Location of the uterus during pregnancy
Anatomy of pregnancy and birth - uterus
Anatomy of pregnancy and birth - uterus | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What does the uterus look like?
One of the most recognised changes in a pregnant woman’s body is the appearance of the ‘baby bump’, which forms to accommodate the baby growing in the uterus. The primary function of the uterus during pregnancy is to house and nurture your growing baby, so it is important to understand its structure and function, and what changes you can expect the uterus to undergo during pregnancy.
The uterus (also known as the ‘womb’) has a thick muscular wall and is pear shaped. It is made up of the fundus (at the top of the uterus), the main body (called the corpus), and the cervix (the lower part of the uterus ). Ligaments – which are tough, flexible tissue – hold it in position in the middle of the pelvis, behind the bladder, and in front of the rectum.
The uterus wall is made up of 3 layers. The inside is a thin layer called the endometrium, which responds to hormones – the shedding of this layer causes menstrual bleeding. The middle layer is a muscular wall. The outside layer of the uterus is a thin layer of cells.
Illustration showing the female reproductive system.The size of a non-pregnant woman's uterus can vary. In a woman who has never been pregnant, the average length of the uterus is about 7 centimetres. This increases in size to approximately 9 centimetres in a woman who is not pregnant but has been pregnant before. The size and shape of the uterus can change with the number of pregnancies and with age.
How does the uterus change during pregnancy?
During pregnancy, as the baby grows, the size of a woman’s uterus will dramatically increase. One measure to estimate growth is the fundal height, the distance from the pubic bone to the top of the uterus.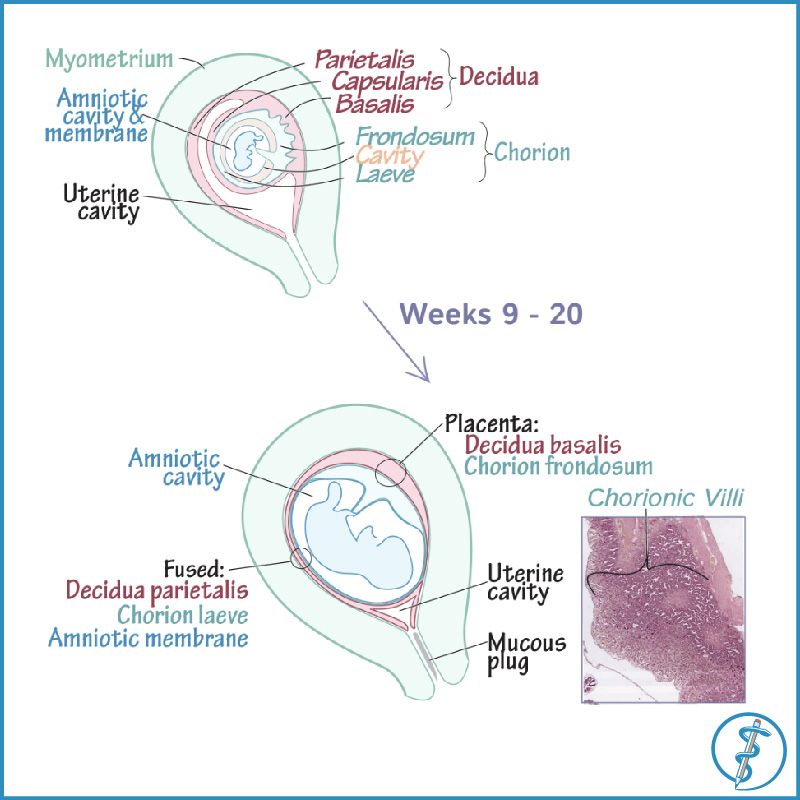 Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Fundal height can vary from person to person, and many factors can affect the size of a pregnant woman’s uterus. For instance, the fundal height may be different in women who are carrying more than one baby, who are overweight or obese, or who have certain medical conditions. A full bladder will also affect fundal height measurement, so it’s important to empty your bladder before each measurement. A smaller than expected fundal height could be a sign that the baby is growing slowly or that there is too little amniotic fluid. If so, this will be monitored carefully by your doctor. In contrast, a larger than expected fundal height could mean that the baby is larger than average and this may also need monitoring.
As the uterus grows, it can put pressure on the other organs of the pregnant woman's body. For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
How does the uterus prepare for labour and birth?
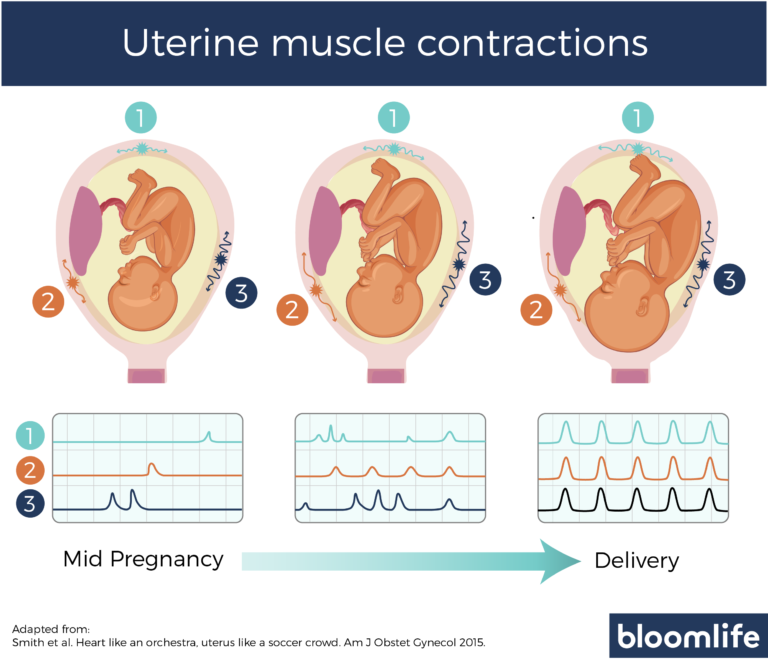
Braxton Hicks contractions, also known as 'false labour' or 'practice contractions', prepare your uterus for the birth and may start as early as mid-way through your pregnancy, and continuing right through to the birth. Braxton Hicks contractions tend to be irregular and while they are not generally painful, they can be uncomfortable and get progressively stronger through the pregnancy.
During true labour, the muscles of the uterus contract to help your baby move down into the birth canal. Labour contractions start like a wave and build in intensity, moving from the top of the uterus right down to the cervix. Your uterus will feel tight during the contraction, but between contractions, the pain will ease off and allow you to rest before the next one builds. Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to the birth.
How does the uterus change after birth?
After the baby is born, the uterus will contract again to allow the placenta, which feeds the baby during pregnancy, to leave the woman’s body. This is sometimes called the ‘after birth’. These contractions are milder than the contractions felt during labour. Once the placenta is delivered, the uterus remains contracted to help prevent heavy bleeding known as ‘postpartum haemorrhage‘.
