Muscle spasm early pregnancy
Leg cramps during pregnancy | Pregnancy Birth and Baby
Leg cramps during pregnancy | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Key facts
- Up to 3 in 10 people who are pregnant get leg cramps.
- Cramps are most common in your calf muscles.
- Cramps commonly happen at night in late pregnancy.
- To prevent leg cramps, try stretching your leg muscles before you go to bed and drink plenty of water.
- To ease a cramp, pull your toes up towards your ankle, rub the muscle, walk around or apply a heat pack.
What are leg cramps?
Leg cramps (pains) affect up to 3 in 10 people who are pregnant. They usually occur in your calf muscles, but can also occur in your thighs or feet. A cramp is a sign that your muscles are contracting very tightly when they shouldn’t be. This happens when acid builds up in your muscles.
Cramps usually happen at night. They are more common in your second and third trimesters.
Leg cramps are not the same as pelvic cramps.
What causes leg cramps during pregnancy?
There are many reasons suggested for cramps while you’re pregnant, such as changes to your metabolism, having a vitamin deficiency, being too active or not being active enough. However, nobody really knows why they occur in pregnancy.
How can I get rid of cramps?
To ease a leg cramp, you can try:
- stretching the muscle by pulling your toes hard up towards the front of your ankle
- rubbing the muscle firmly
- walking around
- a heat pack
If you have a partner, you could ask them to help.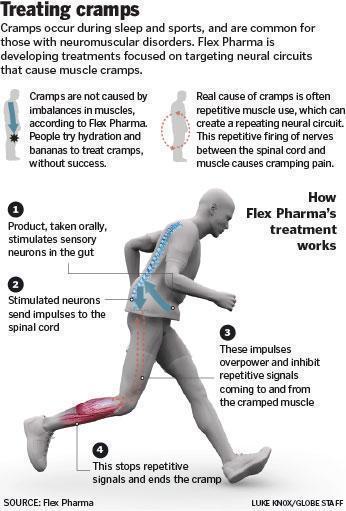
If your muscles are still sore after the cramp has gone, you can take paracetamol for pain relief.
How can I prevent leg cramps?
Things you can try that might help prevent cramps include:
- stretching your calf muscles before you go to bed
- drinking plenty of water
- having a warm bath before you go to bed
- eating a balanced diet
- avoiding stretching your leg while pointing your toes
Magnesium, calcium, vitamin B and vitamin C have been suggested as a treatment for cramps. It’s not clear whether any of these supplements work, but people often try magnesium and calcium. If you’re interested in trying supplements, talk to your doctor or midwife about whether they might be suitable for you.
