Common complications in pregnancy
Complications of Pregnancy | Johns Hopkins Medicine
What are some of the more common complications of pregnancy?
Although the majority of pregnancies are uneventful, sometimes complications do happen. The following are some of the more common pregnancy complications.
Amniotic fluid complications
Too much or too little amniotic fluid in the sac around the fetus may be a sign of a problem with the pregnancy. Too much fluid can put too much pressure on the mother's uterus, leading to preterm labor. It also can cause pressure on the mother's diaphragm. This can lead to breathing difficulties. Fluids tend to build up in cases of uncontrolled diabetes, a multiple pregnancy, incompatible blood types, or birth defects. Too little fluid may be a sign of birth defects, growth retardation, or stillbirth.
Bleeding
Bleeding in late pregnancy may be a sign of placental complications, a vaginal or cervical infection, or preterm labor. Women who bleed in late pregnancy may be at greater risk of losing the fetus and bleeding excessively. Bleeding at any time during the pregnancy should be reported to your healthcare provider right away.
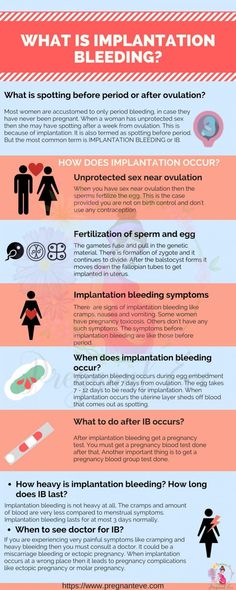
Ectopic pregnancy
An ectopic pregnancy is the development of the fetus outside of the uterus. This can happen in the fallopian tubes, cervical canal, or the pelvic or belly. The cause of an ectopic pregnancy is usually scar tissue in the fallopian tube from infection or disease. The risk of ectopic pregnancy is increased in women who have had tubal sterilization procedures, especially women who were younger than age 30 at the time of sterilization.
Ectopic pregnancies happen in about 1 out of 50 pregnancies and can be very dangerous to the mother. Symptoms may include spotting and cramping. The longer an ectopic pregnancy goes on, the greater the chance that a fallopian tube will rupture. An ultrasound and blood tests may confirm the diagnosis. Treatment of an ectopic pregnancy may include medicine or surgical removal of the fetus.
Miscarriage or fetal loss
A miscarriage is pregnancy loss that happens up to 20 weeks of gestation.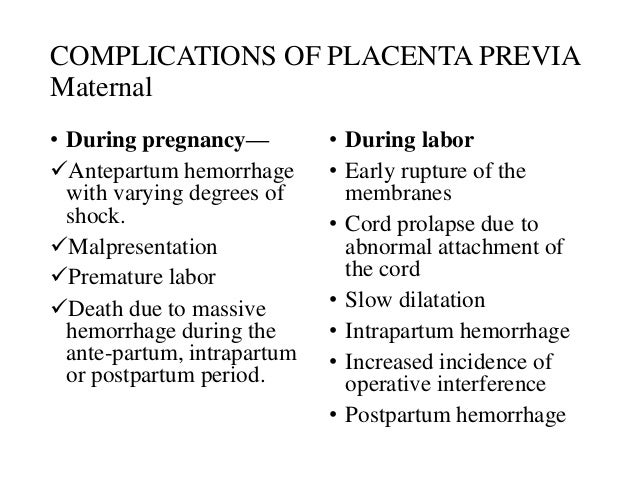 Most miscarriages happen before 12 weeks. Miscarriages happen in about 15% of all pregnancies and are usually due to genetic or chromosomal abnormalities.
Most miscarriages happen before 12 weeks. Miscarriages happen in about 15% of all pregnancies and are usually due to genetic or chromosomal abnormalities.
Miscarriages are usually preceded by spotting and intense cramping. To confirm a miscarriage, an ultrasound and blood tests may be done. The fetus and contents of the uterus are often naturally expelled. If this does not happen, a procedure called a dilation and curettage (D & C) may be necessary. This procedure uses special instruments to remove the abnormal pregnancy.
Fetal loss in the second trimester may happen if the cervix is weak and opens too early. This is called incompetent cervix. In some cases of incompetent cervix, a healthcare provider can help prevent pregnancy loss by stitching the cervix closed until delivery.
Placental complications
Under normal circumstances, the placenta attaches to the uterine wall. However, two types of placental complications may happen, including:
Placental abruption is more common in women who smoke, have high blood pressure, and/or have a multiple pregnancy. It also happens in women who have had previous children or a history of placental abruption. Symptoms and treatment of placental abruption depend on the degree of detachment. Symptoms may include bleeding, cramping, and belly tenderness. Diagnosis is usually confirmed by doing a complete physical exam and an ultrasound. Women are usually put in the hospital for this condition. They may have to deliver the baby early.
It also happens in women who have had previous children or a history of placental abruption. Symptoms and treatment of placental abruption depend on the degree of detachment. Symptoms may include bleeding, cramping, and belly tenderness. Diagnosis is usually confirmed by doing a complete physical exam and an ultrasound. Women are usually put in the hospital for this condition. They may have to deliver the baby early.
Placenta previa. Normally, the placenta is located in the upper part of the uterus. Placenta previa is a condition in which the placenta is attached close to or covering the cervix (the opening into the uterus). This type of placental complication happens in about 1 in every 200 deliveries and happens more often in women who have scarring of the uterus from previous pregnancies. It also happens in women who have fibroids or other problems in the uterus, or in women who have had previous uterine surgeries.
Symptoms may include vaginal bleeding that is bright red and not associated with belly tenderness or pain. Diagnosis is confirmed by doing a physical exam and an ultrasound. Depending on how bad the problem is and the stage of pregnancy, a change in activities or bed rest may be ordered. The baby usually has to be delivered by cesarean section to keep the placenta from detaching early and depriving the baby of oxygen during delivery.
Diagnosis is confirmed by doing a physical exam and an ultrasound. Depending on how bad the problem is and the stage of pregnancy, a change in activities or bed rest may be ordered. The baby usually has to be delivered by cesarean section to keep the placenta from detaching early and depriving the baby of oxygen during delivery.
Preeclampsia or eclampsia
Preeclampsia, formerly called toxemia, is characterized by pregnancy-induced high blood pressure. It is accompanied by protein in the urine. Sometimes swelling due to fluid retention is also present. Eclampsia is the more severe form of this problem. This can lead to seizures, coma, or even death.
The cause of preeclampsia is unknown, but it is more common in first pregnancies. It affects about 5% to 8% of all pregnant women. Other risk factors for preeclampsia include:
A woman carrying multiple fetuses
A teenage mother
A woman older than 40
A woman with high blood pressure, diabetes, and/or kidney disease before she became pregnant
A woman who is obese with a BMI greater than 30
Symptoms may include severe swelling of the hands and face, high blood pressure, headache, dizziness, irritability, decreased urine output, belly pain, and blurred vision.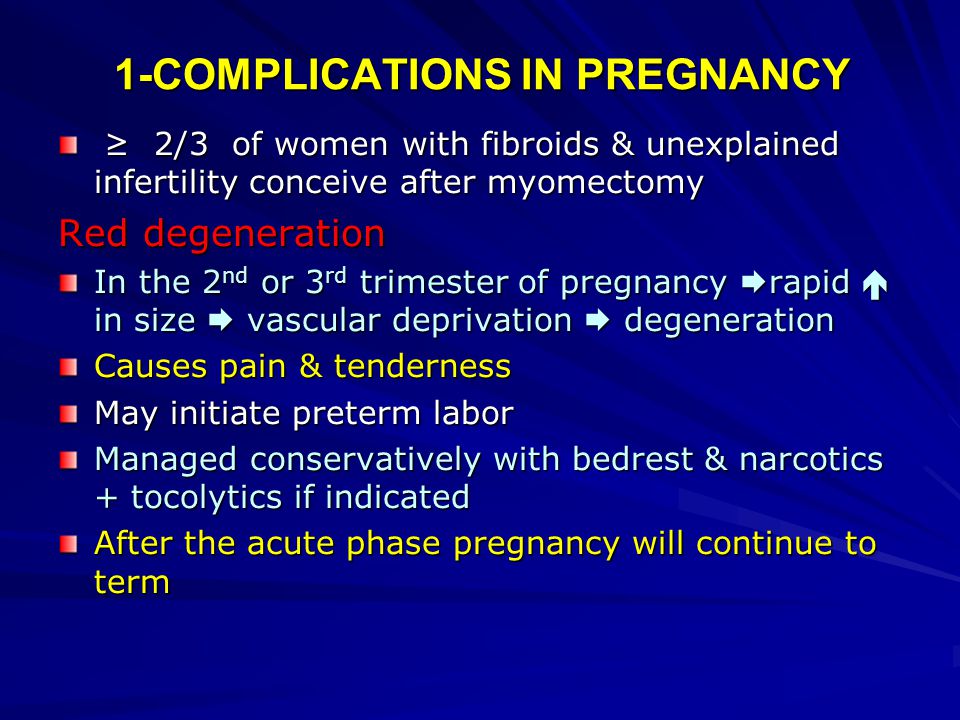 Treatment will vary according to the severity of the condition and the stage of the pregnancy. Treatment may include hospitalization, bed rest, medicine to lower blood pressure, and close monitoring of both the fetus and the mother.
