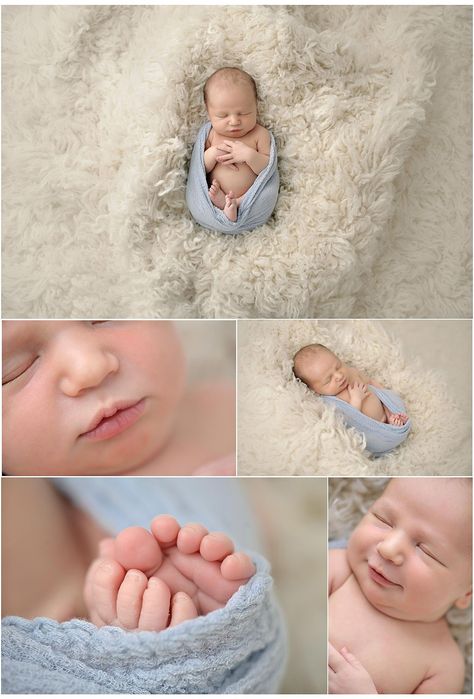
Newborn small baby
Having a small baby | Pregnancy Birth and Baby
Having a small baby | Pregnancy Birth and Baby beginning of content7-minute read
Listen
Some babies may be smaller than others during pregnancy. However, what’s important is that your baby grows at a healthy rate in your womb, regardless of their size.
Here’s what you need to know about your pregnancy if you have been told by your doctor or midwife that your baby is small or growing slower than expected. Your doctor or midwife may refer to a slower growth as ‘small for dates’, ‘small for gestation’ or ‘fetal growth restriction’.
Why is my baby small?
Most babies who are smaller than expected are healthy. In some cases, babies are small and appropriately grown, given the size of their parents and their ethnicity.
However, up to 10% of pregnancies will be affected by ‘fetal growth restriction'. This is a more serious complication that means your pregnancy must be closely monitored. In many instances, babies with fetal growth restriction are small because the placenta hasn’t developed well enough to keep up with the baby’s growing needs for nutrients and oxygen, although a cause may not always be found.
Risk factors for having a baby with fetal growth restriction include:
- previously having a small baby, pre-eclampsia or a stillbirth
- an infection that passes across the placenta, such as cytomegalovirus (CMV)
- heavy bleeding early in pregnancy
- having a chronic health condition, such as high blood pressure, kidney disease or diabetes
- severe anaemia or undernutrition
- smoking, drinking alcohol or using illegal drugs
- a genetic or chromosomal condition in the baby
- having a multiple pregnancy (twins, triplets or more)
How is a baby's size measured?
During routine antenatal check-ups, your doctor or midwife will use a tape measure to estimate the growth and size of your baby by measuring your abdomen, from your pubic bone to the top of your uterus (or fundus). This is known as the ‘symphyseal fundal height measurement’ (SFH) and gives some indication about a baby’s growth during pregnancy.
This is known as the ‘symphyseal fundal height measurement’ (SFH) and gives some indication about a baby’s growth during pregnancy.
If you have risk factors for fetal growth restriction, or if your baby has been diagnosed with this, your baby’s growth may be monitored more closely by ultrasound, instead of using a tape measure.
Every pregnancy is unique. Your doctor or midwife will track your baby’s growth at each check-up. They will talk with you about next steps if there are signs that your baby’s growth has slowed.
Should I be concerned if my baby is small?
Most small babies will be healthy. However, if your baby has fetal growth restriction, this increases the risk of complications and, sadly, also the risk of stillbirth. Your doctor and midwife will monitor you and your baby’s health closely to reduce the risk of this happening.
You can monitor your baby’s health by attending your scheduled antenatal visits and keeping a close eye on your baby’s movements. If you are concerned about your baby’s movements at any stage, call your doctor or midwife immediately.
If you are concerned about your baby’s movements at any stage, call your doctor or midwife immediately.
Your doctor or midwife may also talk to you about the best time for your baby to be born. Sometimes it may be necessary for your baby to be born early, before your due date. Every situation will be different; your doctor or midwife will give you personalised advice each step of the way.
Generally a baby with fetal growth restriction can still be born via normal vaginal delivery, but you and your baby may need extra care both during labour and after the birth. This means it’s best to give birth where you can access specialist medical services.
Talk to your doctor or midwife about the best place for you to give birth.
