Medical tests for pregnancy
Common Tests During Pregnancy | Johns Hopkins Medicine
-
Genetic Screening
-
First Trimester
-
Second Trimester
-
Ultrasound
-
Amniocentesis
-
Chorionic Villus Sampling
-
Fetal Monitoring
-
Glucose
-
Group B Strep Culture
Your health care provider may recommend a variety of screenings, tests and imaging techniques during your pregnancy. These tests are designed to provide information about the health of your baby and may help you optimize your child’s prenatal care and development.
Genetic Screening
Many genetic abnormalities can be diagnosed before birth. Your doctor or midwife may recommend genetic testing during pregnancy if you or your partner has a family history of genetic disorders. You may also choose to have genetic screening if you have had a fetus or baby with a genetic abnormality.
Examples of genetic disorders that can be diagnosed before birth include:
-
Cystic fibrosis
-
Duchenne muscular dystrophy
-
Hemophilia A
-
Polycystic kidney disease
-
Sickle cell disease
-
Tay-Sachs disease
-
Thalassemia
The following screening methods are available during pregnancy:
-
Alpha-fetoprotein (AFP) test or multiple marker test
-
Amniocentesis
-
Chorionic villus sampling
-
Cell-free fetal DNA testing
-
Percutaneous umbilical blood sampling (withdrawing a small sample of the fetal blood from the umbilical cord)
-
Ultrasound scan
First Trimester Prenatal Screening Tests
First trimester screening is a combination of fetal ultrasound and maternal blood testing. This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
First trimester screening includes:
-
Ultrasound for fetal nuchal translucency. Nuchal translucency screening uses an ultrasound to examine the area at the back of the fetal neck for increased fluid or thickening.
-
Ultrasound for fetal nasal bone determination. The nasal bone may not be visualized in some babies with certain chromosome abnormalities, such as Down syndrome. This screen is performed using an ultrasound between 11 and 13 weeks gestation.
-
Maternal serum (blood) tests. These blood tests measure two substances found in the blood of all pregnant women:
-
Pregnancy-associated plasma protein A. A protein produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
Human chorionic gonadotropin. A hormone produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
When used together as first trimester screening tests, nuchal translucency screening and maternal blood tests have a greater ability to determine if the fetus might have a birth defect, such as Down syndrome (trisomy 21) and trisomy 18.
If the results of these first trimester screening tests are abnormal, genetic counseling is recommended. Additional testing, such as chorionic villus sampling, amniocentesis, cell-free fetal DNA or other ultrasounds, may be needed for an accurate diagnosis.
Second Trimester Prenatal Screening Tests
Second trimester prenatal screening may include several blood tests called multiple markers. These markers provide information about your potential risk of having a baby with certain genetic conditions or birth defects.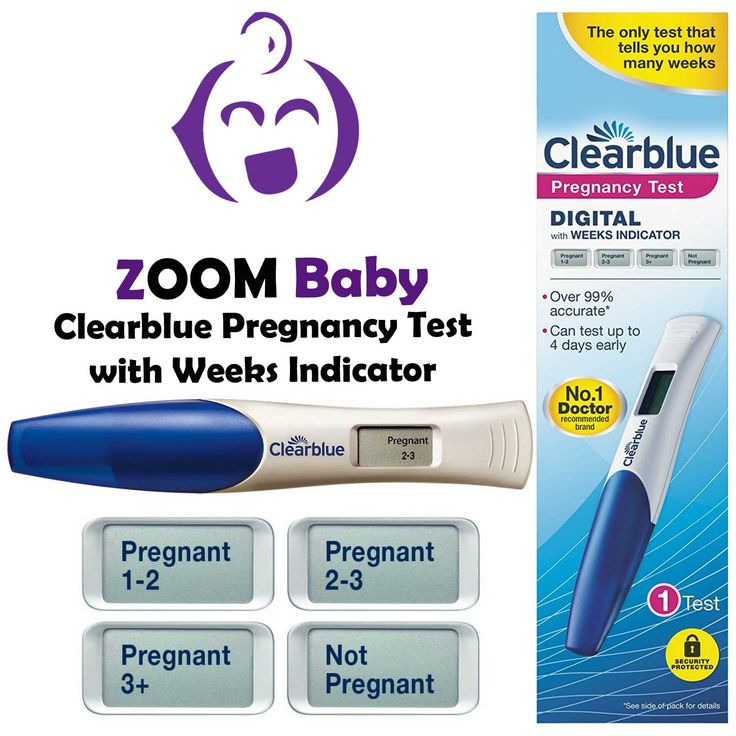 Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
-
AFP screening. Also called maternal serum AFP, this blood test measures the level of AFP in your blood during pregnancy. AFP is a protein normally produced by the fetal liver that is present in the fluid surrounding the fetus (amniotic fluid). It crosses the placenta and enters your blood. Abnormal levels of AFP may indicate:
-
A miscalculated due date, as the levels vary throughout pregnancy
-
Defects in the abdominal wall of the fetus
-
Down syndrome or other chromosomal abnormalities
-
Open neural tube defects, such as spina bifida
-
Twins (more than one fetus is producing the protein)
-
-
Estriol.
 This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health.
This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health. -
Inhibin. This is a hormone produced by the placenta.
-
Human chorionic gonadotropin. This is also a hormone produced by the placenta.
Abnormal test results of AFP and other markers may mean that additional testing is needed. An ultrasound is used to confirm the milestones of your pregnancy and to check the fetal spine and other body parts for defects. An amniocentesis may be needed for an accurate diagnosis.
