Newborn body temp
How to take a newborn’s temperature
Your best bet is to use a digital thermometer. These can be bought inexpensively in any supermarket or pharmacy and can be used to take rectal (in the bottom) or axillary (in the armpit) temperature readings.
Taking a rectal temperature gives the most accurate reading of body temperature in infants and young children. However, if the thought of doing this makes you squeamish, taking an axillary temperature is the next best choice.
Be aware that temperature strips, which are placed on someone's forehead for a reading, have been found to be poor indicators of true body temperature, especially in infants and children, and should be avoided. The digital thermometer is best for temperature taking at home.
Taking a rectal temperature
- Lubricate the tip of the thermometer with a lubricating jelly. Check the manufacturer's directions to see whether water-soluble jelly or petroleum jelly is recommended.
- Place your baby on a firm, flat surface such as a changing table.
- Using your hand, insert the lubricated thermometer through the anal opening, about one-half to one inch or about 1.25 to 2.5 centimeters into the rectum. Stop at less than ½ inch or about 1.25 centimeters if you feel any resistance.
- Steady the thermometer between your second and third fingers as you cup your hand against your baby's bottom. Soothe your baby and speak to him/her quietly as you hold the thermometer in place.
- Wait until you hear the appropriate number of beeps or other signal that the temperature is ready to be read. Read and record the number on the screen, noting the time of day that the reading was taken.
Taking an axillary temperature
- Remove your child's shirt and undershirt. The thermometer should touch skin only, not clothing.
- Insert the thermometer in your child's armpit. Fold your child's arm across his chest to hold the thermometer in place.

- Wait until you hear the appropriate number of beeps or other signal that the temperature is ready to be read. Read and record the number on the screen, noting the time of day that the reading was taken.
Additional tips
- Never take your baby's temperature right after a bath or if he/she has been bundled tightly for a while — this can affect the temperature reading
- Never leave a child unattended while taking his temperature
- Temperature should be taken only if the baby feels hot or is lethargic
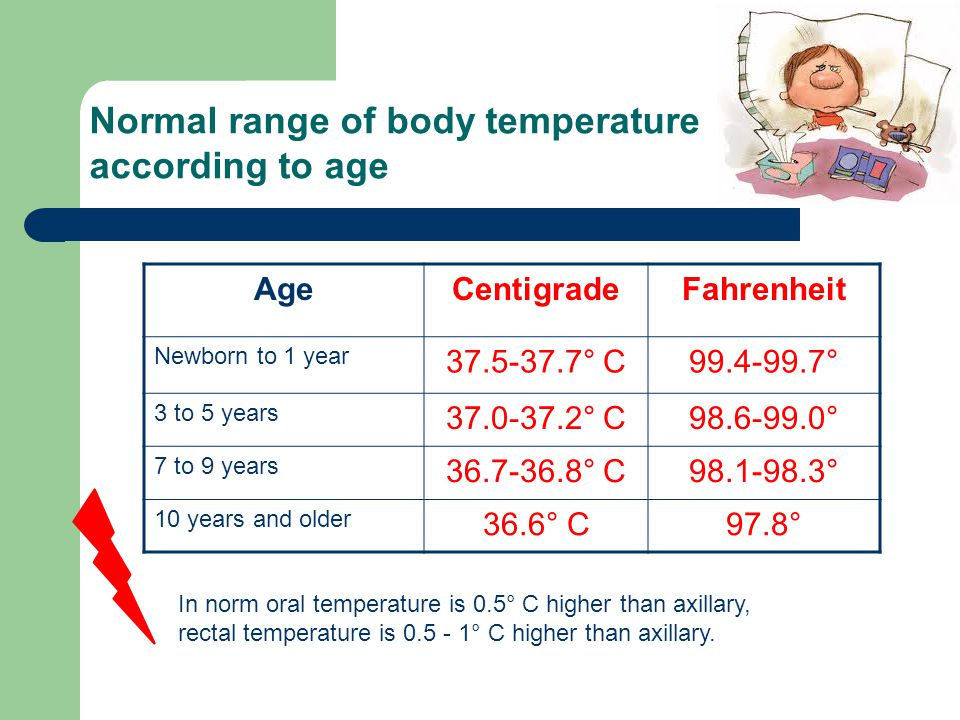
- A baby's normal temperature range:
- Under the arm is 97.5 to 99.3 degrees Fahrenheit or 36.5 to 37.4 degrees Celsius
- Rectal is 100.2 degrees Fahrenheit or less, or 37.9 degrees Celsius or less
- These are the American Academy of Pediatrics recommended ranges. If you have questions or concerns, be sure to discuss them with your baby's healthcare provider
Download the printable version of this page (PDF)
How to Take a Temperature (0-12 Months)
When Does Your Baby Have a Fever??