Can I do anything to reduce the risk of having a small baby?
Often there is nothing you can do to prevent a baby being small. But looking after yourself during pregnancy is important to help reduce the risk of having a baby with fetal growth restriction. You should:
You should:
- quit smoking (if you currently smoke)
- eat a balanced, healthy diet
- keep a healthy weight during pregnancy
- avoid alcohol and illegal drugs
What to expect if your baby is born with low birth weight?
If your baby weighs less than 2.5kg at birth, their head may appear to be a lot bigger than the rest of their body. They may look thin with little body fat.
Babies of low birth weight or those who are born prematurely, may need to be admitted to the neonatal intensive care unit (NICU) or special care nursery (SCN).
Some of the challenges faced by babies with low birth weight can include:
- breathing or heart problems
- low oxygen levels at birth
- difficulty maintaining body temperature
- difficulty feeding and gaining weight
- infection
- bleeding on the brain (called ‘intraventricular haemorrhage’)
- problems with their eyes and vision
- problems with their intestines
These conditions are more likely to occur in premature babies and those with fetal growth restriction.
If there are no other complications, low birth weight babies usually 'catch up' in their physical growth. In later life, however, people who were born smaller than average are more likely to develop diabetes, obesity, heart problems and high blood pressure.
Questions you might want to ask your doctor
Here are some questions you might want to ask your midwife or doctor:
- What does having a small baby mean for me and the health of my baby?
- Will I need more regular check-ups during pregnancy? If so, what does this include?
- How will I know if my baby is well?
- Will having a small baby affect how and where I can give birth?
- Does having a small baby affect my next pregnancy?
Who can I talk to for advice and support?
Always talk to your doctor or midwife first if you have any concerns about your pregnancy, your own health or the health of your baby.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Stillbirth Centre of Research Excellence (Your baby's growth matters), Department of Health (Pregnancy care 2020 edition), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Perinatal post-mortem examination)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2022
Back To Top
Related pages
- Premature baby
- How your baby gains weight
- Special care nursery (SCN)
- Neonatal intensive care unit (NICU)
- Having a large baby
Need more information?
Low-birth weight babies - MyDr.
 com.au
com.au Babies are considered of low birth weight if they weigh less than 2500 g at birth. Low birth weight is associated with an increased risk of disabilities.
Read more on myDr website
Premature birth & premature babies | Raising Children Network
This essential guide for parents of premature babies covers gestational age, premature birth risk factors, premature labour and premature development.
Read more on raisingchildren.net.au website
Specialised care for your baby - Better Health Channel
If your baby is sick at birth or born too early (premature) they will be cared for in a Neonatal Intensive Care Unit (NICU) or Special Care Nursery (SCN) by highly experienced medical and nursing staff.
Read more on Better Health Channel website
Causes of Preterm Labour - Miracle Babies
There are many causes of preterm birth
Read more on Miracle Babies Foundation website
Baby due date - Better Health Channel
Pregnancy is calculated from the first day of your last period, not from the date of conception.
Read more on Better Health Channel website
Oral Health and Pregnancy - Australian Dental Association
Maintaining good oral health during pregnancy is important in ensuring whole-body health and the health of your unborn baby.
Read more on Teeth.org.au website
Developmental dysplasia of the hip (DDH) | Sydney Children's Hospitals Network
What is DDH? DDH occurs when a baby’s hip joint does not grow normally
Read more on Sydney Children's Hospitals Network website
Lactose intolerance - Better Health Channel
Symptoms of lactose intolerance include bloating, gas, abdominal pain and diarrhoea.
Read more on Better Health Channel website
Undescended testicles - Better Health Channel
Undescended testicles means that one or both testicles are missing from the scrotum.
Read more on Better Health Channel website
Pregnancy: blood tests, ultrasound & more | Raising Children Network
In pregnancy, you’ll be offered blood tests, ultrasound scans, urine tests and the GBS test. Pregnancy tests identify health concerns for you and your baby.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Low birthweight | March of Dimes
Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces.

Some low-birthweight babies are healthy, but others have serious health problems that need treatment.
Premature birth (before 37 weeks of pregnancy) and fetal growth restriction are the most common causes of low birthweight.
Being a person of color is not a cause for having a low birthweight baby. However, communities of color are disproportionately affected by racism. This affects their health and well-being and increases the risk of pregnancy complications.
