Baby head coming out
What (and When) Is It and What Does It Feel Like?
You may not have heard Johnny Cash’s 1963 hit song “Ring of Fire,” but if you’ve had a baby or are planning to in the near future, the term may be all too familiar.
Crowning is often referred to as the “ring of fire” in the birthing process. It’s when your baby’s head becomes visible in the birth canal after you’ve fully dilated. It’s the home stretch — in more ways than one.
Why does crowning get so much attention? When your cervix is fully stretched, that usually means that it’s time to push your baby out into the world. For some women, this is very exciting, relieving news. For others, however, crowning is painful or — at the very least — uncomfortable.
However, knowing what to expect during a vaginal delivery is powerful. Let’s take a look at some of the details about crowning that you want to know — but are too afraid to ask.
Labor is divided into four stages:
- early and active labor
- fetal descent through the birth canal (birth)
- delivery of the placenta
- recovery
Crowning occurs in the second stage that results in the birth of your baby.
Leading up to this point, your body will have gone through a number of regular contractions as your cervix thins out and dilates from 0 to 6 centimeters (cm) in early labor. The time this takes can vary from hours to days.
In active labor, the cervix dilates from 6 to 10 cm over the course of 4 to 8 hours — approximately a centimeter an hour. In total, the first stage of labor may take some 12 to 19 hours. This process may be shorter for women who have previously had a baby.
Crowning happens when you’re fully dilated. You may feel like you’ve already done so much work, but you may have a while yet to go. Hang in there, mama!
This second stage of labor — birth — can take anywhere from just a couple minutes up to a few hours, sometimes more. In general, it lasts 20 minutes to 2 hours. First-time moms or those who’ve had an epidural may be on the longer side of these time estimates.
Your doctor or midwife will closely monitor your progress through these stages to give you updates on your individual timeline.
When you’re crowning, you may even be able to reach down and touch your baby’s head or get a look at it by using a mirror. Some women may find the sight motivating. Others may be overwhelmed by the experience or, frankly, a little grossed out. Whatever you feel, don’t feel ashamed! Mixed emotions are perfectly normal.
The good news: Once you reach crowning, your baby may be born within just one or two contractions.
To many women, crowning feels like an intense burning or stinging sensation. This is where that “ring of fire” term comes from. Others share that crowning didn’t feel at all like they had expected. And others say they didn’t feel it at all.
As you can imagine, there’s a spectrum of experiences, and there’s no one right or wrong way to feel.
How long the feeling lasts will vary as well. As your skin stretches, the nerves become blocked and you may feel nothing at all. That’s right — the stretch may be so intense that you may feel more of a numbing sensation than pain.
Speaking of pain, if you choose to have an epidural, you may experience more of a dulled-down burning sensation. Or it may feel more like pressure than burning. It depends on the amount of pain relief you’re receiving. The pressure is likely because your baby is very low in the birth canal.
Keep in mind that what you’ll actually experience during crowning may be different from what your mom, sisters, or friends have experienced. As with all other parts of labor and delivery, what will happen and how it will feel is individual.
That said, when you feel you might be crowning and your doctor or midwife confirms it, resist pushing too quickly. In fact, you should try to relax and let your body go as limp as possible.
That probably sounds crazy, because you may have a strong urge to push — let’s get this show on the road! But try your best to take things slow and let your uterus do most of the work.
Why? Because relaxing may prevent severe tearing.
When you’re crowning, it means that your baby’s head stays stationary in the birth canal. It doesn’t drop back inside after contractions.
It doesn’t drop back inside after contractions.
Your doctor will help coach you through the pushing process at this stage and help guide the baby to prevent damage to the skin between your vagina and rectum. This area is also called the perineum, and you may have been warned about perineum tears.
Ouch! Even with the best guidance, with so much stretching, there’s also an opportunity for tearing while giving birth. (We’re talking about tears that rhyme with cares, not what you produce when you cry. It pains us to say you may have both — but you’re bound to have tears of joy when your newborn babe is placed in your arms.)
