What if you drank alcohol early in pregnancy
Drinking alcohol while pregnant - NHS
Experts are still unsure exactly how much – if any – alcohol is completely safe for you to have while you're pregnant, so the safest approach is not to drink at all while you're expecting.
Is it safe to drink alcohol when pregnant?
The Chief Medical Officers for the UK recommend that if you're pregnant or planning to become pregnant, the safest approach is not to drink alcohol at all to keep risks to your baby to a minimum.
Drinking in pregnancy can lead to long-term harm to the baby, with the more you drink, the greater the risk.
How does alcohol affect my unborn baby?
When you drink, alcohol passes from your blood through the placenta to your baby.
A baby's liver is one of the last organs to develop and does not mature until the later stages of pregnancy.
Your baby cannot process alcohol well, and exposure to alcohol can seriously affect their development.
Drinking alcohol during pregnancy increases the risk of miscarriage, premature birth and your baby having a low birthweight. It can also affect your baby after they're born.
Drinking during pregnancy can cause your baby to develop a serious condition called foetal alcohol spectrum disorder (FASD).
FASD can cause problems with:
- learning and behaviour
- joints, bones, muscles and some organs
- managing emotions and developing social skills
- hyperactivity and impulse control
- communication, such as problems with speech
The risk is likely to be greater the more you drink.
How to avoid alcohol in pregnancy
It may not be as difficult as you think to avoid alcohol completely during pregnancy, as many women go off the taste of alcohol early in pregnancy.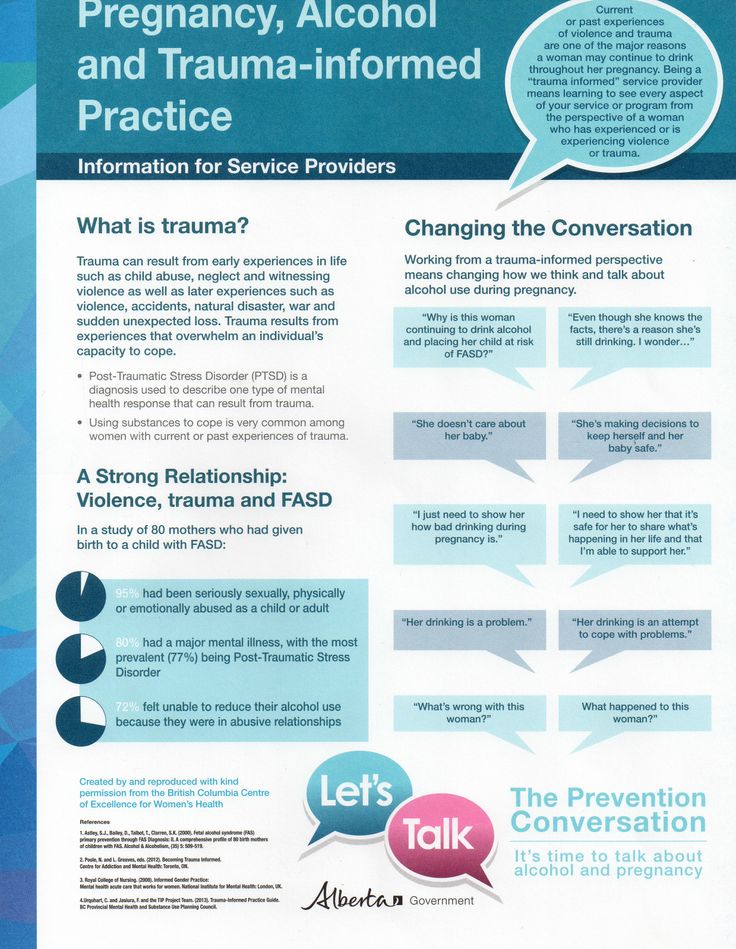
Most women do give up alcohol once they know they're pregnant or when they're planning to become pregnant.
Women who find out they're pregnant after already having drunk in early pregnancy should avoid further drinking.
However, they should not worry unnecessarily, as the risks of their baby being affected are likely to be low.
If you're concerned, talk to a midwife or doctor.
What is a unit of alcohol?
If you do decide to drink when you're pregnant, it's important to know how many units you are consuming.
