Miscarriage in the first week
Early Pregnancy Loss - familydoctor.org
What is early pregnancy loss?
An early pregnancy loss is known as a miscarriage. This represents any pregnancy that ends on its own in the first 20 weeks of gestation. Experts estimate that 10% to 20% of known pregnancies end in miscarriage. There are several classifications of miscarriage:
- Complete – when the embryo and surrounding tissues have emptied out of the uterus. It typically involves cramping and bleeding. These resolve quickly, usually in a few days to a week.
- Incomplete or inevitable – when the cervix opens, and some tissue is expelled (released). The embryo or tissue may not completely leave the uterus. This can cause continued pain and bleeding.
- Missed – when the embryo has died, but it stays in the uterus. You may have no idea that it has happened. It is often discovered when pregnancy symptoms stop, or an ultrasound shows no heartbeat.
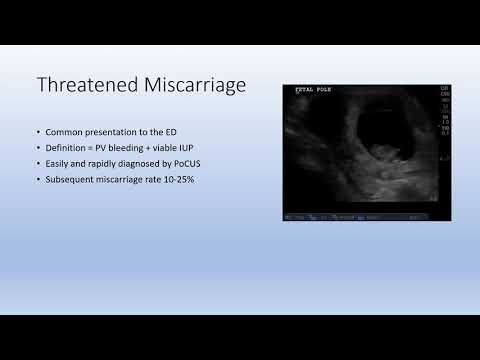
- Threatened – when you experience some bleeding and cramping, but the cervix remains closed. A miscarriage may or may not happen.
- Recurrent –when you have 3 or more miscarriages in your first trimester.
Other problems can also result in an early pregnancy loss:
- Chemical pregnancy – This is a very early miscarriage. It usually happens in the first few weeks after conception. Chromosomal abnormalities keep the embryo from developing normally. The tissue is passed from your uterus around the same time that you normally have your period. Many women don’t even know they are pregnant when they have a miscarriage from a chemical pregnancy.
- Blighted ovum –This is also called an embryonic pregnancy. It happens when the fertilized egg implants in the wall of the uterus, but a fetus never develops.
- Ectopic pregnancy –This is when the fertilized egg implants somewhere other than the uterus.
 Often, it implants in the fallopian tube. This can cause serious problems for the mother. Treatment — usually surgery — is needed right away to remove the tissue. This is never a viable pregnancy.
Often, it implants in the fallopian tube. This can cause serious problems for the mother. Treatment — usually surgery — is needed right away to remove the tissue. This is never a viable pregnancy. - Molar pregnancy –This is a rare problem that starts with a genetic error during fertilization. This causes abnormal tissue to grow instead of an embryo. It is not a viable pregnancy. But it still causes regular pregnancy symptoms. These include a missed period, positive pregnancy test, and nausea.
Symptoms of early pregnancy loss
The most common symptoms of miscarriage are bleeding and cramping. But they don’t necessarily mean you’re having a miscarriage. Up to one-third of pregnancies come with some bleeding early on. About half of those result in normal pregnancies. If you have any bleeding or cramping in your first trimester, call your doctor.
There are other common signs that indicate you may be having a miscarriage. If you experience any of these symptoms, call your doctor right away:
- Mild to severe back pain (worse than menstrual cramps)
- Weight loss
- White-pink mucus discharge from the vagina
- Contractions (painful, happening every 5 to 20 minutes)
- Tissue that looks like a clot passing from the vagina
- Sudden decrease in signs of pregnancy
What causes early pregnancy loss?