When should I talk to my doctor or midwife about cramps?
If leg cramps are bothering you, talk to your doctor or midwife.
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.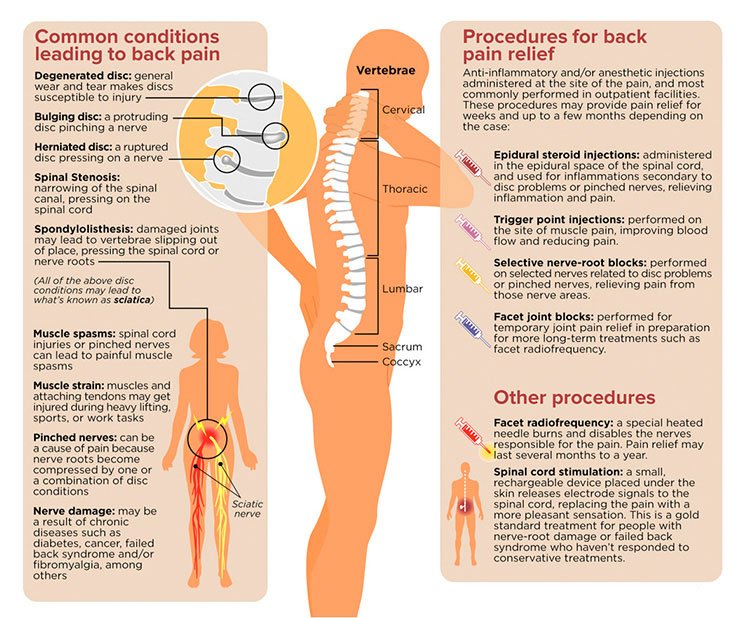
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Therapeutic Guidelines (Muscle cramps, including leg cramps in pregnant women), NSW Government (Having a baby), Queensland Health (6 weird things that may happen to your body during pregnancy), King Edward Memorial Hospital (Minor Symptoms or Disorders in Pregnancy King Edward Memorial Hospital Clinical Guidelines: Obstetrics & Midwifery), Queensland Health (VTE in pregnancy (a blood clot in the vein)), NPS (Magnesium, a treatment for leg cramps?), Royal Women’s Hospital (Common concerns in early pregnancy)Learn more here about the development and quality assurance of healthdirect content.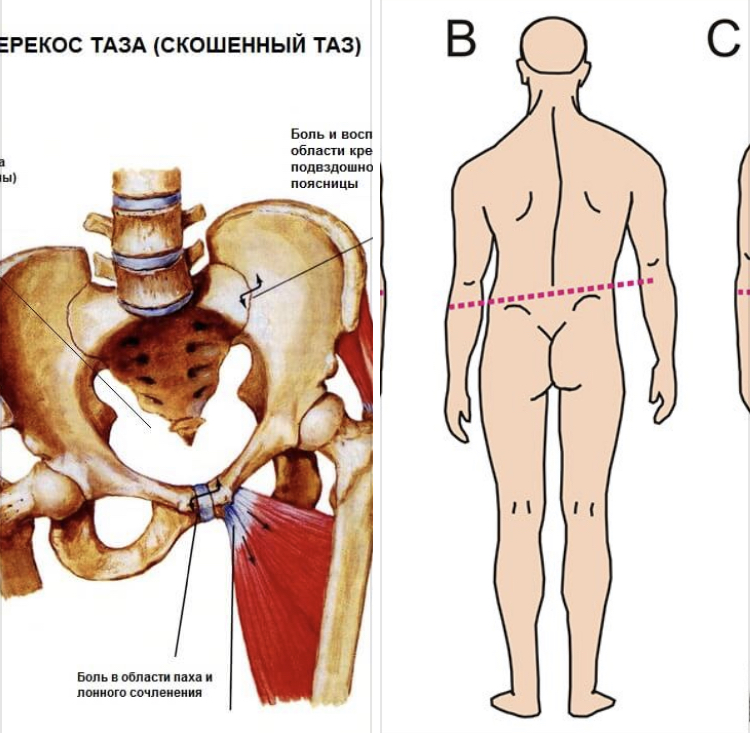
Last reviewed: July 2022
Back To Top
Related pages
- Swelling during pregnancy
- Varicose veins
- Common discomforts during pregnancy
Need more information?
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
The Pink Elephants Support Network - Miscarriage Treatment and Procedures
Early pregnancy loss is an individual experience, and the treatment and procedures around it are different for everyone.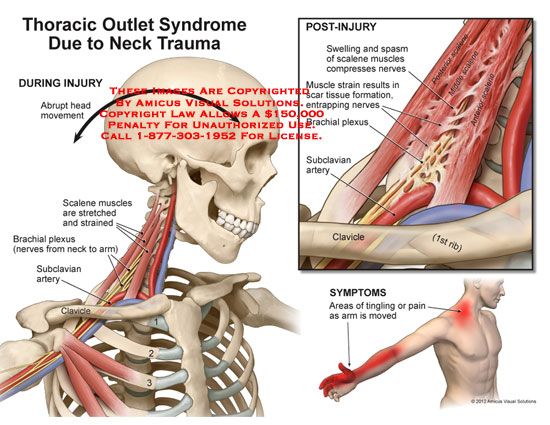 If you’ve been for an ultrasound and it’s been determined that you have lost your baby, there are several treatment options available.
If you’ve been for an ultrasound and it’s been determined that you have lost your baby, there are several treatment options available.
Read more on The Pink Elephants Support Network website
Am I having a miscarriage? - Miscarriage Australia
We describe the common signs or symptoms of miscarriage. Sometimes there are symptoms, but sometimes there aren't.
Read more on Miscarriage Australia website
Having a miscarriage - Miscarriage Australia
Here you can find information about the common symptoms of miscarriage, what happens during a miscarriage, and where to go for help.
