Can vomiting cause miscarriage
Your mom was right: “Morning sickness” means a lower chance of miscarriage
There are a lot of old wives’ tales when it comes to pregnancy. If you have heartburn, it means the baby will have a lot of hair. If the baby’s heartbeat is under 140, you are having a boy. If you have nausea and vomiting, you won’t have a miscarriage.
The first two are myths. A recent study suggests that last one may be true.
Over three-quarters of women report nausea with or without vomiting in early pregnancy. Nausea and vomiting in pregnancy can wreak havoc on a woman’s well-being and quality of life. Many have speculated that nausea is a good sign that indicates a healthy pregnancy, but until now, solid evidence supporting this notion was lacking.
A recent study in JAMA Internal Medicine sheds new light on this issue. This study was powerful because patients were enrolled before conception, and they recorded symptoms of nausea and vomiting even before they knew they were pregnant. This study design is known as a prospective, preconception cohort. Women who participated in the study had either one or two prior pregnancy losses. Nearly two-thirds of women reported nausea by the eighth week of pregnancy, and over a quarter had both nausea and vomiting. Nausea alone or nausea with vomiting was associated with a 50% to 75% reduction in the risk of pregnancy loss.
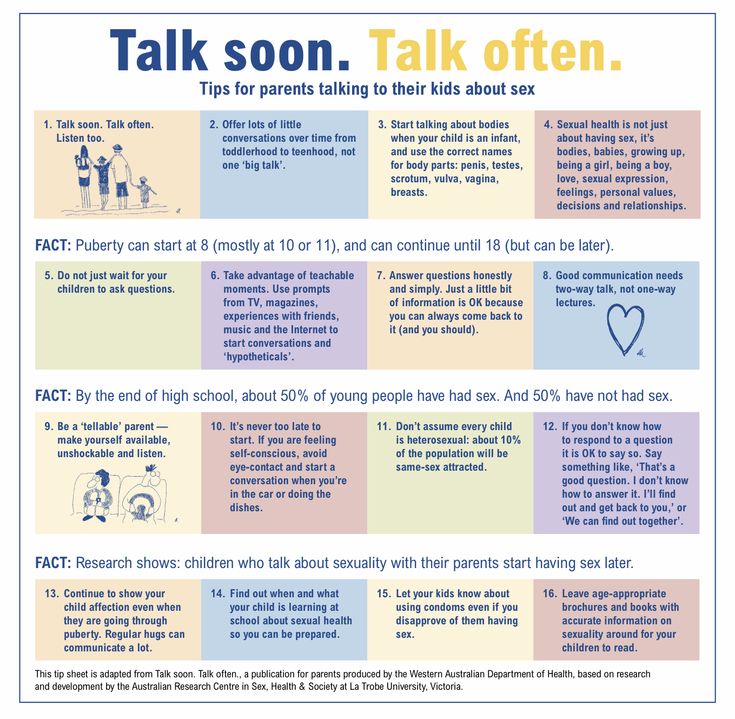
Nausea and vomiting during pregnancy is often called “morning sickness,” but is better termed “all day sickness” since it can occur at any time, including at night. Typically it starts by eight weeks of pregnancy and goes away by the second trimester. For a few unlucky women, it lasts for several weeks or months.
Diet and lifestyle changes can help alleviate it. Most women find eating toast or crackers first thing in the morning, even before getting out of bed, is a good trick, since an empty stomach makes nausea worse. Similarly, nibbling crackers periodically, so called “grazing,” drinking fluids, and eating small, frequent meals instead of three large meals can also help. Ginger (ginger ale or tea made from real ginger, or ginger candy chews) has been shown to ease nausea. Vitamin B6 supplements and doxylamine, a medication found in over-the-counter sleep aids, can help. A prescription drug that combines vitamin B6 and doxylamine is available. These have been found to be safe to take during pregnancy. Your health care provider can also recommend prescription anti-nausea drugs if these measures don’t help.
Ginger (ginger ale or tea made from real ginger, or ginger candy chews) has been shown to ease nausea. Vitamin B6 supplements and doxylamine, a medication found in over-the-counter sleep aids, can help. A prescription drug that combines vitamin B6 and doxylamine is available. These have been found to be safe to take during pregnancy. Your health care provider can also recommend prescription anti-nausea drugs if these measures don’t help.
The news that nausea and vomiting is a positive sign may provide reassurance and help women experiencing these difficult symptoms in pregnancy to endure them, knowing light is at the end of the tunnel.
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Does Morning Sickness Really Prevent Miscarriage?