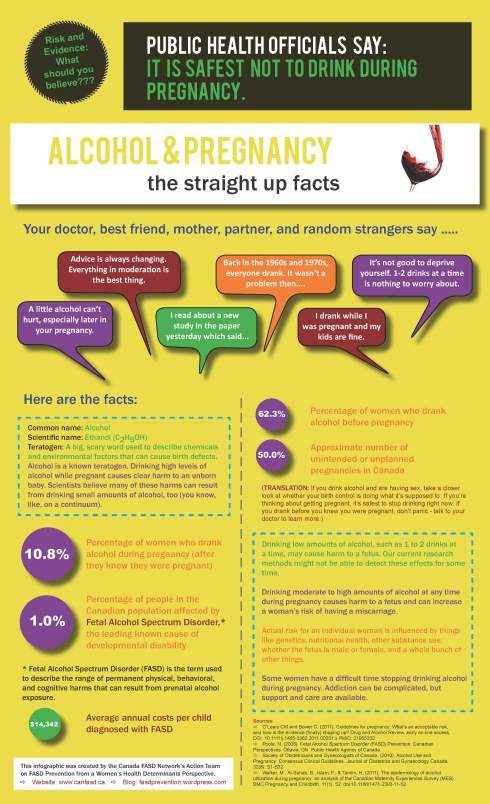
In some cases, the cause of your pregnancy loss is unknown.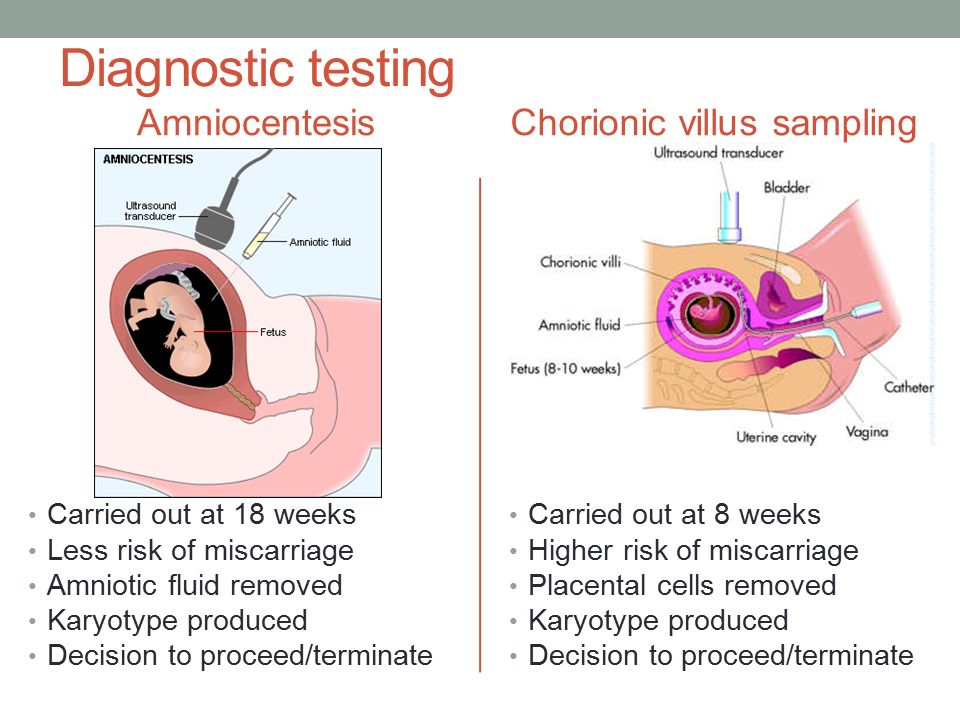 Often, it is a random problem with chromosomes that happens at conception. You might be afraid that you did something that caused your miscarriage. But things like working, exercising, having sex, or morning sickness do not cause miscarriage. Any kind of fall or blow is rarely to blame. The research on the effects of alcohol, tobacco, and caffeine is unclear. So, there is nothing you could have done to prevent it. It is not the result of anything you did or didn’t do. You should never blame yourself for a miscarriage.
Often, it is a random problem with chromosomes that happens at conception. You might be afraid that you did something that caused your miscarriage. But things like working, exercising, having sex, or morning sickness do not cause miscarriage. Any kind of fall or blow is rarely to blame. The research on the effects of alcohol, tobacco, and caffeine is unclear. So, there is nothing you could have done to prevent it. It is not the result of anything you did or didn’t do. You should never blame yourself for a miscarriage.