Go to all your prenatal care checkups during pregnancy. Your health care provider tracks your baby’s growth and development at each visit.
Talk with your provider about what you can do to help reduce your risk for having a baby with low birthweight.
What is low birthweight?
Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces. Some babies with low birthweight are healthy, even though they’re small. But having a low weight at birth can cause serious health problems for some babies. A baby who is very small at birth may have trouble eating, gaining weight and fighting off infections. Some may have long-term health problems, too. About 1 in 12 babies (about 8 percent) in the United States is born with low birthweight.
A baby who is very small at birth may have trouble eating, gaining weight and fighting off infections. Some may have long-term health problems, too. About 1 in 12 babies (about 8 percent) in the United States is born with low birthweight.
What causes a baby to have a low birthweight?
There are two main reasons:
- Preterm birth.
- Fetal growth restriction (also called intrauterine growth restriction or small for gestational age). This means a baby doesn’t gain the weight they should before birth. Some babies may have low birthweight simply because their parents are small. Others may have low birthweight because something slowed or stopped their growth during pregnancy. Your health care provider measures your belly and uses ultrasound to help track your baby’s growth during pregnancy. Ultrasound uses sound waves and a computer screen to show a picture of your baby while you’re pregnant.
If your provider thinks your baby’s growth is being restricted, you may have ultrasounds more often (every 2 to 4 weeks) to track your baby’s growth. Your provider also may do other tests such as heart rate monitoring and tests to check for infections or birth defects. Babies who have birth defects are more likely to be born too early.
Are you at risk of having a low-birthweight baby?
Some things may make you more likely than others to have a low-birthweight baby. These are called risk factors. Having a risk factor doesn’t mean you’ll definitely have a low-birthweight baby, but it may increase your chances. Talk with your health care provider about what you can do to reduce your risk.
Medical risk factors for having a low-birthweight baby
- Preterm labor. This is labor that starts too soon, before 37 weeks of pregnancy.
- Chronic health conditions. These are health conditions that last for a long time or that happen again and again over a long period of time. Chronic health conditions need to be treated by a health care provider.
 Chronic health conditions that may lead to having a baby with low birthweight include high blood pressure, diabetes and heart, lung and kidney problems.
Chronic health conditions that may lead to having a baby with low birthweight include high blood pressure, diabetes and heart, lung and kidney problems. - Taking certain medicines to treat health conditions, such as high blood pressure, epilepsy and blood clots. Tell your provider about any prescription medicine you take. You may need to stop taking a medicine or switch to one that’s safer during pregnancy.
- Infections. Certain infections, especially infections of the internal reproductive organs during pregnancy, can slow a baby’s growth in the womb. These include cytomegalovirus, rubella, chickenpox, toxoplasmosis and certain sexually transmitted infections.
- Problems with the placenta. The placenta grows in the uterus and supplies the baby with food and oxygen through the umbilical cord. Some problems in the placenta can reduce the flow of oxygen and nutrients to the baby, which can limit the baby’s growth.

- Not gaining enough weight during pregnancy. Pregnant people who don’t gain enough weight during pregnancy are more likely to have a low-birthweight baby than those who gain the right amount of weight. If you have an eating disorder or have been treated for an eating disorder, tell your provider. Your provider can check on you and your baby carefully throughout pregnancy to help prevent complications and make sure you’re both healthy.
- Having a baby who was born too early or who had low birthweight in the past.
- Being pregnant with multiples (twins, triplets or more). More than half of multiple birth babies have low birthweight.
- Smoking, drinking alcohol, using street drugs and abusing prescription drugs. Pregnant people who smoke are more than 3 times as likely to have a baby who weighs too little at birth than people who don’t smoke.
 Smoking, drinking alcohol, using street drugs, and abusing prescription drugs during pregnancy can slow the baby’s growth in the womb and increase the risk for preterm birth and birth defects.
Smoking, drinking alcohol, using street drugs, and abusing prescription drugs during pregnancy can slow the baby’s growth in the womb and increase the risk for preterm birth and birth defects. - Exposure to air pollution or lead
- Being a member of a group that experiences the effects of racism and health disparities.
- Domestic violence. This is when your partner hurts or abuses you. It includes physical, sexual and emotional abuse.
- Age. Being a teen (especially younger than 15) or being older than 35 makes you more likely than other parents to have a low-birthweight baby.