The uterus will also continue to have contractions after the birth is completed, particularly during breastfeeding. This contracting and tightening of the uterus will feel a little like period cramps and is also known as 'afterbirth pains'.
Read more here about the first few days after giving birth.
Sources:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), StatPearls Publishing (Anatomy, Abdomen and Pelvis), Department of Health (Clinical practice guidelines: Pregnancy care), Better Health Channel Victoria (Pregnancy stages and changes), Mater Mother's Hospital (Labour and birth information), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (The First Few Weeks Following Birth), Queensland Health (Queensland Clinical Guidelines – maternity and neonatal), King Edward Memorial Hospital (Fundal height: Measuring with a tape measure), Royal Hospital for Women (Fetal growth assessment (clinical) in pregnancy), MSD Manual (Female internal genital organs)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - perineum and pelvic floor
Need more information?
Prolapsed uterus - Better Health Channel
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways, causing uterine prolapse.
Read more on Better Health Channel website
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.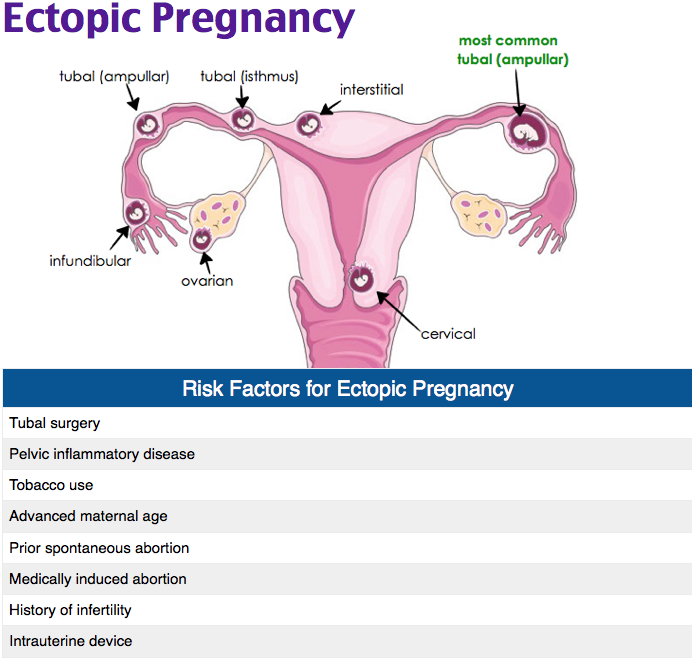
Read more on Jean Hailes for Women's Health website
Uterine differences
Some people have a uterus with a different shape. If your uterus has a different shape, you may have difficulties becoming pregnant, recurrent miscarriages or premature birth.
Read more on Pregnancy, Birth & Baby website
Dilatation and curettage (D&C)
A D&C is an operation to lightly scrape the inside of the uterus (womb).
Read more on WA Health website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
Hormonal IUD (intrauterine device, Mirena®) | Body Talk
The hormonal IUD is a type of contraception and is placed inside the uterus by a specially trained doctor or nurse.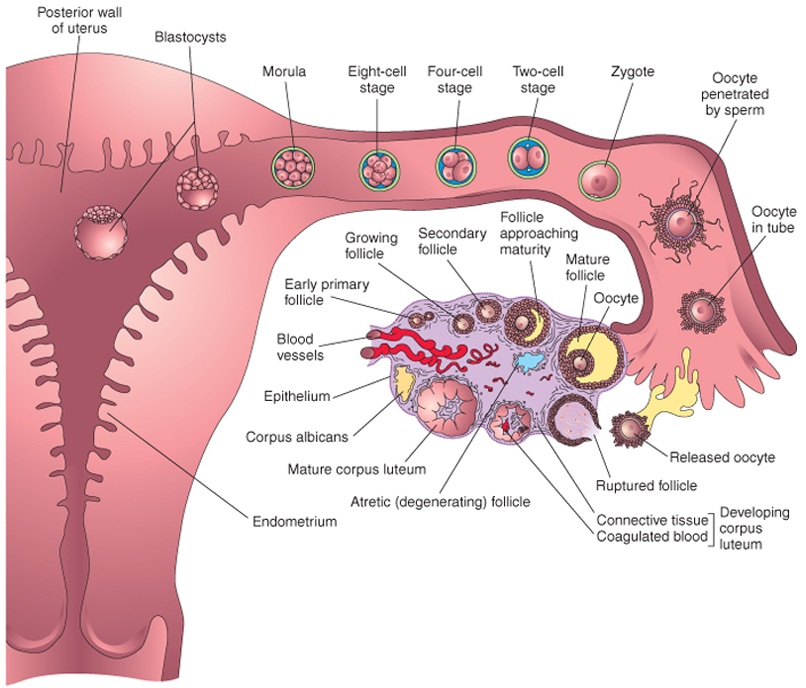 Find out all the facts here.
Find out all the facts here.
Read more on Body Talk website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Copper IUD (intrauterine device) | Body Talk
The copper IUD is a type of contraception and is placed inside the uterus by a specially trained doctor or nurse. Find out all the facts here.