One UK unit is 10 millilitres (ml) – or 8 grams – of pure alcohol. This is equal to:
- just under half a pint of cider (218ml) at 4.5% alcohol by volume (ABV: you can find this on the label)
- just under half a pint of beer (250ml) at 4% ABV
- a single measure of spirit (25ml), such as whisky, gin, rum or vodka, at 40% ABV
- just under half a standard glass of wine (76ml) at 13% ABV
You can find out how many units there are in different types and brands of drinks with the Drinkaware unit and calorie calculator.
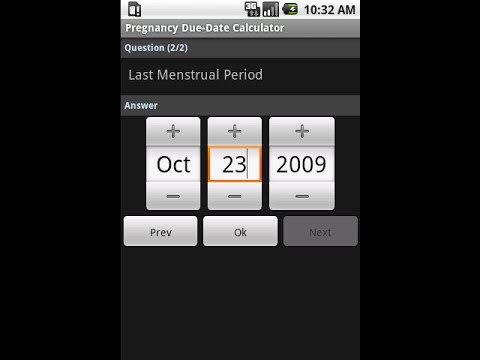
If you have an Android smartphone, iPhone, iPad or iPod touch, you can download the free One You Drinks Tracker from Google Play or the iTunes App Store. It allows you to keep a drinks diary and get feedback on your drinking.
Read more about alcohol units.
Alcohol support services
If you have difficulty cutting down what you drink, talk to a midwife, doctor or pharmacist.
Confidential help and support is also available from local counselling services:
- Drinkline – the national alcohol helpline; if you're worried about your own or someone else's drinking, call this free helpline on 0300 123 1110 (weekdays 9am to 8pm, weekends 11am to 4pm)
- We Are With You – a UK-wide treatment agency that helps individuals, families and communities manage the effects of alcohol and drug misuse
- Alcoholics Anonymous (AA) – a free self-help group; its "12-step" programme involves getting sober with the help of regular support groups
Find your nearest alcohol support services.
Read more advice on cutting down your drinking.
Find maternity services near you.
Page last reviewed: 29 January 2020
Next review due: 29 January 2023
Drinking Alcohol While Pregnant in First 3 Weeks: Is It Safe?
It happens. Perhaps you went off birth control a few months ago to try for a baby, but weren’t expecting to get pregnant so soon. You did cut back on alcohol to up your chances of conceiving, but you continued having a glass of wine here and there.
Or maybe you weren’t trying to get pregnant at all, and it came as a surprise when you realized that your period was over a week late. Now you’re looking at two pink lines on a home pregnancy test and freaking out about the night out with your girlfriends that you enjoyed a few days ago.
Maybe you’ve even known for a couple weeks that you’re pregnant, but you went ahead and toasted the bride and groom at a recent wedding because your friend told you small amounts of alcohol so early in pregnancy don’t do any harm.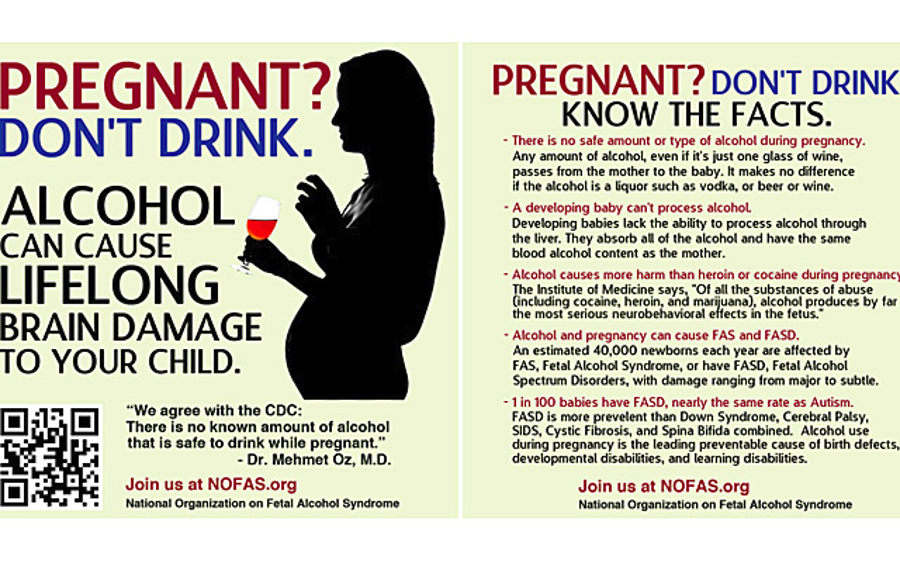
Whatever the case, you’re now worried and want to know what damage, if any, drinking in very early pregnancy can do.