Treatment will vary according to the severity of the condition and the stage of the pregnancy. Treatment may include hospitalization, bed rest, medicine to lower blood pressure, and close monitoring of both the fetus and the mother.
Pregnancy Complications | Maternal and Infant Health
The following are some common conditions that can happen before, during, or after pregnancy. You can help prevent and manage them by seeing a health care provider regularly before, during, and after your pregnancy.
Anemia
Anemia is having lower than the normal number of healthy red blood cells. People with anemia may feel tired and weak. You are more likely to get iron-deficiency anemia during pregnancy because your body needs more iron than normal. Your health care provider will check your number of red blood cells during your pregnancy. Treating the underlying cause of the anemia, if possible, can help restore the number of healthy red blood cells. Your provider may also recommend you take iron and/or folic acid supplements to help prevent and manage anemia.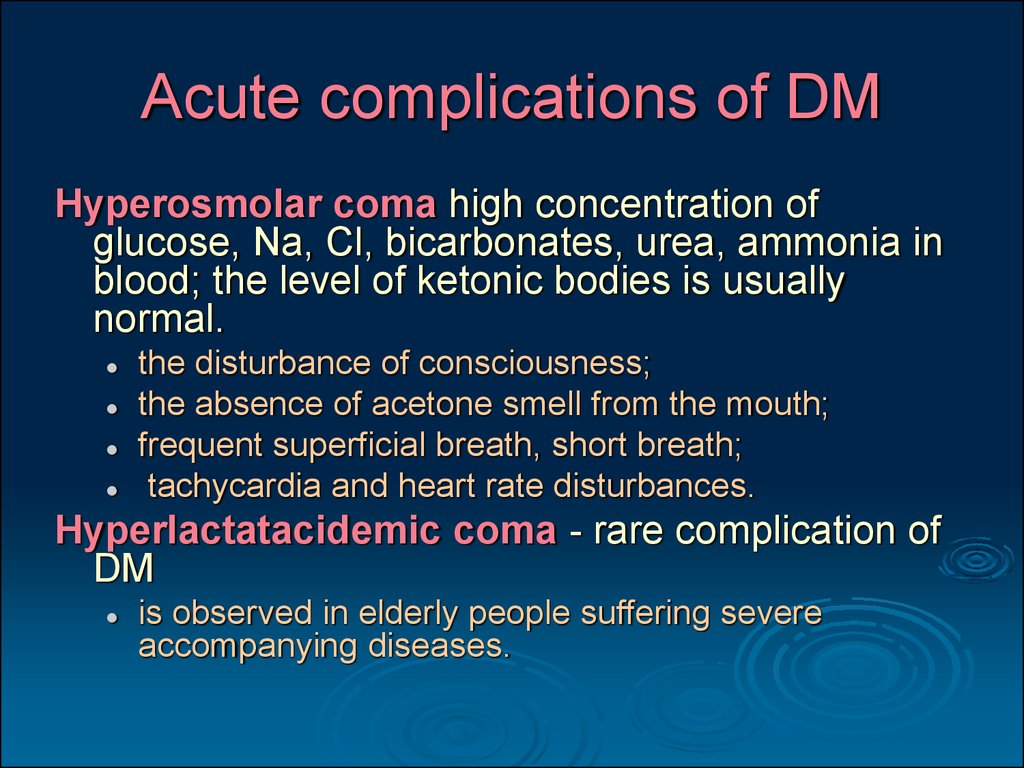
Anxiety
Anxiety disorders are common before, during, and after pregnancy. If you have an anxiety disorder, you may struggle with uncontrollable feelings of anxiety, nervousness, fear, worry, and/or panic. These feelings can be intense and may last a long time. They can also interfere with relationships and daily activities, such as work or school. Anxiety disorders often occur with depression. Getting treatment for anxiety before, during, and after pregnancy is important. Talk to your health care provider as soon as possible if you think you have an anxiety disorder.
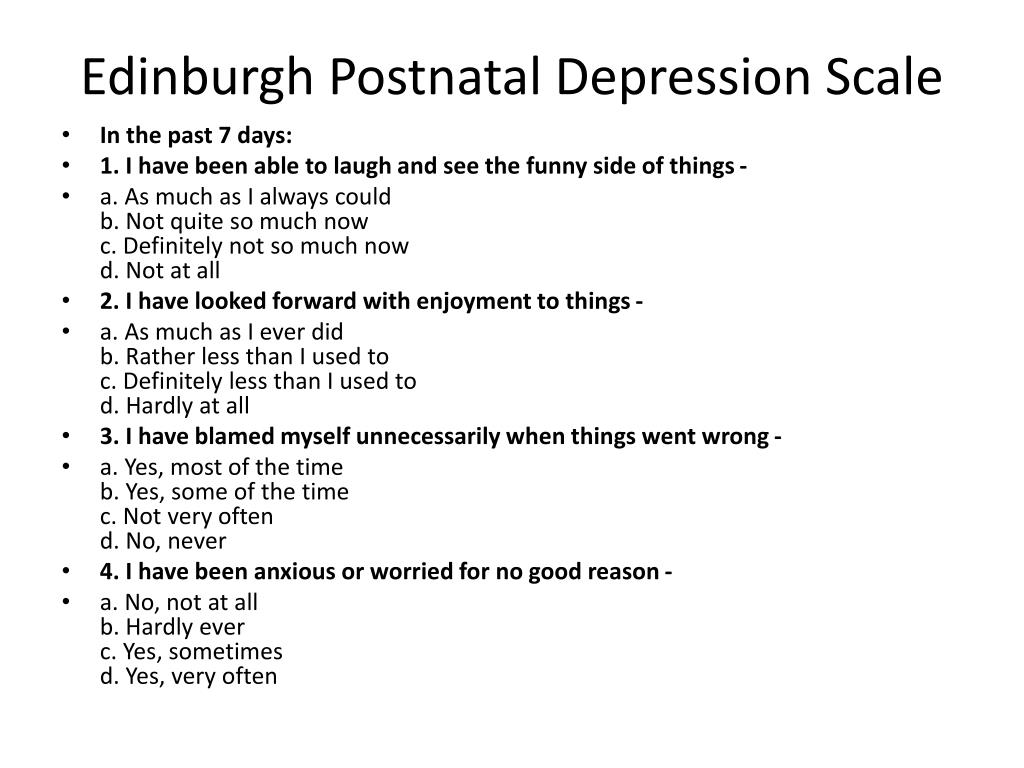
Depression
Everyone feels sad sometimes, but these feelings usually pass in a few days. Depression interferes with daily life and may last for weeks or months at a time. Some people have depression before, during, or after pregnancy. Symptoms of depression include:
- Lasting sad, anxious, or “empty” mood.
- Feelings of hopelessness or pessimism.
- Loss of energy.
- Trouble falling asleep or sleeping too much.
- Overeating or loss of appetite.
- Feelings of irritability or restlessness.
- Problems concentrating, recalling details, and making decisions.
- Feelings of guilt, worthlessness, or helplessness.
- Suicidal thoughts or suicide attempts.
If you have many of these symptoms together, and they last more than 2 weeks, you may have depression. Depression during pregnancy can make it hard for you to care for yourself and your pregnancy. Having depression before or during pregnancy is also a risk factor for postpartum depression, which is depression that occurs after pregnancy. Getting treatment is important for both mother and baby. Talk to your health care provider as soon as possible if you think you have depression. If you have thoughts of harming yourself or your baby, seek medical care immediately. More information is available at Depression During and After Pregnancy.
Top of Page
Diabetes
Diabetes is a disease that affects how your body turns food into energy. There are three main types of diabetes: type 1, type 2, and gestational diabetes. For pregnant people with type 1 or type 2 diabetes, high blood sugar around the time of conception increases the risk of birth defects, stillbirth, and preterm birth. Among people with any type of diabetes, high blood sugar throughout pregnancy can also increase the risk of preeclampsia, cesarean delivery, and the baby being born too large. To manage your diabetes, see your doctor as recommended, monitor your blood sugar levels, follow a good nutrition plan developed with your provider or dietician, be physically active, and take insulin, if directed. Managing diabetes can help you have a healthy pregnancy. If you have diabetes before pregnancy or develop it during pregnancy, it’s important to continue seeing your health care provider after pregnancy to monitor your blood sugar and overall health.
