When is the miscarriage stage over
Miscarriage | March of Dimes
Miscarriage is the loss of a pregnancy in the womb before 20 weeks of pregnancy. Some women have a miscarriage before they know they’re pregnant.
We don’t know all the causes of miscarriage, but chromosome problems are often to blame.
It can take a few weeks to a month or more for your body to recover from a miscarriage. It may take longer to recover emotionally.
Talk to your health care provider about having medical tests before you try to get pregnant again.
Most women who miscarry go on to have a healthy pregnancy later.
What is miscarriage?
Miscarriage (also called early pregnancy loss) is when there is pregnancy loss before 20 weeks. For women who know they’re pregnant, about 10 to 20 in 100 pregnancies (10 to 20 percent) end in miscarriage. Most miscarriages - 8 out of 10 (80 percent) - happen in the first trimester before the 12th week of pregnancy. Miscarriage in the second trimester (between 13 and 19 weeks) happens in 1 to 5 in 100 (1 to 5 percent) pregnancies. Pregnancy loss that happens after 20 weeks is called stillbirth.
Miscarriage is very common. Some research suggests that more than 30 percent of pregnancies end in miscarriage, and many end before a person even knows they’re pregnant. Most people who miscarry go on to have a healthy pregnancy later.
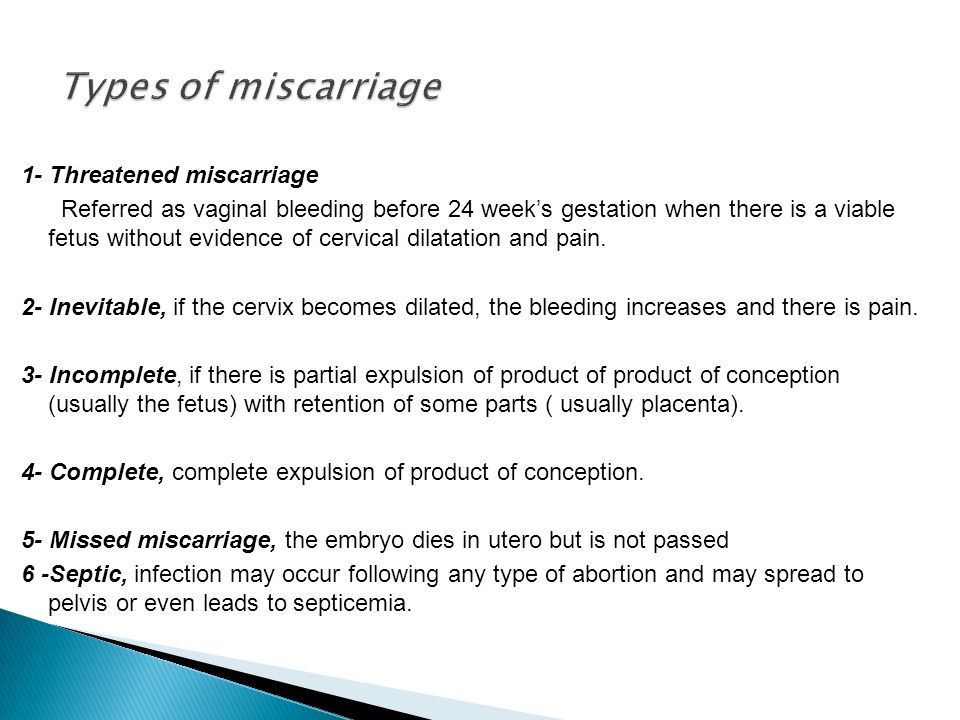
What is a threatened miscarriage?
This is when a pregnant person has bleeding, little or no pain, a closed (undilated) cervix and the baby may have a heartbeat. The cervix is the opening to the uterus that sits at the top of the vagina. Most of the time, threatened miscarriages turn out fine.
What is an incomplete miscarriage?
This is when a miscarriage has happened, but the body doesn’t push out all of the tissue from pregnancy. You may have bleeding, cramping and other signs and symptoms of miscarriage.
What is a complete miscarriage?
This is when your body pushes out all of the tissue from the pregnancy. You may pass tissue suddenly or after having medical treatment.
You may pass tissue suddenly or after having medical treatment.
What is an asymptomatic miscarriage?
This is when you have a miscarriage but don’t have bleeding or cramping and you don’t pass any tissue out of your body. It is sometimes called an empty sac pregnancy. You may need a procedure to empty the uterus or the cervix may dilate on its own and the tissue will be passed like a period.
What are repeat miscarriages?
Repeat miscarriages, or recurrent pregnancy loss, is the loss of two pregnancies in a row. About 1 in 100 pregnant people (1 percent) have repeat miscarriages. The risk of having a second miscarriage is 20 in 100 (20 percent). After two miscarriages in a row, the risk of another miscarriage increases to about 28 in 100 (28 percent). And after three or more miscarriages in a row, the risk of having another miscarriage is about 43 in 100 (43 percent).
What causes miscarriage and repeat miscarriages?
We don’t know what causes every miscarriage. But some miscarriages and repeat miscarriages can be caused by:
But some miscarriages and repeat miscarriages can be caused by:
Problems with chromosomes
Up to 7 in 10 (70 percent) of all miscarriages are caused when an embryo (fertilized egg) gets the wrong number of chromosomes. This usually happens by chance and is not caused by a problem that’s passed from parent to child through genes. Chromosomes are the structures in cells that holds genes. Each person has 23 pairs of chromosomes, or 46 in all. For each pair, you get one chromosome from your mother and one from your father. Miscarriages that happen in the first 3 months of pregnancy are often caused by chromosomal problems. Examples include::
- Blighted ovum. This is when an embryo implants in the body but doesn’t develop into a baby. If you have a blighted ovum, you may have dark-brown bleeding early in pregnancy.