First off, take a deep breath and let go of any guilt or shame that you feel about the past. You’re in a no-judgement zone here. Next, continue reading to learn what the side effects can be — and most importantly, what you can do to ensure good health for you and your baby moving forward.
At the very top of its alcohol and pregnancy information sheet — and in bold type, no less — the Centers for Disease Control and Prevention (CDC) advises that women who are trying to become pregnant or could be pregnant shouldn’t drink.
Why? It’s not really about the harm done by what you drink before you’re even pregnant (though this may affect your ability to conceive). It’s that no amount of alcohol at any point in pregnancy has been absolutely proven to be safe.
Since you can be pregnant without knowing it, the CDC is covering the possibility that you’re in the earliest stages of pregnancy — 3 or 4 weeks, often even before your missed period. (Many people don’t know they’re pregnant until they’re already 4 to 6 weeks.)
(Many people don’t know they’re pregnant until they’re already 4 to 6 weeks.)
Like the CDC in the United States, the NHS in the United Kingdom says that if you’re pregnant or planning to become pregnant, avoid alcohol.
Truly specific research around drinking alcohol in very early pregnancy is pretty tricky. That’s because it would be unethical to put together a study and actually request that any segment of the pregnant population do something (drink alcohol) known to cause harm even some of the time.
What we do have: research that looks at people who self-report alcohol use during pregnancy as well as some animal studies. We also have a lot of science backing our understanding of human development in the womb, including brain and central nervous system development starting at week 3 of pregnancy (right after implantation).
In one 2015 study done in mice, researchers gave the animals alcohol at 8 days gestation — roughly equivalent to the early fourth week in a human pregnancy. They found that the offspring of these mice had changes to their brain structure.
They found that the offspring of these mice had changes to their brain structure.
The results suggested that early alcohol exposure can alter DNA chemical processes. Embryonic stem cells that change as a result of the mother’s alcohol consumption early in pregnancy could even impact adult tissue later on.
To be a little Captain Obvious here, humans aren’t mice. There’s no way to know at this time if this effect happens in the same way in humans. It’s definitely worth further study, though.
On the other hand, a study published in 2013 looked at 5,628 women who self-reported various amounts of alcohol consumption during early pregnancy. (For the purposes of this study, though, “early” meant all the way up until 15 weeks.)
Researchers looked for common effects of alcohol on pregnancy:
- low birth weight
- high maternal blood pressure
- preeclampsia
- smaller-than-expected size for gestational age
- pre-term birth
They didn’t find a strong correlation between drinking early in pregnancy and an increased likelihood of these complications, so some people take this to mean it’s A-OK. But this study only looked at short-term outcomes (not long-term effects that might not show up until childhood) and not fetal alcohol syndrome disorders (FASDs).
But this study only looked at short-term outcomes (not long-term effects that might not show up until childhood) and not fetal alcohol syndrome disorders (FASDs).
These studies represent two ends of the spectrum — one shows some scary possibilities about changed DNA, and the other suggests no ill effects. Most studies fall more in the murky middle, though.
For example, this 2014 study looked at 1,303 pregnant women in the United Kingdom and their alcohol consumption before pregnancy and during all three trimesters. Results suggested that drinking — even fewer than two drinks per week — in the first trimester increased risk of complications, like lower birth weight and pre-term birth.
And this research published in 2012 suggested that even light drinking in the early weeks could increase miscarriage risk, though the risk goes up with heavier drinking.
It might be accurate to look at all the information out there and say that very light drinking in very early pregnancy doesn’t always (or often) cause problems — but it could. And different people define “light” differently, adding to the confusion. So following CDC and NHS guidelines of no alcohol at any point is the safest option and the one that we recommend.
And different people define “light” differently, adding to the confusion. So following CDC and NHS guidelines of no alcohol at any point is the safest option and the one that we recommend.
There are a couple big concerns with drinking early in pregnancy: miscarriage and fetal alcohol syndrome disorders.
It’s an incredibly difficult reality that miscarriages are as common as they are. And even if you do everything by the book, the highest risk of miscarriage is in the first trimester — and it often happens due to issues outside of your control (like chromosomal abnormalities).
Numerous reliable sources and studies (like the one we mentioned above) mention that alcohol use in the first trimester may increase miscarriage risk. Why this happens isn’t entirely clear.
