow to your rectum.
When you use a tub bath, don’t fill the tub all the way. Just put in enough warm water to sit in. That will direct blood flow to your rectum. - Use ice packs or cold compresses to reduce swelling.
- Ask your healthcare provider about creams or other medicines, such as stool softeners, that are safe to use during pregnancy.
It’s important to prevent constipation by including lots of fiber and fluids in your diet.
Also try not to strain with bowel movements, and avoid sitting for a long time. Regular Kegel exercises can help improve muscle tone, These exercises involve squeezing and relaxing the muscles in your vaginal and rectal area.
Most varicose veins that develop during pregnancy get better within the first year after birth.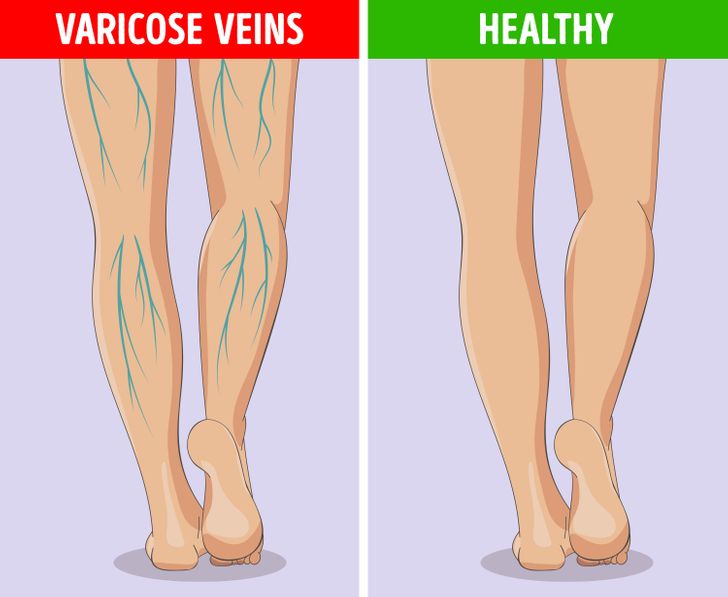 But for now, limit standing or sitting for a long time without a break, and try not to cross your legs. Also try to raise your legs and feet whenever you’re sitting or lying down.
But for now, limit standing or sitting for a long time without a break, and try not to cross your legs. Also try to raise your legs and feet whenever you’re sitting or lying down.
Avoid tight clothing around your waist, thighs, and legs, as it can worsen varicose veins.
Be sure to check with your provider if your symptoms worsen or you have excessive bleeding from hemorrhoids. And remember that these problems are usually short-term and get better after delivery with time and treatment.
What can I do to prevent hemorrhoids and varicose veins in pregnancy?
The best way to help prevent hemorrhoids during pregnancy is to prevent constipation. If you're constipated, don't strain during bowel movements.
Steps to help prevent varicose veins are the same as those used to decrease symptoms:
- Don't stand still or sit for long periods of time.
- Prop your feet up whenever possible.
- Don't wear tight clothes.
Key points about hemorrhoids and varicose veins in pregnancy
- Both hemorrhoids and varicose veins are swollen, twisted veins. These veins are often in the legs, but when they form in the rectum, they're called hemorrhoids.
- Many normal changes in pregnancy can increase the risk for hemorrhoids and varicose veins.
- Hemorrhoids and varicose veins in pregnancy are a short-term problem, and they get better after your baby is born.
- You can do things to ease the discomfort they can cause. These include sitz baths, ice packs, or cold compresses to reduce swelling and creams or other medicines, such as stool softeners, your healthcare provider may recommend.

- The best way to help prevent hemorrhoids during pregnancy is to prevent constipation. If you're constipated, don't strain during bowel movements.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Medical Reviewer: Irina Burd MD PhD
Medical Reviewer: Donna Freeborn PhD CNM FNP
Medical Reviewer: Heather M Trevino BSN RNC
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Varicose veins during pregnancy - what to do and how to treat varicose veins in the legs
Varicose veins are persistent and irreversible enlargement resulting from pathological changes in the walls and valves of blood vessels. The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
Causes
The following reasons contribute to the occurrence of varicose veins during pregnancy:
- Violation of the outflow of blood from the veins of the lower extremities. This is because the growing uterus presses on the inferior vena cava - a large abdominal vein that collects blood from the lower half of the trunk and lower extremities.
- During pregnancy, the blood is more viscous, flows more slowly, this also contributes to venous congestion.
- The increase in body weight during gestation increases the load on the legs.