How is early pregnancy loss diagnosed?
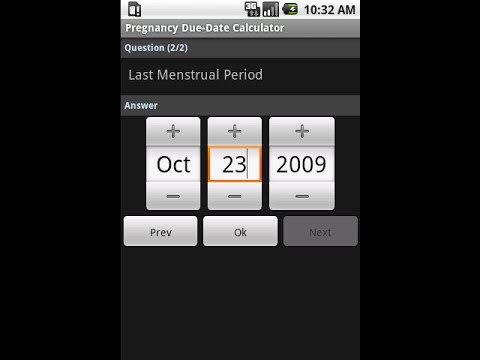
Your doctor will start by asking you questions about your symptoms and when they started. They will do a physical exam. Your doctor might do an ultrasound. This can reveal if the embryo is still growing, and it can check for a heartbeat. They may also order blood tests. These can measure pregnancy hormone levels. This can give your doctor an idea if you are losing the pregnancy.
Can early pregnancy loss be prevented or avoided?
There is no conclusive research that says there is anything you can do to prevent a miscarriage. You didn’t cause it, so you couldn’t have prevented it.
You didn’t cause it, so you couldn’t have prevented it.
Risk factors
Patients who are pregnant and who have had a miscarriage are at greater risk of having another one. Your risk also increases as you get older. You are at highest risk when you are age 35 or older. Some medical conditions also increase your risk. These include:
- Diabetes.
- Thyroid disease.
- Polycystic ovary syndrome.
- Problems with the immune system.
Even if you have one of these conditions, you can’t do anything to avoid having a miscarriage. Many patients who are pregnant and have these health conditions have healthy pregnancies.
Early pregnancy loss treatment
There are two main types of treatment for miscarriage: non-surgical and surgical.
Non-surgical
In many cases, your body passes all of the pregnancy tissue naturally. This could take a few days up to a few weeks. No treatment is needed. If it is taking a long time, your doctor can give you medicine that can help pass the tissue.
The process of passing the tissue can involve heavy bleeding, cramping pain, diarrhea, and nausea. Your doctor may give you pain medicine to help ease your symptoms. If you are in your first trimester, the tissue will be small. It will look like a blood clot. It will not look like a baby.
Your doctor may do an ultrasound or blood tests after you are finished with the miscarriage. This will confirm that the miscarriage is complete, and no tissue remains.
Surgical
Surgical treatment is usually done if there are complications with your miscarriage.
Complications could include:
- An infection
- Heavy bleeding
- Any condition that keeps pregnancy tissue inside your uterus
Common surgical treatments include:
- Vacuum aspiration.In this procedure, a thin tube is inserted into your uterus. It is connected to a suction device. The pregnancy tissue is suctioned out of your body. The procedure is done under local anesthesia.
 Your doctor can perform it in his or her office.
Your doctor can perform it in his or her office. - Dilation and curettage (D&C).This procedure opens the cervix and uses an instrument to remove the pregnancy tissue. It is usually done under regional or general anesthesia. Your doctor will perform it in a hospital or surgery center.
After treatment, your doctor may recommend you not put anything into your vagina for a few weeks. This includes using tampons and having sex. This helps prevent infection. Signs of infection include:
- Heavy bleeding
- Fever
- Chills
- Severe pain
Call your doctor right away if you have any of these symptoms.
Living with early pregnancy loss
Everyone handles loss differently. Some patients who are pregnant may have trouble coping with the feelings that can go along with miscarriage. If you are very upset or feel like you need help, there are resources available. Talk to your doctor. They may be able to refer you to a local support group. There are also national resources you can access, such as SHARE: Pregnancy and Infant Loss Support. It lists local support groups and offers online resources that could help you.
There are also national resources you can access, such as SHARE: Pregnancy and Infant Loss Support. It lists local support groups and offers online resources that could help you.