The other big risk is FASDs. Symptoms include:
- pre-term birth
- low birth weight
- neurological problems
- behavioral problems that show up later in childhood
- certain abnormal facial features (thin upper lip, small eyes, missing vertical crease between the nose and lips)
- cognitive difficulties
Here’s something to remember: in-utero human development doesn’t happen all at once. It happens over a 40-week period (more or less, but you know what we mean) and there are many contributing factors.
It happens over a 40-week period (more or less, but you know what we mean) and there are many contributing factors.
And while drinking at any stage of pregnancy should be avoided, both the American College of Obstetricians and Gynecologists and the Royal College of Obstetricians and Gynaecologists say harm from having a little alcohol before you knew you were pregnant is unlikely.
So if you drank alcohol before you realized you were pregnant, the important thing is that you stop now. Your tiny human’s brain has a lot of development yet to go.
Take your daily prenatal vitamin, maintain a healthy diet, avoid undercooked meats and raw or high-mercury fish, and keep your prenatal appointments — these are all wonderful things you can do to promote your baby’s health.
And while we’re on the topic of those prenatal appointments — talk to your doctor candidly about your concerns and let them know that you had alcohol early on.
If you feel uncomfortable chatting with them about things that may affect your pregnancy, find a new doctor. Being able to speak honestly about your health and the health of your baby during pregnancy is crucial to having a healthy, happy nine months.
Being able to speak honestly about your health and the health of your baby during pregnancy is crucial to having a healthy, happy nine months.
ALCOHOL AND PREGNANCY - Outpatient medical facility
The fact that you can not drink alcohol during pregnancy is known to most. However, different situations can arise in life: one woman is planning a pregnancy, continuing to drink alcohol on holidays in order to avoid uncomfortable questions; another drinks a glass of wine, unaware that she is already pregnant; the third during pregnancy cannot cope with the desire to drink beer, believing that "a little bit is possible." Let's look at these situations in more detail.
Alcohol consumption during pregnancy planning.
Alcohol is a toxin that adversely affects the human reproductive system. In women, alcohol consumption leads to disruption of the menstrual cycle and hormonal balance, which significantly affects the ability to conceive. There are also opinions that even episodic alcohol consumption can have a negative effect on the eggs, leading to their inferiority. Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception.
Drinking alcohol in the first weeks after conception.
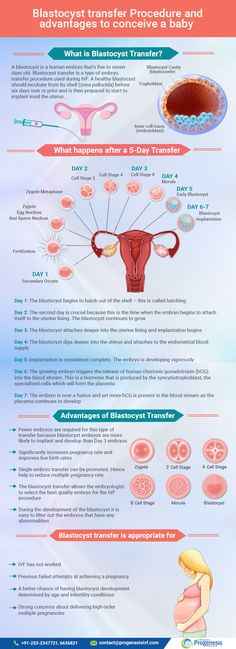
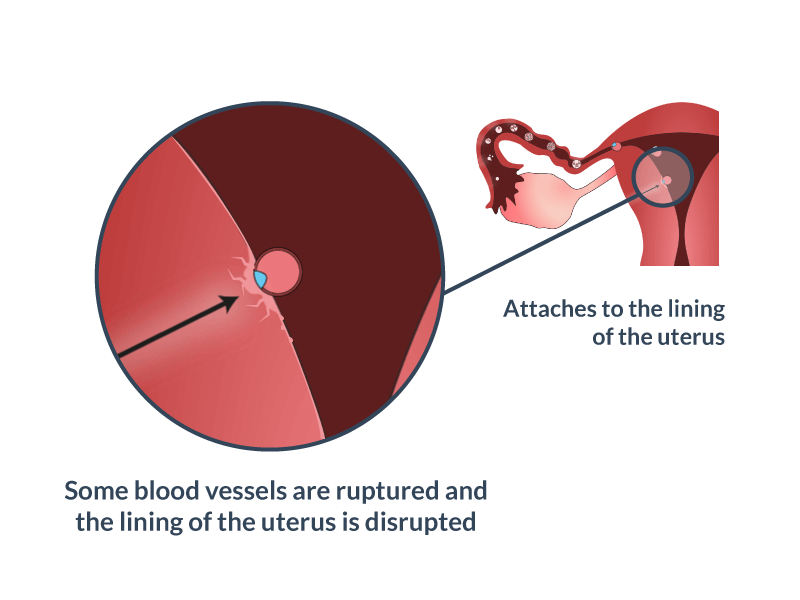
Without a special examination, a woman usually discovers the fact of pregnancy at 3 weeks after conception, when the next menstruation does not come. By this time, the embryo has already firmly attached to the uterine cavity and began to receive nutrition from the mother's blood. If negative factors, including alcohol, affect him before the moment of attachment, then this will lead to his rejection and death, and he will simply leave the uterus with the next menstruation. Thus, a woman may not know that she was pregnant.