The development of varicose veins is facilitated by wearing high-heeled shoes, prolonged work in a standing position, lifting weights, and overweight.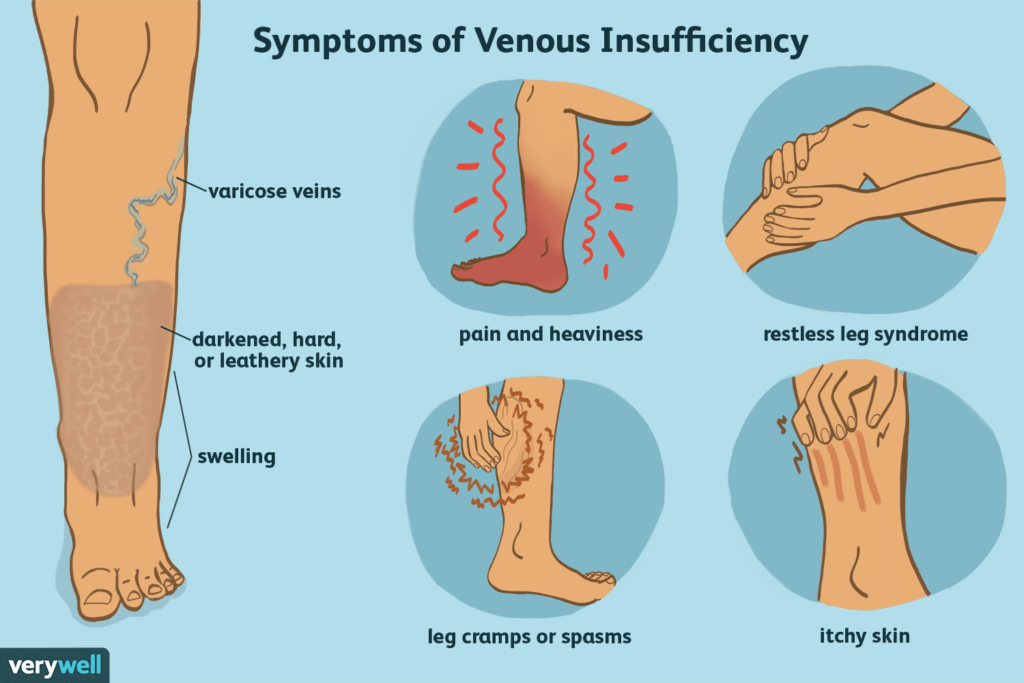
Symptoms
The first symptom is a visible increase in the vessels of the lower extremities. The veins are blue or purple, tortuous, protrude above the surface of the skin, may be serpentine or knobby (nodular) in shape. At the initial stage of the disease, a woman is only concerned about a cosmetic defect.
Other complaints follow. Edema appears, increasing in the evening and decreasing or completely disappearing after rest and a night's sleep. At night, convulsions may disturb. When walking, rapid fatigue is observed, there may be a feeling of fullness and pain.
Varicose veins of the lower extremities are observed in 50% of pregnant women, but not all of them suffer from true varicose veins, when irreversible changes appear in the venous wall. For most, the disease is functional in nature, that is, it is temporary, and after childbirth, when the factors that prevent normal venous outflow are eliminated, the tubes return to normal. This usually happens within a year.
Regression does not occur if the predisposition is independent of pregnancy. In this case, close relatives usually have varicose veins, or the woman herself had some symptoms even before conception.
Diagnostics
As you know, the “gold standard” for diagnosing pathology is ultrasound duplex scanning (USDS) of the veins of the lower extremities. This is a safe procedure for the expectant mother. Experienced obstetricians and gynecologists strongly recommend that pregnant women visit a phlebologist in the early stages of pregnancy, which contributes to the early prevention of complications of varicose veins in the postpartum period.
Stockings for varicose veins during pregnancy
During pregnancy, it is recommended to wear special compression (anti-varicose) tights and stockings. They need to be put on in a prone position, slightly lifting the leg up. There are 4 compression classes (pressure levels):
- 18-21 mmHg
- 23-32 mmHg
- 33-48 mmHg
- over 49 mmHg
During pregnancy, it is recommended to use compression classes 1-2. The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
Tights should be specially designed for expectant mothers so that they do not put pressure on the growing belly, but support it.
How much to wear?
After 20 weeks, you need to wear a bandage. It supports the uterus and reduces pressure on the large vessels of the abdominal cavity, thereby improving the outflow of blood from the lower half of the body.
Compression underwear and a bandage should be bought in pharmacies, it is important to choose the right size for them.