Rates of low birthweight in the United States
Black babies are more likely than others to weigh less than they should at birth. The rates of low birthweight among different ethnic groups are:
- About 1 in 7 Black babies (about 13 percent)
- About 1 in 12 Asian babies (about 8 percent)
- About 1 in 13 Native American or Alaska Native babies (about 8 percent)
- About 1 in 14 Latinx babies (about 7 percent)
- About 1 in 14 White babies (about 7 percent)
March of Dimes recognizes that racism and its effects are factors in the health disparities in pregnancy outcomes and babies’ health. We must work together to bring fair, just and full access to health care for all moms and babies.
We must work together to bring fair, just and full access to health care for all moms and babies.
Does a low birth weight cause problems for the baby?
Yes. Babies who weigh less than they should at birth are more likely than babies whose weight is normal to have health problems. Some need special care in a hospital’s newborn intensive care unit (also called NICU) to treat medical problems. These include:
- Breathing problems, such as respiratory distress syndrome (also called RDS). Babies with RDS don’t have a protein called surfactant that keeps small air sacs in a baby’s lungs from collapsing. Treatment with surfactant helps these babies breathe more easily. Babies who have RDS also may need oxygen and other breathing help to make their lungs work.
- Bleeding in the brain (also called intraventricular hemorrhage or IVH). Most brain bleeds are mild and go away on their own. More severe bleeds can cause pressure on the brain that can cause fluid to build up in the brain.
 This can cause brain damage. In some cases, a surgeon may insert a tube into the baby’s brain to drain the fluid.
This can cause brain damage. In some cases, a surgeon may insert a tube into the baby’s brain to drain the fluid. - Patent ductus arteriosus. Patent ductus arteriosus is when an opening between 2 major blood vessels leading from the heart does not close properly. This can cause extra blood to flow to the lungs. In many babies who have patent ductus arteriosus, the opening closes on its own within a few days after birth. Some babies need medicine or surgery to close the opening.
- Necrotizing enterocolitis. This is a problem in a baby’s intestines. The intestines are long tubes that are part of the digestive system. The digestive system helps the body break down food. Necrotizing enterocolitis can be dangerous for a baby and can cause feeding problems, swelling in the belly, and other complications. Babies who have necrotizing enterocolitis are treated with antibiotics and fed through an intravenous, or IV, tube. Some babies need surgery to remove damaged parts of intestine.

- Retinopathy of prematurity. This eye disease is what happens when a baby’s retinas don’t fully develop in the weeks after birth.
- Jaundice. This is a condition that makes a baby’s eyes and skin look yellow. It’s caused when there’s too much of a substance called bilirubin in the blood.
- Infections. The immune system protects the body from infection. In a baby who is born too early, the immune system may not be fully developed and may not be able to fight off infection.
Does a low weight at birth cause problems later in life?
Babies who are born weighing too little may be more likely than others to have certain health conditions later in life, including:
- Diabetes
- Heart disease
- High blood pressure
- Intellectual and developmental disabilities
- Metabolic syndrome
- Obesity
If you’ve had a baby who weighed less than they should have at birth, talk with their health care provider about what you can do to help your baby be healthy. As your child grows, make sure they eat healthy food, stay active and go to all their health care checkups. Regular checkups can help your baby’s provider spot health conditions that may cause problems as your baby grows older. These checkups also help make sure that your child gets all the vaccinations they need to stay protected from certain harmful diseases.
As your child grows, make sure they eat healthy food, stay active and go to all their health care checkups. Regular checkups can help your baby’s provider spot health conditions that may cause problems as your baby grows older. These checkups also help make sure that your child gets all the vaccinations they need to stay protected from certain harmful diseases.
If my baby has developmental delays, do they need early intervention services?
Yes. If your baby has developmental delays, it’s important to get early intervention services as soon as possible. Developmental delays are when your child doesn’t reach developmental milestones when expected. Early intervention services can help improve your child’s development. They can help children from birth through 3 years old learn important skills. Services include therapy to help a child talk, walk, learn self-help skills and interact with others.
The CDC program Learn the signs. Act early offers tools and information for parents who think their child may have developmental delays. You can find your state’s contact information for early intervention services. You don’t need a doctor’s referral or a medical diagnosis to ask for a free screening.
You can find your state’s contact information for early intervention services. You don’t need a doctor’s referral or a medical diagnosis to ask for a free screening.