There are three main types of diabetes: type 1, type 2, and gestational diabetes. For pregnant people with type 1 or type 2 diabetes, high blood sugar around the time of conception increases the risk of birth defects, stillbirth, and preterm birth. Among people with any type of diabetes, high blood sugar throughout pregnancy can also increase the risk of preeclampsia, cesarean delivery, and the baby being born too large. To manage your diabetes, see your doctor as recommended, monitor your blood sugar levels, follow a good nutrition plan developed with your provider or dietician, be physically active, and take insulin, if directed. Managing diabetes can help you have a healthy pregnancy. If you have diabetes before pregnancy or develop it during pregnancy, it’s important to continue seeing your health care provider after pregnancy to monitor your blood sugar and overall health.
Top of Page
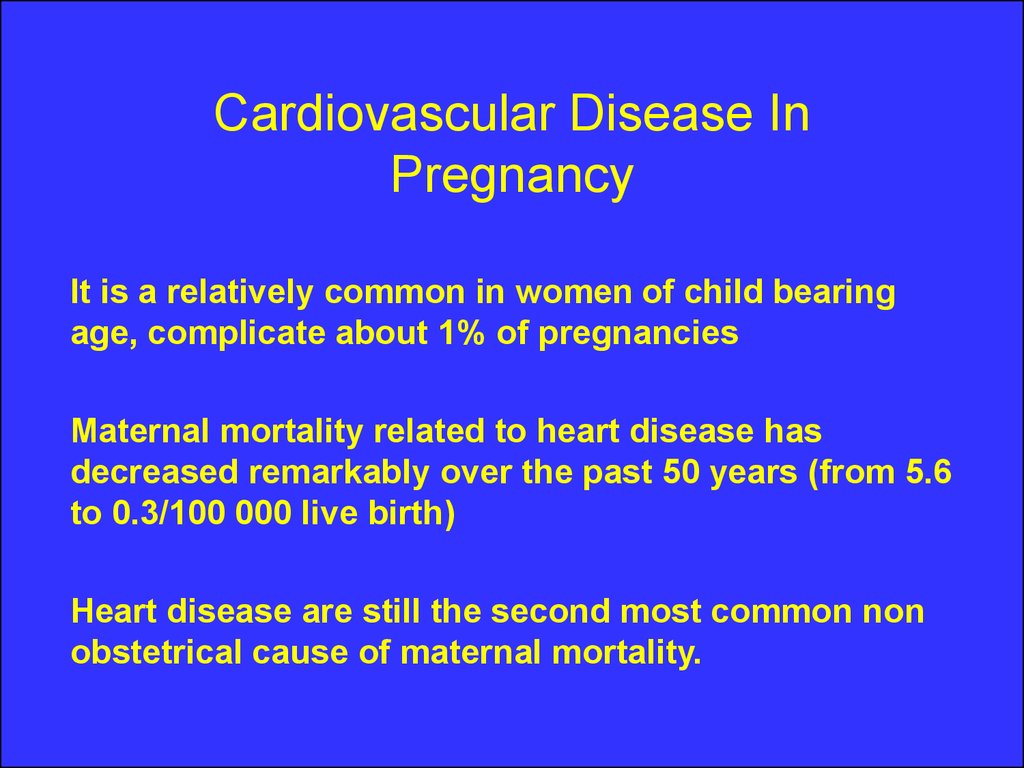
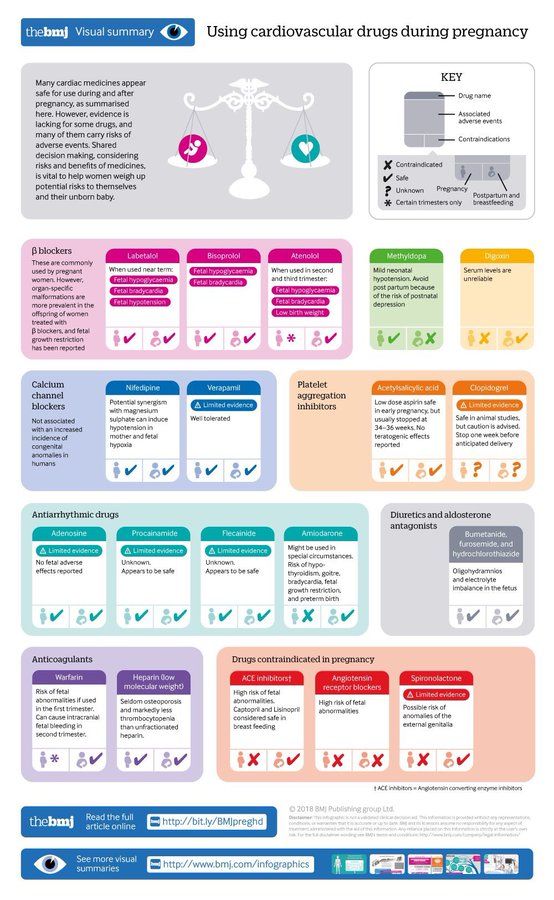
Heart Conditions
Heart conditions, such as coronary artery disease, heart attack, cardiomyopathy, and congenital heart defects, impact the heart and blood vessels. Making healthy food choices, limiting your alcohol intake, quitting smoking if you smoke, and managing any other chronic conditions can help reduce your risk for many heart conditions. Not everyone has symptoms, but you may feel neck, jaw, chest, belly, or back pain if you have a heart condition. Many people with heart conditions have healthy, uneventful pregnancies, but pregnancy can put stress on the heart of people with some types of heart conditions. Having a heart condition may increase the risk of severe illness and death during and after pregnancy.
Making healthy food choices, limiting your alcohol intake, quitting smoking if you smoke, and managing any other chronic conditions can help reduce your risk for many heart conditions. Not everyone has symptoms, but you may feel neck, jaw, chest, belly, or back pain if you have a heart condition. Many people with heart conditions have healthy, uneventful pregnancies, but pregnancy can put stress on the heart of people with some types of heart conditions. Having a heart condition may increase the risk of severe illness and death during and after pregnancy.
If you have a heart condition, it’s important to see your health care provider, ideally before pregnancy or as soon as possible after becoming pregnant. During your first prenatal care visit, let your provider know if you have a heart condition. If you are diagnosed with a heart condition during pregnancy, you may also need to be monitored by your provider earlier or more often after pregnancy. More information can be found at Heart Health and Pregnancy.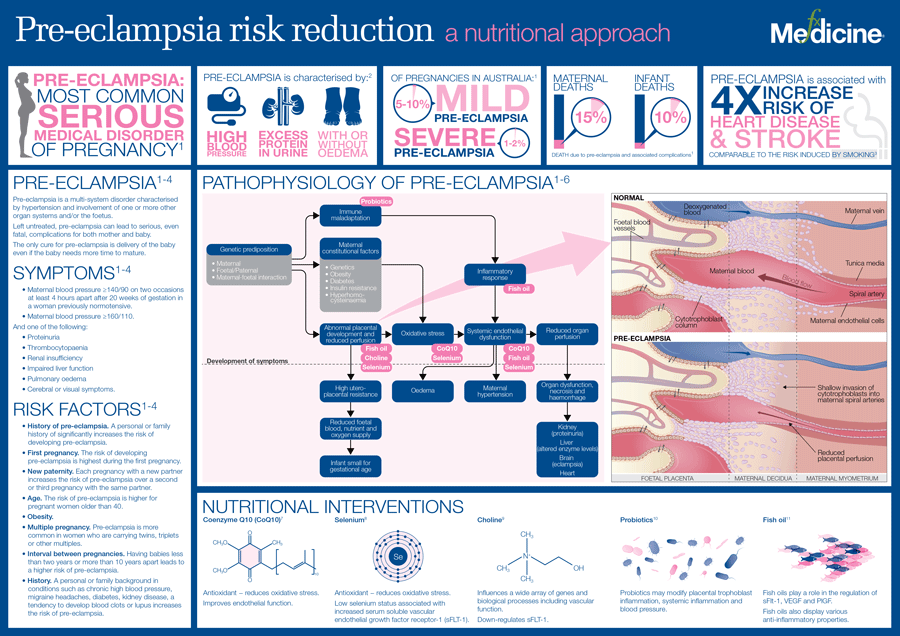
You may be at increased risk for other heart conditions in the future if you have some heart conditions, preeclampsia, or gestational diabetes during or shortly after pregnancy. Work with your health care provider to monitor your risk or manage your heart condition before, during, and after pregnancy.
