Neural tube defects pictures
Neural Tube Defects | MedlinePlus
On this page
Basics
- Summary
- Start Here
- Diagnosis and Tests
- Prevention and Risk Factors
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- No links available
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
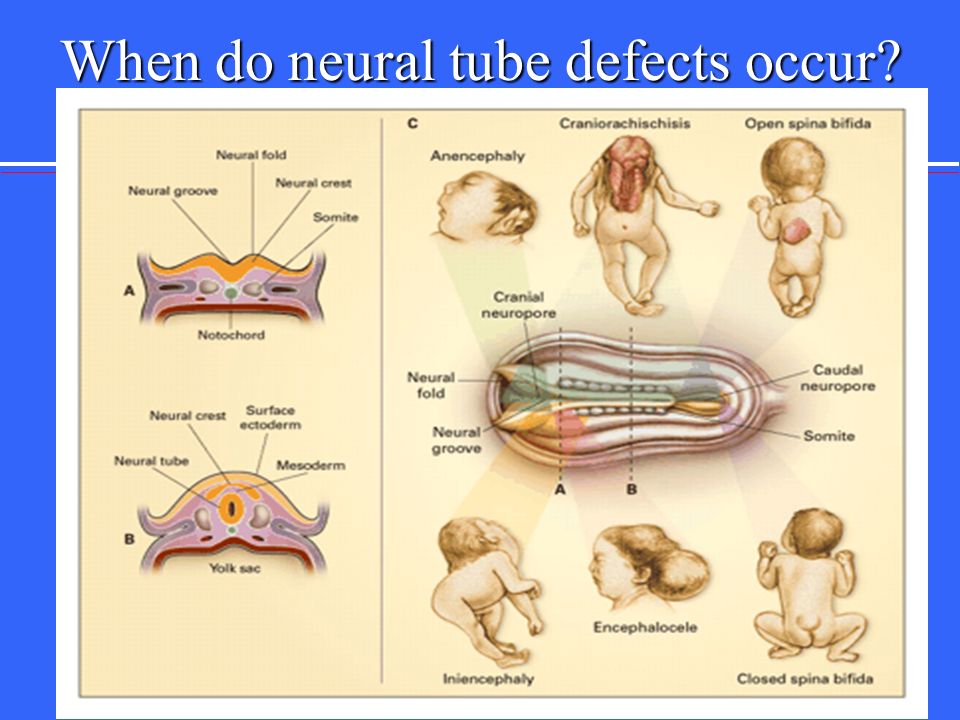
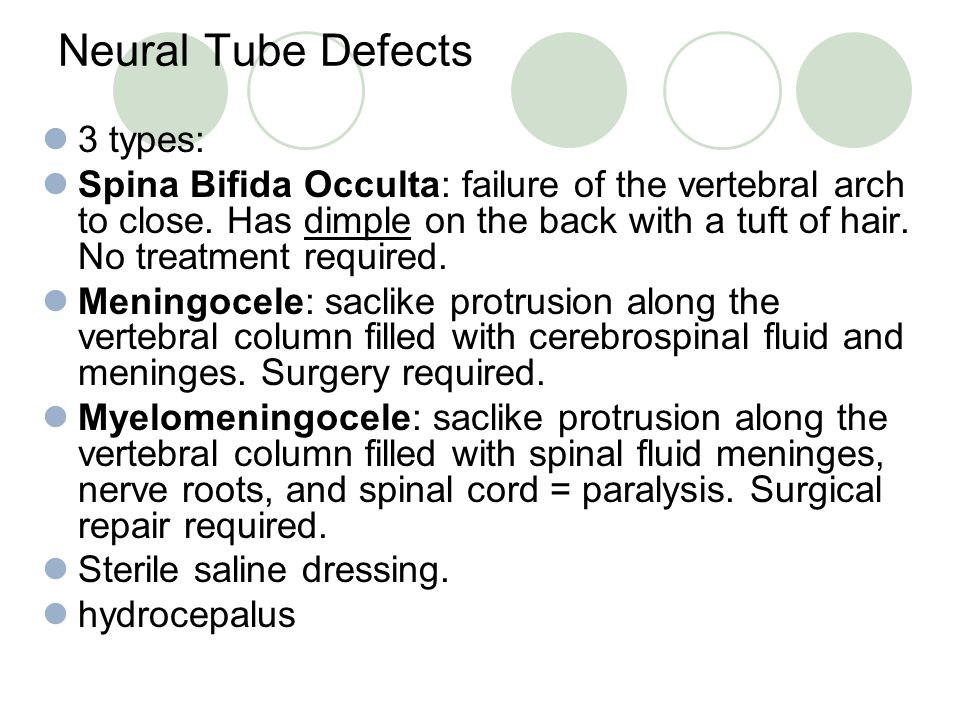
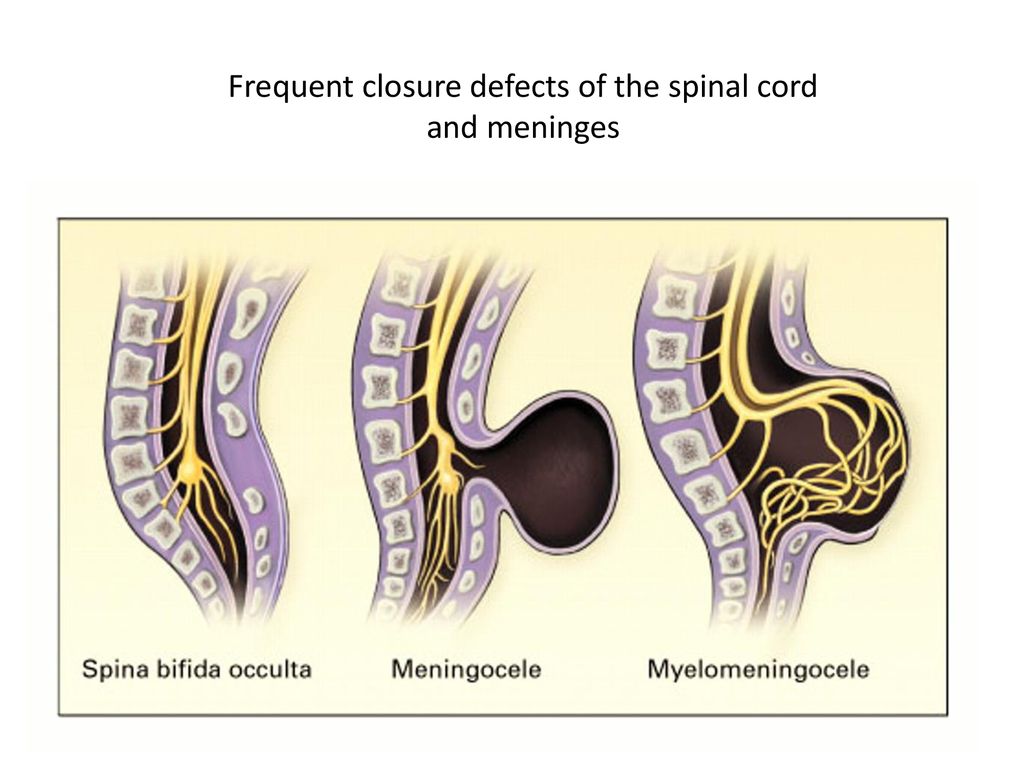
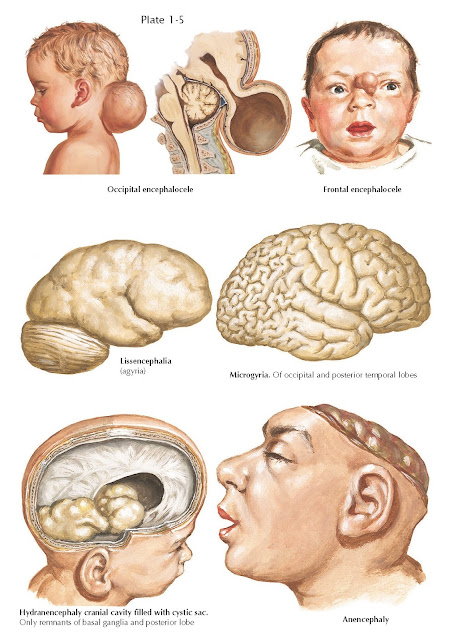
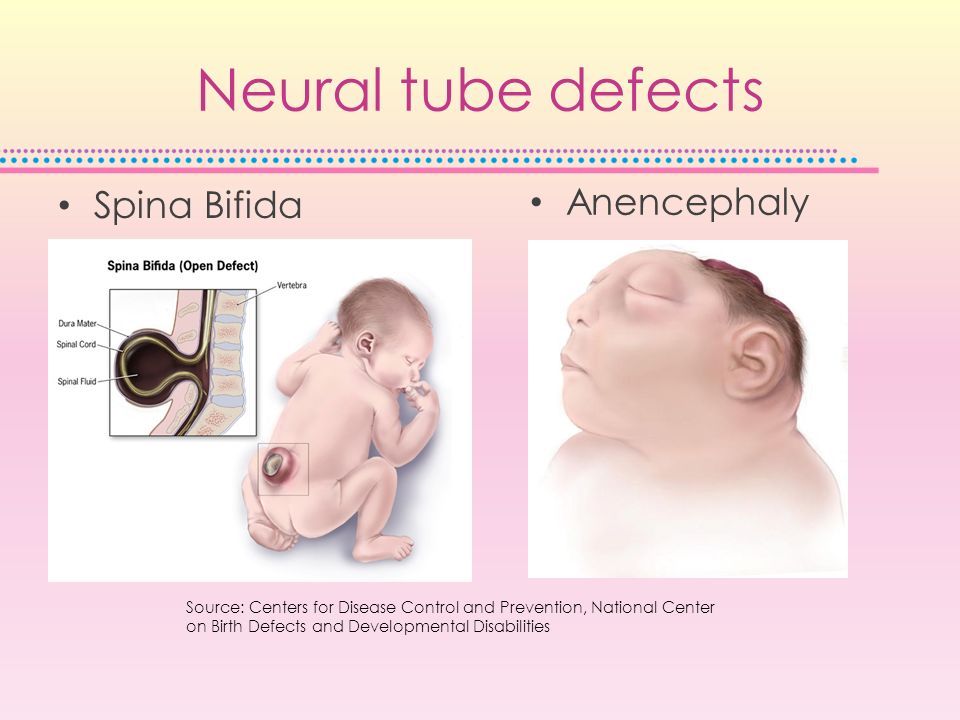
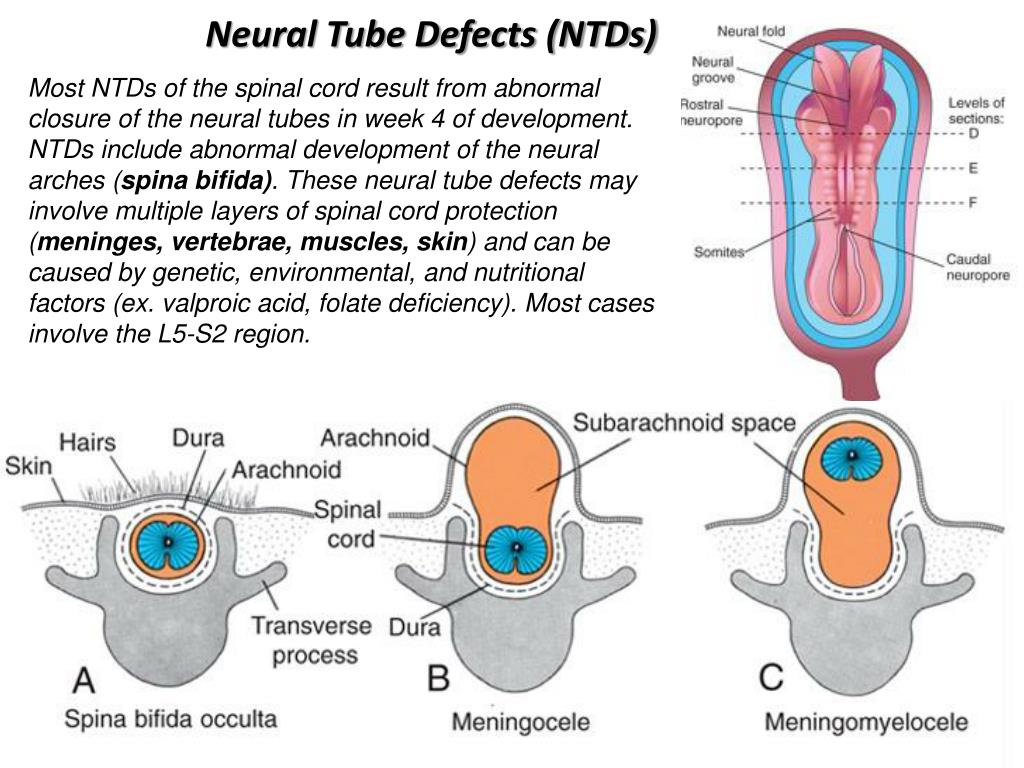
Neural tube defects are birth defects of the brain, spine, or spinal cord. They happen in the first month of pregnancy, often before a woman even knows that she is pregnant. The two most common neural tube defects are spina bifida and anencephaly. In spina bifida, the fetal spinal column doesn't close completely. There is usually nerve damage that causes at least some paralysis of the legs. In anencephaly, most of the brain and skull do not develop. Babies with anencephaly are usually either stillborn or die shortly after birth. Another type of defect, Chiari malformation, causes the brain tissue to extend into the spinal canal.
The exact causes of neural tube defects aren't known. You're at greater risk of having an infant with a neural tube defect if you:
- Have obesity
- Have poorly controlled diabetes
- Take certain antiseizure medicines
Getting enough folic acid, a type of B vitamin, before and during pregnancy prevents most neural tube defects.
Neural tube defects are usually diagnosed before the infant is born, through lab or imaging tests. There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
NIH: National Institute of Child Health and Human Development
- About Neural Tube Defects (NTDs) (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Neural Tube Defects (March of Dimes Birth Defects Foundation)
- Alpha-fetoprotein (AFP) Test (National Library of Medicine) Also in Spanish
- How Do Health Care Providers Diagnose Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Treatments for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Are There Disorders or Conditions Associated with Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Anencephaly (National Institute of Neurological Disorders and Stroke)
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) Also in Spanish
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) - Short Summary
- Encephaloceles (National Institute of Neurological Disorders and Stroke)
- Facts about Anencephaly (Centers for Disease Control and Prevention) Also in Spanish
- Facts about Encephalocele (Centers for Disease Control and Prevention) Also in Spanish