Since multiple marker screening is not diagnostic, it is not 100 percent accurate. It helps determine who in the population should be offered additional testing during pregnancy. False-positive results may indicate a problem when the fetus is actually healthy. On the other hand, false-negative results indicate a normal result when the fetus actually does have a health problem.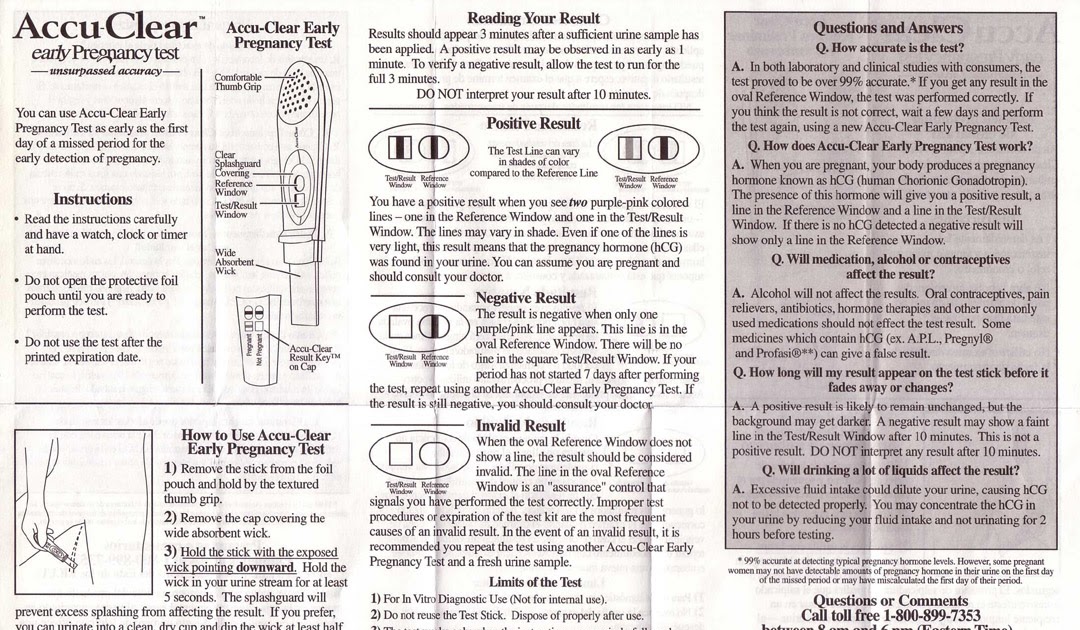
When you have both first and second trimester screening tests performed, the ability of the tests to detect an abnormality is greater than using just one screening independently. Most cases of Down syndrome can be detected when both first and second trimester screenings are used.
Ultrasound
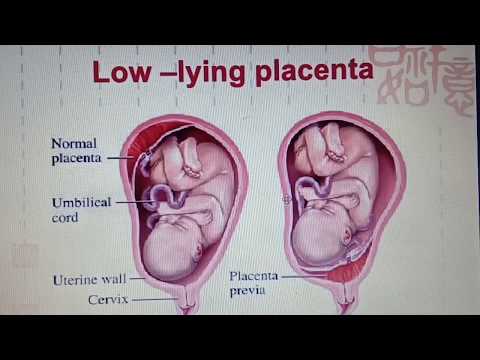
An ultrasound scan is a diagnostic technique that uses high-frequency sound waves to create an image of the internal organs. A screening ultrasound is sometimes done during the course of your pregnancy to check normal fetal growth and verify the due date.
When are ultrasounds performed during pregnancy?
Ultrasounds may be done at various times throughout pregnancy for several reasons:
First Trimester
-
To establish the due date (this is the most accurate way of determining the due date)
-
To determine the number of fetuses and identify placental structures
-
To diagnose an ectopic pregnancy or miscarriage
-
To examine the uterus and other pelvic anatomy
-
To detect fetal abnormalities (in some cases)
Midtrimester (also called the 18- to 20-week scan)
-
To confirm the due date (a due date set in the first trimester is rarely changed)
-
To determine the number of fetuses and examine the placental structures
-
To assist in prenatal tests, such as an amniocentesis
-
To examine the fetal anatomy for abnormalities
-
To check the amount of amniotic fluid
-
To examine blood flow patterns
-
To observe fetal behavior and activity
-
To measure the length of the cervix
-
To monitor fetal growth
Third Trimester
-
To monitor fetal growth
-
To check the amount of amniotic fluid
-
To conduct the biophysical profile test
-
To determine the position of the fetus
-
To assess the placenta
How is an ultrasound scan performed?
Two types of ultrasounds can be performed during pregnancy:
-
Abdominal ultrasound.
 In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image.
In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image. -
Transvaginal ultrasound. In a transvaginal ultrasound, a smaller ultrasound transducer is inserted into your vagina and rests against the back of the vagina to create an image. A transvaginal ultrasound produces a sharper image than an abdominal ultrasound and is often used in early pregnancy.
Which ultrasound imaging techniques are available?
There are several types of ultrasound imaging techniques. As the most common type, the 2-D ultrasound provides a flat picture of one aspect of the baby.
If more information is needed, a 3-D ultrasound exam can be done. This technique, which provides a 3-D picture, requires a special machine and special training. The 3-D image allows the health care provider to see the width, height and depth of the images, which can be helpful during the diagnosis. The 3-D images can also be captured and saved for later review.
The 3-D images can also be captured and saved for later review.
The latest technology is 4-D ultrasound, which allows the health care provider to visualize the unborn baby moving in real time. With 4-D imaging, a three-dimensional image is continuously updated, providing a “live action” view. These images often have a golden color, which helps show shadows and highlights.
Ultrasound images may be captured in still photographs or on video to document findings.
What are the risks and benefits of ultrasound imaging?
Fetal ultrasound has no known risks other than mild discomfort due to pressure from the transducer on your abdomen or in your vagina. No radiation is used during the procedure.
Transvaginal ultrasound requires covering the ultrasound transducer in a plastic or latex sheath, which may cause a reaction in women with a latex allergy.
Ultrasound imaging is constantly being improved and refined. As with any test, the results may not be completely accurate.![]() However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
Fetal ultrasound is sometimes offered in nonmedical settings to provide keepsake images or videos for parents. While the ultrasound procedure itself is considered safe, it is possible that untrained personnel may miss an abnormality or give parents false assurances about their baby’s well-being. It is best to have an ultrasound performed by trained medical personnel who can correctly interpret the results. Talk with your doctor or midwife if you have questions.
Amniocentesis
An amniocentesis involves taking a small sample of the amniotic fluid that surrounds the fetus. It is used to diagnose chromosomal disorders and open neural tube defects, such as spina bifida. Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Who is an ideal candidate for amniocentesis?
An amniocentesis is generally offered to women between the 15th and 20th week of pregnancy who have an increased risk of chromosomal abnormalities. Candidates include women who will be over age 35 at the time of delivery or those who have had an abnormal maternal serum screening test.
How is an amniocentesis performed?
An amniocentesis involves inserting a long, thin needle through your abdomen into the amniotic sac to withdraw a small sample of amniotic fluid. The amniotic fluid contains cells shed by the fetus, which contain genetic information. Although specific details of each procedure may vary, a typical amniocentesis follows this process:
-
Your abdomen will be cleansed with an antiseptic.