Top of Page
High Blood Pressure (Hypertension)
High blood pressure is a common heart condition occurring when your blood pressure is higher than normal. Chronic hypertension means having high blood pressure before you get pregnant or before 20 weeks of pregnancy. Gestational hypertension is high blood pressure that first occurs after 20 weeks of pregnancy. Preeclampsia happens if you previously had normal blood pressure and suddenly develop high blood pressure and protein in your urine or other problems after 20 weeks of pregnancy. If you have chronic hypertension, you can also get preeclampsia.
High blood pressure increases the risk of preterm delivery, and low birth weight, plus more serious issues such as eclampsia, stroke, and placental abruption (the placenta separating from the wall of the uterus).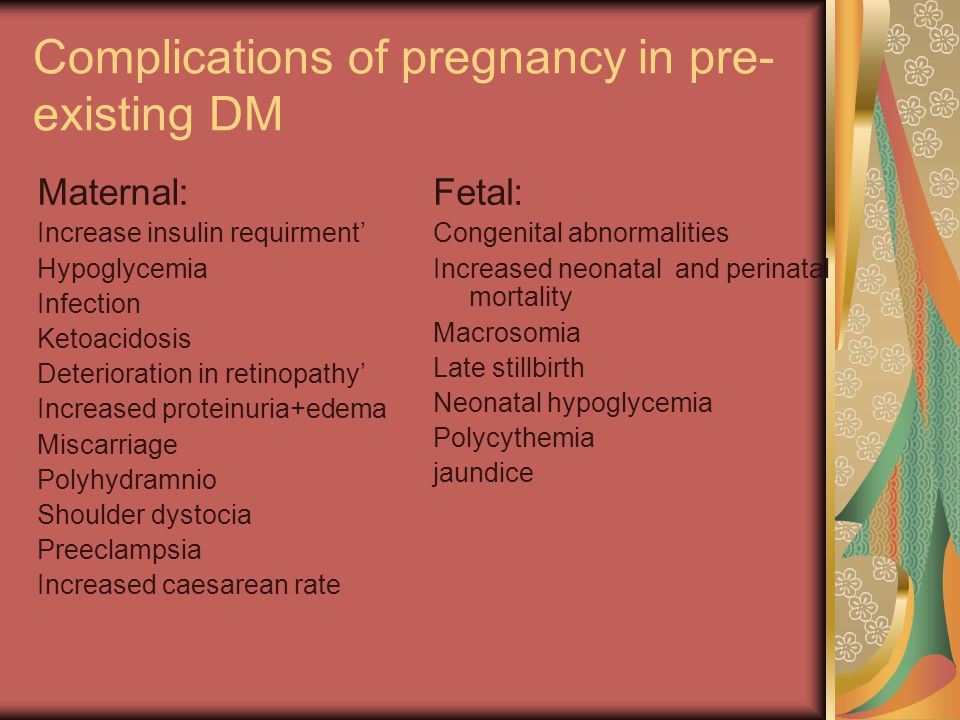 High blood pressure may be prevented and is treatable. These 7 strategies to live a heart-healthy lifestyle, plus at-home self-measured blood pressure monitoring with support from your health care provider, can help you manage your high blood pressure. If you are at high risk for preeclampsia, your provider may recommend low-dose aspirin after 12 weeks of pregnancy. Learn more about High Blood Pressure and Pregnancy.
High blood pressure may be prevented and is treatable. These 7 strategies to live a heart-healthy lifestyle, plus at-home self-measured blood pressure monitoring with support from your health care provider, can help you manage your high blood pressure. If you are at high risk for preeclampsia, your provider may recommend low-dose aspirin after 12 weeks of pregnancy. Learn more about High Blood Pressure and Pregnancy.
Top of Page
Hyperemesis Gravidarum
Many pregnant people have some nausea or vomiting, or “morning sickness,” especially in the first 3 months of pregnancy. Hyperemesis gravidarum, however, is more extreme than “morning sickness.” It refers to persistent nausea and vomiting during pregnancy. This can lead to weight loss and dehydration and may require intensive treatment. If you are concerned about your symptoms, call your health care provider. If you have severe nausea (e.g., you are unable to drink for more than 8 hours or eat for more than 24 hours), seek medical care immediately.
Top of Page
Infections
Infections can complicate pregnancy and may have serious consequences. Being screened and treated for infections, such as HIV and other sexually transmitted infections (STIs) and getting recommended vaccines can prevent many bad outcomes. Easy steps, including hand washing and avoiding certain foods, can also help protect you from some infections. Your health care provider can help you stay up to date with your vaccines. To learn more about different infections and how to protect your health, visit the following CDC pages:
- Pregnancy and HIV, Viral Hepatitis, STI & TB Prevention
- Vaccines During Pregnancy FAQs
- COVID-19 Vaccines While Pregnant and Breastfeeding
- Food Safety During Pregnancy
- 10 Tips for Preventing Infections Before and During Pregnancy
One common bacterial infection during pregnancy is a urinary tract infection (UTI). Your health care provider will likely test your urine early in pregnancy to see if you have a UTI and treat you with antibiotics, if necessary. Treatment will make it better, often in 1 or 2 days. Although not everyone with a UTI has symptoms, you may have a UTI if you have:
Treatment will make it better, often in 1 or 2 days. Although not everyone with a UTI has symptoms, you may have a UTI if you have:
- Pain or burning when you pee.
- Fever, tiredness, or shakiness.
- An urge to pee often.
- Pressure in your lower belly.
- Pee that smells bad or looks cloudy or reddish.
- Nausea or back pain.
Top of Page
Weight
Starting pregnancy at a healthy weight can help reduce the risk of preeclampsia, gestational diabetes, stillbirth, and cesarean delivery. If you are underweight [PDF – 1 MB] or overweight, talk to your health care provider about ways to reach and maintain a healthy weight before you get pregnant. Gaining a healthy amount of weight during pregnancy is also important for your health during and after pregnancy. Learn about pregnancy weight gain recommendations and steps to help you meet your pregnancy weight gain goal.
Complications during pregnancy - how to avoid?, Pasman Clinic
The Honored Doctor of the Russian Federation, Head Department of Obstetrics and Gynecology, Novosibirsk State University, Doctor of Medical Sciences, Professor Natalya Mikhailovna Pasman.
The most vulnerable for a child are the first 12 weeks of intrauterine development, it is at this time that the laying and formation of all its organs and systems takes place: heart, blood vessels, brain, kidneys, liver, as well as organs of the endocrine system.
Emotional background
It is necessary to know and remember that the baby feels the mood of the mother and her emotional background from the 8th week of pregnancy. Try to leave all negative emotions, anxieties and worries beyond the threshold of the onset of conception, enjoy every day of communication with the baby, read to him, listen to classical music with him. A pregnant woman needs a full sleep of at least 8-9 hours, daily walks in the fresh air and proper nutrition.
Healthy nutrition
The maximum weight gain during pregnancy should be from 8 to 10 kg, per week - 350 grams, respectively, daily gain - 40-50 grams. You can often hear from a pregnant woman that a friend has gained 20 kg and feels great.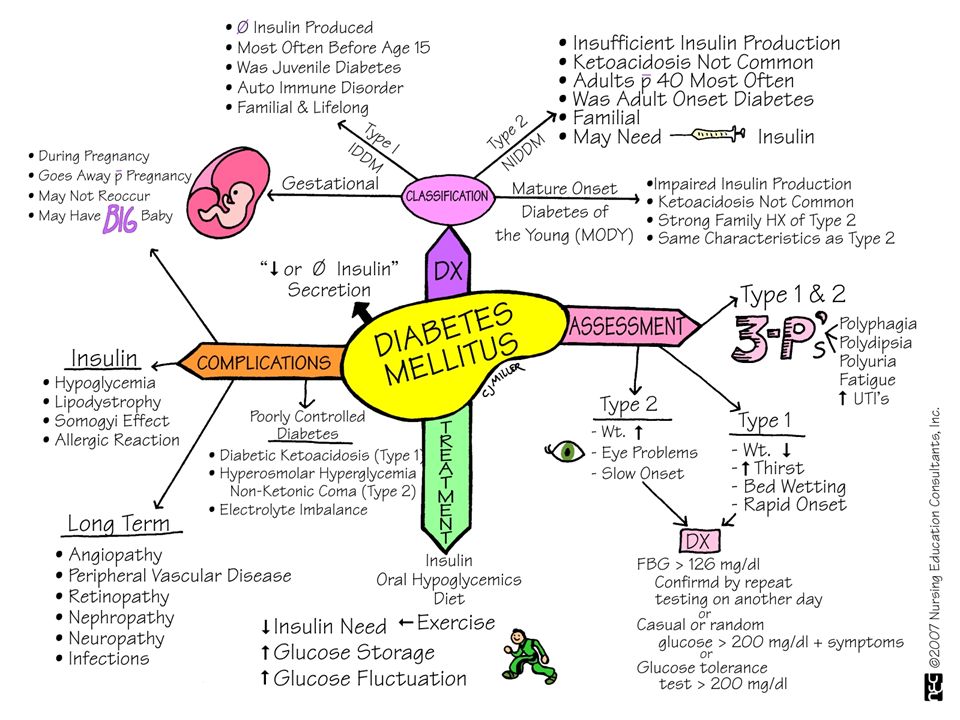 It is possible that at that time this pregnant woman really did not have any complaints. But, unfortunately, the child suffers from maternal inattention to himself. Persistent weight gain is often accompanied by a violation of the microcirculation of blood circulation in small vessels, and the fetus suffers from this in the first place.