- Hydranencephaly (National Institute of Neurological Disorders and Stroke)
- Iniencephaly (National Institute of Neurological Disorders and Stroke)
- Tethered Spinal Cord Syndrome (National Institute of Neurological Disorders and Stroke)
- How Many People Are at Risk for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Anencephaly (National Institutes of Health)
gov: Anencephaly (National Institutes of Health) - ClinicalTrials.gov: Arnold-Chiari Malformation (National Institutes of Health)
- ClinicalTrials.
 gov: Neural Tube Defects (National Institutes of Health)
gov: Neural Tube Defects (National Institutes of Health)
- Article: Global prevalence of congenital anencephaly: a comprehensive systematic review and meta-analysis.

- Article: High Dietary Folic Acid Intake Is Associated with Genomic Instability in...
- Article: High Folate, Perturbed One-Carbon Metabolism and Gestational Diabetes Mellitus.
- Neural Tube Defects -- see more articles
- Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish
- Find a Genetic Counselor (National Society of Genetic Counselors)
- Find a Pediatrician or Pediatric Specialist (American Academy of Pediatrics) Also in Spanish
- March of Dimes Birth Defects Foundation Also in Spanish
- National Institute of Neurological Disorders and Stroke Also in Spanish
Neural tube defects | Pregnancy Birth and Baby
Neural tube defects | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Neural tube defects are abnormalities that occur in the development of the spinal cord and brain of some babies.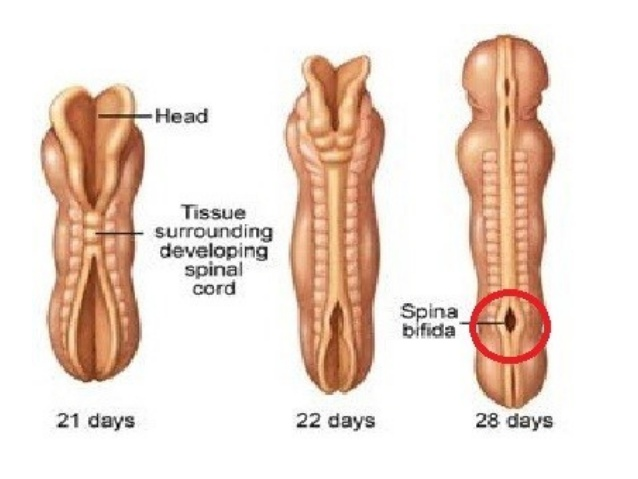 The most common defects are spina bifida (abnormal development of part of the spine and spinal cord) and anencephaly (severely abnormal development of the brain).
The most common defects are spina bifida (abnormal development of part of the spine and spinal cord) and anencephaly (severely abnormal development of the brain).
What are neural tube defects?
During the first month of life, an embryo (developing baby) grows a primitive tissue structure called the ‘neural tube’. As the embryo develops, the neural tube begins to change into a more complicated structure of bones, tissue and nerves that will eventually form the spine and nervous system.
However, in cases of spina bifida, something goes wrong with the development of the neural tube and the spinal column (the ridge of bone that surrounds and protects the nerves) does not fully close. Spina bifida is a Latin term that means ‘split spine’.
The chance that a pregnancy will be affected by a neural tube defect is less than one in 1,000.
What causes neural tube defects?