Health
A new study of pregnant women finds nausea and vomiting are associated with a reduced risk of miscarriage.
By Adrienne LaFrancePregnant women attempt to set an attendance record for prenatal yoga in Beijing, in 2015. (China Stringer Network / Reuters)People are always saying the wrong thing to pregnant women.
Expectant mothers hear everything from the obnoxious (“You’re huge!”) to the outright bizarre (“If you eat that Sriracha, your baby will come out bald”).
Then there are the well-meaning—yet utterly unhelpful—superstitions and platitudes: “I can tell from how you’re carrying that it’s a girl.” (No, you can’t.) “At least the terrible sleep you’re getting now is great preparation for all those sleepless nights you’re going to have with baby!” (Bone-splitting exhaustion is not something you need to practice ahead of time.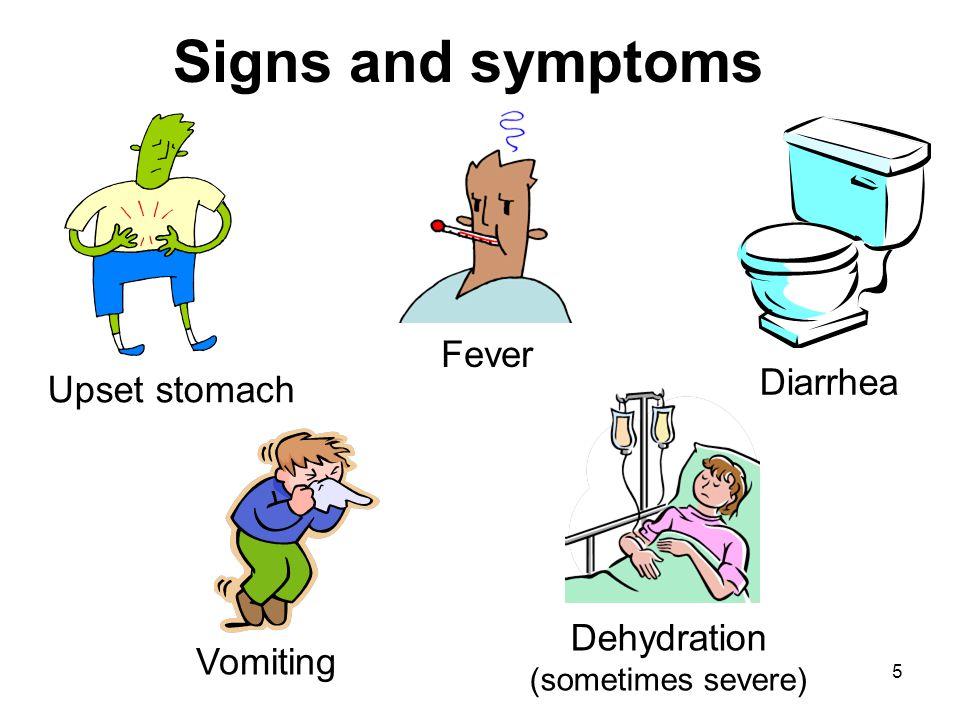 ) “But morning sickness means your baby is healthy!”
) “But morning sickness means your baby is healthy!”
Actually, there might be something to that last one.
Pregnant women have long been told that feeling miserable every single day for several months may indicate that a developing baby is doing well—especially in the first trimester, when nausea and vomiting are most common. Now, there’s more science to support the idea.
A new study from researchers at the National Institutes of Health, and published today in JAMA Internal Medicine, finds morning sickness is associated with a lower risk of miscarriage in pregnant women who have experienced previous losses. The NIH calls the research, which builds on similar studies, “the strongest evidence to date” that nausea and vomiting in pregnant women are associated with a lower risk of pregnancy loss.