It is possible that at that time this pregnant woman really did not have any complaints. But, unfortunately, the child suffers from maternal inattention to himself. Persistent weight gain is often accompanied by a violation of the microcirculation of blood circulation in small vessels, and the fetus suffers from this in the first place.
Visiting a doctor
In some cases, pregnant women find it unnecessary to see a doctor and do not visit the antenatal clinic. This point of view is deeply mistaken. The doctor's task is to prevent possible complications of pregnancy, to identify and treat them in time - either on an outpatient basis or in a hospital.
The most common complications in the first trimester of pregnancy (1-13 weeks) are early toxicosis (nausea, vomiting, salivation) and the threat of miscarriage. More serious are the complications of the second half: fetoplacental insufficiency and preeclampsia (edema, increased blood pressure).
The insidiousness of these complications is the absence of complaints from the mother.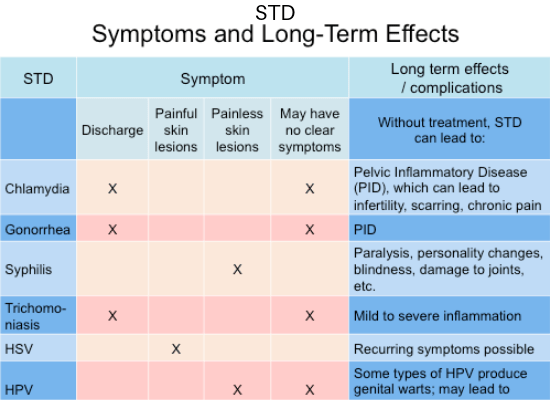 But a subtle indicator of the true state of the mother is the fetus, the assessment of which is carried out at least three times during pregnancy using ultrasound, as well as dopplerometry (assessment of blood flow velocity in the vessels of the placenta) and cardiotocography (recording of fetal heartbeats).
But a subtle indicator of the true state of the mother is the fetus, the assessment of which is carried out at least three times during pregnancy using ultrasound, as well as dopplerometry (assessment of blood flow velocity in the vessels of the placenta) and cardiotocography (recording of fetal heartbeats).
Vitamin complex
So, regimen, rational nutrition, regular visits to the doctor are very important components that determine the outcome of pregnancy. To this should be added the intake of the most important vitamins that contribute to the prevention of fetal malformations: folic acid, vitamins B, E, A, ascorbic acid.
At the same time, it is the vitamin-mineral complexes developed for expectant mothers that are the basis for the prevention of complications and colds in pregnant women. Scientific studies have proven the positive effect of three mineral-vitamin complexes: "Vitrum Prenatal Forte", "Elevit Pronatal" and "Multitabs Perinatal" on the course of pregnancy.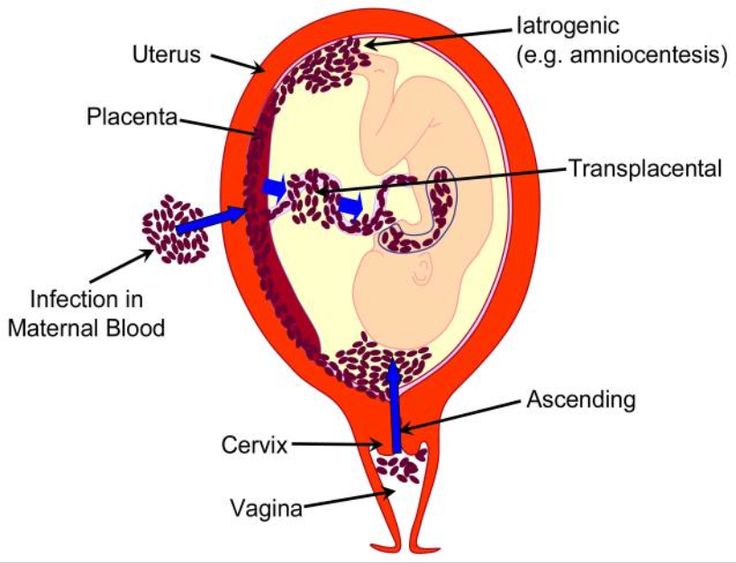
Conception, pregnancy and childbirth are the most important events in a person's life. Remember this, future moms and dads! After all, a lot in the successful outcome of pregnancy depends on you.
Complications of pregnancy. What are Pregnancy Complications?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
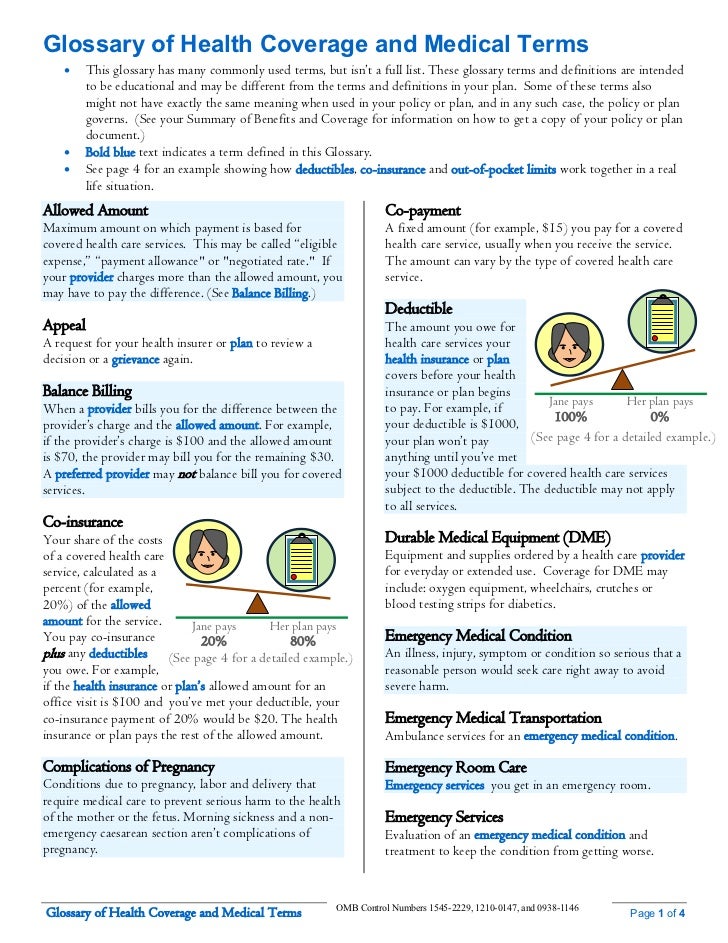
Complications of pregnancy are pathological conditions in obstetric practice that have arisen in connection with gestation and violate its natural course. At the initial stages, they may not be accompanied by clinical symptoms, later they manifest pain in the lower abdomen, vaginal discharge, impaired fetal movement, headaches, and edema. For diagnosis, ultrasound of the uterus and fetus, MRI pelvimetry, laboratory tests, invasive prenatal methods, CTG and other methods are used. Depending on the condition of the woman and the unborn child, treatment may be aimed at maintaining or terminating the pregnancy.
Depending on the condition of the woman and the unborn child, treatment may be aimed at maintaining or terminating the pregnancy.