Last reviewed: June, 2021
Newborn baby in the family
Schedule of appointments, examinations, vaccination of children from 0 to 18 months (in accordance with international medical recommendations)
Medical specialists
Pediatrician 1 time in 7-10 days during the first month
orthopedist
Neurologist
Ophthalmologist
Vaccination
BCG in the maternity hospital
Hepatitis B (1 vaccination) in the maternity hospital
Pertussis-Diphtheria-Tetanus-Poliomyelitis
Pneumococcal infection
Rotavirus infection
meningococcal infection
Mantoux test
Kor-red-parotitis (1 vaccine)
Blood OSPU
Laboratory studies
Neurosonography (NSG), nasal of the stems of stems, uzi of the bath cavities (complex), ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (ECG)
Medical specialists
Ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
Surgeon
Ophthalmologist
vaccination
Hepatitis in
9000 diphors in 9000 diphic -Tetanus-Poliomyelitis-Hemophilus influenzaePneumococcal infection
Rotavirus infection
Meningococcal infection
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chicken pox
Laboratory and functional studies
Neurosonography (NSG), Ultrasound of the hip joints, Ultrasound of the abdominal cavity (complex), Ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, urinalysis
Electrocardiography (ECG)
Medical specialists
Pediatrician
Orthopedic surgeon
Neurologist
Ophthalmologist
Vaccination
0002 Hepatitis BKoklush-Diferia-Stolbnyak-Polyomyelite Hemophilic infection (1 vaccination)
Pneumococcal infection (1 vaccination)
Rotavirus infection (1 vaccine)
Meningococcal infection
Mantoux Par-red-parit (1 vaccination)
Chicken pox
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
Ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
Surgeon of Orthoped
Ophthalmologist
vaccination
Gepatitis in 9000 Tetanus-Polio-Hemophilus influenzae (2 shots)
Pneumococcal disease (2 shots)
Rotavirus (2 shots)
Meningococcal disease
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chicken pox
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex03), ultrasound of the heart
3
Complete blood count, urinalysis
Electrocardiography (ECG)
Medical specialists
Pediatrician
Orthopedic surgeon
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
Koklush-Diferia-Poliomyeltit-hemophilic infection
Pneumococcal infection
Rotavirus infection
Meningococcal Mantoux Paul (1 Popular) Corpace Popular)
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
surgeon orthopedic
Neurologist
Ophthalmologist
Vaccination
Hepatitis B (3 vaccination)
Klush-Diferia. -Tetanus-Polio-Hemophilus influenzae (3 shots)
-Tetanus-Polio-Hemophilus influenzae (3 shots)
Pneumococcal disease (3 shots)
Rotavirus (3 shots)
Meningococcal disease
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chickenpox
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (9complex), ultrasound of the kidneys
ultrasound of the heartComplete blood count, complete urinalysis
Electrocardiography (ECG)
Specialist doctors
Pediatrician
Orthopedic surgeon
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
Koklush-Diferia-Differia-Poliomyelittehtate infection
Pneumococcal infection
Rotavirus infection
Meningococcal infections
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
surgeon-orthopedic
Neurologist
ophthalmologist
Vaccination - Haemophilus influenzae
Pneumococcal infection
Rotavirus infection
Meningococcal infection
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chickenpox
Laboratory and functional studies
Neurosonography (NSG), Ultrasound of the hip joints, Ultrasound of the abdominal cavity (complex), Ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (
)
Specialist doctors
Pediatrician
surgeon-orthopedic
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
cough-diferia-polyomyel-hemophilic infection
Pneumococcal infection
Rotavirus infection
meningococcal infection (1 vaccination)
Mantoux test
Kor-red-parotitis (1 vaccine)
Windle
Laboratory and functional research
Neurosonography (NSG), nusa acres, nusa acres, nazi academics joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (ECG)
Neurosonography (NSG), Ultrasound of the hip joints, Ultrasound of the abdominal cavity (complex), Ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (ECG)
Medical specialists
Pediatrician
Pediatrician -orthopedist
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
Pertussis-Diphtheria-Tetanus-Poliomyelitis-Hemophilus influenzae
Pneumococcal infection
Rotavirus infection
meningococcal infection
Mantoux test
Cor-red-parotitis (1 vaccination)
Wind Ospes
Laboratory and Functional Studies