The cause of neural tube defects is not certain, but it appears to be due to a combination of genetic and environmental factors.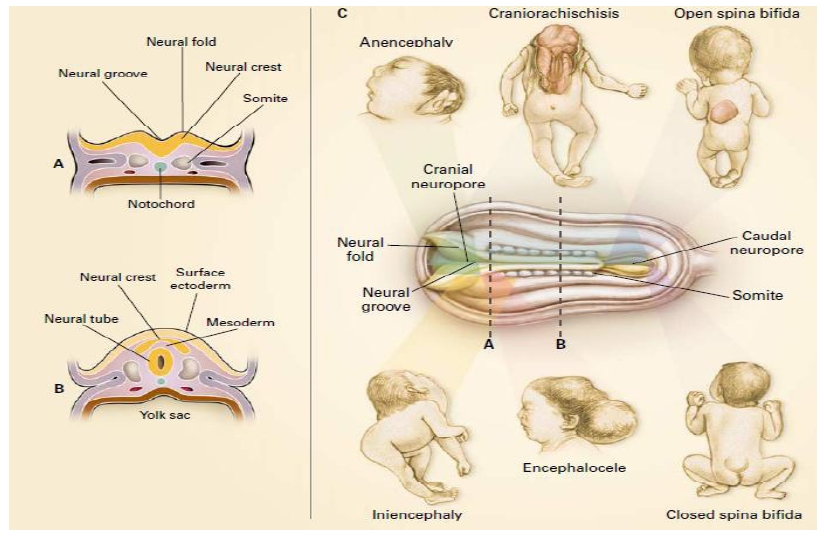
Women are at increased risk of having a baby with a neural tube defect if:
- they have already had a baby with a neural tube defect
- they or their partner have a close relative born with a neural tube defect
- they have type 1 (insulin dependent) diabetes (not gestational diabetes)
- they are obese, or take certain anti-epileptic medications, especially those containing sodium valproate or valproic acid
Prevention
About 2 in 3 neural tube defects can be prevented through increasing folate (folic acid) intake at least a month before pregnancy and during the first 3 months of pregnancy. Adequate folate levels are critical during the early days of the developing embryo, particularly the 3rd and 4th week, the period in which neural tube defects occur and when many women won't know they are pregnant.
You can increase your folate intake by eating folate-rich foods, including folate-fortified foods in your daily diet, or by taking a folic acid supplement.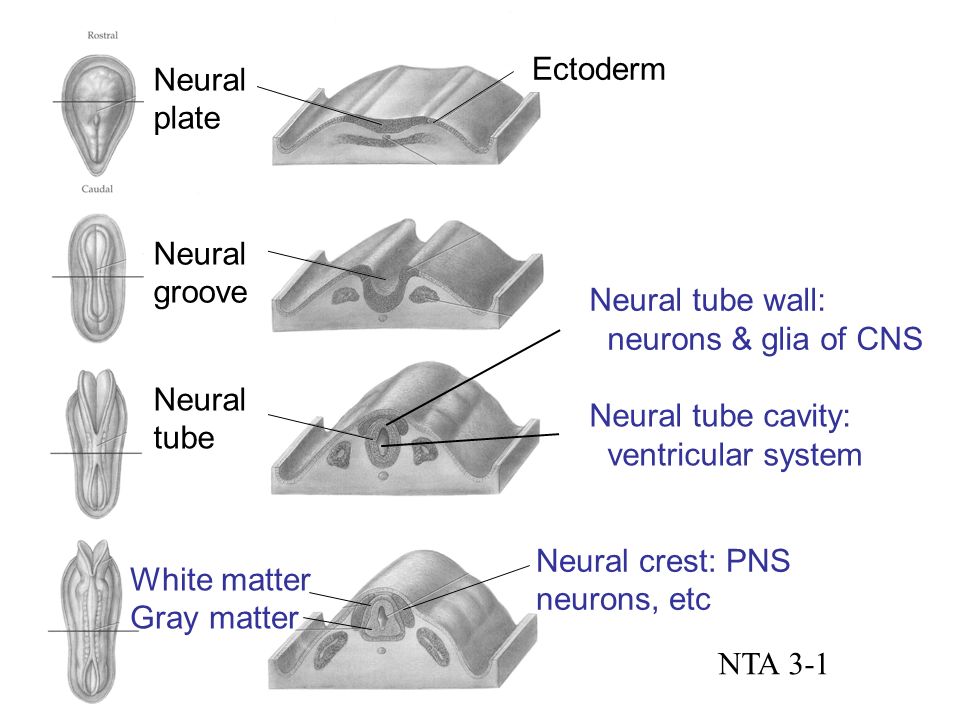 Good sources of folate include green leafy vegetables, fruit (citrus, berries and bananas), legumes and some cereals (bread and many breakfast cereals now have added folate).
Good sources of folate include green leafy vegetables, fruit (citrus, berries and bananas), legumes and some cereals (bread and many breakfast cereals now have added folate).
Women who take medicines to control epilepsy, seizures or psychiatric disorders should talk to their doctor before taking folate because it can interfere with how their medications work.
For more information see folate and pregnancy.
Diagnosis
Neural tube defects may be diagnosed during the ultrasound scan that is carried out around week 12 of the pregnancy or, more likely, during the anomaly scan that is carried out at around weeks 18 to 20.
Ultrasound scans
An ultrasound scan is a safe procedure that uses sound waves to create an image of the inside of your body. Most hospitals will offer women at least 2 ultrasound scans during their pregnancy. The first is usually at around 8 to 14 weeks and is sometimes called the ‘dating scan’ because it can help to determine when the baby is due.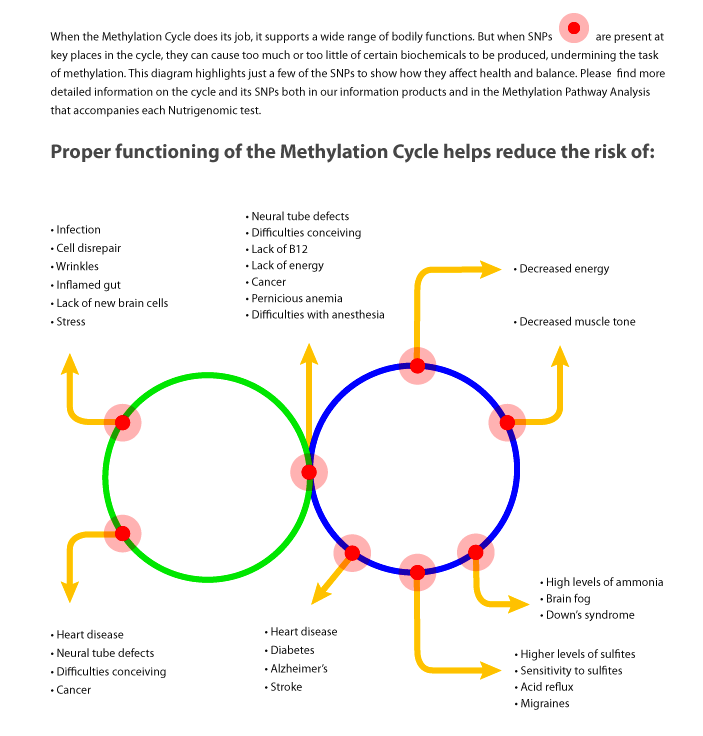 This first scan may be able to detect problems with your baby’s spine that could indicate spina bifida if the condition is severe. If a dating scan is done earlier than 12 weeks, another ultrasound called the nuchal translucency scan is done at 12 weeks to check amongst other things for signs of Down Syndrome, and if a dating scan is not done prior to this then this scan can be used as the dating scan.
This first scan may be able to detect problems with your baby’s spine that could indicate spina bifida if the condition is severe. If a dating scan is done earlier than 12 weeks, another ultrasound called the nuchal translucency scan is done at 12 weeks to check amongst other things for signs of Down Syndrome, and if a dating scan is not done prior to this then this scan can be used as the dating scan.
Morphology scan
The morphology or anomaly scan is an ultrasound scan that is carried out around weeks 18 to 20 of your pregnancy. This scan aims to identify any physical problems with your baby. It is usually during this scan that spina bifida is diagnosed.
Coping with the results
If tests confirm that your baby has spina bifida, the implications will be fully discussed with you. You will need to consider your options carefully. Your options are to:
- continue with your pregnancy while getting information and advice so that you are prepared for caring for your baby
- end your pregnancy
If you are considering ending your pregnancy, you should talk to your doctor or midwife.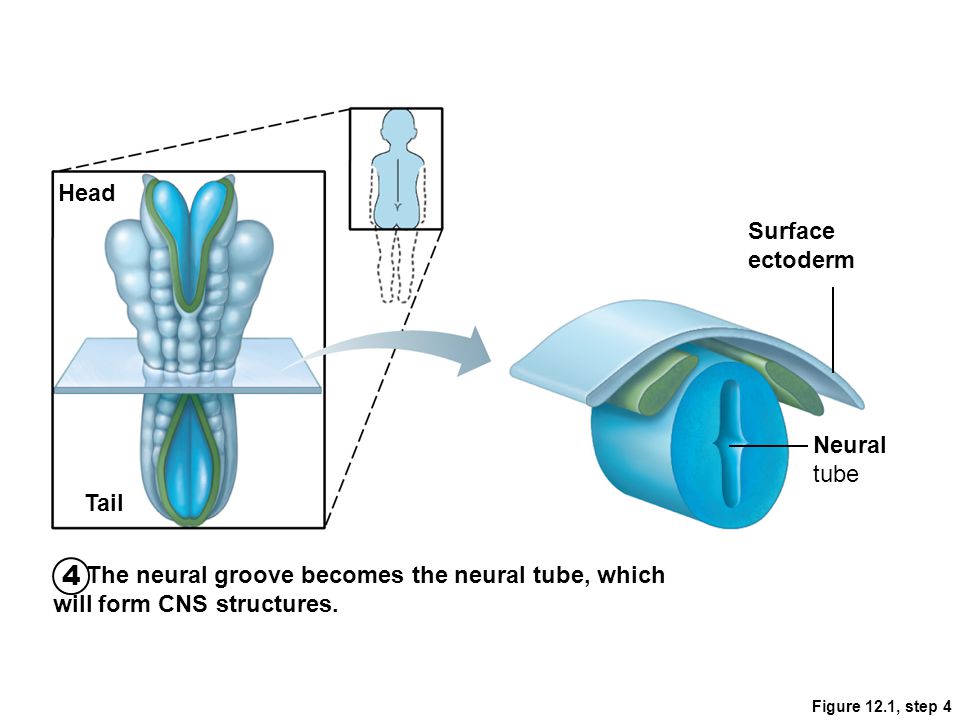 They will be able to provide you with important information and advice.