- Intrauterine fetal demise. This is when an embryo stops developing and dies.
- Molar pregnancy.
 This is when tissue in the uterus forms into a grape-like structure or tumor at the beginning of pregnancy.
This is when tissue in the uterus forms into a grape-like structure or tumor at the beginning of pregnancy. - Translocation. This is when part of a chromosome moves to another chromosome. Translocation causes a small number of repeat miscarriages.
- Other chromosome issues, such as anencephaly (a type of neural tube defect), trisomies (a problem that can cause conditions such as Down syndrome), renal agenesis (a type of kidney defect) or hydrops (a type of thalassemia)
Problems with the uterus or cervix.
Problems with the uterus and cervix that can cause miscarriage after 12 weeks but before 20 weeks include:
- Septate uterus. This is when a band of muscle or tissue (called a septum) divides the uterus in two sections. If you have a septate uterus, your provider may recommend surgery before you try to get pregnant to repair the uterus to help reduce your risk of miscarriage.
 Septate uterus is the most common kind of congenital uterine abnormality. Septate uterus is a common cause of repeat miscarriages.
Septate uterus is the most common kind of congenital uterine abnormality. Septate uterus is a common cause of repeat miscarriages. - Asherman syndrome. If you have this condition, you have scars or scar tissue in the uterus that can damage the endometrium (the lining of the uterus). Before you get pregnant, your provider may use a procedure called hysteroscopy to find and remove scar tissue. Asherman syndrome may often cause repeat miscarriages that happen before you know you’re pregnant.
- Fibroids and polyps or scars from surgery on the uterus. Fibroids, polyps and scars can limit space for your baby or interfere with your baby’s blood supply. Before you try to get pregnant, you may need a surgery called myomectomy to remove them.
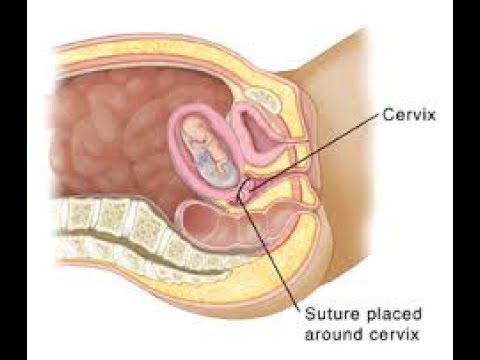
- Cervical insufficiency (also called incompetent cervix). This is when your cervix opens (dilates) too early during pregnancy, usually without pain or contractions.
 To help prevent this, your provider may recommend cerclage. This is a stitch your provider puts in your cervix to help keep it closed.
To help prevent this, your provider may recommend cerclage. This is a stitch your provider puts in your cervix to help keep it closed.
Infections
Infections can cause miscarriage. Common infections include:
- Parvovirus B19. Parvovirus causes fifth disease, a common childhood illness.
- Cytomegalovirus
- Sexually transmitted infections (STIs). STIs, such as genital herpes and syphilis, are infections you can get from having sex with someone who is infected. If you think you may have an STI, tell your health care provider right away. Early testing and treatment can help protect you and your baby.
- Listeriosis. Listeriosis is a kind of food poisoning. If you think you have listeriosis, call your provider right away. Your provider may treat you with antibiotics to help keep you and your baby safe.
Other possible causes of miscarriage include:
- Abnormal blood clots
- Placental abruption
- Premature rupture of the membranes (PROM).
 PROM is when the amniotic sac around your baby breaks (your water breaks) before labor starts.
PROM is when the amniotic sac around your baby breaks (your water breaks) before labor starts. - Preterm labor
Are you at risk for a miscarriage?
Some things may make you more likely than other pregnant people to have a miscarriage. These are called risk factors. Risk factors for miscarriage include:
- Having two or more previous miscarriages
- Being 35 or older. As you get older, your risk of having a miscarriage increases. The age of your partner also may increase the risk of miscarriage.
- Smoking, drinking alcohol or using street drugs. Street drugs include cocaine and methamphetamines. If you’re pregnant or thinking about getting pregnant and need help to quit, tell your provider.
- Being exposed to harmful chemicals. You or your partner having contact with harmful chemicals, like solvents, may increase your risk of miscarriage.
 A solvent is a chemical that dissolves other substances, like some detergent mixtures and paint thinner. Exposure to lead, arsenic, radiation or air pollution can also be harmful. Talk with your provider about what you can do to protect yourself and your baby.
A solvent is a chemical that dissolves other substances, like some detergent mixtures and paint thinner. Exposure to lead, arsenic, radiation or air pollution can also be harmful. Talk with your provider about what you can do to protect yourself and your baby.
Some health conditions may increase your risk for miscarriage. Treatment of these conditions before and during pregnancy can sometimes help prevent miscarriage and repeat miscarriages. If you have any of these health conditions, tell your health care provider before you get pregnant or as soon as you know you’re pregnant:
- Autoimmune disorders. These health conditions happen when the body attacks its own healthy tissue by mistake. Autoimmune disorders that may increase your risk of miscarriage include antiphospholipid syndrome and lupus (also called systemic lupus erythematosus or SLE). If you have antiphospholipid syndrome, your body makes antibodies that attack certain fats that line the blood vessels; this can sometimes cause blood clots.
 If you have antiphospholipid syndrome and have had repeat miscarriages, your provider may give you low-dose aspirin and a medicine called heparin during pregnancy and for a few weeks after you give birth to help prevent another miscarriage.
If you have antiphospholipid syndrome and have had repeat miscarriages, your provider may give you low-dose aspirin and a medicine called heparin during pregnancy and for a few weeks after you give birth to help prevent another miscarriage. - Obesity. This means your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to cdc.gov/bmi.