Neurosonography (NSG), ultrasound of the pond , Ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (ECG)
Medical specialists
Pediatrician
Surgeon-Ortopoped
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
Koklush-Diferia-Poliomyelithic infection 9000
Measles-Rubella-Mumps (1 vaccination)
Chickenpox (1 vaccination)
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
Ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
Surgeon
Ophthalmologist
vaccination
Hepatitis in
9000 diphors in 9000 diphic -Tetanus-Poliomyelitis-Hemophilus influenzaePneumococcal infection
Rotavirus infection
Meningococcal infection
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chickenpox (2 vaccinations)
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
ultrasound of the heart
3 Complete blood count, urinalysis
Electrocardiography (ECG)
Medical specialists
Pediatrician
Orthopedic surgeon
Neurologist
Ophthalmologist
Vaccination
Hepatitis B
Koklush-diphtheria-resistant-poliomyelite hemophilic infection (1 revaccination)
Pneumococcal infection (1 revaccination)
Rotavirus infection
Meningococcal infection
Mantia manti-red. )
)
Chicken pox
Laboratory and functional studies
Neurosonography (NSG), ultrasound of the hip joints, ultrasound of the abdominal cavity (complex), ultrasound of the kidneys
Ultrasound of the heart
General blood test, total urine analysis
Electrocardiography (ECG)
Specialists doctors
Pediatrician
Surgical Ortopoped
Ophthalmologist
Vaccination
Poliomilitis (2 rewards 2 revocation )
Pneumococcal infection
Rotavirus infection
Meningococcal infection
Mantoux test
Measles-Rubella-Mumps (1 vaccination)
Chickenpox
Laboratory and functional studies
Neurosonography (NSG), Ultrasound of the hip joints, Ultrasound of the abdominal cavity (complex), Ultrasound of the kidneys
Ultrasound of the heart
Complete blood count, complete urinalysis
Electrocardiography (
)
The smallest newborn in Russia was discharged from the hospital in Lipetsk.
 News. Channel One In Lipetsk, the smallest newborn in Russia was discharged from the hospital. News. Channel One
News. Channel One In Lipetsk, the smallest newborn in Russia was discharged from the hospital. News. Channel One News
- Issues
- All news
Do you want to receive notifications from the Channel One website?
Matvey has a new record every time he weighs. How this baby grows is watched by the entire department. Today it is difficult to imagine that at birth, Matvey's weight did not exceed half a kilogram, and his height was 30 centimeters.
The child was born prematurely, at the sixth month. The birth was difficult, the doctors saved my mother. At first, doctors spoke cautiously about the chances of the baby. Just before discharge, little Matvey is already trying to smile, and doctors are giving advice to a happy mother. nine0003
And immediately after the birth, the whole department, with undisguised anxiety, nursed the newborn, who could not even feed on his own mother's milk. Matvey spent the premature three months in a special incubator. This device, according to doctors, replaced the child's womb.
This device, according to doctors, replaced the child's womb.
For a boy the size of a palm, he certainly seemed like a full-fledged room with glass walls - there was where to frolic. According to the observations of the doctors, Matveyka tried to move as much as possible, as if he himself was trying to tell the doctors and mother: I will get better. nine0003
Matveyka was brought home sleeping. The crib is a bit big for now, but that's not a problem anymore. Grandmother Galina Vasilievna promises to take nutrition issues under her special control.
Society
See also:
News release at 14:00 on 01/31/2023
News release at 18:00 on 01/30/2023
News release at 14:00 on 01/30/2023
News release at 12:00 on 01/30/2023
News release at 09:00 on 01/30/2023
nine0640 News release at 15:00 on 01/27/2023News release at 09:00 on 01/27/2023
News release at 14:00 on 01/26/2022
Release of the program "Time" at 21:00 from 01/25/2023
News release at 12:00 on 01/25/2023
News release at 09:00 on 01/25/2023
News release at 18:00 on 01/24/2023
News release at 15:00 on 01/24/2023
News release at 14:00 on 01/24/2023
News release at 12:00 on 01/23/2023
Breaking news
18:00
Another settlement in the Donetsk direction was liberated by the Russian military18:02
More than nine thousand illegally mobilized Russians were returned home, said the Prosecutor General of the Russian Federation18:08
Vladimir Putin gave a number of instructions to the government18: 09
The President of Russia had two international telephone callsNews
18:10
In 2023, the Russian economy will grow by 0.