The latest NIH study, which was a secondary analysis of data from a separate clinical trial, involved tracking symptoms logged daily by nearly 800 pregnant women. All of the women in the study had at least one previous pregnancy loss, with about one-third of the participants having experienced two losses.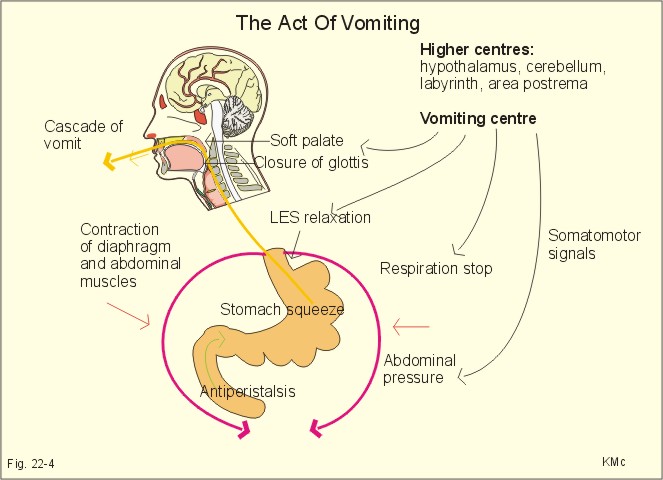
About 84 percent of the women reported nausea, with or without vomiting, by the time they were eight weeks pregnant. (Smaller percentages of women had morning sickness earlier in pregnancy—with about 20 percent of them reporting illness at two weeks pregnant, and more than 50 percent of them reporting nausea or vomiting by five weeks.) Nearly one-quarter of the pregnancies resulted in miscarriage, many of which occurred before the eight-week mark.
Overall, the women who reported nausea by itself or nausea with vomiting were between 50 percent and 75 percent less likely to miscarry than those who didn’t feel sick.(Earlier research, including a 2014 meta-analysis of 10 separate studies conducted between 1992 and 2012, has also found that women who had morning sickness experienced fewer miscarriages and gave birth to larger, healthier babies with fewer birth defects.)
But even though earlier studies have found similar associations, few researchers have taken into account the other potential indicators for miscarriage among study participants—like the number of previous pregnancy losses a woman has experienced, alcohol intake during pregnancy, and fetal characteristics such as chromosomal abnormalities. Such factors might increase the likelihood of miscarriage, even among women who experience morning sickness. The NIH researchers controlled for these and other circumstances in their assessment, giving them a clearer picture that the association between morning sickness and reduced pregnancy loss is strong—without confounding factors getting in the way.
Such factors might increase the likelihood of miscarriage, even among women who experience morning sickness. The NIH researchers controlled for these and other circumstances in their assessment, giving them a clearer picture that the association between morning sickness and reduced pregnancy loss is strong—without confounding factors getting in the way.
The NIH study was unusual, too, in that it began with women who were still trying to conceive—rather than first enrolling participants who were already pregnant. “This is important because it allowed us to get detailed data from diaries that women were keeping about their symptoms in the earliest weeks of pregnancy—even before most women knew they were pregnant,” said Stefanie Hinkle, a staff scientist at the NIH, and the lead author of the study. “We found that in the week after conception, one in five women were already experiencing some nausea symptoms.”
The protective benefit of morning sickness was stronger among women who were throwing up compared with those who just felt crummy—up to a point, anyway.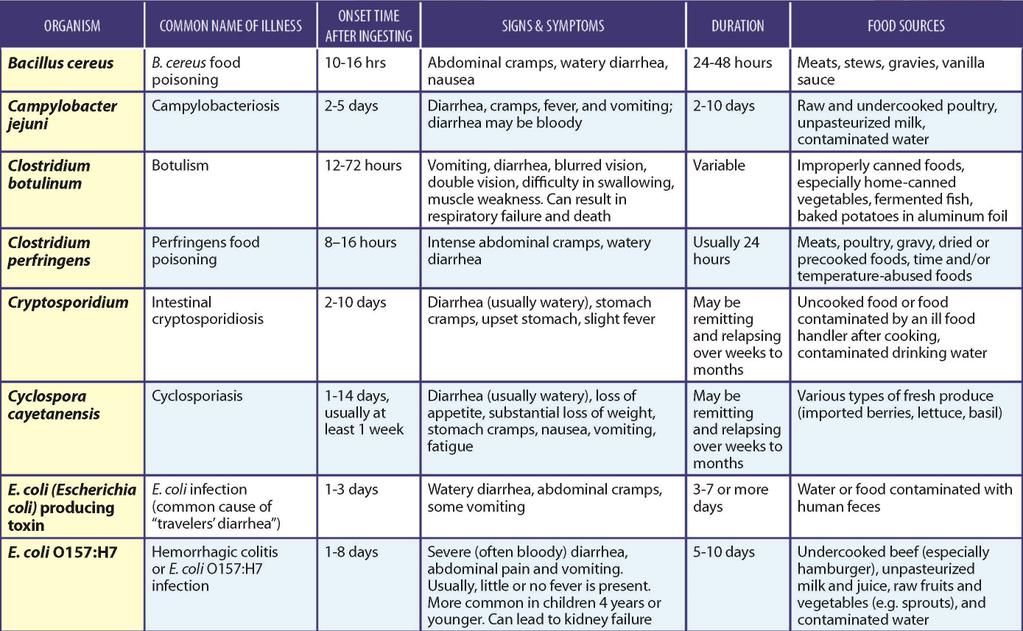 Researchers didn’t include findings from women who experienced hyperemesis, a severe form of nausea and vomiting during pregnancy that can lead to hospitalization—meaning the study’s findings do not apply to women with the very worst symptoms. The study had some other limitations, too. The vast majority of participants were married, highly educated, white women—so the extent to which the findings would apply to women in other demographics is unclear.