- Hormone problems, such as polycystic ovary syndrome (also called PCOS) and luteal phase defect. Hormones are chemicals made by the body. Progesterone is a hormone that helps regulate your periods and gets your body ready for pregnancy. Luteal phase defect is when you have low levels of progesterone over several menstrual cycles. If you have luteal phase defect, your provider may recommend treatment with progesterone before and during pregnancy to help prevent repeat miscarriages.
- Preexisting diabetes
- Preexisting hypertension
- Thyroid problems
- Severe kidney disease
- Congenital heart disease
- Severe malnutrition.
 This means not getting enough food or nutrients before getting pregnant.
This means not getting enough food or nutrients before getting pregnant. - Group B beta strep infection
- Certain prenatal tests, such as amniocentesis and chorionic villus sampling. These tests have a slight risk of causing a miscarriage. Your provider may recommend them if your baby is at risk for certain genetic conditions, such as Down syndrome.
Having an injury to your belly, like from falling down or getting hit, isn’t a high risk for miscarriage. Your body does a good job of protecting your baby in the early weeks of pregnancy.
Having an injury to your belly, such as from falling or getting hit or a motor vehicle accident, may be a risk for miscarriage depending on the force of the injury or fall. Your body usually does a good job of protecting your baby in the early weeks of pregnancy. If this happens contact your provider to make sure you and your baby are not injured.
Other factors that may increase your risk of miscarriage include:
- Certain medications. Some studies show that nonsteroidal anti-inflammatory medications (also called NSAIDS) including ibuprofen, naproxen and diclofenac may increase risk. NSAIDs are a type of medicine used to relieve pain and swelling. The acne medicine isotretinoin has also been linked to miscarriage and fetal abnormalities.
- Getting pregnant while using an intrauterine device (IUD). IUDs are devices placed in your body to prevent pregnancy. In rare cases, people can get pregnant while using an IUD.
- Stress. Both short, intense times of stress and long-term stress can increase the risk of miscarriage.
Socioeconomic status and other social determinants of health. Racial, ethnic or financial inequalities, being at risk for violence, being homeless or not having enough food can negatively affect your health. These factors increase your risk of developing other serious and chronic health conditions that can increase your chances of miscarriage.
You may have heard that getting too much caffeine during pregnancy can increase your risk for miscarriage. Caffeine is a drug found in foods, drinks, chocolate and some medicine. It’s a stimulant, which means it can help keep you awake. More research is needed to understand the effect of caffeine on pregnancy. Until we know more about how caffeine can affect pregnancy, it’s best to limit the amount you get to 200 milligrams each day. This is what’s in about one 12-ounce cup of coffee.
You also may have heard that having sex or exercising while pregnant can cause a miscarriage. There is no proof that this is true.
How can you prevent a miscarriage?
Miscarriages usually can’t be prevented, but being healthy before pregnancy can help prevent pregnancy complications. Good pre-pregnancy health includes getting a pre-pregnancy checkup and talking with your provider about health conditions that can affect your pregnancy. It also includes taking folic acid to help prevent birth defects and making changes in your life that may affect the health of your baby.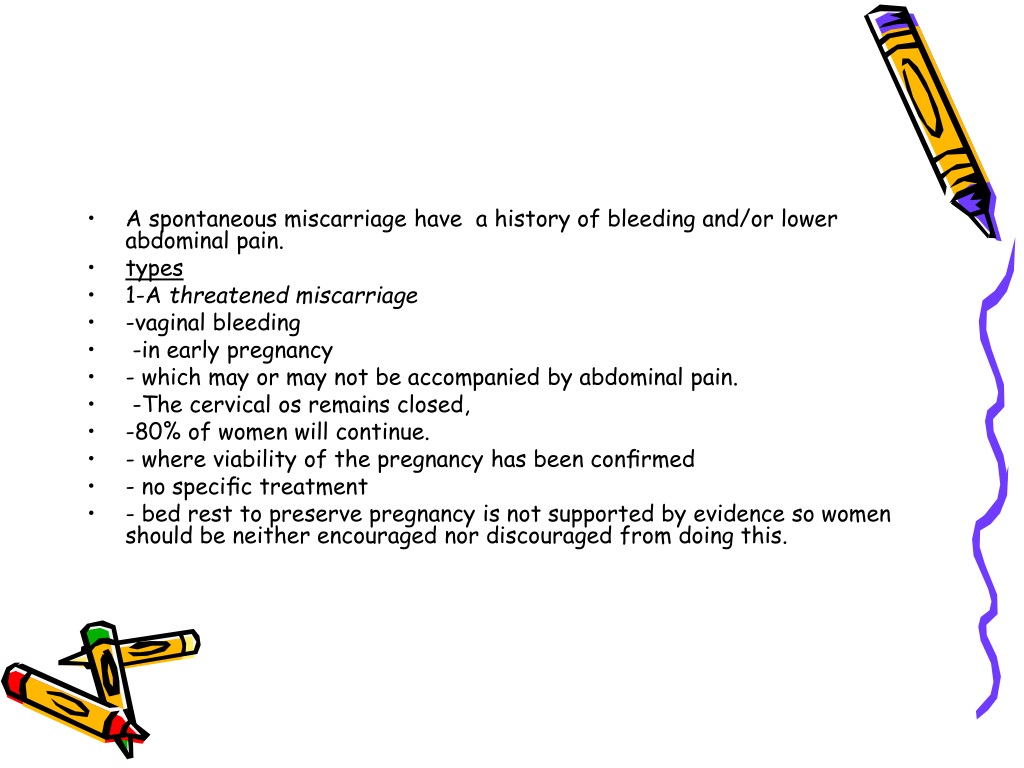
What are the signs and symptoms of miscarriage?