Read more on Body Talk website
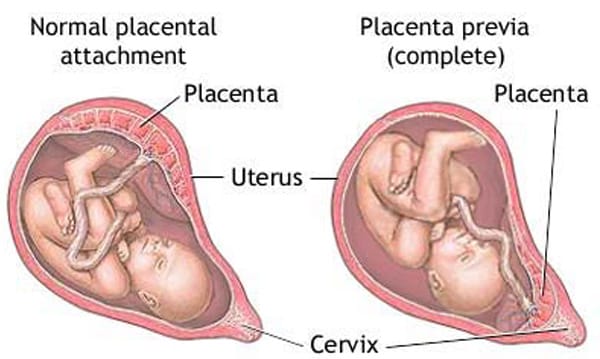
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.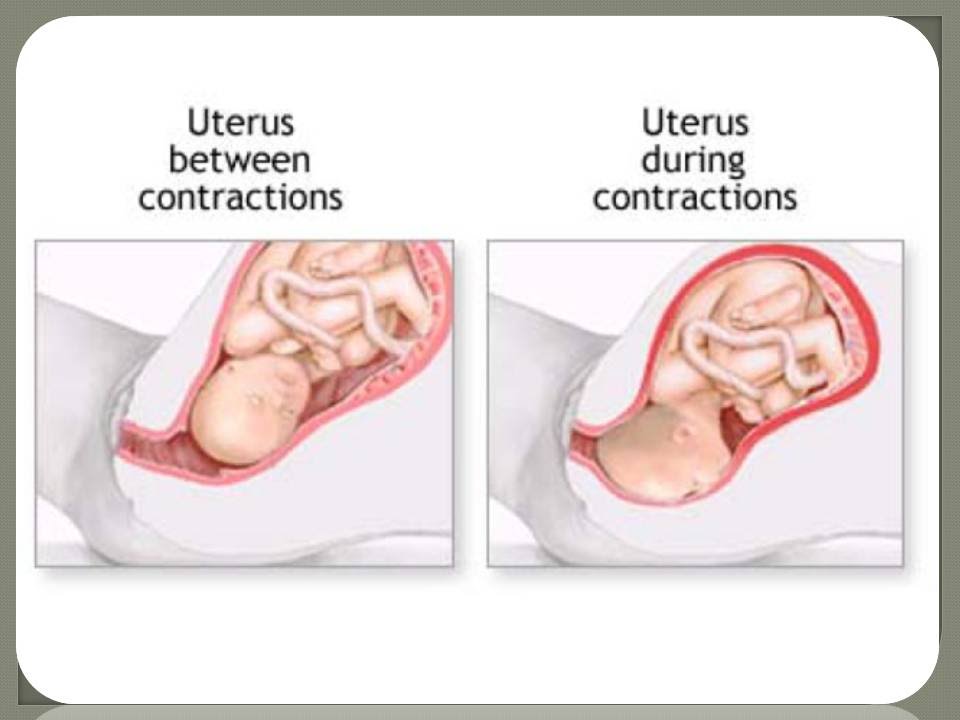
Read more on Better Health Channel website
Mirena IUD | Hormonal IUD Mirena | IUD Mirena insertion | IUD Mirena cost | Mirena IUD Melbourne - Sexual Health Victoria
The hormonal intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Sexual Health Victoria website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.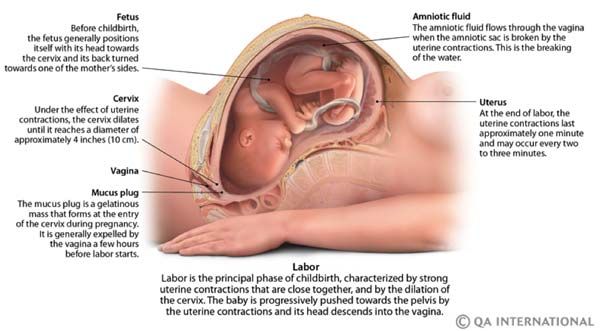
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Your Body throughout Pregnancy
Your Body Before Pregnancy
Next Image
Your Body Before Pregnancy
Before pregnancy, most of the space in your abdomen is taken up by the large and small intestines.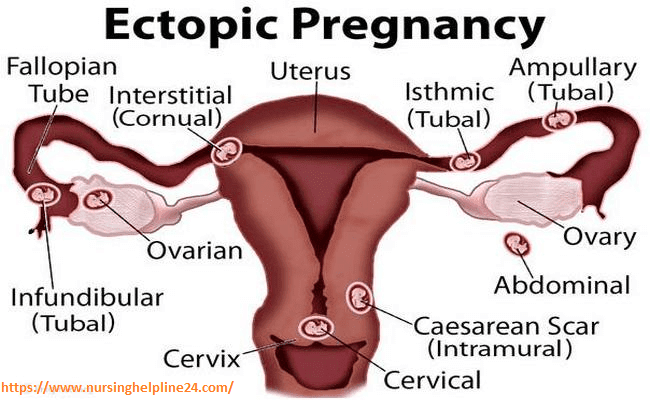 There is no real separation between the areas of your pelvis and abdomen.
There is no real separation between the areas of your pelvis and abdomen.
In the picture here, you can see that the vagina is behind the bladder (sac that collects urine) and urethra (tube for moving urine out of bladder and body). In its normal position, your uterus is above and behind the bladder, with the cervix protruding into the vagina. The pelvic colon, rectum and anal canal are behind the vagina and uterus.
Previous | Next
Your Body at 6-7 Weeks of Pregnancy
Next Image
Your Body at 6-7 Weeks of Pregnancy
When you are between 6 and 7 weeks pregnant, you may be experiencing the early signs of pregnancy: your period has stopped and you may have nausea, breast tenderness and swelling, frequent urination and fatigue.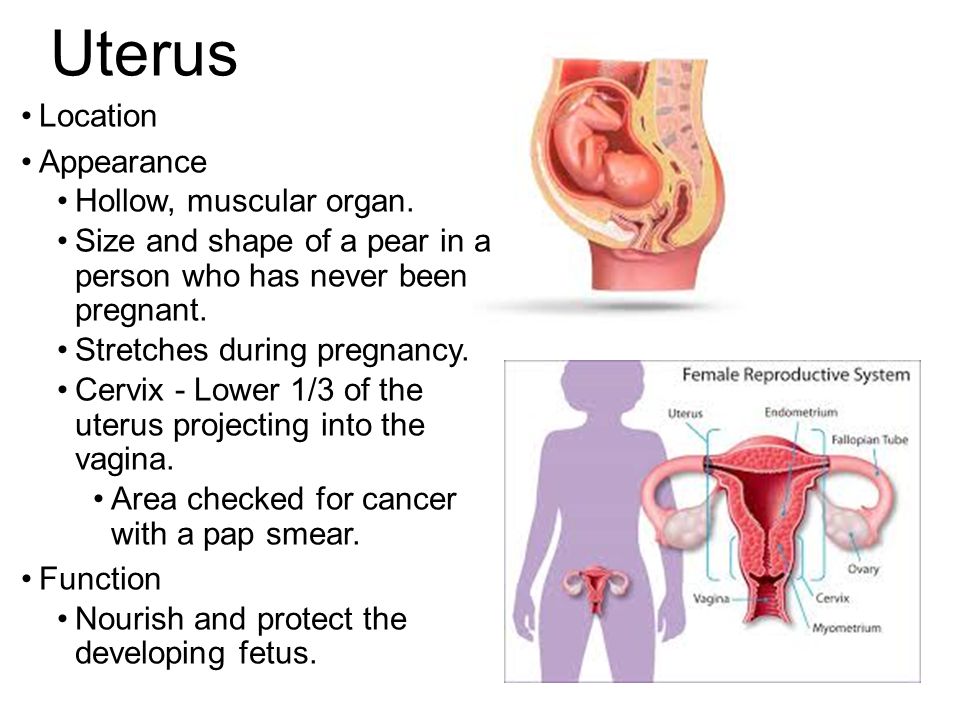
At this point, your uterus has begun to grow and become more egg-shaped. The pressure of the growing uterus on the bladder causes frequent urge to urinate.
In this image, you can see the beginnings of the placenta in the uterus. The embryo is about 1/4 inch to 1/2 inch long and weighs 1/1,000th of an ounce.
The embryo’s head is large in proportion to the rest of the body. The internal organs are forming and the heart has been beating since the end of the 4th week.