Sometimes baby’s head is large (no, this isn’t cause for concern!) and creates tears. Other times, the skin doesn’t stretch well enough and leads to tearing in the skin and/or muscle.
Whatever the case, tears are common and tend to heal on their own within a few weeks after delivery.
There are different degrees of tearing:
- First-degree tears involve the skin and tissue of the perineum.
 These may heal with or without stitches.
These may heal with or without stitches. - Second-degree tears involve the perineum and some of the tissue inside the vagina. This tear requires stitches and a few weeks of recovery.
- Third-degree tears involve the perineum and the muscle surrounding the anus. This tear often requires surgery and may take a bit longer than a few weeks to heal.
- Fourth-degree tears involve the perineum, anal sphincter, and the mucous membrane that lines the rectum. Like third-degree tears, this tear requires surgery and a longer recovery time.
With first- and second-degree tears, you may experience mild symptoms, like stinging or pain while urinating. With third- and fourth-degree tears, the symptoms may be more severe issues, like fecal incontinence and pain during intercourse.
Some 70 percent of women experience damage to the perineum during birth, whether through tearing naturally or receiving an episiotomy.
Episi-what? In some cases, your doctor or midwife may choose to make an incision — a cut — in the area between the vagina and anus (episiotomy). This procedure used to be more common because doctors thought it would prevent the most severe tearing.
This procedure used to be more common because doctors thought it would prevent the most severe tearing.
But they don’t help as much as originally thought, so episiotomies are no longer routinely performed. Instead, they’re saved for cases when baby’s shoulders are stuck, baby’s heart rate is abnormal during labor, or when your healthcare provider needs to use forceps or a vacuum to deliver your baby.
Pain from tears and episiotomies may last two weeks or longer, but taking care of tears after delivery can help. Some women do go on to experience long-lasting pain and discomfort during sex. Talk to your doctor if this happens to you, as there are solutions that can help.
There are things you can do to prepare for the experience of crowning and pushing.
Above all else, consider signing up for a childbirth class at your hospital to learn more about what to expect during labor and delivery. Can’t find a class locally? There are some you can take online, like those offered through Lamaze.
Other tips
- Speak with your doctor about a pain management plan that will work for you. There are many options, including massage, breathing techniques, epidural, local anesthesia, and nitrous oxide.
- Resist the urge to push too fast when you’re told you’re crowning. Relaxing will allow your tissues to stretch and may help prevent severe tearing.
- Learn about different birthing positions that may help ease delivery. Moving onto all fours, side-lying, or semi-sitting are all considered ideal positions. The standard — laying on your back — may actually make pushing difficult. Squatting may increase your chances of tearing.
- Try to remember that once you feel the ring of fire, you’re close to meeting your baby. Knowing this may help you quite literally push through the pain and discomfort.
Was this helpful?
There’s a lot to think about during pregnancy. What colors to paint the nursery, what to put on your registry, and — of course — what the actual birth experience will be like.![]()
Whether you’re feeling excited or anxious, understanding what’s happening to your body during labor may help you feel more empowered.
And if you just want your baby out already, rest assured that your little one will enter the world in one way or another sooner rather than later. You’ve got this, mama!
Your baby in the birth canal Information | Mount Sinai
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
This position is called occiput anterior.
Childbirth is really a series of four stages that culminate in the actual birth and short period thereafter. For more specific information regarding emergency delivery see the information on childbirth, emergency delivery.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Cephalic (head first) presentation is considered normal, but a breech (feet or buttocks first) delivery can be very difficult, even dangerous for the mother and the baby.
In a normal pregnancy, the baby is positioned head down in the uterus.
The term fetal presentation refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part.
 The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet. - Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
FETAL LIE
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
Engagement
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
Descent
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
Flexion
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
Extension
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.