Signs and symptoms of miscarriage include:
- Bleeding from the vagina or spotting. Many people experience spotting early in their pregnancy. In most cases, it is not a sign of miscarriage. To be safe, if you have spotting or any of these signs or symptoms, call your provider.
- Cramps, like the ones you have with your period
- Severe belly pain
- No longer “feeling pregnant,” such as no longer feeling the baby move, feeling nauseated or no longer having breast tenderness
- Back pain
- Vaginal discharge with a bad smell
- Fever
Miscarriages can be dangerous if they’re not treated. Your provider may want to do some tests to make sure everything’s OK. These tests can include blood tests, a pelvic exam and an ultrasound.
Many pregnant people have these signs and symptoms in early pregnancy and don’t have a miscarriage.
What treatment do you get after a miscarriage or repeat miscarriages?
Treatment depends on how far along you were in your pregnancy, your overall health, your age and other factors. If you’ve had a miscarriage, your provider may recommend:
If you’ve had a miscarriage, your provider may recommend:
- Dilation and curettage (also called D&C). This is a procedure to remove any remaining tissue from the uterus. Your provider dilates (widens) your cervix and removes the tissue using an instrument called a curette.
- Dilation and extraction (also called D&E). This is a procedure to remove any remaining tissue from the uterus. Your provider dilates (widens) your cervix and removes the tissue using suction.
- Medicine. Your provider may recommend medicine that can help your body pass tissue that’s still in the uterus. If your blood type is Rh negative, you also may get a shot of Rh immunoglobulin after any miscarriage or bleeding episode in pregnancy. This can help prevent problems with future pregnancies. Rh immunoglobulin is a medicine that stops a person who is Rh negative from reacting to Rh-positive blood.
Do you need any medical tests after a miscarriage or repeat miscarriages?
If you miscarry in your first trimester, you probably don’t need any medical tests.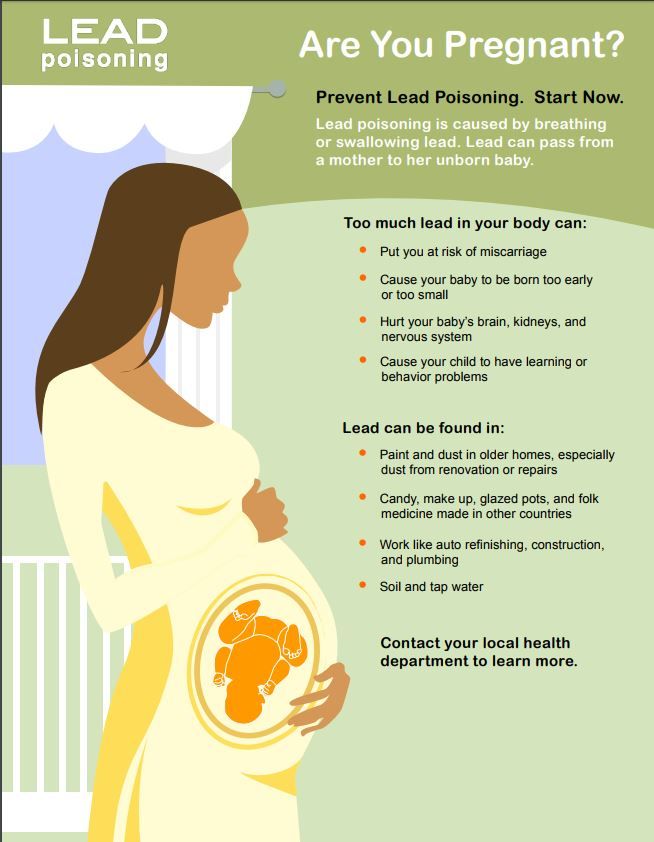 Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
Because we don’t often know what causes a miscarriage in the first trimester, tests may not be helpful in trying to find out a cause.
If you have repeat miscarriages in the first trimester, or if you have a miscarriage in the second trimester, your provider usually recommends tests to help find out the cause. Tests can include:
- Chromosome tests. You and your partner can have blood tests, like karyotyping, to check for chromosome problems. Karyotyping can count how many chromosomes there are and check to see if any chromosomes have changed. If tissue from the miscarriage is available, your provider can test it for chromosomal conditions.
- Hormone tests. You may have your blood tested to check for hormone problems. You may also have a procedure called endometrial biopsy that removes a small piece of the lining of the uterus to check for timing in the cycle and hormones.
- Blood tests to check your immune system.
 Your provider may test you for autoimmune disorders like, APS and lupus.
Your provider may test you for autoimmune disorders like, APS and lupus. - Looking at the uterus. You may have an ultrasound, a hysteroscopy (when your provider inserts a special scope through the cervix to see your uterus) or a hysterosalpingography (an X-ray of the uterus) or other test.
How long does it take to recover from a miscarriage?
It can take a few weeks to a month or more for your body to recover from a miscarriage. Depending on how long you were pregnant, you may have pregnancy hormones in your blood for 1 to 2 months after you miscarry. Most women get their period again 4 to 6 weeks after a miscarriage. Talk to your provider about how to care for yourself during this time.