- Causes of pregnancy complications
- Classification
- Symptoms of pregnancy complications
- Diagnostics
- Treatment of pregnancy complications
- Prognosis and prevention
- Prices for treatment
General
According to experts in the field of obstetrics and gynecology, only about 30-50% of pregnancies proceed physiologically, and this percentage is constantly decreasing. The most common complications of the gestational period, apart from early toxicosis, are miscarriages, which end up to 15-20% of pregnancies, and premature births (6-10%). At the same time, 30-80% of very premature babies suffer from disabling diseases. Approximately 8% of pregnant women develop oligohydramnios, 3-8% - preeclampsia and eclampsia, 2-14% - gestational diabetes mellitus.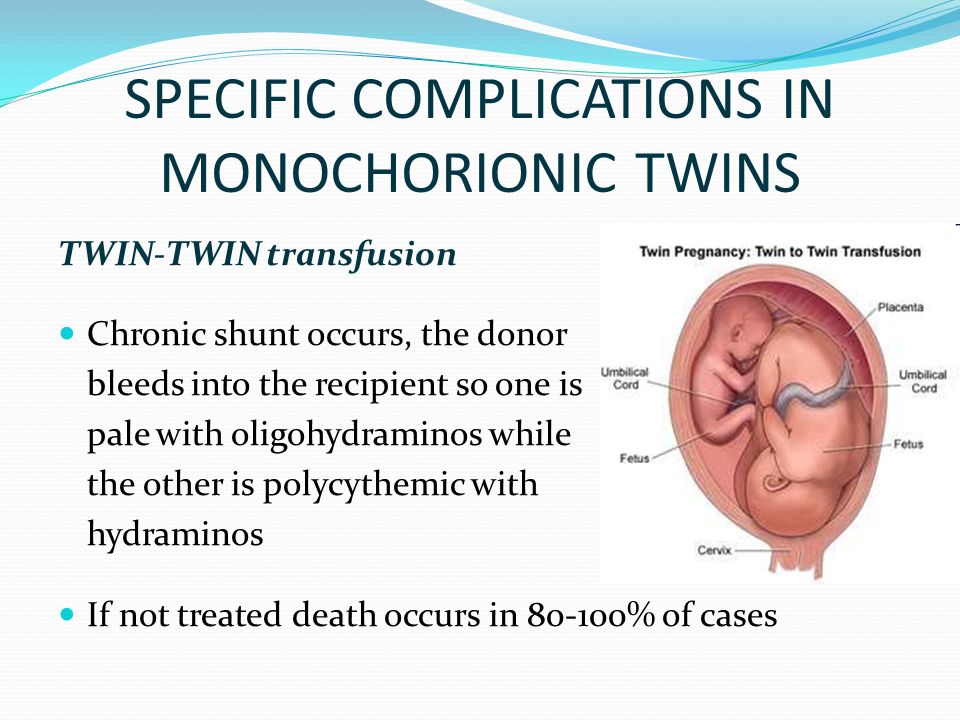 Every fiftieth pregnancy is ectopic, and every two hundredth placenta previa occurs. Other types of complications in pregnant women are less common.
Every fiftieth pregnancy is ectopic, and every two hundredth placenta previa occurs. Other types of complications in pregnant women are less common.
Complications of pregnancy
Causes of pregnancy complications
The complicated course of the gestational period can be triggered by many factors on the part of the mother or fetus. The most common causes of pregnancy complications are:
- Extragenital somatic pathology. With cardiovascular diseases (hypertension, heart defects, arrhythmias) and urological diseases (glomerulonephritis, pyelonephritis), the risk of late preeclampsia increases. Gestation can also lead to decompensation of almost any chronic disease.
- Endocrinopathy. With violations of the hypothalamic-pituitary regulation and endocrine function of the ovaries, the process of implantation of a fertilized egg suffers, and the contractile activity of the myometrium changes. Diabetes mellitus provokes microcirculatory disturbances both in the woman's body and in the fetoplacental system.

- Inflammatory gynecological diseases. With salpingitis, adnexitis, endometritis, the likelihood of ectopic tubal and cervical pregnancy increases. Chronic cervicitis can provoke isthmic-cervical insufficiency. With inflammation, intrauterine infection of the fetus is possible.
- Anomalies in the development of the uterus. In women with an intrauterine septum, a bicornuate, saddle-shaped or infantile uterus, spontaneous abortions, premature births, fetoplacental insufficiency, placental abruption and fetal hypoxia are more often diagnosed.
- Pathological pregnancy and childbirth in the past. Past miscarriages and preterm births increase the likelihood of recurrent miscarriage. Cicatricial deformity of the neck after its rupture is the main cause of isthmic-cervical insufficiency. After a uterine rupture in childbirth, it is likely to rupture in the later stages of the next pregnancy, especially multiples.
- Multiple pregnancy. If there are two or more fetuses in the uterus, chronic extragenital pathology is more often exacerbated, late toxicosis is observed, polyhydramnios occurs, leakage of amniotic fluid, and the threat of premature termination of pregnancy.
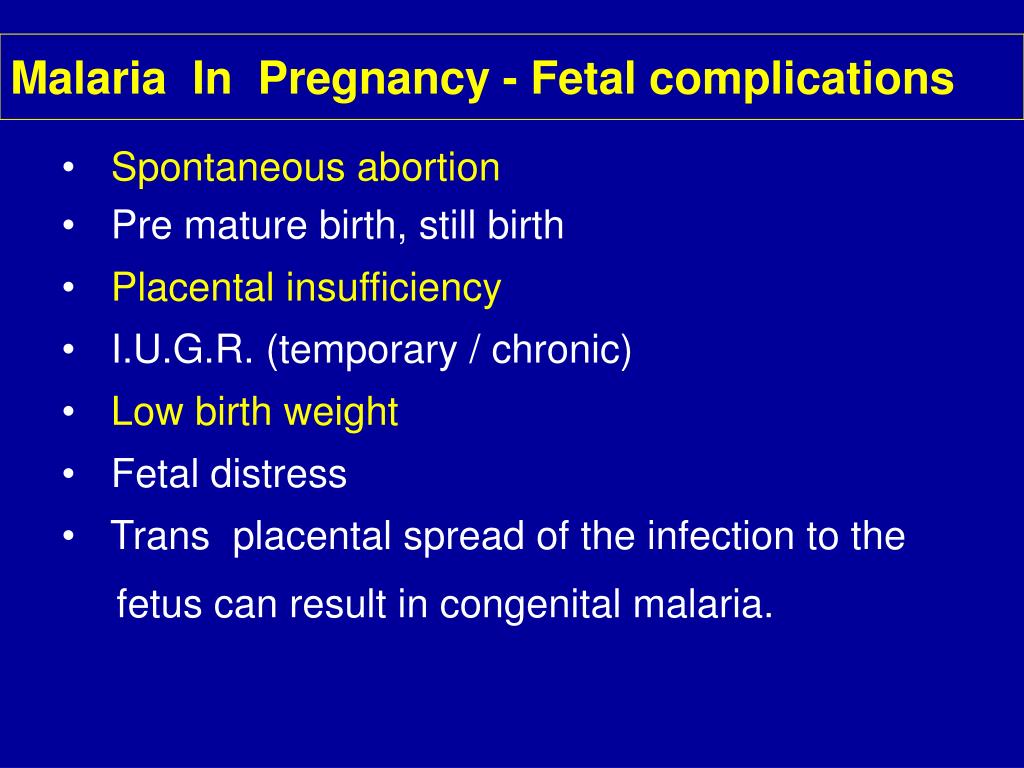
- Infectious diseases. Viral and bacterial infections can provoke miscarriage, premature birth, aggravate the course of preeclampsia, chronic somatic and endocrine diseases, and cause complications in the form of inflammation of the membranes. Some pathogens can infect the fetus in utero.
- Immunological factors. Habitual miscarriage is more often observed when the blood of the mother and fetus is incompatible according to the AB0 system or the Rh factor, and the patient has antiphospholipid syndrome.
- Genetic abnormalities of the fetus. The most common cause of pregnancy termination by early miscarriage is fetal developmental defects incompatible with life.