Exercise
It is recommended to attend gymnastics for pregnant women or do exercises at home. Particularly good prevention of varicose veins are classes in the pool. Sports strengthen the walls of blood vessels and improve blood flow. In addition, gymnastics is the prevention of excess weight.
A contrast shower on the calf muscles is useful.
If you think you have a predisposition to varicose veins, you should avoid saunas and heat treatments.
As often as possible, try to give your legs an elevated position. Don't sit cross-legged for long periods of time.
Wear comfortable shoes with small heels.
You can use creams for pregnant women "to relieve fatigue from the legs", such creams usually contain plant substances that, with regular use, strengthen the walls of superficial veins.
Treatment
Treatment of true varicose veins is surgical. During pregnancy, surgical treatment is carried out only for emergency indications, in view of the development of complications (thrombophlebitis).
A modern method of treatment is sclerotherapy, when a chemical substance is injected into the lumen of the vein, which leads to sclerosis and closure of its lumen. Endovasal methods are also minimally invasive methods of treatment performed on an outpatient basis (described in the relevant sections of our website). They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
All other methods are aimed only at preventing the disease from developing and temporarily reducing symptoms.
Most often, various ointments and gels are used, which are applied to the affected limb. For example, heparin-containing ointments reduce blood clotting and prevent the formation of blood clots. Venotonics (allowed only from the second trimester of pregnancy) have a decongestant and anti-inflammatory effect and strengthen the walls of blood vessels.
The diagnostic equipment used in our center has been tested in ROSTEST and has an appropriate conclusion about the absence of contraindications for use in pregnant women and children.
In the medical center "Yuzhny" they are very kind to expectant mothers and experienced phlebologists are well versed in the methods of diagnosing CVI and the secrets of preserving your beautiful legs after childbirth.
Varicose veins during pregnancy - what to do and how to treat
Veins are actively involved in the complex 9-month pregnancy process, and their changes are significant. Even with complete medical supervision, there is a risk of developing venous insufficiency.
Pregnancy is accompanied by profound changes throughout the female body. One of the first effects of pregnancy is an increase in the load on the veins of the pelvis and lower extremities. Therefore, many pregnant women develop varicose veins, which sometimes disappear after childbirth. This varicose vein is accompanied by discomfort, a feeling of heaviness, pain when walking, but women are mainly concerned with noticeable skin changes and varicose coloration of the legs and ankles, which remain after pregnancy.
From sickness to sickness
Many pregnant women are familiar with the feeling of malaise, accompanied by discomfort in the lower extremities. Functional chronic venous insufficiency is the first stage of venous disease with a feeling of heaviness in the lower extremities, sometimes with itching, paresthesias and, in some cases, convulsions, often nocturnal.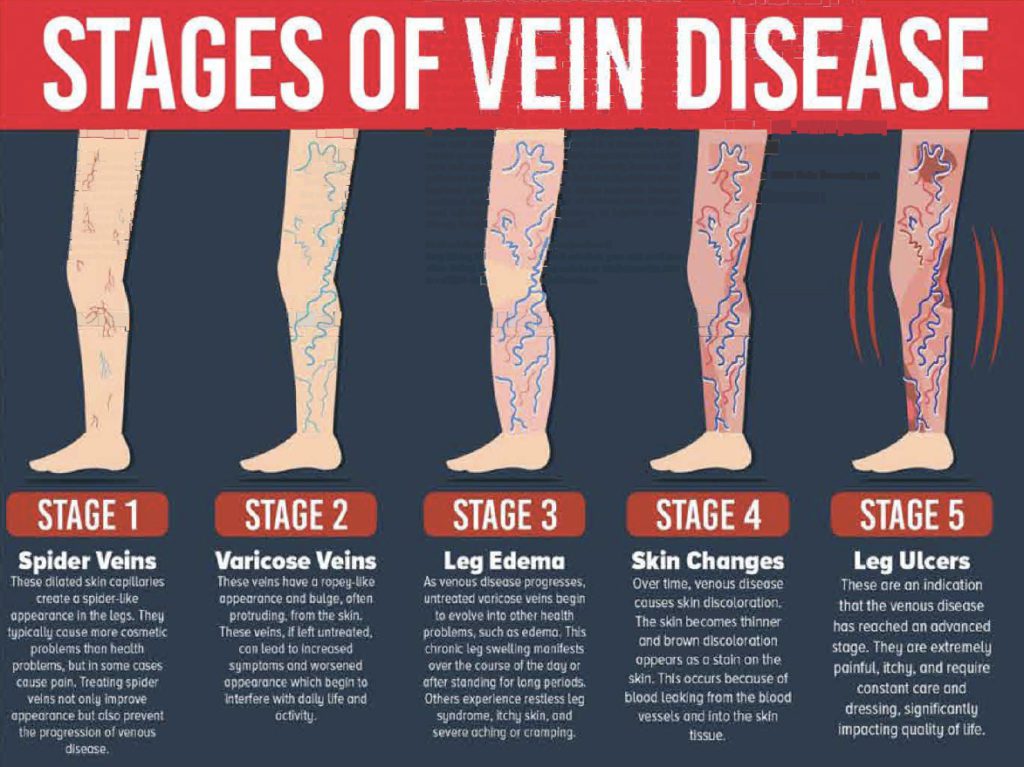
The possibility of thrombosis in pregnant women is 3-5 times higher than in other women. Sometimes blockage of the veins leads to their inflammation - thrombophlebitis. Blood clots that form in this case in the veins can cause a serious and dangerous disease - pulmonary embolism. In addition, the risk of developing thrombosis remains for another 1.5 months after childbirth, especially if they are severe.