They will be able to provide you with important information and advice.
Your options for ending your pregnancy will depend on how many weeks pregnant you are when you make the decision. If you decide to end your pregnancy, you may wish to talk to a counsellor afterwards. Your doctor or midwife will be able to arrange this for you.
Call Pregnancy, Birth and Baby on 1800 882 436 to discuss your options regarding your pregnancy with a maternal child health nurse.
Sources:
Australian Institute of Health and Welfare (Neural tube defects in Australia), The Centre for Genetics Education (Neural tube defects – spina bifida and anencephaly), RANZCOG (Planning for pregnancy), Women's and Children's Health Network (Screening tests for neural tube defects), Sydney Children's Hospital Network (Factsheet: What is spina bifida?)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2020
Back To Top
Need more information?
Pregnancy checkups, screenings and scans
Knowing what check-ups, screenings and scans to have and when to have them during your pregnancy is important information for every pregnant woman.
Read more on Pregnancy, Birth & Baby website
Neural tube defects: children & teens | Raising Children Network
Neural tube defects are brain and spinal cord abnormalities, including spina bifida, encephalocele and anencephaly. Read how they affect children.
Read more on raisingchildren.net.au website
Folate and pregnancy
Folate and folic acid are important for pregnancy since they can help prevent birth defects known as neural tube defects, such as spina bifida.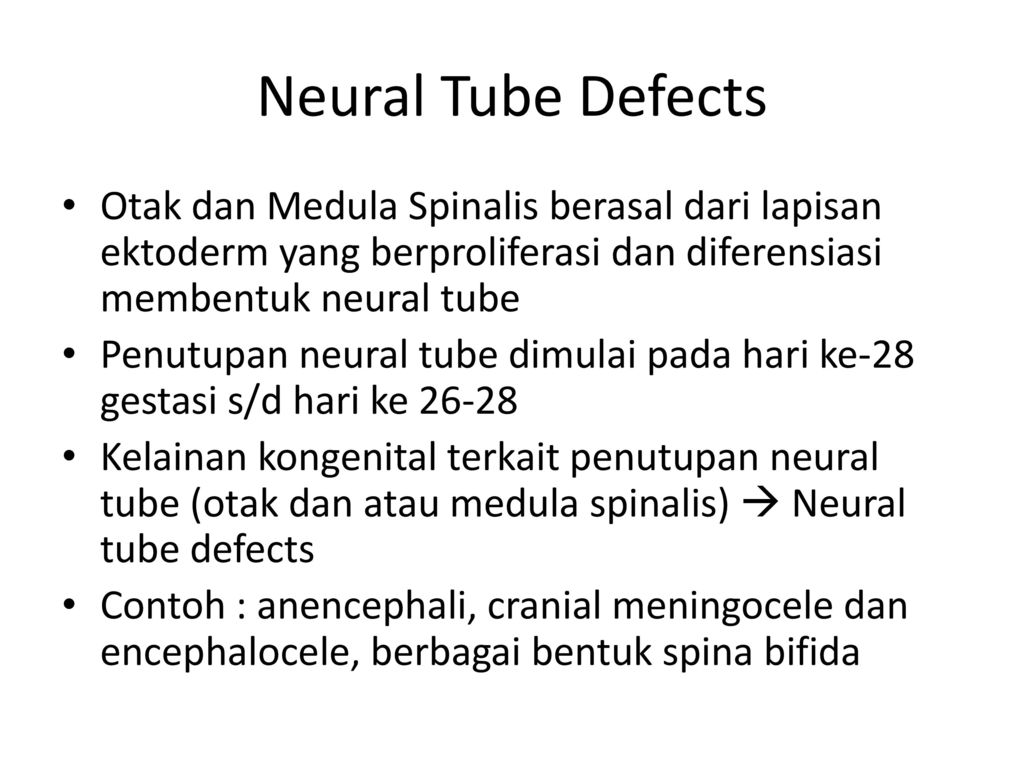
Read more on Pregnancy, Birth & Baby website
Spina bifida
Spina bifida is a condition that affects the normal development of a baby’s spine early in pregnancy.
Read more on Pregnancy, Birth & Baby website
Spina Bifida | Sydney Children's Hospitals Network
Spina Bifida comes from a latin term which means “split spine”
Read more on Sydney Children's Hospitals Network website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Folic acid & iodine fortification, Summary - Australian Institute of Health and Welfare
Mandatory folic acid and iodine fortification of bread resulted in increased levels of folic acid and iodine in the food supply, increased folic acid and iodine intakes, a decreased rate of neural.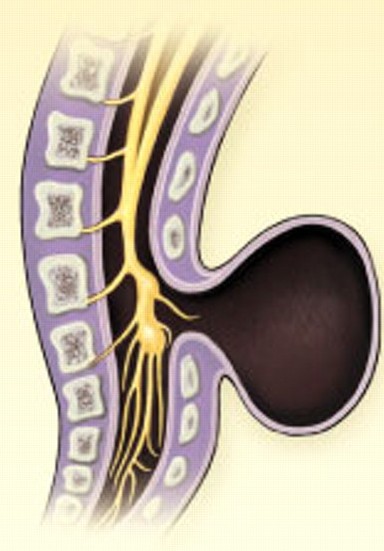 ..
..
Read more on AIHW – Australian Institute of Health and Welfare website
Folate | Jean Hailes
Folate is a B vitamin needed for healthy growing, in particular for the nervous system.
Read more on Jean Hailes for Women's Health website
What supplements should I take during pregnancy? | Queensland Health
Find out what supplements and vitamins you need to take when trying to get pregnant, during pregnancy, after pregnancy and while breastfeeding.