Expulsion
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Last reviewed on: 11/10/2022
Reviewed by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Boyish problems - articles from the specialists of the clinic "Mother and Child"
The head of the penis in boys and men is closed by the so-called foreskin - this is a mobile area of the skin, which consists of two sheets: the outer one (looks like skin) and the inner one (reminiscent of mucous membrane). In an adult male, the foreskin is easily displaced and opens the head. Between the glans penis and the inner leaf of the foreskin there is a space - the cavity of the foreskin, into which the secret of the glands located under the foreskin is secreted. This secret is called smegma, thanks to which the skin is easily displaced from the head of the penis. The head of the penis in men is very sensitive, and the foreskin is needed in order to cover it, and even during intercourse it slides over the head, which increases the man's sexual arousal and reduces friction.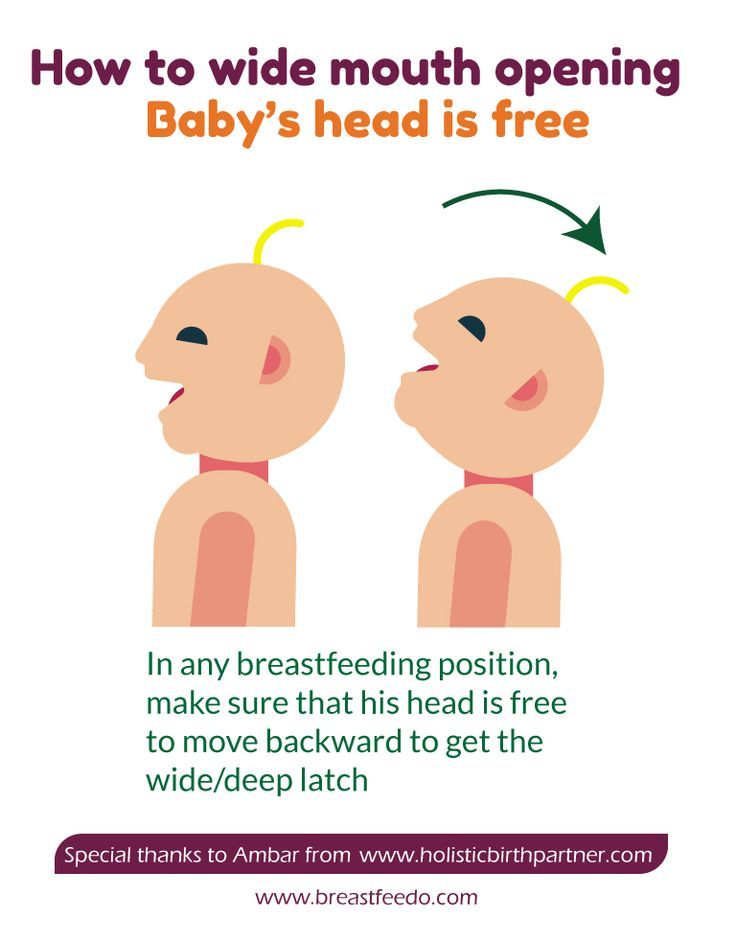
as in boys
In all boys from birth, the foreskin completely covers the glans penis, preventing it from showing out - this is a completely normal condition and is called physiological phimosis. Moreover, from the inside, the foreskin is also glued to the glans penis with the so-called synechiae (thin, tender adhesions), which are also quite common in little boys.
Gradual withdrawal of the head with separation of synechiae begins somewhere around 3 years of age and most often ends at 7–9 years of ageyears. But there are boys whose head opens only at puberty - at about 12 years old. So there is simply no single age at which the head opens, each child has his own.
