Nipple scabs after breastfeeding
Breastfeeding and Nipple Scabs: Treatment, Prevention, and More
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Why do I have nipple scabs?
Breastfeeding is one of the leading causes of nipple scabs. Many women are surprised to find that breastfeeding, which seems so natural, is often a painful experience at first.
The good news is that while nipple pain and even cracked, bleeding, and scabbed nipples occur quite commonly, these are usually short-term issues that can be resolved. Even if it’s difficult at first, most women are able to breastfeed their babies.
One of the primary reasons for nipple scabs caused by breastfeeding is simply that the skin of your nipples is very sensitive. They’re not used to the level of abrasion and stimulation that occurs when breastfeeding.
It’s common for women to experience nipple pain during the first few days of breastfeeding, which then decreases as the nipples become accustomed to the process.
However, if a baby is positioned incorrectly, has a poor latch, or has anatomical issues such as a tongue-tie, nipple pain may not go away. These issues can even cause nipples to crack and bleed, which then leads to scab formation.
Yes, you can continue to nurse if you have nipple scabs. If you’ve developed nipple scabs or are experiencing pain with breastfeeding, it’s best to discuss it with your doctor or a lactation consultant immediately. They’ll be able to help troubleshoot and find solutions so your nipples can heal and you can breastfeed painlessly.
Lactation consultants may be available:
- at the hospital where you deliver your baby
- through your baby’s pediatrician’s office
- from local breastfeeding support groups
They can help ensure that your baby is positioned correctly and latching well. They can also assess your baby for what may be affecting their ability to nurse well.
While breastfeeding is one of the most common causes of nipple scabs, there are other reasons someone might develop scabs on their nipples. These include:
These include:
- Sports. Participating in sports such as running, cycling, or surfing can cause nipples to become chafed and scabbed.
- Eczema of the breast. Eczema is a skin condition that may cause nipples to become irritated to the point that they bleed and scab.
- Paget disease. A serious skin condition that causes scabs on the breast, Paget disease usually indicates cancer of the breast.
- Nipple injury. A nipple may be injured during activities, such as vigorous sucking or rubbing during sexual activity.
- Burns. Nipples may burn from exposure to tanning beds or the sun and scabs may form.
Breastfeeding
If you experience nipple pain, cracking, bleeding, or scabbing from breastfeeding, it’s best to consult your doctor or a certified lactation consultant immediately. They can help you determine the cause of your pain and find a solution. Nipple scabs are often caused by improper latching, which results in nipple trauma and injury.
Your lactation consultant may recommend treatments such as:
- pumping for a day or two while your nipples heal
- using a nipple shield
- applying purified lanolin ointment
- rinsing your breasts in saline after nursing
- using warm compresses or cold gel pads to help soothe your nipples
One study of nursing mothers found that applying peppermint essence to the nipples after feeding significantly reduced pain and promoted healing of injured nipples. Another solution to your nipple scabs may be simply changing the position you sit or lie when breastfeeding.
Exercise
If you’re an athlete with nipple scabs, it’s important to wear sports bras and clothing that fits well. Bras and bodysuits that’re too tight or too loose may exacerbate chafing. Fabric should also be breathable and moisture-wicking.
You also may be able to use purified lanolin ointment or powders to help reduce chafing. If your scabs are severe, you may need to take a short break from the activity that’s causing the scabs to allow them to heal.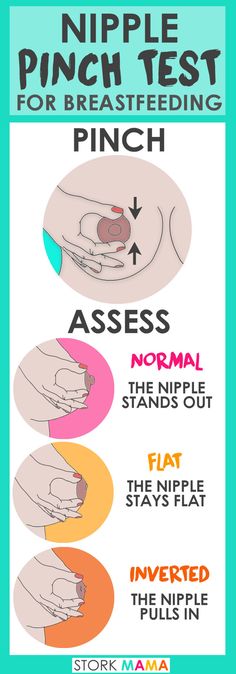
Rash
If you’re experiencing a rash accompanied by nipple scabs or nipple scabs that don’t have an apparent cause, it’s important to see your doctor. They can help determine why you have nipple scabs and ensure that you receive effective treatment.
Breastfeeding mothers can prevent nipple scabs by seeking help with any breastfeeding issues right away. Working with a certified lactation consultant can help you avoid pain.
To keep nipples moist and free of cracks throughout breastfeeding, it’s important to:
- practice good hand-washing to prevent infection
- keep breasts clean and dry
- apply purified lanolin or expressed breast milk
Shop for lanolin nipple cream.