-
Your doctor may or may not give a local anesthetic to numb the skin.

-
Your doctor will use ultrasound technology to help guide a hollow needle into the amniotic sac. He or she will withdraw a small sample of fluid for lab analysis.
You may feel some cramping during or after the amniocentesis. Strenuous activities should be avoided for 24 hours following the procedure.
Women who are pregnant with twins or other higher-order multiples need sampling from each amniotic sac to study each baby. Depending on the position of the baby and placenta, amount of fluid, and woman’s anatomy, sometimes the amniocentesis cannot be done. The fluid is then sent to a genetics lab so that the cells can grow and be analyzed. AFP is also measured to rule out an open neural tube defect. Results are usually available in about 10 days to two weeks, depending on the lab.
Chorionic Villus Sampling (CVS)?
CVS is a prenatal test that involves taking a sample of some of the placental tissue. This tissue contains the same genetic material as the fetus and can be tested for chromosomal abnormalities and some other genetic problems. Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
How is CVS performed?
CVS may be offered to women with an increased risk of chromosomal abnormalities or who have a family history of a genetic defect that is testable from the placental tissue. CVS is usually performed between the 10th and 13th week of pregnancy. Although exact methods may vary, the procedure involves the following steps:
-
Your doctor will insert a small tube (catheter) through your vagina and into your cervix.
-
Using ultrasound technology, your doctor will guide the catheter into place near the placenta.
-
Your doctor will remove some tissue using a syringe on the other end of the catheter.
Your doctor may also choose to perform a transabdominal CVS, which involves inserting a needle through your abdomen and into your uterus to sample the placental cells. You may feel some cramping during and after either type of CVS procedure. The tissue samples are sent to a genetic lab for growth and analysis. Results are usually available in about 10 days to two weeks, depending on the lab.
What if CVS is not possible?
Women with twins or other higher-order multiples usually need sampling from each placenta. However, because of the complexity of the procedure and the positioning of the placentas, CVS is not always feasible or successful with multiples.
Women who are not candidates for CVS or who did not get accurate results from the procedure may require a follow-up amniocentesis. An active vaginal infection, such as herpes or gonorrhea, will prohibit the procedure. In other cases, the doctor may take a sample that does not have enough tissue to grow in the lab, generating incomplete or inconclusive results.
Fetal Monitoring
During late pregnancy and labor, your doctor may want to monitor the fetal heart rate and other functions. Fetal heart rate monitoring is a method of checking the rate and rhythm of the fetal heartbeat. The average fetal heart rate is between 120 and 160 beats per minute. This rate may change as the fetus responds to conditions in the uterus. An abnormal fetal heart rate or pattern may mean that the fetus is not getting enough oxygen or indicate other problems. An abnormal pattern also may mean that an emergency cesarean delivery is needed.
How is fetal monitoring performed?
Using a fetoscope (a type of stethoscope) to listen to the fetal heartbeat is the most basic type of fetal heart rate monitoring. Another type of monitoring is performed with a hand-held Doppler device. This is often used during prenatal visits to count the fetal heart rate. During labor, continuous electronic fetal monitoring is often used. Although the specific details of each procedure may vary, standard electronic fetal monitoring follows this process:
-
Gel is applied to your abdomen to act as a medium for the ultrasound transducer.

-
The ultrasound transducer is attached to your abdomen with straps so it can transmit the fetal heartbeat to a recorder. The fetal heart rate is displayed on a screen and printed onto special paper.
-
During contractions, an external tocodynamometer (a monitoring device that is placed over the top of the uterus with a belt) can record the pattern of contractions.
When is internal fetal monitoring needed?
On occasion, internal fetal monitoring is needed to provide a more accurate reading of the fetal heart rate. Your bag of waters (amniotic fluid) must be broken and your cervix must be partially dilated to use internal monitoring. Internal fetal monitoring involves inserting an electrode through the dilated cervix and attaching the electrode to the scalp of the fetus.
Glucose Testing
Glucose testing is used to measure the level of sugar in your blood.
A glucose challenge test is usually conducted between 24 and 28 weeks of pregnancy. Abnormal glucose levels may indicate gestational diabetes.
Abnormal glucose levels may indicate gestational diabetes.
What is involved in a glucose challenge test?
The initial one-hour test is a glucose challenge test. If the results are abnormal, a glucose tolerance test is needed.
How is a glucose tolerance test performed?
You may be asked to only drink water on the day the glucose tolerance test is given. Although the specific details of each procedure may vary, a typical glucose tolerance test includes the following steps:
-
An initial fasting sample of blood will be drawn from your vein.
-
You will be given a special glucose solution to drink.
-
Blood will be drawn at various times over the course of several hours to measure the glucose levels in your body.
Group B Strep Culture
Group B streptococcus (GBS) is a type of bacteria found in the lower genital tract of about 20 percent of all women. While a GBS infection does not usually cause problems in women before pregnancy, it can cause serious illness in mothers during pregnancy.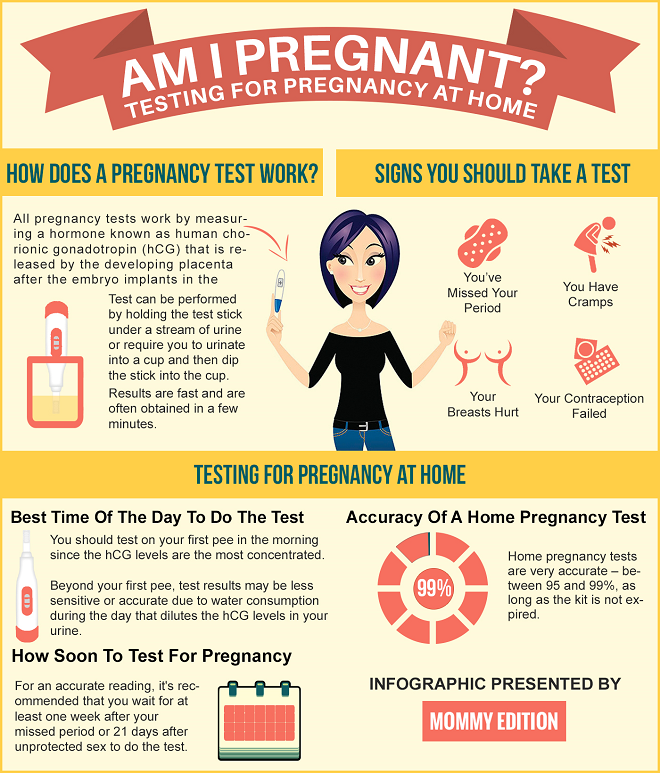 GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies contract the infection during pregnancy or from the mother’s genital tract during labor and delivery.