Read more on Queensland Health website
Pregnancy at weeks 1 to 4
When you conceive, your body’s hormone levels change, but you may not notice any signs that you’re pregnant yet.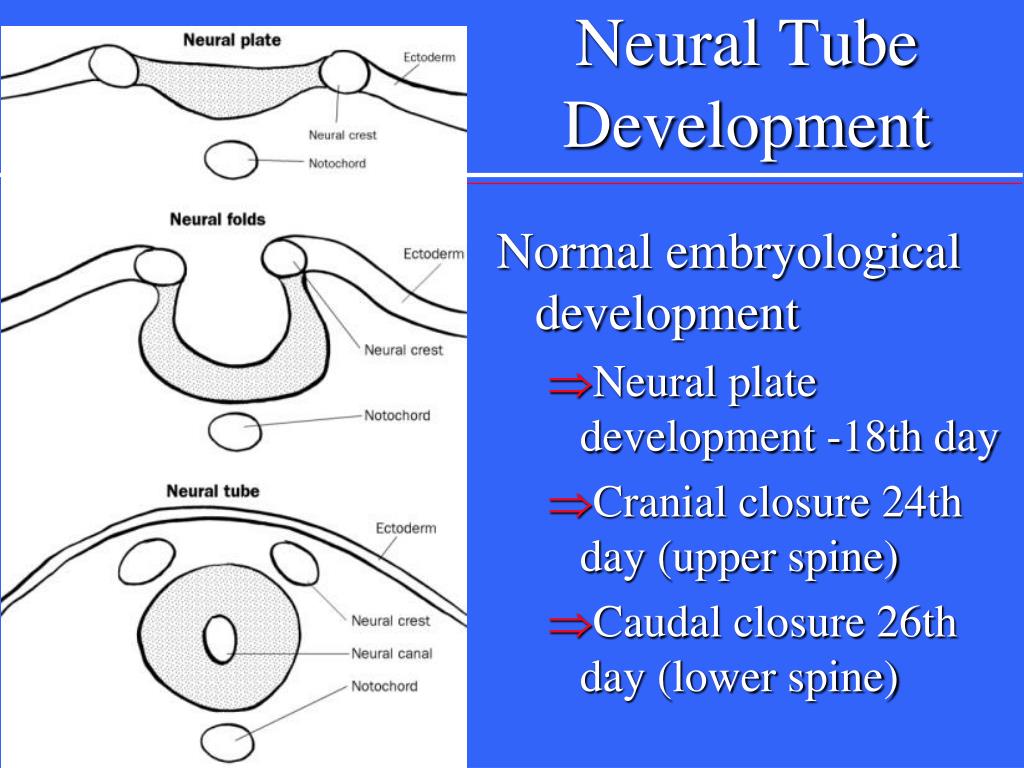
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.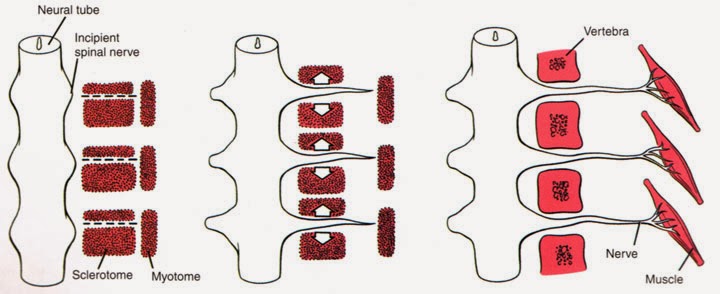
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Malformations
Malformations- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- D
- E
- 9000
- f
- x
- C
- h
- Sh
9000 WHO in countries »- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.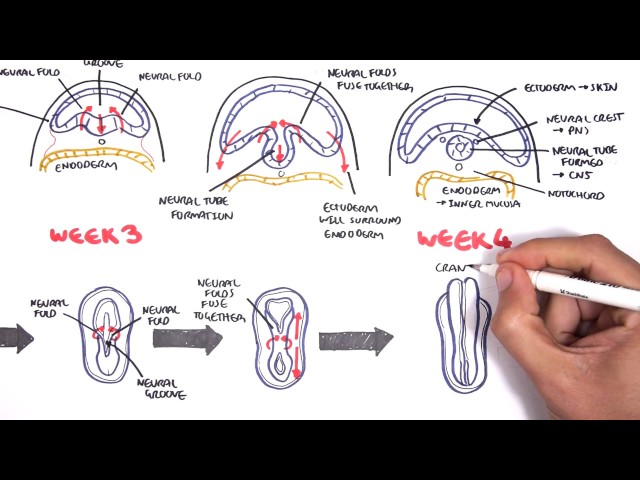 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
\n
Genetic factors
\n
\nIncest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiency in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations.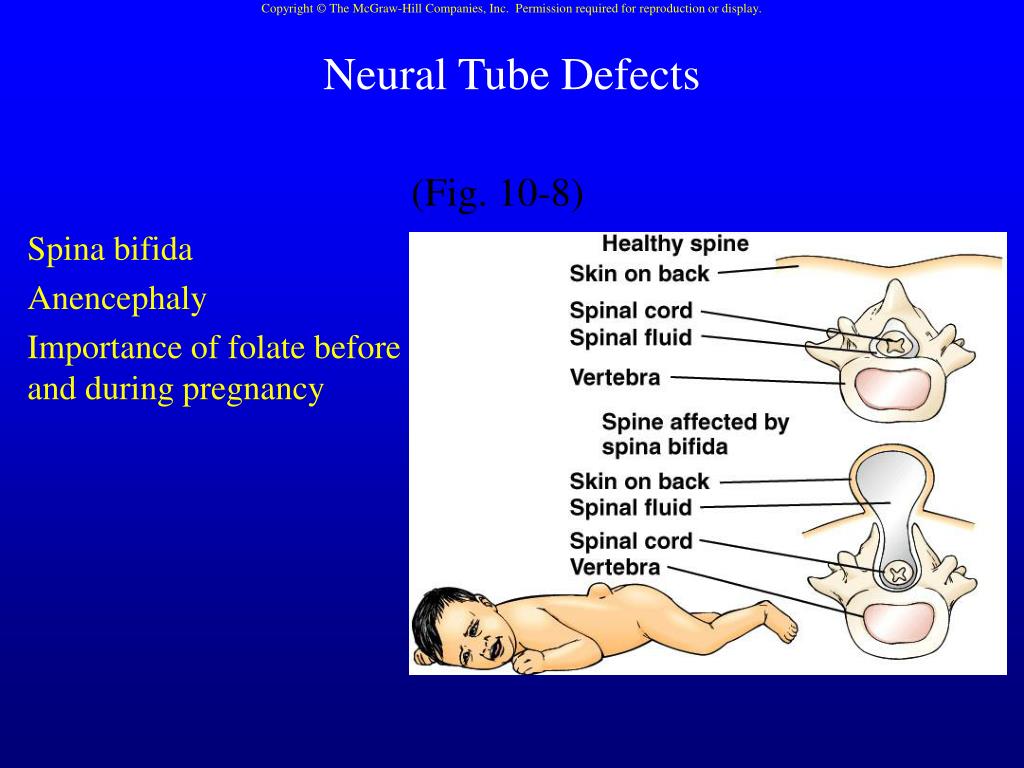 For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
\n
Prevention
\n
\nPregnancy and conception preventive health care, and prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 \n
\n - Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol. \n
- Prevention of diabetes during pre-pregnancy and pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposures (such as x-rays) is justified and based on a careful analysis of the health risks and benefits. \n
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. \n
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and intensifying training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (peri-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 \n
\n - Preconception screening: Maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. \n
- Newborn screening includes a clinical examination, as well as screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and ensure that children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.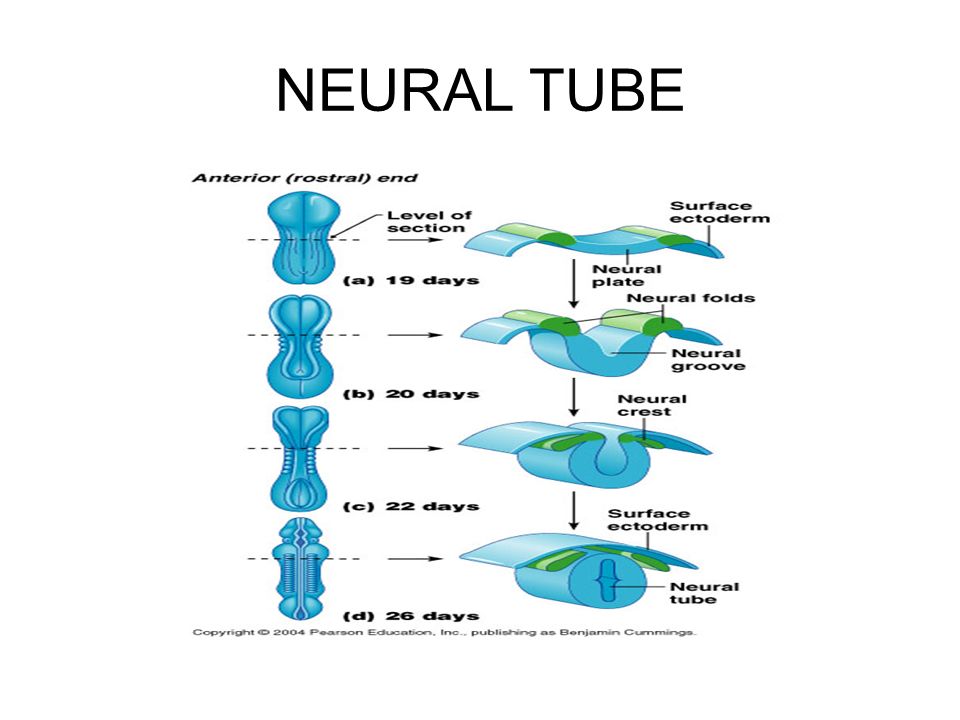