The embryo is floating in the amniotic sac. Buds for the arms and legs emerge in the 5th week and, by the 7th week, buds for fingers and toes also appear. The umbilical cord is lengthening and will continue to grow, allowing the fetus freedom to move. The 7th week represents a milestone in development: the embryo is now considered a fetus.
Previous | Next
Your Body at 12 Weeks of Pregnancy
Next Image
Your Body at 12 Weeks of Pregnancy
At the 12th week of pregnancy, the placenta is much larger.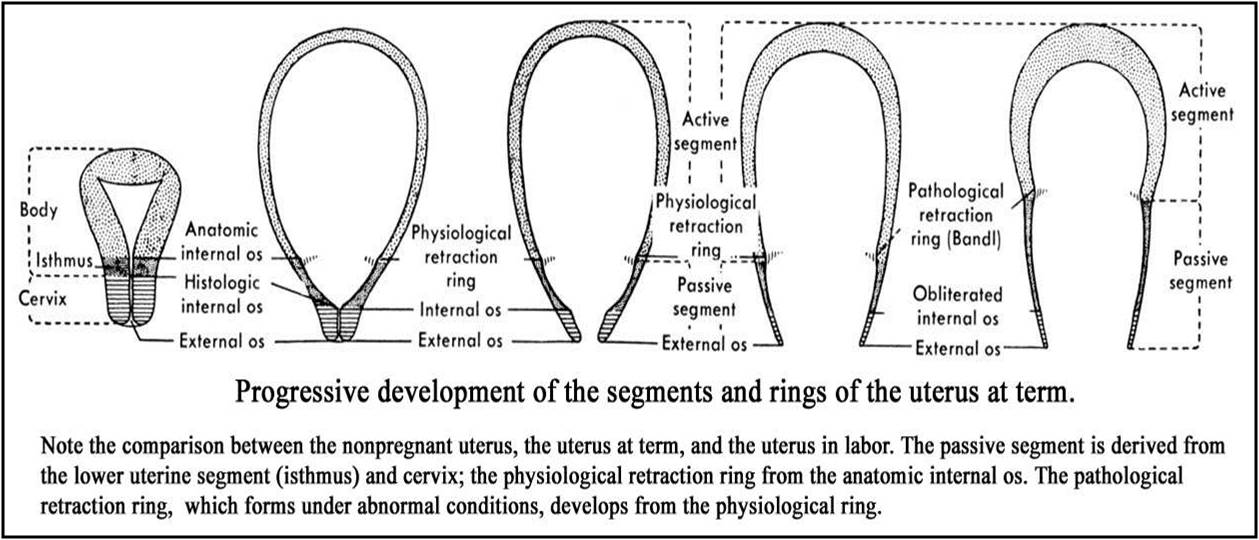 It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
The fetus is now about 3 inches long and weighs about 1 ounce. By this week, the fetus has fingernails and toenails and can open and close the fingers. The fetus will start to move, but you will not feel it yet.
Previous | Next
Your Body at 20 Weeks of Pregnancy
Next Image
Your Body at 20 Weeks of Pregnancy
By the 20th week of pregnancy, your uterus can be felt at the level of your belly button (umbilicus).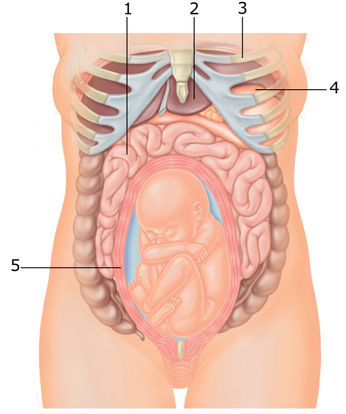 The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
At this point, your uterus is especially enlarged where the placenta attaches to it (usually on the front or back wall). This gives the uterus an uneven bulge. The wall of the uterus, which lengthens and thickens early in pregnancy, stretches as the fetus grows, and becomes thinner now – just 3 to 5 millimeters thick. Your bladder moves up but not as much as your uterus, which straightens as it moves up.
As your uterus moves up, it rests against the lower portion of the front of your abdominal wall, causing it to bulge forward noticeably by your 20th week. The size of the bulge depends on how strong your abdominal muscles are. If they are firm, the uterus may be pressed against the spinal column, and there will be no noticeable bulge; if they are weak, the pressure of the uterus against the inside wall makes a sizeable bulge.
At this point, you should be able to feel light movements of the fetus. This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
Previous | Next
Next Image
At this point in pregnancy, the top of your uterus is about one-third of the distance between the bellybutton and the xiphoid cartilage at the lower end of your breastbone. Constipation is common because your uterus is pressing on your lower colon and hormones slow down your body’s excretion process. Between the growth of your uterus and general weight gain, you may be feeling fatigued. Some women also experience heartburn as your uterus presses against your stomach.
Your breasts are also changing to get ready for breastfeeding. First colostrum and then milk are produced by the grape-like clusters of tiny sacs (alveoli) deep within the breast tissue. Clusters of alveoli form lobules, which come together to form 15 to 20 lobes. Each lobe connects to a lactiferous duct for conveying milk. As the ducts extend toward the nipple and areola (darker area around the nipple), they widen into the lactiferous sinuses. These sinuses (or milk pools) release the milk through 15 to 20 tiny nipple openings in each breast when the baby nurses.