The Centers for Disease Control and Prevention recommends screening all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks gestation. The treatment of mothers with certain risk factors or positive cultures is important to reduce the risk of transmission of GBS to the baby. Babies whose mothers receive antibiotic treatment for a positive GBS test are 20 times less likely to develop the disease than those without treatment.
Routine Tests During Pregnancy | ACOG
Acquired Immunodeficiency Syndrome (AIDS): A group of signs and symptoms, usually of severe infections, in a person who has human immunodeficiency virus (HIV).
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Antibiotics: Drugs that treat certain types of infections.
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Bacteria: One-celled organisms that can cause infections in the human body.
Birth Defects: Physical problems that are present at birth.
Cells: The smallest units of structures in the body.
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Chlamydia: A sexually transmitted infection caused by bacteria. This infection can lead to pelvic inflammatory disease and infertility.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.
Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gene: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Gestational Diabetes: Diabetes that arises during pregnancy.
Glucose: A sugar in the blood that is the body’s main source of fuel.
Gonorrhea: A sexually transmitted infection that can lead to pelvic inflammatory disease, infertility, and arthritis.
Group B Streptococcus (GBS): A type of bacteria that many people carry normally and can be passed to the fetus at the time of delivery. GBS can cause serious infection in some newborns. Antibiotics are given during labor to women who carry the bacteria to prevent newborn infection.
Hepatitis B: An infection caused by a virus that can be spread through blood, semen, or other body fluid infected with the virus.
Hepatitis C: An infection caused by a virus that can be spread through infected blood.
Human Immunodeficiency Virus (HIV): A virus that attacks certain cells of the body’s immune system. If left untreated, HIV can cause acquired immunodeficiency syndrome (AIDS).
Immune: Protected against infectious disease.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.
Measles–Mumps–Rubella (MMR) Vaccine: A shot given to protect against measles, mumps, and rubella. The shot contains live viruses that have been changed to not cause disease. The shot is not recommended for pregnant women.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Rectum: The last part of the digestive tract.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rubella: A virus that can be passed to the fetus if a woman becomes infected during pregnancy. The virus can cause miscarriage or severe birth defects.
Sexually Transmitted Infections (STIs): Infections that are spread by sexual contact. Infections include chlamydia, gonorrhea, human papillomavirus (HPV), herpes, syphilis, and human immunodeficiency virus (HIV, the cause of acquired immunodeficiency syndrome [AIDS]).
Syphilis: A sexually transmitted infection (STI) that is caused by an organism called Treponema pallidum. This infection may cause major health problems or death in its later stages.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Tuberculosis (TB): A disease that affects the lungs and other organs in the body. TB is caused by bacteria.
Urinary Tract Infection (UTI): An infection in any part of the urinary system, including the kidneys, bladder, or urethra.
Vaccine: A substance that helps the body fight disease. Vaccines are made from very small amounts of weak or dead agents that cause disease (bacteria, toxins, and viruses).
Vagina: A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
What is a pregnancy test and how does it work - the blog of the medical center ON Clinic
The question of pregnancy planning has always been relevant in the life of every woman. In the past, confirmation of the fact of motherhood was carried out 2-3 months after fertilization. Modern tests make it possible to confirm or deny pregnancy after 7-10 days.
What is a pregnancy test and how does it work?
Pregnancy tests detect the presence of human chorionic gonadotropin (hCG) in a woman's urine or blood. This hormone begins to be actively produced by the membranes of the embryo 6-8 days after fertilization. It is during these periods that the egg penetrates the walls of the uterus. In a non-pregnant woman, the normal level of the hormone is below 5 mIU / ml and the tests do not respond to it. As soon as a woman begins to bear a future fetus, the concentration of the substance begins to increase sharply, to which the tests respond with a positive result.
This hormone begins to be actively produced by the membranes of the embryo 6-8 days after fertilization. It is during these periods that the egg penetrates the walls of the uterus. In a non-pregnant woman, the normal level of the hormone is below 5 mIU / ml and the tests do not respond to it. As soon as a woman begins to bear a future fetus, the concentration of the substance begins to increase sharply, to which the tests respond with a positive result.
What types of pregnancy tests are available?
There are 2 main types of pregnancy tests: urine and blood tests. Urinalysis is the most practical and convenient, since it can be performed at home. In the pharmacy chain and on the shelves of supermarkets, you can see a wide variety of testers of different price categories. They differ among themselves in the level of sensitivity to hCG.
The more expensive ones respond to relatively low levels of hormone levels (10 mIU / ml), and, therefore, allow you to clarify the fact of motherhood at an earlier date - 7 days after conception (5 days before the delay). A positive result from cheaper testers should be expected from 1-3 days of delay in menstruation, when the concentration of the hormone in the urine will be at least 25 mIU / ml.
A positive result from cheaper testers should be expected from 1-3 days of delay in menstruation, when the concentration of the hormone in the urine will be at least 25 mIU / ml.