Women who aren’t breastfeeding can help prevent nipple scabs by:
- avoiding burns from sun or tanning beds
- wearing breathable bras and clothing that fit properly
- keeping breasts clean and dry
- consulting your doctor if you develop a rash or scabs that don’t go away or don’t appear to have a cause
Nipple scabs commonly occur in breastfeeding mothers, especially at the very beginning. Women who aren’t nursing may also develop nipple scabs.
Women who aren’t nursing may also develop nipple scabs.
If you have nipple scabs, it’s important to talk to your doctor to determine the cause and begin the best course of treatment.
Scab on Nipple: Causes and Treatment Options
Nipple pain is common and may have a number of causes, such as allergies and skin irritation. It can also be caused by hormonal changes such as PMS.
One of the most common causes is breastfeeding. Some nipple pain causes create irritation to the point that part of the nipple bleeds and scabs over.
A scab on your nipple is a normal reaction to a break in the skin. It can be a result of a variety of causes from breastfeeding to friction from your clothing.
When your skin’s broken, platelets in your blood — along with other things like the protein fibrin — start the clotting process. This applies anywhere on your body, including the nipple.
When the clot gets dry and hard, it’s a scab. The scab serves to keep germs out of the opening and allow the cells underneath to heal.
Commonly, women have some nipple pain as they get used to breastfeeding. According to a 2016 study, in the first month after giving birth, 32 percent of women reported cracked nipples due to breastfeeding.
Once your nipples have become accustomed to breastfeeding, the discomfort can continue if your baby:
- doesn’t latch correctly
- is poorly positioned
- has anatomical issues such as tongue tie
If nipple discomfort continues and begins to crack or blister, they can bleed. That can lead to a scab on your nipple.
If you’re concerned about nipple pain or scabs, make an appointment with your doctor or a lactation consultant to help you address the situation and breastfeed painlessly.
If you participate in sports such as running or cycling, the motion of your clothing or sports bra rubbing against your nipple can cause chafing that could eventually result in a scab.
You can prevent this with a proper fitting sports bra. Some runners — including men — apply a lubricant such as petroleum jelly or anti-chafe cream or a product, such as NipEaze or NipGuard, before working out.
Some runners — including men — apply a lubricant such as petroleum jelly or anti-chafe cream or a product, such as NipEaze or NipGuard, before working out.
Eczema is a skin condition characterized by a scaly, itchy rash. It commonly develops in the areola — the area of dark skin around the nipple — and can be caused by a reaction to laundry detergents, soaps, certain materials, and other potential irritants.
Eczema may irritate nipples to the point that they bleed and scab.
Eczema — also referred to as atopic dermatitis — often begins to clear up once you’ve identified and removed the cause. Consider using hypoallergenic detergents and soaps that don’t have dyes and perfumes. Your doctor might recommend topical steroids.
Redness, flakiness, and soreness in and around your areola could be Paget’s disease. It looks like eczema, but it doesn’t go away with eczema treatment. Paget’s disease is an uncommon form of breast cancer.
Your nipple could be seriously irritated or even injured during activities, including sex.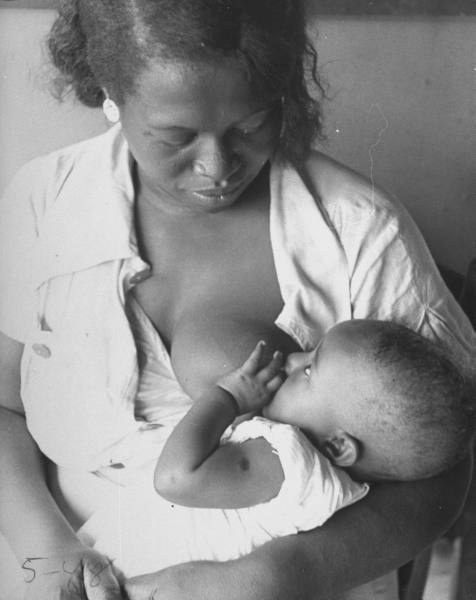
If you spend time in the sun topless or go topless in a tanning bed, your nipples may burn from exposure. Sunburn can result in peeling and scabbing.
Your nipples and areolas have hundreds of nerve endings and the skin is quite delicate. There are a number of activities that can result in nipple irritation to the point of bleeding and eventually scabbing.
Although breastfeeding might be one of the most common causes, there are other culprits including:
- eczema
- friction of clothing
- physical injury
- Paget’s disease
- sunburn
If you’re having trouble with nipple pain and scabbing, make an appointment with your doctor. They should be able to help you discover the root cause and offer advice on the best treatment for your specific situation.