At week 28, the fetus is about 16 inches long and weighs two to three pounds. The skin is wrinkled but will become less so as more fat builds up under the skin in the next few weeks. Fine, downy hair called lanugo, and a waxy white protective substance covering the skin called vernix, are on the fetus’ body. Its eyes are open, and eyebrows and eyelashes were formed in the fourth month. The fetus sucks its thumb and its taste buds have developed.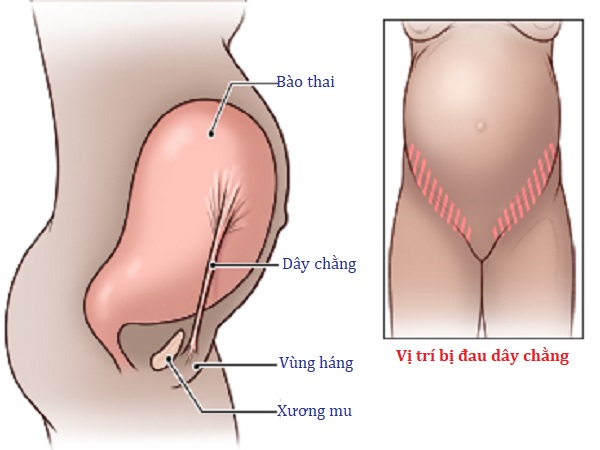 It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
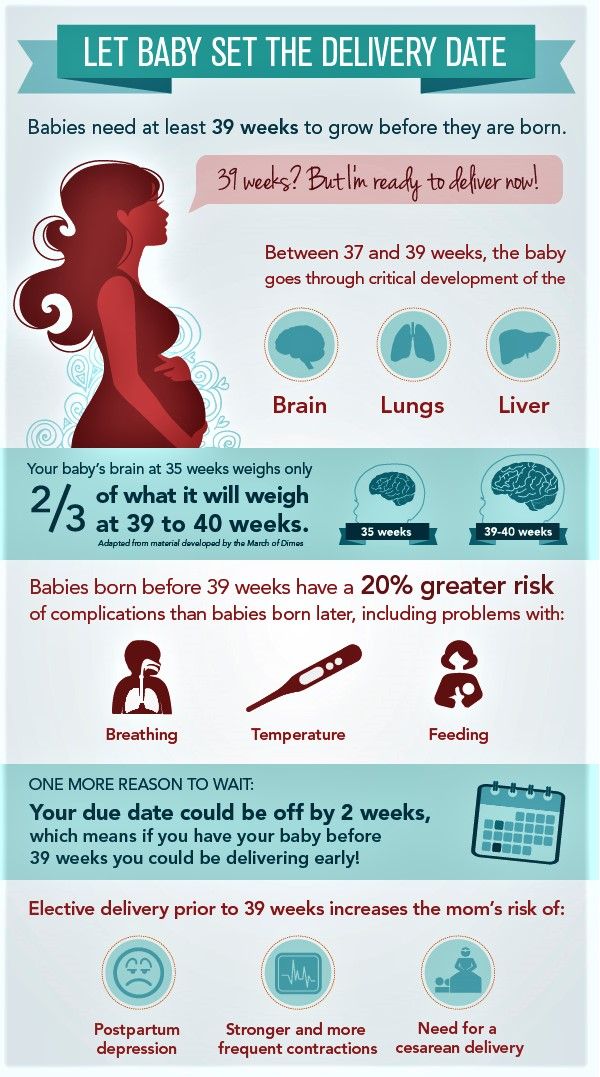
Fetal organs and systems are quite well developed by the 28th week of pregnancy, but the final two months of gestation are important for further maturation of all body systems and organs.
Previous | Next
Your Body at 36 Weeks of Pregnancy
Next Image
Your Body at 36 Weeks of Pregnancy
By the end of the 36th week of pregnancy, your enlarged uterus almost fills the space within your abdomen. The fetus is inside the membrane sac within the uterus and high within the abdomen. The muscles of your abdomen support much of its weight.
During this week, the top of the uterus is at the tip of the xiphoid cartilage at the lower end of the breastbone, which is pushed forward.
The change in the position of the heart and the upward pressure of the diaphragm may make it hard to breathe at this point. The crowding of your stomach and intestines may contribute to discomfort after eating.
Your cervix is long, thick and filled with the mucous plug. By the 36th week, your vagina and urethra are elongated and all the tissues in the perineum (area between vaginal and anal openings) are enlarged. The swollen perineum projects outward in the last weeks of pregnancy and readily expands during labor.
The brain of the fetus is growing rapidly, but bones in the skull are soft so that he or she will fit through your vagina at birth. The lungs are still forming. You will likely feel the fetus kicking and may be aware of rhythmic movements, which could be hiccups or thumb sucking. Another possible sensation, sudden movement, may be a startle response.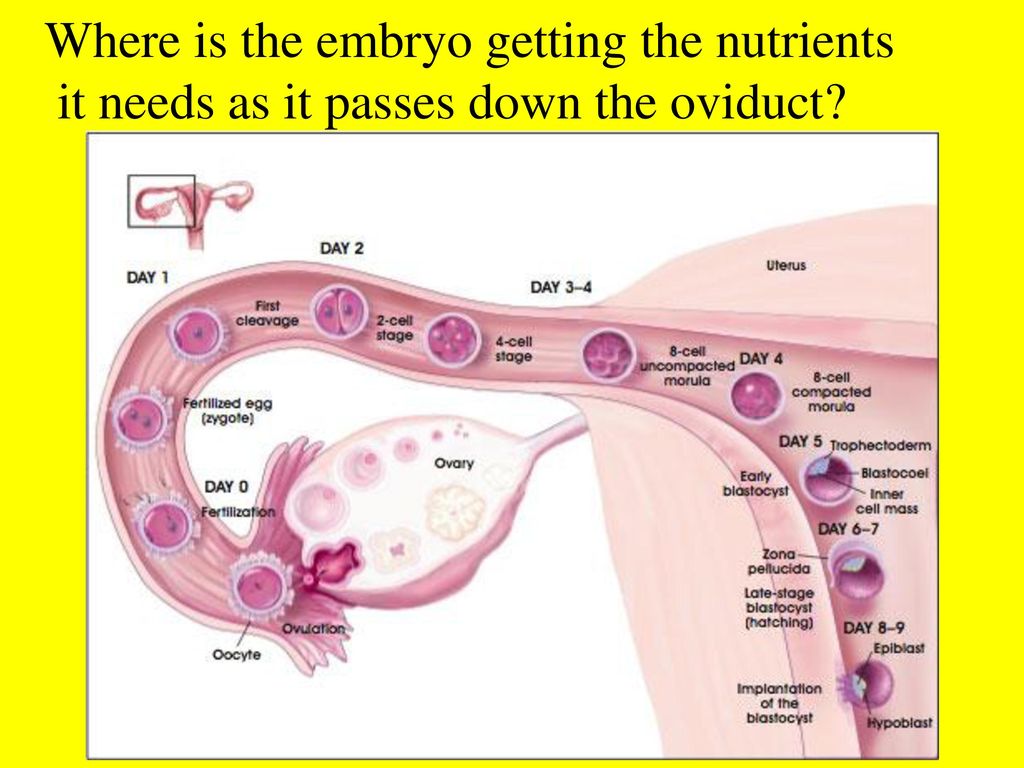
Previous | Next
Your Body at 40 Weeks of Pregnancy (Internal)
Next Image
Your Body at 40 Weeks of Pregnancy (Internal)
At full term, or 40 weeks of pregnancy, the fetus’ head has generally lowered into your pelvis, where it takes up most of the space. This is called “lightening.” In first pregnancies, this may happen a few weeks before labor. In repeat pregnancies, this can happen at the time of labor. The canal of the broad, enlarged cervix is still filled with the plug of mucous. If this is your first pregnancy, the small opening at the bottom of your cervix is usually not dilated, whereas if you have given birth before, it will often be open as wide as two fingers some time before labor begins.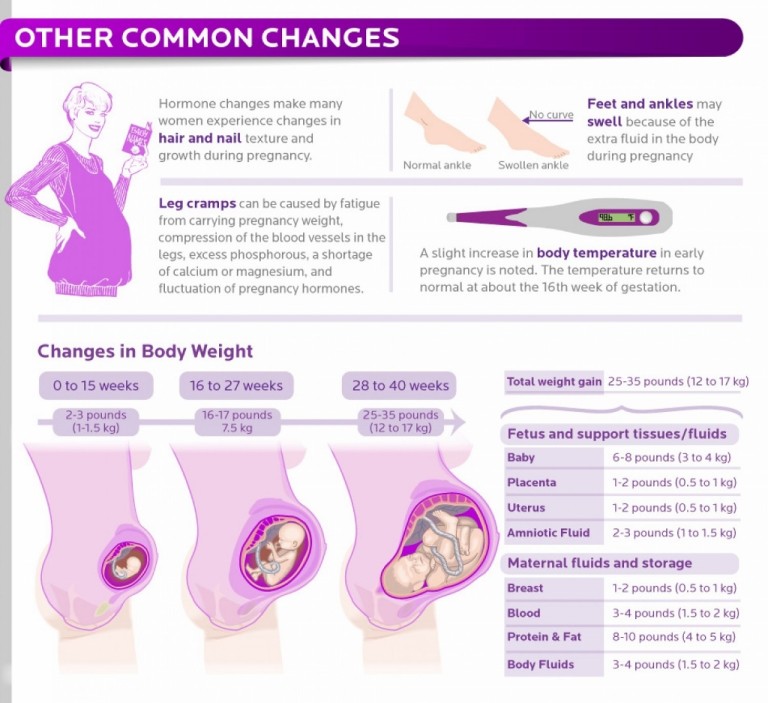
At this point, you may be experiencing frequent urination, increased constipation, edema (water retention) and aching legs or vulva. Varicose veins in the vulva, rectum and legs are also possible. This is because of the position of the uterus, the pressure of the baby's head and a loss of muscle tone as the hormone relaxin loosens your tissues in preparation for birth. Other changes at this time include increased development of blood vessels and increased amount of blood.