- Average body temperature is around 98.
 6° F (37.0° C)
6° F (37.0° C) - A fever is an elevated body temperature with these readings:
- Rectal, Forehead or Ear temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: ear temperatures are not accurate before 6 months of age
Where to Take the Temperature
- Rectal temps are the most accurate. Forehead temps are the next most accurate. Ear temps are also accurate if done properly. Temps done in the armpit are the least accurate. Armpit temps are useful for screening at any age.
- Age under 3 months old (90 days old). An armpit temp is the safest and is good for screening. If the armpit temp is above 99° F (37.2° C), re-check it. Use a rectal reading. Reason: If young babies have a fever, they need to see a doctor now. New research shows that forehead temps may also be accurate under 3 months of age.
- Age 3 months to 1 year old. Rectal or forehead temps are accurate.
 An ear thermometer can be used after 6 months old. An armpit temp is good for screening if it is taken right.
An ear thermometer can be used after 6 months old. An armpit temp is good for screening if it is taken right. - Digital (electronic) thermometers are easily found in stores. They do not cost very much. They can be used for rectal and armpit temps. Most of them give an accurate temp in 10 seconds or less. The AAP suggests you replace any glass thermometer in the house with one of these products.
Rectal Temperature: How to Take
- Age: Birth to 1 year old
- Have your child lie stomach down on your lap. Another way is on the back with the legs pulled up to the chest.
- Put some petroleum jelly on the end of the thermometer and the anus.
- Slide the thermometer gently into the anus no more than 1 inch. If your child is less than 6 months old, put it in no more than ½ inch. That means until you can no longer see the silver tip.
- Be gentle. There should not be any resistance. If there is, stop.
- Hold your child still. Leave a digital thermometer in until it beeps (about 10 seconds).
- Your child has a fever if the rectal temp is above 100.4° F (38° C).
- Warning: do not take rectal temperatures in young children with leukemia or other cancers. Also avoid in other children with weak immune systems such as organ transplant, HIV or sickle cell disease.
Armpit Temperature: How to Take
- Age: Any age for screening
- Put the tip of the thermometer in an armpit. Make sure the armpit is dry.
- Close the armpit by holding the elbow against the chest. Do this until it beeps (about 10 seconds). The tip of the thermometer must stay covered by skin.
- Your child has a fever if the armpit temp is above 99.0° F (37.2° C). If you have any doubt, take your child's temp by rectum or forehead.
Ear Temperature: How to Take
- Age: 6 months and older (not accurate before 6 months)
- This thermometer reads the heat waves coming off the eardrum.
- A correct temp depends on pulling the ear backward. Pull back and up if over 1 year old.

- Then aim the tip of the ear probe between the opposite eye and ear.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution. Being outdoors on a cold day will cause a low reading. Your child needs to be inside for 15 minutes before taking the temp. Earwax, ear infections and ear tubes do not keep from getting correct readings.
Forehead Touch Temperature: How to Take
- Age: Any age
- This thermometer reads the heat waves coming off the temporal artery. This blood vessel runs across the forehead just below the skin.
- This is the one most used in hospitals and doctors’ offices.
- Place the sensor head at the center of the forehead touching the skin.
- Slowly slide the thermometer across the forehead toward the top of the ear. Keep it in contact with the skin.
- Stop when you reach the hairline.
- Read your child's temp on the display screen.

- Note: some newer forehead thermometers don't need to slide across the forehead. Follow the box directions on how to take the temp.
- Used in more doctor's offices than any other thermometer.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution: forehead temperatures must be digital. Forehead strips are not accurate.
Forehead No-Touch Temperature: How to Take
- Age: any age
- Aim the thermometer at the center of the forehead.
- Stay less than 1 inch (2.5 cm) away. Do not touch the forehead.
- Do not move the thermometer.