Questions to ask your doctor
- I’m having symptoms of miscarriage. What are the chances that I will miscarry?
- How will I know what caused my early pregnancy loss?
- Is there an advantage to letting the tissue pass naturally over having a D&C?
- Will a miscarriage affect my ability to get pregnant again?
- How long should I wait after an early pregnancy loss to try to get pregnant again?
Resources
National Institutes of Health, MedlinePlus: Miscarriage
National Institute of Child Health and Human Development: Pregnancy Loss
SHARE: Pregnancy and Infant Loss Support
Miscarriage | NHS inform
A miscarriage is the loss of your baby before 24 weeks. Early miscarriages happen in the first 12 weeks of pregnancy. Late miscarriages happen between 12 and 24 weeks.
Late miscarriages happen between 12 and 24 weeks.
Most of the time there’s no clear reason why it happens, but it’s very unlikely to be caused by anything you did or didn’t do.
About 1 out of 5 pregnancies miscarry. Since many miscarriages aren't recorded the figure might be higher.
What causes a miscarriage?
Doctors think most miscarriages are caused when the building blocks controlling the development of a baby (the chromosomes) aren’t right. Babies with too many or not enough chromosomes won't develop properly. This leads to a miscarriage.
Miscarriages can also be caused by:
- issues with your placenta
- cervical weakness - when your cervix (neck of your womb) starts to open
Early miscarriages
An early miscarriage happens in the first 12 weeks of pregnancy. Most women who miscarry do so in the first 12 weeks of their pregnancy.
Many women have a miscarriage before they even know they’re pregnant. If this happens it can feel like a late period with heavy bleeding.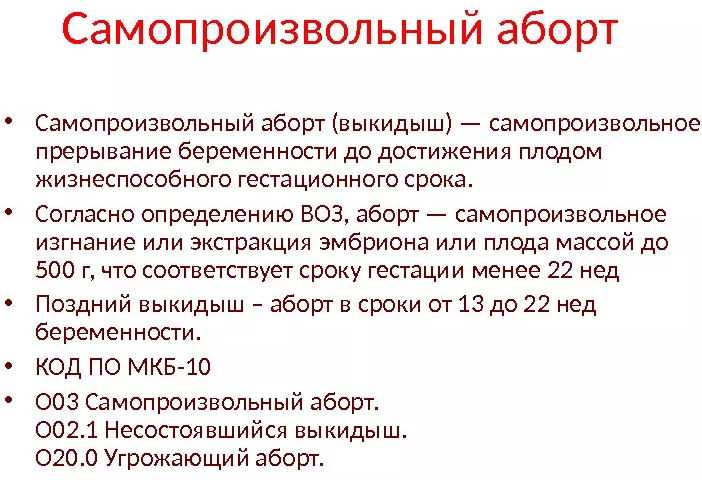
Symptoms of an early miscarriage
You might be having an early miscarriage if:
- you're bleeding from your vagina
- you've cramps in your lower abdomen – these can feel like bad period pains
- there's fluid or tissue coming from your vagina
- your breasts are no longer tender and any morning sickness has passed
Bleeding
Having some light bleeding's fairly common in the first 12 weeks of pregnancy and doesn't necessarily mean you're having a miscarriage.
If you start bleeding, you should always contact your GP or midwife and get advice about what to do.
What happens during an early miscarriage
If you’re in the early weeks of pregnancy:
- you’ll probably be asked to go to the early pregnancy unit at your local hospital straight away
- you’ll have some tests and usually an ultrasound scan
- your body usually completes the miscarriage naturally
Depending on your stage of pregnancy, you may deliver a small baby. That can be a shock and is an understandably upsetting time.
That can be a shock and is an understandably upsetting time.
Late miscarriages
A late miscarriage happens after 12 weeks and before 24 weeks.
For many parents who lose their baby after a late miscarriage, the word ‘miscarriage’ doesn't properly express the impact of their loss. The loss of a baby at any time's a terrible shock and a late miscarriage can be especially hard.