According to most scientists, if alcohol did not disrupt the attachment process and the embryo continued to develop, then this would not lead to the formation of malformations in it. Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Alcohol use in early pregnancy.
As mentioned above, as early as the 3rd week after conception, the embryo begins to come into contact with maternal blood. This means that all the substances in the mother's blood come to him. including ethyl alcohol. From the 3rd to the 13th week of development, the laying of all the main systems of the body of the unborn child occurs and the effect of alcohol no longer leads to rejection and death of the embryo, but to the formation of malformations and deformities of the nervous, cardiovascular, and digestive systems.
Alcohol use in late pregnancy.
The negative impact of alcohol on the course of pregnancy is observed after the 13th week. Ethanol and its decay products lead to spasm of the vessels of the placenta and umbilical cord, impairing the delivery of oxygen and nutrients, leading to a delay in the development of the fetus, disruption of its nervous system and brain. A prolonged lack of oxygen can even lead to the death of a child. Violation of the nervous system in the prenatal period leads to problems in the later life of the child - such children have reduced stress resistance, problems in learning, in communication, a tendency to mental illness and alcohol consumption.
The systematic use of alcohol during pregnancy leads to the formation of fetal alcohol syndrome in a child - this is a complex of physical, mental and intellectual abnormalities in a child that cannot be treated.
Thus, alcohol and pregnancy are not compatible and it is necessary to refuse it at the planning stage.
You need to understand that one glass of wine, drunk before 2 or after 13 weeks of pregnancy, most likely will not lead to disastrous consequences, but is it worth the risk? Remember that your child will “drink” half of this glass.
WOMEN'S PERSONAL HYGIENE - Outpatient medical facility
Compliance with the basic rules of personal hygiene is the key to health, everyone knows this. This rule, no doubt, applies to women's health in general, and to women's intimate hygiene in particular. Talking about such a delicate topic, of course, is best with a gynecologist.
Basic rules:
- Wash with warm, clean water at least twice a day. As a cleaning agent, you can use either special intimate hygiene products sold in pharmacies, or not use any. Soaps, shower gels, etc. have an alkaline environment, while the environment of the vagina is acidic. The acidic pH and the lactobacilli living on the mucosa are a very important component in maintaining a normal vaginal environment and protecting it from harmful microorganisms. Regular use of products with an alkaline environment destroys this defense system and contributes to the development of diseases.
- When performing hygienic procedures, it is necessary to ensure that all movements of the hands or the water jet are directed from front to back. The reverse movement can bring bacteria from the anus to the vaginal mucosa, which will lead to inflammatory diseases.
- The towel must be clean, soft and always individual. Some harmful microorganisms are able to survive on fabrics, napkins, on the surfaces of objects and be transmitted to humans through contact with these surfaces.
- Vaginal douching (i.e. rinsing from the inside) is a medical procedure that is performed only on doctor's orders and using special solutions, depending on the disease. A healthy woman does not need this procedure and can even harm.
- The use of sanitary napkins and synthetic underwear can cause bacterial growth, reduce the protective properties of the vaginal mucosa and, as a result, the development of the disease. Therefore, it is preferable to wear underwear made from natural fabrics and use panty liners only when necessary.
- For early detection and prevention of diseases of the female genital area, a woman of any age who is sexually active should visit a gynecologist at least once a year, even if there are no complaints. It must be remembered that some diseases may not manifest themselves for a very long time.
-
The period of critical days is a special period in a woman's body, when the level of ovarian hormones in the blood is minimal, the body's defenses are reduced, local immune defenses are weakened, and the uterine cavity from the inside is an extensive wound surface.
To maintain women's health during menstruation, the following rules must be observed:
- Pads should be changed every 4-5 hours, tampons every 2 hours. Intimate hygiene products soaked in blood are a good breeding ground for bacteria, so they must be changed in a timely manner.
- You can not swim in the reservoirs, go to the pool, take a bath, i.e. dive into the water. During menstruation, a mucous plug comes out of the narrow cervical canal, which at other times protects the uterine cavity from foreign microorganisms, and the uterine cavity becomes vulnerable to bacteria contained in the water.
- Sexual intercourse during menstruation should also be avoided.