\n
\nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy to fortify foods with salt folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.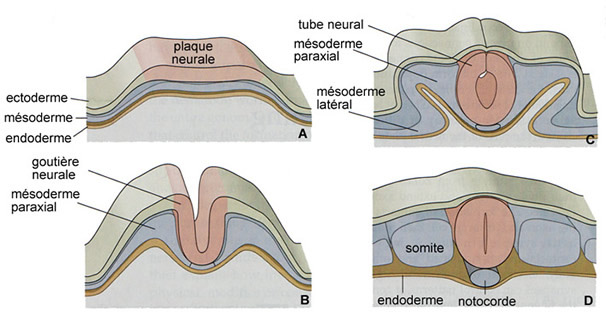 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.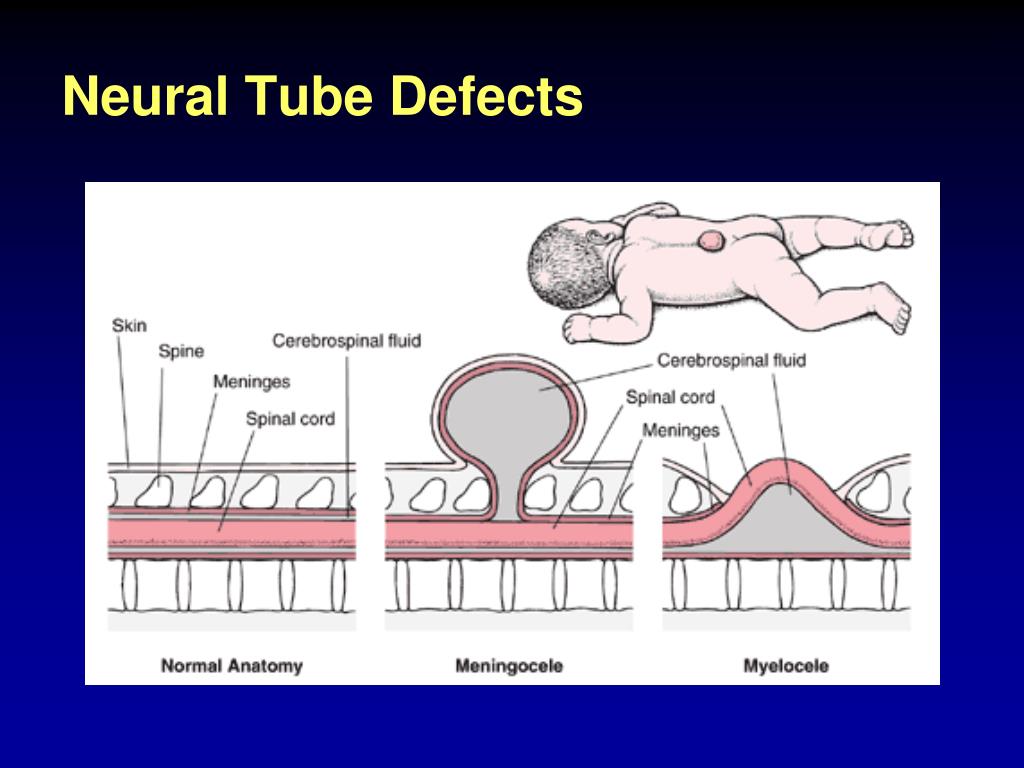
\n
\nWHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).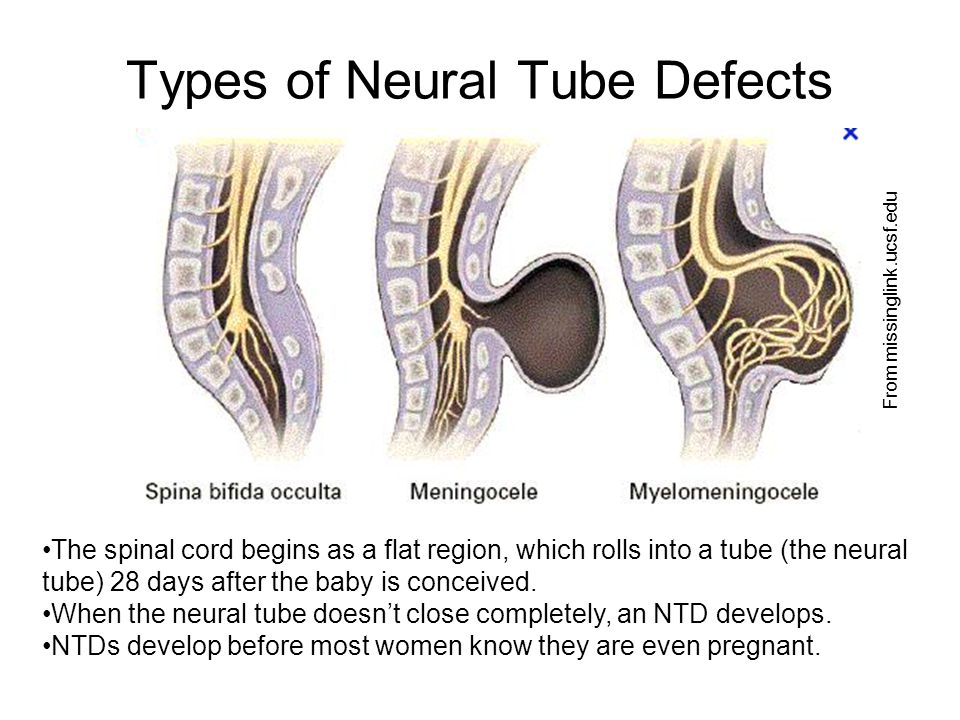
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"};
Key Facts
- An estimated 303,000 children die each year from malformations in the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, with significant impacts on individuals, their families, health systems and society.
- The most severe malformations include heart defects, neural tube defects and Down's syndrome.
- Although malformations may be genetic, infectious or environmental in origin, the exact cause is often difficult to establish.
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect.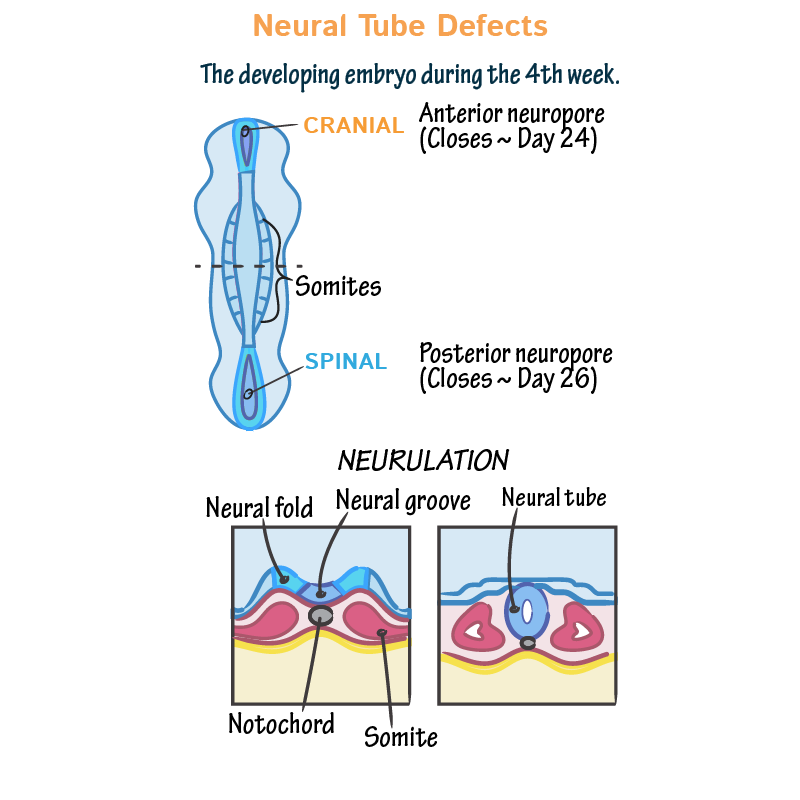 In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .
- Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous environmental substances (eg, heavy metals, pesticides, certain drugs).
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (eg x-rays) is justified and based on a careful analysis of the health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood.
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and intensifying training for health professionals and other staff involved in strengthening the prevention of malformations.
Identification
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: Maternal characteristics may increase risk and screening results should be used to provide appropriate care based on risk.