Previous | Next
Your Body at 40 Weeks of Pregnancy (External)
Next Image
Your Body at 40 Weeks of Pregnancy (External)
You can see that the round ligament is long and enlarged. It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
Because your uterus dropped a bit, you may be able to breathe and eat more comfortably near the end of your pregnancy.
At this time, the lungs of the fetus are likely fully mature and ready to begin breathing. The fetus gains about a half pound every week at the end of pregnancy, for a birth weight of roughly 7 pounds, and is growing longer for a birth length of about 18 to 21 inches.
Labor starting on its own around week 40 is a sign that your body is ready to give birth and your baby is ready to be born.
Previous | Next
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned.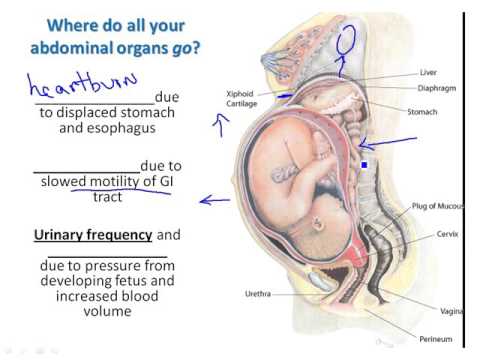 And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina.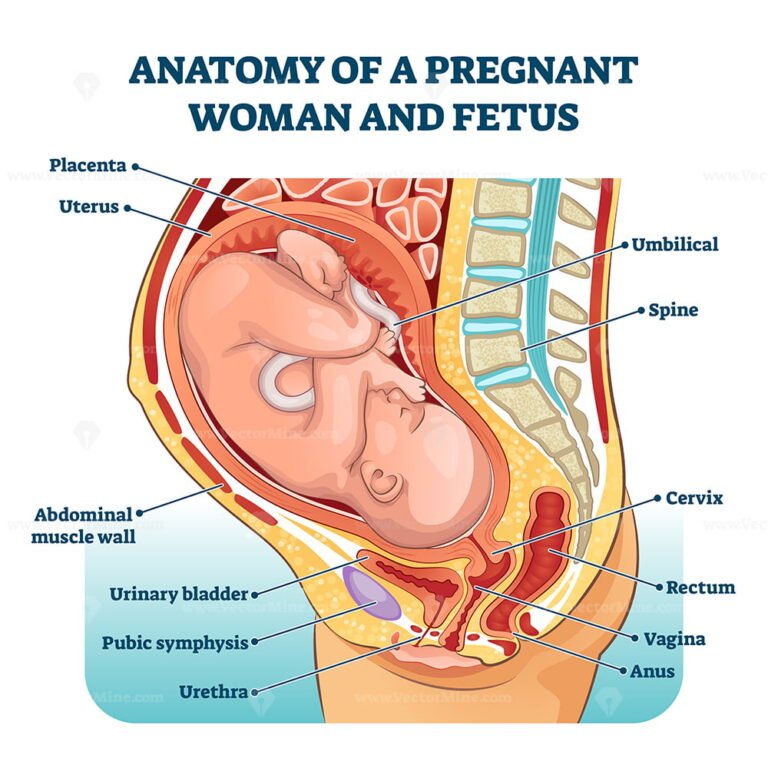 Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft.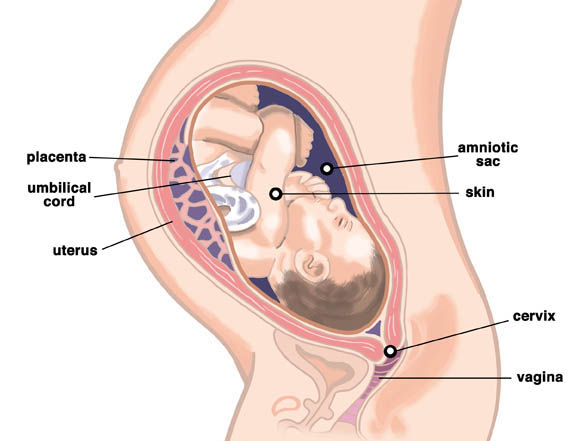 During pregnancy, the cervical glands expand and become more branched.
During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina.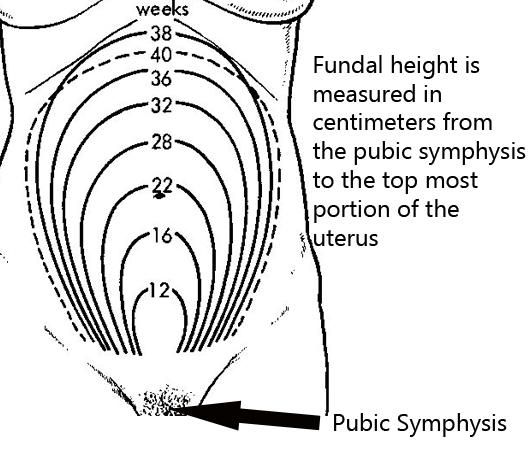 Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents.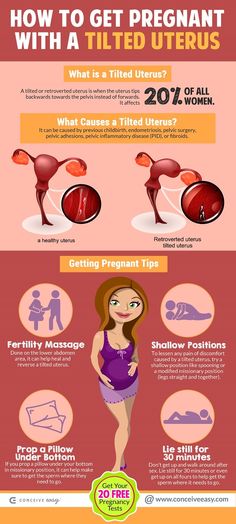 However, this is very rare and usually requires monitoring during pregnancy.