It may take longer to recover emotionally from a miscarriage. You may have strong feelings of grief about the death of your baby. Grief can make you feel sad, angry, confused or alone. It’s OK to take time to grieve after a miscarriage. Ask your friends and family for support, and find special ways to remember your baby.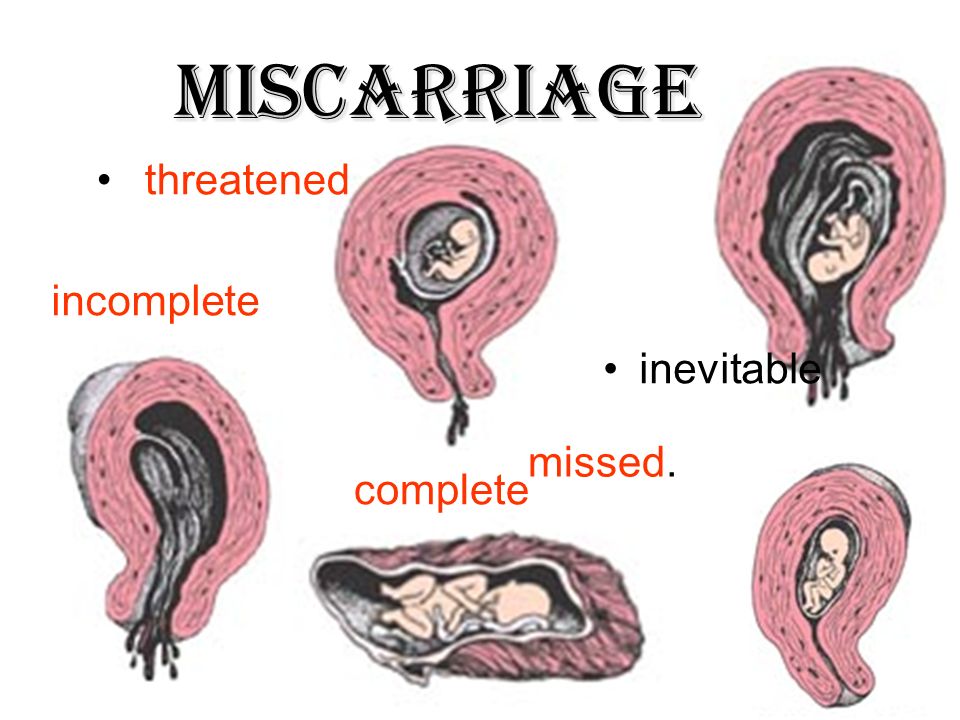 For example, if you already have baby things, like clothes and blankets, you may want to keep them in a special place. Do what’s right for you. Ask your provider about support groups or services that can help you to with recovery from grief.
For example, if you already have baby things, like clothes and blankets, you may want to keep them in a special place. Do what’s right for you. Ask your provider about support groups or services that can help you to with recovery from grief.
Certain things, such as hearing names you were thinking of for your baby or seeing other babies, can be painful reminders of your loss. You may need help learning how to deal with these situations and the feelings they create. A support group can help. Tell your provider if you need help to deal with your grief.
If you miscarry, when can you try to get pregnant again?
This is a decision for you to make with your partner and your provider. It’s probably OK to get pregnant again after you’ve had at least one normal period. Some studies show that trying to get pregnant again soon after a miscarriage can increase your chances of conceiving. Be sure to take a vitamin supplement that has 400mcg of folic acid even if you don’t get pregnant right away.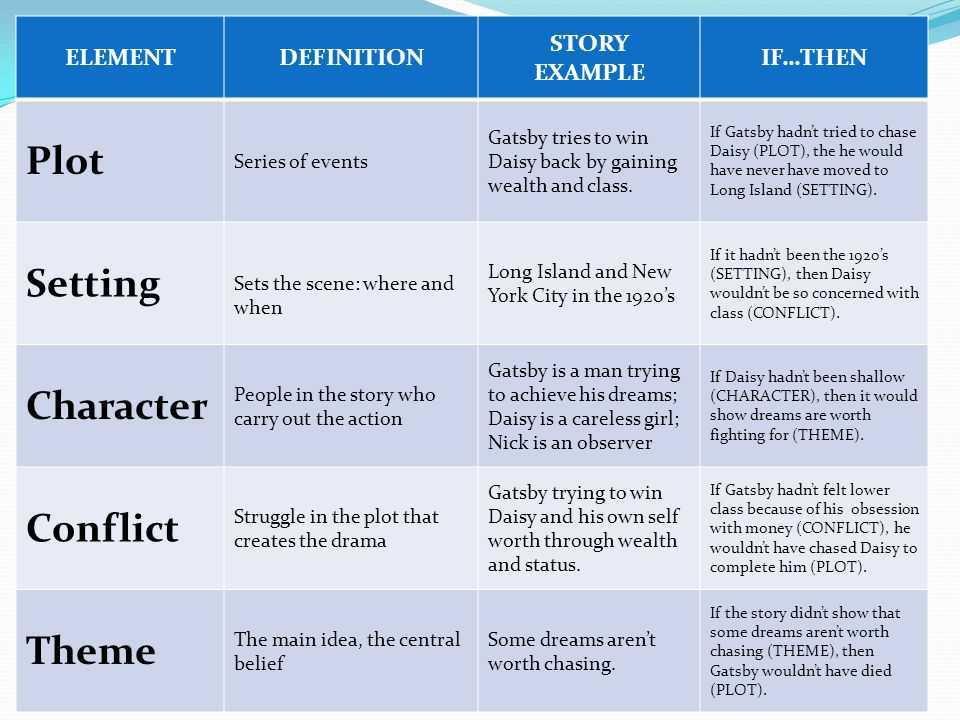 If you’re having medical tests to try to find out more about why you miscarried, you may need to wait until after you’ve had these tests to try to get pregnant again.
If you’re having medical tests to try to find out more about why you miscarried, you may need to wait until after you’ve had these tests to try to get pregnant again.
You may not be emotionally ready to try again so soon. Miscarriage can be hard to handle, and you may need time to grieve. It’s OK if you want to wait a while before trying to get pregnant again.