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. - Newborn screening includes a clinical examination, as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.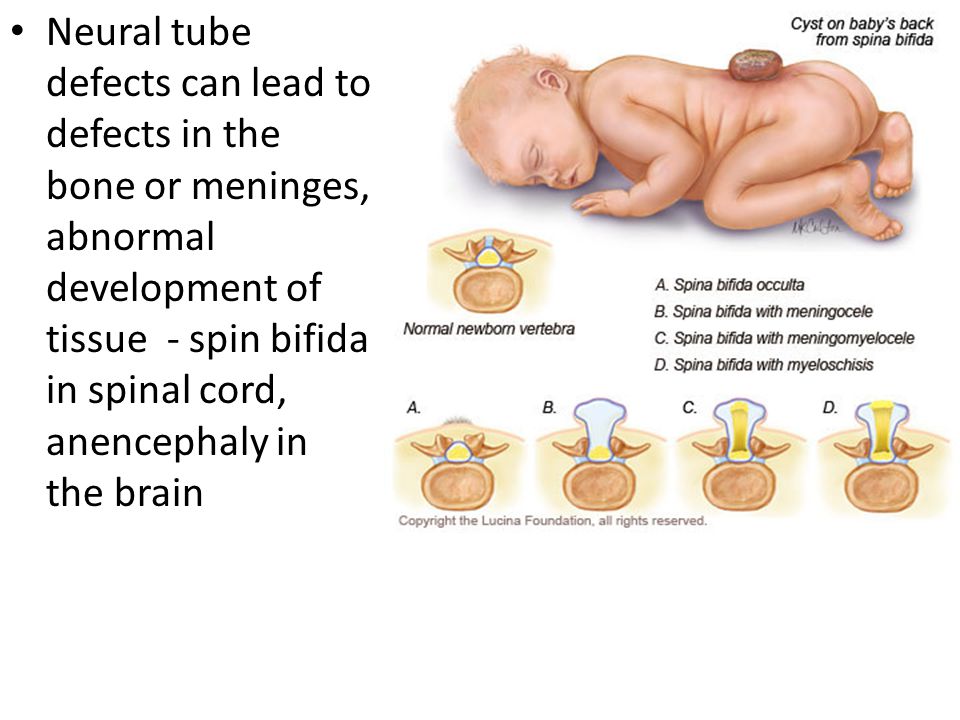
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.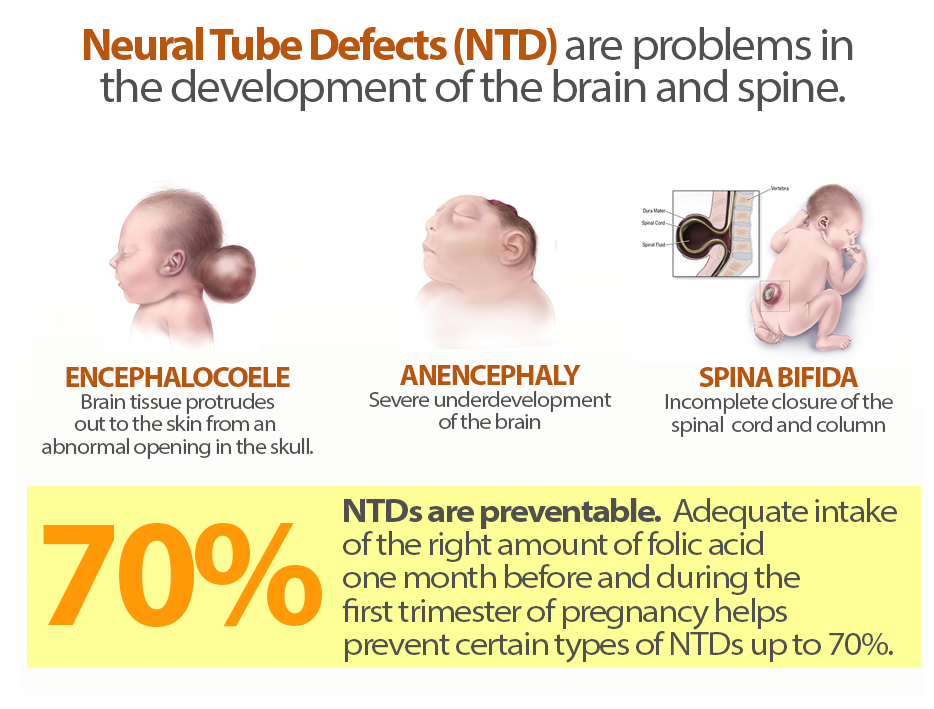
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, not-for-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.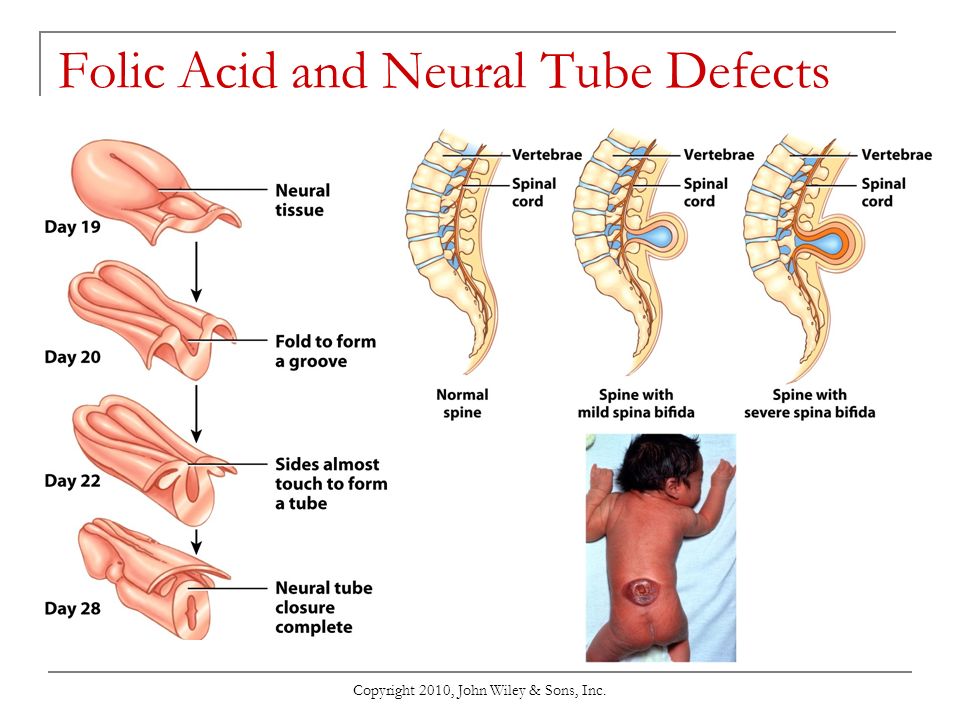
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).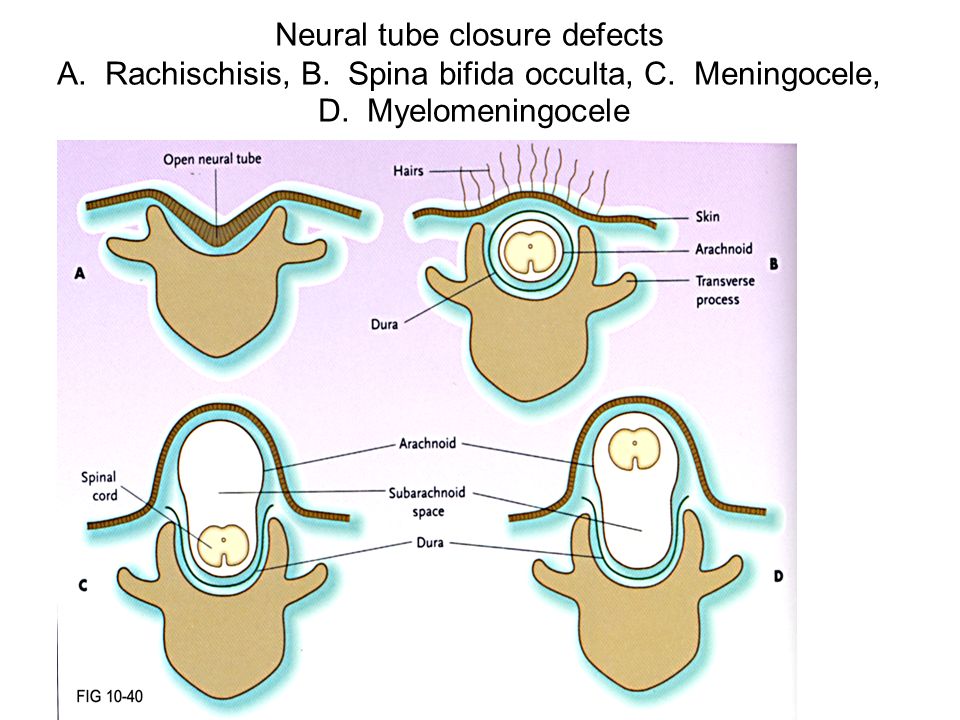
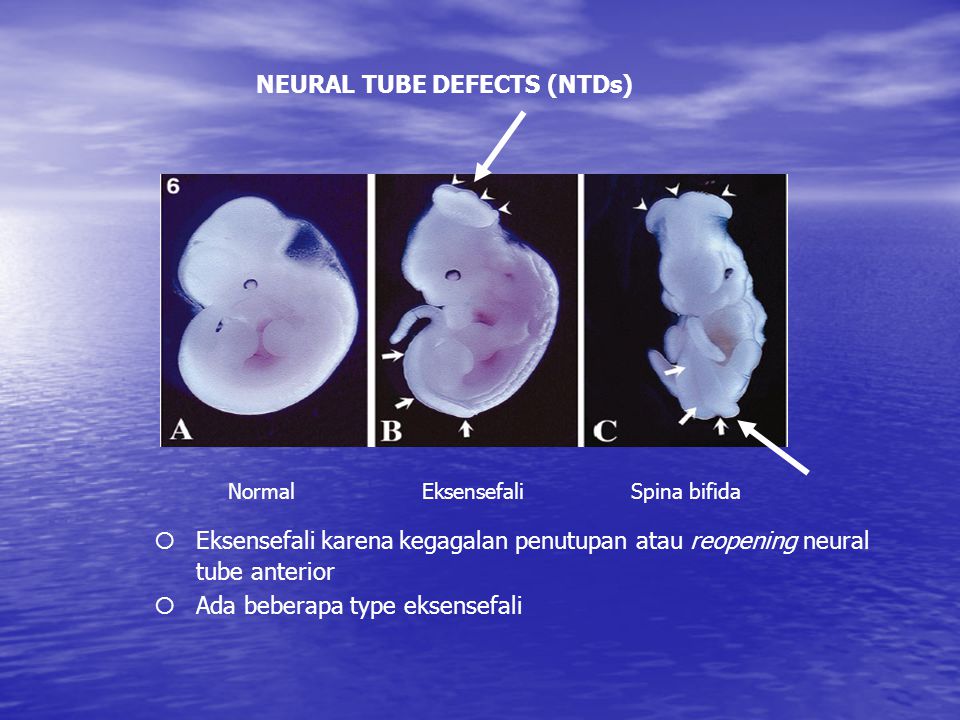
Neural tube formation process and malformations
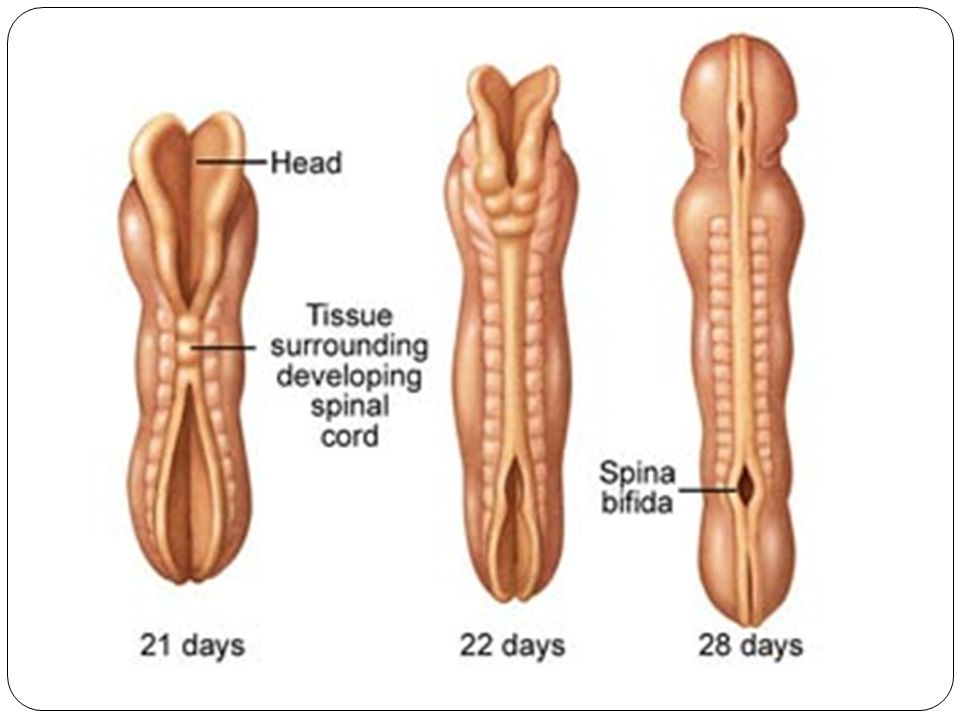
The process of neural tube formation is called neurulation. Neurulation of begins with the appearance of the neural plate, which invaginates into the spine to form a neural network with neural grooves on either side of the spine. Gradually, the neural grooves approach each other along the midline of the spine and merge, thus transforming the neural grooves into a neural tube.