Pregnancy tests also differ in how they are used:
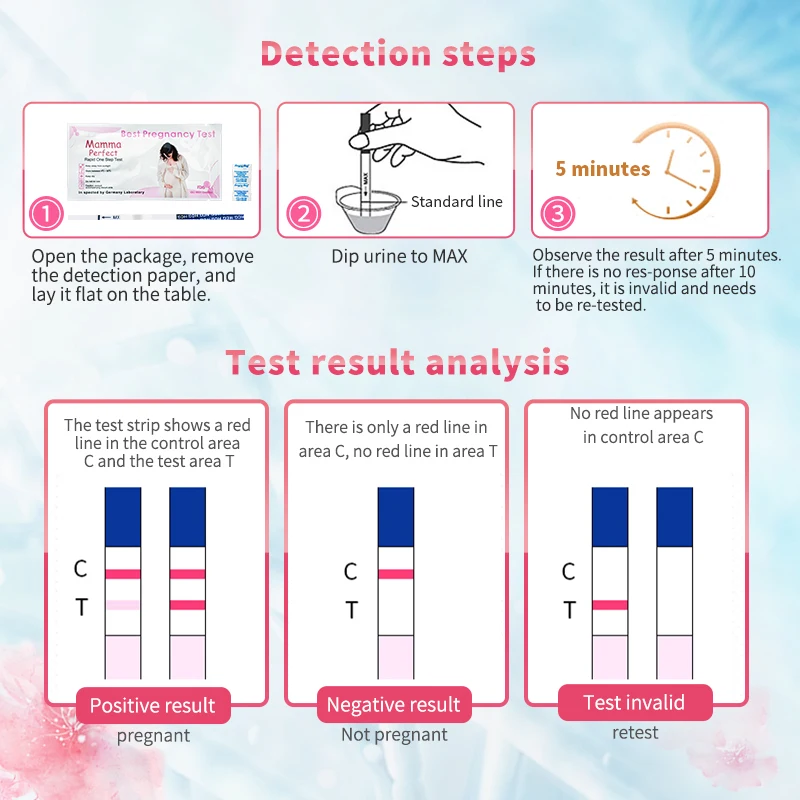
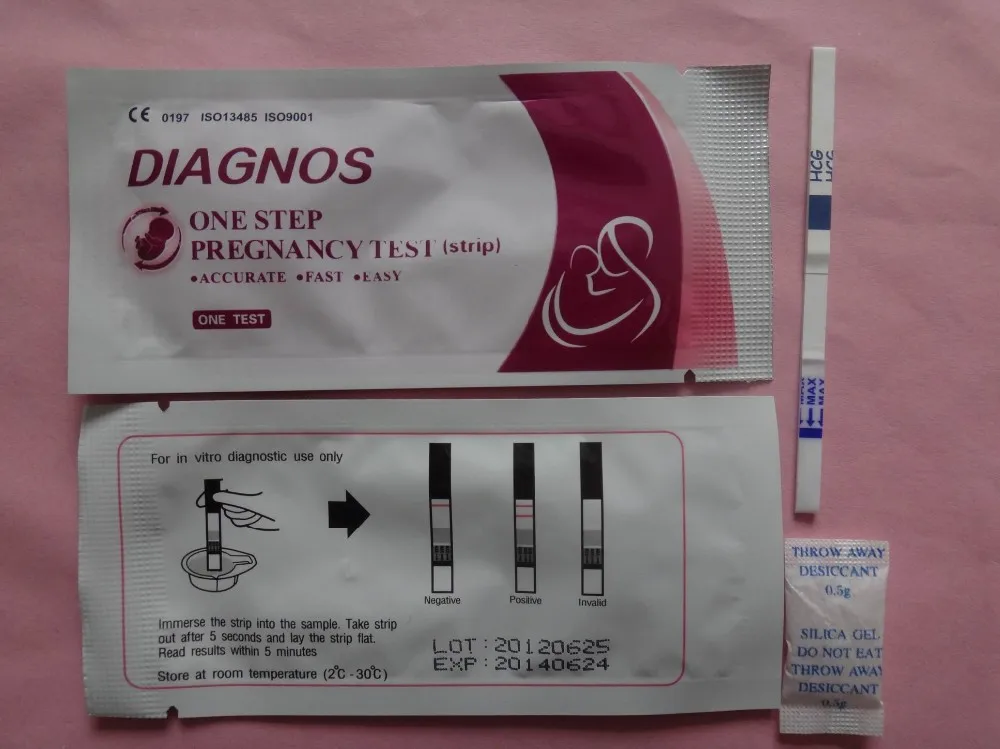
- test strips. They are the most popular option to use. They are impregnated with special reagents that perceive hCG. They must be lowered into a container with urine to a certain mark and wait a few seconds. The result should be expected after 5 minutes, but not later than 10;
- jet tests. For its implementation, there is no need to collect urine. It is enough to hold it under a stream of urine for a few seconds and wait for the result;
- tablet test. This option is a strip placed in a plastic tablet with two windows. In one of them, a small amount of urine is placed using a pipette. In the next window, the result will be visible in a few minutes;
- electronic test. It is the most accurate of all the previous ones.
 The principle of its operation is similar, but the result is displayed on the screen.
The principle of its operation is similar, but the result is displayed on the screen.
Is it difficult to do a pregnancy test at home?
Testing at home is not difficult. It can be purchased at any pharmacy without a prescription or in a supermarket. In addition to being affordable, the tests are highly accurate. The main task in their implementation is to strictly adhere to the instructions. The correct result should be expected after the time interval indicated in the instructions. A result that appeared earlier or later than the specified time is not correct. If a woman has doubts about the reliability of the result, then it is better to contact a gynecologist.
How accurate are pregnancy tests?
Home tests do not give a full guarantee of obtaining a reliable result, mistakes sometimes happen. To achieve more accurate data and minimize possible errors, the following rules must be observed:
- Pregnancy tests should preferably be carried out in the morning, since the greatest amount of the hormone is concentrated in the urine during the night;
- the test must not be exposed to dirt or moisture before the urinalysis;
- it is unacceptable to use the test after the expiration date;
- foreign matter must not enter the urine sample;
- test kit should be stored between 2 and 28°C;
- when performing the test, you must strictly follow the instructions.

HCG blood test
In addition to home tests, doctors recommend taking a blood test. It is more informative, since the concentration of the hormone in the blood is several times higher than in the urine. The study allows you to detect pregnancy earlier than urine tests, but it takes more time to complete.
There are 2 main types of hCG blood test:
- qualitative. Answers the question: is the level of the hormone elevated or not, which indirectly suggests the presence or absence of pregnancy in a woman;
- quantitative (beta hCG). This analysis reflects the exact concentration of a substance in the blood, so that the doctor can control hormonal changes in dynamics.
To obtain correct blood test results, the following rules must be observed:
- the analysis is performed strictly on an empty stomach in the morning;
- Alcohol, physical activity, and smoking should be completely avoided 12 hours before the test;
- water is allowed on the morning of the test;
- all medications should be avoided.
 If this is not possible, the laboratory and the physician should be notified.
If this is not possible, the laboratory and the physician should be notified.
Determining pregnancy is not the only task of a hCG blood test. As noted earlier, during the formation and development of the embryo, the level of the hormone in the woman's body should gradually increase - up to 12-13 weeks of pregnancy. If, with regular monitoring, an increase in the hCG indicator is not observed or the hormone level does not correspond to the generally accepted standard values for a specific period, then this may indicate the development of a missed or ectopic pregnancy, a high probability of miscarriage.