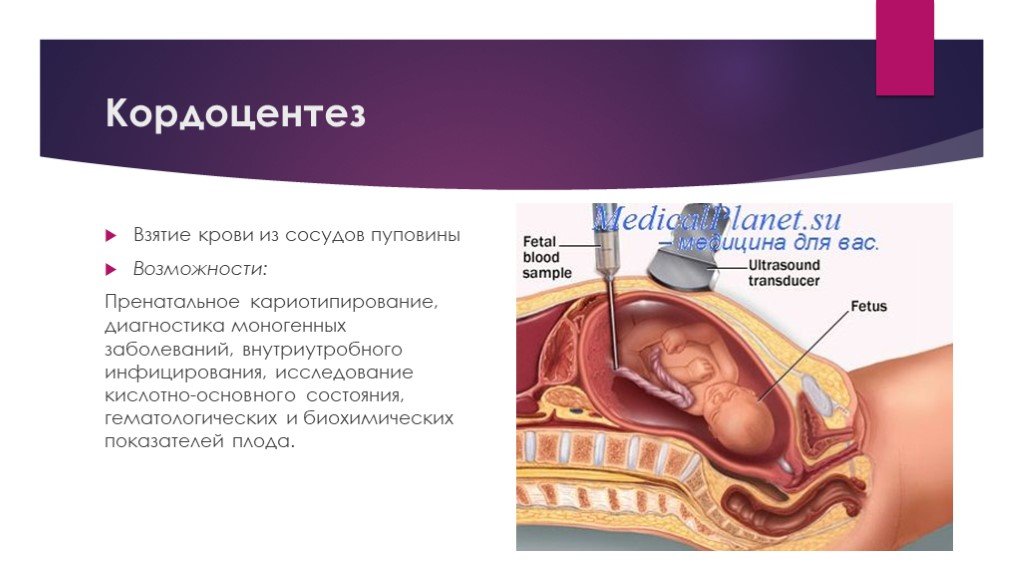
- Iatrogenic complications. Performing amnioscopy, amniocentesis, cordocentesis and chorion biopsy, suturing the cervix increases the risk of high rupture of the amniotic bladder, infection and early termination of pregnancy.
Additional provoking factors, in which complications of pregnancy are more often observed, are addictions (nicotine, alcohol, drugs), an asocial lifestyle. The risk group also includes pregnant women under 18 and over 35 years of age, patients with poor nutrition and obesity, women who lead an inactive lifestyle, experience excessive physical and psychological stress.
The risk group also includes pregnant women under 18 and over 35 years of age, patients with poor nutrition and obesity, women who lead an inactive lifestyle, experience excessive physical and psychological stress.
Classification
The clinical classification of pregnancy complications takes into account who and at what level pathological changes have occurred - in the mother, fetus, in the mother-fetus system or in embryonic structures. The main complications in women are:
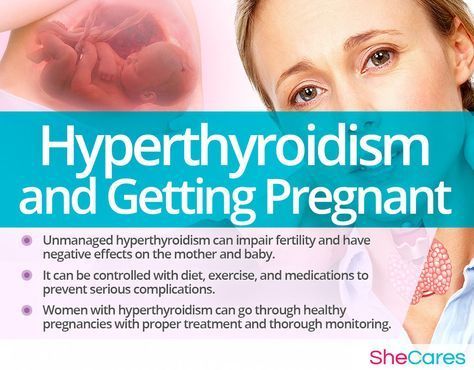
- Conditions and diseases associated with pregnancy. The patient may experience early toxicosis, late gestosis, anemia, gestational diabetes and thyrotoxicosis, varicose veins. Functional changes in the pyelocaliceal system contribute to the rapid development of inflammatory urological diseases.
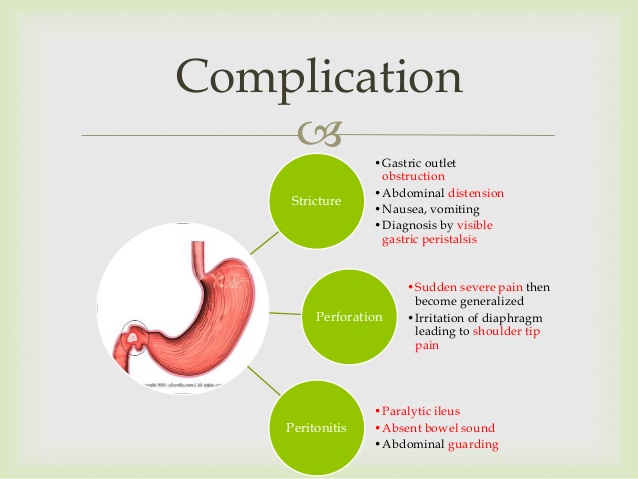
- Complications of existing diseases. Loads on the body of a pregnant woman provoke decompensation of chronic endocrine and somatic pathology - thyrotoxicosis, hypothyroidism, diabetes mellitus, cardiomyopathy, hypertension, gastrointestinal diseases.
 Violation of the function of organs and systems sometimes reaches the degree of insufficiency (cardiovascular, renal, hepatic).
Violation of the function of organs and systems sometimes reaches the degree of insufficiency (cardiovascular, renal, hepatic). - Threatened miscarriage and miscarriage. Gestation can end prematurely with early or late spontaneous abortion (up to 22 weeks inclusive) or preterm birth (from 23 to 37 full weeks).
- Ectopic pregnancy. When a fetal egg is attached outside the uterine cavity, an ectopic pregnancy is observed. Currently, this condition in 100% of cases ends with the death of the fetus and the occurrence of severe complications in a woman (internal bleeding, hypovolemic shock, acute pain syndrome).
In some cases, the main pathological changes occur in the body of the fetus. This group of complications includes:
- Genetic anomalies. Malformations caused by genetic defects cause miscarriages, and during pregnancy - severe neurological, mental and somatic disorders in a child.
- Intrauterine infection. Infection can be caused by bacteria, mycoplasmas, chlamydia, fungi, viruses.
 Its complications are violation of fetal maturation, early termination of pregnancy, multiple malformations, fetal death, pathological course of childbirth.
Its complications are violation of fetal maturation, early termination of pregnancy, multiple malformations, fetal death, pathological course of childbirth. - Fetal hypoxia. This condition is noted with insufficient oxygen supply, can cause ischemia and necrosis in various organs. The result of prolonged hypoxia is a congenital pathology of the newborn or antenatal fetal death.
- Hypotrophy. With a pronounced lag in fetal development from the gestational age, birth hypoxia, problems with spontaneous breathing, meconium aspiration with the subsequent development of pneumonia, thermoregulation disorders, hyperbilirubinemia, and brain damage may occur.
- Incorrect position and presentation. With pelvic and oblique presentation, the likelihood of complications in childbirth is high, with transverse independent childbirth becoming impossible.
- Frozen pregnancy. Intrauterine death of a child with its preservation in the uterine cavity leads to the development of severe inflammatory complications - purulent endometritis, peritonitis, sepsis, which pose a threat to the health and life of a woman.
With complications from the embryonic structures that provide nutrition and protection for the fetus, the unborn child most often suffers, which can develop inflammatory diseases, hypoxia, malnutrition, leading to congenital pathology or antenatal death. In addition, such complications provoke premature and pathological births. Depending on the level of damage, there are:
- Pathology of the placenta. Cysts and tumors can appear in the placental tissue, infectious and inflammatory processes (deciduitis, villitis, intervillezitis) can develop. Anomalies of the placental disc, violations in the attachment of the placenta to the uterine wall are possible - tight attachment, increment, ingrowth and germination. Serious complications are low location, presentation and premature detachment of the placenta.
- Pathology of the umbilical cord. When the inflammatory process spreads to the tissues of the umbilical cord, funiculitis occurs. The main anomalies in the development of the umbilical cord are its shortening, elongation, sheath attachment, the formation of false and true nodes, cysts, hematomas, teratomas, hemangiomas.

- Pathology of the membranes. The most common complications from the side of the fetal sac are low and polyhydramnios, premature rupture and leakage of water, the formation of amniotic bands, chorioamnionitis.
A separate group of complications is represented by disorders in the system of interaction between mother and fetus. The main ones are:
- Rh conflict. The condition is accompanied by the destruction of fetal red blood cells and the development of various complications, from hemolytic jaundice to the death of the child.
- Fetoplacental insufficiency. Violation of the morphological structure and functionality of the placenta, caused by various reasons, leads to hypoxia, malnutrition, and in severe cases, fetal death.
When classifying complications, it is equally important to take into account the time of their occurrence. There are early complications, often leading to abortion, and late ones, affecting the development of the fetus and the course of childbirth.
Symptoms of pregnancy complications
Despite the relationship between certain pathological conditions and gestational age, there are a number of common signs that indicate a complicated pregnancy. The first one is abdominal pain. Usually they are localized in the lower part of the abdominal cavity, they can give to the groin and lower back. Less often, the pain begins in the epigastrium, and then goes to the lower abdomen. Pain syndrome occurs with ectopic pregnancy, the threat of miscarriage and premature birth, threatening rupture of the uterus (in pregnant women with a scar on the uterus). In such cases, weakness, dizziness, and sometimes loss of consciousness are observed. Pain in inflammatory diseases is often combined with fever.
Vaginal discharge indicates a complication of pregnancy. Miscarriage, premature birth, abruption or placenta previa are accompanied by spotting. Purulent and mucopurulent leucorrhoea are observed in inflammatory processes. The watery nature of the discharge is characteristic of premature outflow or leakage of amniotic fluid.