More information
From Hurt to Healing (free booklet from the March of Dimes for grieving parents)
Centering Corporation (grief information and resources)
Compassionate Friends (resources for families after the death of a child)
Journey Program of Seattle Children’s Hospital (resources for families after the death of a child)
Lupus Research Alliance: Pregnancy and family planning
Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
Last reviewed: February 2023
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and Risks- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
By Rena Goldman on October 3, 2018
Pregnancy loss may be more likely during the early weeks of pregnancy. It can occur for different reasons, including genetics and infections, among other causes.
It can occur for different reasons, including genetics and infections, among other causes.
Overview
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past.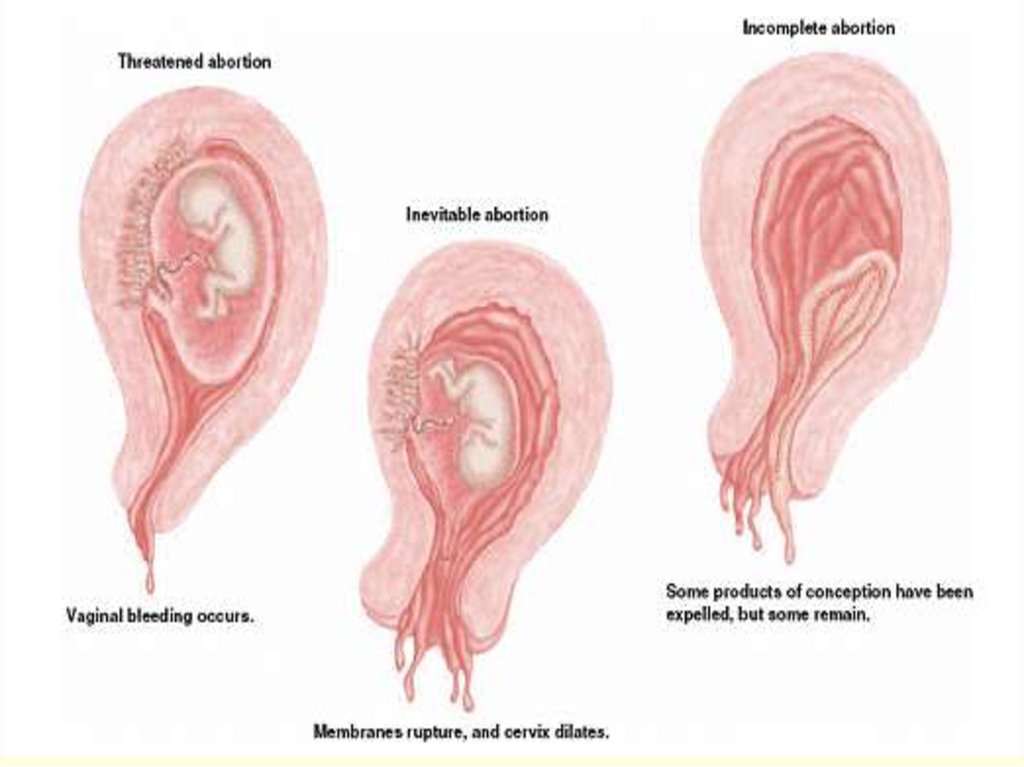 Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities.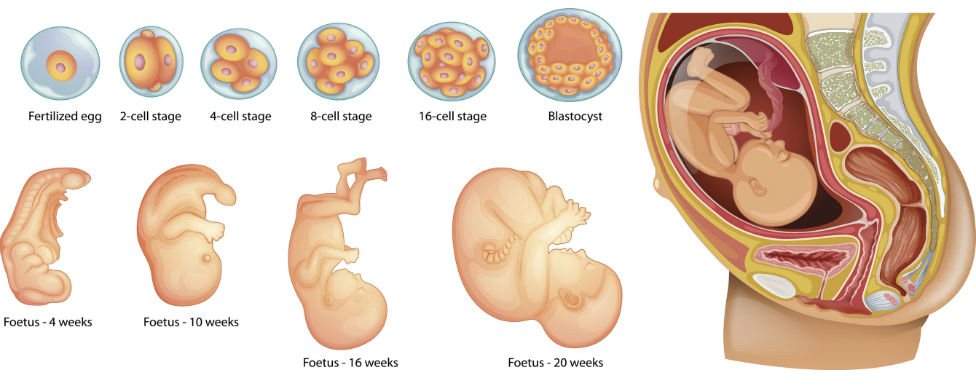 This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage. Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity. If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester. Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent.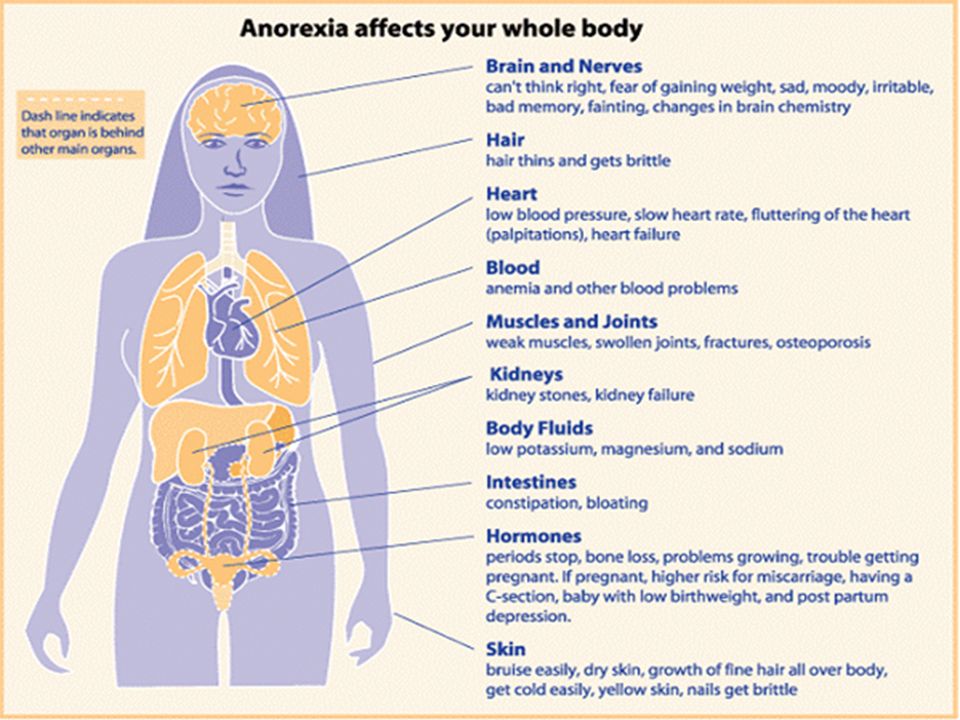 According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent. But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble. But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy. Here are some tips to staying healthy during pregnancy:
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive. A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.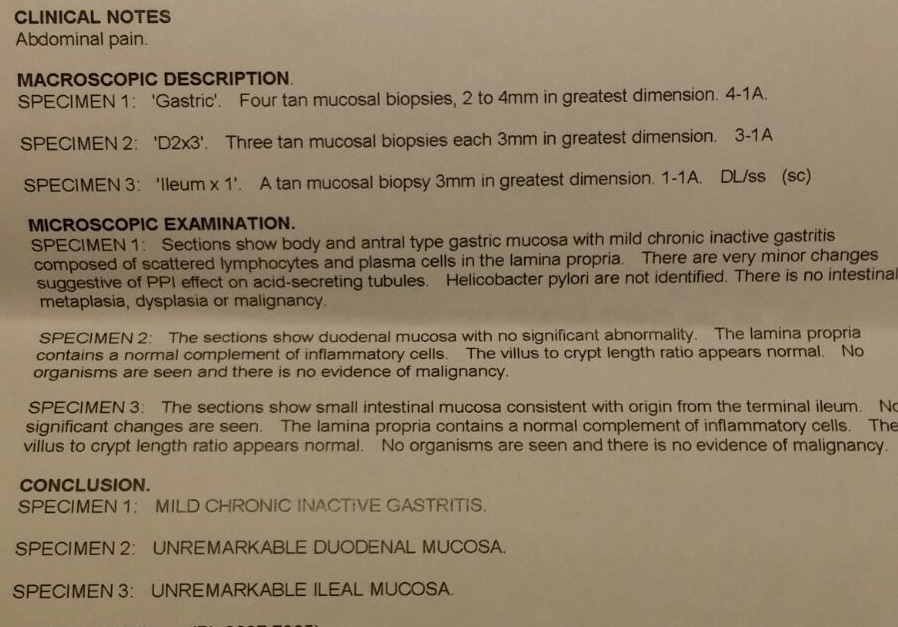 We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chromosomal conditions. (2018).