At a later date, the quantitative determination of hCG can be used as a screening for genetic disorders in the fetus (Down or Edwards syndrome). An important role is also played by the determination of beta-hCG. If a woman has an elevated level of this hormone, and no other characteristic signs of pregnancy are observed, tumor diseases should be suspected.
What do pregnancy test results mean?
If the test is positive, it is more likely that the woman is pregnant. Unfortunately, not always a positive response to a blood or urine test indicates a pregnancy. Such an analysis result is referred to as a false positive. In this case, it is extremely important to find the reason that led to such changes in indicators. It can occur in the following diseases and situations:
Unfortunately, not always a positive response to a blood or urine test indicates a pregnancy. Such an analysis result is referred to as a false positive. In this case, it is extremely important to find the reason that led to such changes in indicators. It can occur in the following diseases and situations:
- hormone-producing tumors - choriocarcinorma, hydatidiform mole;
- Dysfunctional pathologies of the ovaries;
- ectopic pregnancy;
- after spontaneous miscarriage or abortion;
- a woman taking tranquilizers, anticonvulsants, and medicines containing hCG;
- if there is protein or blood in the urine.
If a woman gets a negative test result, she is most likely not pregnant. However, there are situations when the test can "deceive" and in fact the woman is pregnant. This result of the study is called a false negative. It is more common than false positive and the reasons for its appearance lie in the following:
- test expired;
- the test was performed too early and its sensitivity is not enough to detect an increase in hCG levels;
- instructions not followed;
- the woman drank a large amount of liquid before the diagnosis, which caused the urine to become more dilute;
- insufficient amount of hCG is excreted in the urine due to impaired renal function;
- for pathologies of the cardiovascular system;
- the woman is taking diuretics or antihistamines.

A negative result is not complete proof that you are not pregnant. In this case, it is recommended to repeat the test again. It should be noted that the diagnostic capabilities of a blood and urine test for pregnancy should not be overestimated. Their implementation is only one of the diagnostic stages of establishing the fact of pregnancy. The tests do not provide information about the location of the pregnancy. And as already known, the level of the hormone in the ectopic location of the embryo also increases.
In order to clarify the localization of pregnancy and, in general, about its presence and normal course, doctors definitely recommend an ultrasound scan. Ultrasound of the uterus and its appendages does not require complex preparation. To perform an ultrasound with a vaginal probe, empty the bladder, and when using a surface probe, drink 2-3 glasses of non-carbonated water an hour before the examination.
Regardless of the results of the research, you should not draw independent conclusions and conclusions.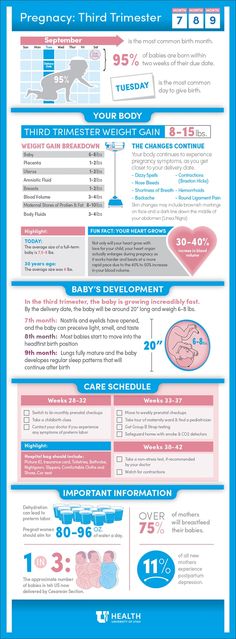 You should always consult your doctor for any questions. A thorough examination by a gynecologist will make a comprehensive assessment of the woman's health status and the presence of pregnancy.
You should always consult your doctor for any questions. A thorough examination by a gynecologist will make a comprehensive assessment of the woman's health status and the presence of pregnancy.
Popular questions
1. What diseases can cause a positive pregnancy test?
A false positive pregnancy test may be due to an increase in the level of human chorionic gonadotropin (hCG) as a result of diseases such as ovarian or corpus luteum cyst, ovarian cancer. A false test result can also occur with kidney pathologies, accompanied by the appearance of blood or leukocytes in the urine, urinary tract infections. In rare cases, the cause of a false positive pregnancy test may be diseases of the pituitary gland.
2. Where do I go with a positive pregnancy test?
If the pregnancy test is positive, you need to make an appointment with a gynecologist. The doctor will conduct a diagnosis (examination in the gynecological chair, ultrasound of the pelvic organs) to confirm or deny the presence of pregnancy, determine its localization (uterine, ectopic) and duration.
3. Why should I take a pregnancy test in the morning?
A pregnancy test taken in the morning is more accurate (assuming you haven't peed at night or drunk a lot of water). The first portion of morning urine is the most concentrated - during the night it accumulates a sufficient amount of human chorionic gonadotropin (hCG), which makes it possible to determine pregnancy at the earliest possible date.
Article rating:
4.5 out of 5 based on 4 ratings
Ask your question to the gynecologist
"ON Clinic"
How home pregnancy tests work
Mikhalina Akulova
nanobiotechnologist
When used correctly, home tests can accurately determine whether a woman is pregnant or not.
We tell you how these tests work, how they differ from laboratory tests, and what needs to be done to get a reliable result.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is a pregnancy test
Rapid pregnancy tests are test strips and other medical devices that allow you to understand at home whether a woman is pregnant or not. They can be different: paper, plastic and even electronic, but the principle of operation is the same for all. There are also laboratory pregnancy tests.
Human chorionic gonadotropin, or hCG, is used as a marker in all pregnancy tests. This is a hormone that is intensively produced from the first hours of pregnancy. As it develops, its concentration in the blood and urine increases.
HCG level - American Academy of Pregnancy Management
It increases daily and peaks around the eighth to eleventh week. Then it starts to slowly decline.
HCG - Medscape
Non-pregnant women and men have very little hCG in the norm: it should be no more than 2 IU / l in the blood. For comparison, during pregnancy it is more than 25 IU / l.
For comparison, during pregnancy it is more than 25 IU / l.
hCG can be measured:
- In the blood - this will be a laboratory test that is carried out in a medical institution.
- In urine - this is how home tests work, which can be done anywhere.
How rapid home pregnancy tests work
Home pregnancy tests work on the basis of immunochromatographic analysis. The same principle is based, for example, on rapid tests for coronavirus infection.
Pregnancy Testing - NHS
The absorbent portion of the test is coated with special dye bound proteins. If hCG is present in the urine, it will bind to these proteins, resulting in the formation of colored complexes.