Read more on Miscarriage Australia website
Pregnancy health problems & complications | Raising Children Network
Many pregnancy health problems are mild, but always call your doctor if you’re worried about symptoms.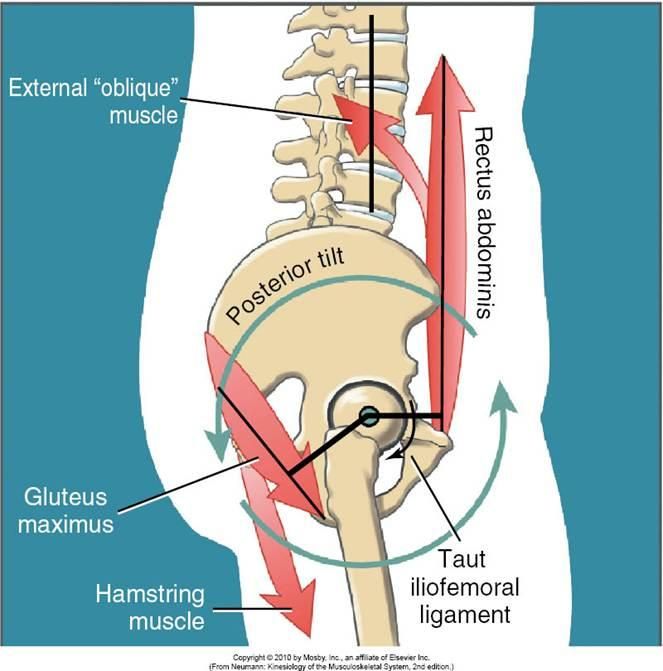 A healthy lifestyle can help you avoid health problems.
A healthy lifestyle can help you avoid health problems.
Read more on raisingchildren.net.au website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
Sleep during pregnancy
Sleep can become a problem when you're pregnant. Here are some tips to help you get as much sleep as possible so you’re ready for your baby's arrival.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 33
Your baby's brain and nervous system are now fully developed, and the baby is continuing to gain weight.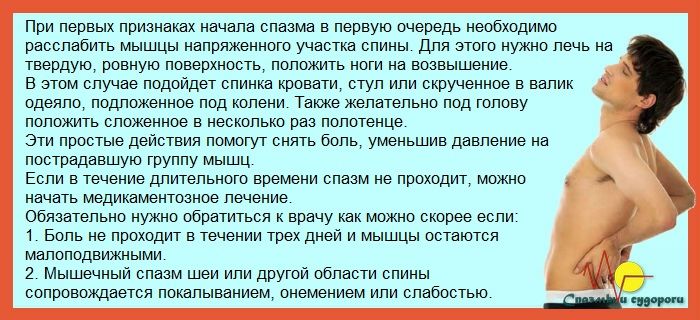 You'll probably also be feeling sore and tired.
You'll probably also be feeling sore and tired.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 25
As you are approaching the end of the second trimester, you might be starting to feel a bit uncomfortable as your baby continues to grow.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How to Manage Back Spasms During Pregnancy
How to Manage Back Spasms During Pregnancy- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Joe Bowman on November 9, 2017
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Joe Bowman on November 9, 2017
Pregnancy can be an exciting time for expectant mothers, but just as bringing a child into the world opens a lot of new doors, pregnancy can bring about new, sometimes uncomfortable sensations for a mother-to-be. One of the most common complaints during pregnancy is back pain and, specifically, back spasms.
“Pregnancy is like the perfect storm for lower back pains and spasms,” explains Dr. Steve Behram, an OB/GYN based in Rockville, Maryland. “Generally speaking, pregnancy can also make women more vulnerable to generalized muscular spasms anywhere, including the back.”
There are a few different explanations as to why back spasms affect pregnant women. The first reason is perhaps the most obvious: weight gain. Pregnancy can cause women to gain significant weight, especially in the abdominal region of the body. This shifts the woman’s center of gravity and tends to adjust posture.
While back spasms are often harmless irritations, they can also be symptomatic of some additional complications.
“Sometimes the referred pain from uterine contractions is misinterpreted as back pain and back spasms,” Behram says. “Uterine contractions can cause referred pain to the back.”
It is important to determine if your back pain is due to uterine contractions. Uterine contractions can be a sign of premature labor. The University of California, San Francisco recommends that you seek medical assistance if uterine contractions occur six or more times within an hour, with or without additional warning signs. In real labor, contractions get longer, stronger, and closer together. Sometimes, contractions are only felt in the lower back, which means the pain you’re experiencing may be contractions. Time them.