Symptoms of a late miscarriage
You might be having a late miscarriage if:
- you're bleeding from your vagina – this can be heavy and you might have blood clots
- you've strong, cramping pains
Always get medical help if:
- you're bleeding
- your baby’s movements have changed or you haven’t felt any movements for a while.
- your waters break and your baby's born very quickly
Contact your midwife or local maternity unit if you’re registered with them. If you’re not registered, contact your GP or phone the NHS 24 111 service.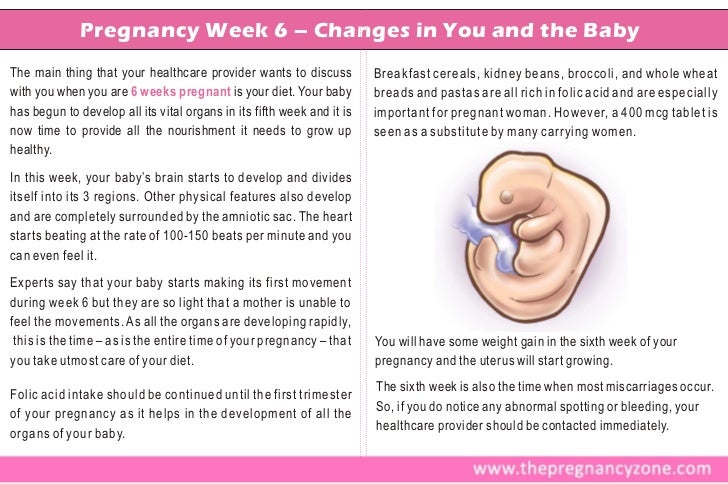
What happens during a late miscarriage
If you’re later on in pregnancy:
- you may be asked to go to the maternity ward
- you’ll have some tests and usually an ultrasound scan
- you're likely to go through labour in hospital and might have your labour induced
While you deliver your baby you're likely to have heavier bleeding and labour-like pains.
Making difficult decisions
If you're having a miscarriage, your doctor or midwife will:
- talk to you about what will happen next
- help you, and your partner if you have one, decide what you’d like to do
You may have many difficult decisions to make at this time and will have overwhelming emotions. Take your time. Your midwife or doctor can help, and there are many organisations that can support you, your baby’s father and your family.
Get support from SANDS
Get support from SiMBA
After a miscarriage
Depending on your circumstances and stage of pregnancy, your midwife or doctor may ask if you'd like to see or hold your baby.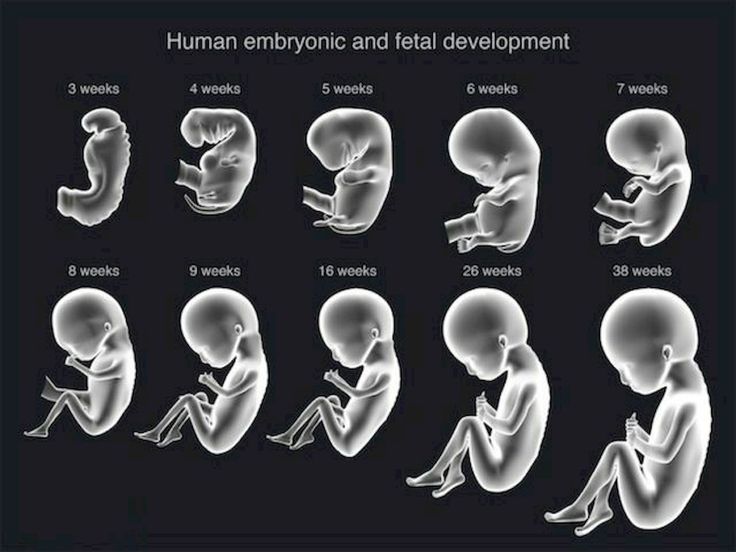
Some parents decide they don't want to see their baby, and others choose not to for faith or cultural reasons. This is a decision only you can make. It can be very hard when you're feeling overwhelmed. Whatever you decide is okay.