However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease.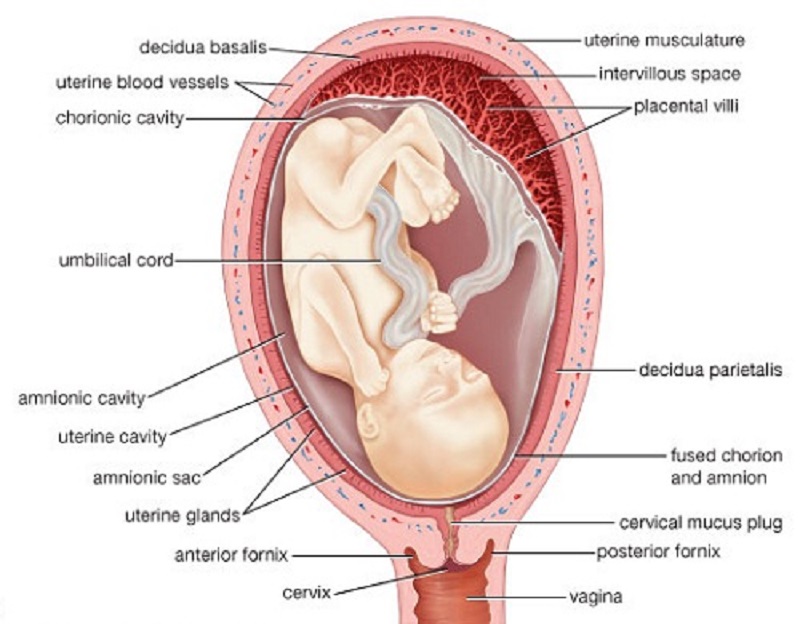 The reasons may be:
The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital IDKMother and Child Clinic Enthusiastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children)Molecular genetics laboratoryGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsAdult ultrasound examinations
01.
Specialist consultations (adults)
02.
Consultations of specialists (children's)
03.
Laboratory of molecular genetics
04.
Adult Telemedicine
08.
Therapeutic Research
09.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
FIRST SIGNS OF PREGNANCY
All girls have heard about the first signs of pregnancy, the so-called discharge .
How else can you tell if you are pregnant or not? Let's say you had a long delay in your menstrual cycle. Time flies, and menstrual bleeding does not start. In this case, you will systematically feel nausea, while the mammary glands will seem heavy to you.
In addition to discharge, another sign of pregnancy is the constant thirst for sleep.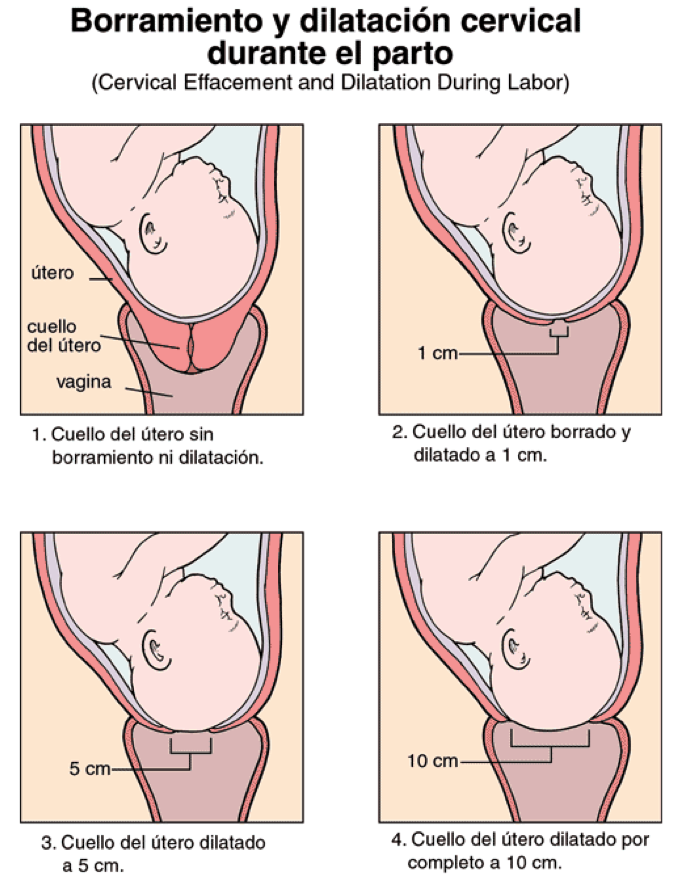 The everyday activities of the people around you are annoying, and besides, you become very nervous about the presence of certain smells.
The everyday activities of the people around you are annoying, and besides, you become very nervous about the presence of certain smells.
In addition to discharge, the first sign of pregnancy is an increase in appetite. Food begins to evaporate from your refrigerator at an astonishing rate and in a variety of combinations of ingredients. At the same time, saliva may still flow, and the number of midnight trips to the toilet will also increase. During the day, you can’t walk for a long time either, this is problematic because of the constant desire to urinate.
All of these discharges and other signs may be present both together and separately. Often a woman talks about a delay in the menstrual cycle in the absence of any deviations in her state of health.
There is an accessible and easy way to clarify these facts. Of course, no method will give you 100% guarantees. You can get a reliable 100% conclusion only after an examination by a gynecologist and a special diagnosis (examination). However, when the first signs of pregnancy appear (discharge, etc.) in the initial 10-12 days of the deviation of the menstrual cycle from the chronology, even in a good clinic you will not be able to guarantee the results of studies to determine pregnancy.
However, when the first signs of pregnancy appear (discharge, etc.) in the initial 10-12 days of the deviation of the menstrual cycle from the chronology, even in a good clinic you will not be able to guarantee the results of studies to determine pregnancy.
If menstruation does not start at the expected time, then after waiting for the morning, measure the body temperature in the rectum. An ordinary thermometer (medical, of course) is inserted into the rectum as soon as you wake up. Do not get out of bed while performing this operation. Doctors advise to prepare a thermometer in the evening and put it near the bed.