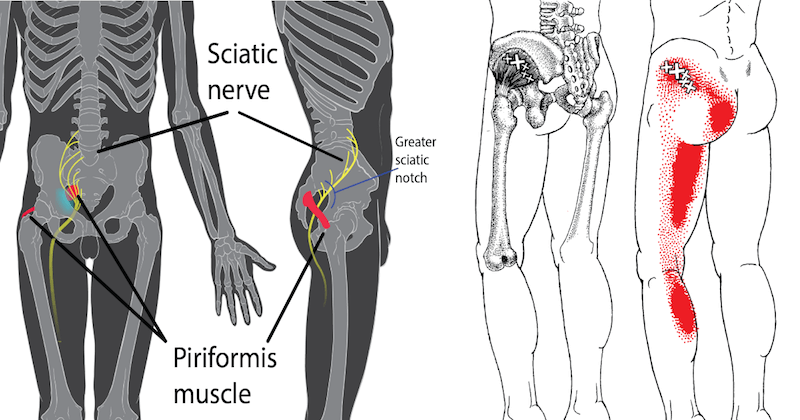
Sciatica, which is pain caused by the sciatic nerve that connects the lower back to each leg through the hips, can also be misdiagnosed as back spasms. Be sure to consult your doctor if your back spasms are accompanied by radiation of pain down one or both legs.
So how does one eliminate back spasms or reduce their frequency? Behram suggests applying heat or ice to the lower back for short durations (under 10 minutes) when you feel spasms.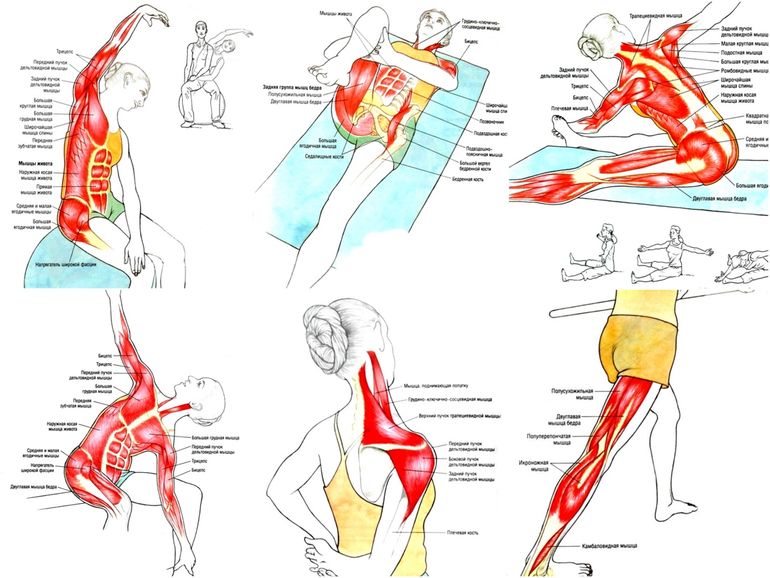
Relaxation and massage therapies can also be extremely beneficial. “Patients should inquire and be assured that their massage therapist is certified in pregnancy message, and has the appropriate equipment for expectant moms,” suggests Behram. Acupuncture can alleviate some of the discomfort caused by back spasms.
Stretches can also soothe back spasms, but expectant mothers should proceed with caution. Behram recommends keeping it simple with some easy leg raises in a reclined position. Over-stretching the back muscles can exacerbate the spasms and lead to even more discomfort.
Transcutaneous electrical nerve stimulation (TENS) has been used by physical therapists for years. Laboring women have used TENS as a noninvasive method of managing labor pains. TENS has been found to be a safe and inexpensive treatment for low back pain in late pregnancy. TENS units are available for purchase in one-time use and rechargeable units.
Behram warns against treating back spasms with medication, noting, “Most medications cannot be used safely during pregnancy. ”
”
Thankfully, back spasms during pregnancy are usually just a nuisance and not cause for alarm. Be sure to check with your doctor if the spasms become more frequent or painful.