as it was before
Even 10–20 years ago (and sometimes even now), doctors believed that if the glans penis does not open in a little boy, especially if there is synechia, this is not a norm, but a pathology. It was believed that during each wash, the head should be tried to slightly open, and the accumulated smegma (the secret of the glands of the penis) should be removed, otherwise inflammation of the foreskin will begin.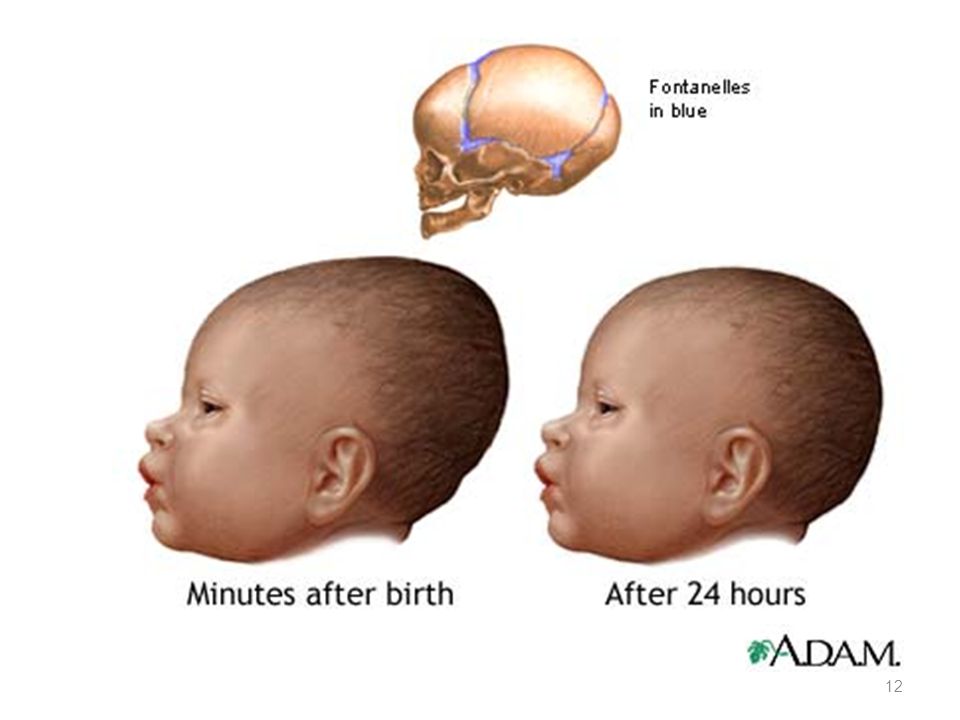 Therefore, when they saw a completely healthy baby at the reception, but with an unopened head, the doctors suggested opening it. Moreover, they recommended doing this if there were synechia or an inflammatory process. Very often, many surgeons opened the head of the penis without even warning the parents about it - simply by sharply displacing the foreskin during a routine examination of the baby. If the boy had synechiae, then they naturally burst, the child was in pain, he cried. The same thing happened if the doctor divided the synechia according to plan: the boys remembered this manipulation for a very long time and reacted extremely painfully to it.
Therefore, when they saw a completely healthy baby at the reception, but with an unopened head, the doctors suggested opening it. Moreover, they recommended doing this if there were synechia or an inflammatory process. Very often, many surgeons opened the head of the penis without even warning the parents about it - simply by sharply displacing the foreskin during a routine examination of the baby. If the boy had synechiae, then they naturally burst, the child was in pain, he cried. The same thing happened if the doctor divided the synechia according to plan: the boys remembered this manipulation for a very long time and reacted extremely painfully to it.
what they are doing now
Now modern and qualified doctors know that physiological phimosis is the norm and nothing needs to be done about it. In addition, over time, doctors saw that after the division of the synechiae and the removal of the head before all this happens on its own, repeated synechiae often occur, but these will no longer be thin, tender adhesions, but coarse cicatricial adhesions. Many boys had to separate synechia more than once, and as a result, everything often ended with circumcision of the foreskin. There is nothing to say about psychological problems after such manipulations.
Many boys had to separate synechia more than once, and as a result, everything often ended with circumcision of the foreskin. There is nothing to say about psychological problems after such manipulations.