- Press the measurement button.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Last Reviewed: 04/18/2023
Last Revised: 01/26/2023
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.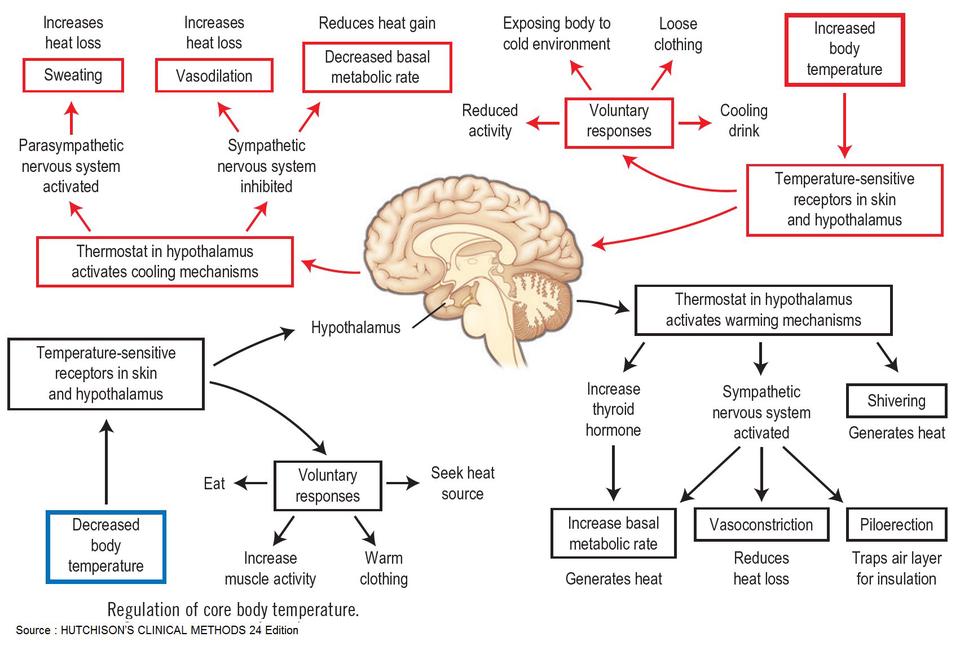
reasons, recommendations of doctors of the Central Medical Clinic CMD Perovo, st. Novogireevskaya
An increase in body temperature in a child is the most common reason for seeking emergency medical care. And of course, it is right when the child's parents, not self-medicating, seek medical help when their child has a fever.
However, it is useful for all parents to know some of the main causes of fever (fever) in a child and ways to normalize it.
Fever is divided into three main degrees of severity:
- A - fever from 37.0 to 37.9 degrees - mild or subfebrile fever, subfebrile condition;
- B - temperature increase from 38.0 to 39.0 degrees C - moderate fever;
- B - from 39.0 to 41.0 - high fever;
- D - increase in body temperature above 41 degrees - excessive (life-threatening) fever.
Fever in an infant
The body temperature of a newborn child during the first 5 - 7 days of life fluctuates around 37. 0, and in some children, an increase in body temperature during this period up to 38.0 - 39.0 is possible. This phenomenon is called transient hyperthermia of the newborn. In addition to hyperthermia, newborns are even more likely to have hypothermia, that is, a decrease in body temperature below normal. Due to the immaturity of the brain structures, not only newborn children, but also children of the younger age group up to 3-5 years old have a tendency to overheat quickly and to quickly hypothermia. Especially such a "volatility" of body temperature is typical, of course, for children in the first year of life. Therefore, if you, having measured the body temperature of a baby, found an increase in body temperature to 37.0 - 37.4 degrees, do not rush to immediately call a pediatrician. It is enough to measure the body temperature, having previously unswaddled the child, or simply remove a warm blanket from him so that after 15-20 minutes the temperature returns to normal.
0, and in some children, an increase in body temperature during this period up to 38.0 - 39.0 is possible. This phenomenon is called transient hyperthermia of the newborn. In addition to hyperthermia, newborns are even more likely to have hypothermia, that is, a decrease in body temperature below normal. Due to the immaturity of the brain structures, not only newborn children, but also children of the younger age group up to 3-5 years old have a tendency to overheat quickly and to quickly hypothermia. Especially such a "volatility" of body temperature is typical, of course, for children in the first year of life. Therefore, if you, having measured the body temperature of a baby, found an increase in body temperature to 37.0 - 37.4 degrees, do not rush to immediately call a pediatrician. It is enough to measure the body temperature, having previously unswaddled the child, or simply remove a warm blanket from him so that after 15-20 minutes the temperature returns to normal.