Last medically reviewed on November 9, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Foster NE, et al. (2016). Evaluating acupuncture and standard care for pregnant women with back pain (EASE Back): A feasibility study and pilot randomised trial.
ncbi.nlm.nih.gov/books/NBK360953/ - Mayo Clinic Staff. (2016). Back pain during pregnancy: 7 tips for relief.
mayoclinic. org/healthy-living/pregnancy-week-by-week/in-depth/pregnancy/art-20046080
org/healthy-living/pregnancy-week-by-week/in-depth/pregnancy/art-20046080 - Mayo Clinic Staff. (2017). Pregnancy weight gain: What’s healthy?
mayoclinic.org/healthy-living/pregnancy-week-by-week/in-depth/pregnancy-weight-gain/art-20044360 - Mayo Clinic Staff. (2015). Sciatica: Definition.
mayoclinic.org/diseases-conditions/sciatica/basics/definition/con-20026478 - Quittan M, et al. (2016). Transcutaneous electrical nerve stimulation (TENS) in patients with pregnancy-induced low back pain and/or pelvic girdle pain. DOI:
10.1055/s-0035-1565058 - Recognizing premature labor. (2017).
ucsfhealth.org/education/recognizing_premature_labor/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 9, 2017
Written By
Joe Bowman
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.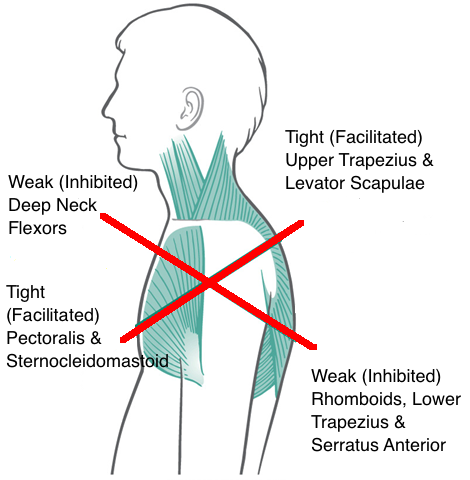 D., MSN, R.N., IBCLC, AHN-BC, CHT — By Joe Bowman on November 9, 2017
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Joe Bowman on November 9, 2017
related stories
Is a Heating Pad Safe for Back or Belly While Pregnant?
Understanding and Treating Lower Back Spasms
How to Deal with Butt Pain During Pregnancy
The 7 Best Natural Muscle Relaxers
Pregnancy Yoga Stretches for Back, Hips, and Legs
Read this next
Is a Heating Pad Safe for Back or Belly While Pregnant?
Medically reviewed by Michael Weber, MD
Many pregnant women experience aches and pains, but wonder if it’s safe to use a heating pad for relief. Here’s what you should know.
READ MORE
Understanding and Treating Lower Back Spasms
Medically reviewed by Gregory Minnis, DPT
Learn how to treat lower back spasms and how to prevent the pain in this article.

READ MORE
How to Deal with Butt Pain During Pregnancy
Medically reviewed by Janine Kelbach, RNC-OB
Many pregnant women report butt pain as a symptom during the third trimester. These treatment options will help you stay comfortable until delivery.
READ MORE
The 7 Best Natural Muscle Relaxers
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
If you experience muscle spasms as a symptom of fibromyalgia, natural muscle relaxers such as magnesium and cayenne pepper could provide relief.
READ MORE
Pregnancy Yoga Stretches for Back, Hips, and Legs
Medically reviewed by Peggy Pletcher, M.S., R.D., L.D., CDE
Practicing yoga during pregnancy can help ease some of your aches and pains. Follow this gentle routine to stretch and relax your muscles.
READ MORE
Orgasm During Pregnancy: Why It’s Fine (and How It’s Different)
If you're wondering if a pregnant orgasm feels different, here's why.
READ MORE
Joy Is Our Birthright: Striving for Black Maternal Health Equity
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Black Maternal Health Week was created to reduce disparities Black women and birthing people face today. Here are 5 solutions that can help.
READ MORE
Anemia in Pregnancy: What It Is and How to Prevent It
Anemia is common during pregnancy. Here’s how to prevent and treat anemia in pregnancy with healthy foods, supplements, and more.
READ MORE
How to Support Black Mothers and Parents with Postpartum Depression
Medically reviewed by Mia Armstrong, MD
Due to medical and social biases, Black mothers are more likely to experience postpartum depression than any other group.