Should I go to the doctor?
There are five groups of factors that affect the body of a pregnant woman, which explain the need for observation by a phlebologist.
Mechanical factor
An enlarged uterus is a barrier to blood circulation, as it compresses the inferior vena cava, pressing it against the spinal column and iliac muscle. This is of particular importance at rest, when a sharp decrease in venous outflow can lead to postural shock, well known to gynecologists. The anatomical structure of the iliac vein, which crosses the right iliac artery, explains the high incidence of thrombosis of the left limb (Cocket's syndrome).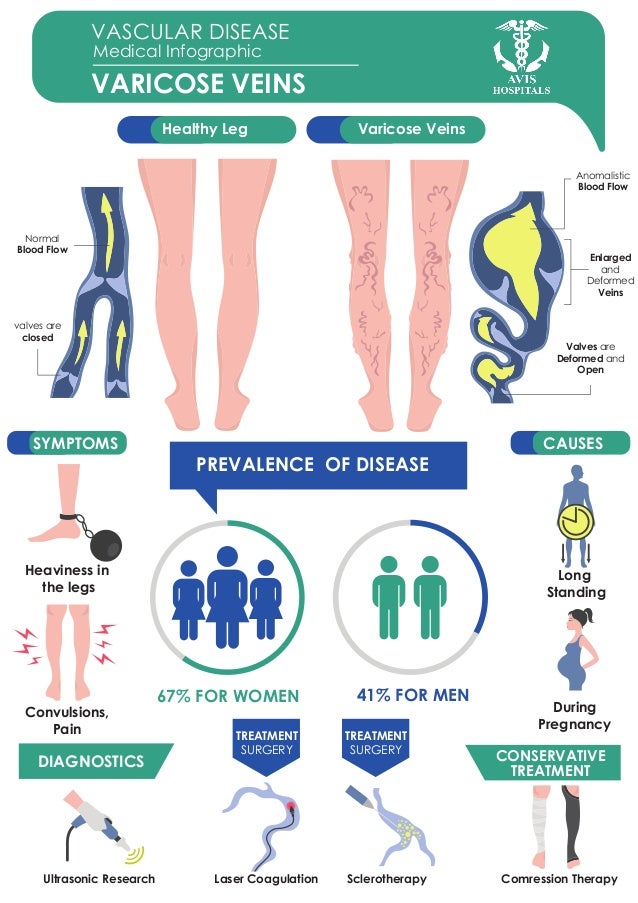
Circulatory factor
An increase in blood volume and outflow of blood from the heart leads to an increase in the load on the vessels, especially veins, and their expansion. This is especially important for the veins of the lower extremities and the vaginal area.
Hormonal factors
Progesterone, due to its relaxing effect on smooth muscle fibers, leads not only to a decrease in the tone of the venous wall, but also to a decrease in the tone of the urethra, bladder and small intestine.
Hemostatic factors
Changes in the hemostasis system always occur in the direction of increased coagulability (increased fibrinogen and factor III levels, increased platelet activity and decreased fibrinolytic activity).
Hemorheological factors
Blood viscosity increases despite a decrease in hematocrit.
Other contributing factors
In addition to the above factors associated with pregnancy, there are other contributing factors such as family history, sedentary lifestyle, immobile posture while working, driving, too low or high thin heels, obesity, underfloor heating, hot baths, and multiple pregnancies with short intervals between them.