Researchers didn’t include findings from women who experienced hyperemesis, a severe form of nausea and vomiting during pregnancy that can lead to hospitalization—meaning the study’s findings do not apply to women with the very worst symptoms. The study had some other limitations, too. The vast majority of participants were married, highly educated, white women—so the extent to which the findings would apply to women in other demographics is unclear.
Researchers still don’t understand what mechanism is responsible for the protective association between feeling miserable and having a healthy pregnancy, though they have some ideas about what might cause the nausea in the first place. Scientists have suggested that pregnancy illness is a byproduct of rapid hormonal changes, especially the increase of human chorionic gonadotropin, or hCG. (The presence of hCG in a woman’s urine is what makes a home pregnancy test positive.) “Another possibility is that nausea and vomiting are markers for viable placental tissue,” Hinkle and her colleagues wrote in the NIH paper. “Thus, less nausea and vomiting may identify failing pregnancies.”
“Thus, less nausea and vomiting may identify failing pregnancies.”
Scientists are also unsure about whether there’s an evolutionary reason for morning sickness to carry protective benefits. It’s possible, many have theorized, that nausea is a way of keeping a pregnant woman from doing (or eating) things that might harm her fetus. “First, symptoms may be part of an evolutionary advantage to change one’s dietary intake, increase consumption of carbohydrate-rich foods, or avert intake of potentially teratogenic substances,” the NIH researchers wrote, referring to drugs or other agents that can cause birth defects. But since their model accounted for smoking and drinking alcohol, it seems “the mechanism is likely not through avoidance of such substances.”
The NIH findings should be reassuring to women enduring morning sickness (which, as any pregnant woman can tell you, also happens at night, and in the afternoon, and sometimes around the clock)—but sickness isn’t a guarantee of a viable pregnancy.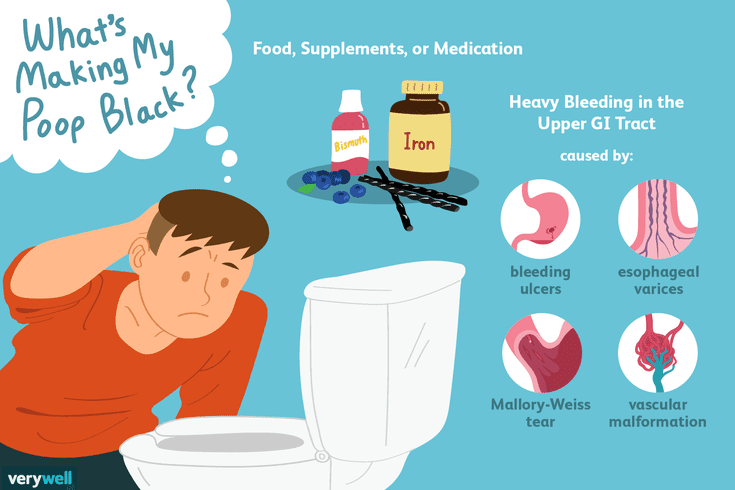 Some women who experience nausea and vomiting will still go on to have miscarriages or stillbirths. Similarly, Hinkle told me, an absence of symptoms isn’t automatically cause for concern.
Some women who experience nausea and vomiting will still go on to have miscarriages or stillbirths. Similarly, Hinkle told me, an absence of symptoms isn’t automatically cause for concern.
“Not all pregnancies are the same and every individual is different,” she said, “So just because they do not have symptoms does not mean that they will go on to have a loss.”
Eating disorders during pregnancy
Pregnancy becomes a real challenge for women with eating disorders. Indeed, on one side of the scale is the desire to give birth to a healthy child, and on the other, the desire to remain beautiful and slim with an abundance of advertising for tempting dishes and round-the-clock food delivery.
Doctors confirm the fact that eating disorders in pregnant women are common, but the frequency of these diseases has not yet been established. It's no secret that proper balanced nutrition during pregnancy is one of the main aspects for the successful birth of a healthy baby. And significant weight deviations from the norm can cause irreparable harm to both the health of the mother and the child. Eating disorders such as bulimia, anorexia and compulsive overeating are becoming more common every year. Experts are sounding the alarm, a little more and a real epidemic will begin.