 Let's look at why and how to…
Let's look at why and how to…READ MORE
The Best Gift for New Dads Just in Time for Father's Day
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
It's not usually dad who is showered with gifts when a new baby comes, but why not? He deserves appreciation too! Here are our picks of the best new…
READ MORE
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
— What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
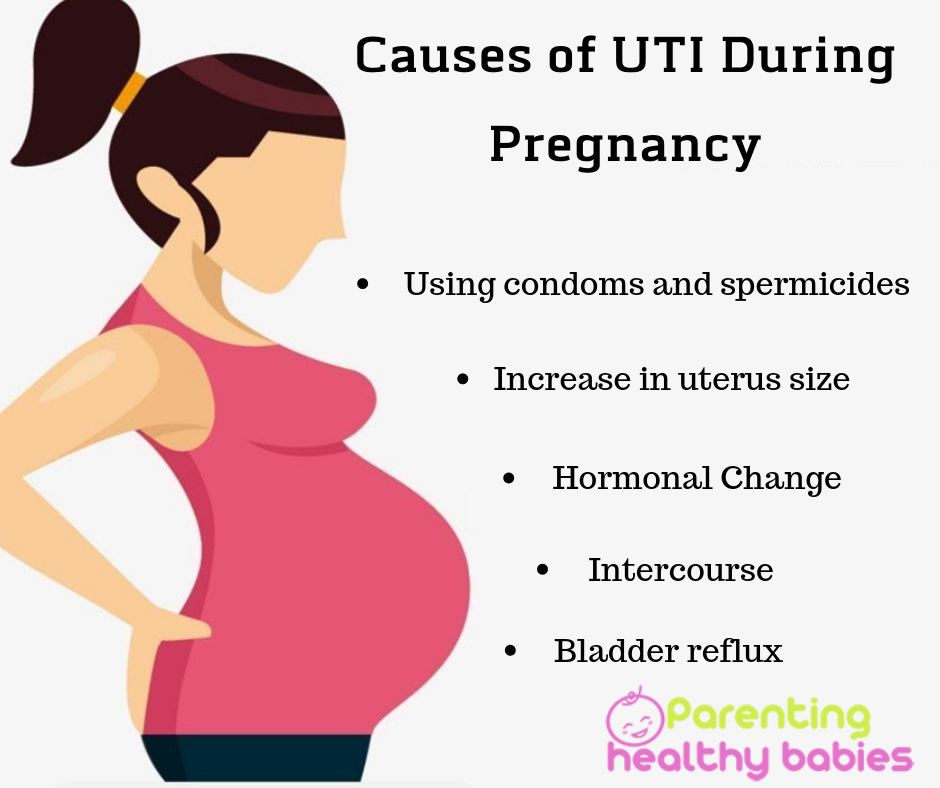
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and the cartilages that connect the pubic bones are affected. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot).
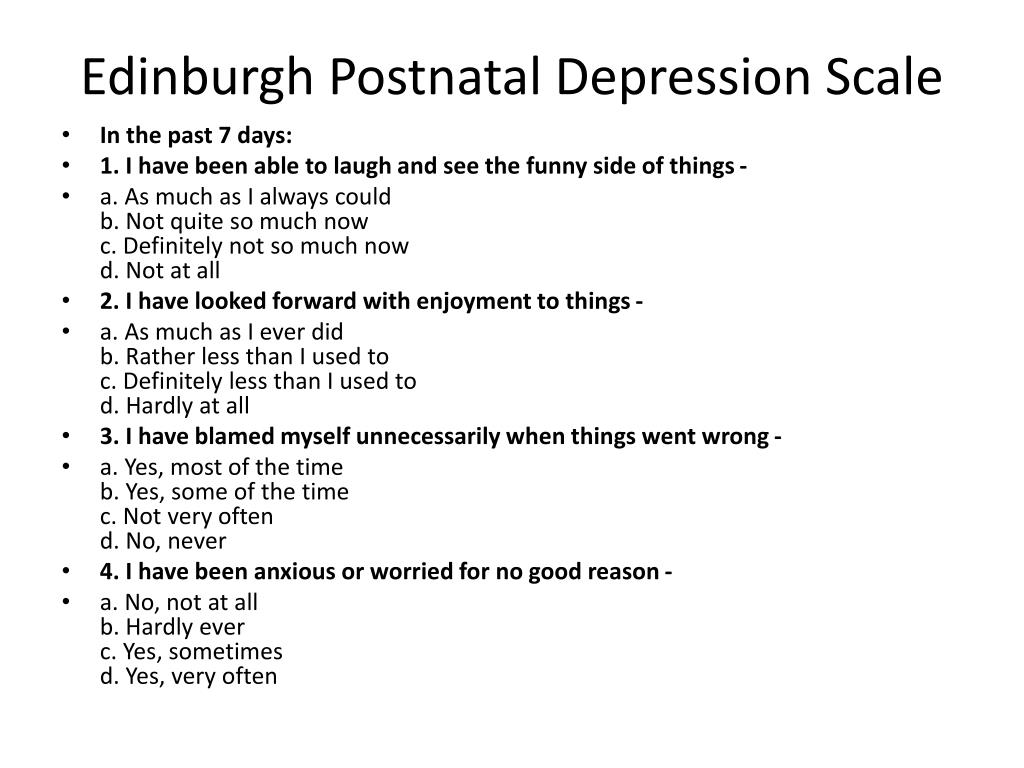
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence. Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.