If you’re worried about what your baby looks like, your midwife or doctor can describe them to help you decide.
If your symptoms continue
You’ll probably have some bleeding for a week or two. If you continue to have symptoms after your miscarriage, it may mean that some of the pregnancy tissue's still in your womb.
Some women may need medicine or a short operation to treat this.
If you’re worried about seeking treatment, maybe a friend can come with you. Having support's really important at this difficult time.
Taking time off work
Many women will want to take time off work after having a miscarriage.
If you have a miscarriage before the end of the 24th week, you’re entitled to:
- take sick leave
- any sick pay you'd normally qualify for
If you lose your baby after the end of the 24th week, you’re entitled to:
- take maternity leave
- any maternity pay you qualify for
Speak to your employer about which choices may be right for you and your family.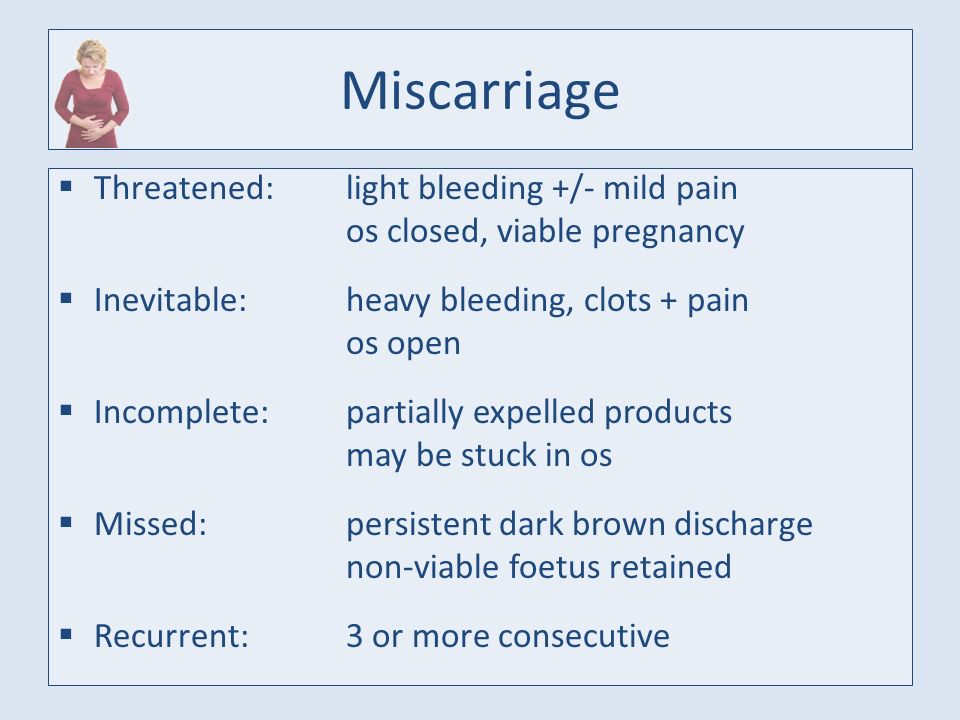
Working Families has more about your rights at work after a miscarriage
Repeated miscarriages
Most women go on to have a successful pregnancy and a healthy baby after a miscarriage. But unfortunately, some women have repeated miscarriages.
If you've had:
- 1 or 2 miscarriages - you're not more likely than anyone else to have another one
- 3 or more miscarriages - your GP can refer you to a specialist to see whether there’s a specific cause
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
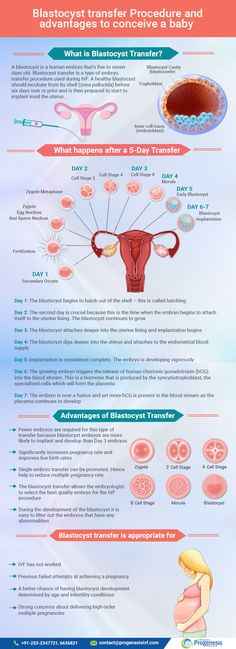
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage:
- the expectant mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies;
- maintenance by the future mother of a life far from a healthy lifestyle. May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
- obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage;
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.