And significant weight deviations from the norm can cause irreparable harm to both the health of the mother and the child. Eating disorders such as bulimia, anorexia and compulsive overeating are becoming more common every year. Experts are sounding the alarm, a little more and a real epidemic will begin.
Pregnancy and bulimia
The expectant mother's body has special requirements, it just needs proper nutrition during pregnancy and peace of mind.
During pregnancy, inducing vomiting means depriving the child of essential vitamins and minerals, which can subsequently affect the development of the baby. Bulimia during pregnancy is especially dangerous. There are cases when induced vomiting brought such harm to the body of a pregnant woman that doctors had to fight for the life of the mother and child.
Bulimia and pregnancy is a threat of miscarriage and a health risk for both the expectant mother and the baby. Vomiting at an early stage can provoke a miscarriage, at a later stage it is fraught with premature birth and all sorts of complications and pathologies of the fetus.
Anorexia and pregnancy
An anorexic girl with a big belly - in the understanding of the majority, this is simply incompatible. Indeed, the cult of a thin body with a lack of body weight often leads to infertility, and the fear of gaining excess weight during pregnancy drives expectant mothers to despair. However, some emaciated women still manage to get into an "interesting position." In the practice of a general practitioner, nutritionist at the Family Clinic "Maternity Hospital on Furshtatskaya" (Maternity Hospital No. 2), Irina Stanislavovna Andreeva, there were pregnant women with eating disorders. As a rule, these clients adhered to strict diets, were fond of vegetarianism or a raw food diet. According to Irina Stanislavovna, the thinness of a pregnant woman can adversely affect the course of pregnancy if weight gain is less than 200 grams per week.
And yet, despite the exhortation of experts that weight gain during pregnancy is a natural and logical process, women continue to restrict food, and therefore harm themselves and the child. The already depleted body of a pregnant woman with anorexia receives a colossal load, because all the forces go to the development of the unborn baby.
The already depleted body of a pregnant woman with anorexia receives a colossal load, because all the forces go to the development of the unborn baby.
Overeating during pregnancy
Not only is underweight during pregnancy bad. If a woman gained a lot of weight during pregnancy, this is also a bad indicator. In any case, overeating is bad for the health of the body as a whole. Often, the understanding that eating disorders can harm the baby motivates a woman to normalize nutrition and follow the instructions of doctors. However, there are cases when women during pregnancy did not give up their "bad habits" - overeating, inducing vomiting or starving themselves.
“Every woman wants the best for her child. Understanding perfectly well that for the growth and development of the baby, a complete and balanced diet with an increase in protein products of animal origin is necessary, the expectant mother may experience an intuitive revision of her usual diet. Those. during pregnancy, even with eating disorders, a woman may experience a so-called remission of the disease - a period in which the manifestations of a chronic illness disappear, but the disease itself remains. Unfortunately, after childbirth, eating disorders can again declare themselves in full voice. A relapse of the disease can be triggered by postpartum depression (present in varying degrees), and changes in relationships within the family (for example, with a husband), and elementary fatigue (sleep disturbance). - explains Andreeva Irina Stanislavovna.
Unfortunately, after childbirth, eating disorders can again declare themselves in full voice. A relapse of the disease can be triggered by postpartum depression (present in varying degrees), and changes in relationships within the family (for example, with a husband), and elementary fatigue (sleep disturbance). - explains Andreeva Irina Stanislavovna.
Anna Vladimirovna Nazarenko, head of the Clinic for Eating Disorders, comments: “Most of the women who sought help at the Clinic for Eating Disorders experienced remission of food addictions during pregnancy. A woman, wanting not to harm her child, adheres to the diet and diet prescribed by doctors. But, as a rule, after pregnancy, a woman experiences a breakdown against the background of a characteristic mental restructuring of consciousness and hormonal changes.
The birth of a child is always a great test for the whole family, and to a greater extent for the mother of a newborn. “For a successful pregnancy, a woman must take care of her nutrition. If you are planning a pregnancy and you have symptoms of food addiction, contact a specialist. Do not endanger your life and your child. We can observe the negative effect of negligent attitude to nutrition during pregnancy very quickly in specific pathologies of both the woman and her baby.
If you are planning a pregnancy and you have symptoms of food addiction, contact a specialist. Do not endanger your life and your child. We can observe the negative effect of negligent attitude to nutrition during pregnancy very quickly in specific pathologies of both the woman and her baby.