marchofdimes.org/baby/chromosomal-conditions.aspx - Early pregnancy loss: FAQs. (2015).
acog.org/Patients/FAQs/Early-Pregnancy-Loss - Early pregnancy loss: Practice bulletin. (2015).
acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Early-Pregnancy-Loss - Ford HB, et al. (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
ncbi.nlm.nih.gov/pmc/articles/PMC2709325/ - Maconochie N, et al. (2007). Risk factors for first-trimester miscarriage—results from a UK-population-based case-control study.
obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2006.01193.x - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage. aspx
aspx - Regan L, et al. (1989). Influence of past reproductive performance on risk of spontaneous abortion.
uptodate.com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19 - Repeated miscarriages. (2016).
acog.org/Patients/FAQs/Repeated-Miscarriages - Tong S, et al. (2008). Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit.
ncbi.nlm.nih.gov/pubmed/18310375 - Tulandi T. (2018). Patient information: Miscarriage (beyond the basics).
uptodate.com/contents/miscarriage-beyond-the-basics
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Rena Goldman
Edited By
Heather Hobbs
Share this article
By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.

READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
Orgasm During Pregnancy: Why It’s Fine (and How It’s Different)
If you're wondering if a pregnant orgasm feels different, here's why.
READ MORE
Miscarriage due to missed pregnancy | Articles by EMC doctors about diseases, diagnosis and treatment
What is a miscarriage?