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. 2
Prevention is better than cure, so check out our tips.
Check your baby's latch-on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue tie
Tongue tie (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin that attaches the tongue to the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding Tips
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples. Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
- Pat the nipples gently with a soft towel or simply let them air dry.
 In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past! - Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's gut microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain. 9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool.
 It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding. - Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit into the bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer. Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.

When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al. development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
8 Mohammadzadeh A et al. The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
9 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № № ФСЗ 2010/07352 dated 19.07.2010
** RU No. FCZ 2009/05592 dated 11/25/2009
ᐈ PROMENTARY • How candidiasis of the skin of the nipples at
Pain in the chest during lactation: norm or symptom
You probably heard complaints of other mothers about pain and severe discomfort during breastfeeding. Such stories could be told by a mother, aunt or grandmother, adding: “at first it’s always like that, you need to endure it.” Therefore, you think that discomfort in the mammary gland is normal and should be so.
Such stories could be told by a mother, aunt or grandmother, adding: “at first it’s always like that, you need to endure it.” Therefore, you think that discomfort in the mammary gland is normal and should be so.
But things are not so simple. Yes, discomfort in some cases may appear immediately after you start breastfeeding. It will be a response to new sensations. But also chest pain indicates diseases that need to be recognized and cured. In this case, you need to answer yourself the following questions:
- What is the nature of the pain?
- Does it hurt in one nipple or two?
- Is the pain localized only in the nipples or does it spread to the whole breast?
- When exactly does discomfort occur - at the beginning or at the end of feeding?
- What does the breast look like, is there any redness or swelling?
- How long does the pain last?
- Do nipples hurt between feedings?
- When did the pain - start from the first days of feeding or later?
Often the cause of pain in the mammary gland is an inflammatory process caused by a fungus of the genus Candida.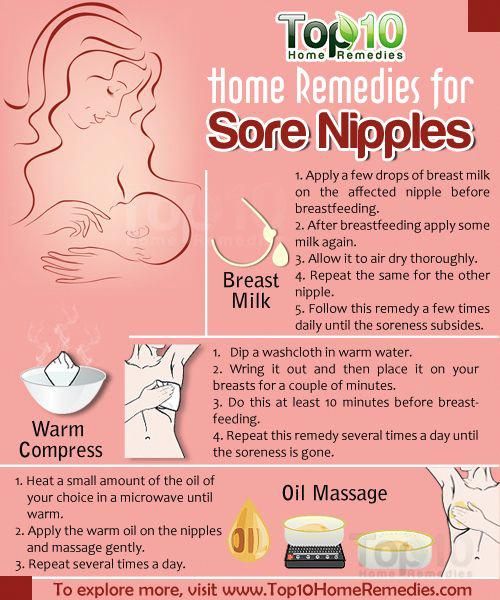 This is thrush of the breasts - a fairly common disease.
This is thrush of the breasts - a fairly common disease.
Photo 1. Any pain is a reason to see a doctor.
Symptoms thrush on the nipples
You don't need to diagnose yourself. And "Doctor Google" is not the best assistant in the treatment of a nursing mother. Similar or similar symptoms are typical for dermatitis of the skin of the nipples, eczema and psoriasis, damage to the epidermis of the breast with improper attachment or pumping.
If you have any complaints, see a dermatologist or mammologist. The doctor takes into account the symptoms and predisposing factors, makes an accurate diagnosis.
Make an appointment for an examination
Make an appointment at the center
Treatment of thrush in 7 steps
- Provide air to the affected nipples. During treatment, do not use breast pads or, if this is not possible, change them as often as possible.
- Maintain personal hygiene: wash your hands thoroughly after changing a diaper and washing your baby, after going to the toilet, before every feeding.

- Wash your nipples with baking soda (1 teaspoon per glass of water) after each breastfeed to relieve symptoms.
- Thoroughly sterilize everything that comes into contact with the breast (pads, breast pump) and change your bra as often as possible.
- Choose underwear made from natural materials (cotton, linen, silk), as synthetics cause additional irritation.
- Temporarily eliminate sweets, baked goods, alcoholic and sugary carbonated drinks from your diet.
- Take medication that is compatible with breastfeeding as directed by your doctor at your appointment.
Photo 2. Your comfort is key when breastfeeding
How to feed your baby with candidiasis
Maintain basic personal hygiene, and also:
9005