The question is asked by Natalia, - a question-answer from the specialists of the clinic "Mother and Child"
Natalia:
23.10.2014
Hello! I really need your help. I am 10 weeks pregnant. (Last period July 26) This is my third pregnancy. The first one went well without complications and in 2001 I gave birth to a healthy boy. True, she gave birth with ruptures and there was a divergence of the sutures in the vagina, but after the birth it did not bother me at all. The second time the pregnancy ended at 9weeks of abortion, because the doctors said that the pregnancy stopped ... After that, I once again passed all the tests - they all gave a negative. the result, except for ureaplasmosis () but I had it in my first pregnancy and I did not treat it with anything. In March last year, my husband and I were completely treated and here is a new pregnancy. But since the 4th week, my lower abdomen has been constantly hurting. Was at the reception: at 6 weeks they did an ultrasound scan, everything is fine with the child, the development is acc. term, but the uterus is in good shape. I took a course of duphaston for 10 days, 1 tab. 2 times a day, suppositories with papaverine-2r / d, and intramuscularly 5 injections of hCG (1 time / d every other day). There were no discharges and there are none, but the stomach still hurts. I passed hormonal tests: DHA-1, 5 (at a rate of up to 1, 3), all tests for infections (there is immunity to rubella, cytomegalovirus, the rest are negative), TSH, hCG, testosterone, progesterone are normal. The doctor prescribed dexamethasone 1r / d for 1/4, but in the annotation I read that in the first trimester it is possible only for health reasons.
the result, except for ureaplasmosis () but I had it in my first pregnancy and I did not treat it with anything. In March last year, my husband and I were completely treated and here is a new pregnancy. But since the 4th week, my lower abdomen has been constantly hurting. Was at the reception: at 6 weeks they did an ultrasound scan, everything is fine with the child, the development is acc. term, but the uterus is in good shape. I took a course of duphaston for 10 days, 1 tab. 2 times a day, suppositories with papaverine-2r / d, and intramuscularly 5 injections of hCG (1 time / d every other day). There were no discharges and there are none, but the stomach still hurts. I passed hormonal tests: DHA-1, 5 (at a rate of up to 1, 3), all tests for infections (there is immunity to rubella, cytomegalovirus, the rest are negative), TSH, hCG, testosterone, progesterone are normal. The doctor prescribed dexamethasone 1r / d for 1/4, but in the annotation I read that in the first trimester it is possible only for health reasons. Even at 6 weeks for 3 days there was a severe runny nose with lacrimation, it was very hard to endure. Could this have affected the child? Please, I know you have a lot of questions, but I really need your answer. Why can the stomach hurt and is it dangerous for the child - we really want a healthy child! And is it necessary to take dexamethasone, maybe you can get by with less dangerous means, please advise?! Thank you in advance, good health to you and your loved ones.
Clinic "Mother and Child" Kuntsevo:
01/26/2021
Dear Natalia, Drawing pains in the lower abdomen is a fairly common symptom in the first 12-14 weeks of pregnancy. If all the data (tests, ultrasound) are within the normal range, this indicates a normal pregnancy. Pregnancy develops in the uterus, the uterus is a muscular organ, the property of the muscle is sometimes reduced and this is the norm. These contractions can be manifested by pulling sensations in the lower abdomen. These pulling pains do not carry any risk for the development of the baby.