In very famous medical clinics in St. Petersburg, doctors recommend that women get pregnant to get rid of food addictions. Thus, they underestimate the seriousness of these diseases. Such medical negligence and ignorance of the specifics of eating disorders are horrific: in America, the problem of food addiction is put in third place after alcoholism and drug addiction. And in most Russian medical institutions, eating disorders continue to be interpreted as a consequence or concomitant factor of depression, promiscuity and lack of will.
In our Clinic, we have not encountered the fact that a woman would get rid of food addiction due to pregnancy, at most a remission could occur.
It is encouraging that many women with eating disorders come to us at a time when they are just starting to plan a pregnancy. This is a very correct and conscious approach to motherhood,” says Anna Vladimirovna Nazarenko.
This is a very correct and conscious approach to motherhood,” says Anna Vladimirovna Nazarenko.
Irina Stanislavovna Andreeva, nutritionist at Maternity Hospital No. 2, warns expectant mothers: “A pregnant woman's body has a natural need for a balanced intake of nutrients. The lack of protein, vitamins, macro- and micronutrients with nutrition increases the risk of spontaneous miscarriage in the early stages, intrauterine growth retardation, impaired placental circulation, and premature birth. It can also cause a formidable complication of the second half of pregnancy - gestosis - extremely dangerous for health, and sometimes for life, both for the mother and the child. To date, it has been proven that the trigger for this negative process is an excess of simple, quickly digestible carbohydrates in a woman's diet already in the very early stages of pregnancy.
In addition, a well-balanced diet during pregnancy is very important. Anna Vladimirovna Nazarenko and Irina Stanislavovna Andreeva share the opinion that strict diets, vegetarianism and other nutrition systems that limit or completely exclude proteins, fats or carbohydrates can cause significant harm to an unborn baby. For the formation of the musculoskeletal system and the immune system, animal proteins (meat, fish, eggs and dairy products) are needed, vegetable proteins will not replace elements important for the development of the child. No need to eat "for two". Doctors recommend frequent fractional meals, a variety of foods, and also reduce fast carbohydrates (sweets, starchy foods). The main thing is to listen to your body, it will tell you what it needs at the moment. Keep calm and inner harmony, happy motherhood to you.
For the formation of the musculoskeletal system and the immune system, animal proteins (meat, fish, eggs and dairy products) are needed, vegetable proteins will not replace elements important for the development of the child. No need to eat "for two". Doctors recommend frequent fractional meals, a variety of foods, and also reduce fast carbohydrates (sweets, starchy foods). The main thing is to listen to your body, it will tell you what it needs at the moment. Keep calm and inner harmony, happy motherhood to you.
Other articles
Pregnancy and childbirth after 35
The desire to fulfill the dream of motherhood will be as long as the world exists. A woman of the 21st century stands on the same level as a man in achieving career growth. It is only after reaching full perfection in the business sphere that most couples think about having a baby.
Childbirth after IVF (in vitro fertilization)
Currently, infertility is one of the most urgent and significant problems in modern obstetrics and gynecology. There is a continuous increase in the frequency of infertility, especially in developed countries, which is due to the influence of environmental factors on the generative function; unhealthy lifestyle due to bad habits; late age of marriage and postponing the birth of a child to a later date; an increase in the frequency of endocrine pathology and inflammatory diseases of the female genital organs; high migration of the population, which negatively affects the generative function of both men and women.
There is a continuous increase in the frequency of infertility, especially in developed countries, which is due to the influence of environmental factors on the generative function; unhealthy lifestyle due to bad habits; late age of marriage and postponing the birth of a child to a later date; an increase in the frequency of endocrine pathology and inflammatory diseases of the female genital organs; high migration of the population, which negatively affects the generative function of both men and women.
Anesthesia Pros and Cons
Childbirth is a natural, natural process. For a woman giving birth, this is not only the expectation of a miracle and happiness, but also serious hard work. It has been proven that pain triggers pathological processes in the human body, and we should try to minimize pain during childbirth.
Nausea and vomiting of pregnant women: the view of an anesthesiologist-resuscitator
Despite the fact that nausea and vomiting are very common during pregnancy, the questions of their etiology and pathogenesis still remain open. Head of the Department of Anesthesiology and Resuscitation of the Krasnoyarsk Regional Clinical Center for Maternal and Childhood Protection, Assistant of the Department of Anesthesiology and Resuscitation, IPO KrasSMU named after. Professor V. F. Voyno-Yasenetsky Yuri Raspopin analyzed the literature over the past 10 years in order to study the current state of the problem and determine further research prospects.