Need more than 6 hours of sleep. The thermometer is inserted behind the muscle that compresses the anus. The insertion depth of the thermometer is 2 centimeters, and the measurement time is from five to seven minutes. Record the measurement results. Measure body temperature every day for 7-10 days. If the temperature is most often more than 37 C, then this indicates the presence of the first signs of pregnancy.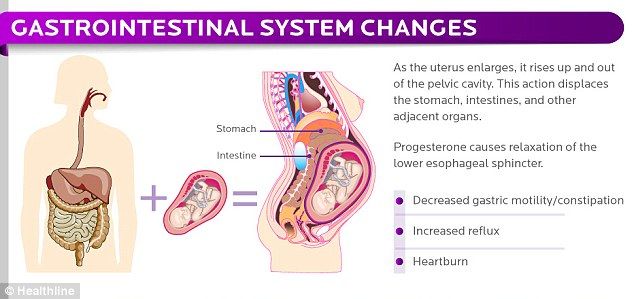
In the absence of menstruation for 3 or more days, as well as in the presence of the first signs of pregnancy (discharge), gynecologists recommend doing a test to determine early pregnancy (most of the tests that are commercially available detect the presence of pregnancy already on the 1st day of delay !). They are easy to use and quite reliable.
The confidence probability of the test turns out to be much greater if it is carried out two or three times.
Outwardly, these tests are all different, but they are based on one chemical reaction to a specific hormone called human chorionic gonadotropin. This hormone is produced during pregnancy. The breakdown products of the hormone are excreted in the urine. The chemical reagent that drinks the dough plate interacts with these products.
Check that the test has not expired. For the experiment, the purpose of which are the first signs of pregnancy (discharge, etc.) it is better to use morning urine. After sleep, the content of the hormone and its decay products in the female body increases. This means that the probability that the tester will detect this increases. If you are a person who does not trust such tests, then as an option you can do a urine test to quantify the content of hCG. Although, this analysis is carried out by far not every medical and diagnostic center.
After sleep, the content of the hormone and its decay products in the female body increases. This means that the probability that the tester will detect this increases. If you are a person who does not trust such tests, then as an option you can do a urine test to quantify the content of hCG. Although, this analysis is carried out by far not every medical and diagnostic center.
Suppose 3-4 weeks have passed, the temperature in the rectum is systematically over 37 degrees, and the test for determining signs of pregnancy gave a positive result 2 times. At the same time, you feel great, there are no subjective disorders and you are full of energy. There may even be an emotional upsurge. Do you need a women's consultation to determine the first signs of pregnancy? Need. To begin with, to confirm that the pregnancy is uterine, and also that the fetal egg was formed precisely in the uterine cavity.
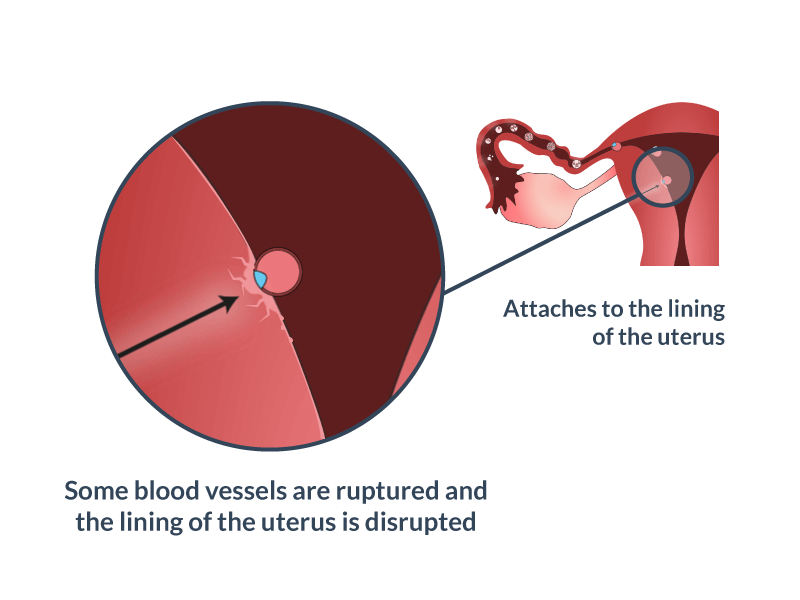
In the normal course of pregnancy, fertilization occurs in the uterine cavity itself.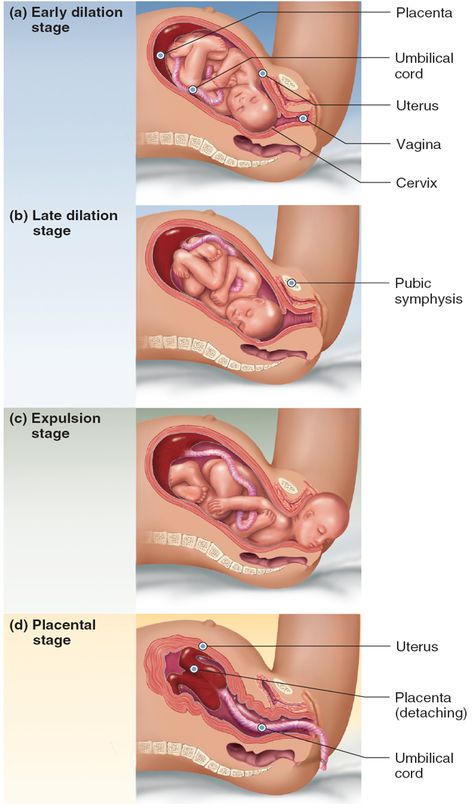 After all, a fertilized egg must reach the site of implantation (through the fallopian tube). If there are any obstacles in the way of the fetal egg (narrowing in the fallopian tube or in the tubal angle of the uterus), and also if the fertilized egg moves for a very long time, or the egg is too large to pass the fallopian tube, then such an egg will not enter the uterine cavity.
After all, a fertilized egg must reach the site of implantation (through the fallopian tube). If there are any obstacles in the way of the fetal egg (narrowing in the fallopian tube or in the tubal angle of the uterus), and also if the fertilized egg moves for a very long time, or the egg is too large to pass the fallopian tube, then such an egg will not enter the uterine cavity.
In this case, an ectopic or ectopic pregnancy may occur and develop. Remember that an ectopic pregnancy in the earliest period shows the same qualitative reactions as the uterine one. In general, the first signs of pregnancy, discharge for example, are universal for pregnancy in the general case.
A gynecologist can detect only indirect first signs of pregnancy, such as plethora of the external genital organs, discoloration of the mucous membrane of the cervix and vagina. It turns blue (acquires a cyanotic hue). In addition, softening of the isthmus (the place where the body of the uterus and its cervix connects) may be noted.
In general, the body of the uterus may be quite large and soft, and may also appear asymmetrical due to swelling at the site of implantation of the ovum.
The uterine appendages are palpated (felt) by a gynecologist. Sometimes it happens that during a normally developing pregnancy, growths are found in the places where the appendages of the cervix are projected. These changes are usually reversible and the normal structure of the ovary is gradually restored. Such growths may appear as corpus luteum or corpus luteum cysts. However, these formations can also be pathological.
To find out if this is the case, you need to resort to other methods of determining the presence of discharge and other first signs of pregnancy.
Ultrasound of the pelvic organs is the safest method. Depending on which research method is chosen (transvaginal or transabdominal), already three weeks after conception, you can get information about the fact of pregnancy, as well as its localization.