The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs:
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.
All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy.
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future. Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Gynecologists of the corresponding department of our private clinic in Ryazan will help you find out what could have caused the miscarriage, as well as make recommendations on how to prepare for pregnancy. They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped!
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- Documentation
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, injury, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this.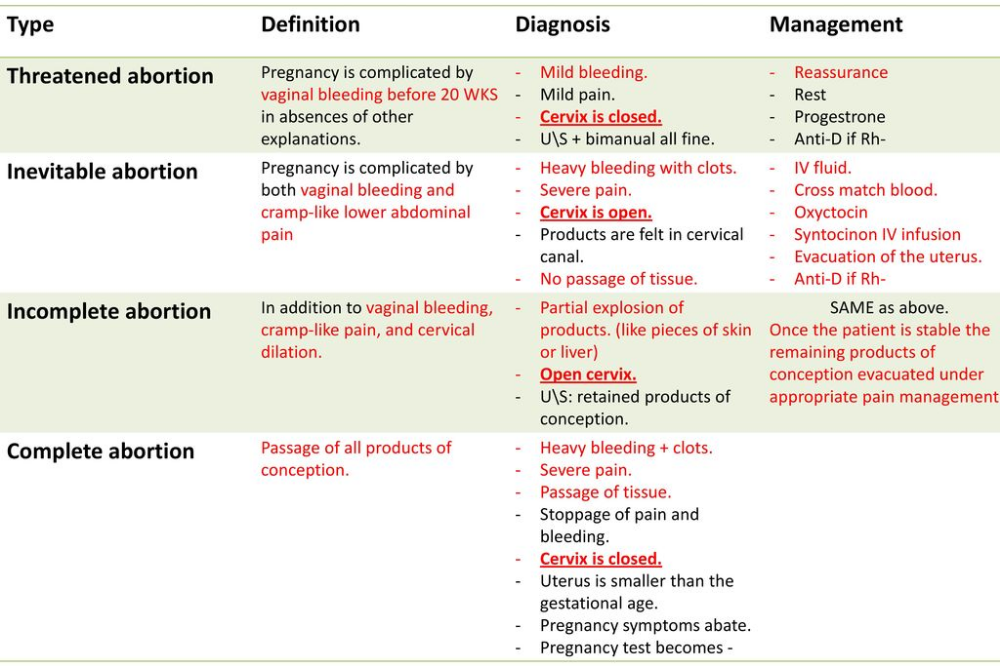 However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Hormone imbalance in a woman's body is likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogens and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.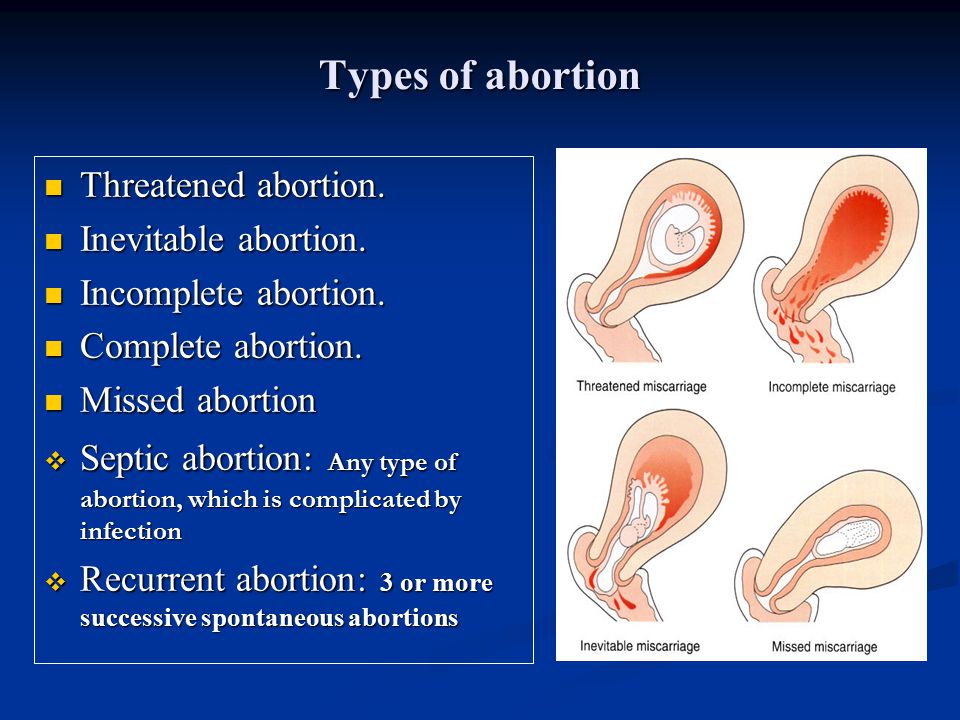
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 o C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - a mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.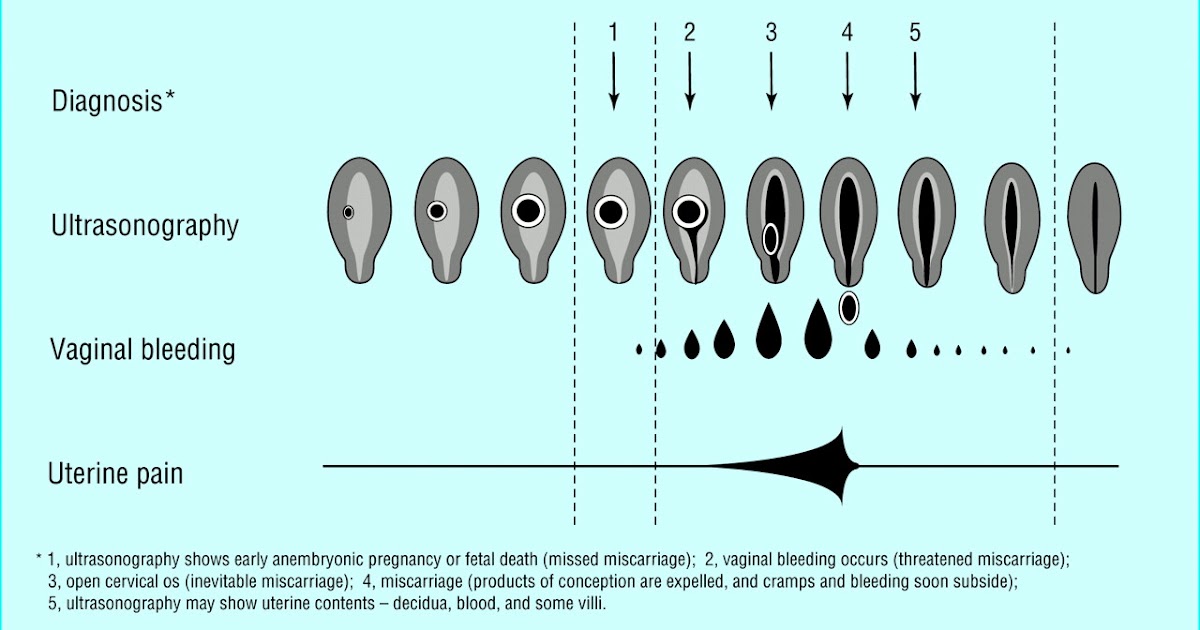
Miscarriage due to impaired hemostasis
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Disorders of the blood coagulation system leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (a tendency to bleed). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can manifest themselves even in childhood in the form of increased bleeding during cuts, extractions of teeth, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of a blood clotting disorder.