The watery nature of the discharge is characteristic of premature outflow or leakage of amniotic fluid.
Almost any change in a woman's general well-being can be a sign of possible complications. In the first trimester, pregnant women are worried about nausea, vomiting and other signs of early toxicosis. With late gestosis, dizziness, pain in the occipital region, the appearance of "flies" before the eyes, swelling in the legs, nausea, and vomiting occur. A sudden increase in temperature can be observed with the development of inflammatory complications or with an infectious disease. A pregnant woman may notice the appearance or intensification of symptoms characteristic of extragenital pathology - dry mouth, palpitations, shortness of breath, heartburn, varicose veins, etc.
Complications of pregnancy from the side of the fetus are often detected by a change in the frequency of movements. If movements are not felt for more than 4 hours, there is no reaction to the usual stimuli (stroking the abdomen, music, food), you should urgently contact an obstetrician-gynecologist. Hypoxia is characterized by active stirring and a feeling of fetal hiccups.
Hypoxia is characterized by active stirring and a feeling of fetal hiccups.
Diagnostics
If a pregnancy complication is suspected, in the process of collecting an anamnesis, provoking factors are identified, an examination is prescribed to determine the type and degree of violations. Recommended for diagnosis:
- External obstetric examination. The size and shape of the uterus, the tone of its muscles, and areas of pain are determined.
- Inspection in mirrors. Allows you to detect discharge, assess the condition of the vaginal mucosa and cervix.
- Microscopy and culture of a vaginal smear. Indicated for assessing the state of the vaginal secretion, identifying pathogens of infectious diseases.
- Ultrasound of the pelvic organs. It is aimed at determining the size of the uterus, the state of its wall and scar (if any), assessing the size and condition of the fetus, placenta, umbilical cord, and the volume of amniotic fluid.

- MRI pelvimetry. Effectively detects anomalies in the development of the fetus and embryonic membranes, suspected by ultrasound.
- Invasive prenatal diagnosis. With the help of amnioscopy, amniocentesis, chorion biopsy, cordocentesis, placentocentesis and fetoscopy, congenital chromosomal abnormalities are excluded, the condition of the fetal membranes, the amount and color of the amniotic fluid are assessed.
- Non-invasive rapid tests. The determination of specific markers allows, in doubtful cases, to diagnose an ectopic pregnancy, to establish leakage of amniotic fluid, to confirm the premature onset of labor.
- Laboratory monitoring of pregnancy. Determination of the level of hormones - hCG, free beta-hCG and estriol, PAPP-A, placental lactogen and alpha-fetoprotein - is indicative of placental disorders, the presence of fetal pathologies and the complication of the gestation process.
- TORCH complex. In the course of a serological study, infectious diseases that affect the fetus in utero are diagnosed - toxoplasmosis, rubella, cytomegalovirus, herpes, hepatitis B and C, chlamydia, syphilis, gonorrhea, listeriosis, HIV, chickenpox, enterovirus.
- Dopplerography of uteroplacental blood flow. Provides an objective assessment of transplacental hemodynamics.
- Cardiotocography. It is prescribed to assess the fetal heartbeat, timely detection of bradycardia and tachycardia, indicating hypoxia and other complications that are critical for the child.
For dynamic control over the condition of the pregnant woman and fetus, identification of additional risk factors, general blood and urine tests, blood pressure and temperature control, ECG, and other instrumental and laboratory research methods can be used. Differential diagnosis of pregnancy complications is carried out with concomitant diseases (hypertension, renal colic, glomerulo- and pyelonephritis), acute surgical pathology (appendicitis, acute cholecystitis), inflammatory and non-inflammatory gynecological diseases. In difficult cases, a urologist, surgeon, therapist, anesthesiologist-resuscitator, infectious disease specialist, immunologist and other narrow specialists are involved in the diagnosis.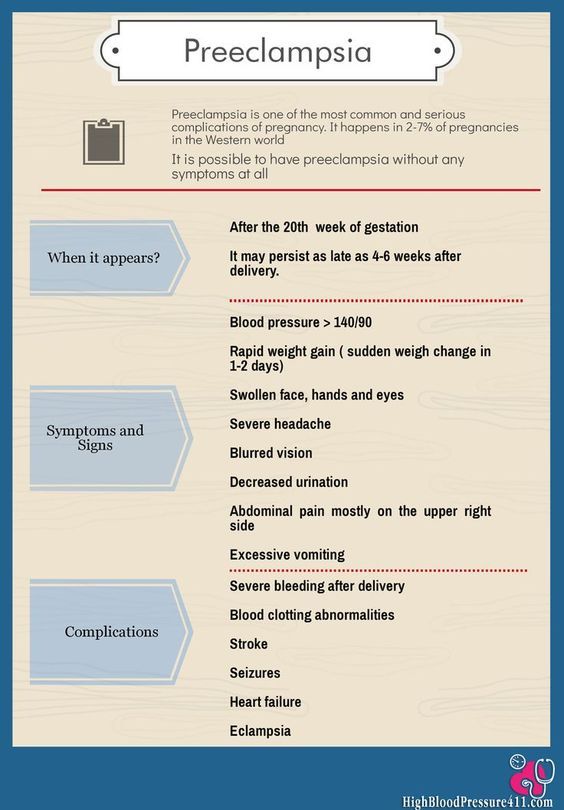
Treatment of pregnancy complications
The tactics of managing a pregnant woman in the presence of complications depends on their nature, severity, and the degree of risk to the fetus and mother. In the normal state of the child and pathological disorders that do not pose a serious threat to the life of a woman, drug therapy is prescribed to prolong pregnancy. The treatment plan may include:
- Hormonal preparations. Normalize the endocrine balance in the body.
- Tocolytics. Reduce the contractile activity of the myometrium.
- Antibacterial agents. Destroy pathogenic flora or prevent the development of infection.
- Anti-inflammatory drugs. Reduce the severity of the inflammatory process and pain syndrome.
- Glucocorticoids. Promote the maturation of lung tissue and accelerate the synthesis of surfactant.
- Sedatives. Relieve emotional stress.
According to indications, a woman is given symptomatic therapy for extragenital pathology, vitamin-mineral complexes, infusions of solutions are used.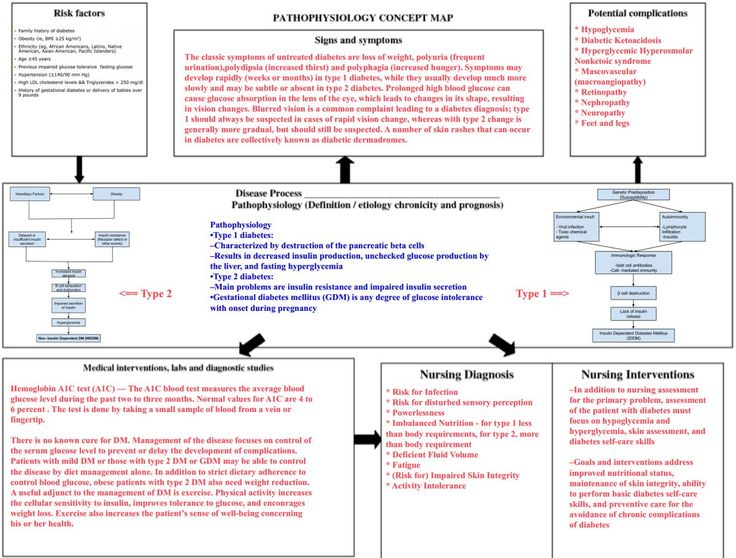 If necessary, suture the neck or install an obstetric pessary in the vagina. When certain types of pathology of the fetus, placenta and amniotic fluid are detected, fetal drainage and fetoscopic operations, intrauterine transfusions and infusions are indicated.
If necessary, suture the neck or install an obstetric pessary in the vagina. When certain types of pathology of the fetus, placenta and amniotic fluid are detected, fetal drainage and fetoscopic operations, intrauterine transfusions and infusions are indicated.
For the treatment of placental insufficiency, drugs that improve microcirculation and uteroplacental blood flow are used - antiplatelet agents and anticoagulants. With Rhesus conflict, the administration of anti-Rhesus immunoglobulin is effective. The detection of gross malformations, the death of a child, an abortion that has begun, and conditions that threaten the life of the mother are indications for abortion and intensive care. Taking into account the term, a drug, mini- or medical abortion or artificial birth is performed.
Prognosis and prevention
The prognosis of a complicated pregnancy depends on the nature of the pathology. With genetic defects, ectopic pregnancy and miscarriage, the fetus cannot be saved.