Evolution of Lateral Flow Immunoassay Systems - Lateral Flow Immunoassay Book
With the flow of liquid, these complexes will rise higher - to the test strip. There are already other proteins that will “catch” the colored hCG complexes, and the strip will appear on the test.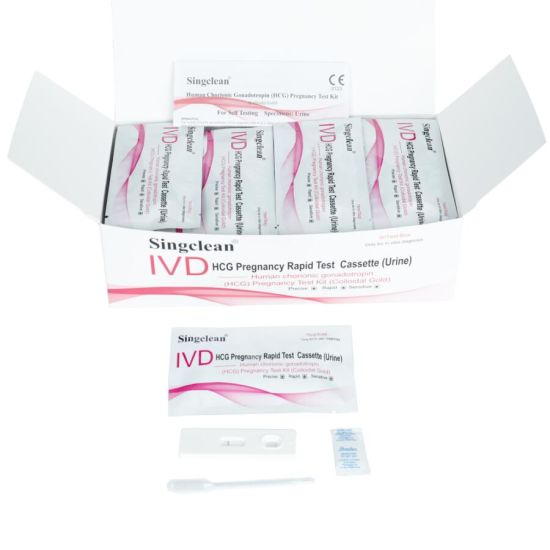 If there is no or too little hCG in the urine, this strip will not appear.
If there is no or too little hCG in the urine, this strip will not appear.
The second - control - strip contains proteins of the third group, which already bind to the pure colored protein, without hCG. This strip appears regardless of the result of the control and confirms that the test is not damaged.
If the woman is not pregnant, there will be one line on the test. And if there is a pregnancy, then two.
All pregnancy tests work according to this principle, even if they do not look like a test strip at all.
This is how home pregnancy tests work: in the reaction zone, hCG binds to colored complexes, then they settle in the test zone. And particles of colored protein settle in the control zone. This is how home pregnancy tests work: in the reaction zone, hCG binds to colored complexes, then they settle in the test zone. And in the control zone particles of colored protein settleHow home pregnancy tests differ from laboratory ones
The main advantage of home pregnancy tests over laboratory ones is that they can be done anywhere.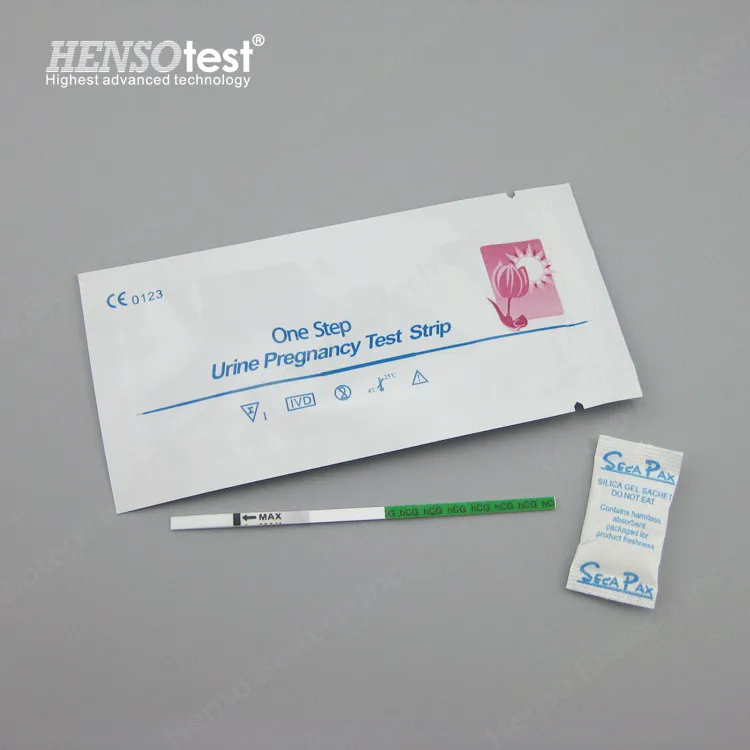 They are freely sold in pharmacies and supermarkets.
They are freely sold in pharmacies and supermarkets.
At the same time, they have slightly less sensitivity. So, a laboratory analysis can determine an increase in the level of hCG already on the sixth or eighth day after conception, and most home ones - on the 12th-14th day after conception, usually already after a missed period.
Some home tests can be used up to four days before the expected period, but their accuracy in this case is reduced to 65%.
Although some expensive rapid tests may indicate the estimated gestational age, the doctor will most likely ask for a blood test for hCG or an ultrasound to clarify.
/list/gynecology/
17 important questions for gynecologist Tatyana Rumyantseva
Comparison of two methods for determining pregnancy
| Laboratory blood test | Home pregnancy test | |
|---|---|---|
| Price | About 500 R | About 150 R |
| Precision | Accurate; can determine the duration of pregnancy | Not as accurate; some tests show an approximate period of |
| Done | In a laboratory or health facility | Anywhere |
| Result | After a few hours or even days | A few minutes later |
Laboratory blood test
Price
About 500 R
Accuracy
Accurate; You can determine the gestational age
in the laboratory or medical institution
result
after a few hours or even days
Pregnancy Home
Price
about 150 p
accuracy is not so accurate; some tests show an approximate term of
Done
Anywhere
Result
In a few minutes
What are the pregnancy tests for home use
Test strips. Show the result as a bar. For analysis, you need a container for collecting urine. The test is lowered into the container with urine to a certain level, wait a few seconds, then removed. You will see results in about 10 minutes.
Show the result as a bar. For analysis, you need a container for collecting urine. The test is lowered into the container with urine to a certain level, wait a few seconds, then removed. You will see results in about 10 minutes.
Test cassettes. Similar to test strips but requires less urine. The test itself is in a plastic package with two windows. A little urine is dripped into one of them with a pipette. In another, after the time specified by the manufacturer, the result will appear.
9 useful applications for pregnant women
Jet tests. The result will be indicated as a bar or plus sign, no urine container needed. Such a test must be held under a stream of urine, and then wait for the result to appear.
Electronic or digital tests. The result will appear as text on the screen, sometimes the estimated gestational age will also be indicated. A urine container is not required. Some digital tests can be used four days before the expected period, that is, they are more sensitive than others.
Home pregnancy tests: can you trust the results? — Mayo Clinic
When to Take a Pregnancy Test
Because pregnancy tests rely on the concentration of hCG in the urine, they should not be taken immediately after unprotected intercourse. You need to wait for the moment when pregnancy occurs and the concentration of the hormone rises to a level when the test can recognize it.