Another common cause of an increase in body temperature in the first 1. 5 - 2 years of a child's life is a reaction to teething. We wrote about this problem in a separate article on our website. In a nutshell, let me remind you that the reaction to teething in children is very individual. An increase in body temperature, most often, fits into the range from 37.1 to 37.6 degrees. Elevated temperature during teething usually lasts no more than 2-3 days, and in most children does not require the use of antipyretic drugs. However, in some cases, when teething, the child may have a fairly high fever of up to 38.0 and even up to 39.0 degrees. In this case, you can not do without the use of special anti-inflammatory gels for application to the gums and antipyretics in the form of suppositories (candles), such as Nurofen.
5 - 2 years of a child's life is a reaction to teething. We wrote about this problem in a separate article on our website. In a nutshell, let me remind you that the reaction to teething in children is very individual. An increase in body temperature, most often, fits into the range from 37.1 to 37.6 degrees. Elevated temperature during teething usually lasts no more than 2-3 days, and in most children does not require the use of antipyretic drugs. However, in some cases, when teething, the child may have a fairly high fever of up to 38.0 and even up to 39.0 degrees. In this case, you can not do without the use of special anti-inflammatory gels for application to the gums and antipyretics in the form of suppositories (candles), such as Nurofen.
Prolonged, subfebrile fever in a child
If in infants the cause of sudden “temperature jumps”, most often, is the immaturity of the nervous system and the reaction to teething, then in older children, often prolonged subfebrile body temperature is kept against the background of psycho-emotional experiences, academic failure, conflict situations in the family.![]() A separate problem is the active introduction of various electronic gadgets into the lives of modern children, sometimes from a very early age. So, for a child from 4 to 6 years old, who is already used to spending several hours a day at a computer or a game console, prolonged subfebrile condition can generally become commonplace, and parents, when they grab their heads from the thermometer readings, drag their child to neurologists , immunologists and infectious disease specialists, passing a bunch of tests, instead of just finding something more useful and healthy for the child.
A separate problem is the active introduction of various electronic gadgets into the lives of modern children, sometimes from a very early age. So, for a child from 4 to 6 years old, who is already used to spending several hours a day at a computer or a game console, prolonged subfebrile condition can generally become commonplace, and parents, when they grab their heads from the thermometer readings, drag their child to neurologists , immunologists and infectious disease specialists, passing a bunch of tests, instead of just finding something more useful and healthy for the child.
Temperature in a newborn baby. How to bring down?
When the temperature rises in adults, the algorithm of actions is known. But here we have a newborn baby with a hot forehead - the worries of parents are absolutely understandable: you should be especially courteous with babies. Yes, and such little ones are unable to either say, or show, or make it clear what specifically worries.
In this article, we will figure out what is the normal temperature of a newborn baby and how to measure it correctly, where it comes from and what to do for new moms and dads in general - when to sound the alarm.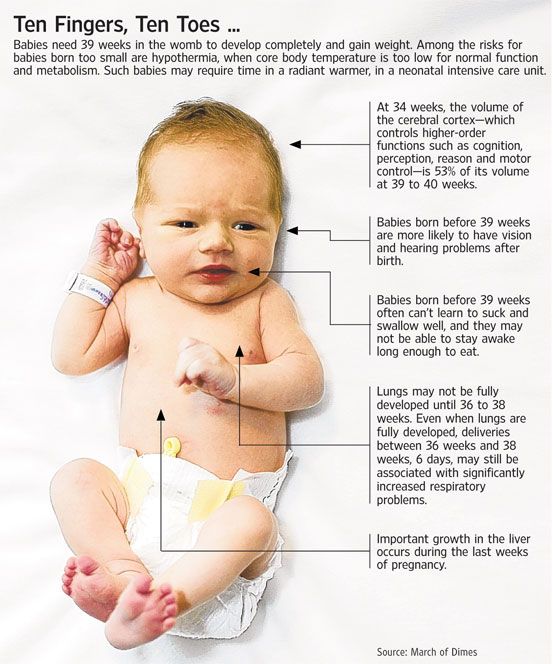
What is the normal body temperature of a newborn baby?
The rise in temperature is the main indicator of the functioning of the immune system. And he does not always report the course of an infectious disease! The fact is that the thermoregulation of the body of a newborn is imperfect. It simply reacts to the general temperature of the room in which it is located.
In a child of the first year of life, the body temperature can be 36, and 36.8, and 37, and 37.5. And that's okay.
If the temperature in the room is above 25 degrees, the baby's body temperature can rise to 37. For the generally accepted 36.6 in the room where the small child is, it should not be higher than 22-23 degrees, and the baby should not be very warmly dressed.