Head of the Department of Anesthesiology and Resuscitation of the Krasnoyarsk Regional Clinical Center for Maternal and Childhood Protection, Assistant of the Department of Anesthesiology and Resuscitation, IPO KrasSMU named after. Professor V. F. Voyno-Yasenetsky Yuri Raspopin analyzed the literature over the past 10 years in order to study the current state of the problem and determine further research prospects.
Clinical picture
Nausea and vomiting are the most common symptoms of advanced pregnancy: up to 80% of women experience them. As a rule, they appear on the 4th week of pregnancy and disappear on their own at the 12-14th week. However, about 20% of women continue to experience nausea and vomiting throughout the entire period.
Excessive vomiting of pregnancy is characterized by severe nausea, uncontrollable vomiting that continues until the 22nd week of pregnancy, as defined by the 2016 WHO. As the most severe form, it occurs in 0.3–4% of women. It is one of the most common reasons for hospitalization in early pregnancy. Left untreated or failing, it can lead to maternal morbidity and poor neonatal outcomes.
As the most severe form, it occurs in 0.3–4% of women. It is one of the most common reasons for hospitalization in early pregnancy. Left untreated or failing, it can lead to maternal morbidity and poor neonatal outcomes.
A large population-based cohort study in Sweden over 12 years (1997–2009) of more than 1 million women with excessive pregnancy vomiting found that admission in the 2nd trimester more than doubled the risk of severe preeclampsia, 3 times the risk of placental abruption and 39% the risk of having a fetus with extremely low body weight.
From an economic point of view, the cost of treating and maintaining women with nausea and vomiting of pregnancy is enormous. In 2012, in the United States, the treatment of one such patient cost $47,351, and the annual cost was about $1.7 billion. Of this, the direct cost of treatment takes 60%, the rest is indirect economic losses. And in Canada, for example, the treatment of one patient with nausea and vomiting of pregnancy is 653 Canadian dollars per week.
Currently, the world community is switching to ICD-11, which is distinguished by the degree of sophistication. The concept of excessive vomiting of pregnant women is spelled out in it along with mild vomiting of pregnant women, vomiting of pregnant women with metabolic disorders.
In terms of recommendations, we were able to find 3 documents on this issue at the international level: the American Society of Obstetricians and Gynecologists for 2018, the Royal College of Obstetricians and Gynecologists of Great Britain and the Society of Obstetricians and Gynecologists of Canada for 2016.
Risk factors:
- history of nausea and vomiting;
- the presence of nausea and vomiting in close relatives;
- young women under 20;
- nulliparous;
- multiple pregnancy;
- taking oral contraceptives;
- history of miscarriage;
- motion sickness, migraine;
- ethnic etc.

Severity score
A modified PUQE (Pregnancy-Unique Quantification of Emesis and Nausea) scale is used. Patients are asked 3 questions:
Concept difference
There is a fine line between pregnancy nausea and vomiting and excessive pregnancy vomiting.
Diagnosis
It must be remembered that nausea and vomiting of pregnant women can be both primary and secondary conditions against the background of severe somatic pathology, including hepatitis, pancreatitis, pancreatic necrosis, pyelonephritis, migraine, diabetic ketoacidosis and others.
First of all, it is necessary to carefully collect an anamnesis, which is the cornerstone in the diagnosis of this condition. Laboratory and instrumental diagnostics are also helpful. For example, nausea and vomiting of pregnant women is characterized by an increase in liver enzymes up to 300 U / l, as well as bilirubin - up to 40 mg / l. In hepatitis, for comparison, the first indicator increases several thousand times, and the second - more than 40 mg / l.
In hepatitis, for comparison, the first indicator increases several thousand times, and the second - more than 40 mg / l.
Screening for ketonuria is now the gold standard in all guidelines. It is often used as an aid in diagnosis, fluid therapy, or admission/discharge decisions for patients. With ketosis as a condition that develops against the background of carbohydrate starvation of cells, fat begins to break down with the formation of a large number of ketone bodies. Accordingly, this is one of the adaptive reactions of the body to the absence of carbohydrates in food, it acts as a certain measure of starvation. Increased metabolic demands during pregnancy, even in the absence of vomiting or poor oral nutrition, are a predisposing factor in the development of ketonuria.
It should be remembered that nausea and vomiting of pregnancy is characterized by the first appearance before 9 weeks. After that, it is necessary to carry out a differential diagnosis, with which this condition may be associated.
Etiology and pathogenesis
There are several theories of nausea and vomiting of pregnancy, including excessive vomiting. This suggests that this problem has not been fully studied.