Pregnancy takes some time: up to six days until the egg is fertilized, and then another five days before it is implanted in the uterine wall. From that moment on, pregnancy has come, hCG begins to rise - and after a few more days, tests can detect pregnancy.
/analiz-hgch/
HCG blood test: when to donate and how much it costs
Most home tests will work already on the first or second day of the expected menstruation. There are ultra-sensitive options that promise results even earlier - five days before the delay.
If menstruation is irregular and a woman does not know when she has her period, then it is worth doing the test at least 21 days after unprotected intercourse.
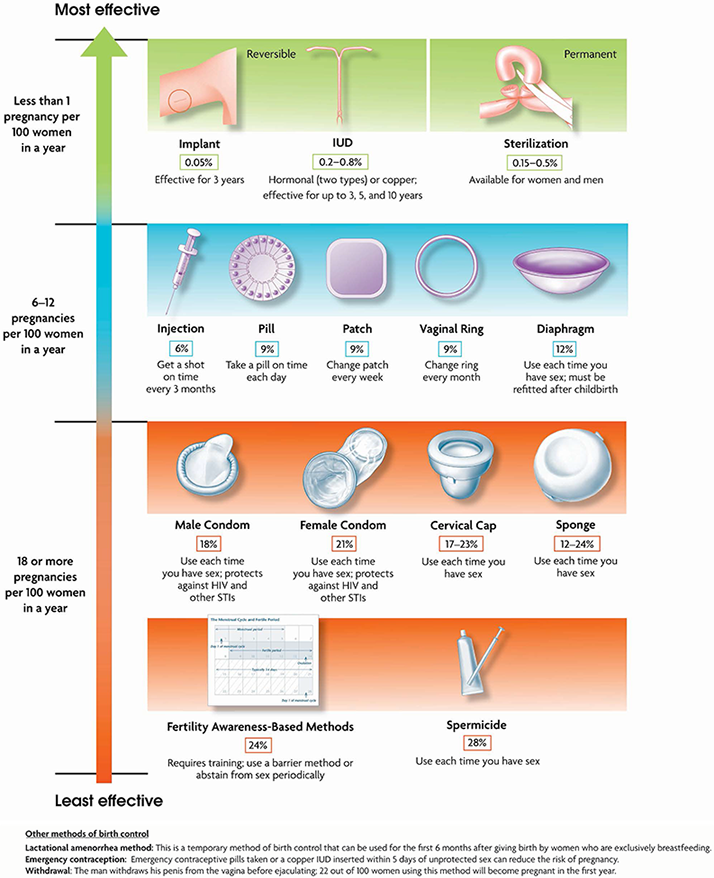
Contraceptive effectiveness - NHS
You should also check for pregnancy in case of changes in health, even if the couple is protected: with swelling or soreness of the breast, frequent nausea, pain in the abdomen. With any method of contraception, there is still some chance of getting pregnant. For example, when using condoms, it can reach 18%.
How accurate are home pregnancy tests? If pregnancy has occurred, then the test will be more accurate in the first days after the delay in menstruation, because then the level of hCG is higher.
If the test is taken too early, it is more difficult to determine the hormone in the urine and the error of the result is higher. That is why pregnancy tests, which can be done before a missed period, have an accuracy of about 65%.
8 reliable methods of contraception: from COCs to the intrauterine device
In addition, if a woman has irregular periods, it is possible to incorrectly determine the time of their onset and the length of the delay - this can also affect how accurate the result can be expected.
What can affect the results of a home test
When using rapid tests, it is important to carefully read the instructions and follow them. Then it will be possible to increase the reliability of the result. It is also worth checking the expiration date of the test. Expired ones can be returned to a pharmacy or store - the seller is obliged to return the money.
False negative. If the test result is negative, but menstruation still does not come, you can repeat it in three to four days. Perhaps the concentration of hCG in the urine was simply still very low.
A false-negative result for a correctly done test can be:
False positive. This is when there is no pregnancy, but a second strip appears on the test. This rarely happens, it is worth consulting a doctor, because it can be caused by some diseases.
This rarely happens, it is worth consulting a doctor, because it can be caused by some diseases.
A false-positive result in a correctly done test can be:
- when taking hormonal preparations containing hCG;
- recent termination of pregnancy, including spontaneous, when a woman has an imperceptible miscarriage at a very early stage. In this case, hCG may remain in the body, and the test will show a false positive result. This is called a biochemical pregnancy;
- ectopic pregnancy;
- cysts, some tumor and other diseases of the ovaries;
- menopause.
/list/ya-tebe-ne-veryu/
“Give birth and everything will pass”: 6 dangerous myths about women’s health do not affect the accuracy of rapid pregnancy tests.
How to use home pregnancy tests correctly
It is better to use morning urine, as it contains the maximum concentration of hCG, which means that you are more likely to get a reliable result. But this is not necessary, the test can be done during the day.
But this is not necessary, the test can be done during the day.
For some tests a few drops of urine are enough, for others it is important to dip the test strip in the liquid for 20-30 seconds. Be sure to check which parts of the dough cannot be wetted.
Especially with , it is important to observe the test time specified by the manufacturer. If you look at the test too early, the result may be a false negative because the reaction has not yet occurred.
/med-abort/
How I had a medical abortion
And if you look at the test too late, you will get a false positive result, because after the liquid evaporates, the dye appears anywhere on the strip.
If a control line does not appear on the test, it means that it does not work correctly and it is better to repeat the test again with another one.
How much do home rapid pregnancy tests cost
The price of a pregnancy test depends on the complexity of the design, the need to use additional containers and the reliability of the result.
In general, you can choose any home test that you feel comfortable using. The inkjet test does not require additional utensils, the digital one itself interprets the result, which reduces the likelihood of error and indicates the approximate gestational age. You will have to tinker with the test strip, but this option is cheaper than the others.
/pregnancy-plan/
How I spent on preparing for pregnancy during the pandemic 390,000 R
The cost of home pregnancy tests
| Test type | Average price |
|---|---|
| Digital test | 400 R |
| Test cassette | 195 Р |
| Jet test | 190 R |
| Test strip | 100-150 P |
Type of test
Average price
Digital test
400 R
Test cassette
195 r
Inflastic test
190 R
Test strip
100-150 R
Where to buy a high-quality pregnancy test
Pregnancy tests at a temperature of +2 .