According to medical statistics, miscarriage is the most common complication during pregnancy.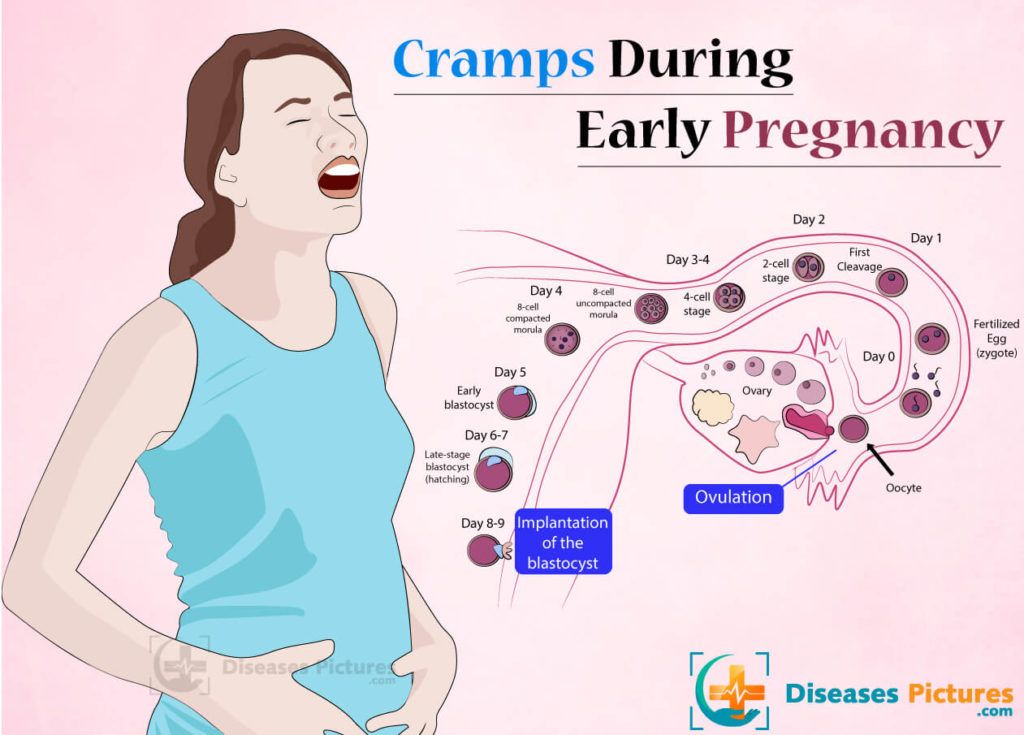 About 10-20% of all recorded pregnancies end in miscarriage. Miscarriage is a sporadic, sudden, termination of pregnancy, which is accompanied by complete or partial emptying of the uterus.
About 10-20% of all recorded pregnancies end in miscarriage. Miscarriage is a sporadic, sudden, termination of pregnancy, which is accompanied by complete or partial emptying of the uterus.
Missed pregnancy loss (MP) can be seen on ultrasound. It consists in confirming the non-viability of the fetus without bleeding. The ST can end in a miscarriage, when the body gets rid of the dead fetus on its own, or in a medical abortion, when medical or surgical manipulations are used to clean the uterine cavity.
Causes of miscarriage and miscarriage
80% of miscarriages occur in the first trimester before 12 weeks. In 50% of cases, this occurs due to genetic defects in the fetus. The threat of miscarriage due to chromosomal abnormalities decreases with the course of pregnancy: by 20 weeks it is 10-20% versus 41-50% in the first trimester. The main cause of genetically determined early miscarriages are autonomous trisomies - when three homologous chromosomes are present in the cells instead of two. Such defects occur at the time of conception and are not subject to correction. They lead to miscarriage or to the development of severe genetic diseases. In addition to genetics, immunological, endocrine and infectious causes are distinguished.
In the second trimester, various diseases and disorders in the mother's body become the main cause of miscarriage.
There is a list of factors that can trigger early pregnancy loss:
-
woman's age. At the age of 20-30 years, the risk of spontaneous miscarriage is 9-17%, at 35-40 years old - 20%, at 40-45 - 40%;
-
alcohol abuse;
-
abuse of caffeine;
-
smoking;
-
drug use;
-
chronic diseases of the mother;
-
maternal infections;
-
use of medications incompatible with pregnancy;
-
history of spontaneous abortion. The risk of subsequent pregnancy loss in women with one miscarriage in history is 18-20%, with two - 30%, with three - 43%.
Symptoms and signs of miscarriage
You can suspect a miscarriage by sudden spotting and sharp pain in the lower abdomen. If these symptoms appear, seek immediate medical attention. The doctor must conduct an ultrasound diagnosis. Transvaginal scanning (TVS) is considered the gold standard for diagnostics - when the sensor is inserted into the uterus through the vagina. If TVS is not available, a transabdominal scan can be applied - through the anterior abdominal wall.
Missed pregnancy may be asymptomatic and not manifest until the next scheduled ultrasound.
How does a miscarriage occur?
The miscarriage process has four stages. This does not happen overnight and lasts from several hours to several days.
The first stage - the threat of miscarriage. Among the symptoms: pulling pains in the lower abdomen, scanty blood discharge, increased uterine tone. The process of detachment of the placenta from the place of attachment in the uterus begins. The internal os is closed. The main thing is to seek help in time, then with proper therapy if there is a chance to stop the miscarriage and save the pregnancy.
The second stage - the beginning of a miscarriage. Strong discharge, the cervical canal is ajar, the doctor diagnoses the final detachment of the placenta.
The third stage is a miscarriage in progress. You can feel the regular contractions of the uterus, the outcome of the fetus, placenta and uterine contents, profuse blood discharge has begun.
The last fourth stage is a complete miscarriage. The pregnancy is interrupted, the uterine cavity does not contain the fetus and products of conception.
How to determine the ST?
It should be remembered that a miscarriage can be diagnosed only during an ultrasound examination. Home tests will not give reliable results. Ultrasound will show the presence or absence of a heartbeat in the fetus.
Treatment of miscarriage and miscarriage
Due to the fact that the vast majority of spontaneously terminated pregnancies are due to genetic abnormalities (non-viability) of the fetus, then, speaking about the treatment of miscarriage, it is worth talking about ensuring complete and safe cleansing of the uterus, preventing infection and preventing bruising. With the help of an ultrasound examination, the doctor will check whether the uterus has completely cleared. If yes, then no additional treatment is required. In the event of an incomplete miscarriage or STD, the patient will be indicated for surgical or medical cleaning. If the miscarriage is only in a state of threat, the treatment tactics will be aimed at blocking uterine contractions and stopping the development of a miscarriage. If you need treatment for a missed pregnancy in Moscow, contact our specialists.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen.
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy;
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramp-like pulling pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin. Pregnancy cannot be saved, cleaning is required;
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them.
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.