Therefore, if the child is not bothered by anything, then modern urologists strongly advise not to touch the foreskin.
how to care
Parents who try to wash their child as often and as cleanly as possible are advised by doctors not to overdo it. Until the moment when the foreskin can separate, the boy's penis should only be washed with plain water and nothing more. It is not even necessary to slightly pull the foreskin, it will open when the time comes. If smegma accumulates behind the foreskin (it looks like a white curdled substance), do not worry and try to wash it completely with all your might. Smegma in boys is a normal manifestation of the work of the glands, it is easily washed off under running water and this is quite enough.
when to go to the doctor and to which one
If physiological phimosis is the norm, then what is the pathology? If a boy suddenly begins to complain that it hurts or is unpleasant for him to write, if his parents see that urine does not come out in a jet, that during urination the skin of the foreskin swells with a ball, redness, swelling or purulent discharge appears on the penis - this is an occasion immediately visit a doctor.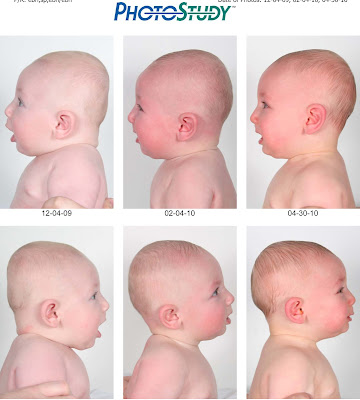 Ideally, contact a urologist (these are doctors who deal with the genitourinary organs), and if not, then a surgeon. A qualified urologist will always act in the interests of the child and will not prescribe him unnecessary traumatic manipulations. First, the doctor will always offer conservative treatment - to remove the inflammatory process, then soften and stretch the foreskin. And only if the boy really has serious changes leading to a violation of urine excretion, and conservative treatment is ineffective, the doctor will begin surgical treatment.
Ideally, contact a urologist (these are doctors who deal with the genitourinary organs), and if not, then a surgeon. A qualified urologist will always act in the interests of the child and will not prescribe him unnecessary traumatic manipulations. First, the doctor will always offer conservative treatment - to remove the inflammatory process, then soften and stretch the foreskin. And only if the boy really has serious changes leading to a violation of urine excretion, and conservative treatment is ineffective, the doctor will begin surgical treatment.
Look for a good doctor, do not rush to agree to a surgical manipulation or operation until you are sure that conservative methods of treatment do not work. Fortunately, in most cases, a small patient manages to avoid unpleasant procedures, since this vast majority is not a manifestation of pathology.
Phimosis in a child: what is dangerous and how to treat?
A normal question of the parents of a small son: is everything in order with the child's genitals? Usually they are embarrassed to ask about this, but it can help keep the boy healthy.
This question should be addressed to a pediatric urologist.
One of the most common penile health problems in boys is phimosis.
Pediatric urologist, Euromed Kids surgeon Kagan Maria Aleksandrovna told about what it is and how to deal with it.
An important point! Usually in children from birth to 5-6 years there is a physiological narrowness of the foreskin. This is the norm. After 5-6 years, as a rule, the head opens a little. If this does not happen, this is a reason to see a pediatric urologist.
What can go wrong?
Cicatricial phimosis may develop.
Causes of occurrence:
- 1st reason : you tried to open the head and tore the foreskin - a scar formed.
- 2nd cause : Lichen sclerosus is a chronic inflammatory disease of unknown etiology, often affecting the foreskin with subsequent scarring.

- 3rd reason: recurring balanoposthitis - inflammatory processes of the foreskin and glans penis (often due to poor hygiene, since the head cannot be opened due to the narrow foreskin and, accordingly, not washed properly).
Why is phimosis dangerous?
- As we have already learned, phimosis can cause inflammation of the foreskin (balanoposthitis).
- A formidable complication of phimosis can be paraphimosis - infringement of the glans penis by a narrow foreskin. In this case, if you do not consult a doctor in time, necrosis (death) of the penis may develop.
- Also in adolescence, phimosis can lead to psychological discomfort, and then to the problems of becoming a full-fledged sexual life.
What to do?
If you suspect that the child is not all right with the penis, the first thing to do is contact a pediatric urologist. It is also normal to visit this specialist annually for a preventive examination.