The hormonal theory is related to several hormones:
- HCG . This is the time factor. As a rule, the peak of symptoms of nausea and vomiting of pregnant women is observed against the background of an increase in hCG. They also increase in conditions such as multiple pregnancy or female pregnancy, since in such cases the level of hCG is elevated. However, the failure of some studies to show an association between nausea and vomiting and hCG levels may be due to the different biological activity of different isoforms of this hormone.
- Estrogen . It is also a temporary factor. There are studies that show that nausea and vomiting of pregnancy is common with an increase in estrogen levels, and less often with a decrease.

- Progesterone . Alone or in combination with estrogen at elevated levels, it can cause stomach arrhythmias, resulting in increased nausea and vomiting.
More attention is currently being paid to the hormone GDF15, which, like hCG, is produced by the placenta. Its level increases in early pregnancy when symptoms of nausea and vomiting occur. However, several recent studies point to the leading role of GDF15, rather than hCG, in the development of excessive vomiting during pregnancy. It is this hormone that plays a leading role in appetite control and is associated with the development of cachexia in cancer patients by activating the ICFBP17 gene, which is symptomatically similar to excessive vomiting of pregnant women (weight loss, muscle atrophy).
Another theory is related to serotonin receptors located in the vagus afferent neurons of the gastrointestinal tract and the vomiting center in the brain. It has been proposed because, like progesterone and the hormone GDF15, they play a role in altering GI motility.
The genetic theory is based on a 2016 population cohort study of 1,723 female twins. Genetic predisposition was confirmed in 73%. In 53%, excessive vomiting of pregnant women was observed. And 28% of women reported that their mothers had it, at 19% of cases are in twin sisters.
It is important to pay attention to another theory. She suggests that nausea and vomiting of pregnancy is an evolutionary adaptation to potentially dangerous foods, which is a protective reaction.
Therapy
Mild (≤6 PUQE)
Non-drug therapy with lifestyle and diet changes. It involves frequent small meals, a high protein and carbohydrate diet, avoiding spicy foods, etc.
Further treatment is based on ruling out other causes of nausea and vomiting. At each stage, it is necessary to remember the importance of enteral nutrition, and in case of dehydration, the replacement infusion therapy.
Remember the importance of prevention. There are several studies that have shown that women who took multivitamins during fertilization were less likely to need medical attention and hospitalization if they developed vomiting during pregnancy. The authors suggest that this may have been due to increased levels of vitamin B6. Therefore, there is a standard recommendation: start taking prenatal vitamins a month before pregnancy.
There are several studies that have shown that women who took multivitamins during fertilization were less likely to need medical attention and hospitalization if they developed vomiting during pregnancy. The authors suggest that this may have been due to increased levels of vitamin B6. Therefore, there is a standard recommendation: start taking prenatal vitamins a month before pregnancy.
Rest and restriction of various external irritants (odors, humidity, noise and others) will help relieve the initial signs of nausea and vomiting.
Recommendations include taking ginger-based preparations (250 mg capsules 4 times a day). You should also consider electrical stimulation, acupressure, acupuncture point P6, which is located on the back of the hand near the wrist. Most studies report the benefits of this stimulation. But there are significant methodological shortcomings. For example, the last 2 large studies have shown no benefit over sham stimulation.
Moderate (PUQE 7-12)
First-line drugs are pyridoxine or its combination with doxylamine. A number of studies have shown the effectiveness of this combination in the treatment of varying degrees of severity of nausea and vomiting during pregnancy. They act on the vestibular pathway of nausea and vomiting by blocking the connection of histamine receptors in the vomiting center with the chemoreceptor trigger zone. Cases of harmful effects on the fetus are not described. However, caution should be exercised when using several antiemetics at the same time, as this may lead to an increased risk of extrapyramidal disorders.
A number of studies have shown the effectiveness of this combination in the treatment of varying degrees of severity of nausea and vomiting during pregnancy. They act on the vestibular pathway of nausea and vomiting by blocking the connection of histamine receptors in the vomiting center with the chemoreceptor trigger zone. Cases of harmful effects on the fetus are not described. However, caution should be exercised when using several antiemetics at the same time, as this may lead to an increased risk of extrapyramidal disorders.
Diphenhydramine and metoclopramide and ondansetron are recommended as second line.
Severe (13 or more points on the PUQE scale)
Initial treatment includes rehydration, elimination of electrolyte deficiency. In this case, replacement infusion therapy of balanced solutions with the inclusion of thiamine 100 mg daily for 2-3 days is carried out, followed by the introduction of multivitamins.