What to do when a newborn has a temperature?
The very first thing is to undress the baby. Let it lie quietly for 15 minutes and measure the temperature again.
An increase in body temperature in a newborn baby up to 3 months is a reason to call a pediatrician ALWAYS.
From 3 months it is reasonable to assess the situation as a whole - look at the general condition of the baby. What can they be?
- If the temperature is about 37 degrees, the child is cheerful and active, eats well, without unnecessary whims, then it is worth keeping calm.
- If, even at a normal body temperature of 36.8-37, the child is apathetic, refuses to eat and is naughty a lot, or vice versa - he constantly sleeps - it is definitely worth calling a pediatrician. As well as when rising above 38-38.5, even without the slightest cold symptoms (runny nose, cough), or rash (by the way, we already wrote how to treat prickly heat). It is better to do this without delay - within the first two days!
- Pay attention to the trembling of the limbs in the baby (febrile convulsions), or rolling of the eyes at a temperature of 37.5-37.8! This is also a signal for an immediate call to the doctor.
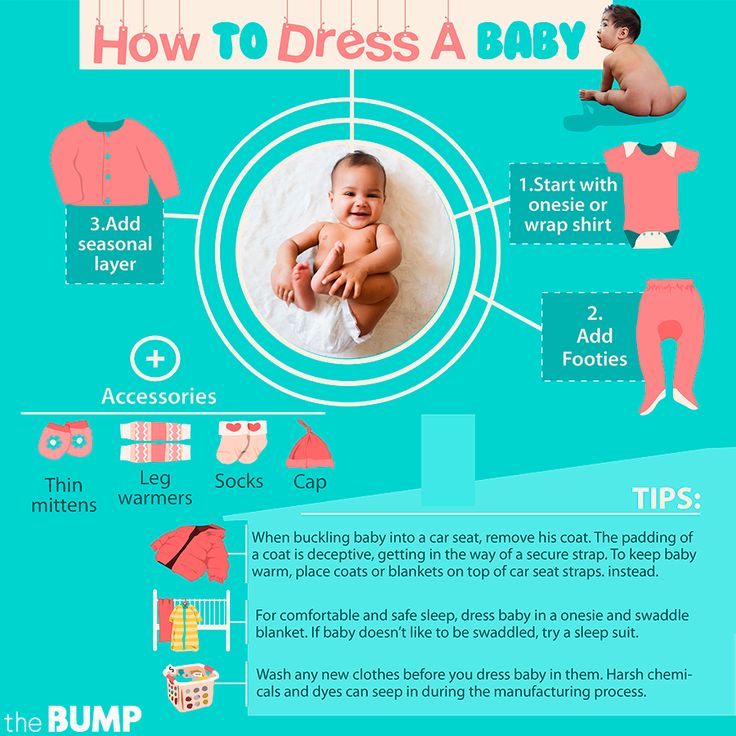
- If the temperature of a newborn child rises, you take certain actions: for example, physical methods of cooling (undressing, airing the room) or giving antipyretics, but within 3-4 hours the temperature does not subside. Call the pediatrician!
- Maintaining an even temperature, for example, 37.5, but for more than 5 days is another reason to consult a doctor.
- Fever above 38-39 degrees. And she always has a reason. There are 2 types of fever: white and red type.
Consider the type of fever
- White type - hot forehead, but cold hands and feet with a marble tint. Plus there may be chills. This is the reaction of the nervous system and blood vessels to intoxication. In this situation, it is worth giving an antipyretic, and simply rubbing the arms and legs (massage) - to restore blood supply, relieve spasm from small vessels, due to which the limbs turn pale or turn blue.

- Red type - the child is all hot, wet from sweating. It is worth giving an antipyretic, wiping the baby with water, increasing heat transfer - offering more liquid.
!!! Children up to a year old cannot be rubbed with vinegar or alcohol solution, it is dangerous.
How to measure the temperature of a newborn baby?
The most famous thermometers are mercury and electronic. For all their convenience for kids, electronic thermometers are not very reliable.
A modern and safe analogue of a mercury thermometer - Galinstan. It looks the same, but instead of mercury, a mixture of liquid metals, harmless to humans. They are sold in pharmacies and you probably already have one at home. So Galinstan's thermometers, like mercury ones, are more accurate.
The common practice of measuring body temperature under the armpit is quite revealing. It is better to measure alternately in two armpits and in dynamics.