Formation of the neural tube begins in the region of the future neck at the level of the 4th somite (4 segments of the cervical spine). Neurulation begins 16 days after fertilization and ends on days 21-22. Neurulation in humans occurs in several stages. First, the dorsal section of the spine closes, then the closure occurs in the area from the forehead to the parietal tubercles, the third stage closes the facial section of the skull, then the section from the occipital lobes to the cervical spine, and the last stage closes the sacral section.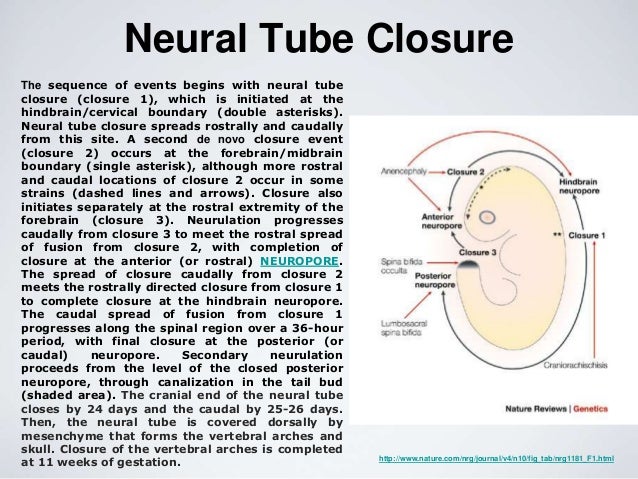
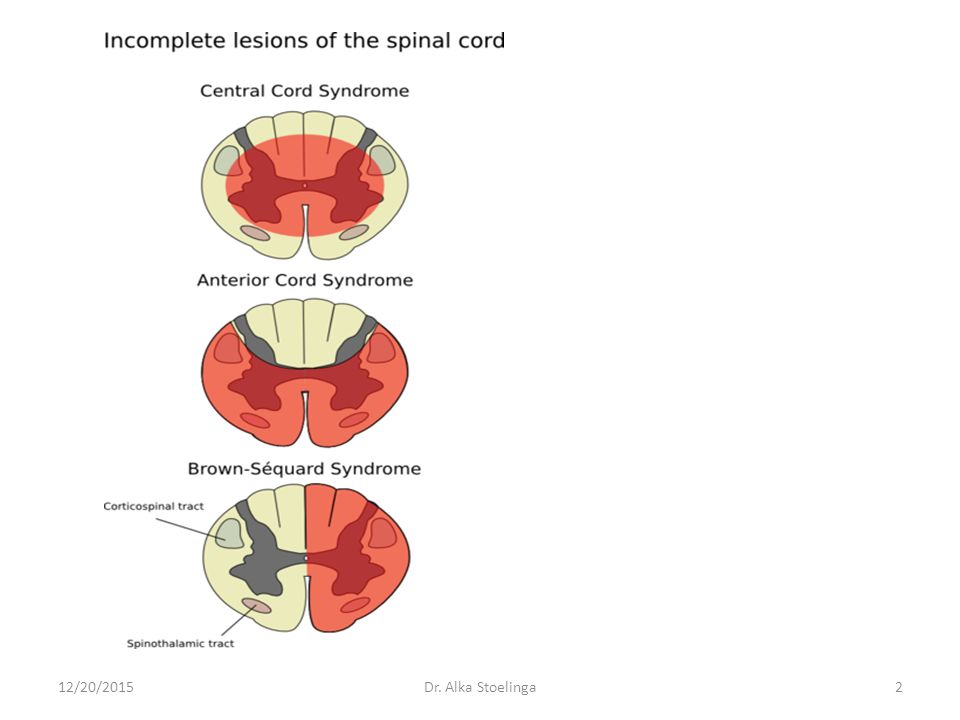
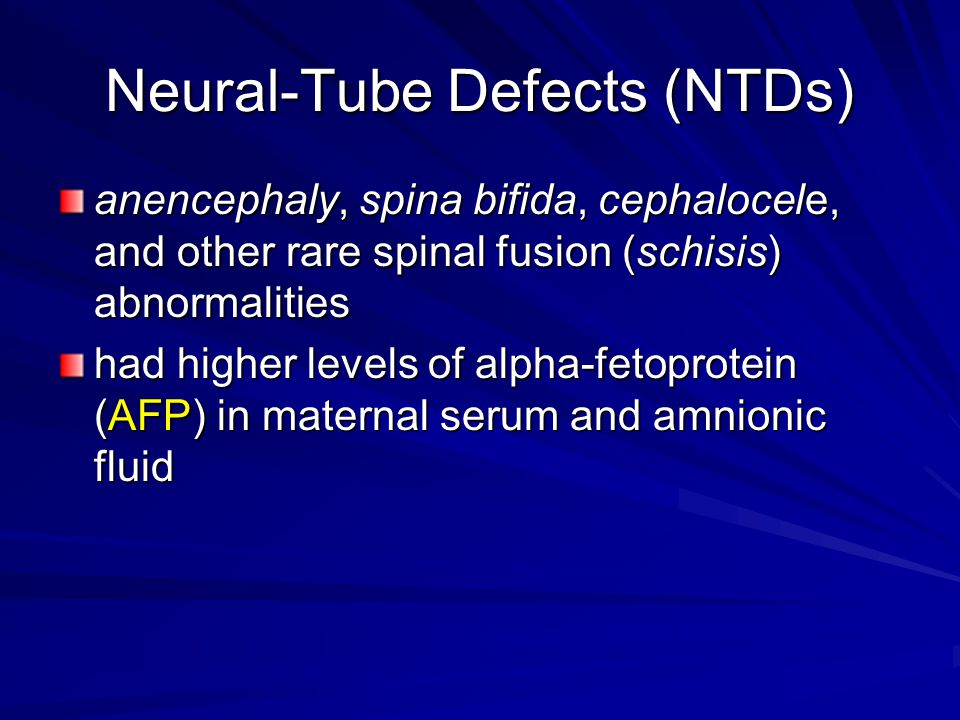
In case of neurulation disorders congenital malformations are detected at the stages of neural tube closure, such as:
- anencephaly (congenital absence or underdevelopment of the brain and cerebellum),
- spina bifida - Spina Bifida,
- exencephaly (absence of skull bones)
and other defects of the central nervous system. Neural tube closure defects are quite rare. With severe defects in the development of the neural tube, such as anencephaly, spina bifida, the fetus dies in the womb or is born non-viable and dies in the coming days after birth. Modern equipment helps to detect neural tube malformations at regular check-ups during pregnancy. With early diagnosis of malformations of the neural tube, termination of pregnancy is indicated.
The formation of the human neural tube is a complex interaction between genetic and environmental factors. Some genes are important for neural tube formation, but dietary factors such as cholesterol and folic acid levels are also important for proper neural tube formation.